Abstract
Aims and Objectives:
Pregnant women are at risk of dental caries and periodontal disease. The purpose of this study was to assess the effectiveness of health education program based on health belief model (HBM) on oral and dental hygiene behaviors in pregnant women in Fasa city.
Materials and Methods:
This is a clinical trial study carried out on 110 pregnant women selected using random sampling method from health centers in Fasa city in 2016 (55 patients in the experimental group and 55 individuals in control group). Data collection with questionnaire was based on construct HBM, as well as their performance about oral health. At first, two groups completed the questionnaires. And then, the intervention was conducted for the experimental group based on HBM. Four months after intervention, two groups completed the questionnaires twice. To analyze the collected data, the researchers used SPSS version 22 and descriptive and analytical statistics tests such as independent t-test and Chi-square and Mann–Whitney test.
Results:
The age of the pregnant mothers was 28.25 ± 3.02 years in the experimental group and 27.8 ± 4.20 years in the control group. Compared to the control group, the experimental group showed a significant increase in their knowledge, perceived susceptibility, perceived severity, perceived benefits, self-efficacy, cues to action, and performance and decrease in perceived barriers 4 months after the intervention.
Conclusion:
Applying the HBM is very effective for developing an educational program for oral health in pregnant women. Moreover, in the implementation of these programs, control, monitoring, and follow-up educational are recommended.
KEYWORDS: Fasa city, health belief model, oral health, performance, pregnancy
INTRODUCTION
Oral and dental diseases, especially dental caries and periodontal diseases, are the most common diseases. The disease can affect economy and the quality of life of people.[1] More than 33% of the world's populations suffer from dental caries.[2] According to the World Health Organization (WHO), observing oral hygiene is a must and considered to be a part of public health in all human life. The WHO suggests that poor oral hygiene and dental and oral diseases, if left untreated, can have a profound effect on the quality of life.[3] In comparison to other members of the society, pregnant women are at a greater risk of caries and periodontal diseases. Due to special circumstances, such as pregnancy cravings and impatience and specific mental conditions, this group of people is not particularly concerned about personal hygiene. The problem along with congestion and hormonal and dietary changes create favorable conditions for tooth decay and gingival diseases in pregnant women. Gingivitis and periodontal diseases are very common during pregnancy.[4,5] Taking dental treatment measures is considered to be harmful by many pregnant women. The results of a study show that 45% of women believe that pregnant women should not undergo any dental procedure during pregnancy.[6]
According to the results of previous studies, it is vital that measures be planned for the prevention of dental caries in all population groups, especially vulnerable group of pregnant women. In this regard, there are a number of theories and models in health education that can be used to design appropriate teaching interventions to change behavior and habits of self-care oral hygiene procedure and to establish healthy habits and to prevent the disease progression. One of these efficacious models in the education and promotion of health is health belief model (HBM).[7,8] In this model, perceived susceptibility serves to measure mothers’ perception about the rate they are prone to tooth decay. The perceived susceptibility also measures mothers’ perception severity and the complications of dental decay brought about to themselves and their fetus. The perceived threat together with the benefits and the barriers is actually the analysis of the advantages of adopting dental hygiene and that of potential barriers to take appropriate preventive measures to avoid the risk of dental caries. Moreover, mothers’ perceived capabilities to watch out as well as cues for action or influential internal and external incentives including friends and relatives, dentist, and midwife and fear for developing complications from dental caries and feeling at peace of mind following dental hygiene motivate them to comply with oral health care.[9]
Despite the importance of dental and oral hygiene during pregnancy, the results of the studies showed that pregnant women do not pay due attention to oral and dental care during pregnancy. For instance, in a group of Asian women residing in England, the researchers observed that 63% of pregnant women increased their intake of sugary stuff, and 65% brushed their teeth only once a day, and about 59% of the women experienced bleeding from gums while brushing their teeth.[10] Such a problem occurs in Iran. A study carried out in Ahwaz (the center of Khuzestan Province) reported that decayed, missed, and filled teeth (DMFT) score for pregnant women was 6.23 ± 3.01.[11] The researchers even observed that many pregnant women considered dental services as detrimental to themselves and their fetus. In another study, the findings showed that 45% of women believed that they must not undergo dental services during pregnancy.[6]
The present study was carried out to design and educate based on HBM so that it could pave the way toward improving maternal and neonatal health conditions.
