Abstract
JAK inhibitors have been developed following the discovery of the JAK2V617F in 2005 as the driver mutation of the majority of non- BCR-ABL1 myeloproliferative neoplasms (MPNs). Subsequently, the search for JAK2 inhibitors continued with the discovery that the other driver mutations ( CALR and MPL) also exhibited persistent JAK2 activation. Several type I ATP-competitive JAK inhibitors with different specificities were assessed in clinical trials and exhibited minimal hematologic toxicity. Interestingly, these JAK inhibitors display potent anti-inflammatory activity. Thus, JAK inhibitors targeting preferentially JAK1 and JAK3 have been developed to treat inflammation, autoimmune diseases, and graft-versus-host disease. Ten years after the beginning of clinical trials, only two drugs have been approved by the US Food and Drug Administration: one JAK2/JAK1 inhibitor (ruxolitinib) in intermediate-2 and high-risk myelofibrosis and hydroxyurea-resistant or -intolerant polycythemia vera and one JAK1/JAK3 inhibitor (tofacitinib) in methotrexate-resistant rheumatoid arthritis. The non-approved compounds exhibited many off-target effects leading to neurological and gastrointestinal toxicities, as seen in clinical trials for MPNs. Ruxolitinib is a well-tolerated drug with mostly anti-inflammatory properties. Despite a weak effect on the cause of the disease itself in MPNs, it improves the clinical state of patients and increases survival in myelofibrosis. This limited effect is related to the fact that ruxolitinib, like the other type I JAK2 inhibitors, inhibits equally mutated and wild-type JAK2 (JAK2WT) and also the JAK2 oncogenic activation. Thus, other approaches need to be developed and could be based on either (1) the development of new inhibitors specifically targeting JAK2V617F or (2) the combination of the actual JAK2 inhibitors with other therapies, in particular with molecules targeting pathways downstream of JAK2 activation or the stability of JAK2 molecule. In contrast, the strong anti-inflammatory effects of the JAK inhibitors appear as a very promising therapeutic approach for many inflammatory and auto-immune diseases.
Keywords: JAK inhibitors, MPN, auto-immune diseases, inflammation, allosteric inhibitor
Introduction
Janus kinases (JAKs) play a central role in the regulation of hematopoiesis as being mandatory for signaling by receptors for hematopoietic/immunological cytokines 1. They control survival, proliferation, and differentiation of hematopoietic cells as well as the function of mature cells by binding to hematopoietic type I and type II cytokine receptors, which are devoid of catalytic activity ( Figure 1). JAKs pre-associated to these receptors to form a functional signaling complex 1. Cytokine binding induces or re-orients receptor dimerization, such that JAK kinase domains face each other in a productive conformation for transactivation and phosphorylation of the cytokine receptor cytoplasmic tails 1. The latter and JAKs themselves become scaffolds for signaling molecules, particularly for the members of the signal transducer and activator of transcription (STAT) family, which in turn are phosphorylated and homo/hetero-dimerize before translocating to the nucleus. JAK activation also initiates activation of mitogen-activated protein kinase (MAPK), phosphatidylinositol-3′-kinase (PI3K), and AKT/mammalian target of rapamycin (mTOR) ( Figure 2) 2.
Figure 1. Janus kinases (JAKs) and the cytokine receptor superfamily.
Schematic representation of type I and type II cytokine receptor subfamilies based on the extracellular domain sequence homologies. The different JAKs (JAK1, JAK2, JAK3, and TYK2) are employed by each class of receptors, as indicated. Type I receptors can form homodimers (α/α), heterodimers (α/β), or oligomers (gp130/α/gp130);(α/β/γ), although the α chain is mainly responsible for cytokine binding. Cytokine receptor complexes composed of two or more different chains activate at least two different JAKs, while single-chain receptors such as homodimeric receptors activate JAK2 only (although TpoR/MPL and G-CSFR/CSF3R can also use TYK2 and JAK1, respectively). The myelopoiesis-related cytokine receptors are denoted in red, and the lymphopoiesis-related cytokines receptors are denoted in green.
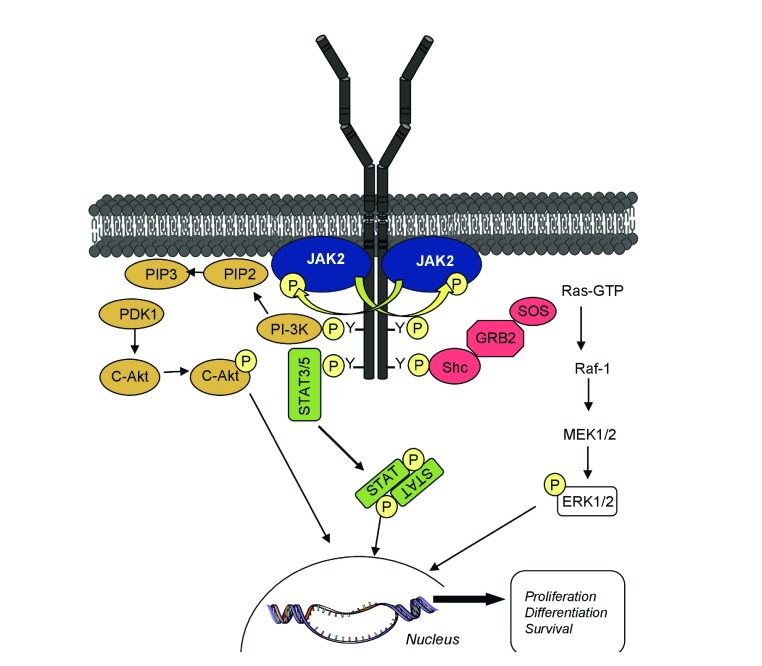
Figure 2. Principal signaling pathways activated by homodimeric cytokine receptors.
Cytokine binding to the extracellular domain of receptors induces conformation changes that enable cross-phosphorylation of the appended Janus kinases (JAKs), which then can activate each other. As a result, JAK molecules phosphorylate tyrosine residues on the intracellular part of the receptor, which then can serve as docking sites for SH2 domain containing signaling molecules such as signal transducer and activator of transcription (STAT) but also proteins from the phosphatidylinositol-3′-kinase (PI3K) and mitogen-activated protein kinase (MAPK) pathways.
The JAK/STAT pathway is frequently dysregulated in malignant diseases and in disorders with an abnormal immunological response 3.
The discovery that classic BCR-ABL1–negative myeloproliferative neoplasms (MPNs) are constantly associated with abnormal JAK2 activation due to different mutations, has paved the way for the development of JAK inhibitors in the therapy of these disorders as well as of other diseases with either genetic alterations in the JAK pathway or JAK-induced activation by autocrine and paracrine cytokine loops 4, 5. Here, we focus on the role of JAKs as potential therapeutic targets, the development of JAK inhibitors and their limitations, and potential new strategies targeting the JAKs.
Janus kinases
The human genome codes for four JAKs: JAK1, JAK2, JAK3, and TYK2 1. Like the god Janus, who has two faces and opens doors, JAKs possess two kinase domains—one catalytically active domain at the C-terminus and an upstream pseudokinase domain that binds ATP—but does not phosphorylate substrates (except weakly itself). At the N-terminus, JAKs possess a FERM (band four-point-one, ezrin, radixin, moesin)-like domain and an Src homology 2 (SH2)-like domain ( Figure 3A). The non-covalent attachment of JAKs to cytokine receptor tails is specific and depends on the FERM domain and on the juxtamembrane receptor sequence containing a proline-rich Box 1 and a motif denoted Box 2 with both hydrophobic and negatively charged residues as well as the sequences stretching from Box 1 to Box 2 6, 7. JAK2 associates with the three homodimeric receptors: erythropoietin receptor (EPOR), thrombopoietin receptor (MPL/TPOR), and the granulocyte colony-stimulating factor receptor (G-CSFR/CSF3R). JAK1, JAK2, and TYK2 can also associate with heterodimeric or trimeric receptors, and JAK3 only with receptors containing the γ-chain with solely JAK1 as partner ( Figure 1) 1. The precise structure of receptor/JAK complexes remains unknown. Recently, the structures of the kinase and pseudokinase domains of JAK1, JAK2, and TYK2 were obtained and represent a major asset for the identification of novel (allosteric) inhibitors (see below) 8– 10. Interestingly, JAKs also play a role of chaperones for traffic and stability at the cell surface of several cytokine receptors 11.
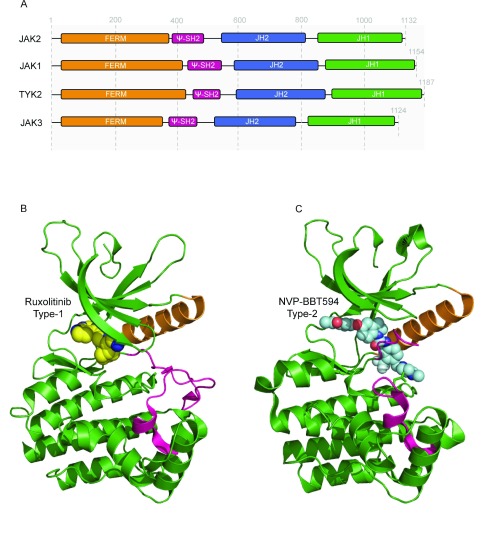
Figure 3. The kinase domain of Janus kinase 2 (JAK2) has been commonly targeted by the current inhibitors.
( A) Secondary structure of JAK molecules. They are composed (from the N- to C-terminal end) of a FERM domain (band 4.1, erzin, radixin, moeisin domain), a pseudo-SH2 domain (ψ-SH2), a pseudokinase domain (JH2), and a kinase domain (JH1). While the major function of the N-terminus region is to specifically bind to cytokine receptor intracellular tail, the carboxyl-terminal region contains the catalytically active kinase domain, JH1, and the regulatory domain, JH2, of which the exact function is still matter of debate. ( B) Three-dimensional representation of JAK2 kinase domain in its active conformation (PDB: 3KRR 12) bound to type 1 inhibitor, ruxolitinib (show in yellow spheres). The binding of ruxolitinib has been modelled on the basis of the co-crystal of ruxolitinib-bound Scr (PDB: 4U5J 13). The activation loop, colored in pink, adopts an ‘open’ (active) conformation stabilized by phosphorylation of tyrosine residues 1007 and 1008. The αC is colored in orange. ( C) Three-dimensional representation of JAK2 kinase domain in its inactive conformation bound to a type 2 inhibitor, NVP-BTT594 (PDB: 3UGC 14). The activation loop, colored in pink, adopts a ‘closed’ (inactive) conformation. The compound is shown in cyan spheres, and the αC in orange. (D) Illustration of the structures of the main compounds discussed in this review.
Disease associated with abnormal JAK activation
Autonomous activation of the JAK/STAT pathway is central in several pathologies. Genetic alterations targeting this signaling pathway are associated mainly with hematologic malignancies. Pathological JAK activation also occurs in diseases linked to abnormal cytokine stimulation.
Hematologic malignancies
In many myeloid and lymphoid malignancies, driver mutations leading to constitutive JAK activation can be found. The paradigm is represented by BCR-ABL1–negative MPNs as they are all related to mutations activating JAK2, which in more than 50% of the cases both initiate and drive the disease phenotype. Thus, the development of JAK2 inhibitors is particularly critical for MPNs.
Classic BCR-ABL1–negative MPNs. The classic BCR-ABL1–negative MPNs (hereafter, MPNs) include three different disorders—essential thrombocythemia (ET), polycythemia vera (PV), and primary myelofibrosis (PMF)—and are caused by constitutive activation of the cytokine receptor/JAK2 pathway due to acquired somatic mutations in three major genes 15. JAK2V617F is the most prevalent mutation in MPNs associated with the three disorders (65–70%) and is present in 95% of PVs. Mutations in the exon 12 of JAK2 are found in around 2% of PV, which are negative for the JAK2V617F mutation (reviewed in 15). Interestingly, these two JAK2-activating mutations are not located in the kinase domain of the protein but involve amino acid changes in the pseudokinase (JH2) domain ( JAK2V617F) and the SH2-JH2 linker domain ( JAK2 exon 12) ( Figure 3A and see below). Mutations in the thrombopoietin receptor ( MPL) gene are much rarer than JAK2 mutations and are present in 3% of MPNs (4–5% of ET and myelofibrosis [MF]). The recurrent mutations are located in the exon 10. The most frequent are substitutions of the W515 residue to many other amino acids, mostly L or K but also R or A (reviewed in 15). In MPNs, the MPLS505N mutation is also found but less frequently than in hereditary thrombocytosis. Rarer mutations of MPL have been described in both the extracellular and intracellular domains. The third gene found frequently mutated in MPNs is calreticulin ( CALR), which is affected by mutations leading to a +1 frameshift in the exon 9 16, 17. As for MPL, CALR mutations are associated with ET and MF but with a higher frequency (25%). CALR is not a molecule directly involved in activation of JAK2, but the new C-terminus common to all mutants allows the CALR mutants to tightly bind and activate MPL and JAK2 18– 21.
