Abstract
Aims and Objective:
To assess the effect of root tilt on the fracture resistance and failure pattern of endodontically-treated premolars restored with different post-core systems.
Materials and Methods:
Ninety endodontically-treated premolars were mounted in acrylic blocks with 0°, 12°, and 24° axial root tilt. Teeth in each group were restored in three subgroups with cast post-core, readymade metal posts and composite cores, and fiber post and composite cores. Crowns of all teeth were prepared coinciding with the long axis of the acrylic blocks to receive all-ceramic crowns. All restored teeth were stressed to record the maximum load at failure and the associated failure pattern. The collected data were statistically analyzed using two-way ANOVA, Tukey's, and Kruskal–Wallis tests at α = 0.05 on past software to detect any differences between subgroups.
Results:
Analysis of the collected data indicated significant differences between the tested subgroups (ANOVA, P = 3.86). Further analysis showed significant difference between all test subgroups and the control (Tukey's, P < 0.05). In general, teeth with 0° tilt seemed more resistant to fracture than the tilted ones. For all groups, teeth restored with fiber post and composite cores (SG3) were more resistant to fracture compared to other post-core systems (SG1 and SG2) (Tukey's, P < 0.05). The root fracture was the most commonly seen mode of failure.
Conclusions:
Root tilting usually affects the fracture resistance of teeth restored with post-core systems. The fiber post and composite cores seemed to be the best choice to restore teeth with different root tilting possibilities.
KEYWORDS: Failure pattern, fiber post, fracture resistance, post-core, root tilt
INTRODUCTION
Restoring endodontically-treated teeth can be a challenge for most clinicians particularly, when a significant amount of tooth structure is lost.[1] These teeth, most of the time, require the use of different post-core system to support and retain extracoronal prostheses.[2] Although the teeth restored with post-core system are expected to be weaker than the intact teeth,[3,4] their clinical longevity could be affected by the selected post-core materials.[4,5,6,7] In spite of the fact that metal posts have been used commonly throughout the last decades, they do not fulfill the requirements of the ideal post characteristics.[8] Metal post-core systems are documented to be hazardous to the restored teeth increasing the potential risk of root fracture and limiting the possibility of retreatment if required.[6,9,10,11] Many researchers[12,13,14,15] referred the aforementioned drawbacks to the higher modulus of elasticity of metal posts compared to that of dentin, in addition to their low adhesion values. Fiber reinforced composite posts were recently introduced[16,17] with the advantage of bonding to and reinforcing both dentin and core buildup material.[9,18,19] Their comparable elasticity to that of dentin usually helps absorb stresses and minimize the chances of root fracture.[16,18,20] In addition, the lower fracture resistance of fiber posts, compared with metal ones, could also help in preserving tooth roots from fracture in cases of excessive loading.[13,21]
It is known that the appropriate degree of tilt of fixed partial denture (FPD) abutment teeth should not exceed 24°.[22] However, for the excessively tilted endodontically-treated teeth, it is usually difficult to decide whether to choose either orthodontic treatment to upright them or to use a post-core to adjust their axial inclination. Although orthodontic management is the treatment of choice for tilted teeth, using the same for the endodontically-treated teeth is considered a challenge to orthodontists. At the same time, post-core restorations are usually chosen to manage the tilted teeth because of their convenience, less time consumption, and lower cost.[23] However, few studies evaluated the ability of the restored teeth to resist fracture. Hou et al.[23] reported strong relationship between the fracture resistance of teeth restored with different post-core systems and their tilt angle. Other investigators showed contradicting results when comparing the fracture resistance of teeth restored with different post-core systems.[23,24,25,26]
Therefore, the current in vitro study aimed to evaluate the influence of root tilt on the fracture resistance and mode of failure of teeth restored with three different post-core systems and covered with all-ceramic crowns. The null hypothesis was that either root tilt or the type of post-core system will have no effect on the fracture resistance and the failure pattern of the restored teeth.