MATERIALS AND METHODS
This is a clinical trial study whose subjects were 110 pregnant women referring to Fasa Health Centers for a period of 5 months. With regard to the study by Shamsi et al.,[5] the standard deviation obtained was 9.5, and considering the reliability level as 0.95, standard error as 0.80, and accuracy as 5, the number of samples in each group was decided to be 55. In sampling, two health centers were randomly selected out of six existing health centers located in Fasa, Fars, I.R. Iran. In one center, 25 individuals were randomly selected as experimental group and 30 as control group. However, in the other center, 30 individuals were randomly selected as experimental group and 25 as control group. In all, 55 individuals were allocated to each experimental and control group. To address the research purpose, the researchers designed and implemented a randomized one-blind study in a way that the participants did not know to which group they belonged.
The required criteria for subject's inclusion were being pregnant and resident at Fasa and knowingly willing to participate in the study. However, exclusion criteria included employment in a profession related to dentistry, suffering from progressive dental and oral diseases, and lack of consent to participate in the study.
Teaching intervention in this study consisted of six sessions held every other week during pregnancy through the HBM. Meanwhile, the two groups were given routine care in health centers by health-care personnel. Data collection was conducted in two stages. The data were collected in two phases, the first of which began at the start of the study. The second phase began 4 months after the completion of teaching intervention, during which the data were collected through interviews and filling out questionnaires. The data were collected through the same questionnaire used in Shamsi et al.'s study[5] and following Ajzen et al.'s[9] recommended procedure. The question items of HBM constructs included eight questions on perceived susceptibility (to what extent do mothers consider themselves to be at risk of dental caries); seven question items on perceived serverity (about complications for the mothers or fetus due to dental caries); 10 question items on perceived benefits (about the benefits of oral health care behaviors, benefits of the prevention of tooth decay, etc.); 12 question items on perceived barriers (about issues such as unfamiliarity with the proper techniques of brushing or flossing); eight question items on self-efficacy (the ability to brush and floss teeth properly, etc.); and two questions on cues for action (about internal and external incentives for pregnant women regarding oral hygiene practice including dentists, midwives, husbands, and wives and others which were assessed through questionnaires). It should be noted that all the question items on attitudinal parts were designed based on standard 5-point Likert scale and the question items on cues for action were calculated in terms of their cumulative frequency.
The checklist performance was assessed based on 12 question items of the questionnaire or a checklist of some behaviors expected regarding oral hygiene, brushing, and flossing. According to Ajzen et al., due to difficulties in obtaining data on time limits, measurement of immediate target behavior and using self-report and relying on individual reports rather than direct observation are acceptable procedures in the researches on HBM theory and other theories.[9,12] In scoring the items of the questionnaire for each construct of perceived susceptibility, perceived severity, perceived benefits, perceived barriers, and self-efficacy, the score ranged from 0 to 4 in a way that a zero score was assigned to “strongly disagree,” 1 to “disagree,” 2 to “neutral,” 3 to “agree,” and 4 to “strongly agree.” Overall, the total score for each construct (susceptibility, severity, benefits, barriers, and self-efficacy) were calculated based on 100 scores. Regarding the scoring of the checklist, point 1 was assigned to each correct behavior and a zero score to the wrong behavior. Like the constructs, the total score for the checklist was computed on 100 score basis.
The validity of data collection was measured through content validity and an extensive review of literature. The reliability of the research instrument to calculate was Cronbach's alpha formula which was confirmed to be a value equivalent to 0.84. In this section, the construct of perceived susceptibility had the reliability of 0.73, perceived severity 0.70, perceived benefits 0.75, perceived barriers 0.71, cues for action 0.73, and self-efficacy 0.76. The checklist's reliability was calculated to be 0.89 using Kappa coefficient correlation.