All of these activating mutations mimic the effects of hematopoietic cytokines by inducing constitutive signaling via the STAT, PI3K, and ERK/MAPK pathways. To achieve this, JAK2V617F must be bound to cytokine receptors, more particularly homodimeric receptors (EPOR, CSF3R/G-CSFR, and MPL/TPOR), which allow its dimerization and activation 22. CALR mutants specifically activate MPL and (to a lesser extent) G-CSFR, and MPL mutations result in an active conformation of the receptor 18. Loss-of-function mutations in SH2B3, a negative regulator of JAK2, have been described as drivers in MPNs and idiopathic erythrocytosis 23, 24, but there is evidence that in the majority of the cases it is either a secondary mutation or a germ-line mutation predisposing to MPNs 25.
In 20–30% of patients with MPNs, mutations besides driver JAK2-activating mutations have been identified in genes involved in splicing ( SRSF2 and U2AF1) and epigenetic regulation ( TET2, DNMT3A, ASXL1, EZH2, and IDH1/IDH2) and in tumor suppressor genes ( TP53) 15, 26, 27. They could predate or follow the driver mutations 28– 30. Mutations, such as in TET2, DNMT3A, or EZH2, favor clonal dominance and disease initiation 28, 31. Of note, these associated mutations promote progression to MF or leukemic transformation ( ASXL1, IDH1/2, EZH2, and TP53) 32, 33. Almost always, one such mutation is present in PMF, and the number of such mutations correlates with the severity of the disease 32, 33 and might modulate the response to JAK2 inhibition.
Other myeloid malignancies
MPN associated with JAK2 fusion proteins
Four fusion proteins—ETV6 (TEL)-JAK2 (t(9;12) (p24;p13), PCM1-JAK2 (t(8;9) (p22;p24), BCR-JAK2 (t(9;22) (p24;q11.2), and RPN1-JAK2 (t(3;9) (q21;p24)—have been described in some MPNs—PMF, chronic eosinophilic leukemia (CEL), atypical chronic myeloid leukemia (aCML), and unclassified MPNs—or in mixed MPN/myelodysplastic syndrome (MPN/MDS) 34– 37. The translocation partner of JAK2 sets the expression level and induces dimerization of JAK2 kinase domains.
Chronic neutrophilic leukemia, an MPN associated with G-CSFR ( CSFR3 ) mutations
Acquired activating CSF3R mutations have been found in the great majority of chronic neutrophilic leukemias (CNLs). Most CNLs carry a T618I mutation (T595I if the first counted residue is after the peptide signal sequence) 38. The T615N (T592N) mutation has also been described but more rarely. CSF3R mutations have also initially been described in aCML but are much less frequent than in CNL.
JAK2V617F and (to a lower extent) MPL and CALR mutations are extremely prevalent in refractory anemia with ring sideroblasts and thrombocytosis and are associated with SF3B1 mutations 39.
Mutations in JAK2 or cytokine receptors are rare in the other myeloid malignancies. They can be found in chronic myelomonocytic leukemia (CMML) but always associated with other mutations.
In acute myeloid leukemia (AML), mutations in JAKs are rare and, when present, mostly involve JAK1. CSF3R mutations have also been described but as late events. The only AML associated frequently with JAK mutations is Down syndrome acute megakaryoblastic leukemia (AMKL), where JAK1, JAK2, and also JAK3 mutations are found in around 20% of cases 40, 41.
In acute myeloid leukemia (AML), mutations in JAKs are rare and, when present, mostly involve JAK1. CSF3R mutations have also been described but as late events. The only AML associated frequently with JAK mutations is Down syndrome acute megakaryoblastic leukemia (AMKL), where JAK1, JAK2, and also JAK3 mutations are found in around 20% of cases 40, 41.
Lymphoid malignancies. JAK2 activation may play a more significant role in the pathogenesis of B and T neoplasms than previously thought, although they might be only secondary events. JAK/STAT activation occurs via either mutations/translocations or cytokine paracrine/autocrine loops.
Acute lymphoblastic leukemia
In B-cell acute lymphoblastic leukemia (B-ALL), a new subtype has emerged called BCR-ABL1-like subtype (15% of pediatric ALL and 50% of ALL with Down syndrome), as it exhibits a transcriptional profile similar to that of BCR-ABL1 –positive ALL with poor prognosis 42. Half of them have JAK1 and JAK2 mutations and rearrangement of CRLF2, a gene encoding a cytokine receptor 43, 44. The most frequent JAK2 mutations target the R683 (R683G/S), a residue present in the DIREED motif located in the hinge between the N- and C-lobes of the pseudokinase domain of JAK2 44, 45. Fusion with partners ETV6, BCR, PAX, and SSBP2 results in the activation of JAK2 kinase domain. Mutations in JAK1 are relatively rare in B-ALL in comparison with T-cell ALL (T-ALL) 46 and are located in the FERM domain and the pseudokinase domain. For instance, JAK1V658F is the equivalent of JAK2V617F 47. In most cases, JAK2 mutations are associated with an aberrant expression of CRLF2, a cytokine receptor chain which associates with IL-7RA to bind the thymic stromal lymphopoietin (TSLP) 48. The F232C-activating mutation in CRLF2 induces homodimerization of CRLF2 and is detected in 10% of cases overexpressing CRLF2 49. Activating mutations in the IL-7RA have been described either as point mutation (S185C) or as an insertion-deletion in the transmembrane domain inducing homodimerization of the IL-7RA 50. Truncating rearrangements of the EPOR have also been identified 51.
In T-ALL, mutations in JAK1, JAK2, JAK3, and the IL-7R are found in around 15% of cases, more particularly in early T-cell progenitor (ETP)-ALL 52. Targeting JAKs in these two types of ALL appears to be a valuable approach.
Hodgkin lymphoma and primary mediastinal B-cell lymphoma
Hodgkin lymphoma and primary mediastinal B-cell lymphoma (PMBL) have some common mechanisms of lymphomagenesis, being driven by alterations in the nuclear factor-kappa B (NFκB) and JAK/STAT pathways 53, 54. In rare cases (3%), a JAK2 fusion protein (SEC31A-JAK2) is present 55.
Other lymphoma
In T-cell pro-lymphocytic leukemia, mutations in JAK1 (8%) and JAK3 (30%) (more particularly M511I) have been described 56. JAK3 mutations (particularly A572V and A573V) are frequent (35%) in natural killer/T-cell lymphomas 57. Mutations or silencing of negative regulators of JAKs ( PTPN2 and SOCS1) is also frequent in diffuse large B-cell lymphoma, follicular lymphoma, and peripheral T-cell lymphoma.
An autocrine/paracrine cytokine loop induced by IL-6, IL-10, and IL-13 activates JAKs. This occurs in several types of lymphoma as well as in chronic lymphocytic leukemia and Waldenström macroglobulinemia 58.
Disorders other than hematologic malignancies
Inherited disorders of the hematopoietic system. The majority of inherited thrombocytosis are related to spontaneous activation of the MPL/JAK2 pathways due to MPL or JAK2 mutations 59, 60. The other mechanism is related to an excess of plasma thrombopoietin (TPO) due either to an excessive synthesis or to a defect in its clearance as a consequence of MPL mutations affecting receptor trafficking. This excess of TPO induces JAK2 activation 59, 60.
Inherited erythrocytosis are related to excess erythropoietin (EPO) synthesis or to gain-of-function mutations in EPOR that activate JAK2 60. Hereditary neutrophilia carry activating mutations of CSF3R that activate JAK2 61.
Inflammatory and autoimmune diseases. A large spectrum of diseases of the immune system involves an activation of JAKs through autocrine or paracrine cytokine loops 62. In inflammatory pathologies, such as rheumatoid arthritis (RA), psoriasis, inflammatory bowel disease, and alopecia areata, the most important JAK to be targeted is JAK1 62. In autoimmune disease, JAK1 is also the main JAK to be targeted as both the IL-6 and the type 1 interferon (IFN) pathways are involved. Blocking JAK1/2 in graft-versus-host disease (GVHD) is useful as type II IFN and IL-6 are pathogenic 63. Lastly, JAK inhibition can be useful to curb oncogenic inflammatory responses in a wide range of solid tumors.
JAK inhibitors
Several types of inhibitors exist according to their mechanism/region targeted in JAKs 64.
Type I inhibitors
Type I inhibitors target the ATP-binding site of the JAKs under the active conformation of the kinase domain ( Figure 3B) 64. All clinically tested inhibitors are type I. They differ in their specificity for each JAK. Many inhibitors target JAK2, JAK1, and eventually TYK2 (ruxolitinib, momelotinib, AZD1480, and baricitinib) or JAK3 and JAK1 (tofacitinib). Some are pan-JAK inhibitors (gandotinib, XL019, NVP-BSK805, peficitinib, and pyridone 6). Less frequently, they target only JAK2 (NS-018, pacritinib, CEP-33779, NVP-BVB808, TG101209, fedratinib, and AZD960), JAK1 (filgotinib and itacitinib), or JAK3 (decernotinib, janex1, and JAK3-IN-1). However, they also target other kinases, in particular FLT3 (pacritinib, NVP-BVB808, TG101209, and fedratinib), Src (NS018), or Aurora A (AZD1480) ( Table 1 and Figure 3B).
Table 1. JAK inhibitors, their targets, and their applications to pathologies.
| Inhibitors | Selectivity | Off-
target |
Diseases | Clinical phases |
|---|---|---|---|---|
| Type I | ||||
| Ruxolitinib | JAK2>JAK1>JAK3 | MF and hydroxyurea resistant or intolerant PV
Refractory leukemia (post-MPN leukemia) Pancreatic cancers Corticosteroid refractory-GVHD Psoriasis Alopecia Vitiligo |
FDA-approved
77–
79
Phase 2 80 Phase 2 in combination with capecitabine (after gemcitabine failure) 81 In evaluation 82 Phase 2 83 Open-label clinical trial 84 Case report 85 |
|
| Momelotinib
(CYT-387) |
JAK2>JAK1>JAK3 | ALK-2
TBK1 IKKε |
PMF
Post PV/ET MF PV/ET |
Phase 3 - SIMPLIFY-1/2
(Stopped) 86 Phase 2 (terminated) 87 |
| AZD1480 | JAK2>JAK1 | Aurora A
FGFR1 FLT4 |
PMF
Post PV/ET MF B-ALL Solid tumors |
Phase 1
(completed) 88 In evaluation (preclinic) 89 Phase 1 (terminated) 90 |
| Baricitinib
(INCB-028050) |
JAK2>JAK1 | Rheumatoid arthritis
Psoriasis |
Phase 3 (FDA approval in
process, EMA-approved) 91 Phase 2 92 |
|
| Tofacitinib | JAK1>JAK3 | Methothrexate-resistant rheumatoid arthritis
Crohn’s Psoriasis Alopecia areata Dermatomyositis, vitiligo |
FDA-approved
93
Phase 2 94 Phase 3 95 Phase 2 96 Case report 96 |
|
| Gandotinib
(LY2784544) |
Pan-JAK
JAK2V617F>JAK2 |
JAK2V617F-positive MF, ET and PV patients | Phase 1
97
Phase 2 (in progress) |
|
| XL019 | Pan-JAK | PV, MF | Phase 1
(terminated) 98 |
|
| NVP-BSK805 | JAK2 | JAK2V617F | Cellular models 99 | |
| NS-018 | JAK2V617F>JAK2 | Src | PMF, post PV/ET MF patients
JAK2V617F selective |
Phase 2
12
In vitro 100 |
| Pacritinib
(SB11518) |
JAK2 | FLT3 | MF | Phase 3
PERSIST-1 101, PERSIST-2 102 PAC203 study evaluating the effect of lower doses |
| CEP-33779 | JAK2 | Rheumatoid arthritis, colorectal cancer, lupus nephritis | Preclinical mouse models 103 | |
| NVP-BVB808 | JAK2 | FLT3 | MPN | Cell lines 104 |
| TG101209 | JAK2 | FLT3 | MPN, systemic sclerosis | Cellular models 105 |
| Fedratinib
(TG101348) |
JAK2 | FLT3
BRD4 |
MF | Phase 3
JAKARTA 106 FDA removed the clinical hold in August 2017 |
| AZ960 | JAK2 | ATL, other leukemia | Cell lines | |
| Filgotinib
(GLPG0634) |
JAK1>JAK2 | Rheumatoid arthritis
Bowel and Crohn’s diseases Lupus and psoriasis |
Phase 3
107
Phase 2 108 Phase 2 109 |
|
| Itacitinib
(INCB-039110) |
JAK1 | MF
Psoriasis Non-small cell lung cancer GVHD B-cell lymphoma BRAF-mutant melanoma and other solid tumors |
Phase 2
(alone or in combination with low-dose of ruxolitinib) 110 Phase 2 111 Phase 2 (combination with EGFR inhibitor, osimertinib) (in progress) Phase 3 (combination with corticosteroids) (in progress) Phase 1/2 (combination with BTK inhibitor, ibrutinib) (in progress) Phase 1 (in combination with MAPK inhibitors, dabrafenib or trametinib) (in progress) |
|
| INCB52793 | JAK1 | Advanced malignancies | Phase 1 (in progress) | |
| PF-04965842 | JAK1 | Moderate to severe psoriasis | Phase 2 112 | |
| Upadacitinib
(ABT-494) |
JAK1 | Rheumatoid arthritis | Phase 2
113
Phase 3 (in progress) |
|
| Decernotinib
(VX-509) |
JAK3 | Rheumatoid arthritis | Phase 2/3 114 | |
| WHI-P131/
JANEX-1 |
JAK3 | GVHD | Preclinical mouse model 115 | |
| JAK3-IN-1 | JAK3 | N/A | N/A | |
| Peficitinib
(ASP015K) |
JAK3 | Psoriasis
Rheumatoid arthritis |
Phase 2
116
Phase 2 117 |
|
| Type II | ||||
| NVP-BBT594 | JAK2 | BCR-ABL KDR FLT3
RET |
Cellular models 14 | |
| NVP-CHZ868 | JAK2 | KIT,
PDGFR VEGFR |
MPN
B-ALL |
Preclinical mouse models 75 |
|
Allosteric
inhibitors |
||||
| LS104 | JAK2 | BCR-
ABL |
MPN | JAK2V617F
cell lines 118 |
| ON044580 | JAK2 | BCR-
ABL |
MPN | BCR-ABL
cell lines 119 |
ATL, adult T-cell leukemia; B-ALL, B-cell acute lymphoblastic leukemia; BTK, Bruton’s tyrosine kinase; EGFR, epidermal growth factor receptor; EMA, European Medicines Agency; ET, essential thrombocythemia; FDA, US Food and Drug Administration; GVHD, graft-versus-host disease; JAK, Janus kinase; MAPK, mitogen-activated protein kinase; MF, myelofibrosis; MPN, myeloproliferative neoplasm; N/A, not applicable; PMF, primary myelofibrosis; PV, polycythemia vera.