MATERIALS AND METHODS
Ninety single-rooted, caries-free human premolars of comparable size, extracted for orthodontic reasons, were collected at outpatient clinics following the registration with and the approval of the scientific and research committee, College of Dentistry, King Khalid University (#SRC/REG/2015-2016/17). The post hoc power test was used to assure the accuracy (OSP = 0.974) of the selected sample size. All teeth were meticulously cleaned using hand scaler (Hu Friedy, Chicago, IL, USA) to remove surface deposits and stored in water at 4°C (FLOCCHETTI, Frigoriferi Scientifici, Luzzara, Italy) for <1 month. In simulation to natural periodontal ligament, roots of all teeth were coated with a single layer of low viscosity rubber impression material (Imprint, 3M ESPE, St. Paul, MN, USA) and vertically embedded into acrylic blocks (Hygenic, Coltene/Whaledent AG. Alstatten, Switzerland) by the aid of custom-made metal guides with 0° axial inclination (GI, Control, n = 30), 12° distal inclination (GII, n = 30), and 24° distal inclination (GIII, n = 30) before cutting their crowns 2 mm above the CEJ by the use of high-speed rotary diamond points (#199/016, Mani, Tochigi-Ken, Japan) in the presence of water cooling.
The root canals of all teeth were endodontically prepared using ProTaper file system (Dentsply Maillefer Instruments, Switzerland) and obturated with ProTaper Universal Gutta-Percha points (Dentsply, York, PA, USA) and AH Plus endodontic sealer (Dentsply, DeTrey, Konstanz, Germany). Standardized post-spaces, 10-mm long, were then prepared 24 h after obturation using #2 drill (Fiber post, GC America Inc., IL, USA), irrigated with distilled water and dried with paper points. Roots in each group were then divided into 3 subgroups (SG 1–3, n = 10) according to the type of post to be luted into the prepared post-spaces. In SG1, cast post-cores were fabricated out of nickel-chromium alloy (Ruby Dental Products Inc., Osaka, Japan). A 1.5 mm-wide shoulder finish line and 1 mm of ferrule height were first prepared on the remaining coronal tooth structure. Standardized direct post-core acrylic patterns were then prepared with their core portion coinciding with the long axis of the acrylic blocks [Figure 1] with 6° axial taper and 6 mm overall occlusogingival height including the ferrule.
Figure 1.
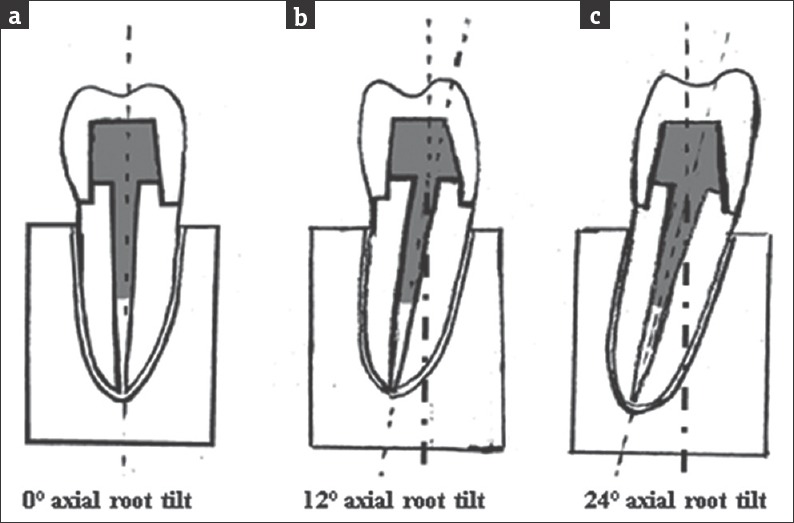
Schematic drawing of the performed post-core-crown restorations in teeth with (a) 0°, (b) 12°, and (c) 24° axial root tilt
The fabricated cast post-cores were cemented to their respective post-spaces using dual-cure resin cement (Variolink II, Ivoclar vivadnt, Schaan, Lechtenstien). The post-spaces were etched with 37% phosphoric acid solution for 15 s, washed, and dried with paper points. The cement base and catalyst were mixed in 1:1 ratio on a mixing pad for 10 s and applied into the post-space with a lentulo spiral instrument. Each post was gently seated to the full depth of its respective post-space, and the excess cement was removed with a microbrush before curing the exposed part using light curing device (Elipar FreeLight, 3M ESPE, Seefeld, Germany) for 40s.