Before any intervention in both control and experimental groups, the data were collected through aforementioned questionnaire. After data collection, the type of teaching intervention was selected and implemented in six teaching sessions, each lasting for 60–55 min held every other week in forms of lecture, questions and answers, group discussions, and practical demonstrations using mouth and teeth replica, toothbrush, and dental floss and using the PowerPoint presentations. The material and the content for teaching intervention were based on educational goals and taken from reliable references approved by the Iranian Ministry of Health and Medical Education and what mothers ought to know about proper oral hygiene during pregnancy. The use of informative videos on oral health care increased capability of mothers in oral hygiene. In addition, the use of mouth and teeth replica and informative videos, pamphlets, and posters increased practical skills of the mothers on how to use toothbrush and dental floss properly. After the teaching intervention, two follow-up sessions were held for 1 and 2 months after the intervention to review the content, and then again, after 4 months, the data were recollected from both control and experimental groups. To comply with ethical considerations, the participants filled out the informed written consent forms. The research project was then ratified by the Research Council of Fasa University of Medical Sciences and the Ethics Committee (Ethical approval letter no: IR.FUMS.REC.1395.76). To analyze the collected data, the researchers used a Statistical Package for the Social Sciences (SPSS version 22, SPSS Inc., IBM, Chicago, IL, USA) and descriptive and analytical statistics tests such as independent t-test and Chi-square and Mann–Whitney test.
RESULTS
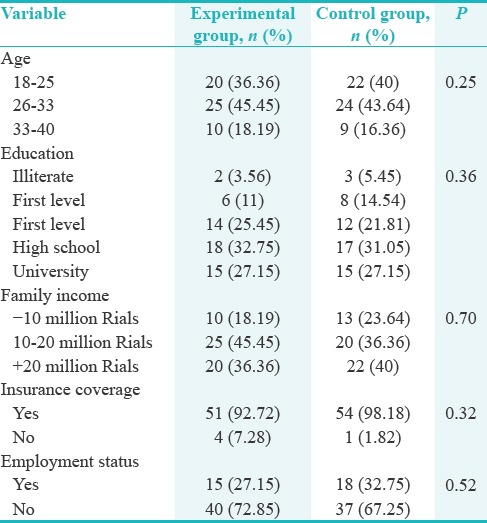
The age of the pregnant mothers was 28.25 ± 3.02 years in the experimental group and 27.8 ± 4.20 years in the control group. The period of gestation in the experimental and control groups was 19 ± 6 and 19 ± 8 weeks. 92.72% and 98.18% of the participants in the experimental group and control group had Health Insurance Services, respectively. In terms of formal education, most of them were in secondary and tertiary levels. Independent t-test showed no difference between the two groups regarding demographic variables [Table 1].
Table 1.
Demographics and some of the factors affecting oral health of pregnant women
The most significant perceived barriers reported by the mothers were not having enough time to visit the dentist, high dental costs, fear of injury to the fetus, fatigue, sluggish, and lack of sufficient skills to proper use of toothbrush and dental floss.
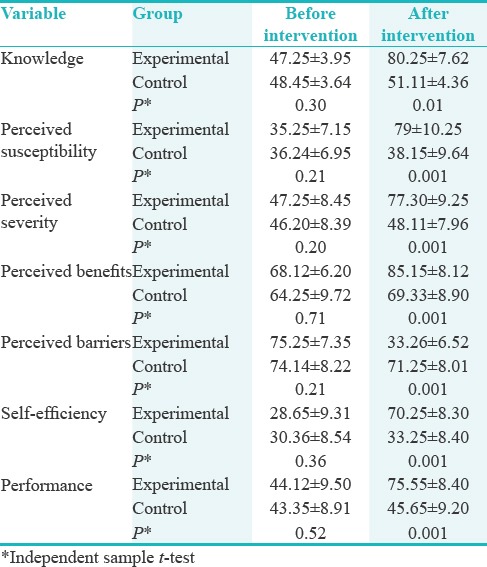
The findings showed that there was no significant difference between the experimental and control groups in terms of the constructs of HBM and the subjects’ performance. However, there was a significant difference between the experimental and control groups in all the variables after the teaching intervention [Table 2].
Table 2.
