Abstract
Aim
In this study, we intend to compare two different setup procedures for female breast cancer patients.
Background
Imaging in radiotherapy provides a precise localization of the tumour, increasing the accuracy of the treatment delivery in breast cancer.
Materials and methods
Twenty breast cancer patients who underwent whole breast radiotherapy (WBRT) were selected for this study. Patients were divided into two groups of ten. Group one (G1) was positioned by tattoos and then the patient positioning was adjusted with the aid of AlignRT (Vision RT, London, UK). In group two (G2), patients were positioned only by tattoos. For both groups, the first 15 fractions were analyzed, a daily kilovoltage (kV) cone beam computed tomography (CBCT) image was made and then the rotational and translational displacements and, posteriorly, the systematic (Σ) and random (σ) errors were analyzed.
Results
The comparison of CBCT displacements for the two groups showed a statistically significant difference in the translational left–right (LR) direction (ρ = 0.03), considering that the procedure with AlignRT system has smaller lateral displacements. The results of systematic (Σ) and random (σ) errors showed that for translational displacements the group positioned only by tattoos (G2) demonstrated higher values of errors when compared with the group positioned with the aid of AlignRT (G1).
Conclusions
AlignRT could help the positioning of breast cancer patients; however, it should be used with another imaging method.
Keywords: Breast cancer, Whole breast radiotherapy, 3D surface imaging, AlignRT, Cone beam computed tomography
1. Background
Belgium has the highest incidence of breast cancer in the world and it is the third country in the world with the highest mortality rate.1
In early stages of breast cancer, adjuvant radiotherapy has shown great results reducing the risk of locoregional recurrence.2, 3 For adjuvant whole breast irradiation, the typical fractionation is 45–50 Gy delivered in 1.8–2 Gy per fraction.4 The main disadvantage of this fractionation scheme is a longer treatment time increasing the health care costs.5 Another study showed that hypofractionated schedules, 40–42.5 Gy, delivered in 15–16 daily fractions, did not show inferiority when compared with conventional schemes in tumour control and treatment toxicity.6
Nowadays, hypofractionated WBRT has been more used in radiotherapy treatments7 and requires a precise patient immobilization and positioning.8, 9
The errors during breast cancer radiotherapy treatments are caused by several variations, which can happen interfraction, like daily setup errors and intrafraction errors, such as respiratory motion.10 The uncertainties can also be defined by systematic and random errors. Systematic errors represent displacements that can happen in the same direction and similar magnitude.11 This type of errors describes a constant deviation of patient positioning during the entire treatment.11, 12
A random error can be defined as a day-to-day variation in the patient positioning12 and can occur in different directions and magnitudes for each fraction of the treatment.11
To assure a correct dose distribution, an image guided radiation therapy (IGRT) has been emphasized.8, 11, 13 IGRT provides a precise localization of the volumes of interest by comparing verification images at the time of treatment with the reference image.8, 11, 14, 15 Thus, it is possible to detect patient displacements13 and increase the accuracy of the treatment delivery in breast cancer.8
For years, in WBRT the common patient setup was the alignment with lasers, skin marks and megavoltage (MV) electronic portal image (EPI) verifications.13 With the objective of guiding the setup by alignment of the chest wall, EPIs are taken before the treatment to evaluate the integrity of the patient setup and treatment isocenter.15, 16 With this system, it is possible to correct patient positioning in 3 to 6 degrees of freedom.15 However, portal images provide an insufficient visible anatomy9 and represent considerable additional dose over the course of the treatment.9, 15
The CBCT represents a technological advance in IGRT.14 The kilovoltage (kV)-CBCT system is a method of generating 3D images for computed tomography (CT) reconstruction using rotational large fields cone beams.17 This system provides 3D information of the breast region and shows soft tissues images.17 This technology allows a high definition of anatomic and geometric imaging with a good spatial resolution, essential to evaluate the patient position, target volume and increase the geometric accuracy of the treatment.17 The disadvantages of this system are a more complex and time-consuming imaging modality and an additional radiation exposure.17
Recently, new surface-based monitoring systems have been introduced, with the advantage of monitoring patients in 3D, without the use of ionizing radiation.9, 18, 19 With 3D surface systems, a surface model of the breast is acquired and used to align the patient for daily setup.15 In each treatment fraction an image of patient breast surface is acquired to be then compared with a reference surface model.15, 16, 18
2. Aim
With this study we intend to evaluate the translational and rotational displacements – left–right (LR), craniocaudal (CC), anterior–posterior (AP), comparing two different setup procedures for two groups of patients. The systematic (Σ) and random (σ) errors in translational and rotational displacements will also be analyzed for both groups.