In subgroups 2 and 3, ready-made passive metal posts (Dentatus Classic Surtex Titanium posts, Dentatus AB, Spånga, Sweden) and glass fiber posts (GC fiber postsize 2; Bisco Inc) were, respectively, selected to fit into the prepared post-spaces. The lengths of the selected posts were adjusted to be 4 mm above the cut teeth surfaces using doubled-faced diamond disc (#911H, Brasseler, Savannah, GA) under copious water cooling. All posts were then cemented into their respective spaces using the same dual-cured cement used in SG1. After light curing of the exposed cement surfaces, composite cores (Filtek Z250 Universal Restorative System, 3M ESPE, Seefeld, Germany) were incrementally built-up enveloping the exposed portion of the posts. All cores, together with 1 mm of the sound tooth structure were then prepared following standardized criteria; 1.5-mm shoulder finish line, 6° of axial taper, 6 mm axial height, and flat occlusal surfaces using flat end tapered diamond points (Coarse Modified Shoulder Flat-End Taper DuraBraze Diamond, Brasseler, USA) on a CNC lathe machine (BenchTurn 7000 CNC Turning Center, Derry, NH, USA).
All prepared teeth were restored with standardized machinable all-ceramic crowns. The preparation surfaces of the teeth were coated with contrast spray, and an optical impression was taken with the camera of Ceramill motion 2 “Amann Girrbach, Austria.” The shapes of the future crowns were adjusted on screen with the Ceramill match 2 computer-aided manufacturing software supplied with the milling machine. Standardized ceramic crowns were milled from Ceramill Zi, presintered y-TZP zirconium oxide blocks (Amann Girrbach, Kolbach, Austria) using Ceramill motion 2 milling machine. Finally, the ceramic crowns were luted using self-adhesive luting cement (RelyX Unicem Aplicap, 3M ESPE, St. Paul, MN, USA.) following the manufacturer's instructions. The materials used, composition, and manufacturers are reported in Table 1.
Table 1.
Chemical composition of the materials used in the study

Specimens in all test subgroups were subjected to thermocycling for 5000 cycles at 5°C–55°C with 1-min dwell time. Each specimen was then vertically stressed on compression to fracture using a steel rod with rounded end on the universal testing machine (Instron Model 5565; Instron Corporation, Canton, MA, USA) running at a crosshead speed of 1.0 mm/min. The maximum load at failure (N) were recorded and analyzed using two-way ANOVA and Tukey's pair-wise comparisons at α = 0.05 to test the significance of possible differences between test subgroups. The mode of failure was then assessed for each specimen, categorized and ranked as follows; dislodgement of post-core-crown system (Rank 1), fracture of the ceramic crown (Rank 2), crown and core fracture (Rank 3), and catastrophic root fracture (Rank 4). The calculated ranks of failures were then analyzed using the Kruskal–Wallis and Mann–Whitney tests to determine the significance of differences (if any) between the modes of failure in different test subgroups.