The differences in specificities for JAK are the basis for the different trials: JAK2 specificity for MPNs and certain malignant disorders 65, 66 and JAK1 and JAK3 for inflammation and auto-immune diseases 67. The clinical toxicity can be related to the precise JAK protein that is inhibited—hematological toxicity, eventually immune suppression for JAK2 66,—immune suppression and long-term effects on hematopoietic stem cells (HSCs) for JAK1 and JAK3 68. It can be also due to an off-target inhibition. It has been suggested that the gastrointestinal toxicity was related to FLT3 inhibition 69 and the Wernicke encephalitis observed in rare patients treated with fedratinib to inhibition of thiamine uptake 70.
Currently, only three JAK inhibitors are US Food and Drug Administration (FDA) or European Medicines Agency (EMA)-approved for treatment: ruxolitinib for the treatment of MF and hydroxyurea (HU)-resistant or -intolerant PVs 65, tofacitinib and Baricitinib for the treatment of methotrexate-resistant RA 71.
The major limitation of type I inhibitors that bind to active state kinases is that while they block catalysis they allow increased phosphorylation of the activation loop on Y1007, which upon overexpression of JAK2 or other JAKs can create heteromeric JAK complexes that re-set signaling 72. This might explain why resistance to JAK2 inhibition is not related to mutations but to functional inhibition 73.
Type II inhibitors
The type II inhibitors bind to the ATP-binding pocket of kinase domains in inactive conformation, and the F of the DFG pocket is in an out conformation ( Figure 3C) 64, 74. Inhibition is more efficient and is not reversed by drug detachment 14. The best example is imatinib and the second generation of BCR-ABL inhibitors 74. Two type II JAK2 inhibitors (NVP-BBT594 and NVP-CHZ868) have been developed. NVP-CHZ868 has been used in preclinical models and was very effective 75, 76. Both inhibitors were not amenable for drug development. Owing to their powerful activity, the type II JAK2 inhibitors present the risk of inducing profound cytopenia, limiting its future use in PV or ET.
Allosteric inhibitors
Allosteric inhibitors are molecules that do not bind to the active kinase site but to another site 64. Theoretically, they would be more specific than an ATP-pocket inhibitor given the high homology of ATP-binding sites. Allosteric inhibition could be interesting to specifically target only the mutated JAKs ( JAK2V617F: 60–70% of MPNs and JAK2 exon 12: 1%) as JAK2WT is indispensable for normal hematopoiesis. An efficient JAK2WT inhibition will always lead to a cytopenia.
Within allosteric inhibitors, type III bind to a site close to the ATP-binding site while type IV bind to an allosteric site distant from the ATP-binding site. This means that in the case of JAK2V617F it might be important to target the pseudokinase domain (type IV inhibitors, see last section). To our knowledge, there is currently no allosteric inhibitor of JAK2V617F in development.
Other types of inhibitors
For kinases other than JAKs, additional types of inhibitors have been developed 64:
Type V. Such inhibitors reversibly bind to two sites of the kinase domain.
Covalent. They irreversibly bind on a nucleophilic residue (usually a cysteine) located in the ATP-binding site.
JAK inhibitor therapies
BCR-ABL –negative MPNs
Triggered by the discovery of JAK2V617F, JAK2 inhibitors have been developed, but none of them is specific to the mutant protein and most of them also target other kinases such as JAK1 and FLT3. One advantage is that their use can be extended to the JAK2V617F-negative MPNs or other pathologies associated with JAK2 activation that include inflammatory diseases and certain other cancers. Theoretically, it is not conceivable to completely inhibit JAK2 in the long term, because this will lead to a profound cytopenia and eventually aplastic anemia. Thus, these inhibitors can be used because they only partially inhibit JAK2 in vivo for different reasons (pharmacokinetics and resistance). This explains why such inhibitors give similar clinical results in MF’s improving quality of life, decreasing the splenomegaly, and improving survival. The evolution of the disease is not changed, nor apparently is the rate of MPN transformation. The differences between inhibitors concern the side effects that may essentially be related to distinct off-targets ( Table 1).
Ruxolitinib. Ruxolitinib ( Figure 3B and D) was the first JAK2 inhibitor approved for therapy of MF (high and intermediate risks). It is now the only JAK inhibitor for which a long-term follow-up has been reached. In intermediate-2 and high-risk MF, a very significant effect is found in more than 50% of the patients with a reduced spleen size (clinical trials COMFORT-1 and COMFORT-2) at any point in the trial and even a more marked effect on the general symptoms, in particular the pruritus 77– 79. These results have been extended to low- and intermediate-1 risk MF 120. In HU-refractory PVs, ruxolitinib allows the control of hematocrit in more than 60% of patients and induces a spleen volume reduction in 38% of cases at 32 weeks. In addition, a molecular decrease of JAK2V617F allele burden reaching a mean of 40% at 208 weeks was observed 78, 121. In HU-resistant or -intolerant ET, there are divergent results. In one study, ruxolitinib offered no advantage compared with other therapies in the control of the thrombocytosis and disease complications but did alleviate general symptoms and pruritus 122. In the other 123, which was an open-label phase 2 trial, ruxolitinib induced a meaningful reduction in platelet levels and attenuated ET-related symptoms. These preliminary results seemed superior to historically observed results, but this study was done in the absence of a comparison with another treatment.
Overall, ruxolitinib is a well-tolerated oral treatment with approximately 25–33% of adverse effects. The main toxicities are hematological, moderate anemia that may correct with time, and thrombocytopenia, which can be very severe in high-risk MF. Weight gain is also observed with possible abnormalities in lipid metabolism. Middle-term toxicity is an immune suppression that may be responsible for reactivation of viral infections, particularly herpes zoster and HIV1 and bacterial infections such as pneumonia, tuberculosis reactivation and urinary tract infections 124, 125. Long-term monitoring will be important because ruxolitinib decreases natural killer cell functions with a potential risk of solid tumor and lymphoma development 126, 127. This is particularly important if indications are extended to low-risk MF, PV, and ET. Analysis of patients treated for several years with ruxolitinb indicates an increase in survival in MF, but progression to leukemia is not significantly different 128. It is possible that most pro-survival effects derive from its palliative anti-inflammatory effects 65.
Other JAK2 inhibitors. Momelotinib (CYT38) ( Figure 3D) is a JAK1/JAK2 inhibitor that has shown activity resembling ruxolitinib with respect to spleen size reduction and constitutional symptom alleviation 129– 131. Importantly, momelotinib was shown to ameliorate anemia, which is a major concern in MF. The mechanism appears to be the reduction of hepcidin production through a direct inhibition of the activin receptor-like kinase-2 (ALK-2) 132. Thus, momelotinib was thought to be an alternative to ruxolitinib for patients with anemia. These promising results led to the opening of a phase III trial for the SIMPLIFY-1 and -2 studies in MF. However, the results of the two clinical trials did not show a major advantage of momelotinib on ruxolitinib, although momelotinib was associated with a decrease in transfusion requirement 86. Momelotinib development has been stopped.
NS-018 ( Figure 3D) is a JAK2/Src inhibitor that has been assessed in patients with JAK2V617F-positive MF, ET, and PV. NS-018 shows an apparent increased potency for the JAK2V617F mutant in mouse models, possibly leading to less immunosuppressive effects 100. It was tested in MF with symptom improvement but minor impact on the numbers of JAK2V617F cells 133. Gandotinib (LY2784544) ( Figure 3D) is a potent JAK2 inhibitor, which also exhibits a certain selectivity toward JAK2V617F. It was evaluated for safety and tolerability in ET, PV, and MF 97.
Pacritinib (SB1518) ( Figure 3D) is a JAK2/FLT3 inhibitor. Promising results were obtained in phase 1–2 clinical trials. It showed good activity in patients with less immunosuppressive effects 134. Pacritinib could be administered to patients with low platelet levels, as it does not induce thrombocytopenia. The reasons behind this feature are unclear; they could be linked to reduced specificity for MPL/JAK2 complexes. Subsequently, two phase 3 clinical trials (PERSIST 1 and 2) were started with different doses of pacritinib. In 2016, the FDA put a complete clinical hold on the trials because of an excess of intracranial hemorrhage and cardiac failure in treated patients 135. This hold was lifted in 2017 136. As a consequence, CTI BioPharma has just launched the PAC203 study evaluating the effect of pacritinib at different doses.
Fedratinib (TG101348) ( Figure 3D) was assessed during the JAKARTA trials with interesting clinical results, including fibrosis reduction 137– 139, but rare patients developed Wernicke encephalopathy, which led to its stop 139. It was assumed that it was related to an inhibition of thiamine uptake, although fedratinib does not lead to inhibition of thiamine uptake in rats 70, 140. FDA removed the clinical hold in august 2017 and clinical trials are being planned in 2018.
JAK1 inhibition has also been proposed in MPNs, as an anti-inflammatory strategy, and an alternative to JAK2 inhibitors to avoid anemia and thrombocytopenia 65, 66. A preliminary study has produced mixed results with a modest reduction in spleen size 110. Recently, it has been demonstrated that JAK1 plays essential and non-redundant roles at the level of HSC and therefore long-term JAK1 inhibition might have negative effects on HSCs 68.
Other malignant disorders
Ruxolitinib was also used in refractory leukemia, including post-MPN leukemia, and 3 out of 18 patients achieved complete remission 80. Ruxolitinib was unexpectedly used in combination with chemotherapeutic agents in solid cancers (pancreatic and lung cancer) and there was some benefit 141. This was based on JAK1 involvement in the signaling of several cytokine receptors, inflammation, and possibly progression of the malignant clone 81, 142.
Ruxolitinib has been used both in myeloid malignancies with JAK2 fusion proteins and in CNL with a very good initial response but was inefficient to cure the diseases 143– 146.
Itacitinib (INCB39110), which is also a selective JAK1 inhibitor, is being tested in non-small cell lung cancer in combination with an epidermal growth factor receptor inhibitor. Another JAK1 inhibitor, INCB52793, is also in development in advanced malignancies.
Inflammatory and autoimmune diseases
JAK1 inhibitors have been used in inflammatory/immune diseases 67, 147. Tofacitinib was authorized by the FDA in RA 148 but is currently being tested in Crohn’s disease, psoriasis, and other diseases 149, 150. It decreases inflammation particularly by lowering T-cell and macrophage infiltrates. Filgotinib is currently in phase 3 clinical trials in RA and Crohn’s disease and in phase 2 clinical trials in lupus and psoriasis. Itacitinib (INCB39110) is being tested in phase 2 trials in psoriasis and in MF with meaningful improvements.
