Abstract
Objective:
Diabetes mellitus (DM) is one of the major public health problems. Association of diabetes and periodontitis is widely proven and can influence each other in the development and progression of the disease and its complications, which are largely preventable. Hence, if data could be collected on the knowledge and awareness about the association between DM and periodontal disease, the results could be applied in creating public health campaigns and can bring about lifestyle modification among people. The aim of the present study is to assess the awareness, attitude, and practices of diabetic patients regarding their periodontal health in Davangere city with the objective of enhancing dental health education for this population, which would upgrade their knowledge and awareness.
Materials and Methods:
The present cross-sectional survey was carried out on 600 diabetic patients from various clinics. A time limit of 3 months was set for the data collection which was then subjected to statistical software SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1, Systat 12.0, and R environment version 2.11.1 for statistical analysis.
Results:
On correlation of gender and education with overall knowledge of association between periodontal disease and DM, females and participants below secondary school education and lower duration of DM were significantly associated with lack of knowledge. Other questions revealed limited awareness, sources, and need for more information about this association and depicted poor knowledge and attitude toward the oral health.
Conclusion:
Dental professionals need to create awareness about the importance of maintaining good oral health influencing overall general health in diabetic patients. Oral screening and referral by health professionals to dentists may benefit diabetic patients by improving access to dental care.
KEYWORDS: Association, diabetes, glycemic control, oral health awareness, periodontitis, questionnaire, survey
INTRODUCTION
Diabetes is a chronic metabolic disorder causing hyperglycemia which leads to long-term damage of different organs including the heart, eyes, kidneys, nerves, and vascular system including periodontium. Its chronic nature imposes significant increase in morbidity and mortality rates. Periodontitis is the most common oral infection in humans and is the major cause of tooth loss in adults. It has been considered as the sixth complication of diabetes due to its signs and symptoms.[1] The relationship between periodontal diseases and diabetes has become a recent focus of attention among health-care professionals because of substantial evidence supporting two-way relationship with diabetes; diabetes mellitus (DM) increases the risk of periodontitis and the periodontal inflammation negatively affecting glycemic control.[2] The recent rise in diabetes is not a genetic shift only but also an environmental as a result of lifestyle habits. The International Diabetes Federation plans on prevention of Type 2 diabetes based on controlling modifiable risk factors can be divided into two target groups: people at a high risk of developing Type 2 diabetes and the entire population similarly with the periodontal disease.[3] For successful treatment of DM and periodontitis as well, patients themselves are the most determining factor. Lack of information is one of the reasons for no adherence to lifestyle modification. Patients comply better with health-care regimens when informed and positively reinforced. Those who believe that they are highly susceptible to disease make more preventive dental visits.[4] Health education attempts to change behaviors by altering an individual's knowledge, attitudes, and beliefs about health matters. The present study aimed to gather baseline information on awareness, attitude, and practices of diabetic patients in Davangere city regarding their periodontal health in view of enhancing dental health education for the targeted population, which would upgrade their knowledge and awareness.
MATERIALS AND METHODS
The present study was a hospital-based, descriptive cross-sectional survey conducted in the city of Davangere, Karnataka state. Ethical clearance for the study was obtained from the Institutional Ethical Committee of Bapuji Dental College and Hospital, Davangere. Informed verbal consent was obtained from each participant before data collection, who was willing to participate in the study. The survey was conducted from November 2012 to January 2013.
METHODS OF COLLECTION OF DATA
The proposed study was carried out by requesting diabetic patients to fill a pretested questionnaire printed in English and local language (Kannada) focusing on the awareness of various diabetic complications and periodontal disease. Data were collected by visiting diabetic centers and private dental clinics and from the outpatient department of Bapuji Dental College and Hospital, Davangere.
Male and female participants with a known history of diabetes were included in the study. Pregnant, lactating mothers and participants not willing to participate in the study were excluded.
SAMPLE SIZE
A sample size of 600 was calculated based on a diabetic prevalence rate of 12.1% from a national survey[5] with allowable error of 20% (5% risk) using the statistical formula, n = 4pq/L2.