RESULTS
The mean fracture loads in different subgroups and standard deviations are listed in Table 2. Statistical analysis of the collected data using two-way ANOVA indicated the presence of differences between the tested groups (root tilt) and between the tested subgroups (type of post-core system), in addition to a significant interaction between the two test variables (P < 0.0001). Further analysis using Tukey's comparisons showed significant difference between most of the test subgroups and the control (P < 0.05). Exceptions were noticed with SG2 of G2 specimens (metal post and composite core in teeth with 12° root tilt) and SG3 of G3 specimens (Fiber post and composite core in teeth with 24° root tilt); those showed no difference from the control (P = 0.5485 and 1.000, respectively). At the same time, SG3 of G1 and G2 specimens (fiber post and composite core in teeth with 0° and 12° root tilt) showed higher fracture resistance than the control (P < 0.05). The type of post-core system (subgroups) in all groups showed significant effect on the fracture resistance, where teeth restored with fiber post and composite cores (SG3) revealed the highest resistance to fracture, and those restored with cast post and cores (SG1) provided the least resistance to fracture (Tukey's, P < 0.05). Within the same subgroup, the root tilt had also a significant effect on the fracture resistance, where teeth with no root tilt in G1 were more resistant to fracture than the tilted ones in G2 and G3 (Tukey's, P < 0.05).
Table 2.
Fracture load (Newton) in different test subgroups

The assessment of the mode of specimens’ failure indicated that root fracture [Figure 2] was the most seen mode of failure in all subgroups [30%–60%, Table 3]. The fracture of ceramic crowns either alone or together with the composite cores [Figure 2] was found to be of moderate incidence (20%–40%) regardless the test subgroup. The minimal incidence of failure (0%–30%) in all test subgroups was referred to the dislodgement of post-core-crown system [Figure 2]. However, the statistical analysis of the calculated ranks of failure modes [Table 3] using Kruskal–Wallis test indicated no difference (P = 0.9753) between all test subgroups in regard to the mean rank of failure modes.
Figure 2.
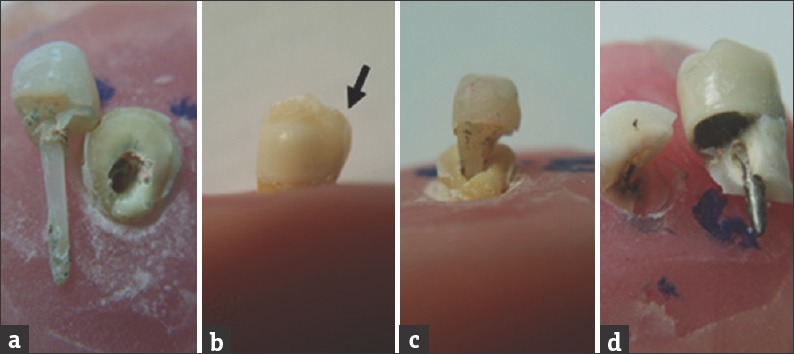
Different modes of failure; (a) dislodged post-core-crown system, (b) fractured ceramic crown, (c) fractured crown and core, and (d) catastrophic root fracture
Table 3.
Incidences (%) of different modes of failure

DISCUSSION
Utilizing the tilted endodontically-treated teeth as FPD abutments usually represents a challenging situation to dental practitioners. Orthodontic uprighting of these teeth is not too simple to be considered as the first line of management. Alternatively, the post-core restorations are preferably chosen to manage such cases because of their convenience, less time consumption, and lower cost.[23] However, the evaluation of the fracture resistance of those abutments and the pattern of their failure were the concern of few studies.[23,27,28] Therefore, the current in vitro study aimed to assess the effect of root tilt on the fracture resistance and failure pattern of endodontically-treated premolars intended to be FPD abutments. The selection of different post-core systems to restore teeth in this study was also considered as it could influence the restoration's success.[7] The null hypothesis, accordingly, assumed no effect of either root tilt or the type of post-core system on the fracture resistance and failure pattern of the restored teeth.
