Abstract
Aims and Objectives:
Dental implants have emerged as new treatment modality for the majority of patients and are expected to play a significant role in oral rehabilitation in the future. The present study was conducted to assess various factors affecting the survival rate of dental implants.
Materials and Methods:
The present retrospective study was conducted in the Department of Prosthodontics. In this study, 5200 patients with dental implants which were placed during June 2008–April 2015 were included. Exclusion criteria were patients with hormonal imbalance, patients with chronic infectious disease, patients receiving immunosuppressive therapy, pregnant women, drug and alcohol addicts, and patients with severe periodontal diseases. Parameters such as name, age, gender, length of implant, diameter of implant, location of implant, and bone quality were recorded. Data were tabulated and statistically evaluated with IBM SPSS Statistics for Windows, Version 20.0., IBM Corp., Armonk, NY, USA.
Results:
Out of 5200 patients, 2800 were males and 2400 females. Maximum implants failures (55) were seen in age group above 60 years of age (males – 550, females –700). Age group <40 years (males – 750, females – 550) showed 20 failed implants. Age group 41–60 years (males – 1500, females – 1150) showed 45 failed implants. The difference was nonsignificant (P = 0.21). Maximum implant failure was seen in implants with length >11.5 mm (40/700) followed by implants with <10 mm (20/1650) and 10–11.5 mm (60/2850). The difference was significant (P < 0.05). Maximum implants failure (30/1000) was seen in implants with diameter <3.75 mm followed by implants with diameter >4.5 mm (16/1600) and implants with diameter 3.75–4.5 mm (50/2600). The Chi-square test showed significant results (P < 0.05). Mandibular posterior showed 3.3% implants failure, maxillary posterior revealed 2.2%, maxillary anterior showed 2.1%, and mandibular anterior showed 1% failure rate; this difference was significant (P < 0.05). Type I bone showed 0.3% implant failure, Type II showed 1.95%, Type III showed 3%, and Type IV revealed 0.8% failure rate; this difference was significant (P < 0.05).
Conclusion:
Age, length of implant, diameter of implant, bone quality, and region of implant are factors determining the survival rate of implants. We found that implant above 11.5 mm length, and with diameter <3.75 mm, placed in the mandibular posterior region, in Type III bone showed maximum failures.
KEYWORDS: Bone quality, failure, implant, length of implant, success
INTRODUCTION
In ancient times, either removable or fixed partial dentures were the treatment modalities for the missing teeth. Dental implants have emerged as new treatment modality for the majority of patients and are expected to play a significant role in oral rehabilitation in the future.
A dental implant is a surgical component that interfaces with the bone of the jaw or skull to support a dental prosthesis such as a crown, bridge, denture, facial prosthesis or to act as an orthodontic anchor. 90%–95% has been reported as the success rate of implants over the 10 years.[1] Although it has become the treatment of choice for most of the dentists, still, the complications arising from dental implant placement are the biggest challenge.
Among various complications, bleeding from implant site, infection, and pain are early complications of implant. Dental implant failure is quite common. Lack of osseointegration during early healing, infection of the peri-implant tissues, and breakage are the reasons for implants failure. There are few indications and contraindications for implant placements. The contraindications of implant placement are patients with epilepsy, children and adolescents, patients having endocarditis, history of osteoradionecrosis, smokers, and diabetic patients. Absolute contraindications are patients with history of myocardial infarction, cerebrovascular accident, patients with history of bleeding, history of heart transplant, immune suppression, active treatment of malignancy, drug abusers, and psychiatric illness.[2]
There are many related factors affecting implant failure. First, group of factors are host related, second, related to implant placement site-related factors, third, related to surgery-related factors and fourth are implant fixture-related factors and fifth are implant prosthesis-related factor. Age and gender of the patient, smoking habits, systemic disease, and oral hygiene are host-related factors. Position in arch, quality, and quantity of bone are implant placement site-related factors. Initial stability, angulations and direction of implant and the skillfulness of an operator come under surgery-related factors. Surface roughness, length and diameter of dental implant, macrostructure and microstructure of an implant fixture are implant fixture-related factors. Type of prosthesis, retention method, and occlusal scheme are implant prosthesis-related factors.[3] Albrektsson et al. concluded that factors such as design and surface of implant, condition of implant placement site, surgery technique, and occlusal loading affect osteointegration.[4]
The present study was conducted in the Department of Prosthodontics to assess various factors affecting survival rate of dental implants.
