Abstract
Schwannoma is a benign tumor of the nerve sheath arising from the perineural schwann cells. The nerves most commonly involved in schwannomas of the head and neck are the vagus and the cervical sympathetic chain. Trigeminal schwannomas are rare tumours. A 17 year old male patient with a chief complaint of swelling on face was diagnosed as suffering from bening tumor extending from cranial base (from foramen ovale) to the parapharengeal space. Mandibular access osteotomy was done to expose the tumor. Surgical excision of the tumor was done along with the preservation of the nerve. Schwannomas can occur along the pathway of any somatic or sympathetic nerve. Superficial schwannomas require simple exposure and excision but the one which are deep and large, may require complex access osteotomies. Careful surgery is required to preserve the nerve function. Once completely excised, the prognosis is excellent.
Keywords: Access osteotomy, schwannoma, trigeminal nerve
INTRODUCTION
Schwannoma is a benign tumor of the nerve sheath arising from the perineural schwann cells. About 25%–45% of all schwannoma variants occur in the head and neck, generally presenting in the fourth decade of life.[1] Schwannomas can occur along the course of any somatic or sympathetic nerve. These lesions are freely mobile, except for a single attachment at the nerve of origin. The lesions are solitary, slow growing, and generally not associated with pain or neurologic symptoms, except in the setting of the third form of neurofibromatosis termed “schwannomatosis.”[2]
The nerves most commonly involved in schwannomas of the head and neck are the vagus and the cervical sympathetic chain.[3] Trigeminal schwannomas are rare tumors and extension into parapharyngeal space is exceptionally uncommon.
Hereby, we are presenting a case of giant trigeminal schwannoma which was present in the parapharyngeal space extending to the cranial base in a young patient.
CASE REPORT
A 17-year-old male patient reported in the department, with a chief complaint of swelling on left side of face [Figure 1] for the last 5 years. On examination, a large diffuse swelling was present on left side of face, causing facial asymmetry. Overlying skin was in normal color, it was smooth surfaced with free overlying skin, firm in consistency, nonfluctuant, and no thrill was present on palpation. Intraorally, the extension of swelling was present on the left side of soft palate and lateral pharyngeal wall. The overlying mucosa was normal in color and texture [Figure 2]. According to the patient, he was unable to chew properly from the left side.
Figure 1.
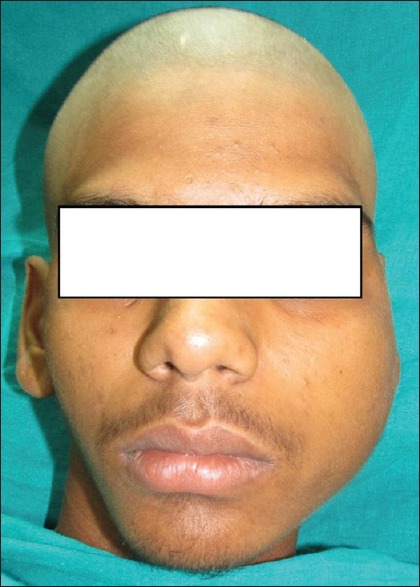
Preoperative photograph showing large swelling on left side of face causing facial asymmetry
Figure 2.

Intraoral photograph showing displaced soft palate
Magnetic resonance imaging (MRI) showed a well-defined hyperintense mass extending superiorly from the region below the left cavernous sinus passing through foramen ovale and extending below in left parapharyngeal space up to the level of hyoid [Figure 3]. The patient was scheduled for surgical excision and diagnosis was made after the histopathological examination.
Figure 3.
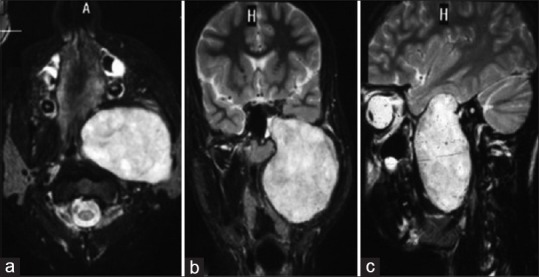
T2-weighted (a) axial, (b) coronal, and (c) sagittal images showing a large well-defined hyperintense oval mass extending from the region below left cavernous sinus, passing through foramen ovale (which is widened) and extending below in the left parapharyngeal space between medial and lateral pterygoid muscles
Extended submandibular with lip split incision was given. Paramedian mandibular split osteotomy was done to expose the tumor mass. The tumor was detached from the surrounding tissue with finger dissection. Intracranial access was taken through left temporal craniotomy and tumor was freed from the trigeminal nerve by the neurosurgeon. The tumor mass was retrieved [Figure 4] through oral cavity and was sent for histopathological examination. The mandible was repositioned and fixed with titanium plates and screws. Closure was done in layers. Postoperative healing was uneventful except mild weakness of mandibular nerve. On 1-year follow-up, his facial asymmetry was reduced [Figures 5 and 6] and his radiographs showed no signs of recurrence [Figure 7].