Comparison of scores on the health belief model in oral health care for pregnant women before and 4 months after intervention
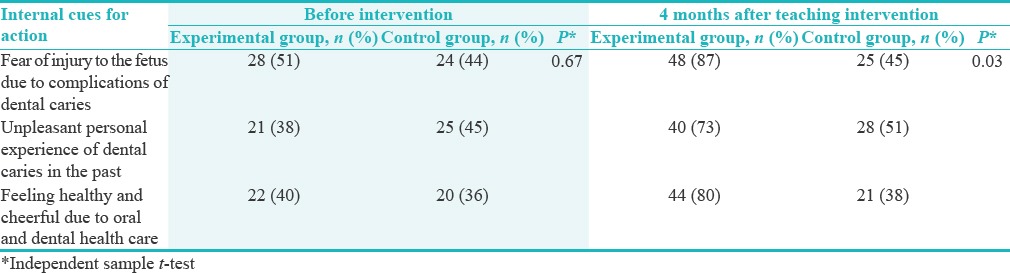
There was no statistically significant difference between the two groups in terms of internal and external cues for action before teaching intervention, while 4 months after the intervention, there was such a statistically significant difference between experimental and control groups regarding internal and external cues for action [Tables 3 and 4].
Table 3.
Distribution of external cues for action on oral health behaviors taken by pregnant women before and 4 months after intervention
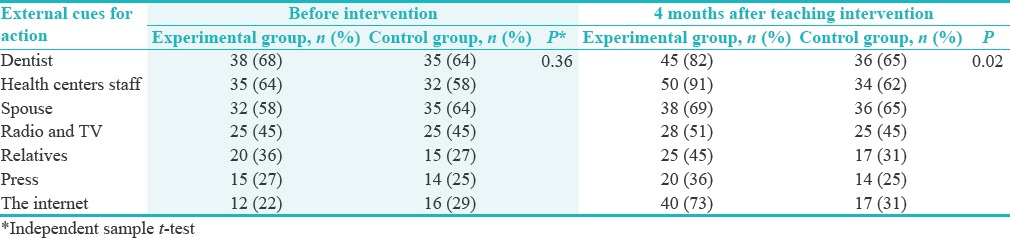
Table 4.
Distribution of internal cues for action on oral health behaviors taken by pregnant women before and 4 months after intervention
DISCUSSION
This study sought to provide further insight into the effect of teaching intervention on HBM in adopting oral health behaviors in pregnant women living in Fasa. The findings of the present study indicate that providing health education based on the HBM has positive effects on the oral health perceived threat, benefits, barriers, self-efficacy, knowledge, cues to action, and behaviors of the pregnant women in experimental group 4 months after the intervention.
The findings of this study showed that 4 months after the teaching intervention and following training sessions related to oral health promotion program based on HBM, there was rather a significant increase in the constructs of HBM and oral and dental hygiene practices in the experimental group than the control group. The findings of teaching interventions were indicative of their being successful to promote the knowledge of the subjects in experimental group compared to control one. In Mohebbi et al.'s study, teaching interventions led to promote the knowledge of midwifery students about oral health of pregnant women.[13] The findings of Shamsi et al.,[5] DiMarco et al.,[14] Bates and Riedy,[15] Bahri et al.,[16] Kullberg et al.,[17] Nogueira et al.,[18] and Shanthini et al.[19] are consistent with the present study.
Therefore, it is essential to promote pregnant women's knowledge about the oral health, especially those with low socioeconomic status.[20] The findings showed that the mean score for perceived susceptibility and perceived severity (perceived threat) of pregnant women before teaching intervention in both experimental and control groups was the same, but 4 months after the teaching intervention, the experimental group showed a more significant difference compared to the control group. As pregnant women are more prone to gum diseases and dental caries during pregnancy, it is vital that mothers are more sensitive to the consequences. In this study, the presence of such a significant difference between experimental group following the teaching intervention and control group can be a successful evidence of the impact of teaching intervention on promoting perceived susceptibility and seriousness in the control group so that after the teaching intervention, the majority of mothers in the experimental group believed that they would probably be exposed to the risk of tooth decay. An increase in their knowledge provided an opportunity to adopt oral health behaviors.