SAMPLING METHODOLOGY
The city of Davangere is the district headquarters and considered to be urban-based population. The list of diabetic centers and dental clinics was prepared by obtaining the required data from district health office and from the Indian Dental Association and Indian Medical Association Davangere branch. Efforts were made to include all the diabetic and dental clinics through personal attempts and visits. From the list prepared, a total of 600 participants from various clinics were selected based on inclusion and exclusion criteria.
DESCRIPTION OF QUESTIONNAIRE
The questionnaire was chosen as an appropriate methodology since it can be used to obtain standardized information. A structured questionnaire containing 34 questions divided into six parts based on a thorough review of the literature on diabetes and periodontal disease was designed. Development of questionnaire was based on the pilot study and from the previously published studies,[6,7] whereas some questions which were related to the knowledge about periodontal diseases were constructed by the authors based on the understanding of the disease. The validation of the questionnaire was regulated by means of face validation, content validation, reliability, and consistency tests by piloting it on 30. There was a complete anonymity of all the data collected in the study. The study was conducted by a single examiner.
STATISTICAL ANALYSIS
The statistical software SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1, Systat 12.0, and R environment version 2.11.1 were used for the analysis of the data. Descriptive and inferential statistical analysis has been carried out in the present study. Significance is assessed at 5% level of significance. The following assumptions on data are made.
Dependent variables should be normally distributed
Samples drawn from the population should be random, and cases of the samples should be independent.
Chi-square/Fisher's exact test has been used to find the significance of study parameters on categorical scale between two or more groups.
RESULTS
DEMOGRAPHIC STRUCTURE OF THE INTERVIEWED POPULATION
Majority of the participants were in the age group of 41–50 years (36.8%). Correlating gender with overall knowledge [Graph 1], it revealed that females were significantly associated with the absence of knowledge on association between periodontal disease and DM. Education level of the participants varied from below secondary to above secondary school level with the majority (54.3%) belonging to the latter group. Correlation of education with overall knowledge [Graph 2] revealed that below secondary school education was significantly associated with the lack of knowledge on association between periodontal disease and DM.
Graph 1.
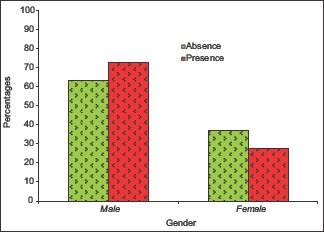
Overall knowledge of association between periodontal disease and diabetes mellitus
Graph 2.
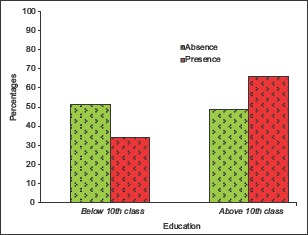
Overall knowledge of association between periodontal disease and diabetes mellitus
QUESTIONS ON THE LEVEL OF INFORMATION ABOUT DIABETES
Duration of diabetics among the participants ranged from <1 year to >15 years, among which majority of them were between 1 and 5 years (36%): When the participants were asked for type of diabetes, 63% did not know which type of diabetes they had. The percentage of participants taking medication was higher 87.7% than in participants not taking any medication, 12.3%. Correlation of duration of DM with overall knowledge showed that lower duration of DM is significantly associated with the absence of knowledge on association between periodontal disease and DM (with χ2 = 17.706; P = 0.001**) [Graph 3].
Graph 3.
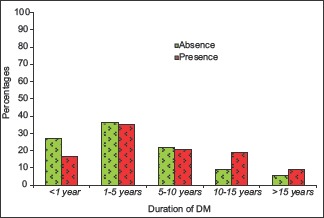
Overall knowledge of association between periodontal disease and diabetes mellitus
QUESTIONS ON THE LEVEL OF INFORMATION ABOUT SYSTEMIC COMPLICATIONS OF DIABETES
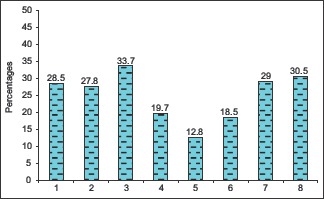
The percentage of participants who were aware of complication of eye disease was 63.3%, heart disease was 50.7%, kidney disease was 52.5%, stroke was 43.2%, and delayed wound healing was 62.2% [Graph 4].