The results of the current in vitro study indicated inverse relation between the root tilt and the fracture resistance of the restored teeth in all test groups. This finding came in agreement with Kondoh et al.,[7] who stated that the endodontically-treated teeth with noticeable axial tilt are normally more susceptible to fracture on loading when restored with post-core-crown system and used as an abutment for a bridge. Hou et al.[23] also reported strong relationship between the fracture resistance of teeth restored with different post-core systems and their axial tilt angle. They also reported that the fiber post-core restorations had higher fracture resistance in different tilt angles compared with that of metal post-core restorations. These findings could be explained by the fact that the tooth structure can withstand more vertical forces compared to oblique ones.[23] In spite of the aforementioned explanation, Hayashi et al.[28] recorded a reduction of 31%–37% in the fracture resistance against oblique loads for teeth restored with cast and prefabricated metals posts, respectively, in comparison to 67% for teeth restored with fiber post. They referred the noticed higher reduction in the fracture resistance of teeth restored with fiber posts to the possible bending of the restored roots on oblique loading.
The statistical analysis of the results showed that teeth in all groups restored with fiber post and composite cores (SG3) revealed higher resistance to fracture in comparison to those restored with either prefabricated metal posts (SG2) or the cast post and cores (SG1) which provided the least resistance to fracture. These findings came in agreement with the results of some studies;[9,10] those showed higher fracture resistance of fiber post-core systems compared to metal post-core systems. These findings could be referred to the favorable biomechanical properties of fiber posts and composite cores.[29,30] Giovani et al.[31] utilized the same concept to explain his supporting results. They reported that glass fiber posts with modulus of elasticity similar to dentin can absorb the stresses better, reducing the probability of catastrophic root fracture accordingly. Schwartz and Robbins[30] also supported that explanation stating that posts that flex with the tooth on function should, theoretically, result in better stress distribution and less serious fracture. In addition, Al-Wahadni et al.[24] recommended resin composites for core building up; from the mechanical point of view, these materials showed adequate compressive strength and usually provide good bonding to both tooth and fiber posts. These features probably help in distribution of stresses and reducing the chance of the catastrophic root fracture, and this could also be applied to explain the recorded results for teeth restored with prefabricated metal posts in SG2.
At the same time, the results of this study disagreed with the findings of other studies[32,33] which indicated greater fracture resistance of teeth restored with metal posts than fiber posts, although that conflict could be a result of the different experimental protocols and the applied testing conditions. Darabi and Namazi[33] reported higher fracture resistance of teeth restored with cast post-cores and they explained their results depending on the higher modulus of elasticity of cast post-core material which provides less dentinal stress concentration. Other investigator[34] mentioned that the flexibility of fiber posts directed the stresses toward the core or post-tooth interface leading to an increased failure rate. The conflicting reports on the mechanical performance of different post-core systems directed some investigators[24] not to declare the superiority of any type to the others.
Failures in teeth with post-core-crown restorations are usually classified into restorable and non-restorable fractures. Fracture of crown superstructure alone or together with the supporting core buildups in addition to the dislodgement of the entire post-core-crown system can be restored with crown lengthening or core rebuilding up, while root fractures beyond the level of the alveolar bone crest are considered catastrophic leaving no chance of subsequent restoration of the affected tooth.[18] The results of the current study revealed both categories of failure, with more favorable findings for subgroups 2 and 3 (restored with either ready-made metal and fiber posts together with composite cores, respectively) than subgroup 1 (restored with cast post-core). In response, the stress distribution along roots of the restored teeth is much dependent on the mechanical characteristics of the restorative systems. Because of the reported similarities to tooth biomechanical characters, fiber post and composite core restorative system could facilitate normal on-loading flexure of roots resulting in minimal values of harmful stresses.[4,35] In agreement with the results of the current study, Gu et al.[36] reported higher incidence of restorable failures (crown or core fracture) in teeth restored by fiber post, in comparison to teeth restored by cast post and core those most of the time showed non-restorable root fractures. Freedman[37] indicated that vertical root fracture usually the result of accumulation of higher stresses at the apical area of roots having cast post-cores. Akkayan and Gülmez[38] also observed the dominance of catastrophic fractures in association with cast posts compared with fiber posts. They referred their findings to rigidity of the metal post that transferred the forces directly to the tooth causing this type of non-restorable failure. In addition, the presence of composite cores could contribute favorably in regard to the mode of specimens’ failure. Pilo et al.[39] reported no effect of core stiffness on the fracture resistance of the restored teeth; however, composite cores are most likely to show repairable failures when compared to metal cores. Another study by Torabi and Fattahi[8] also showed more serious fracture patterns in teeth restored with cast post-core system in comparison to teeth restored with fiber post and composite cores. These findings could be explained based on the lower rigidity of the core materials that tend to deform under occlusal loading and reduce the concentration of stresses at core-dentin interface. This feature can accordingly result in core failure in cases utilizing composite cores, while those utilizing cast post-core usually show root fracture.[26,29,40]
Depending on the results of the current in vitro study, utilizing fiber posts and composite cores to restore teeth with different tilting possibilities could be clinically advisable. However, long-term clinical assessment of their performance is recommended for further studies.