3. Materials and methods
3.1. Patient data
Twenty breast cancer patients from Cliniques Universitaires Saint Luc (CUSL) were selected for this study. These patients underwent WBRT and the displacements were analyzed in the first 15 fractions.
3.2. Planning CT
All patients were given CT scans in a supine position, with a breast board and were instructed to perform free breath. After the acquisition of the CT scan, six tattoos were made, two in the middle of the chest, two in the right side of the patient and two in the left side of the patient.
The CT data were imported to the AlignRT and treatment planning system – XIO (Elekta AB, Sweden).
3.3. Dosimetric planning
In the treatment planning system, the planning target volume (PTV) was defined as the mammary gland. The organs at risk contoured were the contralateral and ipsilateral lungs, contralateral breast, heart and spinal cord. A 3D-conformal radiotherapy (3D-CRT) plan was performed using two tangential fields, each one with 6 MV and field-in-field to improve dose homogeneity.
3.4. AlignRT setup
The images were imported by the CT to AlignRT software to generate a reference image. In this system, were defined the 3D body outline and the region of interest as the mammary gland.
AlignRT system consists of two (typical setup) or three camera units. Each camera unit has two data cameras, a texture camera, a speckle projector and a light flash.20 In our study, three camera units were used, two laterals and one central.
The 3D surface model of the patient is daily computed by a pseudo random optical pattern projected into the patient via the speckle projector.20, 21
3.5. Patient setup
Patients were divided into two groups of ten patients each, group one (G1) and group two (G2).
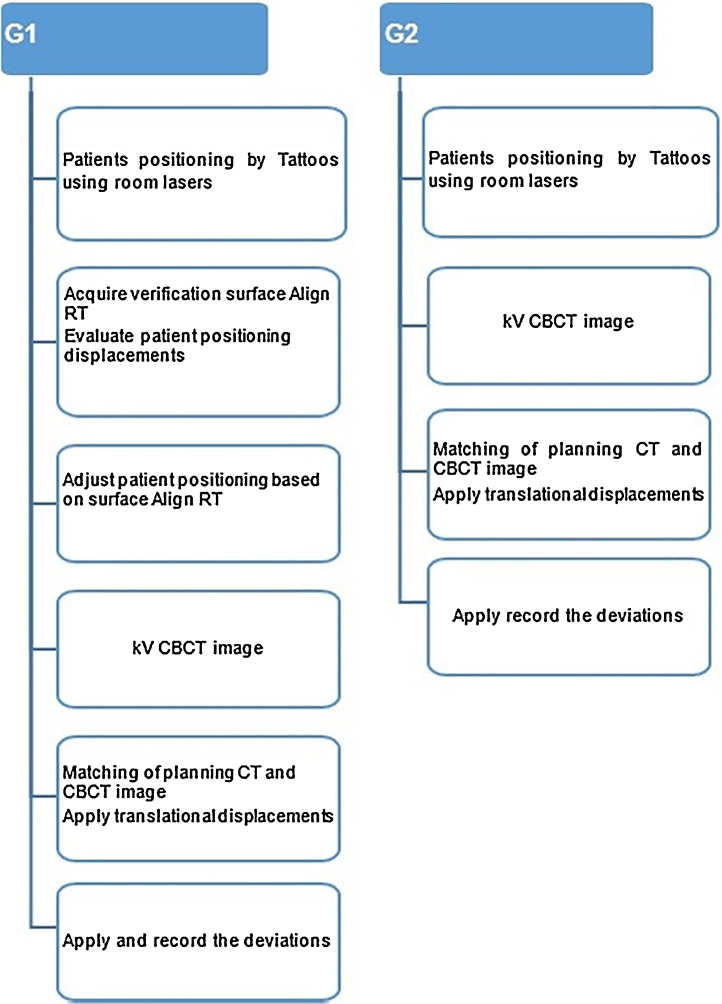
Fig. 1 summarizes setup procedures for both groups.
Fig. 1.
Description of procedures for groups G1 and G2.
3.5.1. G1
For G1, patients were positioned by tattoos using lasers.
In each fraction, a 3D surface image was acquired in real time, and matched with the reference surface model. Then, translational and rotational adjustments were made in patient setup with the aid of AlignRT system, with the objective of minimizing the differences/disagreements between the reference surface image and the surface image in real time.
