Abstract
Purpose
To compare needle and microcannula injection techniques in regards to the microanatomical location of hyaluronic acid gel injected in the upper lip vermillion border of cadaver specimens.
Methods
The upper lip vermillion border was injected transcutaneously with hyaluronic acid gel in 8 fresh hemifaces of 4 female human cadavers. Each hemiface was injected by a single experienced injector, the right side using a 27-gauge microcannula and the left side using a 30-gauge needle. A 2cm region of each lip was excised lateral to a point 1cm lateral to the philtrum. Specimens were fixed in 95% alcohol, embedded in paraffin, and stained with hematoxylin and eosin for histologic examination.
Results
The majority of hyaluronic acid injected with either a needle or microcannula was located within the orbicularis oris muscle, and the remaining hyaluronic acid resided within the subcutaneous fat. In 3/4 right (microcannula) hemifaces, 100% of the hyaluronic acid was located within the muscle. Only 2/4 left (needle) hemifaces had at least 95% of the hyaluronic acid located within the muscle. Overall, in right (microcannula) hemifaces 93% of the filler was located within the muscle and in left (needle) hemifaces 79% of the filler was located within the muscle (p =0.14 ).
Conclusions
The majority of hyaluronic acid filler injected into the vermillion border after either microcannula or needle injection resides within the orbicularis oris muscle rather than in a subcutaneous/submucosal location. Injection with a microcannula shows a trend for more uniform intramuscular location compared to needle injection.
Introduction
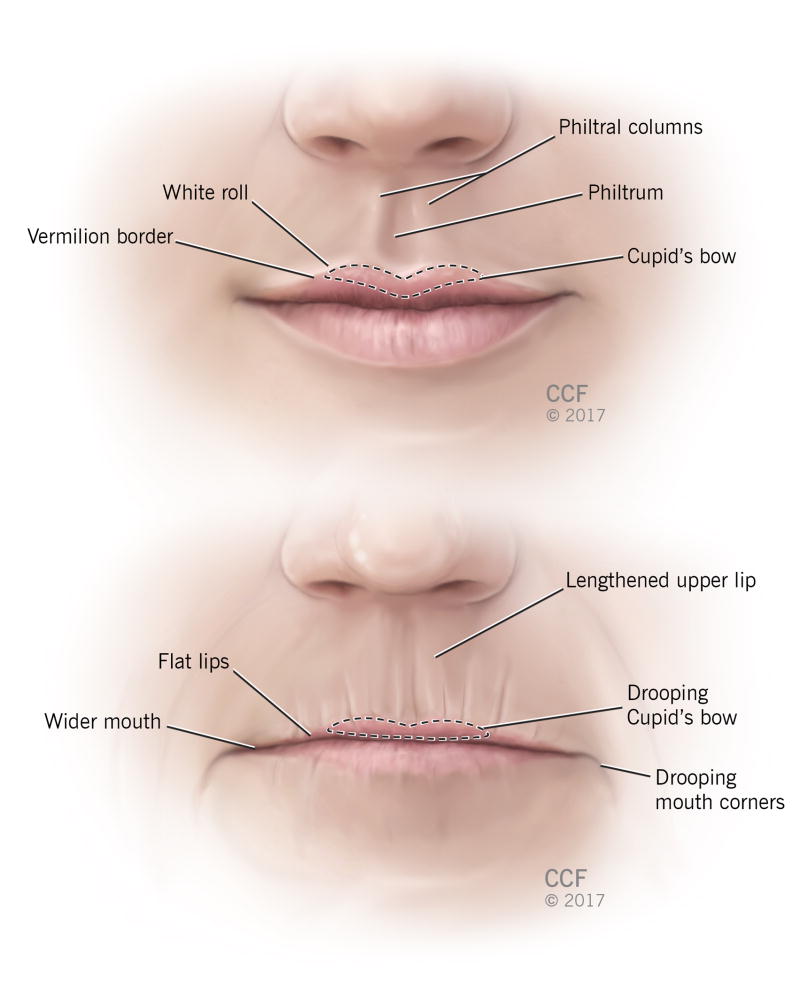
Small gel-particle hyaluronic acid (HA) fillers safely and effectively augment lip volume to improve several anatomic changes associated with aging.1, 2 Senescent changes of the lip include both volume related changes such as fat atrophy and maxillary bone loss, as well as other changes, including weakened orbicularis oris strength, actinic skin changes and ptosis of the malar fat pad and oral commissures (FIG. 1).3 Hyaluronic acid fillers can help restore several characteristics of the youthful aesthetic lip, including a full red lip, a pronounced central “lazy M” configuration within the Cupid's bow and accentuation of the “white roll” of the vermillion border of the upper lip (FIG. 1).4
Figure 1.