MATERIALS AND METHODS
This retrospective study was conducted in the Department of Prosthodontics DY Patil Dental College, Pune. In this study, all the dental implants which were placed during June 2008–April 2015 which met the inclusion criteria were enrolled. The study was carried out by two trained persons by radiographic and clinical examination of patients with dental implants at follow-up visits based on survival rate of dental implant according to implant length, diameter (<3.75–11.5 mm), and bone quality. Sample size of 5200 was selected form total 7010 treated cases at 95% confidence level and 0.69 of confidence interval. In 5200 patients, 2800 were males and 2400 were females with age range of >41 years to <60 years. Informed consent was obtained from all the participating individuals. Ethical approval was obtained from Institutional Ethical Committee (ethical committee letter Ref No-DYP: 242A/2015). Exclusion criteria were patients with hormonal imbalance, patients with chronic infectious disease, patients receiving immunosuppressive therapy, pregnant women, drug and alcohol addicts, and patients with severe periodontal diseases.
Parameters such as name, age, gender, length of implant, diameter of implant, location of implant, and bone quality were recorded. Survival rate of implants was evaluated based on length, diameter, location (maxilla or mandible), and bone quality (Type-I, II, II, IV).
Results thus obtained were subjected to statistical analysis. P < 0.05 was considered significant. Data were statistically evaluated with IBM SPSS Statistics for Windows, Version 20.0., IBM Corp., Armonk, NY, USA using Chi-square test at significance of 0.05.
RESULTS
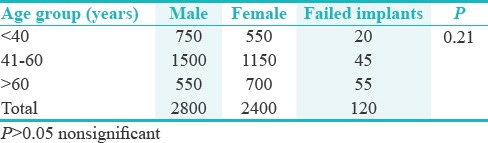
Table 1 shows that out of 5200 patients, 2800 were male and 2400 were females. Table 1 shows that maximum implants failures (55) were seen in age group above 60 years of age (males – 550, females – 700). Age group <40 years (males – 750, females – 550) showed 20 failed implants. Age group 41–60 years (males – 1500, females – 1150) showed 45 failed implants. The Chi-square test indicates nonsignificant P value [Table 1]. Graph 1 shows that maximum implants failure was seen in implants with length >11.5 mm (40/700) followed by implants with <10 mm (20/1650) and 10–11.5 mm (60/2850) and the difference was significant (P < 0.05).
Table 1.
Total number of failed implants
Graph 1.
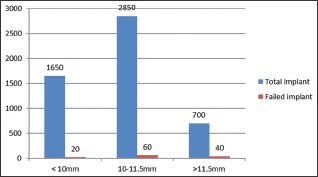
Survival rate according to implant length
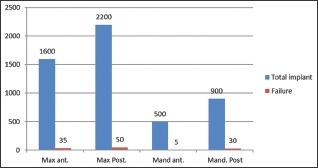
Graph 2 shows that maximum implants failure (30/1000) was seen in implants with diameter <3.75 mm followed by implants with diameter >4.5 mm (16/1600) and implants with diameter 3.75–4.5 mm (50/2600). The Chi-square test showed significant results (P < 0.05). Graph 3 shows that mandibular posterior had 3.3% implants failure, maxillary posterior revealed 2.2%, maxillary anterior showed 2.1%, and mandibular anterior showed 1% failure rate. The difference was significant (P < 0.05). Graph 4 shows that Type I bone showed 0.3% implant failure, Type II showed 1.95%, Type III showed 3%, and Type IV revealed 0.8% failure rate. The difference was significant (P < 0.05).
Graph 2.
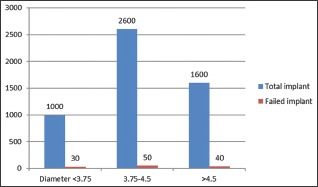
Survival rate according to implant diameter
Graph 3.
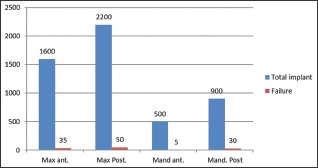
Survival rate according to bone quality
Graph 4.
Survival rate according to bone quality
DISCUSSION
Recent advancements in the field of dentistry have revolutionarized the use of dental implants. Thus, missing teeth can be well managed. Nowadays, there is increase in demand for dental implant. However, failures in implants are also common. Failure rates are early failure and late failure. Early failure is one that failed osseointegration within several weeks to months. Bone necrosis, bacterial infection, surgical trauma, inadequate initial stability, and early occlusal loading can result into early failure. Late failure is failure that turns up after functional loading of several period of time. It takes place because of infection and excessive loading.[5] The present study was to assess various factors affecting survival rate of dental implants.