3.5.2. G2
In G2, patients were positioned only by tattoos with the aid of lasers.
3.6. Imaging protocol
For both groups, a daily kV CBCT image was made and, then, the matching was performed. First, an automatic matching was done based on the grey value. Therefore, in the same images, the radiotherapist performed a manual matching and the displacements were accomplished. Only translational displacements were applied in the treatment couch, because the couch was not able to apply setup corrections in 6 degrees of freedom.
3.7. Data analysis
For both groups, rotational (R) and translational (T) displacements were analyzed in a total of 300 images of CBCT.
3.8. Statistical analysis
To evaluate the R and T displacements for each group of patients, a statistical analysis was made with a 95% confidence interval. The Shapiro–Wilk test was used to examine whether the samples were normally distributed. Since the data of all translational displacements and rotational LR displacement fit a normal distribution, the t-test was used. To analyze the rotational AP and CC displacements and also the difference between accepted values of translational variables from manual and automatic matching (Dif LR, Dif CC, Dif AP), a nonparametric statistic test Mann–Whitney U was used.
3.9. Systematic and random errors
For both groups of patients the systematic (Σ) and random (σ) errors were qualified through the values of displacements (rotational and translational) obtained by automatic matching.12
The systematic error (Σ) was assessed by the standard deviation (SD) from the values of mean displacement for all individual patients. The random error (σ) was expressed by the root mean square (RMS) of SD of all patients.12
4. Results
Table 1 shows the mean and standard deviation of translational displacements (obtained by automatic matching) for both groups. Only for the LR direction (p = 0.03), there is a statistically significant difference between the two groups.
Table 1.
Mean ± standard deviation of translational displacements for G1 and G2.
| T (cm) | Groups | Mean (cm) | Standard deviation (cm) | p-Value |
|---|---|---|---|---|
| LR | G1 | −0.02 | 0.13 | 0.03* |
| G2 | 0.22 | 0.29 | ||
| CC | G1 | 0.05 | 0.29 | 0.07 |
| G2 | −0.22 | 0.33 | ||
| AP | G1 | −0.21 | 0.14 | 0.33 |
| G2 | −0.31 | 0.29 | ||
T, translational; LR, left–right; CC, craniocaudal; AP, anterior–posterior.
Statistically significant difference
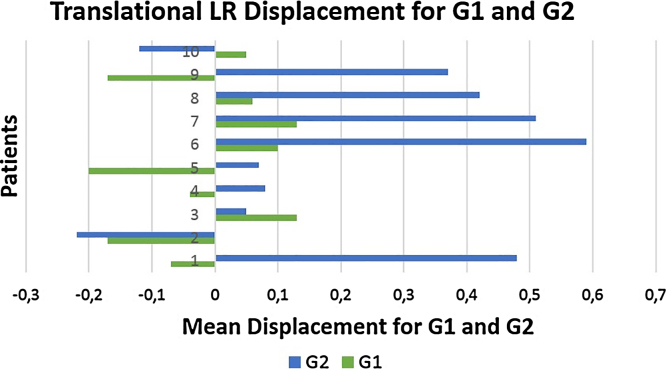
Fig. 2 presents the translational LR displacements between the groups and depicts that in the G2 the mean values of LR displacements are higher. In this way, it is considered that the procedure with Align RT has smaller lateral displacements.
Fig. 2.
LR translational displacements for G1 and G2.
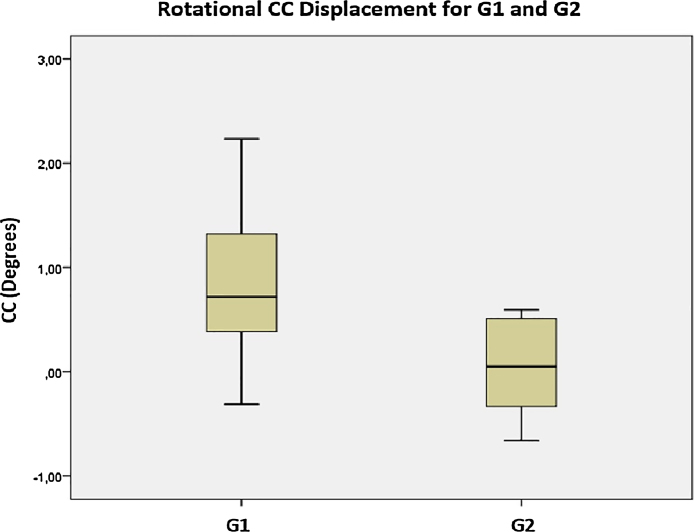
Table 2 summarizes rotational displacements (obtained by automatic matching) for G1 and G2. Only CC showed statistically significant differences between the two groups (p = 0.02). It can be observed that G2 presents smaller displacements in the CC direction.
