Abstract
Among people living with HIV/AIDS (PLHIV), health-related quality of life (HRQOL) is an important clinical metric of perceived well-being. Baseline data from the BEACON study (N=383) were used to examine relationships between HRQOL and negative social support, HIV-related stigma, viral suppression, and physical and mental health service use among a vulnerable population of low-income, urban PLHIV who currently or formerly used substances, and were primarily African American. Factor analyses and structural equation modeling indicated that increases in negative social support, stigma, mental health care visits and HIV physician visits were associated with lower HRQOL, while viral suppression was associated with greater HRQOL. The association between negative social support and HRQOL suggests the importance of intervening at the dyad or network levels to shape the type of social support being provided to PLHIV. HIV-related stigma is another negative social factor that is prevalent in this sample and could be addressed by intervention. Results indicate that greater mental and physical health service use can be used to identify individuals with lower HRQOL. Therefore, findings increase an understanding of HRQOL in this understudied population and have implications for designing interventions to improve HRQOL among PLHIV.
Keywords: health-related quality of life, HIV/AIDS, African American or Black, drug use disorder, HIV-related stigma, negative social support
INTRODUCTION
Among people living with HIV/AIDS (PLHIV), health-related quality of life (HRQOL) is an important metric of perceived well-being and merits research attention to its correlates among vulnerable populations. HRQOL has been conceptualized as a global assessment of the effects of health conditions on the whole person, and is especially important for understanding well-being among persons with multiple chronic conditions, such as older populations and PLHIV. HRQOL is the most widely used construct employed to assess subjective health among patients with chronic illness. (1,2) For patients with HIV, biological markers of immune status, namely serum viral load, are often the metrics of major focus in clinical care.
Most measures of HRQOL include mental and physical dimensions of an individual’s response to illness signs and symptoms and other aspects of the lived experience of the health condition, rather than focusing exclusively on the physical process of disease. (3) The most widely used HRQOL scales tend to include items regarding general health perceptions, physical functioning, bodily pain, mental health, and social role functioning. (4–6) HIV can have detrimental effects on psychological and physical domains of HRQOL due to direct illness signs and symptoms and potential toxicities of treatments, (7) and due to how people respond to someone living with the virus. Understanding HRQOL is particularly important among PLHIV who are often coping with co-morbid conditions that are highly stigmatized.
Correlates of health-related quality of life
While it is well established that HRQOL is associated with positive social support, (8) less is known about the relationship between negative social support and HRQOL among PLHIV. However, negative support has a greater impact than positive support on psychological and physical health in the general population and likely among PLHIV. (9–11) Negative support has been conceptualized as negatively interpreted or unsupportive behaviors (such as criticism, anger) from supportive others. (11,12) A study by Oetzel and colleagues (13) revealed significant positive associations between HRQOL and positive social support, and, importantly, significant negative associations between HRQOL and a measure of negative support, defined as social undermining, which is expressing disapproval or not valuing the person.
Stigma has also been associated with HRQOL and its dimensions of physical and mental health in PLHIV. Stigma often causes distress because others blame the PLHIV for becoming infected and disapprove of the behaviors that led to HIV infection. (14,15) Stigma among PLHIV has been associated with depressive symptoms (15) and overall quality of life. (16,17)
While depression and HIV/AIDS-related physical signs and symptoms are associated with HRQOL, it is not clear from the prior research the degree to which mental health care or HIV primary care clinic attendance are related to HRQOL. (18,19) Health services use may be proxy measures for mental and physical health status, which are among the primary dimensions in HRQOL.
Few studies have investigated HRQOL among disadvantaged, primarily African American PLHIV with current or former substance use. Furthermore, few studies have examined psychosocial factors as correlates of HRQOL, including HIV-related stigma, negative support provided by social network members, and mental and physical health service use.
The objective of the present study was to examine relationships between HRQOL and psychosocial variables, including social support and stigma; service use; and viral load among a highly vulnerable population of low-income urban PLHIV who currently or formerly use substances, and are primarily African American. Specifically, we hypothesized that having more negative social support, HIV-related stigma, and greater mental and physical health service use would have negative associations with HRQOL, while viral suppression would have a positive association. While previous studies have investigated relationships between social support and stigma with HRQOL(13,16,17), there is no research, to our knowledge, that examines relationships between physical and mental health care service use with HRQOL. Therefore, the analyses of relationships between service use and HRQOL were more exploratory in nature, rather than confirmatory, and likely were proxies for level of physical and mental wellness. It is important to not only increase our understanding of the correlates of HRQOL in this population, but also to understand the significance of both individual-level and network-level factors associated with HRQOL. Therefore, investigating HRQOL among PLHIV may increase the ability to design better interventions to increase HRQOL, regardless of HIV disease status.