Figure 4.
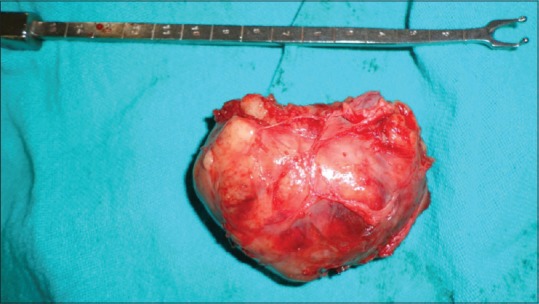
Excised tumor
Figure 5.

1-year follow-up photograph showing reduced facial asymmetry
Figure 6.

Intraoral photograph un-displaced soft palate
Figure 7.
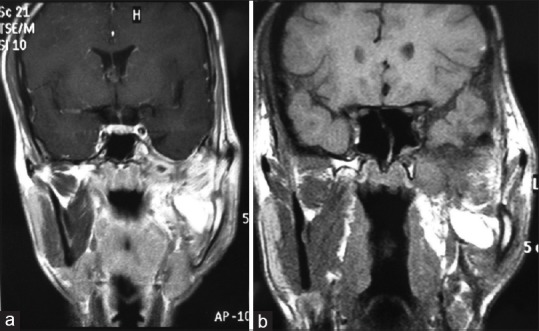
(a) Coronal T1-weighted image shows a mass to be hyperintense to muscle. (b) Coronal postcontrast T1-weighted image showing no enhancement, suggestive of fat
DISCUSSION
Schwannomas are sluggishly growing, benign neoplasms derived from the sheath cells that encompass myelinated nerve fibers. They may be encapsulated and are most often located in the head and neck.[4]
Schwannomas are more frequently seen in the second and third decades of life[5] and probably both sexes are affected equally. They are usually well defined and firm in consistency. They are typically asymptomatic and slowly increase in size until it causes functional or esthetic deformities. Similar findings were seen in our case.
The neural origin has been of particular curiosity to clinicians. Nerves which are most commonly involved in head and neck schwannomas are the vagus and the cervical sympathetic chain.[3] Trigeminal schwannomas are unusual tumors and extension into parapharyngeal space is exceptionally uncommon, reported only a few times in literature. These tumors usually present as large masses due to undisturbed growth of the tumor in the parapharyngeal space leading to the delay in the diagnosis and so in their surgical treatment[6] as was seen in our case. Facial dysesthesias and paresthesias are the most frequent clinical manifestations, together with facial pain, chewing disturbance, trismus, and facial swelling with changes in the temporofacial outline.[6] In the present case, no paresthesia or dysesthesia was present though chewing disturbance and facial swelling were present with displaced soft palate and lateral pharyngeal wall.
Neuroimaging plays a key role in the diagnosis and MRI is the gold standard for evaluating trigeminal schwannomas. Tumors show isointense or slightly hyperintense T1-weighted images and have high-signal intensity on T2-weighted images, with significant enhancement after contrast injection.[6] Asaumi et al.[7] reported the characteristics of advanced imaging findings associated with a common schwannoma of the upper lip. They indicated that computed tomography will illustrate a soft tissue mass, with clear margins and areas of cystic degeneration, depending on the variant. In our case, MRI showed mass which was slightly hyperintense on T1-weighted images and high-signal intensity on T2-weighted images, with significant enhancement after contrast injection.
The diagnosis of a schwannoma is established by histologic examination.[4] The rarity of these tumors and the paucity of symptoms make these tumors clinically impossible to differentiate from other encapsulated benign tumors. In the present case, confirmatory diagnosis was established only after histopathologic examination.