Graph 4.
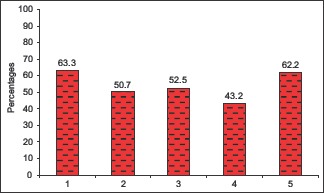
Questions on the level of information about systemic complications of diabetes
QUESTIONS ON ORAL HEALTH BEHAVIORS
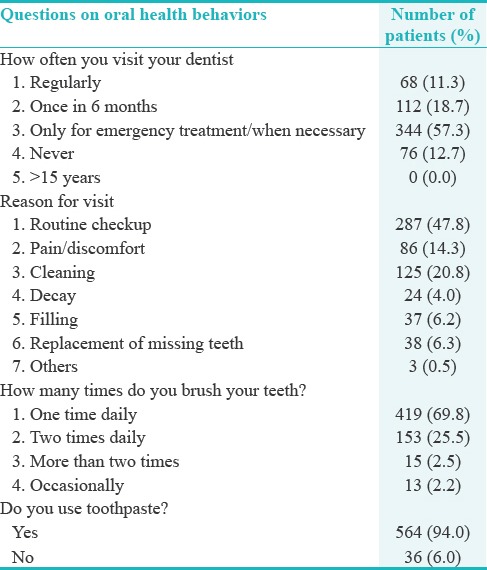
Upon asking how often they visit their dentist, 57.3% of them visited only when necessary. The reason for their visit was mainly routine checkup in 47.8%. Majority (69.8%) brushed once daily and 94.0% used toothpaste [Table 1].
Table 1.
Questions on oral health behaviors (n=600)
QUESTIONS ON AWARENESS OF SIGNS OF PERIODONTAL OR GUM DISEASE
The participants were asked for the signs of periodontal disease [Graph 5]; the percentage of them who answered “Yes” for various questions was less.
Graph 5.
Questions on awareness of signs of periodontal or gum disease
QUESTIONS ON THE LEVEL, SOURCE, AND NEED FOR MORE INFORMATION ABOUT THE ASSOCIATION BETWEEN PERIODONTAL DISEASE AND DIABETES MELLITUS
The answers to various questions are as described in Tables 2 and 3. On asking the participants, 69.0% were not aware that diabetics are more prone for gum infection than nondiabetics. Source of the information among 46.8% was from dentist. 64.8% reported their dentist knew that they had diabetes. Among all participants, 33.7% were told by the dentist that they have gum problem/disease. 65.0% were never told that they should be extra careful of oral health and visit a dentist often because they have diabetes. Only 33.2% had been told diabetes affects periodontal health, 34.0% had been told gum disease affects blood glucose control, and 71.7% were not aware that treatment of gum disease among diabetics may help in reducing blood glucose levels. Only 30.8% believed that their oral health would be better if they did not have diabetes. Among the participants, only 24.2% were aware about the association between oral health and diabetes unlike 75.8% who were not aware of the same; 48.0% of participants would like to get more reliable information by the dentist.
Table 2.
Questions on the level, source, and need for more information about the association between periodontal disease and diabetes mellitus (n=600)
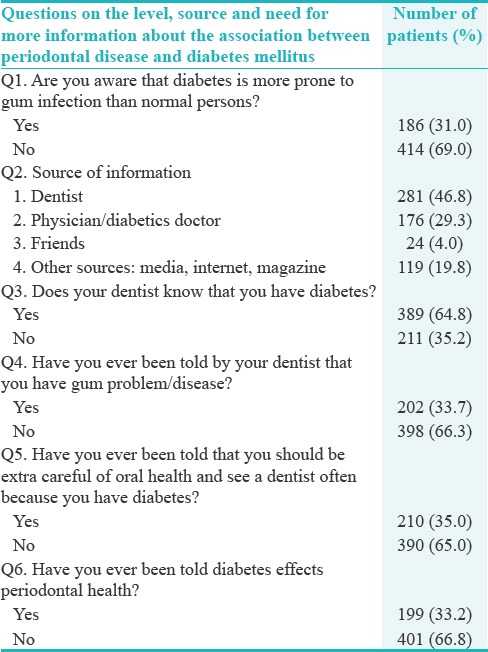
Table 3.