METHOD
Procedure
Data were from the baseline survey of the BEACON (Being Active and Connected) study, which examined social environmental factors associated with health outcomes and well-being among disadvantaged PLHIVs and their informal caregivers. PLHIV were recruited from an academic hospital and community venues. Selection criteria included: HIV seropositive adult on antiretroviral treatment (ART); Baltimore City resident; having a history of injection drug use; and willingness to invite a main supportive person or caregiver to participate in the study. All PLHIV completed informed consent and were given $35 for survey participation. Survey items were administered both by Computer-Assisted Personal Interview (CAPI) and Audio Computer-Assisted Self-Interview (ACASI). The study on which this manuscript is based is fully approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board.
Measures
Outcome
The BEACON study assessed HRQOL by gathering data on general health perceptions, physical functioning limitations, social functioning, emotional health, and pain, which were 5 of the 8 domains that were measured by Hays and colleagues in the HIV Costs and Utilization Survey.(20) These domains included general health, physical functioning, social functioning, pain, emotional well-being, energy, and disability. The BEACON study contained three items that measured general health and social functioning; four items measuring physical functioning; an item measuring pain; and 20 items measuring emotional well-being. The general health and social functioning items in the BEACON study were taken from the SF-36, SF-12 and SF-8,(4,5,21) namely general health rating (from 1 = poor to 5 = excellent) and two items assessing the degree to which physical and mental health problems interfered with social functioning (0 = a lot to 2 = not at all). Physical functioning was included in the HRQOL latent factor and measured by four items such as, “How much does your health affect your ability to…bend, lift, or squat,” with response options from 0 = a lot to 2 = not at all. Chronic pain was measured based on a single item from the Memorial Symptom Assessment Scale- Short Form, “In the past 6 months, how often have you been bothered by pain” (0 = often/always versus 1 = sometimes/never). (22–24) Mental health status was assessed by the Center for Epidemiologic Studies - Depression (CES-D-20) scale. (25)
Although we did not use a standard quality of life measure, we have construct validity because the measures that we used were the same as measures used in previous HRQOL scales. For example, we used measures from the Medical Outcomes Study Short Form HRQOL survey, which is a widely used scale (SF-36) that has shown validity in the shorter versions (e.g., SF-12, SF-8). Our items also matched those used in the HIV Costs and Utilization survey. From the theoretical and conceptual literature on HRQOL, our items assess the primary domains of HRQOL, including general health and well-being; physical and mental health; pain; and social functioning.
Independent Measures
Negative support, which was defined as either too little support or conflictive support, was measured with ten items from the Social Exchange Scale (11) (e.g., “In the past 30 days, how often did someone you know let you down when you needed help?” with response options from 0 = most or all of the time to 2 = rarely or none of the time). HIV stigma was measured by six items (e.g., “Thinking about having HIV, how much do you fear you will lose your friends?”), with response options 0 = very much to 3 = not at all, which were measures developed for the SAIL study.(26) Recent mental health care or treatment was measured with the item, “In the past year, have you received any counseling, therapy, or medication for your nerves or any emotional problems, not including drug treatment?” Number of HIV medical visits was measured by, “In the past 6 months, how many primary healthcare visits for HIV or AIDS have you had?” HIV primary care was defined as “a visit to a doctor or nurse to have a checkup during which you may have discussed HIV medications, had your blood drawn, or talked about your blood test results.” (27) Viral load was measured by the Roche Cobas Amplicor and values were dichotomized with undetectable (<50 copies per mL) = 1 versus detectable (≥50 copies per mL) = 0. (28)
Data Analysis
Frequencies of demographic and independent variables were run in SPSS 22.0. (29) For constructs measured with multiple items, exploratory factor analysis with oblique rotation was conducted in Mplus(30) to determine the optimal number of factors for each construct. For the HRQOL factor, second-order confirmatory factor analyses were conducted, due to the second-order factor structure of the physical functioning factor being loaded on the overall HRQOL factor. A correlation matrix was constructed to present the bivariate associations among all of the manifest variables and latent factors. A structural model was fit in Mplus(30) and, in the case of lack of fit, modification indices were used to explore whether theoretically sound modifications would improve the fit of the model.