Ruxolitinib, also a good inhibitor of JAK1, was shown to reduce GVHD in mice and in patients with corticosteroid-refractory GVHD 82, 151. Indeed, in GVHD, severe complications are due to high levels of proinflammatory cytokines that are inhibited by ruxolitinib. Itacitinib will be assessed as monotherapy in GVHD.
A JAK1 inhibitor, PF-04965842, is also in clinical trials in atopic dermatis and severe psoriasis 112. Both topical tofacitinib and ruxolitinib are tested for alopecia and vitiligo.
Baricitinib (Olumiant), a JAK1/2 inhibitor (half maximal inhibitory concentration [IC 50] values of 5.9 and 5.7 nM, respectively), has been initially identified by Incyte and subsequently developed by Eli Lilly and Company for RA. It also inhibits TYK2 (IC 50 of around 53 nM). A phase 3 clinical trial was conducted, and the molecule was approved by the EMA but not yet by the FDA 148, 152. It may be of interest in MPN treatment given its similarities with ruxolitinib but with a longer half-life (12.5 hours). Upadacitinib (ABT-494, AbbVie) is a highly selective JAK1 inhibitor that will enter phase 3 trials for RA, psoriasis, and ulcerative colitis.
Two JAK3 inhibitors were evaluated. ASP015K, also designated JNJ-54781532, displays a moderate selectivity on JAK3 over JAK1 and JAK2. It was shown to induce efficacy and safety in psoriasis 116. It has demonstrated efficacy in preclinical models of RA and dermatitis. Decernolitinib is also a potent and selective inhibitor of JAK3 developed as a second-generation inhibitor in autoimmune diseases, particularly in RA. However, at high doses, it leads to anemia, indicating that its selectivity in vivo could be different 153. In MPNs, these types of inhibitors could also be useful to decrease inflammation, especially in MF.
The major drawback of these JAK1 and JAK3 inhibitors affecting the inflammatory response is that they can induce autoimmune diseases (thyroiditis or myocarditis) or can prime the development of many infections in patients with MPN. Furthermore, it appears that for the IL-2/IL-4/IL-7/IL-9/IL-15/IL-21 complexes, JAK1 is the initiating kinase for signaling, and a JAK3 that is inhibited can still fulfill its scaffolding role in the complex, its inhibition not giving results comparable to the absence of JAK3 by autosomal mutation 154.
Perspectives in JAK inhibition
The goal of JAK2 inhibition in MPNs has switched from a curative therapy to a symptomatic and anti-inflammatory therapy with certain clinical benefits 65. However, this aim is far from what is expected for a targeted therapy 69. Although several in vitro studies identified potential kinase domain mutations that would give resistance to JAK2 inhibitors 155, 156, no such mutations were identified in patients 72, further arguing that the current inhibitors are weak. Thus, there is a need for new inhibitors or combination of therapies.
New inhibitors
First, a new generation of JAK2-specific compounds, including allosteric inhibitors targeting unique sequences in JAK2, should come to light. Such inhibitors would provide more specificity toward JAK2 or JAK2V617F, thereby ameliorating normal JAK2 inhibition-based immune suppression. Two inhibitors have been developed (LS104 and ON044580) that inhibit kinase activities in a non-ATP-competitive manner 118, 119. LS104 preferentially inhibits JAK2V617F kinase and can synergize with ATP-competitive inhibitors 118, whereas ON044580 inhibits BCR-ABL and its T315I mutant 119. The precise targeted residues remain unknown.
Identification of allosteric sites in enzymes has been accomplished for several years and is the basis for the development of a new class of pharmaceuticals. One example is the development of the BCR-ABL allosteric inhibitor GNF-2 that can overcome the effect of resistant mutations and also exhibits an increased potency when used in combination with classic ATP-competitive inhibitors 157. Another example is the development of MEK allosteric inhibitors. It was shown that analogues of PD184352 could specifically bind to a unique region adjacent to the ATP pocket created by the displacement of the helix αC of the kinase in the active conformation 158.
As the main conformational difference between JAK2V617F and JAK2WT is around the helix αC of the pseudokinase JH2 domain 159, a rational design of similar molecules targeting this region could be efficient ( Figure 4). Recent structural and mechanistic data on JH2 V617F might help in designing such small molecules. Moreover, targeting JH2 might become feasible as shown by the recent publication of co-crystals of JH2 with several compounds. Future therapeutics should target small conformational changes that are specific for a particular mutant protein or its constitutive activity.
Figure 4. Graphic representation of the V617F-activation mechanism in Janus kinase2 (JAK2).
The V617F activation has been suggested to derive from a combination of several molecular events triggered from a region surrounding the JH2 αC but also involving the SH2-JH2 linker. Phenylalanine 617 interacts with F594 and F595 from the JH2 αC and F537 from the SH2-JH2 linker, as supported by structural data 9, 159, then induces putative conformational changes that are transmitted to the adjacent catalytic kinase domain where activation is initiated. Targeting the ATP-binding pocket of JH2 that is spatially close the αC represents an appealing approach for specific targeting of the mutant JAK2V617F. Small molecules, such as BI-D1870 (as represented here 160), have been co-crystallized as bound to the JH2 ATP-binding site. The use of amendable compounds targeting the JH2 pocket has recently become a tantalizing concept and will represent the future challenge for drug design.
The activating mutation, JAK2V617F, is located in the pseudokinase domain of JAK2 and allosterically regulates the activity of JAK2 kinase domain. Another strategy would be to interrupt these specific intramolecular changes induced by V617F on the kinase domain of JAK2. The aromatic phenylalanine at position 617 interacts with the αC helix phenylalanines 594 and 595 161 and with phenylalanine 537 from the SH2-JH2 linker 9 to produce an autonomous activation to the adjacent catalytically active domain, JH1 ( Figure 4). Both of these aberrant hydrophobic contacts induce critical conformational changes that can be visualized on the JH2 V617F crystal structures 9, 159. Any small molecules that would interfere with these specific atomic configurations exclusively present in the conformation of JAK2V617F would most likely generate mutant-specific inhibitors. Evidence was provided that V617F activates JAK2 through a community of residues across JAK2 (from JH2 to JH1 through the SH2-JH2 linker) and that reversing the charge of the negative residue, E596, located on the solvent-exposed face of the JH2 αC helix, can efficiently uncouple JAK2V617F activation from cytokine-induced activation, thereby restoring auto-inhibition of JAK2.
Finally, methotrexate, a well-known drug used in autoimmune disease was shown to also inhibit the JAK/STAT pathway and in theory could be tested for selective effects on the MPN clones 162. An advantage of this treatment is its low cost, while its side effects are well known.
Combination of therapies
The goal of certain combinations is to improve the anemia of MF, which can be worsened by ruxolitinib 65. Trials have been performed in combination with androgen without benefit. Trials are ongoing with pomalidomide or thalidomide and also with sotartercept, an activin receptor IIa ligand trap 163. Treatment with erythropoiesis-stimulating agents is also conceivable, although they are theoretically antagonistic with JAK2 inhibitors 164.
Downstream JAK2 are activations of STATs, PI3K-AKT/mTOR, and RAS-MAPK ERK1/2 ( Figure 2) 165. Specific inhibitors of STAT5 and STAT3 are now being tested in preclinical studies 166. A combination of JAK2 and STAT5 inhibitors might be effective in MPNs. In preclinical models, JAK2 and pan type I PI3K and mTOR inhibitors synergize to block JAK2V617F-induced proliferation 167, 168 but less on mutant CALR-induced proliferation 18. Other molecules involved in the inhibition of the PI3K, AKT, or mTOR pathway were tested in preclinical models or clinical trials.
The HSP90 chaperone is involved in JAK2 stability and is controlled via its acetylation status 169. HSP90 inhibitors or histone deacetylase inhibitors were tested 169. Notably, panobinostat and pracinostat were studied in combination with ruxolitinib in a phase 2 trial with a better spleen response in MF 170. Furthermore, a preliminary trial using an HSP90 inhibitor showed some clinical benefit 171. Combinations of ruxolitinib with CDK4/6 inhibitors, PIM1 kinase inhibitors, BH3 mimetics, or MDM2 inhibitors appear logical because they target molecules, which are downstream of JAK2 signaling, thus curbing any residual activation due to incomplete JAK2 inhibition due to short half-life of inhibitor and type I inhibition mechanism that allows rapid reactivation. Intriguingly, it has been reported that an association of ruxolitinib with pegylated interferon alpha was synergistic in a preliminary clinical trial, and a new larger clinical trial is ongoing 172. Normally, a JAK1 inhibitor should decrease interferon alpha signaling and should limit the effects of pegylated interferon; thus, the synergy might reflect how inefficiently ruxolitinib can actually inhibit JAKs in vivo. The main risk of all these different associations is to induce important cytopenia.
In MF, it has also been suggested to combine ruxolitinib with MEK inhibitors and PRM-151, a molecule that inhibits differentiation of fibrocytes 173, which are implicated in fibrosis development 174. Both drugs exhibit an effect on bone marrow fibrosis in preclinical studies or in clinical trials 175. An inhibitor of hedgehog signaling pathway (LDE225) was also tested in phase I in ET/PV and MF with disappointing results 176. However, recent evidence points to targeting Gli1 in association with ruxolitinib because Gli1 + mesenchymal cells may play a central role in fibrosis development 177.
JAK2V617F can increase the protein methylation demonstrated by activation of PRMT5 arginine methyltransferase 178. It also prevents the binding of heterochromatin factor HP1 to chromatin 179. It is possible that some key genes could be hypermethylated as in many cancers. Therefore, it was postulated that demethylating agents such azacytidine and decitabine may have some impact. However, administered alone, they showed minor responses in two clinical trials 180, 181. They were thus combined with ruxolitinib in a few patients with MF and the clinical response was good.
Conclusions
After the discovery of JAK2V617F and the demonstration that BCR-ABL–negative MPNs are driven by abnormal JAK2 activation, there were curative expectations for JAK inhibitors. Despite nearly 10 years of development in MPNs, only one JAK2 inhibitor (ruxolitinib) has been clinically approved. Most other inhibitors had their development stopped because of neurotoxicity or the absence of superiority compared with ruxolitinib. Only pacritinib ( Figure 3B) is still in phase 3 clinical testing and fedratinib is being reevaluated. Although ruxolitinib offers clear benefits for patients, its effects are quite limited on the disease itself in MF. On one hand, this may be explained by the additional mutations detected by MF clones, which act independently from JAK2 and which place MF at the boundary between MPN and MDS. On the other hand, ruxolitinib has a short half-life and acts as a type I inhibitor, which means that each time inhibitor is consumed, re-activation of JAK2 will occur.
Thus, it seems important in PV and ET, which are JAK2-dependent MPNs, to obtain specific inhibitors of JAK2V617F or even to preferentially target the constitutive active JAK2 over cytokine-activated JAK2 in the cases of mutated MPL and CALR ET and MF. It is expected that such inhibitors will be less toxic and will really target the clonal disease. In MF, the low-hanging fruit of combination therapies could be a valuable approach that holds a risk for significant toxicities.
An important finding of the clinical trials in MPNs was the discovery that JAK inhibition is a valuable approach for treatment of inflammatory diseases. Thus, it can be expected that one of the main applications of JAK inhibitors will be for inflammatory diseases, autoimmune diseases, and possibly other diseases, which may include an inflammatory response, including neurodegenerative disorders or cancers where inflammation contributes to oncogenesis.
Editorial Note on the Review Process
F1000 Faculty Reviews are commissioned from members of the prestigious F1000 Faculty and are edited as a service to readers. In order to make these reviews as comprehensive and accessible as possible, the referees provide input before publication and only the final, revised version is published. The referees who approved the final version are listed with their names and affiliations but without their reports on earlier versions (any comments will already have been addressed in the published version).
The referees who approved this article are:
Srdan Verstovsek, Division of Cancer Medicine, Department of Leukemia, The University of Texas MD Anderson Cancer Center, Houston, USA
Ann Mullally, Division of Hematology, Department of Medicine, Brigham and Women's Hospital, Harvard Medical School, Boston, USA
Funding Statement
This work was supported by grants from Ligue Nationale Contre le Cancer (‘Equipe labellisée 2016’ to WV and IP), Institut National du Cancer (PLBIO2015 to IP), MPN Research Foundation (IP), and Institut National de la Santé et de la Recherche Médicale (Inserm). The Laboratory of Excellence Globule Rouge-Excellence (IP and WV) is funded by the program ‘Investissements d’avenir’. SNC has received funding from the Ludwig Institute for Cancer Research, FRS-FNRS, Salus Sanguinis, Fondation contre le cancer, Project Action de Recherche Concerte of the Université Catholique de Louvain ARC10/15-027, the PAI (Interuniversity Support Program) Belgian Medical Genetics Initiative, and the Foundation ‘Les avions de Sébastien’ (Belgium).