Table 2.
Rotational displacements for G1 and G2.
| Groups | Mean (degree) | Standard deviation (degree) | p-Value | |
|---|---|---|---|---|
| LR | G1 | 0.30 | 1.22 | 0.55 |
| G2 | 0.25 | 1.11 |
| Groups | Median (degree) | Interquartile range (degree) | p-Value | |
|---|---|---|---|---|
| CC | G1 | 0.72 | 1.04 | 0.02* |
| G2 | 0.05 | 0.93 | ||
| AP | G1 | −0.01 | 1.07 | 0.32 |
| G2 | −0.28 | 1.17 | ||
T, translational; LR, left–right; CC, craniocaudal; AP, anterior–posterior.
Statistically significant difference
Fig. 3 shows the box-plot of the rotational displacements in the CC direction. Through this figure, it can be found that the patients positioned by tattoos using lasers and AlignRT system (G1) show more displacements in the CC direction when compared with G2.
Fig. 3.
Rotational CC displacement for G1 and G2.
Table 3 describes the translational displacements obtained by the difference from the automatic and manual matching in both groups.
Table 3.
Translational displacements, obtained by the difference from the automatic and manual matching in G1 and G2.
| T (cm) | Groups | Median (cm) | Interquartile range (cm) | ρ-Value |
|---|---|---|---|---|
| Dif LR | G1 | −0.02 | 0.12 | 0.08 |
| G2 | −0.06 | 0.17 | ||
| Dif CC | G1 | −0.11 | 0.59 | 0.35 |
| G2 | 0.03 | 0.48 | ||
| Dif AP | G1 | 0.05 | 0.14 | 0.39 |
| G2 | 0.02 | 0.25 | ||
T, translational; Dif LR, difference left–right; Dif CC, difference craniocaudal; Dif AP, difference anterior–posterior.
It can be noted from this table that no statistically significant differences were identified for the two groups. However, through the analysis of Table 3, we observed that the LR differences in G1 (−0.02 cm) were relatively lower than G2 (−0.06 cm). Hence, fewer adjustments were made in manual matching in patients that were positioned with the aid of the AlignRT system.
This fact supports the results analyzed in Table 1, when AlignRT system was used as aid in positioning patients a reduction in lateral displacements was observed.
For G1 in the CC and AP directions, more corrections in manual matching were made.
Table 4 shows the systematic (Σ) and random (σ) errors calculated for the two groups of patients. Through the analysis of translational displacements, we observed that G2 presents higher values of systematic (Σ) and random (σ) errors as compared to G1.
Table 4.
Systematic and random errors in the translational and rotational displacements for G1 and G2.
| Translational (cm) |
Rotational (degree) |
||||||
|---|---|---|---|---|---|---|---|
| LR | CC | AP | LR | CC | AP | ||
| G1 | Systematic errors (Σ) | 0.13 | 0.29 | 0.14 | 1.22 | 0.74 | 0.81 |
| Random errors (σ) | 0.19 | 0.27 | 0.18 | 0.72 | 1.14 | 0.90 | |
| G2 | Systematic errors (Σ) | 0.29 | 0.33 | 0.29 | 1.11 | 0.51 | 0.83 |
| Random errors (σ) | 0.24 | 0.31 | 0.29 | 0.76 | 0.78 | 1.02 | |
LR, left–right; AP, anterior–posterior; CC, craniocaudal.
The LR direction for G1, compared with G2 and the other directions, has inferior values of random and systematic errors. This fact supports the analysis done in Table 1 and Fig. 2, where the displacements for this direction were smaller with the AlignRT system.
In addition, it can be noted for translational displacements in both groups that the CC direction presents superior values of systematic and random errors relative to the LR and AP directions.
In rotational uncertainties, it was visible that systematic and random errors obtained by G2 were lower than in G1 in the CC direction. This result is in agreement with the results presented in Table 2. On the other hand, we observed that G2 shows higher systematic and random errors than G1 in the AP direction.