RESULTS
The majority of the PLHIV sample was male (61.4%), had a high school education or less (83.8%), and earned less than $1,000 per month (79.9%)(Table 1). Approximately two-thirds had used substances in the past 6 months (63.3%) and were virally suppressed (70.7%). Nearly all of the respondents (95.6%) reported at least some stigma on one or more of the HIV stigma items (Table 2).
Table 1.
Sample demographic characteristics for PLHIV (N = 383) in the BEACON study.
| Variable | N (%) or Mean (SDa) | Range |
|---|---|---|
| Sex (male) | 235 (61.4) | |
| Education (High School/GED or less) | 321 (83.8) | |
| Income (< 1,000 per month) | 306 (79.9) | |
| Race/ethnicity (African American/Black) | 329 (85.9) | |
| Current substance use | 243 (63.3) | |
| Age | 48 (6) | 28–63 |
SD = Standard Deviation
Table 2.
Frequencies and means of measured variables and latent factor loadings (BEACON study; N = 383).
| Latent Factors Health-Related Quality of Lifea |
||||||
|---|---|---|---|---|---|---|
| Excellent | Very good | Good | Fair | Poor | Factor Loadings | |
| General health | 70 (18.3) | 66 (17.2) | 137 (35.8) | 89 (23.2) | 21 (5.5) | .48 |
| Not at all | A bit | A lot | ||||
| Physical health Interference | 193 (50.4) | 149 (38.9) | 41 (10.7) | .88 | ||
| Mental health interference | 213 (55.6) | 123 (32.0) | 47 (12.3) | .72 | ||
| Not at all | A bit | A lot | ||||
| Physical Functioningb | .64 | |||||
| Bend, lift, squat | 147 (38.3) | 152 (39.6) | 84 (21.9) | .83 | ||
| Walk one block | 212 (55.2) | 126 (32.8) | 45 (11.7) | .90 | ||
| Walk uphill | 115 (29.9) | 154 (40.1) | 114 (29.7) | .94 | ||
| Moderate activities | 135 (35.2) | 169 (44.0) | 79 (20.6) | .83 | ||
| Always/Often | Some/Never | |||||
| Pain, bothersome€ | 122 (32.4) | 255 (67.6) | .62 | |||
| Mean (SD) | Range | |||||
| Depressive symptoms | 14.3 (10.09) | 0–51 | .50 | |||
| Negative Supportc | ||||||
| Rarely/none | Some/little | Most/all | ||||
| Let you down | 182 (47.4) | 148 (38.5) | 53 (13.8) | .61 | ||
| Insufficient time | 199 (51.8) | 138 (35.9) | 46 (12.0) | .65 | ||
| Asked for too much | 206 (53.6) | 117 (30.5) | 60 (15.6) | .50 | ||
| Meddle in your affairs | 191 (49.7) | 138 (35.9) | 54 (14.1) | .53 | ||
| Leave you out | 243 (63.3) | 115 (29.9) | 25 (6.5) | .68 | ||
| Unwanted advice | 162 (42.2) | 157 (40.9) | 64 (16.7) | .56 | ||
| Forget or ignore you | 221 (57.6) | 137 (35.7) | 25 (6.5) | .79 | ||
| Thoughtless | 205 (53.4) | 141 (36.7) | 37 (9.6) | .73 | ||
| Angry, upset | 189 (49.2) | 162 (42.2) | 32 (8.3) | .72 | ||
| Not enough attention | 204 (53.1) | 142 (37.0) | 37 (9.6) | .74 | ||
| Stigma, HIVd | ||||||
| Not at all | Just a little | Somewhat | Very much | |||
| Need to hide HIV | 186 (48.6) | 90 (23.5) | 69 (18.0) | 38 (9.9) | .56 | |
| Others blame you | 262 (68.4) | 55 (14.4) | 45 (11.7) | 21 (5.5) | .71 | |
| HIV is a punishment | 236 (61.6) | 44 (11.5) | 50 (13.1) | 53 (13.8) | .56 | |
| Others uncomfortable around you | 179 (46.9) | 91 (23.8) | 85 (22.1) | 27 (7.0) | .63 | |
| Fear will lose friends | 224 (58.5) | 70 (18.3) | 49 (12.8) | 40 (10.4) | .87 | |
| Fear family rejection | 317 (82.8) | 23 (6.0) | 27 (7.0) | 16 (4.2) | .79 | |
|
Measured Variables
| ||||||
| Yes | No | |||||
| Mental health care£ | 189 (49.3) | 194 (50.7) | ||||
| Viral load suppression | 251 (70.7) | 104 (29.3) | ||||
| Mean (SD) | Range | |||||
| HIV clinic visits, no.€ | 3.7 (2.9) | 1–23 | ||||
Comparative Fit Index (CFI) = .98, Tucker-Lewis Index (TLI) = .98, Root Mean Square Error of Approximation = .07 [.06, .09].