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 1; referees: 2 approved]
References
- 1. Ihle JN: The Janus protein tyrosine kinases in hematopoietic cytokine signaling. Semin Immunol. 1995;7(4):247–54. 10.1006/smim.1995.0029 [DOI] [PubMed] [Google Scholar]
- 2. Constantinescu SN, Ghaffari S, Lodish HF: The Erythropoietin Receptor: Structure, Activation and Intracellular Signal Transduction. Trends Endocrinol Metab. 1999;10(1):18–23. 10.1016/S1043-2760(98)00101-5 [DOI] [PubMed] [Google Scholar]
- 3. Vainchenker W, Constantinescu SN: JAK/STAT signaling in hematological malignancies. Oncogene. 2013;32(21):2601–13. 10.1038/onc.2012.347 [DOI] [PubMed] [Google Scholar]
- 4. Rampal R, Al-Shahrour F, Abdel-Wahab O, et al. : Integrated genomic analysis illustrates the central role of JAK-STAT pathway activation in myeloproliferative neoplasm pathogenesis. Blood. 2014;123(22):e123–33. 10.1182/blood-2014-02-554634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vainchenker W, Constantinescu SN, Plo I: Recent advances in understanding myelofibrosis and essential thrombocythemia [version 1; referees: 2 approved]. F1000Res. 2016;5: pii: F1000 Faculty Rev-700. 10.12688/f1000research.8081.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Huang LJ, Constantinescu SN, Lodish HF: The N-terminal domain of Janus kinase 2 is required for Golgi processing and cell surface expression of erythropoietin receptor. Mol Cell. 2001;8(6):1327–38. 10.1016/S1097-2765(01)00401-4 [DOI] [PubMed] [Google Scholar]
- 7. Ferrao R, Lupardus PJ: The Janus Kinase (JAK) FERM and SH2 Domains: Bringing Specificity to JAK-Receptor Interactions. Front Endocrinol (Lausanne). 2017;8:71. 10.3389/fendo.2017.00071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Leroy E, Dusa A, Colau D, et al. : Uncoupling JAK2 V617F activation from cytokine-induced signalling by modulation of JH2 αC helix. Biochem J. 2016;473(11):1579–91. 10.1042/BCJ20160085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Toms AV, Deshpande A, McNally R, et al. : Structure of a pseudokinase-domain switch that controls oncogenic activation of Jak kinases. Nat Struct Mol Biol. 2013;20(10):1221–3. 10.1038/nsmb.2673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Silvennoinen O, Ungureanu D, Niranjan Y, et al. : New insights into the structure and function of the pseudokinase domain in JAK2. Biochem Soc Trans. 2013;41(4):1002–7. 10.1042/BST20130005 [DOI] [PubMed] [Google Scholar]
- 11. Royer Y, Staerk J, Costuleanu M, et al. : Janus kinases affect thrombopoietin receptor cell surface localization and stability. J Biol Chem. 2005;280(29):27251–61. 10.1074/jbc.M501376200 [DOI] [PubMed] [Google Scholar]
- 12. Verstovsek S, Talpaz M, Ritchie EK, et al. : Phase 1/2 Study of NS-018, an Oral JAK2 Inhibitor, in Patients with Primary Myelofibrosis (PMF), Post-Polycythemia Vera Myelofibrosis (postPV MF), or Post-Essential Thrombocythemia Myelofibrosis (postET MF). Blood, 58th Annual Meeting and Exposition of the American-Society-of-Hematology, San Diego, CA.2016;128(22):1936 Reference Source [Google Scholar]
- 13. Duan Y, Chen L, Chen Y, et al. : c-Src binds to the cancer drug Ruxolitinib with an active conformation. PLoS One. 2014;9(9):e106225. 10.1371/journal.pone.0106225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Andraos R, Qian Z, Bonenfant D, et al. : Modulation of activation-loop phosphorylation by JAK inhibitors is binding mode dependent. Cancer Discov. 2012;2(6):512–23. 10.1158/2159-8290.CD-11-0324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vainchenker W, Kralovics R: Genetic basis and molecular pathophysiology of classical myeloproliferative neoplasms. Blood. 2017;129(6):667–79. 10.1182/blood-2016-10-695940 [DOI] [PubMed] [Google Scholar]
- 16. Klampfl T, Gisslinger H, Harutyunyan AS, et al. : Somatic mutations of calreticulin in myeloproliferative neoplasms. N Engl J Med. 2013;369(25):2379–90. 10.1056/NEJMoa1311347 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 17. Nangalia J, Massie CE, Baxter EJ, et al. : Somatic CALR mutations in myeloproliferative neoplasms with nonmutated JAK2. N Engl J Med. 2013;369(25):2391–405. 10.1056/NEJMoa1312542 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 18. Chachoua I, Pecquet C, El-Khoury M, et al. : Thrombopoietin receptor activation by myeloproliferative neoplasm associated calreticulin mutants. Blood. 2016;127(10):1325–35. 10.1182/blood-2015-11-681932 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 19. Marty C, Pecquet C, Nivarthi H, et al. : Calreticulin mutants in mice induce an MPL-dependent thrombocytosis with frequent progression to myelofibrosis. Blood. 2016;127(10):1317–24. 10.1182/blood-2015-11-679571 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 20. Elf S, Abdelfattah NS, Chen E, et al. : Mutant Calreticulin Requires Both Its Mutant C-terminus and the Thrombopoietin Receptor for Oncogenic Transformation. Cancer Discov. 2016;6(4):368–81. 10.1158/2159-8290.CD-15-1434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Araki M, Yang Y, Masubuchi N, et al. : Activation of the thrombopoietin receptor by mutant calreticulin in CALR-mutant myeloproliferative neoplasms. Blood. 2016;127(10):1307–16. 10.1182/blood-2015-09-671172 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 22. Lu X, Huang LJ, Lodish HF: Dimerization by a cytokine receptor is necessary for constitutive activation of JAK2V617F. J Biol Chem. 2008;283(9):5258–66. 10.1074/jbc.M707125200 [DOI] [PubMed] [Google Scholar]
- 23. Oh ST, Simonds EF, Jones C, et al. : Novel mutations in the inhibitory adaptor protein LNK drive JAK-STAT signaling in patients with myeloproliferative neoplasms. Blood. 2010;116(6):988–92. 10.1182/blood-2010-02-270108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lasho TL, Pardanani A, Tefferi A: LNK mutations in JAK2 mutation-negative erythrocytosis. N Engl J Med. 2010;363(12):1189–90. 10.1056/NEJMc1006966 [DOI] [PubMed] [Google Scholar]
- 25. Rumi E, Harutyunyan AS, Pietra D, et al. : LNK mutations in familial myeloproliferative neoplasms. Blood. 2016;128(1):144–5. 10.1182/blood-2016-04-711150 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 26. Nangalia J, Grinfeld J, Green AR: Pathogenesis of Myeloproliferative Disorders. Annu Rev Pathol. 2016;11:101–26. 10.1146/annurev-pathol-012615-044454 [DOI] [PubMed] [Google Scholar]
- 27. Viny AD, Levine RL: Genetics of myeloproliferative neoplasms. Cancer J. 2014;20(1):61–5. 10.1097/PPO.0000000000000013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Delhommeau F, Dupont S, Della Valle V, et al. : Mutation in TET2 in myeloid cancers. N Engl J Med. 2009;360(22):2289–301. 10.1056/NEJMoa0810069 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 29. Saint-Martin C, Leroy G, Delhommeau F, et al. : Analysis of the ten-eleven translocation 2 ( TET2) gene in familial myeloproliferative neoplasms. Blood. 2009;114(8):1628–32. 10.1182/blood-2009-01-197525 [DOI] [PubMed] [Google Scholar]
- 30. Ortmann CA, Kent DG, Nangalia J, et al. : Effect of mutation order on myeloproliferative neoplasms. N Engl J Med. 2015;372(7):601–12. 10.1056/NEJMoa1412098 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 31. Shimizu T, Kubovcakova L, Nienhold R, et al. : Loss of Ezh2 synergizes with JAK2-V617F in initiating myeloproliferative neoplasms and promoting myelofibrosis. J Exp Med. 2016;213(8):1479–96. 10.1084/jem.20151136 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 32. Guglielmelli P, Lasho TL, Rotunno G, et al. : The number of prognostically detrimental mutations and prognosis in primary myelofibrosis: an international study of 797 patients. Leukemia. 2014;28(9):1804–10. 10.1038/leu.2014.76 [DOI] [PubMed] [Google Scholar]
- 33. Tefferi A, Vannucchi AM: Genetic Risk Assessment in Myeloproliferative Neoplasms. Mayo Clin Proc. 2017;92(8):1283–90. 10.1016/j.mayocp.2017.06.002 [DOI] [PubMed] [Google Scholar]
- 34. Griesinger F, Hennig H, Hillmer F, et al. : A BCR-JAK2 fusion gene as the result of a t(9;22)(p24;q11.2) translocation in a patient with a clinically typical chronic myeloid leukemia. Genes Chromosomes Cancer. 2005;44(3):329–33. 10.1002/gcc.20235 [DOI] [PubMed] [Google Scholar]
- 35. Mark HF, Sotomayor EA, Nelson M, et al. : Chronic idiopathic myelofibrosis (CIMF) resulting from a unique 3;9 translocation disrupting the janus kinase 2 (JAK2) gene. Exp Mol Pathol. 2006;81(3):217–23. 10.1016/j.yexmp.2006.07.004 [DOI] [PubMed] [Google Scholar]
- 36. Peeters P, Raynaud SD, Cools J, et al. : Fusion of TEL the ETS-variant gene 6 ( ETV6), to the receptor-associated kinase JAK2 as a result of t(9;12) in a lymphoid and t(9;15;12) in a myeloid leukemia. Blood. 1997;90(7):2535–40. [PubMed] [Google Scholar]
- 37. Reiter A, Walz C, Watmore A, et al. : The t(8;9)(p22;p24) is a recurrent abnormality in chronic and acute leukemia that fuses PCM1 to JAK2. Cancer Res. 2005;65(7):2662–7. 10.1158/0008-5472.CAN-04-4263 [DOI] [PubMed] [Google Scholar]
- 38. Maxson JE, Gotlib J, Pollyea DA, et al. : Oncogenic CSF3R mutations in chronic neutrophilic leukemia and atypical CML. N Engl J Med. 2013;368(19):1781–90. 10.1056/NEJMoa1214514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Patnaik MM, Tefferi A: Refractory anemia with ring sideroblasts (RARS) and RARS with thrombocytosis (RARS-T): 2017 update on diagnosis, risk-stratification, and management. Am J Hematol. 2017;92(3):297–310. 10.1002/ajh.24637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Yoshida K, Toki T, Okuno Y, et al. : The landscape of somatic mutations in Down syndrome-related myeloid disorders. Nat Genet. 2013;45(11):1293–9. 10.1038/ng.2759 [DOI] [PubMed] [Google Scholar]
- 41. Malinge S, Ragu C, Della-Valle V, et al. : Activating mutations in human acute megakaryoblastic leukemia. Blood. 2008;112(10):4220–6. 10.1182/blood-2008-01-136366 [DOI] [PubMed] [Google Scholar]
- 42. Mullighan CG: The molecular genetic makeup of acute lymphoblastic leukemia. Hematology Am Soc Hematol Educ Program. 2012;2012:389–96. [DOI] [PubMed] [Google Scholar]
- 43. Mullighan CG, Collins-Underwood JR, Phillips LA, et al. : Rearrangement of CRLF2 in B-progenitor- and Down syndrome-associated acute lymphoblastic leukemia. Nat Genet. 2009;41(11):1243–6. 10.1038/ng.469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mullighan CG, Zhang J, Harvey RC, et al. : JAK mutations in high-risk childhood acute lymphoblastic leukemia. Proc Natl Acad Sci U S A. 2009;106(23):9414–8. 10.1073/pnas.0811761106 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 45. Malinge S, Ben-Abdelali R, Settegrana C, et al. : Novel activating JAK2 mutation in a patient with Down syndrome and B-cell precursor acute lymphoblastic leukemia. Blood. 2007;109(5):2202–4. 10.1182/blood-2006-09-045963 [DOI] [PubMed] [Google Scholar]
- 46. Flex E, Petrangeli V, Stella L, et al. : Somatically acquired JAK1 mutations in adult acute lymphoblastic leukemia. J Exp Med. 2008;205(4):751–8. 10.1084/jem.20072182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hornakova T, Staerk J, Royer Y, et al. : Acute lymphoblastic leukemia-associated JAK1 mutants activate the Janus kinase/STAT pathway via interleukin-9 receptor alpha homodimers. J Biol Chem. 2009;284(11):6773–81. 10.1074/jbc.M807531200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Tasian SK, Loh ML: Understanding the biology of CRLF2-overexpressing acute lymphoblastic leukemia. Crit Rev Oncog. 2011;16(1–2):13–24. 10.1615/CritRevOncog.v16.i1-2.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hertzberg L, Vendramini E, Ganmore I, et al. : Down syndrome acute lymphoblastic leukemia, a highly heterogeneous disease in which aberrant expression of CRLF2 is associated with mutated JAK2: a report from the International BFM Study Group. Blood. 2010;115(5):1006–17. 10.1182/blood-2009-08-235408 [DOI] [PubMed] [Google Scholar]
