Abstract
Background
Health-related quality of life (HRQoL) measurement in elderly people can provide appropriate information for an optimal management of physical/mental conditions. The main objective of the present study was to quantitatively assess the HRQoL among healthy elder Iranian individuals as measured by the Short-Form 36 (SF-36) questionnaire, both overall and at the level of each its single component/domain.
Methods
This study was designed as a systematic review and meta-analysis, following the "Preferred Reporting Results of Systematic Reviews and Meta-Analyses" (PRISMA) guidelines. Embase, PubMed/MEDLINE, ISI/Web of Science (WOS), Scopus, and Iranian databases such as MagIran, SID and Irandoc were mined from inception up to 1st September 2017. Also the grey literature (via Google Scholar) was mined. Two reviewers independently screened titles/abstracts, assessed full-text articles, extracted data, and appraised their quality using the "Strengthening the Reporting of Observational Studies in Epidemiology" (STROBE) checklist.
Results
Twenty five studies were included. Mean overall HRQoL was 54.92 [95%CI 51.50–58.33], lower than the value found by studies done in other countries, especially in those economically developed. The sensitivity analysis indicated stability and reliability of results. Pooled scores of each HRQoL domain/sub-scale of the SF-36 questionnaire ranged from 49.77 (physical role functioning) to 63.02 (social role functioning).
Conclusions
HRQoL among healthy elder Iranian individuals is generally low. Health policy-makers should put HRQoL among the elderly as a priority of their agenda, implementing ad hoc programs and providing social, economic and psychological support, as well as increasing the participation of old people in the community life and use their experiences.
Electronic supplementary material
The online version of this article (10.1186/s12955-018-0845-7) contains supplementary material, which is available to authorized users.
Keywords: Health-related quality of life, Systematic review and meta-analysis, Iran, Elderly
Background
Recent scientific achievements and medical advancements have resulted in increasing life expectancy and in ageing of the population, both in developed and developing countries [1]. This has led to a higher risk of developing chronic degenerative diseases. Iran is one of the developing countries, which, in the recent years, has seen a growing increase in the number of elderly together with declining fertility rates. In particular, the proportion of elderly population has significantly increased from 7.22% in 2006 to 8.20% in 2011, and, according to some estimates, is projected to further increase to 10.5% within 2025 and to 21.7% within 2050 [2].
Health outcome measurement and assessment enable to evaluate the performance of health plans and their impact, informing decision- and policy-makers in adopting scientific evidence-based, effective decisions [3]. Among the patient-reported outcomes (PROs), health-related quality of life (HRQoL) is the perceived quality of an individual’s health status and daily life, in terms of physical, mental and spiritual well-being. HRQoL represents a very useful indicator of overall health, capturing detailed information on both the physical and mental health status of subjects, and on their impact on quality of life. Various factors, such as gender and age as well as culturally prevailing values and standards, individual interests, social relationships, personal beliefs, economic and environmental features, can affect HRQoL [4, 5].
Ageing and ageing-related disease can impact too on both HRQoL and health-related costs. Due to limited financial resources in the health sector and the increased demand for healthcare services [6], HRQoL measurement in elderly people can provide both researchers and stakeholders with appropriate information for an optimal management of physical and mental conditions.
Extant studies conducted in different countries show that healthy ageing generally does not impact negatively on HRQoL, indicating that spending a long period in good quality of life is possible. Cultural differences do not usually influence the subjective dimension of quality of life, whereas they impact on its objective dimension [7].
Several Iranian studies have explored HRQoL in elderly population: however, they have produced contrasting findings. For instance, Tajvar and colleagues have found that HRQoL among elderly in Iran is particularly poor and low, whilst Tanjani and coworkers have concluded that HRQoL in Iran is well comparable with the values obtained in other countries [8]. To overcome the limitations that plague single primary studies (for example, in terms of small sample sizes), it is possible to carry out a systematic review and meta-analysis, which, pooling together different researches, increases their statistical power and enable to obtain more statistically robust and reliable findings.
As such, the present study was designed as a systematic review and meta-analysis of the literature and was conducted with the main objective of quantitatively assessing the HRQoL among healthy elderly Iranian individuals, both overall and of its single domain or component, since HRQoL is a multi-dimensional concept. The results of the present study could provide Iranian decision- and policy-makers with valuable insights for evidence-based decisions.