The findings of this study are consistent with that of Peyman and Pourhaji,[21] Kasmaei et al.,[22] Solhi et al.,[23] Shamsi et al.,[5] Shahnazi et al.,[24] and Hazavehei et al.[25] The present study shows that the mean score of perceived benefits in the experimental group obtained 4 months after the teaching intervention was significantly more than that of the control group. Shamsi et al. in their study stated that oral health behaviors in pregnant women were improved as their perception of benefits increased.[5] In Peyman and Pourhaji's study, too, the mean score of perceived benefits regarding oral health behaviors in the experimental group was significantly higher than that of control group after the teaching intervention completed.[21] The results of other studies are consistent with the present study.[23,26] The results of this study showed that the mean score of perceived barriers in the experimental group lowered after the teaching intervention; however, in the control group, it remained constant. The perception of mothers toward barriers was not having enough time to visit the dentist, high dental costs, fear of injury to the fetus, and lack of adequate skills to use a toothbrush and dental floss. In a study by Jessani et al.,[27] lack of insurance coverage for dentistry expenses and not affording time to visit the dentist were of the major barriers of the women under study. More than half of the women studied had not visited a dentist during pregnancy. In the study by Al Habashneh et al.,[28] while 60% of the subjects did not know that they should have visited a dentist during pregnancy, 68% of them preferred to postpone it until after pregnancy. The researchers found that is essential that oral health education be presented to the pregnant women by health professionals (doctors, dentists, and midwives before and during pregnancy).[21] In this regard, the results of this study are consistent with other studies.[5,29,30] The findings of this study showed that there was not a significant difference between the perceived self-efficacy of the subjects in the experimental and control groups before the teaching intervention, but 4 months after the teaching intervention, compared to the control group, the mean score of experimental group significantly increased. In Shahnazi et al.'s study, too, there was a significant increase in the mean score of self-efficacy of the subjects in the experimental group 4 months after the teaching intervention.[24]
The results of this study demonstrated that the mean scores of perceived susceptibility and self-efficacy had a significant relationship with DMFT so that the pregnant women whose mean scores of perceived susceptibility and self-efficacy were higher had a lower mean of DMFT.[31]
The findings of such studies by Shamsi et al.,[5] Bahmanpour et al.,[32] Buglar et al.,[33] and Zhianian et al.[34] are consistent with this research.
In this study, there was a significant increase in the mean score of the internal and external cues for action in the experimental group compared to the control group.
In Shamsi et al.'s study, too, there was no significant difference between the internal and external cues for action in the two groups before the teaching intervention, but the mean score of the experimental group significantly increased 3 months after teaching intervention.[5] Lopes Marinho's study has shown that the conditions of oral health and oral health care in pregnant women are worrisome. Educational interventions improved the perceptions of dental care, and they pointed out the need dentists have as effective members of the prenatal team.[35]
In Keirse and Plutzer's study, mothers were more concerned about the preservation of their fetus (babies) teeth than their own ones. Only 35% of them sought or received oral and dental care during pregnancy, 27% of them considered expenses as a barrier, and 41% reported they had experienced gum disease during pregnancy.[36]
In this regard, the results of other studies are consistent with those of this study.[37,38] In this study, the performance score of the mothers in the experimental group did significantly increase after the teaching intervention which can be attributed to the positive impact of education based on HBM. An increase in the perceived threat along with promotion of perceived benefits and perceived capabilities of the mothers to care and a decrease in the perceived barriers together with the effect of internal and external cues for action have driven mothers to the oral health care. In this regard, in a systematic review, it has been shown that oral health education is effective in improving oral health status; data show that oral hygiene is improved by decrease in plaque and gingival bleeding, and also, there was a significant decrease in dental caries.[39]
The findings of this study are consistent with those studies of Zarei,[40] Shamsi et al.,[5] Zhianian et al.,[34] Shahnazi et al.,[24] Noguchi et al.,[41] Khani Jeihooni et al.,[42] and Asgharnia et al.[43]
The strengths of our study are the randomized selection of the subjects and performing the study in two separate centers with acceptable distance from one anothe, so that there was no possibility of information exchange, which in turn increases the generalizability of the results. Among the limitations, this study faced was the use of self-report instrument for data collection. Still, the other limitation was that the study was bounded by the findings on those pregnant women referred to Fasa Health Centers. Therefore, it cannot be generalized to all pregnant women, especially mothers who referred to private doctors’ offices and clinics, to obtain dental care due to their severe dental problems. The subjects selected from this two health centers through convenience sampling. Thus, future studies are recommended to select health centers based on simple random sampling.