- 50. Shochat C, Tal N, Bandapalli OR, et al. : Gain-of-function mutations in interleukin-7 receptor-α ( IL7R) in childhood acute lymphoblastic leukemias. J Exp Med. 2011;208(5):901–8. 10.1084/jem.20110580 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 51. Iacobucci I, Li Y, Roberts KG, et al. : Truncating Erythropoietin Receptor Rearrangements in Acute Lymphoblastic Leukemia. Cancer Cell. 2016;29(2):186–200. 10.1016/j.ccell.2015.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Neumann M, Greif PA, Baldus CD: Mutational landscape of adult ETP-ALL. Oncotarget. 2013;4(7):954–5. 10.18632/oncotarget.1106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Rui L, Emre NC, Kruhlak MJ, et al. : Cooperative epigenetic modulation by cancer amplicon genes. Cancer Cell. 2010;18(6):590–605. 10.1016/j.ccr.2010.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Gunawardana J, Chan FC, Telenius A, et al. : Recurrent somatic mutations of PTPN1 in primary mediastinal B cell lymphoma and Hodgkin lymphoma. Nat Genet. 2014;46(4):329–35. 10.1038/ng.2900 [DOI] [PubMed] [Google Scholar]
- 55. Van Roosbroeck K, Cox L, Tousseyn T, et al. : JAK2 rearrangements, including the novel SEC31A-JAK2 fusion, are recurrent in classical Hodgkin lymphoma. Blood. 2011;117(15):4056–64. 10.1182/blood-2010-06-291310 [DOI] [PubMed] [Google Scholar]
- 56. Bellanger D, Jacquemin V, Chopin M, et al. : Recurrent JAK1 and JAK3 somatic mutations in T-cell prolymphocytic leukemia. Leukemia. 2014;28(2):417–9. 10.1038/leu.2013.271 [DOI] [PubMed] [Google Scholar]
- 57. Lee S, Park HY, Kang SY, et al. : Genetic alterations of JAK/STAT cascade and histone modification in extranodal NK/T-cell lymphoma nasal type. Oncotarget. 2015;6(19):17764–76. 10.18632/oncotarget.3776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Ngo VN, Young RM, Schmitz R, et al. : Oncogenically active MYD88 mutations in human lymphoma. Nature. 2011;470(7332):115–9. 10.1038/nature09671 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 59. Plo I, Bellanné-Chantelot C, Mosca M, et al. : Genetic Alterations of the Thrombopoietin/MPL/JAK2 Axis Impacting Megakaryopoiesis. Front Endocrinol (Lausanne). 2017;8:234. 10.3389/fendo.2017.00234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Hong WJ, Gotlib J: Hereditary erythrocytosis, thrombocytosis and neutrophilia. Best Pract Res Clin Haematol. 2014;27(2):95–106. 10.1016/j.beha.2014.07.002 [DOI] [PubMed] [Google Scholar]
- 61. Plo I, Zhang Y, Le Couédic JP, et al. : An activating mutation in the CSF3R gene induces a hereditary chronic neutrophilia. J Exp Med. 2009;206(8):1701–7. 10.1084/jem.20090693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Clark JD, Flanagan ME, Telliez JB: Discovery and development of Janus kinase (JAK) inhibitors for inflammatory diseases. J Med Chem. 2014;57(12):5023–38. 10.1021/jm401490p [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 63. Choi J, Ziga ED, Ritchey J, et al. : IFNγR signaling mediates alloreactive T-cell trafficking and GVHD. Blood. 2012;120(19):4093–103. 10.1182/blood-2012-01-403196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Leroy E, Constantinescu SN: Rethinking JAK2 inhibition: towards novel strategies of more specific and versatile janus kinase inhibition. Leukemia. 2017;31(5):1023–38. 10.1038/leu.2017.43 [DOI] [PubMed] [Google Scholar]
- 65. Bose P, Verstovsek S: JAK2 inhibitors for myeloproliferative neoplasms: what is next? Blood. 2017;130(2):115–25. 10.1182/blood-2017-04-742288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Tefferi A: Challenges facing JAK inhibitor therapy for myeloproliferative neoplasms. N Engl J Med. 2012;366(9):844–6. 10.1056/NEJMe1115119 [DOI] [PubMed] [Google Scholar]
- 67. Schwartz DM, Bonelli M, Gadina M, et al. : Type I/II cytokines, JAKs, and new strategies for treating autoimmune diseases. Nat Rev Rheumatol. 2016;12(1):25–36. 10.1038/nrrheum.2015.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Kleppe M, Spitzer MH, Li S, et al. : Jak1 Integrates Cytokine Sensing to Regulate Hematopoietic Stem Cell Function and Stress Hematopoiesis. Cell Stem Cell. 2017;21(4):489–501.e7. 10.1016/j.stem.2017.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 69. Tefferi A: JAK inhibitors for myeloproliferative neoplasms: clarifying facts from myths. Blood. 2012;119(12):2721–30. 10.1182/blood-2011-11-395228 [DOI] [PubMed] [Google Scholar]
- 70. Zhang Q, Zhang Y, Diamond S, et al. : The Janus kinase 2 inhibitor fedratinib inhibits thiamine uptake: a putative mechanism for the onset of Wernicke's encephalopathy. Drug Metab Dispos. 2014;42(10):1656–62. 10.1124/dmd.114.058883 [DOI] [PubMed] [Google Scholar]
- 71. Fleischmann R: Tofacitinib in the treatment of active rheumatoid arthritis in adults. Immunotherapy. 2018;10(1):39–56. 10.2217/imt-2017-0118 [DOI] [PubMed] [Google Scholar]
- 72. Koppikar P, Bhagwat N, Kilpivaara O, et al. : Heterodimeric JAK-STAT activation as a mechanism of persistence to JAK2 inhibitor therapy. Nature. 2012;489(7414):155–9. 10.1038/nature11303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Meyer SC, Levine RL: Molecular pathways: molecular basis for sensitivity and resistance to JAK kinase inhibitors. Clin Cancer Res. 2014;20(8):2051–9. 10.1158/1078-0432.CCR-13-0279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Blanc J, Geney R, Menet C: Type II kinase inhibitors: an opportunity in cancer for rational design. Anticancer Agents Med Chem. 2013;13(5):731–47. 10.2174/1871520611313050008 [DOI] [PubMed] [Google Scholar]
- 75. Meyer SC, Keller MD, Chiu S, et al. : CHZ868, a Type II JAK2 Inhibitor, Reverses Type I JAK Inhibitor Persistence and Demonstrates Efficacy in Myeloproliferative Neoplasms. Cancer Cell. 2015;28(1):15–28. 10.1016/j.ccell.2015.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 76. Wu SC, Li LS, Kopp N, et al. : Activity of the Type II JAK2 Inhibitor CHZ868 in B Cell Acute Lymphoblastic Leukemia. Cancer Cell. 2015;28(1):29–41. 10.1016/j.ccell.2015.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 77. Harrison C, Kiladjian JJ, Al-Ali HK, et al. : JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis. N Engl J Med. 2012;366(9):787–98. 10.1056/NEJMoa1110556 [DOI] [PubMed] [Google Scholar]
- 78. Vannucchi AM, Kiladjian JJ, Griesshammer M, et al. : Ruxolitinib versus standard therapy for the treatment of polycythemia vera. N Engl J Med. 2015;372(5):426–35. 10.1056/NEJMoa1409002 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 79. Verstovsek S, Mesa RA, Gotlib J, et al. : A double-blind, placebo-controlled trial of ruxolitinib for myelofibrosis. N Engl J Med. 2012;366(9):799–807. 10.1056/NEJMoa1110557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Eghtedar A, Verstovsek S, Estrov Z, et al. : Phase 2 study of the JAK kinase inhibitor ruxolitinib in patients with refractory leukemias, including postmyeloproliferative neoplasm acute myeloid leukemia. Blood. 2012;119(20):4614–8. 10.1182/blood-2011-12-400051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Hurwitz HI, Uppal N, Wagner SA, et al. : Randomized, Double-Blind, Phase II Study of Ruxolitinib or Placebo in Combination With Capecitabine in Patients With Metastatic Pancreatic Cancer for Whom Therapy With Gemcitabine Has Failed. J Clin Oncol. 2015;33(34):4039–47. 10.1200/JCO.2015.61.4578 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 82. Zeiser R, Burchert A, Lengerke C, et al. : Ruxolitinib in corticosteroid-refractory graft-versus-host disease after allogeneic stem cell transplantation: a multicenter survey. Leukemia. 2015;29(10):2062–8. 10.1038/leu.2015.212 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 83. Punwani N, Scherle P, Flores R, et al. : Preliminary clinical activity of a topical JAK1/2 inhibitor in the treatment of psoriasis. J Am Acad Dermatol. 2012;67(4):658–64. 10.1016/j.jaad.2011.12.018 [DOI] [PubMed] [Google Scholar]
- 84. Mackay-Wiggan J, Jabbari A, Nguyen N, et al. : Oral ruxolitinib induces hair regrowth in patients with moderate-to-severe alopecia areata. JCI Insight. 2016;1(15):e89790. 10.1172/jci.insight.89790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Harris JE, Rashighi M, Nguyen N, et al. : Rapid skin repigmentation on oral ruxolitinib in a patient with coexistent vitiligo and alopecia areata (AA). J Am Acad Dermatol. 2016;74(2):370–1. 10.1016/j.jaad.2015.09.073 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 86. Mesa RA, Kiladjian JJ, Catalano JV, et al. : SIMPLIFY-1: A Phase III Randomized Trial of Momelotinib Versus Ruxolitinib in Janus Kinase Inhibitor-Naïve Patients With Myelofibrosis. J Clin Oncol. 2017;35(34):3844–50. 10.1200/JCO.2017.73.4418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Verstovsek S, Courby S, Griesshammer M, et al. : A phase 2 study of momelotinib, a potent JAK1 and JAK2 inhibitor, in patients with polycythemia vera or essential thrombocythemia. Leuk Res. 2017;60:11–7. 10.1016/j.leukres.2017.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Verstovsek S, Hoffman R, Mascarenhas J, et al. : A phase I, open-label, multi-center study of the JAK2 inhibitor AZD1480 in patients with myelofibrosis. Leuk Res. 2015;39(2):157–63. 10.1016/j.leukres.2014.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Suryani S, Bracken LS, Harvey RC, et al. : Evaluation of the in vitro and in vivo efficacy of the JAK inhibitor AZD1480 against JAK-mutated acute lymphoblastic leukemia. Mol Cancer Ther. 2015;14(2):364–74. 10.1158/1535-7163.MCT-14-0647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Plimack ER, Lorusso PM, McCoon P, et al. : AZD1480: a phase I study of a novel JAK2 inhibitor in solid tumors. Oncologist. 2013;18(7):819–20. 10.1634/theoncologist.2013-0198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Keystone EC, Taylor PC, Tanaka Y, et al. : Patient-reported outcomes from a phase 3 study of baricitinib versus placebo or adalimumab in rheumatoid arthritis: secondary analyses from the RA-BEAM study. Ann Rheum Dis. 2017;76(11):1853–61. 10.1136/annrheumdis-2017-211259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Papp KA, Menter MA, Raman M, et al. : A randomized phase 2b trial of baricitinib, an oral Janus kinase (JAK) 1/JAK2 inhibitor, in patients with moderate-to-severe psoriasis. Br J Dermatol. 2016;174(6):1266–76. 10.1111/bjd.14403 [DOI] [PubMed] [Google Scholar]
- 93. NICE issues positive recommendation for XELJANZ®▼(tofacitinib citrate) as a new treatment option for adults with severe rheumatoid arthritis. Rheumatology (Oxford). 2017;56(12):e49. 10.1093/rheumatology/kex407 [DOI] [PubMed] [Google Scholar]
- 94. Panés J, Sandborn WJ, Schreiber S, et al. : Tofacitinib for induction and maintenance therapy of Crohn's disease: results of two phase IIb randomised placebo-controlled trials. Gut. 2017;66(6):1049–59. 10.1136/gutjnl-2016-312735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Feldman SR, Thaçi D, Gooderham M, et al. : Tofacitinib improves pruritus and health-related quality of life up to 52 weeks: Results from 2 randomized phase III trials in patients with moderate to severe plaque psoriasis. J Am Acad Dermatol. 2016;75(6):1162–1170.e3. 10.1016/j.jaad.2016.07.040 [DOI] [PubMed] [Google Scholar]