CFI = 1.00, TLI = 1.00, RMSEA = .06 [.00, .13].
CFI = .97, TLI = .96, RMSEA = .07 [.05, .09].
CFI = 1.00, TLI = 1.00, RMSEA = .09 [.06, .12].
Prior 6 months;
Prior year.
Exploratory factor analyses, used to fit the negative support, stigma, and physical functioning latent factors, achieved adequate factor loadings of the measured variables on each of their respective factors (Table 2). Loadings ranged from .50 to .79 for negative support, .56 to .87 for stigma, and .83 to .94 for physical functioning. Reliability for the factors is reflected in the factor loadings for the indicator variables. Each of the factors including negative social support (Confirmatory Fit Index [CFI] = .97, Tucker Lewis Index [TLI] = .96, Root Mean Square Error of Approximation [RMSEA] = .07 [.05, .09]), stigma (CFI = 1.00, TLI = 1.00, RMSEA = .09 [.06, .12], and physical functioning (CFI = 1.00, TLI = 1.00, RMSEA = .06 [.00, .13] achieved good model fit.(31) Bivariate correlations between latent factors and measured variables indicated significant correlations were between HRQOL and each of the predictors (all p’s < .001)(Table 3). In addition, a sizable correlation (r = .46, p < .001) existed between negative support and stigma.
Table 3.
Correlation matrix for all study latent factors and measured variables reported by persons living with HIV/AIDS who currently or formerly used drugs (BEACON study; N = 383).
| I | II | III | IV | V | VI | ||
|---|---|---|---|---|---|---|---|
| I | HRQOL | 1.00 | −.46*** | −.46*** | −.39*** | −.22*** | .05*** |
| II | Negative Support | 1.00 | .46*** | −.06 | −.03 | −.02 | |
| III | Stigma | 1.00 | .15* | .03 | .02 | ||
| IV | Mental health care | 1.00 | .14* | .02 | |||
| V | HIV visits, no. | 1.00 | −.02 | ||||
| VI | Viral Load | 1.00 |
Due to the second-order factor structure of the HRQOL factor, a confirmatory, rather than exploratory, factor analysis was run with five measured indicator variables and one latent factor for physical functioning limitations. Loadings ranged from .48 to .88 and the HRQOL factor achieved good fit (CFI = .98, TLI = .98, RMSEA = .07 [.06, .09]).(31) The loadings provide statistical support for the reliability of the HRQOL factor.
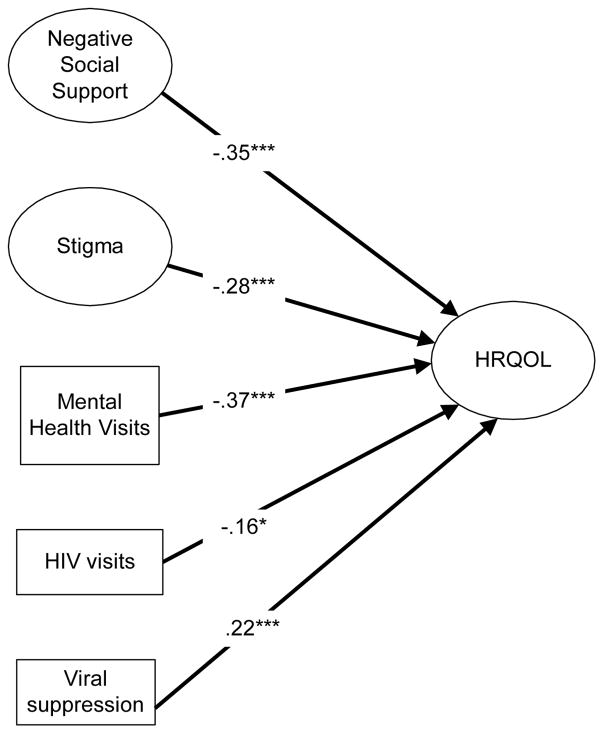
After fitting the measurement model, we ran a structural equation model regressing the HRQOL factor on factors for negative social support and stigma, and on measured variables for number of mental health visits, number of HIV visits, and viral suppression. Examination of modification indices led to adding residual correlations between four variable pairs (ie., reduced social functioning due to physical limitations with bending down, depressive symptoms, and reduced social functioning due to mental health; and between pain and moderate exercise) in order to improve the fit of the measurement model. The resulting model achieved good fit (CFI = .95, TLI = .94, RMSEA = .04 [.04, .05].(31) HRQOL was negatively associated with negative social support, stigma, mental health care usage, and HIV primary care visits. HRQOL was positively associated with viral suppression (Figure 1). The predictors explained 50% of the variance in the HRQOL factor.