Questions on the level, source, and need for more information about the association between periodontal disease and diabetes mellitus (n=600)
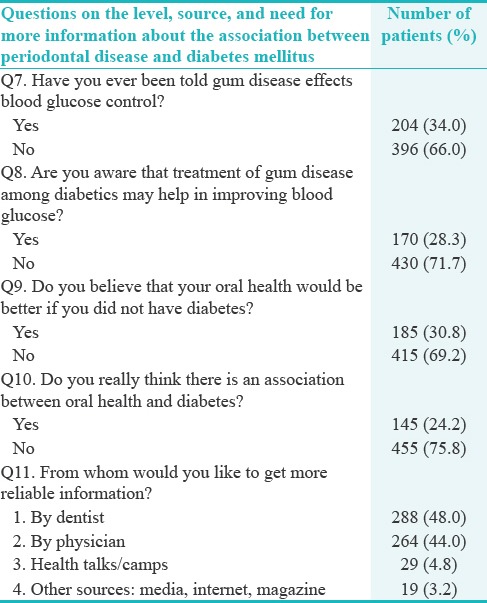
Overall level, source, and need for more information about the association between periodontal disease and DM [Graph 6] showed that the presence of knowledge is 34.0% (95% CI: 32.71%–35.32%) which is not statistically significant. Nine questions are identified for assessing the knowledge; any participant satisfying the five questions is assumed to have the knowledge (>50%).
Graph 6.
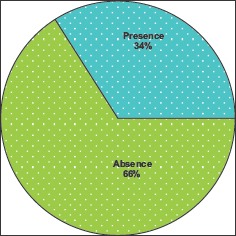
Overall level, source and need for more information about the association between periodontal disease and diabetes mellitus
DISCUSSION
The greatest increase in prevalence of DM is occurring in low- and middle-income countries[8] including Asia and Africa, affecting majority of its population by 2030.[9] A systematic review and meta-analysis of epidemiologic studies concluded that overall prevalence and odds of having diabetes are higher within periodontitis populations compared to people without periodontitis. Self-reported diabetes underestimates the prevalence when compared to this condition assessed clinically.[10] Further, in a review on relationship between diabetes and periodontal infection, the authors have concluded that periodontal disease is more prevalent and severe in diabetic than in healthy subjects and the level of metabolic control and duration of diabetes appear to influence the risk for periodontal disease, with a significant heterogeneity among diabetics.[11]
Evidence points to a vicious cycle of diabetes and periodontitis exacerbating each other, which ultimately brings the diabetics to the attention of oral health practitioners. Furthermore, the management of DM is largely dependent on patients’ ability to self-care in their daily lives, which is often better when the patient is educated regarding the importance of oral health. Therefore, patient education is always considered as an essential element.
Many studies have been conducted to assess the knowledge and awareness of diabetic patient about oral health in several countries, but very limited literature exists in India. Hence, the purpose of this study was to assess the awareness and attitude of diabetic patients about their periodontal health in view of enhancing dental health education, which would upgrade their knowledge, in turn controlling diabetes, and ultimately, the quality of life.
In the present study, majority of the participants belonged to the age group of 41–50 years (36.8%). The relationship of awareness of periodontal health was independent of age. Gender distribution of the study included male participants in higher proportion (66.3%) than females, and they were significantly associated with lack of knowledge on association between periodontal disease and DM (P = 0.021*). Correlating education, below secondary school education was significantly associated with lack of knowledge on association between periodontal disease and DM (P < 0.001**). A study done by Tang et al. reported that health literacy and patient awareness scores were negatively correlated to diabetic control;[12] Bakhshandeh et al.[13] demonstrated that diabetics with lower education levels were more likely to be diagnosed with periodontal disease. Attaining the primary outcome of evaluating the knowledge and awareness of the diabetics about their periodontal health status, which was found to be lower, a strong correlation between educational status and awareness was found whereas a weak positive correlation with age was established satisfying the secondary outcome of the study. This signifies that to develop effective patient education and to improve patients’ diabetic control, educational strategies also need to be considered for patients’ health literacy levels.
