1. Introduction
Vascular leiomyomas are benign smooth muscle tumors that originate from the tunica media layer of the vein. They are apparently rare tumors that occur mostly in the extremities and are generally associated with pain or tenderness. We report herein a patient with a painless vascular leiomyoma, located between the vaginal wall and the bladder serosa, that was incidentally detected during a tension-free vaginal mesh operation.
2. Presentation of case
An 80-year-old Japanese woman had suffered from disordered micturition and was referred to our hospital. She had an unremarkable medical history, with no diagnosis of diabetes or neurological disorders such as Parkinson's disease or cerebrovascular disease. She was not taking any anticholinergic medications that could have induced a micturition disorder. Gynecological examination revealed a stage 2 cystocele. There were no neurologic abnormalities and no masses in the extremities or torso. As we recommend surgery for all of our patients with stage 2–4 cystocele, this patient was admitted to our hospital for placement of anterior tension-free vaginal mesh (A-TVM) in September 2016.
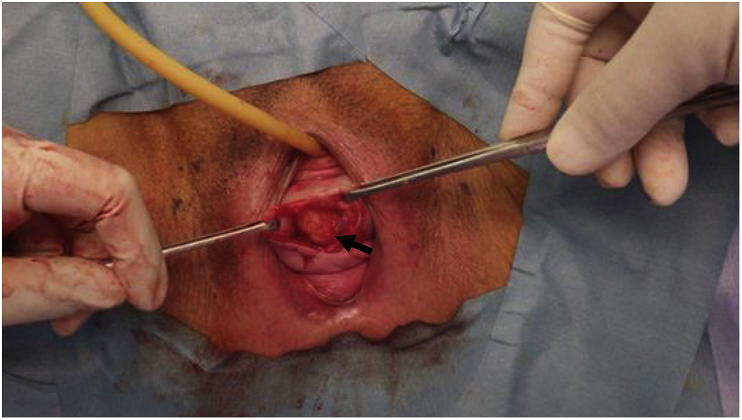
At the time of surgery, when the midline incision was created in the anterior vaginal wall and the anterior vaginal wall was dissected, a 1-cm, yellow, soft, mobile mass was detected between the vaginal wall and the bladder serosa (Fig. 1). Although the patient reported no subjective symptoms and no pain, the mass was resected thoroughly and sent for pathological diagnosis.
Fig. 1.
Operative view. The arrow shows a 1-cm, yellow, soft, mobile mass located between the vaginal wall and the bladder serosa (the vaginal wall is grasped with forceps). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
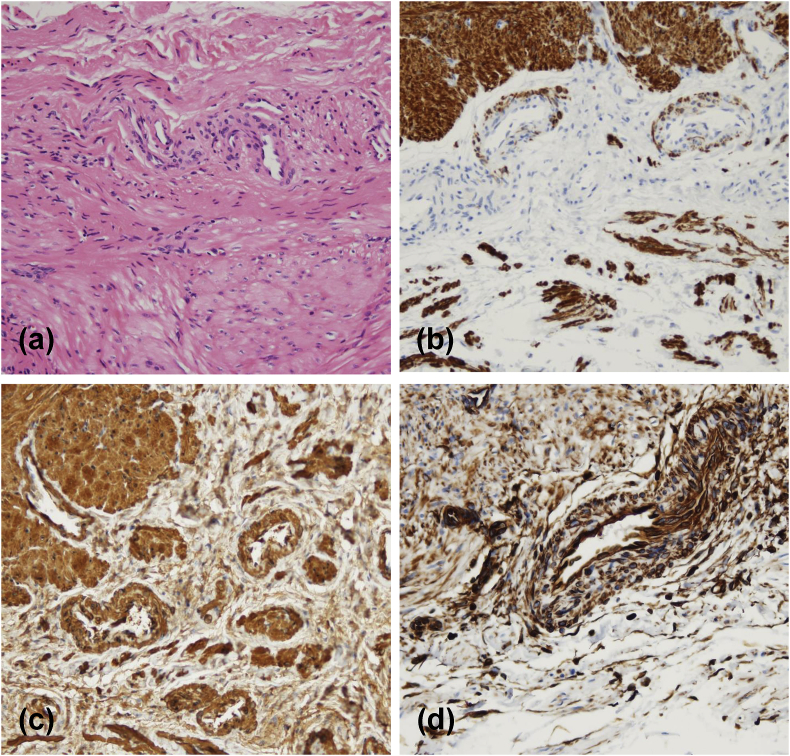
The tumor contained smooth muscle and blood vessels (Fig. 2A), and we diagnosed a vascular leiomyoma using the results of immunostaining for desmin (Fig. 2B), smooth muscle actin (Fig. 2C), and vimentin (Fig. 2D). During 8 months of follow-up after the A-TVM procedure, the patient reported no subjective symptoms or pain.
Fig. 2.
Histopathological analyses. a: The tumor contains smooth muscle tissue and blood vessels (hematoxylin and eosin; × 200). b: Immunohistochemical staining for desmin highlights the smooth muscle component ( × 200). c,d: The tumor cells express smooth muscle actin and vimentin ( × 200).