Figure 1.
Negative social support, HIV-related stigma, health service use, and viral suppression associated with health-related quality of life among former or current drug using persons living with HIV/AIDS. (Beacon Study; N = 383).
R2 = .50.
Model fit: CFI = .95, TLI = .94, RMSEA = .04, 90% CI = .04, .05.
* p < .05,*** p ≤ .001.
DISCUSSION
Our findings revealed interpersonal- and network level factors that were associated with HRQOL among vulnerable PLHIV, above and beyond viral load, an individual factor emphasized in the literature. We identified two latent factors, namely, HIV-related stigma and negative social support, which were associated with reduced HRQOL. Our study results suggest the importance of intervention at the dyad and network levels that use psychosocial approaches to enhance mental and physical health outcomes among this vulnerable population.
Our findings contribute to the conceptual and methodological understandings of contextually specific aspects of the social environment that represent social risks to a vulnerable, chronically ill population’s HRQOL. Indeed, it goes beyond previous social support literature that tends to conceptualize social support as invariably positive and operationalizes it simplistically; most often as perceived availability of emotional support. (32,33)
Interestingly, we found that negative aspects of the social environment, namely negative social support and stigma, had some of the strongest associations with HRQOL, as did recent mental health care. These findings are consistent with prior literature indicating that negative as compared to positive experiences or events have greater associations with mental health, which is the negativity effect. (34) Indeed, stronger associations have been found between negative constructs and low HRQOL than between positive constructs and high HRQOL. (13)
Social support is an important factor in preventing morbidity and mortality and an be strengthened in this population of PLHIV, most of whom have informal caregivers. However, some of the relationships between PLHIV and their caregivers can be strained due to drug use and other stressors common in this marginalized population, such as stigma and low socioeconomic status. Therefore, it is important to examine the effects of negative social support as a focus of intervention to potentially improve HRQOL.
Considerable research attention has established adverse effects of perceived (internalized) HIV-related stigma on HIV health outcomes. Our results suggest that stigma was highly associated with but distinct from negative interactions with caregivers and ostensibly supportive others as well as mental illness, indicated by mental health service use. This is consistent with the literature on social pain, defined as the emotional response to the perception that one is being excluded, rejected or devalued by a significant individual or group.(35) For the study population, multiple stigmas from drug use, poverty, and disability, in addition to HIV, may covary with negative social interactions and perceptions of the social environment. Indeed, HIV-stigma is common in this population with nearly all of the respondents (95.6%) reporting at least some stigma on one or more of the stigma items in our study, which makes this construct particularly salient to our sample of PLHIV. Previous research has found that stigma is associated with poorer mental health(36), and depression in particular, which is one of the measures in our HRQOL factor. Therefore, it is reasonable that the stigma and HRQOL constructs would be associated in our study. However, further research is merited on support networks and caregiving relationship dynamics on HIV health outcomes in vulnerable populations and ways to promote effective caregiving and network functioning as a way to improve PLHIVs’ HRQOL.
Our study indicated that negative support was associated with lower HRQOL. For example, PLHIV reporting that supportive others’ “meddled” in their affairs, offered unwanted advice, or were critical or irritating, have been found to be associated with negative psychological outcomes. (37,38) Our study suggests that dyadic- or network-focused interventions to promote support exchange and the social skills required may help ensure network members’ provision of support matched to the type of support needed.
Results indicated that primary care visits were important to include in the model, as this variable was expected to covary with the HRQOL construct, which was comprised of both mental and physical health indicators. Primary care visits were relatively high in this sample, given that it is recommended that PLHIV have at least one HIV visit in the previous 6 months, while sample members had 3.7 visits on average in the past 6 months. This could be an indicator of good access to care, but it could also be an indicator of having more physical health problems, which would likely be associated with HRQOL.