The level of information about diabetes was inadequate. In our study, about 3/4th of the participants were not aware of what type of diabetes they had. Lower duration of DM was significantly associated with the lack of knowledge on association between periodontal disease and DM similar to the study done by Bakhshandeh et al.,[13] where patients with longer duration were likely to have higher level of awareness. More than half of the participants in our study were aware of systemic complications (72%) and their percentage was high with eye disease and delayed wound healing. This could be probably due to the frequent visits to the physicians and ophthalmologists. However, as the study shifts from diabetes to correlation of diabetes and oral diseases, the percentage of awareness sinks down to 58%.
Various questions were asked specifically to assess oral health behaviors. Among the participants, 57.3% visited only when necessary. Similar findings were reported in other studies; the majority of them delayed their dental visit until they had toothache.[14,15,16] This shows that patients visit the dentist only when a problem arises which can be correlated with poor attitude of the patients. The self-reported awareness of signs of periodontal or gum disease was very low; similar results were reported by other studies where patients with periodontal disease were unaware.[17,18] This signifies that periodontal disease progresses as it is unnoticed by the patient.
Overall level, source, and need for more information about the association between periodontal disease and DM showed that the presence of knowledge was 34.0% which was not statistically significant, which is lower than previously reported by a Jordanian's study and Bahammam's study,[19,20] and Ummadisetty et al. indicated that 47.7% and 47.8% of the investigated diabetic patients were aware that they were more often affected by gum diseases and oral health complications than nondiabetic individuals, respectively,[21] signifying the need for dental health education and awareness among general public.
Nearly 60% of the diabetic patients were uninformed of mutual influence of diabetes and periodontal disease; among those who were aware, dentists were the main source of information; similar to other studies, half of the participants had got information from dentist.[19,20] Books, magazines and pamphlets, family and friends,[13] and television and internet were the other sources of information. According to a study conducted on Asian subjects, Tokuda et al.[22] concluded that there exists considerable association between trust in mass media and health of public. This vertical trust of public on the mass media can be effectively utilized for the education of periodontitis–DM association.
The majority of the patients in the present study reported that their dentist knew that they had diabetes. This was in accordance with other studies done by Sandberg et al.[23] (52%) and Jansson et al.[17] (91%) claiming that their dentist knew about their diabetes. 66.3% of the participants of our study stated that they had never been told by the dentist that they have gum problem/disease. This shows that either patient did not have the periodontal disease or dentists did not make an effort to inform the patient. This was similar to another study where 29% of subjects were advised by their health care professional to perform adequate oral hygeine and obtain routine dental care in patients with type 2 DM. Observation from our study recognizes that screening and referral by health professionals may benefit diabetic patients by improving access to dental care. A survey conducted among the students of medical, Ayurveda, and engineering colleges reported a substantial lack of oral hygiene understanding and limited knowledge of oral hygiene practices even in health professionals and engineering students.[24] Results from the research conducted by Al Habashneh et al. on diabetes and oral health: doctors’ knowledge, perception, and practices reported that only half advised their diabetic patients to consult a dentist concerning their oral health. Only a one-third of doctors agreed that oral health was an issue in controlling diabetes. General medical practitioners were less informed than specialized doctors about the relationship between oral health and diabetes.[19] Conference convened by the Columbia University College of Dental Medicine on “Diabetes and Oral Disease: Implications for Health Professionals” summarized and emphasized that interprofessional patient management is essential to achieve improved health outcomes in affected individuals. Hence, there is need for comprehensive educational programs to promote good oral health and impart education among professionals too.[25] The National Diabetes Education Program introduced the PPOD Checklist to promote proper diabetes management by pharmacists, podiatrists, optometrists, and dentists. Its goals are to ease communication among multiple providers, educate people with diabetes about needed examinations and of course the importance of metabolic control.