Features of the Aged (top) and Youthful upper lip.
Similar to the orbicularis oculi muscle, the orbicularis oris consists of three concentric aspects: the musculus incisivus, the pars peripheralis, and pars marginalis. The musculus incisivus arises superiorly from the inferior maxilla and inserts into the dermis in the upper philtral area and nasal spine. The pars peripheralis is more posterior and confined to the lip outside the vermillion border and the pars marginalis is more anterior and confined within the lip vermillion.5-7 The vermillion border may not absolutely delineate the muscle divisions and the pars marginalis may extend outside the vermillion border up to 2.5mm.8
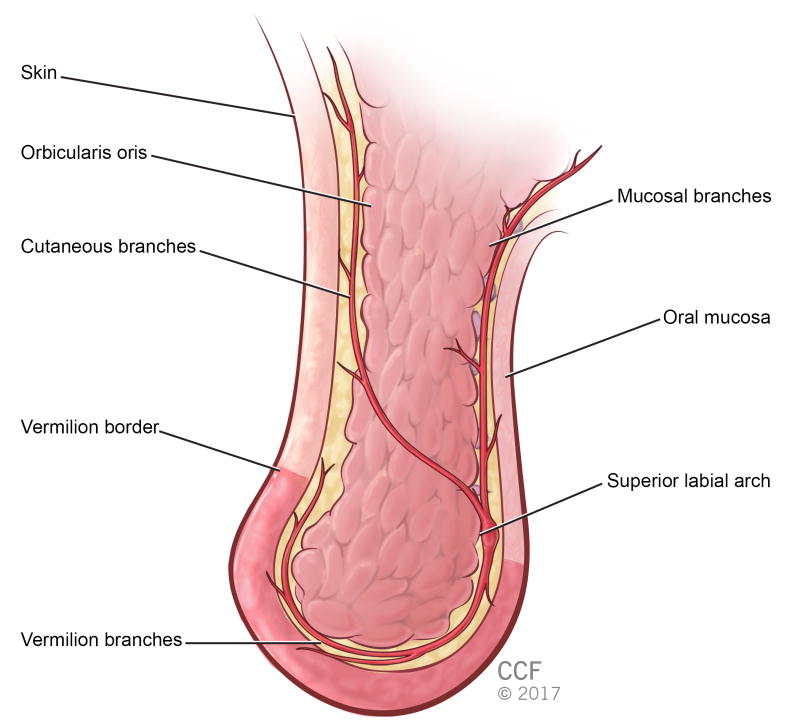
Proper placement and depth of injection determines the aesthetic and functional outcome.9 Too superficial of an injection may lead to a “speed bump” appearance of the upper lip, while too deep an injection may fail to accentuate the white roll of the lip. The lip also contains the superior labial artery, which must be avoided during injection (FIG. 2). One potential variable in the position of HA gel is the use of either a microcannula or a needle.
Figure 2.
Sagittal cross-section of upper lip showing posterior location of superior labial artery.
While the depth of injection represents a critical factor in HA gel lip augmentation, few studies have actually investigated the location of the gel after injection. One study using optical coherence tomography and ultrasonography found both subcutaneous and intramuscular HA gel after injecting the deep red lip, the vermillion border, and the philtrum using sharp and non-blunt cannulas.10 The authors did not specifically evaluate the location of filler after injection along the vermillion border, and they noted significant limitations in the non-invasive methods used to localize the filler.10 While histologic studies exist to show the location of HA gel fillers injected into the brows, tear trough, temple, and nasolabial folds, to our knowledge, no studies exist to determine the microanatomical location of HA gel fillers after injection into the vermillion border.9, 11-13 We sought to determine the position of HA gel using tissue histology after transcutaneous injection into the vermillion border using either a microcannula or a needle.