We found that maximum implants failures (55) were seen in age group above 60 years of age. Age group <40 years showed 20 failed implants. Age group 41–60 years showed 45 failed implants. It has been seen that when patients age increases, failure rate had a tendency of increment.
We found that maximum implants failure was seen in implants with length >11.5 mm followed by implants with <10 mm and 10–11.5 mm. This is similar to the results of Albrektsson et al.[4] However, Esposito revealed that maximum failures were seen in implants with length between 10 and 11.5 mm.[6] Misch in his study showed that implants <10 mm had lower success rates (7%–25%) than longer 10 mm implants.[7]
In the present study, maximum implants failure was seen in implants with diameter <3.75 mm followed by implants with diameter >4.5 mm and implants with diameter 3.75–4.5 mm. This is in agreement with the results of Shirota et al.[8]
In the present study, mandibular posterior showed 3.3% implants failure, maxillary posterior revealed 2.2%, maxillary anterior showed 2.1%, and mandibular anterior showed 1% failure rate.
We observed that Type I bone showed 0.3% implant failure, Type II showed 1.95%, Type III showed 3%, and Type IV revealed 0.8% failure rate. Type I is the best bone with maximum implant survival rate.
Renouard in 2006 conducted a structured review based on Medline and hand search database during 1990–2005 period studies (53 studies) to evaluate the relationship between implant survival rates and their length and diameter. Published studies relevant to following factors were recorded: (i) implant length and diameter, (ii) implant survival rates, and (iii) criteria for implant failure which were placed in healed sites. He concluded that increased implant failure was associated with shorter and wider implant due to poor bone density and operator skill; however, short or wide implant may be considered in unfavorable site such as lesser bone density.[9] Borie et al. in the review article concluded that length, diameter, and connection of each implant have a degree of influence in bone biomechanics. They also stated that despite the influence of diameters and lengths of implant, peri-implant bone stress and strain should remain within the physiological limits to avoid a pathological overload, bone resorption, and consequent risk to the long-term success of implant prosthetic.[10]
Arsalanloo et al. stated that shorter implants can be used adjunct to longer one in case of bone grafting and wider implant used for scarce bone.[11] Busenlechner et al. stated that smoking and periodontal conditions double the implant failure rate.[12] Bataineh and Al-Dakes suggested that increase in implant length improves implant stability even with poor bone quality.[13] Yeşildal et al. suggested increase implant diameter over length for success.[14] Abraham et al. found lower compressive and tensile stresses in the peri-implant bone in the RP model compared to the NP model.[15] Topkaya et al. concluded that implant length and diameter are important in its success. They also stated that loss of neck alveolar bone has decreased success rate.[16] Wang et al. stated that adequate soft and hard tissues are needed for implant healing.[17] Narrow implant diameter has greater stress and higher failure rate than larger implant diameter.[18] Shigehara et al. done a study to evaluate long-term outcome of immediately loaded full-arch, fixed, one-piece prostheses supported by dental implants and suggested immediate implant for edentulous jaws.[19] French et al. observed longer survival rate in tissue- and bone-level implants than tapered effect implants.[20]
It has been observed from our study that higher failure rate is associated with smaller or wider diameter implants but higher success can be found with increased length. The success also depends on operators’ skill and available bone height and quality. Hence, careful selection of case and absence of systemic conditions help in improving the survival rate of implants.
Limitation of our study was that it was restricted to particular geographic location and patients reporting to particular hospital were only included.
Further long-term clinical studies are required to evaluate the various risk factors and implant diameter length on its success on different populations.