Paquette et al. stated that medical and dental professionals should be taught to practice more collaboratively to actively participate in their patients’ overall health management.[26]
Bowyer et al. reported that 69.1% of the interviewed study participants were never advised by health-care professionals on the correlation of oral hygiene with diabetes.[27]
Findings of the present study showed that most of the participants would like to get more reliable information by dentist and physician. Participants failed to recognize that periodontal disease might affect their glycemic level and the need for its control to prevent periodontal infections in diabetics; similar results were reflected in other studies too.[15,20,28] Weinspach et al.[29] reported that 56% of the participants of their study had an insufficient knowledge about the mutual influence between diabetes and periodontitis, which correlates with the current study (50.2%). Lin et al.[30] stated that endocrinologists and dentists are not equally equipped with the knowledge about the relationship between DM and periodontitis. In our study, only 46% (P < 0.0001) of the general physicians suggested their patients to visit a dentist. Our findings about the deficiency of oral health information in diabetics are similar to other clinical trials.[13,28,30,31] One of the studies showed that those with higher HbA1c levels had poor tooth brushing self-efficacy and higher plaque level.[27] Based on the scientific evidence, the European Federation for Periodontology/American Academy of Periodontology recommended that patients with diabetes should be monitored carefully and periodontitis, if present, should be treated promptly providing various guidelines to physicians and dentists.[32]
Studies have consistently shown that improved glycemic control reduces the rate of complications and evidence suggests that patients, who are knowledgeable about DM self-care, have better long-term glycemic control.[33,34,35] Thus, it is indispensable to ensure that patients’ knowledge, attitudes, and practices are adequate for preventive behaviors such as brushing, flossing, and periodic dental visits.
STRENGTH OF THE STUDY
A large number of sample size (586) from only one city was considered to draw a conclusion that was satisfactory
Participants from all the educational strata of the society were considered to avoid any bias based on their existing knowledge
Both the groups of diabetes were included that helped us to draw a better conclusion on the existing awareness of the patients
Few questions were formulated by the authors, which add onto the already existing literature for the same
Patients were more aware of the systemic complications related to the eye and wound healing, and there was less awareness related to the oral health which can be thus promoted after achieving this conclusion.
LIMITATIONS AND RECOMMENDATIONS
A future study of a larger Indian diabetic population will be needed to substantiate the findings from the present study and inclusion of economic status might potentiate the study.
In our study, the questionnaire has been used as a tool to assess the awareness and it would be more substantiating if we do the oral examination as well, to correlate the clinical findings and the presence of periodontitis. The idea of diabetes screening in the dental office has been suggested by several research groups. For this, chairside tests to measure HbA1C can be used. By conducting continuing education programs, we can improve the knowledge, attitude, and awareness about various dental and systemic diseases. A PPOD (by pharmacists, podiatrists, optometrists, and dentists) checklist tool can be introduced in Indian scenario too although the feasibility is questionable. Furthermore, emphasizing the field of periodontal medicine among the medical and dental fraternity will broaden the path of knowledge and directs the practitioner to treat successfully.