In recent years, 3D surface systems have been introduced and studied in radiotherapy.19 The use of AlignRT system has shown good results in monitoring procedures.21
Several studies report that kV CBCT registration with AlignRT is used in patients that performed deep inspiration breath hold (DIBH). Besides, the kV CBCT scan was acquired simultaneously with 3D surface system for setup verification.20, 21, 22
It is important to remember that in our study, contrary to the others, the patients did free-breathing.
A clinical study by Tanja et al. compared translational and rotational setup displacements in two modalities of image (CBCT and 3D surface imaging) in the same group of patients to investigate the applicability of 3D surface imaging in DIBH radiotherapy for left-sided breast cancer. For this study the CBCT images were acquired at the same time that 3D surface imaging.21 In our study, we analyzed the applicability of AlignRT through kV CBCT images in two different setup procedures. Thus, the CBCT image was used solely as a tool to study the applicability of AlignRT to help in patient positioning and reduce the setup errors. The study by Tanja et al. demonstrated a poor correlation for rotational setup variations between CBCT and 3D surface imaging.21 However, in our study we found significant differences between the two groups in CC displacements. Furthermore, the study does not recommend the use of 3D surface imaging solely, for verification and monitoring, since this system demonstrated difficulty in distinguishing if translational AP displacements were caused by anatomic changes or variations in breath hold.21 In our study, we observed that in the AP translational direction the procedure with AlignRT presents inferior values of setup displacements.
Another study by Tanja et al. compared the setup displacements between 3D surface imaging and CBCT. An overview of the results demonstrated that the CC direction showed superior values of systematic and random errors.22 This result is in agreement with our study. An excellent correlation was also noted between set-up errors obtained by CBCT and 3D surface imaging.22 In addition, this study demonstrated that the residual errors with CBCT registrations were statistically higher than the ones associated with 3D surface imaging registrations. Thus, the authors concluded that with the AlignRT system the errors were lower.22 In our study, the errors are lower in G1 and this supports the importance of the AlignRT system in the reduction of setup displacements. An overview of our clinical experience demonstrated a statistically significant difference in the translational LR displacement, and for this variable the procedure that uses AlignRT showed smaller lateral setup displacement, compared with the group positioned only by tattoos. Only rotational CC displacement showed statistically significant differences between the two groups. For this direction, the group positioned with the aid of AlignRT indicated more setup variability.
5. Conclusion
Daily alignment with the AlignRT system was found useful for clinical practice and valuable for reducing setup errors in breast cancer patients. Furthermore, this system has the advantage of being non-invasive and not using ionizing radiation. Our results suggest that AlignRT could help in the positioning of breast cancer patients. However, 3D surface systems have the limitation of a superficial acquisition which does not provide internal information. Therefore, AlignRT systems should be used with another imaging method like CBCT. In our study the patients did free-breathing. However, the chest wall does a lot of movement due to respiratory movements. For that reason, for future studies, we suggest that respiratory monitoring techniques should be used, such as DIBH, to reduce setup errors associated with the respiratory movement.
Conflict of interest
None declared.
Financial disclosure
None declared.
References
- 1.Burrion J.-B. Dépistage et cancer en. Fond Contre Le Cancer. 2014;2014:9–13. [Google Scholar]
- 2.Jacob J., Heymann S., Borget I. Dosimetric effects of the interfraction variations during whole breast radiotherapy: a prospective study. Front Oncol. 2015;5:199. doi: 10.3389/fonc.2015.00199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ozyigit G. Current role of modern radiotherapy techniques in the management of breast cancer. World J Clin Oncol. 2014;5:425. doi: 10.5306/wjco.v5.i3.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Edwards-Bennett S.M., Correa C.R., Harris E.E. Optimization of adjuvant radiation in breast conservation therapy: can we minimize without compromise? Int J Breast Cancer. 2011;2011:1–6. doi: 10.4061/2011/321304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yarnold J. PG 10.01 Hypofractionated radiotherapy in early breast cancer: clinical, dosimetric and radio-genomic issues. Breast. 2015;24:S19. doi: 10.1016/j.breast.2015.07.025. [DOI] [PubMed] [Google Scholar]