- 96. Vu M, Heyes C, Robertson SJ, et al. : Oral tofacitinib: a promising treatment in atopic dermatitis, alopecia areata and vitiligo. Clin Exp Dermatol. 2017;42(8):942–4. 10.1111/ced.13290 [DOI] [PubMed] [Google Scholar]
- 97. Verstovsek S, Mesa RA, Salama ME, et al. : A phase 1 study of the Janus kinase 2 (JAK2) V617F inhibitor, gandotinib (LY2784544), in patients with primary myelofibrosis, polycythemia vera, and essential thrombocythemia. Leuk Res. 2017;61:89–95. 10.1016/j.leukres.2017.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 98. Verstovsek S, Tam CS, Wadleigh M, et al. : Phase I evaluation of XL019, an oral, potent, and selective JAK2 inhibitor. Leuk Res. 2014;38(3):316–22. 10.1016/j.leukres.2013.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Baffert F, Régnier CH, De Pover A, et al. : Potent and selective inhibition of polycythemia by the quinoxaline JAK2 inhibitor NVP-BSK805. Mol Cancer Ther. 2010;9(7):1945–55. 10.1158/1535-7163.MCT-10-0053 [DOI] [PubMed] [Google Scholar]
- 100. Nakaya Y, Shide K, Niwa T, et al. : Efficacy of NS-018, a potent and selective JAK2/Src inhibitor, in primary cells and mouse models of myeloproliferative neoplasms. Blood Cancer J. 2011;1(7):e29. 10.1038/bcj.2011.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Mesa RA, Vannucchi AM, Mead A, et al. : Pacritinib versus best available therapy for the treatment of myelofibrosis irrespective of baseline cytopenias (PERSIST-1): an international, randomised, phase 3 trial. Lancet Haematol. 2017;4(5):e225–e236. 10.1016/S2352-3026(17)30027-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Mascarenhas J, Hoffman R, Talpaz M, et al. : Results of the Persist-2 Phase 3 Study of Pacritinib (PAC) versus Best Available Therapy (BAT), including Ruxolitinib (RUX), in Patients with Myelofibrosis and Platelet Counts <100,000/μL. Blood, 58th AmericanSociety of Hematology (ASH) Annual Meeting, 3–6 Dec 2016, San Diego.2016. Reference Source [Google Scholar]
- 103. Stump KL, Lu LD, Dobrzanski P, et al. : A highly selective, orally active inhibitor of Janus kinase 2, CEP-33779, ablates disease in two mouse models of rheumatoid arthritis. Arthritis Res Ther. 2011;13(2):R68. 10.1186/ar3329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Ringel F, Kaeda J, Schwarz M, et al. : Effects of Jak2 type 1 inhibitors NVP-BSK805 and NVP-BVB808 on Jak2 mutation-positive and Bcr-Abl-positive cell lines. Acta Haematol. 2014;132(1):75–86. 10.1159/000356784 [DOI] [PubMed] [Google Scholar]
- 105. Pardanani A, Hood J, Lasho T, et al. : TG101209, a small molecule JAK2-selective kinase inhibitor potently inhibits myeloproliferative disorder-associated JAK2V617F and MPLW515L/K mutations. Leukemia. 2007;21(8):1658–68. 10.1038/sj.leu.2404750 [DOI] [PubMed] [Google Scholar]
- 106. Pardanani A, Tefferi A, Jamieson C, et al. : A phase 2 randomized dose-ranging study of the JAK2-selective inhibitor fedratinib (SAR302503) in patients with myelofibrosis. Blood Cancer J. 2015;5(8):e335. 10.1038/bcj.2015.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Vanhoutte F, Mazur M, Voloshyn O, et al. : Efficacy, Safety, Pharmacokinetics, and Pharmacodynamics of Filgotinib, a Selective JAK-1 Inhibitor, After Short-Term Treatment of Rheumatoid Arthritis: Results of Two Randomized Phase IIa Trials. Arthritis Rheumatol. 2017;69(10):1949–59. 10.1002/art.40186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Vermeire S, Schreiber S, Petryka R, et al. : Clinical remission in patients with moderate-to-severe Crohn's disease treated with filgotinib (the FITZROY study): results from a phase 2, double-blind, randomised, placebo-controlled trial. Lancet. 2017;389(10066):266–75. 10.1016/S0140-6736(16)32537-5 [DOI] [PubMed] [Google Scholar]
- 109. Baker KF, Isaacs JD: Novel therapies for immune-mediated inflammatory diseases: What can we learn from their use in rheumatoid arthritis, spondyloarthritis, systemic lupus erythematosus, psoriasis, Crohn's disease and ulcerative colitis? Ann Rheum Dis. 2017; pii: annrheumdis-2017-211555. 10.1136/annrheumdis-2017-211555 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 110. Mascarenhas JO, Talpaz M, Gupta V, et al. : Primary analysis of a phase II open-label trial of INCB039110, a selective JAK1 inhibitor, in patients with myelofibrosis. Haematologica. 2017;102(2):327–35. 10.3324/haematol.2016.151126 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 111. Bissonnette R, Luchi M, Fidelus-Gort R, et al. : A randomized, double-blind, placebo-controlled, dose-escalation study of the safety and efficacy of INCB039110, an oral janus kinase 1 inhibitor, in patients with stable, chronic plaque psoriasis. J Dermatolog Treat. 2016;27(4):332–8. 10.3109/09546634.2015.1115819 [DOI] [PubMed] [Google Scholar]
- 112. Schmieder GJ, Draelos ZD, Pariser DM, et al. : Efficacy and safety of the Janus Kinase 1 inhibitor PF-04965842 in patients with moderate to severe psoriasis: phase 2, randomized, double-blind, placebo-controlled study. Br J Dermatol. 2017. 10.1111/bjd.16004 [DOI] [PubMed] [Google Scholar]
- 113. Klünder B, Mohamed MF, Othman AA: Population Pharmacokinetics of Upadacitinib in Healthy Subjects and Subjects with Rheumatoid Arthritis: Analyses of Phase I and II Clinical Trials. Clin Pharmacokinet. 2017;1–12. 10.1007/s40262-017-0605-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Fleischmann RM, Damjanov NS, Kivitz AJ, et al. : A randomized, double-blind, placebo-controlled, twelve-week, dose-ranging study of decernotinib, an oral selective JAK-3 inhibitor, as monotherapy in patients with active rheumatoid arthritis. Arthritis Rheumatol. 2015;67(2):334–43. 10.1002/art.38949 [DOI] [PubMed] [Google Scholar]
- 115. Uckun FM, Roers BA, Waurzyniak B, et al. : Janus kinase 3 inhibitor WHI-P131/JANEX-1 prevents graft-versus-host disease but spares the graft-versus-leukemia function of the bone marrow allografts in a murine bone marrow transplantation model. Blood. 2002;99(11):4192–9. 10.1182/blood.V99.11.4192 [DOI] [PubMed] [Google Scholar]
- 116. Papp K, Pariser D, Catlin M, et al. : A phase 2a randomized, double-blind, placebo-controlled, sequential dose-escalation study to evaluate the efficacy and safety of ASP015K, a novel Janus kinase inhibitor, in patients with moderate-to-severe psoriasis. Br J Dermatol. 2015;173(3):767–76. 10.1111/bjd.13745 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 117. Takeuchi T, Tanaka Y, Iwasaki M, et al. : Efficacy and safety of the oral Janus kinase inhibitor peficitinib (ASP015K) monotherapy in patients with moderate to severe rheumatoid arthritis in Japan: a 12-week, randomised, double-blind, placebo-controlled phase IIb study. Ann Rheum Dis. 2016;75(6):1057–64. 10.1136/annrheumdis-2015-208279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Lipka DB, Hoffmann LS, Heidel F, et al. : LS104, a non-ATP-competitive small-molecule inhibitor of JAK2, is potently inducing apoptosis in JAK2V617F-positive cells. Mol Cancer Ther. 2008;7(5):1176–84. 10.1158/1535-7163.MCT-07-2215 [DOI] [PubMed] [Google Scholar]
- 119. Jatiani SS, Cosenza SC, Reddy MV, et al. : A Non-ATP-Competitive Dual Inhibitor of JAK2 and BCR-ABL Kinases: Elucidation of a Novel Therapeutic Spectrum Based on Substrate Competitive Inhibition. Genes Cancer. 2010;1(4):331–45. 10.1177/1947601910371337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Al-Ali HK, Griesshammer M, Le Coutre P, et al. : Safety and efficacy of ruxolitinib in an open-label, multicenter, single-arm phase 3b expanded-access study in patients with myelofibrosis: a snapshot of 1144 patients in the JUMP trial. Haematologica. 2016;101(9):1065–73. 10.3324/haematol.2016.143677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Passamonti F, Griesshammer M, Palandri F, et al. : Ruxolitinib for the treatment of inadequately controlled polycythaemia vera without splenomegaly (RESPONSE-2): a randomised, open-label, phase 3b study. Lancet Oncol. 2017;18(1):88–99. 10.1016/S1470-2045(16)30558-7 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 122. Harrison CN, Mead AJ, Panchal A, et al. : Ruxolitinib vs best available therapy for ET intolerant or resistant to hydroxycarbamide. Blood. 2017;130(17):1889–97. 10.1182/blood-2017-05-785790 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 123. Verstovsek S, Passamonti F, Rambaldi A, et al. : Ruxolitinib for essential thrombocythemia refractory to or intolerant of hydroxyurea: long-term phase 2 study results. Blood. 2017;130(15):1768–71. 10.1182/blood-2017-02-765032 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 124. Curto-Garcia N, Harrison CN: An updated review of the JAK1/2 inhibitor (ruxolitinib) in the Philadelphia-negative myeloproliferative neoplasms. Future Oncol. 2017;14(2):137–150. 10.2217/fon-2017-0298 [DOI] [PubMed] [Google Scholar]
- 125. Saeed I, McLornan D, Harrison CN: Managing side effects of JAK inhibitors for myelofibrosis in clinical practice. Expert Rev Hematol. 2017;10(7):617–25. 10.1080/17474086.2017.1337507 [DOI] [PubMed] [Google Scholar]
- 126. Schönberg K, Rudolph J, Vonnahme M, et al. : JAK Inhibition Impairs NK Cell Function in Myeloproliferative Neoplasms. Cancer Res. 2015;75(11):2187–99. 10.1158/0008-5472.CAN-14-3198 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 127. Curran SA, Shyer JA, St Angelo ET, et al. : Human Dendritic Cells Mitigate NK-Cell Dysfunction Mediated by Nonselective JAK1/2 Blockade. Cancer Immunol Res. 2017;5(1):52–60. 10.1158/2326-6066.CIR-16-0233 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 128. Verstovsek S, Gotlib J, Mesa RA, et al. : Long-term survival in patients treated with ruxolitinib for myelofibrosis: COMFORT-I and -II pooled analyses. J Hematol Oncol. 2017;10(1):156. 10.1186/s13045-017-0527-7 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 129. Pardanani A, Abdelrahman RA, Finke C, et al. : Genetic determinants of response and survival in momelotinib-treated patients with myelofibrosis. Leukemia. 2015;29(3):741–4. 10.1038/leu.2014.306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Gupta V, Mesa RA, Deininger MW, et al. : A phase 1/2, open-label study evaluating twice-daily administration of momelotinib in myelofibrosis. Haematologica. 2017;102(1):94–102. 10.3324/haematol.2016.148924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Pardanani A, Gotlib JR, Gupta V, et al. : Update On The Long-Term Efficacy and Safety Of Momelotinib, a JAK1 and JAK2 Inhibitor, For The Treatment Of Myelofibrosis. Blood. 2013;122(21):108 Reference Source [DOI] [PubMed] [Google Scholar]
- 132. Asshoff M, Petzer V, Warr MR, et al. : Momelotinib inhibits ACVR1/ALK2, decreases hepcidin production, and ameliorates anemia of chronic disease in rodents. Blood. 2017;129(13):1823–30. 10.1182/blood-2016-09-740092 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 133. Verstovsek S, Talpaz M, Ritchie E, et al. : A phase I, open-label, dose-escalation, multicenter study of the JAK2 inhibitor NS-018 in patients with myelofibrosis. Leukemia. 2017;31(2):393–402. 10.1038/leu.2016.215 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 134. Verstovsek S, Odenike O, Singer JW, et al. : Phase 1/2 study of pacritinib, a next generation JAK2/FLT3 inhibitor, in myelofibrosis or other myeloid malignancies. J Hematol Oncol. 2016;9(1):137. 10.1186/s13045-016-0367-x [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 135. BioPharma C: CTI BioPharma Provides Update On Clinical Hold Of Investigational Agent Pacritinib And New Drug Application In U.S.2016. Reference Source [Google Scholar]
- 136. PR Newswire CB: CTI BioPharma Announces Removal Of Full Clinical Hold On Pacritinib.2017. Reference Source [Google Scholar]