Material and methods
The current systematic review and meta-analysis has been performed according to the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” (PRISMA) guidelines [9]. Two authors independently searched different scholarly databases: namely, Embase, PubMed/MEDLINE, ISI/Web of Science (WOS), Scopus, and Iranian databases such as MagIran, SID and Irandoc from 1st January 2000 up to 1st September 2017. Also the grey literature (via Google Scholar) was mined. Studies written in English or in Persian language were searched. Our search strategy was as follows: (“Quality of Life” OR “Health-Related Quality of Life” OR “Life Style” OR “QOL” OR “HRQoL”) AND (“Short-form questionnaire 36” OR “Questionnaire SF-36” OR “SF-36”) AND (“Elderly” OR “Aging”) AND “Iran”. Medical subject headings (MeSH) and wild-card options were used where appropriate. This search strategy was planned together with an information specialist.
In addition, reference lists of each identified study were examined for potentially eligible studies.
Inclusion criteria were: i) studies assessing HRQoL among health elderly people using the Short-Form 36 (SF-369 questionnaire, which is a validated, highly reliable and psychometrically sound instrument, comprising eight different domains/subscales: namely, physical functioning (PF), physical role functioning (PRF), bodily pain (BP), general health perceptions (GHP), vitality (VT), social role functioning (SRF), emotional role functioning (ERF), and mental health (MH) [6, 7]; and ii) studies reporting sufficient quantitative details such as standard deviation or standard error.
Exclusion criteria were: i) studies assessing HRQoL in sick elderly people; ii) studies with unclear results; iii) studies designed as clinical trials or reviews; iv) studies assessing overlapping populations (that is to say, dealing with the same populations); v) studies assessing HRQoL but not using the SF-36 questionnaire; and vi) studies not carried out in Iran.
Quality assessment of the included studies was evaluated using the 22-item “Strengthening the Reporting of Observational Studies in Epidemiology” (STROBE) checklist [10]. Studies were classified in good (score in the range 17–22), medium [8–16] and poor [1–7] quality studies.
Two authors independently extracted the following data from the selected studies: first author, publication year, sample size, mean age of the participants, mean overall HRQoL score and scores of each domain of the SF-36 questionnaire.
Statistical analysis
The mean overall HRQoL score and the scores for each domain/sub-scale of the SF-36 questionnaire were estimated with their 95% confidence intervals (CI). To assess heterogeneity between studies I2 test was used [11]. If this amount was less than 50%, the fixed model was used, otherwise a stochastic model (IV-Heterogeneity) was used.
Since SF-36 is a multi-dimensional construct, with eight domains/sub-scales, which can show different aspects of HRQoL, scores for each component were collected and synthesized separately. Additionally, two summary measures, namely the Physical Component Summary (PCS) and the Mental Component Summary (MCS) scores were pooled together in order to obtain a direct picture of HRQoL.
A sensitivity analysis was performed to ensure the stability and robustness of the results [12]. To assess heterogeneity, meta-regression analyses were conducted on the basis of the sample and publication year. Egger’s test was used to investigate the presence of publication bias [13]. P-values < 0.05 were considered as statistically significant. All statistical analyses were performed using the software STATA (version 12.0).
Results
After the initial search and after deleting duplicates, 25 studies, meeting the inclusion criteria, were retained and analyzed [14–38], as shown in Fig. 1.
Fig. 1.