Findings also indicated that mental health problems were prevalent in this disadvantaged population of PLHIV with a sizable proportion of the sample (49.3%) having sought mental health care services in the past year. Due to the number of sample members coping with mental health issues, this was a salient variable to include in the model that further describes the important correlates of HRQOL. Our substantial R-square value (.50) suggests that we were able to include important correlates of HRQOL that explained a great deal of variance in the outcome.
Limitations
We chose to use a universal measure of HRQOL rather than an HIV-specific measure that includes illness symptomology. While the Medical Outcomes Study measures are widely used, (39) they may not adequately assess the level of burden and hardship that impact physical and mental health as a result of HIV/AIDS. Our outcome variable did not include items on vitality or pain interference with regular or occupational activities as included in standard measures of HRQOL; (4,5,21,40) rather, our measure emphasized physical and emotional health interference with social activities (i.e., social functioning), and multiple components of psychological symptoms (CES-D), including social and somatic symptoms. However, the model fit and congruence of our findings with previous literature on HRQOL in PLHIV support the validity of our HRQOL measure for the study population and the factor loadings support the reliability of the indicator variables that loaded on the latent factors. In addition, the second order HRQOL factor has better psychometric properties than summed measured variables, which have measurement error that can attenuate associations with correlated variables. Another limitation is that our data are cross-sectional, which precludes conclusions regarding the causal direction of associations. Prospective studies are needed to identify additional antecedents and mediators of HRQOL. Furthermore, generalizability of the findings to other former or current drug using PLHIV may be limited as most of the sample was recruited from an academic clinic and the entire sample reported engagement in HIV care and treatment.
Conclusions
Our research adds to the scientific study of the HRQOL of a vulnerable PLHIV population. Our study advances the investigation of HRQOL by elucidating complexities of social environmental factors involved in HRQOL among vulnerable persons with serious chronic conditions. Our findings indicate that social and structural factors are associated with HRQOL above and beyond the effects of viral load emphasized in the HIV HRQOL literature.
HRQOL was correlated with negative aspects of the social environment. These results suggest the importance of interpersonal and network-oriented intervention approaches to promoting the study population’s HRQOL by improving their network support, and reducing HIV-related stigma and negative support perceptions. Such interventions are especially indicated for persons who often use physical and mental health services and those with a detectable viral load.
Acknowledgments
This study was supported by grants R01 DA019413 and R01 NR14050-01 from the National Institutes of Health. TQN’s time is partially supported by NIDA grant T-32DA007292 and Center For AIDS Research (CFAR) grant 1P30 AI094189.
Footnotes
Compliance with Ethical Standards:
All of the authors declare that they have no conflicts of interest.
Informed consent was obtained from all individual participants included in the study.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Perez IR, Bano JR, Ruz ML, et al. Health-related quality of life of patients with HIV: impact of sociodemographic, clinical and psychosocial factors. Quality of Life Research. 2005;14(5):1301–1310. doi: 10.1007/s11136-004-4715-x. [DOI] [PubMed] [Google Scholar]
- 2.Wu A, Lamping D. Assessment of quality of life in HIV disease. AIDS-LONDON-CURRENT SCIENCE THEN RAPID SCIENCE PUBLISHERS THEN LIPPINCOTT RAVEN- 1994;8:S349–S349. [Google Scholar]
- 3.Buseh AG, Kelber ST, Stevens PE, Park CG. Relationship of Symptoms, Perceived Health, and Stigma With Quality of Life Among Urban HIV-Infected African American Men. Public Health Nursing. 2008;25(5):409–419. doi: 10.1111/j.1525-1446.2008.00725.x. [DOI] [PubMed] [Google Scholar]