CONCLUSION
Association of DM and periodontal disease must be made aware to the general public and as well as also to the medical fraternity, who in turn can guide and motivate the patient for better diabetic control by maintaining good oral health. More dental health campaigns and awareness programs need to be conducted in India.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- 1.Löe H. Periodontal disease. The sixth complication of diabetes mellitus. Diabetes Care. 1993;16:329–34. [PubMed] [Google Scholar]
- 2.Preshaw PM, Alba AL, Herrera D, Jepsen S, Konstantinidis A, Makrilakis K, et al. Periodontitis and diabetes: A two-way relationship. Diabetologia. 2012;55:21–31. doi: 10.1007/s00125-011-2342-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.3rd ed. Brussels: International Diabetes Federation; 2006. International Diabetes Federation. Diabetes Atlas. [Google Scholar]
- 4.Kegeles SS. Some motives for seeking preventive dental care. J Am Dent Assoc. 1963;67:90–8. doi: 10.14219/jada.archive.1963.0231. [DOI] [PubMed] [Google Scholar]
- 5.Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, et al. High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia. 2001;44:1094–101. doi: 10.1007/s001250100627. [DOI] [PubMed] [Google Scholar]
- 6.Eldarrat AH. Diabetic patients: Their knowledge and perception of oral health. Libyan J Med. 2011;6:5691. doi: 10.3402/ljm.v6i0.5691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith RM, Fleming LE, Arheart KL, Wilkinson JD. Periodontal disease and diabetes: Knowledge and attitudes assessment project. Flo Public Health Rev. 2007;4:12–7. [Google Scholar]
- 8.World Health Organization. Global Report on Diabetes. Geneva: World Health Organization; 2016. [Last accessed on 2016 Aug 30]. Available from: www.who.int/diabetes/global-report/en/ [Google Scholar]
- 9.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 10.Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: A systematic review and meta-analysis. Int J Epidemiol. 2011;40:804–18. doi: 10.1093/ije/dyr029. [DOI] [PubMed] [Google Scholar]
- 11.Llambés F, Arias-Herrera S, Caffesse R. Relationship between diabetes and periodontal infection. World J Diabetes. 2015;6:927–35. doi: 10.4239/wjd.v6.i7.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang YH, Pang SM, Chan MF, Yeung GS, Yeung VT. Health literacy, complication awareness, and diabetic control in patients with type 2 diabetes mellitus. J Adv Nurs. 2008;62:74–83. doi: 10.1111/j.1365-2648.2007.04526.x. [DOI] [PubMed] [Google Scholar]
- 13.Bakhshandeh S, Murtomaa H, Vehkalahti MM, Mofid R, Suomalainen K. Oral self-care and use of dental services among adults with diabetes mellitus. Oral Health Prev Dent. 2008;6:279–86. [PubMed] [Google Scholar]
- 14.Taani DQ. Periodontal awareness and knowledge, and pattern of dental attendance among adults in Jordan. Int Dent J. 2002;52:94–8. doi: 10.1111/j.1875-595x.2002.tb00607.x. [DOI] [PubMed] [Google Scholar]
- 15.Almas K, Albaker A, Felembam N. Knowledge of dental health and diseases among dental patients, a multicentre study in Saudi Arabia. Indian J Dent Res. 2000;11:145–55. [PubMed] [Google Scholar]
- 16.Quteish Taani DS. Dental fear among a young adult Saudian population. Int Dent J. 2001;51:62–6. doi: 10.1002/j.1875-595x.2001.tb00823.x. [DOI] [PubMed] [Google Scholar]
- 17.Jansson H, Lindholm E, Lindh C, Groop L, Bratthall G. Type 2 diabetes and risk for periodontal disease: A role for dental health awareness. J Clin Periodontol. 2006;33:408–14. doi: 10.1111/j.1600-051X.2006.00929.x. [DOI] [PubMed] [Google Scholar]
- 18.Brady WF. Periodontal disease awareness. J Am Dent Assoc. 1984;109:706–10. doi: 10.14219/jada.archive.1984.0187. [DOI] [PubMed] [Google Scholar]
- 19.Al Habashneh R, Khader Y, Hammad MM, Almuradi M. Knowledge and awareness about diabetes and periodontal health among Jordanians. J Diabetes Complications. 2010;24:409–14. doi: 10.1016/j.jdiacomp.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 20.Allen EM, Ziada HM, O’Halloran D, Clerehugh V, Allen PF. Attitudes, awareness and oral health-related quality of life in patients with diabetes. J Oral Rehabil. 2008;35:218–23. doi: 10.1111/j.1365-2842.2007.01760.x. [DOI] [PubMed] [Google Scholar]