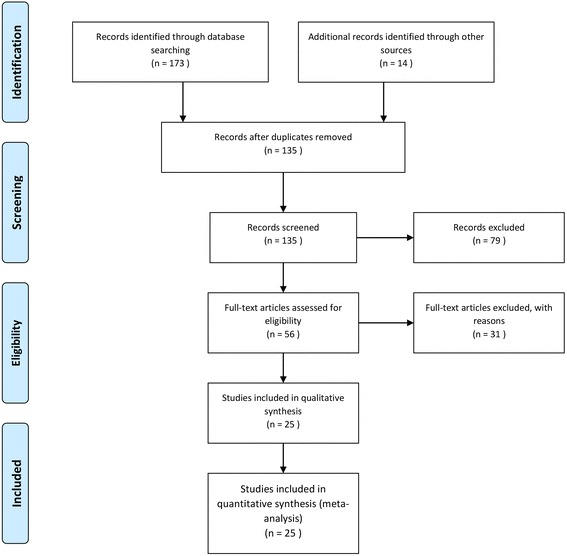
Flow-chart of the search strategy utilized in the current systematic review and meta-analysis
Among the included studies, 25 articles reported the overall HRQoL score, whilst 24 of them reported also the scores of each domain or sub-scale of the SF-36 questionnaire. The total number of participants in the current systematic review and meta-analysis was 12,328 elderly individuals. The sample size of the studies ranged from 56 to 5600 subjects. Characteristics of the included studies are shown in Table 1.
Table 1.
Main characteristics of the studies included in the current systematic review and meta-analysis
| Author | Year | City | Province | Sample size | Mean |
|---|---|---|---|---|---|
| Ghaderi | 2014 | Tabriz | East Azerbaijan | 56 | 51.64 |
| Farhadi | 2011 | Bushehr | Bushehr | 69 | 32.1 |
| Abdoli | 2012 | Tehran | Tehran | 80 | 67.04 |
| Shirvani | 2016 | Borujen | Chaharmahal and Bakhtiari | 80 | 70.06 |
| Naseh | 2014 | Shahrekord | Chaharmahal and Bakhtiari | 87 | 41.56 |
| Jadidi | 2015 | Tehran | Tehran | 141 | 50.36 |
| Abdollahi | 2013 | Sari | Mazandaran | 153 | 70.39 |
| Aghanuri | 2012 | Arak | Markazi | 165 | 55.66 |
| Mohammadiannia | 2013 | Bushehr | Bushehr | 173 | 56.41 |
| Heravi-Karimooi | 2013 | Tehran | Tehran | 180 | 66.49 |
| Salehi | 2012 | Tehran | Tehran | 203 | 72.1 |
| Heydari | 2012 | Sari | Mazandaran | 220 | 46.031 |
| Hedayati | 2014 | Shiraz | Fars | 220 | 50.76 |
| Hekmatpou | 2014 | Arak | Markazi | 269 | 50.22 |
| Zahmatkeshan | 2012 | Bushehr | Bushehr | 360 | 47.75 |
| Nejati | 2008 | Kashan | Isfahan | 389 | 62.35 |
| Vahdaninia | 2005 | Tehran | Tehran | 396 | 53.9 |
| Tajvar | 2008 | Tehran | Tehran | 400 | 59.43 |
| Darvishpoor Kakhki | 2013 | Tehran | Tehran | 400 | 45.24 |
| Salarilak | 2013 | Kamyaran | Kurdistan | 400 | 60.62 |
| Farzianpour | 2016 | Tehran | Tehran | 400 | 49.7 |
| Rakhshani | 2014 | Shiraz | Fars | 500 | 50.8 |
| Babak | 2016 | Isfahan | Isfahan | 637 | 54.64 |
| Hajian-Tilaki | 2017 | Babol | Mazandaran | 750 | 56.8 |
| Abbasimoghadam | 2009 | Tehran | Tehran | 5600 | 51.589 |
Based on the STROBE checklist, 17, 5 and 3 studies were considered of high, medium and poor quality, respectively.
The pooled overall HRQoL score based on the random model was computed to be 54.92 [95%CI 51.50–58.33], with a statistically significant amount of heterogeneity (I2 = 99.1%) (Fig. 2).
Fig. 2.
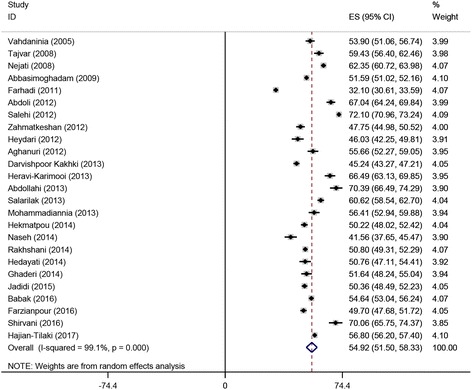
Forest plot of the studies included in the current systematic review and meta-analysis and reporting the overall health-related quality of life score assessed with the Short-Form 36 questionnaire
The result of the sensitivity analysis is shown in Fig. 3, indicating stability and reliability of results. Findings of the meta-regression analyses stratified according to the year of publication and to the sample size are shown in Fig. 4a and b. Both meta-regressions were not statistically significant (p-value for publication year = 0.867, and p-value for sample size = 0.701).