- 4.Ware JE, Jr, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care. 1995:AS264–AS279. [PubMed] [Google Scholar]
- 5.Ware JE, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Wu AW, Hays RD, Kelly S, Malitz F, Bozzette SA. Applications of the Medical Outcomes Study health-related quality of life measures in HIV/AIDS. Quality of Life Research. 1997;6(6):531–554. doi: 10.1023/a:1018460132567. [DOI] [PubMed] [Google Scholar]
- 7.Peter E, Kamath R, Andrews T, Hegde BM. Psychosocial Determinants of Health-Related Quality of Life of People Living with HIV/AIDS on Antiretroviral Therapy at Udupi District, Southern India. Int J Prev Med. 2014;5(2):203–209. [PMC free article] [PubMed] [Google Scholar]
- 8.Bekele T, Rourke SB, Tucker R, et al. Direct and indirect effects of perceived social support on health-related quality of life in persons living with HIV/AIDS. AIDS Care. 2013;25(3):337–346. doi: 10.1080/09540121.2012.701716. [DOI] [PubMed] [Google Scholar]
- 9.Lincoln KD. Social support, negative social interactions, and psychological well-being. Soc Serv Rev. 2000;74(2):231–252. doi: 10.1086/514478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kiecolt-Glaser JK, Glaser R, Cacioppo JT, Malarkey WB. Marital stress: Immunologic, neuroendocrine, and autonomic correlatesa. Ann N Y Acad Sci. 1998;840(1):656–663. doi: 10.1111/j.1749-6632.1998.tb09604.x. [DOI] [PubMed] [Google Scholar]
- 11.Newsom JT, Nishishiba M, Morgan DL, Rook KS. The relative importance of three domains of positive and negative social exchanges: a longitudinal model with comparable measures. Psychol Aging. 2003;18(4):746. doi: 10.1037/0882-7974.18.4.746. [DOI] [PubMed] [Google Scholar]
- 12.Rook KS, Pietromonaco P. Close relationships: Ties that heal or ties that bind. Advances in personal relationships. 1987;1:1–35. [Google Scholar]
- 13.Oetzel J, Wilcox B, Archiopoli A, et al. Social support and social undermining as explanatory factors for health-related quality of life in people living with HIV/AIDS. J Health Commun. 2014;19(6):660–675. doi: 10.1080/10810730.2013.837555. [DOI] [PubMed] [Google Scholar]
- 14.Herek GM. Thinking about AIDS and stigma: A psychologist’s perspective. JL Med & Ethics. 2002;30:594. doi: 10.1111/j.1748-720x.2002.tb00428.x. [DOI] [PubMed] [Google Scholar]
- 15.Herrmann S, McKinnon E, Hyland NB, et al. HIV-related stigma and physical symptoms have a persistent influence on health-related quality of life in Australians with HIV infection. Health and quality of life outcomes. 2013;11(1):1. doi: 10.1186/1477-7525-11-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Holzemer, William L, et al. Exploring HIV stigma and quality of life for persons living with HIV infection. Journal of the Association of Nurses in AIDS Care. 2009;20(3):161–168. doi: 10.1016/j.jana.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 17.Li X, Huang L, Wang H, Fennie KP, He G, Williams AB. Stigma mediates the relationship between self-efficacy, medication adherence, and quality of life among people living with HIV/AIDS in China. AIDS patient care and STDs. 2011;25(11):665–671. doi: 10.1089/apc.2011.0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bucciardini R, Pugliese K, Weimer L, et al. Relationship between health-related quality of life measures and high HIV viral load in HIV-infected triple-class-experienced patients. HIV clinical trials. 2014;15(4):176–183. doi: 10.1310/hct1504-176. [DOI] [PubMed] [Google Scholar]
- 19.Degroote Sophie, Vogelaers Dirk, Vandijck Dominique M. What determines health-related quality of life among people living with HIV: an updated review of the literature. Archives of Public Health. 2014;72(1):1–10. doi: 10.1186/2049-3258-72-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hays, Ron D, et al. Health-related quality of life in patients with human immunodeficiency virus infection in the United States: results from the HIV Cost and Services Utilization Study. The American journal of medicine. 2000;108(9):714–722. doi: 10.1016/s0002-9343(00)00387-9. [DOI] [PubMed] [Google Scholar]
- 21.Ware JE. How to score and interpret single-item health status measures: a manual for users of the of the SF-8 health survey:(with a supplement on the SF-6 health survey) QualityMetric, Incorporated; 2001. [Google Scholar]