CONCLUSIONS
Root tilting usually affects the fracture resistance of teeth restored with post-core systems. The fiber post and composite cores seem to be the best choice to restore teeth with different root tilting possibilities.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- 1.Helal MA, Wang Z. Biomechanical assessment of restored mandibular molar by endocrown in comparison to a glass fiber post-retained conventional crown: 3D finite element analysis. J Prosthodont. 2017 doi: 10.1111/jopr.12690. doi: 10.1111/jopr.12690. [DOI] [PubMed] [Google Scholar]
- 2.Marchionatti AM, Valli V, Wandscher VF, Monaco C, Baldissara P. Influence of elastic modulus of intraradicular posts on the fracture load of roots restored with full crowns. Rev Odontol UNESP. 2017;46:232–7. [Google Scholar]
- 3.Gholami F, Kohani P, Aalaei S. Effect of nickel-chromium and non-precious gold color alloy cast posts on fracture resistance of endodontically treated teeth. Iran Endod J. 2017;12:303–6. doi: 10.22037/iej.v12i3.10586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uthappa R, Mod D, Kharod P, Pavitra S, Ganiger K, Kharod H. Comparative evaluation of the metal post and fiber post in the restoration of the endodontically treated teeth. J Dent Res Rev. 2015;2:73–7. [Google Scholar]
- 5.Al Subait A, Albawardi A, Alghomlas A, Daabash M, Alotaibi M, Alturki Y. Success and survival rates of teeth restored with cast post and core among National Guard health affairs patients, Riyadh, Saudi Arabia. Adv Dent Oral Health. 2016;2:555–83. [Google Scholar]
- 6.Lazari PC, de Carvalho MA, Del Bel Cury AA, Magne P. Survival of extensively damaged endodontically treated incisors restored with different types of posts-and-core foundation restoration material. J Prosthet Dent. 2017 doi: 10.1016/j.prosdent.2017.05.012. pii: S0022-3913(17)30368-2. [DOI] [PubMed] [Google Scholar]
- 7.Kondoh Y, Takeda T, Ozawa T, Narimatsu K, Konno M, Fujii T, et al. Influence of different post-core systems on impact stress: A pilot study. Open Dent J. 2013;7:162–8. doi: 10.2174/1874210601307010162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Torabi K, Fattahi F. Fracture resistance of endodontically treated teeth restored by different FRC posts: An in vitro study. Indian J Dent Res. 2009;20:282–7. doi: 10.4103/0970-9290.57359. [DOI] [PubMed] [Google Scholar]
- 9.Mitsui FH, Marchi GM, Pimenta LA, Ferraresi PM. In vitro study of fracture resistance of bovine roots using different intraradicular post systems. Quintessence Int. 2004;35:612–6. [PubMed] [Google Scholar]
- 10.Fernandes AS, Shetty S, Coutinho I. Factors determining post selection: A literature review. J Prosthet Dent. 2003;90:556–62. doi: 10.1016/j.prosdent.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Kimmel SS. Restoration and reinforcement of endodontically treated teeth with a polyethylene ribbon and prefabricated fiberglass post. Gen Dent. 2000;48:700–6. [PubMed] [Google Scholar]
- 12.Ichikawa Y, Akagawa Y, Nikai H, Tsuru H. Tissue compatibility and stability of a new zirconia ceramic in vivo . J Prosthet Dent. 1992;68:322–6. doi: 10.1016/0022-3913(92)90338-b. [DOI] [PubMed] [Google Scholar]