CONCLUSION
Age, length of implant, diameter of implant, bone quality, and region of implant are factors determining the survival rate of implants. We found that implant above 11.5 mm, implant with diameter <3.75 mm, implant placed in mandibular posterior region, implant placed in Type III bone showed maximum failures.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- 1.Tricio J, Laohapand P, van Steenberghe D, Quirynen M, Naert I. Mechanical state assessment of the implant-bone continuum: A better understanding of the Periotest method. Int J Oral Maxillofac Implants. 1995;10:43–9. [PubMed] [Google Scholar]
- 2.Buser D, Mericske-Stern R, Bernard JP, Behneke A, Behneke N, Hirt HP, et al. Long-term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multi-center study with 2359 implants. Clin Oral Implants Res. 1997;8:161–72. doi: 10.1034/j.1600-0501.1997.080302.x. [DOI] [PubMed] [Google Scholar]
- 3.Tonetti MS, Schmid J. Pathogenesis of implant failures. Periodontol. 2000;1994(4):127–38. doi: 10.1111/j.1600-0757.1994.tb00013.x. [DOI] [PubMed] [Google Scholar]
- 4.Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52:155–70. doi: 10.3109/17453678108991776. [DOI] [PubMed] [Google Scholar]
- 5.Kim SH, Kim SJ, Lee KW, Han DH. The effects of local factorson the survival rate of dental implants: A 19 year retrospective study. J Korean Acad Prosthodont. 2010;48:28–40. [Google Scholar]
- 6.Esposito M, Grusovin MG, Coulthard P, Thomsen P, Worthington HV. A 5-year follow-up comparative analysis of the efficacy of various osseointegrated dental implant systems: A systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants. 2005;20:557–68. [PubMed] [Google Scholar]
- 7.Misch CE. Short dental implants: A literature review and rationale for use. Dent Today. 2005;24:64–6. 68. [PubMed] [Google Scholar]
- 8.Shirota T, Ohno K, Suzuki K, Michi K. The effect of aging on the healing of hydroxylapatite implants. J Oral Maxillofac Surg. 1993;51:51–6. [PubMed] [Google Scholar]
- 9.Renouard F, Nisand D. Impact of implant length and diameter on survival rates. Clin Oral Implants Res. 2006;17(Suppl 2):35–51. doi: 10.1111/j.1600-0501.2006.01349.x. [DOI] [PubMed] [Google Scholar]
- 10.Borie E, Orsi IA, de Araujo CP. The influence of the connection, length and diameter of an implant on bone biomechanics. Acta Odontol Scand. 2015;73:321–9. doi: 10.3109/00016357.2014.961957. [DOI] [PubMed] [Google Scholar]
- 11.Arsalanloo Z, Telchi R, Osgouie KG. Optimum selection of the dental implants according to length and diameter parameters by FE Method in the anterior position. Int J Biosci Biochem Bioinform. 2014;4:265–9. [Google Scholar]
- 12.Busenlechner D, Fürhauser R, Haas R, Watzek G, Mailath G, Pommer B, et al. Long-term implant success at the academy for oral implantology: 8-year follow-up and risk factor analysis. J Periodontal Implant Sci. 2014;44:102–8. doi: 10.5051/jpis.2014.44.3.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bataineh AB, Al-Dakes AM. The influence of length of implant on primary stability: An in vitro study using resonance frequency analysis. J Clin Exp Dent. 2017;9:e1–6. doi: 10.4317/jced.53302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yeşildal R, Karabudak F, Bayındır F, Zamanlou H, Yildirim MP, Saǧsöz NP et al. Effect of implant diameter and length on stress distribution for titanium and zirconia implants by using finite element analysis (FEA) Open Access Libr J. 2015;2:1–7. [Google Scholar]
- 15.Abraham HM, Philip JM, Jain AR, Venkatakrishnan CJ. The effect of implant and abutment diameter on peri-implant bone stress: A three-dimensional finite element analysis. J Oral Res Rev. 2016;8:49–52. [Google Scholar]
- 16.Topkaya T, Solmaz MY, Dündar S, Eltas A. Numerical analysis of the effect of implant geometry to stress distributions of the three different commercial dental implant system. Cumhuriyet Dent J. 2015;18:17–24. [Google Scholar]
- 17.Wang F, Zhang Z, Monje A, Huang W, Wu Y, Wang G, et al. Intermediate long-term clinical performance of dental implants placed in sites with a previous early implant failure: A retrospective analysis. Clin Oral Implants Res. 2015;26:1443–9. doi: 10.1111/clr.12485. [DOI] [PubMed] [Google Scholar]
- 18.Termeie D, Klokkevold PR, Caputo AA. Effect of implant diameter and ridge dimension on stress distribution in mandibular first molar sites-A photoelastic study. J Oral Implantol. 2015;41:e165–73. doi: 10.1563/aaid-joi-D-14-00008. [DOI] [PubMed] [Google Scholar]
- 19.Shigehara S, Ohba S, Nakashima K, Takanashi Y, Asahina I. Immediate loading of dental implants inserted in edentulous maxillas and mandibles: 5-year results of a clinical study. J Oral Implantol. 2015;41:701–5. doi: 10.1563/aaid-joi-D-14-00018. [DOI] [PubMed] [Google Scholar]
- 20.French D, Larjava H, Ofec R. Retrospective cohort study of 4591 Straumann implants in private practice setting, with up to 10-year follow-up. Part 1: Multivariate survival analysis. Clin Oral Implants Res. 2015;26:1345–54. doi: 10.1111/clr.12463. [DOI] [PubMed] [Google Scholar]