Methods
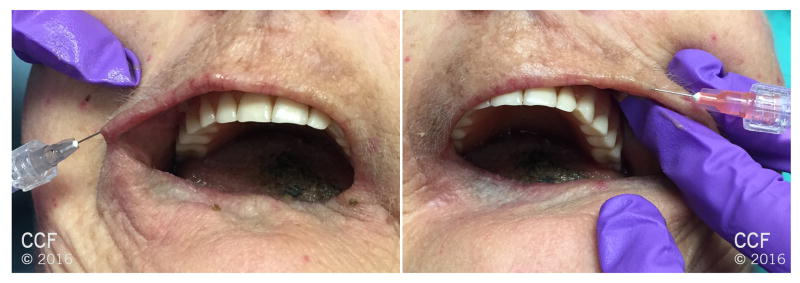
Four consecutive intact fresh human female cadaver heads (8 hemifaces) were selected for inclusion. Cadaver age upon death, gender, BMI, and race were recorded. An experienced oculofacial plastic surgeon (C.J.H) injected each side of each upper lip with 0.1 mL of Restylane (Galderma Laboratories, L.P., Fort Worth, TX, U.S.A.). For microcannula injections, an oblique stab incision through the skin was created with a 25-Gauge needle at the white line of the upper lateral oral commissure. The 27-gauge microcannula was then inserted into the oblique stab incision without the use of a trochar. For the ½ inch, 30-gauge needle injections, the needle was inserted into the white line at a similarly oblique angle, at 2-3 equidistant intervals (based on the length of the lip) between the lateral commissure and the philthrum. For both the microcannula and needle injections, the tip was advanced parallel to the skin surface, approximately 1-2mm deep within the white line, and filler injected in a retrograde threading fashion. All injections were performed by the same experienced injector (CJH) (Figure 3).
Figure 3.
Photograph depicts a cadaver undergoing HA injection into the white roll at the vermillion border of the upper lip using a microcannula (left image) and a 30-gauge needle (right image)
Following injection, dissection was performed to excise the soft tissues of the upper lip. The skin was incised with a #15 blade approximately 1cm from the oral commissure laterally and 1 cm from the philtrum medially in an approximately 2cm × 2cm block extending to the maxillary bone superiorly. The medial border of the specimen was tagged with a 4-0 polypropylene suture. Care was taken to avoid handling of tissue near the vermillion border.
The tissue blocks were fixed in 95% alcohol for 12 days according to previously published methods studying the microanatomic location of HA gel.11-13 The specimens were then embedded in paraffin and 4 μm sections were utilized for histologic analysis. The sections were stained with hematoxylin and eosin and examined under light microscopy to determine the histopathologic location of the HA gel. The percentage of filler was determined by visual inspection and estimation using a technique similar to that described by Markin et al for hepatic adiposity.14 This technique has also been used for several histologic studies of periocular tissues, including a study measuring the location of HA gel filler injected in the temporal region.13
A paired T-test was used to compare the percent of intramuscular HA gel between the microcannula and needle group. Statistical significance was defined as a p-value < 0.05.
Results
The average age of injected cadavers was 71 years old (range 66-77 years old) and all were Caucasian. The average BMI at time of death was 26.5 (range 20-34). After careful histologic examination, hyaluronic acid gel was identified in all specimens. In 7 of 8 specimens, the vast majority of the HA gel was found within the orbicularis oris muscle. In 3 of 4 specimens in the microcannula group 100% of the HA gel was intramuscular (Figure 4). In 2 of 4 specimens in the needle group, more than 95% of the HA gel was intramuscular. In 1 of 4 specimens in the needle group, only 40% of the HA gel was intramuscular while 60% was in the subcutaneous fat (Figure 4). There was no evidence of intrarterial HA gel, or arterial compression from gel, in any of the 8 specimens. Although there was a trend toward a higher percent present intramuscularly in the microcannula group, it was not statistically significant (p=0.14).
Figure 4.