- 137. Harrison CN, Schaap N, Vannucchi AM, et al. : Janus kinase-2 inhibitor fedratinib in patients with myelofibrosis previously treated with ruxolitinib (JAKARTA-2): a single-arm, open-label, non-randomised, phase 2, multicentre study. Lancet Haematol. 2017;4(7):e317–e324. 10.1016/S2352-3026(17)30088-1 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 138. Jamieson C, Hasserjian R, Gotlib J, et al. : Effect of treatment with a JAK2-selective inhibitor, fedratinib, on bone marrow fibrosis in patients with myelofibrosis. J Transl Med. 2015;13:294. 10.1186/s12967-015-0644-4 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 139. Pardanani A, Harrison C, Cortes JE, et al. : Safety and Efficacy of Fedratinib in Patients With Primary or Secondary Myelofibrosis: A Randomized Clinical Trial. JAMA Oncol. 2015;1(5):643–51. 10.1001/jamaoncol.2015.1590 [DOI] [PubMed] [Google Scholar]
- 140. Hazell AS, Afadlal S, Cheresh DA, et al. : Treatment of rats with the JAK-2 inhibitor fedratinib does not lead to experimental Wernicke's encephalopathy. Neurosci Lett. 2017;642:163–7. 10.1016/j.neulet.2017.01.041 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 141. Buchert M, Burns CJ, Ernst M: Targeting JAK kinase in solid tumors: emerging opportunities and challenges. Oncogene. 2016;35(8):939–51. 10.1038/onc.2015.150 [DOI] [PubMed] [Google Scholar]
- 142. Yu HA, Perez L, Chang Q, et al. : A Phase 1/2 Trial of Ruxolitinib and Erlotinib in Patients with EGFR-Mutant Lung Adenocarcinomas with Acquired Resistance to Erlotinib. J Thorac Oncol. 2017;12(1):102–9. 10.1016/j.jtho.2016.08.140 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 143. Dao KT, Solti MB, Maxson JE, et al. : Significant clinical response to JAK1/2 inhibition in a patient with CSF3R-T618I-positive atypical chronic myeloid leukemia. Leuk Res Rep. 2014;3(2):67–9. 10.1016/j.lrr.2014.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Lierman E, Selleslag D, Smits S, et al. : Ruxolitinib inhibits transforming JAK2 fusion proteins in vitro and induces complete cytogenetic remission in t(8;9)(p22;p24)/ PCM1-JAK2-positive chronic eosinophilic leukemia. Blood. 2012;120(7):1529–31. 10.1182/blood-2012-06-433821 [DOI] [PubMed] [Google Scholar]
- 145. Rumi E, Milosevic JD, Selleslag D, et al. : Efficacy of ruxolitinib in myeloid neoplasms with PCM1-JAK2 fusion gene. Ann Hematol. 2015;94(11):1927–8. 10.1007/s00277-015-2451-7 [DOI] [PubMed] [Google Scholar]
- 146. Schwaab J, Knut M, Haferlach C, et al. : Limited duration of complete remission on ruxolitinib in myeloid neoplasms with PCM1-JAK2 and BCR-JAK2 fusion genes. Ann Hematol. 2015;94(2):233–8. 10.1007/s00277-014-2221-y [DOI] [PubMed] [Google Scholar]
- 147. Welsch K, Holstein J, Laurence A, et al. : Targeting JAK/STAT signalling in inflammatory skin diseases with small molecule inhibitors. Eur J Immunol. 2017;47(7):1096–107. 10.1002/eji.201646680 [DOI] [PubMed] [Google Scholar]
- 148. Winthrop KL: The emerging safety profile of JAK inhibitors in rheumatic disease. Nat Rev Rheumatol. 2017;13(4):234–43. 10.1038/nrrheum.2017.23 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 149. Archer TP, Moran GW, Ghosh S: Tofacitinib in ulcerative colitis. Immunotherapy. 2016;8(5):495–502. 10.2217/imt-2015-0031 [DOI] [PubMed] [Google Scholar]
- 150. Costa L, Del Puente A, Peluso R, et al. : Small molecule therapy for managing moderate to severe psoriatic arthritis. Expert Opin Pharmacother. 2017;18(15):1557–67. 10.1080/14656566.2017.1378343 [DOI] [PubMed] [Google Scholar]
- 151. Spoerl S, Mathew NR, Bscheider M, et al. : Activity of therapeutic JAK 1/2 blockade in graft-versus-host disease. Blood. 2014;123(24):3832–42. 10.1182/blood-2013-12-543736 [DOI] [PubMed] [Google Scholar]
- 152. Richez C, Truchetet M, Kostine M, et al. : Efficacy of baricitinib in the treatment of rheumatoid arthritis. Expert Opin Pharmacother. 2017;18(13):1399–407. 10.1080/14656566.2017.1359256 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 153. Genovese MC, Yang F, Østergaard M, et al. : Efficacy of VX-509 (decernotinib) in combination with a disease-modifying antirheumatic drug in patients with rheumatoid arthritis: clinical and MRI findings. Ann Rheum Dis. 2016;75(11):1979–83. 10.1136/annrheumdis-2015-208901 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 154. Haan C, Rolvering C, Raulf F, et al. : Jak1 has a dominant role over Jak3 in signal transduction through γc-containing cytokine receptors. Chem Biol. 2011;18(3):314–23. 10.1016/j.chembiol.2011.01.012 [DOI] [PubMed] [Google Scholar]
- 155. Deshpande A, Reddy MM, Schade GO, et al. : Kinase domain mutations confer resistance to novel inhibitors targeting JAK2V617F in myeloproliferative neoplasms. Leukemia. 2012;26(4):708–15. 10.1038/leu.2011.255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Hornakova T, Springuel L, Devreux J, et al. : Oncogenic JAK1 and JAK2-activating mutations resistant to ATP-competitive inhibitors. Haematologica. 2011;96(6):845–53. 10.3324/haematol.2010.036350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Zhang J, Adrián FJ, Jahnke W, et al. : Targeting Bcr-Abl by combining allosteric with ATP-binding-site inhibitors. Nature. 2010;463(7280):501–6. 10.1038/nature08675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Ohren JF, Chen H, Pavlovsky A, et al. : Structures of human MAP kinase kinase 1 (MEK1) and MEK2 describe novel noncompetitive kinase inhibition. Nat Struct Mol Biol. 2004;11(12):1192–7. 10.1038/nsmb859 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 159. Bandaranayake RM, Ungureanu D, Shan Y, et al. : Crystal structures of the JAK2 pseudokinase domain and the pathogenic mutant V617F. Nat Struct Mol Biol. 2012;19(8):754–9. 10.1038/nsmb.2348 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 160. Puleo DE, Kucera K, Hammarén HM, et al. : Identification and Characterization of JAK2 Pseudokinase Domain Small Molecule Binders. ACS Med Chem Lett. 2017;8(6):618–21. 10.1021/acsmedchemlett.7b00153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Dusa A, Staerk J, Elliott J, et al. : Substitution of pseudokinase domain residue Val-617 by large non-polar amino acids causes activation of JAK2. J Biol Chem. 2008;283(19):12941–8. 10.1074/jbc.M709302200 [DOI] [PubMed] [Google Scholar]
- 162. Thomas S, Fisher KH, Snowden JA, et al. : Methotrexate Is a JAK/STAT Pathway Inhibitor. PLoS One. 2015;10(7):e0130078. 10.1371/journal.pone.0130078 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 163. Dussiot M, Maciel TT, Fricot A, et al. : An activin receptor IIA ligand trap corrects ineffective erythropoiesis in β-thalassemia. Nat Med. 2014;20(4):398–407. 10.1038/nm.3468 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 164. McMullin MF, Harrison CN, Niederwieser D, et al. : The use of erythropoiesis-stimulating agents with ruxolitinib in patients with myelofibrosis in COMFORT-II: an open-label, phase 3 study assessing efficacy and safety of ruxolitinib versus best available therapy in the treatment of myelofibrosis. Exp Hematol Oncol. 2015;4:26. 10.1186/s40164-015-0021-2 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 165. Ihle JN, Witthuhn BA, Quelle FW, et al. : Signaling through the hematopoietic cytokine receptors. Annu Rev Immunol. 1995;13:369–98. 10.1146/annurev.iy.13.040195.002101 [DOI] [PubMed] [Google Scholar]
- 166. Lai P, Rosa DA, Magdy Ali A, et al. : A STAT inhibitor patent review: progress since 2011. Expert Opin Ther Pat. 2015;25(12):1397–421. 10.1517/13543776.2015.1086749 [DOI] [PubMed] [Google Scholar]
- 167. Bartalucci N, Tozzi L, Bogani C, et al. : Co-targeting the PI3K/mTOR and JAK2 signalling pathways produces synergistic activity against myeloproliferative neoplasms. J Cell Mol Med. 2013;17(11):1385–96. 10.1111/jcmm.12162 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 168. Choong ML, Pecquet C, Pendharkar V, et al. : Combination treatment for myeloproliferative neoplasms using JAK and pan-class I PI3K inhibitors. J Cell Mol Med. 2013;17(11):1397–409. 10.1111/jcmm.12156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Marubayashi S, Koppikar P, Taldone T, et al. : HSP90 is a therapeutic target in JAK2-dependent myeloproliferative neoplasms in mice and humans. J Clin Invest. 2010;120(10):3578–93. 10.1172/JCI42442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Mascarenhas J, Sandy L, Lu M, et al. : A phase II study of panobinostat in patients with primary myelofibrosis (PMF) and post-polycythemia vera/essential thrombocythemia myelofibrosis (post-PV/ET MF). Leuk Res. 2017;53:13–9. 10.1016/j.leukres.2016.11.015 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 171. Hobbs GS, Hanasoge Somasundara AV, Kleppe M, et al. : Hsp90 inhibition disrupts JAK-STAT signaling and leads to reductions in splenomegaly in patients with myeloproliferative neoplasms. Haematologica. 2018;103(1):e5–e9. 10.3324/haematol.2017.177600 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 172. Bjørn ME, Hasselbalch HC: Minimal residual disease or cure in MPNs? Rationales and perspectives on combination therapy with interferon-alpha2 and ruxolitinib. Expert Rev Hematol. 2017;10(5):393–404. 10.1080/17474086.2017.1284583 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 173. Duffield JS, Lupher ML, Jr: PRM-151 (recombinant human serum amyloid P/pentraxin 2) for the treatment of fibrosis. Drug News Perspect. 2010;23(5):305–15. 10.1358/dnp.2010.23.5.1444206 [DOI] [PubMed] [Google Scholar]
- 174. Verstovsek S, Manshouri T, Pilling D, et al. : Role of neoplastic monocyte-derived fibrocytes in primary myelofibrosis. J Exp Med. 2016;213(9):1723–40. 10.1084/jem.20160283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Stein BL, Swords R, Hochhaus A, et al. : Novel myelofibrosis treatment strategies: potential partners for combination therapies. Leukemia. 2014;28(11):2139–47. 10.1038/leu.2014.176 [DOI] [PubMed] [Google Scholar]
- 176. Sasaki K, Gotlib JR, Mesa RA, et al. : Phase II evaluation of IPI-926, an oral Hedgehog inhibitor, in patients with myelofibrosis. Leuk Lymphoma. 2015;56(7):2092–7. 10.3109/10428194.2014.984703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Schneider RK, Mullally A, Dugourd A, et al. : Gli1 + Mesenchymal Stromal Cells Are a Key Driver of Bone Marrow Fibrosis and an Important Cellular Therapeutic Target. Cell Stem Cell. 2017;20(6):785–800.e8. 10.1016/j.stem.2017.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 178. Liu F, Zhao X, Perna F, et al. : JAK2V617F-mediated phosphorylation of PRMT5 downregulates its methyltransferase activity and promotes myeloproliferation. Cancer Cell. 2011;19(2):283–94. 10.1016/j.ccr.2010.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Dawson MA, Bannister AJ, Göttgens B, et al. : JAK2 phosphorylates histone H3Y41 and excludes HP1alpha from chromatin. Nature. 2009;461(7265):819–22. 10.1038/nature08448 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 180. Badar T, Kantarjian HM, Ravandi F, et al. : Therapeutic benefit of decitabine, a hypomethylating agent, in patients with high-risk primary myelofibrosis and myeloproliferative neoplasm in accelerated or blastic/acute myeloid leukemia phase. Leuk Res. 2015;39(9):950–6. 10.1016/j.leukres.2015.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 181. Quintás-Cardama A, Tong W, Kantarjian H, et al. : A phase II study of 5-azacitidine for patients with primary and post-essential thrombocythemia/polycythemia vera myelofibrosis. Leukemia. 2008;22(5):965–70. 10.1038/leu.2008.91 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation