Highlights
-
•
We report two cases of type A intramural hematoma of the aorta.
-
•
We found radiological and intraoperative evidence of an intimal tear.
-
•
This finding supports the hypotesis that IMH belong to “aortic dissection” disease.
Keywords: Intramural hematoma, Aortic dissection, Intimal lesion, Case series
Abstract
Introduction
Aortic intramural hematoma (IMH) is described as “dissection without intimal tear” due to rupture of vasa vasorum, which results in bleeding within the tunica media in the absence of intimal disruption or blood flow communication. The aim of our study is to validate perioperative evidence of intimal entry tear in patients with IMH and to suggest that this entity may represent a part of a disease and not a separate disease.
Presentation of cases
We report two patients admitted to our institution with sudden onset thoracic pain. A CT scan showed an aneurysm of the ascending aorta complicated by type A IMH. The patients underwent open operation. Surgical set-up has included right axillary artery as arterial inflow, no cross-clamp before hypothermic circulatory arrest and Kazui protocol for selective antegrade cerebral perfusion. We found no evidence of intimal flap, but we identified an intimal tear in both patients. A hemiarch procedure associated with root replacement, using two-grafts techniques was performed in both cases. The postoperative course was uneventful and the patients were discharged home.
Discussion
Recent data are emerging from the radiologic literature about the evidence of intimal lesions in IMH, but surgical reports are scant. The evidence of intimal tears contributes to consider as questionable the etiological role of vasa vasorum and it may justify updates in the management.
Conclusion
We consider that IMH may represent a part of a disease (aortic dissection), depicted by radiological images in a specific single instant of its clinical evolution.
1. Introduction
Intramural hematoma (IMH) of the aorta is classically described as a “dissection without intimal tear”, due to rupture of vasa vasorum, with an incidence ranging from 10% up to 30% of all acute aortic syndromes [[1], [2]]. This disease represents a dynamic entity associated with polymorphic evolutions such as regression, progression to acute dissection (AD), expansion or rupture [3]. Recent radiological reports emphasize the evidence of an intimal tear in IMH, defined as “ulcer-like projection” (ULP) [[4], [5]]. This finding contributes to consider as questionable the etiological role of vasa vasorum and it may justify updates in the management.
The aim of our report is to validate the evidence of intimal entry tear in IMH and to suggest that this entity may represent a part of a disease and not a separate disease.
This work has been reported in line with the PROCESS criteria [6].
2. Presentation of cases
We report two consecutive cases of type A intramural hematoma of the aorta treated in our Institution (university hospital). CT images were evaluated with multiplanar (MPR) and volume rendering (VR) reconstructions, using the software “syngo.via” (Siemens Healthcare, Germany). Surgical set-up has included right axillary artery as arterial inflow, no cross-clamp before hypothermic circulatory arrest (HCA) and Kazui protocol for selective antegrade cerebral perfusion. The procedures were performed by two senior surgeons.
2.1. Case 1
82 years old male, hypertensive, admitted for sudden onset of thoracic pain. A contrast-enhanced computed tomography (CT) showed an aneurysm of the ascending aorta complicated by type A IMH, an ulcer-like projection (ULP) and pericardial effusion (Fig. 1A, B). The patient was promptly addressed to surgery.
Fig. 1.
A) Coronal unenhanced computed tomography (CT) image shows a crescent-shaped thickening of the aortic wall (arrowheads) with greater attenuation than the lumen, and pericardial effusion (circles). B) Sagittal contrast-enhanced CT image shows a localized blood-filled pouch (arrow) protruding into the intramural hematoma from the aortic lumen, characteristic for ulcer-like projection. C) Intraoperative findings of 2 cm transverse-shaped intimal tear (arrow) identified above the non-coronary sinus.
During HCA no intimal flap was evident, a fresh IMH placed 4 cm above the non-coronary sinus was evacuated and 2 cm transverse shaped intimal tear was identified (Fig. 1C). Hemiarch procedure associated with root replacement, using two-grafts techniques, was performed. The postoperative course was uneventfully and the patient was discharged home on 10th postoperative day (POD).
2.2. Case 2
78 years old female, hypertensive, referred to us with CT diagnosis of aneurysm of the ascending aorta complicated by type A IMH. The CT images showed the presence of an ULP in the ascending aorta 1 cm below the origin of brachiocephalic artery (Fig. 2A, B).