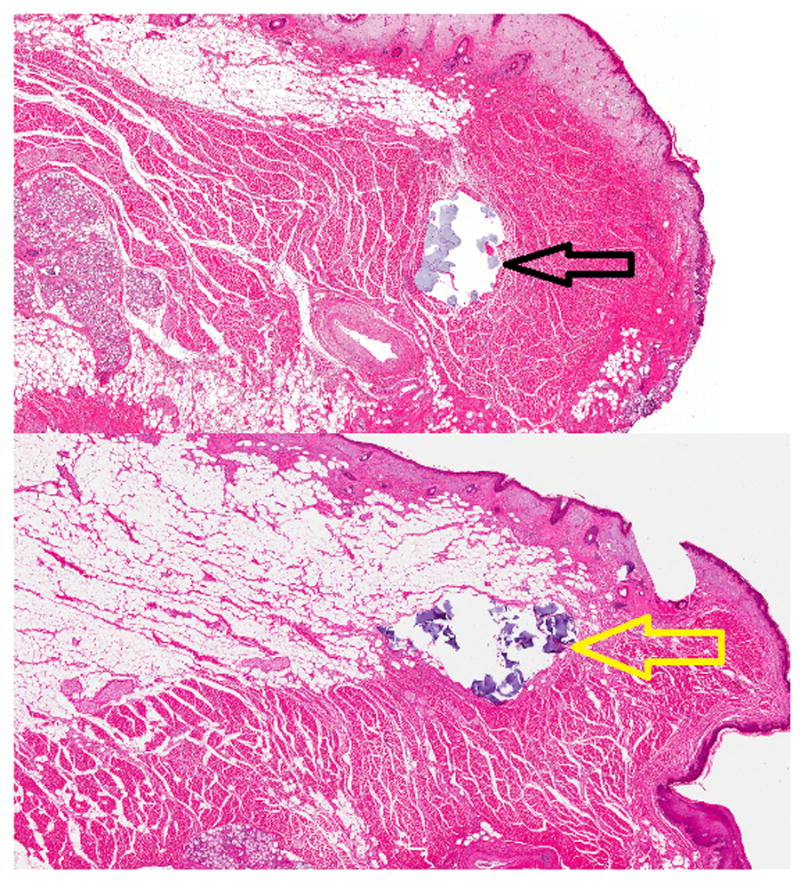
(Top) Representative hematoxylin and eosin stain showing intramuscular HA gel (black arrow) after injection with a microcannula. (Bottom) Hematoxylin and eosin stain showing both intramuscular HA gel and within the subcutaneous fat (yellow arrow) in one cadaver injected using a 30-gauge needle (Hemiface N4 as seen in Table 1)
The distance of the HA gel to the mucocutaneous junction was also evaluated histologically and quantified. Three of the 4 microcannula specimens demonstrated HA gel > 1mm from the mucocutaneous junction with an average distance of 2.05mm. Only 1 of the 4 needle specimens showed HA gel > 1mm from the mucocutaneous junction with an average of 0.7mm. While there was a trend for the needle specimen HA gel to reside closer to the mucocutaneous junction, this was not statistically significant (p=0.09). Our results are summarized in Table 1.
Table 1. Demonstration of the percentage of total injected HA for both microcannula and needle within each upper lip hemiface tissue block.
| Hemiface C= cannula N= needle | % intramuscular (orbicularis oris) | % extramuscular (subcutaneous fat) | Distance to Mucocutaneous Junction (mm) | Artery Involved? |
|---|---|---|---|---|
| C1 | 100 | 0 | 1.25 | No |
| C2 | 100 | 0 | 1.65 | No |
| C3 | 100 | 0 | 3.30 | No |
| C4 | 70 | 30 | 2.00 | No |
| N1 | 80 | 20 | 1.30 | No |
| N2 | 95 | 5 | 0.35 | No |
| N3 | 100 | 0 | 0.75 | No |
| N4 | 40 | 60 | 0.40 | No |
Discussion
Senescent changes of the upper lip lead to loss of muscular volume and weakening of connective tissues, creating a flatter philtrum, decreased vertical height of the upper lip vermillion, and inversion of the upper lip into the oral cavity. These volume changes, coupled with actinic and elastic changes produce perioral rhytides. Hyaluronic acid gel augmentation addresses the volume-related aging changes of the upper lip.
HA gel fillers can augment both the lip vermillion and the white roll of the lip, and gel location determines both the functional and cosmetic outcome. The relatively posterior course of the superior labial artery, running 3.3- 7.6mm deep to the skin, allows for safe superficial injection of hyaluronic acid fillers within the vermillion border and anterior lip vermillion.15-17 While none of the gel was found within the superior labial artery, some sections demonstrated perivascular location of the product. Compression from gel filler may represent one mechanism of post-injection ischemia 13, especially toward the midline where anastomoses diminish and where the nasal septal branches are more superficial.1317 Augmentation of the medial lip should be approached with care.