CONCLUSION
In this study, what remains important is the use of teaching intervention model which can lead to proper planning education and can have a significant role in adopting oral and dental health care practices. In fact, the use of this model in the present study combined with special teaching methods as well as the use of other important people in every phase of the study in motivating and changing mothers’ psychological-behavioral factors as background variables including perceived susceptibility, severity, and benefits (as independent variable) was effective in adoption of preventive behaviors such as toothbrushes and dental floss (as dependent variable). Regarding the sensitivity and vulnerability of pregnant mothers, the necessity for coming up with basic solution and proper planning to prevent oral and dental diseases seems sensible. It is also vital that mothers, midwives, doctors, and other health staff be provided with teaching programs.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- 1.Olabisi AA, Udo UA, Ehimen UG, Bashiru BO, Gbenga OO, Adeniyi AO, et al. Prevalence of dental caries and oral hygiene status of a screened population in Port Harcourt, Rivers state, Nigeria. J Int Soc Prev Community Dent. 2015;5:59–63. doi: 10.4103/2231-0762.151979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mehri A, Morowatisharifabad M. Utilizing the health promotion model to predict oral health behaviors in the students of Islamic Azad University of Sabzevar 2008. J Dent Med. 2009;22:81–7. [Google Scholar]
- 3.Torabi M, Karimi Afshar SA, Sheyghzadeh A, Karimi Afshar M. Appraisal of DMET in Kerman adults aged 35 to 44. J Dent Isfahan. 2009;2:93–8. [Google Scholar]
- 4.Kloetzel MK, Huebner CE, Milgrom P, Littell CT, Eggertsson H. Oral health in pregnancy: Educational needs of dental professionals and office staff. J Public Health Dent. 2012;72:279–86. doi: 10.1111/j.1752-7325.2012.00333.x. [DOI] [PubMed] [Google Scholar]
- 5.Shamsi M, Hidarnia A, Niknami SH, Rafiee M, Zareban I, Karimy M. The effect of educational program on increasing oral health behavior among pregnant women: Applying health belief model. Health Educ Health Promot. 2013;1:21–36. [Google Scholar]
- 6.Kandan PM, Menaga V, Kumar RR. Oral health in pregnancy (guidelines to gynaecologists, general physicians & oral health care providers) J Pak Med Assoc. 2011;61:1009–14. [PubMed] [Google Scholar]
- 7.Glanz K, Rimer B, Viswanath K. 2nd ed. New York: John Wily & Sons; 2008. Health Behavior and Health Education: Theory, Research, and Practice; pp. 65–94. [Google Scholar]
- 8.Naderifar M, Ghaljaei F, Akbarizadeh MR. Determination of the mothers’ practice about orodental health of their children up to six years old. Zahedan J Res Med Sci J Zahedan Univ Med Sci (Tabib-e-shargh) 2010;12:43–8. [Google Scholar]
- 9.Ajzen I, Czasch C, Flood MG. From intentions to behavior: Implementation intention, commitment and conscientiousness. J Appl Soc Psychol. 2009;39:1356–72. [Google Scholar]
- 10.Ahmadian Y, Sanathhani M. A descriptive survey of the oral health on a group of the Asian pregnant women resident in the UK. J Mashad Dent Sch. 2004;27:93–9. [Google Scholar]
- 11.Gharizadeh N, Haghiighizadeh MH, Sabarhaji W, Karimi A. A study of DMFT and oral hygiene and gingival status among pregnant women attending Ahwaz Health Centres. Sci Med J Ahwaz Jundishapur Univ Med Sci. 2005;43:40–7. [Google Scholar]
- 12.Astrøm AN. Applicability of action planning and coping planning to dental flossing among Norwegian adults: A confirmatory factor analysis approach. Eur J Oral Sci. 2008;116:250–9. doi: 10.1111/j.1600-0722.2008.00538.x. [DOI] [PubMed] [Google Scholar]