- 13.Kar S, Tripathi A, Trivedi C. Effect of different ferrule length on fracture resistance of endodontically treated teeth: An in vitro study. J Clin Diagn Res. 2017;11:49–52. doi: 10.7860/JCDR/2017/24669.9675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heydecke G, Butz F, Strub JR. Fracture strength and survival rate of endodontically treated maxillary incisors with approximal cavities after restoration with different post and core systems: An in-vitro study. J Dent. 2001;29:427–33. doi: 10.1016/s0300-5712(01)00038-0. [DOI] [PubMed] [Google Scholar]
- 15.Martínez-Insua A, da Silva L, Rilo B, Santana U. Comparison of the fracture resistances of pulpless teeth restored with a cast post and core or carbon-fiber post with a composite core. J Prosthet Dent. 1998;80:527–32. doi: 10.1016/s0022-3913(98)70027-7. [DOI] [PubMed] [Google Scholar]
- 16.Stricker EJ, Göhring TN. Influence of different posts and cores on marginal adaptation, fracture resistance, and fracture mode of composite resin crowns on human mandibular Premolars. An in vitro study. J Dent. 2006;34:326–35. doi: 10.1016/j.jdent.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 17.Bateman G, Ricketts DN, Saunders WP. Fibre-based post systems: A review. Br Dent J. 2003;195:43–8. doi: 10.1038/sj.bdj.4810278. [DOI] [PubMed] [Google Scholar]
- 18.Newman MP, Yaman P, Dennison J, Rafter M, Billy E. Fracture resistance of endodontically treated teeth restored with composite posts. J Prosthet Dent. 2003;89:360–7. doi: 10.1067/mpr.2003.75. [DOI] [PubMed] [Google Scholar]
- 19.Asmussen E, Peutzfeldt A, Heitmann T. Stiffness, elastic limit, and strength of newer types of endodontic posts. J Dent. 1999;27:275–8. doi: 10.1016/s0300-5712(98)00066-9. [DOI] [PubMed] [Google Scholar]
- 20.Moosavi H, Afshari S, Manari F. Fracture resistance of endodontically treated teeth with different direct corono-radicular restoration methods. J Clin Exp Dent. 2017;9:454–9. doi: 10.4317/jced.53160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cormier CJ, Burns DR, Moon P. In vitro comparison of the fracture resistance and failure mode of fiber, ceramic, and conventional post systems at various stages of restoration. J Prosthodont. 2001;10:26–36. doi: 10.1111/j.1532-849x.2001.00026.x. [DOI] [PubMed] [Google Scholar]
- 22.Hood JA, Farah JW, Craig RG. Modification of stresses in alveolar bone induced by a tilted molar. J Prosthet Dent. 1975;34:415–21. doi: 10.1016/0022-3913(75)90159-6. [DOI] [PubMed] [Google Scholar]
- 23.Hou Y, Wu G, Qing H, Zhu Z. Effect of a differently tilted angle of mandibular premolar on fracture resistance of 3 post-core restorations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:518–23. doi: 10.1016/j.tripleo.2011.02.027. [DOI] [PubMed] [Google Scholar]
- 24.Al-Wahadni AM, Hamdan S, Al-Omiri M, Hammad MM, Hatamleh MM. Fracture resistance of teeth restored with different post systems:In vitro study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:77–83. doi: 10.1016/j.tripleo.2008.03.038. [DOI] [PubMed] [Google Scholar]
- 25.Atash R, Arab M, Duterme H, Cetik S. Comparison of resistance to fracture between three types of permanent restorations subjected to shear force: An in vitro study. J Indian Prosthodont Soc. 2017;17:239–49. doi: 10.4103/jips.jips_24_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sirimai S, Riis DN, Morgano SM. An in vitro study of the fracture resistance and the incidence of vertical root fracture of pulpless teeth restored with six post-and-coresystems. J Prosthet Dent. 1999;81:262–9. doi: 10.1016/s0022-3913(99)70267-2. [DOI] [PubMed] [Google Scholar]