- 21.Ummadisetty T, Chava VK, Bhumanapalli VR. Diabetes and periodontitis: How well are the patients aware about an established relation? J Indian Soc Periodontol. 2016;20:472–5. doi: 10.4103/0972-124X.184035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tokuda Y, Fujii S, Jimba M, Inoguchi T. The relationship between trust in mass media and the healthcare system and individual health: Evidence from the Asia Barometer Survey. BMC Med. 2009;7:4. doi: 10.1186/1741-7015-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sandberg GE, Sundberg HE, Wikblad KF. A controlled study of oral self-care and self-perceived oral health in type 2 diabetic patients. Acta Odontol Scand. 2001;59:28–33. doi: 10.1080/000163501300035742. [DOI] [PubMed] [Google Scholar]
- 24.Dayakar MM, Kumar J, Pai GP, Shivananda H, Rekha R. A survey about awareness of periodontal health among the students of professional colleges in Dakshina Kannada district. J Indian Soc Periodontol. 2016;20:67–71. doi: 10.4103/0972-124X.168487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Albert DA, Ward A, Allweiss P, Graves DT, Knowler WC, Kunzel C, et al. Diabetes and oral disease: Implications for health professionals. Ann N Y Acad Sci. 2012;1255:1–5. doi: 10.1111/j.1749-6632.2011.06460.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paquette DW, Bell KP, Phillips C, Offenbacher S, Wilder RS. Dentists’ knowledge and opinions of oral-systemic disease relationships: Relevance to patient care and education. J Dent Educ. 2015;79:626–35. [PubMed] [Google Scholar]
- 27.Bowyer V, Sutcliffe P, Ireland R, Lindenmeyer A, Gadsby R, Graveney M, et al. Oral health awareness in adult patients with diabetes: A questionnaire study. Br Dent J. 2011;211:E12. doi: 10.1038/sj.bdj.2011.769. [DOI] [PubMed] [Google Scholar]
- 28.Moore PA, Orchard T, Guggenheimer J, Weyant RJ. Diabetes and oral health promotion: A survey of disease prevention behaviors. J Am Dent Assoc. 2000;131:1333–41. doi: 10.14219/jada.archive.2000.0388. [DOI] [PubMed] [Google Scholar]
- 29.Weinspach K, Staufenbiel I, Memenga-Nicksch S, Ernst S, Geurtsen W, Günay H, et al. Level of information about the relationship between diabetes mellitus and periodontitis – Results from a nationwide diabetes information program. Eur J Med Res. 2013;18:6. doi: 10.1186/2047-783X-18-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin H, Zhang H, Yan Y, Liu D, Zhang R, Liu Y, et al. Knowledge, awareness, and behaviors of endocrinologists and dentists for the relationship between diabetes and periodontitis. Diabetes Res Clin Pract. 2014;106:428–34. doi: 10.1016/j.diabres.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 31.Moore PA, Weyant RJ, Mongelluzzo MB, Myers DE, Rossie K, Guggenheimer J, et al. Type 1 diabetes mellitus and oral health: Assessment of periodontal disease. J Periodontol. 1999;70:409–17. doi: 10.1902/jop.1999.70.4.409. [DOI] [PubMed] [Google Scholar]
- 32.Chapple IL, Genco R. Working group 2 of joint EFP/AAP workshop. Diabetes and periodontal diseases: Consensus report of the joint EFP/AAP workshop on periodontitis and systemic diseases. J Clin Periodontol. 2013;40(Suppl 14):S106–12. doi: 10.1111/jcpe.12077. [DOI] [PubMed] [Google Scholar]
- 33.Tash RH, O’Shea RM, Cohen LK. Testing a preventive-symptomatic theory of dental health behavior. Am J Public Health Nations Health. 1969;59:514–21. doi: 10.2105/ajph.59.3.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Saengtipbovorn S, Taneepanichskul S. Effectiveness of lifestyle change plus dental care (LCDC) program on improving glycemic and periodontal status in the elderly with type 2 diabetes. BMC Oral Health. 2014;14:72. doi: 10.1186/1472-6831-14-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saengtipbovorn S, Taneepanichskul S. Lifestyle change plus dental care (LCDC) program improves knowledge, attitude, and practice (KAP) toward oral health and diabetes mellitus among the elderly with type 2 diabetes. J Med Assoc Thai. 2015;98:279–90. [PubMed] [Google Scholar]