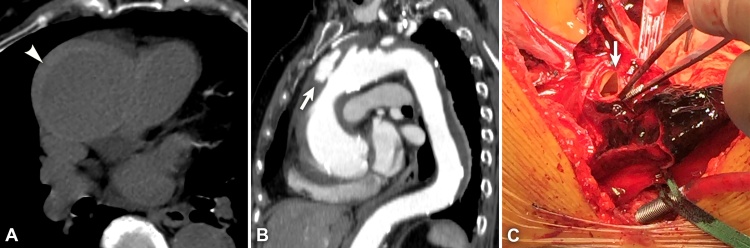
Fig. 2.
A) Axial unenhanced computed tomography (CT) image shows a crescent-shaped thickening of the aortic wall (arrowheads) with greater attenuation than the lumen. B) Oblique contrast-enhanced CT image shows a localized blood-filled pouch (arrow) protruding into the intramural hematoma from the aortic lumen, characteristic for ulcer-like projection. C) Intraoperative findings of 1.5 cm linear-shaped intimal tear (arrow) just below the origin of innominate artery.
During HCA hematoma was evacuated, no intimal flap was detected and 1.5 cm linear shaped intimal tear was identified 1 cm below the origin of brachiocephalic artery (Fig. 2C). Hemiarch procedure associated to root replacement using two-grafts technique was performed; the postoperative course was uneventfully and the patient was discharged home on 13th POD.
The two patients have been followed for the last three years, with a CT scan and an echocardiogram every six months for the first year, and every year in the next two years. No progression of the lesions were observed.
3. Discussion
The aforementioned theory, that defines IMH as a dissection without intimal tear due to the bleeding within the media in the absence of intimal disruption and blood flow communication, has not ever been validated scientifically. Moreover, the causative role of vasa vasorum appears as questionable because the pressure generated by their rupture seems too low to overcome the pressure existing in the inner lumen [7].
Some authors believe that all IMH are acute dissections with thrombosis of the false lumen and that an intimal tear is always present but not identified, consequently IMH could not exist [8]. Therefore, the major source of controversy is the mechanism that generates IMH.
Improvement in non-invasive diagnostic imaging, particularly multidetector computed tomography (MDCT), has permitted to identify lesions considered as intimal tears.
Kitai and Park, in two recent radiologic reports, have observed that IMH may partially result from an entry tear similar to classic AD rather than bleeding from the vasa vasorum [[4], [5]]. In Park experience, on a total of 37 patients with IMH, intimal defects were found in 12 cases [5]. In Kitai experience, on a total of 66 patients with IMH, 8 patients showed intimal defects in the ascending aorta in the follow-up studies [4]. These findings may imply another potential pathophysiology of IMH, such as an intimal defect with closed and thrombosed false lumen. Kitai has proposed that the term “AD with closed and thrombosed false lumen” would be better than “IMH” [9].
In our experience, patients have developed IMH as a complication occurred in an aortic aneurysm. These findings suggest that new intimal disruption of IMH may be also related to shear stress, considering that the ascending aorta and the arch are exposed to a greater hydraulic stress than the descending aorta.
In the radiological findings, a localized blood-filled pouch protruding from the true lumen into the thrombosed false lumen of the aorta is defined as ulcer-like projection (ULP) and it has been usually considered to represent the site of the intimal disruption [[4], [5]]. Moreover, the hypothesis of an entry tear is confirmed by the evidence of intimal communication documented at the time of surgery [[10], [11]].
Adding two new consecutive cases of IMH where the preoperative and intraoperative findings reveal the presence of an intimal tear, we believe that the elegant argumentation of Lansman has been demonstrated [7]. This author states that propagation of flow in the media is governed by two factors: the magnitude of the source and the resistance to flow in the media. If these factors yield restricted flow, then thrombosis occurs, and a discrete hematoma or IMH ensues; conversely, a large source of blood with low medial resistance will result in AD. Mukohara has recently confirmed Lansman's hypothesis, stating that the rupture of vasa vasorum in the aortic wall has never been seen by his pathologist [12].
4. Conclusion
Recent data are emerging from the radiologic literature about the evidence of intimal lesions in IMH, but surgical reports are scant. In our opinion and according to Estrera [11], we assume IMH as a moment of the same disease, represented by aortic dissection, depicted by radiological images in a specific single instant of its clinical evolution. Finally, considering that the natural history is dismal and surgical results are excellent [3], we suggest, according to Matsushita [13], a more aggressive approach reconsidering IMH as a part of one disease and not a separate disease. The publication of further case reports would be advisable. With a larger number of cases available, a review of the literature could confirm the aforementioned hypothesis.
Conflicts of interest
None.
Funding
None.
Ethical approval
Ethical approval has been exempted by our Institution.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Gianfranco Filippone: conception and design of the study, operator, paper drafting.