Interestingly, we found that HA gel fillers injected transcutaneously to fill the vermillion border of the lip actually resided primarily in an intramuscular location, rather than a subcutaneous one. The high percentage of intramuscular HA gel may be a result of dehydration of the fresh cadaver skin and subcutaneous tissues. However, the fresh cadaver tissue posed no challenges to injection with either the needle or the cannula, and our results more likely illustrate that in vivo filler injections to the vermillion border result in filler placement deeper than previously expected. Another limitation to this study includes the small number of injected hemifaces; however, given the limited resources involved in studying fresh, non-frozen, non-preserved human cadavers, the n of this study was in line with other published cadaver studies of HA gel fillers.11-13 While the quantitative assessment was inexact, there are few ways to accurately measure histologic volumes, the method has been previously reported, and all cadavers demonstrated significant intramuscular location of filler.13, 14
Other factors may have contributed to the surprising location of the HA gel after intended injection into the vermillion border. Given the advanced age of the cadavers injected (mean, 71 years), it is possible that senescent changes resulted in subcutaneous fat atrophy, obliteration of the subcutaneous plane or other anatomic factors that precluded injection within the subcutaneous space. Our findings may have been different in a younger cadaver population. In a similar way, all cadavers were female and presumably postmenopausal, which may have produced changes to the lip that may not be applicable to other populations. Third, all cadavers were Caucasian and had an average BMI of 26.5 (range 20-34) at time of death. Results may be different in other ethnic groups and in patients with different body habitus. Despite these possibilities, it is patients with thinner lips that typically undergo volume augmentation, so some of the factors that produced intramuscular injection in this population may translate to other populations as well. Thinner lips may have more dense subcutaneous attachments or other factors that prevent injection into this plane.
While some data exist to support claims of less pain, less bruising, shorter recovery, less risk of intravascular injection, and better product distribution following microcannula injection compared to needle injection, little data exists regarding filler location after injection between the two techniques.18, 19 Although we identified a trend toward more uniform intramuscular injection using a microcannula compared to a needle for injection of the vermillion border, the difference was not statistically significant, and both techniques seem to produce relatively predictable filler location within the orbicularis oris muscle. We found adequate and similar cosmetic restoration of the white roll using the microcannula and the needle, despite significant and different amounts of unintended intramuscular location of gel filler with each technique.
It is interesting that the cannula produced more consistent distribution of filler, but that it deposited filler further from the intended subcutaneous plane compared to the needle injections. The single cannula injection, compared to multiple injection points required for the ½ inch needle, may account for the more consistent distribution of material using the cannula. While the cannula injections were more consistent, they produced a higher percentage of intramuscular filler. This may be due to the pointed shape of the 25 gauge stab incision needle exposing slightly deeper tissue planes, the blunt nature of the cannula decreasing tactile feedback to find the immediate subcutaneous plane, and/or dense subcutaneous attachments with a thin subcutaneous plane not allowing for placement of the blunt, larger cannula within the plane.
HA gel filler augmentation of the vermillion border may result in deeper filler location than previously expected, with the vast majority of the filler residing within the orbicularis oris muscle. This injection plane seems safe regarding the location of the superior labial artery, and both microcannula and needle injection seem to produce relatively predictable intramuscular location of the gel. Further studies regarding the location of HA gel fillers into the lip vermillion may provide more information to better tailor augmentation in this area. Further studies regarding the location of HA gel fillers into the lip vermillion, with the associated higher volumes required, may provide more information to better tailor augmentation in this area.
Acknowledgments
Financial support– This study was supported in part by the NIH-NEI P30 Core Grant (IP30EY025585-01A1) and Unrestricted Grant from The Research to Prevent Blindness, Inc, awarded to the Cole Eye Institute.
Footnotes
Proprietary interest statement– none of the authors have any conflict of interest to disclose.