Simple excision or enucleation of the tumor is the indicated treatment. As a rule, schwannomas are well encapsulated and excision is performed without any difficulty. When the tumor involves a large nerve, separation, and preservation of the nerve throughout surgical removal deserves particular attention by the surgeon. Vigilant stripping of the nerve bundles from the surface of the growth will allow enucleation of the tumor in the majority of cases.
The literature suggests that the nerve should be separated from these tumors and preserved when the lesion is being removed.[8] However, a few reports state that the nerve of origin should be resected due to the possible risk of recurrence even if the tumor is benign.[9] In our case, careful dissection and stripping of the nerve bundles were done so as to preserve the nerve's function.
The involvement of nerve branch and location of these tumors govern the surgical approach. Various surgical approaches, such as transmaxillary and orbitozygomatic approaches,[6] have been proposed for the treatment of extracranial trigeminal schwannomas. Adequate treatment of tumors that occupy both extra- and intra-cranial part of the nerve is difficult. In these cases, a combination of craniotomy and transcervical/transmandibular approaches is proposed as one of the preeminent routes for tumor removal, which was done in our case.
A schwannoma does not recur if excised completely and the prognosis is usually outstanding. Malignant transformation is rare.[10] Radiotherapy has no place in the therapeutic management as these tumors are radioresistant.[8]
Schwannomas are benign tumors with outstanding prognosis after surgical resection. As the size and site of these tumors may vary in patients, treatment often requires multidisciplinary approach. We suggest that along with the riddance of the tumor, focus should also be on the safeguarding of the nerve.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Argenyi ZB, Cooper PH, Santa Cruz D. Plexiform and other unusual variants of palisaded encapsulated neuroma. J Cutan Pathol. 1993;20:34–9. doi: 10.1111/j.1600-0560.1993.tb01246.x. [DOI] [PubMed] [Google Scholar]
- 2.MacCollin M, Woodfin W, Kronn D, Short MP. Schwannomatosis: A clinical and pathologic study. Neurology. 1996;46:1072–9. doi: 10.1212/wnl.46.4.1072. [DOI] [PubMed] [Google Scholar]
- 3.Saydam L, Kizilay A, Kalcioglu T, Gurer I. Ancient cervical vagal neurilemmoma: A case report. Am J Otolaryngol. 2000;21:61–4. doi: 10.1016/s0196-0709(00)80127-1. [DOI] [PubMed] [Google Scholar]
- 4.Redman RS, Guccion JG, Spector CJ, Keegan BP. Cellular schwannoma of the mandible: A case report with ultrastructural and immunohistochemical observations. J Oral Maxillofac Surg. 1996;54:339–44. doi: 10.1016/s0278-2391(96)90756-9. [DOI] [PubMed] [Google Scholar]
- 5.Hatziotia JC, Asprides H. Neurilemoma (schwannoma) or the oral cavity. Oral Surg Oral Med Oral Pathol. 1967;24:510–26. doi: 10.1016/0030-4220(67)90431-8. [DOI] [PubMed] [Google Scholar]
- 6.Servadei F, Romano A, Ferri A, Magri AS, Sesenna E. Giant trigeminal schwannoma with parapharyngeal extension: Report of a case. J Craniomaxillofac Surg. 2012;40:15–8. doi: 10.1016/j.jcms.2010.11.012. [DOI] [PubMed] [Google Scholar]
- 7.Asaumi J, Konouchi H, Kishi K. Schwannoma of the upper lip: Ultrasound, CT, and MRI findings. J Oral Maxillofac Surg. 2000;58:1173–5. doi: 10.1053/joms.2000.9584. [DOI] [PubMed] [Google Scholar]
- 8.Artzi Z, Taicher S, Nass D. Neurilemmoma of the mental nerve. J Oral Maxillofac Surg. 1991;49:196–200. doi: 10.1016/0278-2391(91)90112-y. [DOI] [PubMed] [Google Scholar]
- 9.Thoma KH. Oral Surgery 4th ed St Louis, MO. The CV Mosby Company. 1963:848. [Google Scholar]
- 10.Rasbridge SA, Browse NL, Tighe JR, Fletcher CD. Malignant nerve sheath tumour arising in a benign ancient schwannoma. Histopathology. 1989;14:525–8. doi: 10.1111/j.1365-2559.1989.tb02189.x. [DOI] [PubMed] [Google Scholar]