- 22.Portenoy RK, Thaler HT, Kornblith AB, et al. The Memorial Symptom Assessment Scale: an instrument for the evaluation of symptom prevalence, characteristics and distress. Eur J Cancer. 1994;30(9):1326–1336. doi: 10.1016/0959-8049(94)90182-1. [DOI] [PubMed] [Google Scholar]
- 23.Mitchell MM, Maragh-Bass AC, Nguyen TQ, Isenberg S, Knowlton AR. The Role of Chronic Pain and Current Substance Use In Predicting Negative Social Support Among Disadvantaged Persons Living with HIV/AIDS. AIDS Care. 2016:1–7. doi: 10.1080/09540121.2016.1168916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Knowlton AR, Nguyen TQ, Robinson AC, Harrell PT, Mitchell MM. Pain symptoms associated with opioid use among vulnerable persons with HIV: An exploratory study with implications for palliative care and opioid abuse prevention. Journal of Palliative Care. 2015a;31(4):328–335. doi: 10.1177/082585971503100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied psychological measurement. 1977;1(3):385–401. [Google Scholar]
- 26.Knowlton AR, Latkin CA, Chung SE, Hoover DR, Ensminger M, Celentano DD. HIV and depressive symptoms among low-income illicit drug users. AIDS and Behavior. 2000 Dec 1;4(4):353–60. [Google Scholar]
- 27.Purcell DW, Metsch LR, Latka M, et al. Interventions for seropositive injectors—research and evaluation: an integrated behavioral intervention with HIV-positive injection drug users to address medical care, adherence, and risk reduction. JAIDS J Acquired Immune Defic Syndromes. 2004;37:S110–S118. doi: 10.1097/01.qai.0000140609.44016.c4. [DOI] [PubMed] [Google Scholar]
- 28.Arribas JR, Pulido F, Delgado R, et al. Lopinavir/ritonavir as single-drug therapy for maintenance of HIV-1 viral suppression: 48-week results of a randomized, controlled, open-label, proof-of-concept pilot clinical trial (OK Study) JAIDS J Acquired Immune Defic Syndromes. 2005;40(3):280–287. doi: 10.1097/01.qai.0000180077.59159.f4. [DOI] [PubMed] [Google Scholar]
- 29.IBM Corp. SPSS Statistics 22.0 Command Syntax Reference. SPSS Inc; 2013. 20.0. [Google Scholar]
- 30.Muthén L, Muthén B. Mplus user. 1998. [Google Scholar]
- 31.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal. 1999;6(1):1–55. [Google Scholar]
- 32.Blaney NT, Goodkin K, Morgan RO, et al. A stress-moderator model of distress in early HIV-1 infection: Concurrent analysis of life events, hardiness and social support. J Psychosom Res. 1991;35(2):297–305. doi: 10.1016/0022-3999(91)90084-2. [DOI] [PubMed] [Google Scholar]
- 33.Galvan FH, Davis EM, Banks D, Bing EG. HIV stigma and social support among African Americans. AIDS Patient Care STDS. 2008;22(5):423–436. doi: 10.1089/apc.2007.0169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rook KS. Stressful aspects of older adults’ social relationships: Current theory and research. Stress and coping in later-life families. 1990:173–192. [Google Scholar]
- 35.MacDonald Geoff, Leary Mark R. Why does social exclusion hurt? The relationship between social and physical pain. Psychological bulletin. 2005;131(2):202. doi: 10.1037/0033-2909.131.2.202. [DOI] [PubMed] [Google Scholar]
- 36.Mitchell MM, Knowlton AR. Stigma, disclosure, and depression among caregivers of HIV positive individuals. AIDS Patient Care & STDs. 23(8):611–617. doi: 10.1089/apc.2008.0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rook KS. Parallels in the study of social support and social strain. Journal of Social and Clinical Psychology. 1990;9(1):118–132. [Google Scholar]
- 38.Walen HR, Lachman ME. Social support and strain from partner, family, and friends: Costs and benefits for men and women in adulthood. Journal of Social and Personal Relationships. 2000;17(1):5–30. [Google Scholar]
- 39.Clayson DJ, Wild DJ, Quarterman P, Duprat-Lomon I, Kubin M, Coons SJ. A comparative review of health-related quality-of-life measures for use in HIV/AIDS clinical trials. Pharmacoeconomics. 2006;24(8):751–765. doi: 10.2165/00019053-200624080-00003. [DOI] [PubMed] [Google Scholar]
- 40.Wu AW, Huang I, Gifford AL, Spritzer KL, Bozzette SA, Hays RD. Creating a crosswalk to estimate AIDS Clinical Trials Group quality of life scores in a nationally representative sample of persons in care for HIV in the United States. HIV clinical trials. 2005;6(3):147–157. doi: 10.1310/BPNB-XELF-AXFQ-QQTL. [DOI] [PubMed] [Google Scholar]