Giovanni Caruana: CT images editing and interpretation.
Claudia Calia, Violetta Moscaritolo: contribution to the writing process, comments.
Vincenzo Argano: proof-reading, comments, operator.
Registration of research studies
UIN 3220.
Guarantor
Gianfranco Filippone.
Footnotes
Presented as 66th ESCVS, Thessaloniki, Greece, May 11–14, 2017.
References
- 1.Yamada T., Tada S., Harada J. Aortic dissection without intimal rupture: diagnosis with MR imaging and CT. Radiology. 1988;168(2):347–352. doi: 10.1148/radiology.168.2.3393653. [DOI] [PubMed] [Google Scholar]
- 2.Harris K.M., Braverman A.C., Gutierrez F.R., Barzilai B., Dávila-Román V.G. Transesophageal echocardiographic and clinical features of aortic intramural hematoma. J. Thorac. Cardiovasc. Surg. 1997;114(4):619–626. doi: 10.1016/S0022-5223(97)70052-7. [DOI] [PubMed] [Google Scholar]
- 3.Chou A.S., Ziganshin B.A., Charilaou P., Tranquilli M., Rizzo J.A., Elefteriades J.A. Long-term behavior of aortic intramural hematomas and penetrating ulcers. J. Thorac. Cardiovasc. Surg. 2016;151(2):361–373. doi: 10.1016/j.jtcvs.2015.09.012. e1. [DOI] [PubMed] [Google Scholar]
- 4.Kitai T., Kaji S., Yamamuro A. Clinical outcomes of medical therapy and timely operation in initially diagnosed type a aortic intramural hematoma: a 20-year experience. Circulation. 2009;120(11_Suppl_1):S292–S298. doi: 10.1161/CIRCULATIONAHA.108.843615. [DOI] [PubMed] [Google Scholar]
- 5.Park K.-H., Lim C., Choi J.H. Prevalence of aortic intimal defect in surgically treated acute type a intramural hematoma. Ann. Thorac. Surg. 2008;86(5):1494–1500. doi: 10.1016/j.athoracsur.2008.06.061. [DOI] [PubMed] [Google Scholar]
- 6.Agha R.A., Fowler A.J., Rajmohan S. Preferred reporting of case series in surgery; the PROCESS guidelines. Int. J. Surg. 2016;36:319–323. doi: 10.1016/j.ijsu.2016.10.025. [DOI] [PubMed] [Google Scholar]
- 7.Lansman S.L., Saunders P.C., Malekan R., Spielvogel D. Acute aortic syndrome. J. Thorac. Cardiovasc. Surg. 2010;140(6):S92–S97. doi: 10.1016/j.jtcvs.2010.07.062. [DOI] [PubMed] [Google Scholar]
- 8.Uchida K., Imoto K., Karube N. Intramural haematoma should be referred to as thrombosed-type aortic dissection. Eur. J. Cardio-Thorac. Surg. 2013;44(2):366–369. doi: 10.1093/ejcts/ezt040. [DOI] [PubMed] [Google Scholar]
- 9.Kitai T., Kaji S., Yamamuro A. Impact of new development of ulcer-like projection on clinical outcomes in patients with type B aortic dissection with closed and thrombosed false lumen. Circulation. 2010;122(11_Suppl_1):S74–S80. doi: 10.1161/CIRCULATIONAHA.109.927517. [DOI] [PubMed] [Google Scholar]
- 10.Berdat P.A., Carrel T. Aortic dissection limited to the ascending aorta mimicking intramural hematoma. Eur. J. Cardio-Thorac. Surg. 1999;15(1):108–109. doi: 10.1016/s1010-7940(98)00259-0. [DOI] [PubMed] [Google Scholar]
- 11.Estrera A.L. Timing is everything. J. Thorac. Cardiovasc. Surg. 2016;151(2):374–375. doi: 10.1016/j.jtcvs.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 12.Mukohara N. Intramural hematoma -contradiction to the theory of rupture of the vasa vasorum at onset. Ann. Thorac. Cardiovasc. Surg. 2014;20(6):949–950. doi: 10.5761/atcs.ed.14-00219. [DOI] [PubMed] [Google Scholar]
- 13.Matsushita A., Fukui T., Tabata M., Sato Y., Takanashi S. Preoperative characteristics and surgical outcomes of acute intramural hematoma involving the ascending aorta: a propensity score-matched analysis. J. Thorac. Cardiovasc. Surg. 2016;151(2):351–358. doi: 10.1016/j.jtcvs.2015.09.055. [DOI] [PubMed] [Google Scholar]