- 27.Haralur SB, Lahig AA, Al Hudiry YA, Al-Shehri AH, Al-Malwi AA. Influence of post angulation between coronal and radicular segment on the fracture resistance of endodontically treated teeth. J Clin Diagn Res. 2017;11:90–3. doi: 10.7860/JCDR/2017/27965.10470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hayashi M, Takahashi Y, Imazato S, Ebisu S. Fracture resistance of pulpless teeth restored with post-cores and crowns. Dent Mater. 2006;22:477–85. doi: 10.1016/j.dental.2005.03.017. [DOI] [PubMed] [Google Scholar]
- 29.Panitiwat P, Salimee P. Effect of different composite core materials on fracture resistance of endodontically treated teeth restored with FRC posts. J Appl Oral Sci. 2017;25:203–10. doi: 10.1590/1678-77572016-0306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schwartz RS, Robbins JW. Post placement and restoration of endodontically treated teeth: A literature review. J Endod. 2004;30:289–301. doi: 10.1097/00004770-200405000-00001. [DOI] [PubMed] [Google Scholar]
- 31.Giovani AR, Vansan LP, de Sousa Neto MD, Paulino SM. In vitro fracture resistance of glass-fiber and cast metal posts with different lengths. J Prosthet Dent. 2009;101:183–8. doi: 10.1016/S0022-3913(09)60025-1. [DOI] [PubMed] [Google Scholar]
- 32.Martinez-Inusa A, da Silva L, Rilo B, Santana U. Comparison of the fracture resistance of pulpless teeth restored with a cast post and core or carbon-fiber post with a composite core. J Prosthet Dent. 1997;78:5–9. doi: 10.1016/s0022-3913(98)70027-7. [DOI] [PubMed] [Google Scholar]
- 33.Darabi F, Namazi L. A comparison of the fracture resistance of endodontically treated teeth using two different restoration systems. Dent Res J. 2008;5:65–9. [Google Scholar]
- 34.Stockton LW. Factors affecting retention of post systems: A literature review. J Prosthet Dent. 1999;81:380–5. doi: 10.1016/s0022-3913(99)80002-x. [DOI] [PubMed] [Google Scholar]
- 35.Habibzadeh S, Rajati HR, Hajmiragha H, Esmailzadeh S, Kharazifard M. Fracture resistances of zirconia, cast Ni-Cr, and fiber-glass composite posts under all-ceramic crowns in endodontically treated premolars. J Adv Prosthodont. 2017;9:170–5. doi: 10.4047/jap.2017.9.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gu XH, Huang JP, Wang XX. An experimental study on fracture resistance of metal-ceramic crowned incisors with different post-core systems. Zhonghua Kou Qiang Yi Xue Za Zhi. 2007;42:169–72. [PubMed] [Google Scholar]
- 37.Freedman GA. Esthetic post-and-core treatment. Dent Clin North Am. 2001;45:103–16. [PubMed] [Google Scholar]
- 38.Akkayan B, Gülmez T. Resistance to fracture of endodontically treated teeth restored with different post systems. J Prosthet Dent. 2002;87:431–7. doi: 10.1067/mpr.2002.123227. [DOI] [PubMed] [Google Scholar]
- 39.Pilo R, Cardash HS, Levin E, Assif D. Effect of core stiffness on the in vitro fracture of crowned, endodontically treated teeth. J Prosthet Dent. 2002;88:302–6. doi: 10.1067/mpr.2002.127909. [DOI] [PubMed] [Google Scholar]
- 40.Caputo AA, Standlee JP. 1st ed. Chicago: Quintessence; 1987. Biomechanics in Clinical Dentistry; p. 134. [Google Scholar]