References
- 1.Brandt F, Bassichis B, Bassichis M, et al. Safety and effectiveness of small and large gel-particle hyaluronic acid in the correction of perioral wrinkles. J Drugs Dermatol. 2011;10(9):982–7. [PubMed] [Google Scholar]
- 2.Smith SR, Vander Ploeg HM, Sanstead M, et al. Functional safety assessments used in a randomized controlled study of small gel particle hyaluronic acid for lip augmentation. Dermatol Surg. 2015;41(Suppl 1):S137–42. doi: 10.1097/DSS.0000000000000164. [DOI] [PubMed] [Google Scholar]
- 3.Kaur M, Garg R, Singla S. Analysis of facial soft tissue changes with aging and their effects on facial morphology: A forensic perspective. Egyptian Journal of Forensic Sciences. 2015;5(2):46–56. [Google Scholar]
- 4.Niamtu J. Rejuvenation of the lip and perioral areas. In: Bell W, Guerrero C, editors. Distraction Osteogenesis of the Facial Skeleton. 1st. Canada: BC Decker; 2007. pp. 38–48. [Google Scholar]
- 5.Lightoller GS. The facial musculature of the australian aboriginal: Part I. J Anat. 1926;61(Pt 1):14–39. [PMC free article] [PubMed] [Google Scholar]
- 6.Briedis J, Jackson IT. The anatomy of the philtrum: Observations made on dissections in the normal lip. Br J Plast Surg. 1981;34(2):128–32. doi: 10.1016/s0007-1226(81)80077-x. [DOI] [PubMed] [Google Scholar]
- 7.Rogers CR, Mooney MP, Smith TD, et al. Comparative microanatomy of the orbicularis oris muscle between chimpanzees and humans: Evolutionary divergence of lip function. J Anat. 2009;214(1):36–44. doi: 10.1111/j.1469-7580.2008.01004.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hwang K, Kim DJ, Hwang SH. Musculature of the pars marginalis of the upper orbicularis oris muscle. J Craniofac Surg. 2007;18(1):151–4. doi: 10.1097/01.scs.0000248649.77168.ec. [DOI] [PubMed] [Google Scholar]
- 9.Arlette JP, Trotter MJ. Anatomic location of hyaluronic acid filler material injected into nasolabial fold: A histologic study. Dermatol Surg. 2008;34(Suppl 1):S56, 62. doi: 10.1111/j.1524-4725.2008.34244.x. discussion S62-3. [DOI] [PubMed] [Google Scholar]
- 10.Vent J, Lefarth F, Massing T, et al. Do you know where your fillers go? an ultrastructural investigation of the lips. Clin Cosmet Investig Dermatol. 2014:7191–9. doi: 10.2147/CCID.S63093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Griepentrog GJ, Lucarelli MJ. Anatomical position of hyaluronic acid gel following injection to the eyebrow. Ophthal Plast Reconstr Surg. 2013;29(5):364–6. doi: 10.1097/IOP.0b013e31829a72bd. [DOI] [PubMed] [Google Scholar]
- 12.Griepentrog GJ, Lemke BN, Burkat CN, et al. Anatomical position of hyaluronic acid gel following injection to the infraorbital hollows. Ophthal Plast Reconstr Surg. 2013;29(1):35–9. doi: 10.1097/IOP.0b013e318272d4b0. [DOI] [PubMed] [Google Scholar]
- 13.Chundury RV, Weber AC, McBride J, et al. Microanatomical location of hyaluronic acid gel following injection of the temporal hollows. Ophthal Plast Reconstr Surg. 2015;31(5):418–20. doi: 10.1097/IOP.0000000000000507. [DOI] [PubMed] [Google Scholar]
- 14.Markin RS, Wisecarver JL, Radio SJ, et al. Frozen section evaluation of donor livers before transplantation. Transplantation. 1993;56(6):1403–9. doi: 10.1097/00007890-199312000-00025. [DOI] [PubMed] [Google Scholar]
- 15.Magden O, Edizer M, Atabey A, et al. Cadaveric study of the arterial anatomy of the upper lip. Plast Reconstr Surg. 2004;114(2):355–9. doi: 10.1097/01.prs.0000131876.45116.77. [DOI] [PubMed] [Google Scholar]
- 16.Tansatit T, Apinuntrum P, Phetudom T. A typical pattern of the labial arteries with implication for lip augmentation with injectable fillers. Aesthetic Plast Surg. 2014;38(6):1083–9. doi: 10.1007/s00266-014-0401-8. [DOI] [PubMed] [Google Scholar]
- 17.Lee SH, Gil YC, Choi YJ, et al. Topographic anatomy of the superior labial artery for dermal filler injection. Plast Reconstr Surg. 2015;135(2):445–50. doi: 10.1097/PRS.0000000000000858. [DOI] [PubMed] [Google Scholar]
- 18.Fulton J, Caperton C, Weinkle S, et al. Filler injections with the blunt-tip microcannula. J Drugs Dermatol. 2012;11(9):1098–103. [PubMed] [Google Scholar]
- 19.Berros P, Braz AV, Trevidic P, et al. Evolution in technique: Use of hyalurostructure for lips rejuvenation as an alternative to needle injection without troncular anesthesia. J Cosmet Laser Ther. 2013;15(5):279–85. doi: 10.3109/14764172.2013.803367. [DOI] [PubMed] [Google Scholar]