- 6.Kron T., Chua B. 2014. Radiotherapy for breast cancer: how can it benefit from advancing technology? pp. 83–90. [Google Scholar]
- 7.Koulis T., Phan T., Olivotto I. Hypofractionated whole breast radiotherapy: current perspectives. Breast Cancer Targets Ther. 2015;363 doi: 10.2147/BCTT.S81710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goyal S., Kataria T. Image guidance in radiation therapy: techniques and applications. Radiol Res Pract. 2014;2014:1–10. doi: 10.1155/2014/705604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wiant D.B., Wentworth S., Maurer J.M., Vanderstraeten C.L., Terrell J.A., Sintay B.J. Surface imaging-based analysis of intrafraction motion for breast radiotherapy patients. J Appl Clin Med Phys. 2014;15:147–159. doi: 10.1120/jacmp.v15i6.4957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fein D.A., McGee K.P., Schultheiss T.E., Fowble B.L., Hanks G.E. Intra- and interfractional reproducibility of tangential breast fields: a prospective on-line portal imaging study. Int J Radiat Oncol. 1996;34:733–740. doi: 10.1016/0360-3016(95)02037-3. [DOI] [PubMed] [Google Scholar]
- 11.Royal College of Radiologists . 2008. On target: ensuring geometric accuracy in radiotherapy; pp. 1–76. [Google Scholar]
- 12.Gupta T., Chopra S., Kadam A. Assessment of three-dimensional set-up errors in conventional head and neck radiotherapy using electronic portal imaging device. Radiat Oncol. 2007;2:44. doi: 10.1186/1748-717X-2-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shah A.P., Dvorak T., Curry M.S., Buchholz D.J., Meeks S.L. Clinical evaluation of interfractional variations for whole breast radiotherapy using 3-dimensional surface imaging. Pract Radiat Oncol. 2013;3:16–25. doi: 10.1016/j.prro.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Michalski A., Atyeo J., Cox J., Rinks M. Inter- and intra-fraction motion during radiation therapy to the whole breast in the supine position: a systematic review. J Med Imaging Radiat Oncol. 2012;56:499–509. doi: 10.1111/j.1754-9485.2012.02434.x. [DOI] [PubMed] [Google Scholar]
- 15.Mundt A.J., Roeske J.C. 2011. Image-guided radiation therapy: a clinical perspective; pp. 289–290. [Google Scholar]
- 16.Bert C., Metheany K.G., Doppke K.P., Taghian A.G., Powell S.N., Chen G.T.Y. Clinical experience with a 3D surface patient setup system for alignment of partial-breast irradiation patients. Int J Radiat Oncol Biol Phys. 2006;64:1265–1274. doi: 10.1016/j.ijrobp.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 17.De Puysseleyr A., Mulliez T., Gulyban A. Improved cone-beam computed tomography in supine and prone breast radiotherapy: surface reconstruction, radiation exposure, and clinical workflow. Strahlentherapie Und Onkol. 2013;189:945–950. doi: 10.1007/s00066-013-0435-x. [DOI] [PubMed] [Google Scholar]
- 18.Schöffel P.J., Harms W., Sroka-Perez G., Schlegel W., Karger C.P. Accuracy of a commercial optical 3D surface imaging system for realignment of patients for radiotherapy of the thorax. Phys Med Biol. 2007;52:3949–3963. doi: 10.1088/0031-9155/52/13/019. [DOI] [PubMed] [Google Scholar]
- 19.Mitterlechner B., Huber S., Weichenberger H. Three-dimensional surface scanning for accurate patient positioning and monitoring during breast cancer radiotherapy. Strahlentherapie Und Onkol. 2013;189:887–893. doi: 10.1007/s00066-013-0358-6. [DOI] [PubMed] [Google Scholar]
- 20.Betgen A., Alderliesten T., Sonke J.J., Van Vliet-Vroegindeweij C., Bartelink H., Remeijer P. Assessment of set-up variability during deep inspiration breath hold radiotherapy for breast cancer patients by 3D-surface imaging. Radiother Oncol. 2013;106:225–230. doi: 10.1016/j.radonc.2012.12.016. [DOI] [PubMed] [Google Scholar]
- 21.Alderliesten T., Sonke J.-J., Betgen A., Honnef J., van Vliet-Vroegindeweij C., Remeijer P. Accuracy evaluation of a 3-dimensional surface imaging system for guidance in deep-inspiration breath-hold radiation therapy. Int J Radiat Oncol. 2013;85:536–542. doi: 10.1016/j.ijrobp.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 22.Alderliesten T., Sonke J.-J., Betgen A., Honnef J., van Vliet-Vroegindeweij C., Remeijer P. Application of 3D surface imaging in breast cancer radiotherapy. In: Holmes D.R. III, Wong K.H., editors. vol. 8316. 2012. p. 83160A. (Proc. SPIE—the Int. Soc. Opt. Eng.). [Google Scholar]