- 13.Mohebbi SZ, Yazdani R, Mirmolaei ST, Tartar Z, Janeshin A. Effect of an educational intervention on midwifery students’ knowledge and preparedness about oral health care in pregnant mothers. J Dent Med Tehran Univ Med Sci. 2014;26:306–13. [Google Scholar]
- 14.DiMarco MA, Huff M, Biordi D, Marino D, Taylor E, Stempfel S, et al. Oral health education for low- Income pregnant women; findings of a pilot study. J Dent Appl. 2015;2:190–5. [Google Scholar]
- 15.Bates SB, Riedy CA. Changing knowledge and beliefs through an oral health pregnancy message. J Public Health Dent. 2012;72:104–11. doi: 10.1111/j.1752-7325.2011.00289.x. [DOI] [PubMed] [Google Scholar]
- 16.Bahri N, Tohidinik HR, Bahri N, Iliati HR, Moshki M, Darabi F, et al. Educational intervention to improve oral health beliefs and behaviors during pregnancy: A randomized-controlled trial. J Egypt Public Health Assoc. 2015;90:41–5. doi: 10.1097/01.EPX.0000464139.06374.a4. [DOI] [PubMed] [Google Scholar]
- 17.Kullberg E, Sjögren P, Forsell M, Hoogstraate J, Herbst B, Johansson O, et al. Dental hygiene education for nursing staff in a nursing home for older people. J Adv Nurs. 2010;66:1273–9. doi: 10.1111/j.1365-2648.2010.05298.x. [DOI] [PubMed] [Google Scholar]
- 18.Nogueira BM, Nogueira BC, Fonseca RR, Brandao GA, Menezes TO, Tembra DP. Knowledge and attitudes of pregnant women about oral health. Int J Odontostomat. 2016;10:297–302. [Google Scholar]
- 19.Shanthini RP, Garla BK, Karuppaiah RM, Taranath M. Effectiveness of anticipatory guidance on the knowledge and attitude of pregnant women attending government hospital, Thirumangalam, Madurai. J Adv Oral Res. 2017;8:6. [Google Scholar]
- 20.Hashim R. Self-reported oral health, oral hygiene habits and dental service utilization among pregnant women in United Arab Emirates. Int J Dent Hyg. 2012;10:142–6. doi: 10.1111/j.1601-5037.2011.00531.x. [DOI] [PubMed] [Google Scholar]
- 21.Peyman N, Pourhaji F. The effects of educational program based on the health belief model on the oral health behaviors of elementary school students. Mod Care J. 2015;12:74–8. [Google Scholar]
- 22.Kasmaei P, Amin Shokravi F, Hidarnia A, Hajizadeh E, Atrkar-Roushan Z, Karimzadeh Shirazi K, et al. Brushing behavior among young adolescents: Does perceived severity matter. BMC Public Health. 2014;14:8. doi: 10.1186/1471-2458-14-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Solhi M, Zadeh DS, Seraj B, Zadeh SF. The application of the health belief model in oral health education. Iran J Public Health. 2010;39:114–9. [PMC free article] [PubMed] [Google Scholar]
- 24.Shahnazi H, Hosseintalaei M, Esteki Ghashghaei F, Charkazi A, Yahyavi Y, Sharifirad G, et al. Effect of educational intervention on perceived susceptibility self-efficacy and DMFT of pregnant women. Iran Red Crescent Med J. 2016;18:e24960. doi: 10.5812/ircmj.24960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hazavehei SM, Khani Jeihooni A, Hasanzadeh A, Amini S. The effect of educational program based on BASNEF model for eye care in non-insulin dependent diabetic patients. J Res Health Sci. 2010;10:81–90. [PubMed] [Google Scholar]
- 26.Hajimiri KH, Sharifirad GH, Hasanzade A. The effect of oral health education based on health belief model in mothers who had 3-6 year old children on decreasing dental plaque index in Zanjan. J Med Sci Zanjan Uni. 2010;18:77–86. [Google Scholar]
- 27.Jessani A, Laronde D, Mathu-Muju K, Brondani MA. Self-perceived oral health and use of dental services by pregnant women in surrey, British Columbia. J Can Dent Assoc. 2016;82:g28. [PubMed] [Google Scholar]