3. Discussion
Vascular leiomyomas are benign smooth muscle tumors that originate from the tunica media of a vein. They commonly arise in the dermis or subcutaneous tissue and represent 5% of all benign soft tissue tumors. They occur most frequently in the superficial fascia of the lower extremities: Zang et al. reported that 78% (110 of 141 vascular leiomyomas) are in the lower.1 Tumors have also been reported in the upper extremities, face and buttocks.2, 3, 4 There are no previous case reports of a vascular leiomyoma located between the vaginal wall and the bladder serosa.
We could find no clear explanation in the literature as to why our patient's vascular leiomyoma was not painful,2, 3, 4 as it is known that pain with a vascular leiomyoma is often evoked by touch.2 Considering our patient's advanced age and the fact that she was not sexually active, we presume that there was no pain because there was no stimulation of the vaginal wall.
On physical examination, vascular leiomyomas of the extremities are associated with pain or tenderness; this distinguishes them from other soft tissue masses. The pain is considered to be related to local ischemia resulting from smooth muscle contraction,5 but the precise origin of this pain or tenderness remains unclear to date.
Ultrasonography and MRI are valuable in the diagnosis of vascular leiomyomas. The typical ultrasonographic appearance is a hypoechoic, homogeneous nodule with well-defined margins. The results of MRI show slight hyperintensity to muscle on T1-weighted imaging, mixed iso- or hyperintensity to muscle on T2-weighted imaging, and enhancement after gadolinium injection.3 We always obtain MRI or computed tomography in patients with pelvic organ prolapse before placing A-TVM in order to examine the level of pelvic organ prolapse and any comorbidities. However, this vascular leiomyoma of the vaginal wall was not detected by MRI at our institution. If this tumor had been larger or the MRI had been performed with thinner slices, the tumor might have been detected.
Initially it was unclear whether this patient had a benign tumor such as a hemangioma, lipoma, or angiolipoma, or a malignant tumor such as a malignant leiomyoma, malignant fibrous histiocytoma, or synovial sarcoma. However, this tumor was a soft, mobile mass with clear boundaries and was detected only after the incision into the anterior vaginal wall was made. It appears that this tumor had a mesenchymal cell origin. We assumed, based on these findings, that the tumor was benign, and we completed the A-TVM procedure using artificial mesh.
We performed histopathological identification with hematoxylin-eosin staining. Furthermore, immunohistochemical stains for vimentin (a mesenchymal marker), desmin (a protein marker for muscle tissue) and smooth muscle actin were performed. Through these analyses, this tumor was diagnosed as a vascular leiomyoma.
Treatment of a vascular leiomyoma typically requires only simple resection with ligation of the feeding vessels. The diagnosis of vascular leiomyoma is hardly ever reached before resection. Recurrence is very rare after complete resection.2, 3, 4 We were able to reassure our patient that tumor recurrence was unlikely.
4. Conclusion
Vascular leiomyoma is a rare benign tumor, and the present report is the first to describe a vascular leiomyoma located between the vaginal wall and the bladder serosa. Histopathological identification was performed using several known indicators. During operative treatments like A-TVM, a vascular leiomyoma without experiencing any pain may be present at an unexpected location in lower urinary tract.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgments
We wish to thank Kouich Nishimura for preparing the figures. No funding was provided for this case report.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eucr.2017.12.005.
Contributor Information
Kaori Yamashita, Email: kaori-yamashita@tokiwa.or.jp.
Hiroaki Shimmura, Email: shimmura@tokiwa.or.jp.
Suguru Tokiwa, Email: suguru-tokiwa@tokiwa.or.jp.
Shigeaki Kato, Email: uskato0525@tokiwa.or.jp.
Appendix A. Supplementary data
The following is/are the supplementary data related to this article:
References
- 1.Zhang J.Z., Zhou J., Zhang Z.C. Subcutaneous angioleiomyoma: clinical and sonographic features with histopathologic correlation. J Ultrasound Med. 2016;35:1669–1673. doi: 10.7863/ultra.15.06056. [DOI] [PubMed] [Google Scholar]
- 2.Woo K.S., Kim A.H., Kim H.S., Cho P.D. Clinical experience with treatment of angioleiomyoma. Arch Plast Surg. 2014;41:374–378. doi: 10.5999/aps.2014.41.4.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sayit E., Sayit A.T., Zan E., Bakirtas M., Akpinar H., Gunbey H.P. Vascular leiomyoma of an extremity: report of two cases with MRI and histopathologic correlation. J Clin Orthop Trauma. 2014;5:110–114. doi: 10.1016/j.jcot.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Willoughby A.D., Schlussel A.T., Freeman J.H., Lin-Hurtubise K. Angioleiomyoma in a rare location: a case report. Hawai‘i J Med Public Health. 2013;72:45–48. [PMC free article] [PubMed] [Google Scholar]
- 5.Yoo H.J., Choi J.A., Chung J.H. Angioleiomyoma in soft tissue of extremities: MRI findings. AJR Am J Roentgenol. 2009;192:W291–W294. doi: 10.2214/AJR.07.3952. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.