- 28.Al Habashneh R, Guthmiller JM, Levy S, Johnson GK, Squier C, Dawson DV, et al. Factors related to utilization of dental services during pregnancy. J Clin Periodontol. 2005;32:815–21. doi: 10.1111/j.1600-051X.2005.00739.x. [DOI] [PubMed] [Google Scholar]
- 29.Khani Jeihooni A, Hidarnia A, Kaveh MH, Hajizadeh E. The effect of a prevention program based on health belief model on osteoporosis. J Res Health Sci. 2015;15:47–53. [PubMed] [Google Scholar]
- 30.Karami K, Shakerinejad G, Kabiry B. Effect of education based on health belief model on students’ oral health behavior change. SJIMU. 2014;21:134–41. [Google Scholar]
- 31.Hosseintalaei M, Shahnazi H, Mohammadi M. The relationship of perceived susceptibility and self-efficacy with the decayed, missing, and filled teeth in pregnant women: A study based on the health belief model. Biomed Res. 2017;28:8142–8. [Google Scholar]
- 32.Bahmanpour K, Nouri R, Nadrian H, Salehi B. Determinants of oral health behavior among high school students in Marivan County, Iran based on the Pender's health promotion model. J Sch Public Health Inst Public Health Res. 2011;9:93–106. [Google Scholar]
- 33.Buglar ME, White KM, Robinson NG. The role of self-efficacy in dental patients’ brushing and flossing: Testing an extended health belief model. Patient Educ Couns. 2010;78:269–72. doi: 10.1016/j.pec.2009.06.014. [DOI] [PubMed] [Google Scholar]
- 34.Zhianian A, Zareban I, Ansari-Moghaddam A, Rahimi F. Improving self-care behaviors in pregnant women in Zahedan: Applying self-efficacy theory. Caspian J Health Res. 2015;1:18–26. [Google Scholar]
- 35.Lopes Marinho AM, Dutra FT, Lucas SD, Guimarães Abreu MH. Conditions and perceptions of oral health in Brazilian pregnant women. Braz Res Pediatr Dent Integr Clin. 2016;16:257–68. [Google Scholar]
- 36.Keirse MJ, Plutzer K. Women's attitudes to and perceptions of oral health and dental care during pregnancy. J Perinat Med. 2010;38:3–8. doi: 10.1515/jpm.2010.007. [DOI] [PubMed] [Google Scholar]
- 37.Jeihooni AK, Hidarnia A, Kaveh MH, Hajizadeh E, Askari A. Application of the health belief model and social cognitive theory for osteoporosis preventive nutritional behaviors in a sample of Iranian women. Iran J Nurs Midwifery Res. 2016;21:131–41. doi: 10.4103/1735-9066.178231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Walker KK, Steinfort EL, Keyler MJ. Cues to action as motivators for children's brushing. Health Commun. 2015;30:911–21. doi: 10.1080/10410236.2014.904030. [DOI] [PubMed] [Google Scholar]
- 39.Prabhu S, John J. Oral health education for improving oral health status of school children – A systematic review. IOSR J Dent Med Sci. 2015;14:101–6. [Google Scholar]
- 40.Zarei F. The effect of health education on oral health through role playing and painting on awareness and function of children. Qom Univ Med Sci J. 2010;14:92–4. [Google Scholar]
- 41.Noguchi M, Tagaya A, Sakoda A, Komatsuzawa H, Fujiwara N, Sugai M. Effectiveness of oral health education program on prevention of periodontal disease in Japanese pregnant women. Open J Nurs. 2016;6:282–93. [Google Scholar]
- 42.Khani Jeihooni A, Askari A, Kashfi SM, Khiyali Z, Kashfi SH, Safari O, et al. Application of health belief model in prevention of osteoporosis among primary school girl students. Int J Pediatr. 2017;5:6017–29. [Google Scholar]
- 43.Asgharnia M, Mirblouk F, Faraji R. Knowledge of post -partum women about oral health. J Med Fac Guilan Univ Med Sci. 2010;19:46–57. [Google Scholar]