Fig. 3.
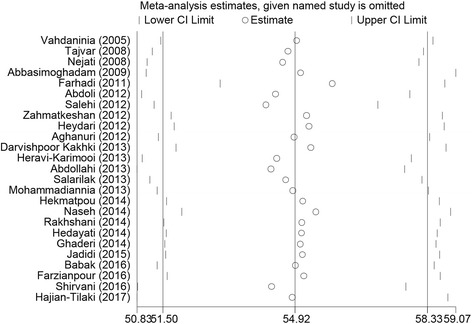
Sensitivity analysis of the studies included in the current systematic review and meta-analysis and reporting the overall health-related quality of life score assessed with the Short-Form 36 questionnaire
Fig. 4.
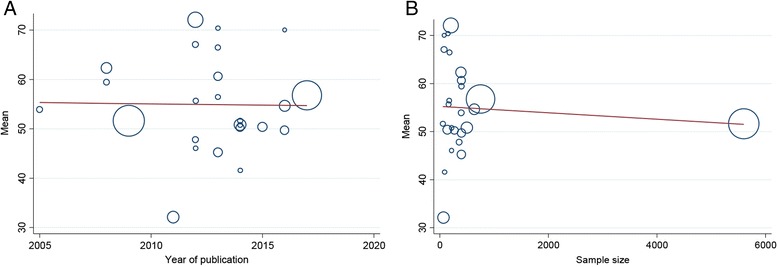
Meta-regressions carried out on the basis of publication year (a) and sample size (b)
Pooled scores of each HRQoL domain/sub-scale of the SF-36 questionnaire (ranging from 49.77 to 63.02) are shown in Fig. 5, while PCS (pooled ES 53.65 [95%CI 49.36–57.94]) and MCS (pooled ES 57.58 [95%CI 53.79–61.37]) scores are pictorially represented in Figs. 6 and 7, respectively.
Fig. 5.
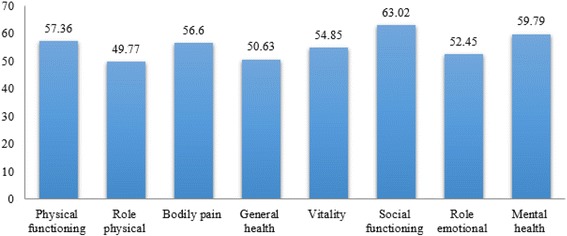
Pooled scores of each health-related quality of life domain/sub-scale assessed with the Short-Form 36 questionnaire
Fig. 6.

The Physical component summaries (PCS)
Fig. 7.
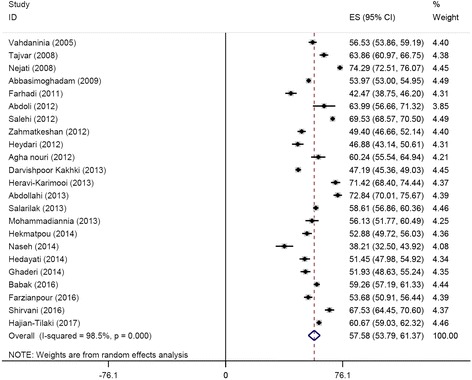
The mental component summaries (MCS)
Subgroup analyses were carried out stratifying the results according to the score of each domain/subscale of the SF-36 questionnaire (Table 2). Egger’s test value for the overall score and for the scores of the eight domains did not show any evidence of publication bias (overall p = 0.0948, PF p = 0.063, PRF p = 0.143, BP p = 0.690, GHP p = 0.529, VT p = 0.907, SRF p = 0.967, ERF p = 0.672, and MH p = 0.560).
Table 2.
Subgroup analyses of the studies included in the current systematic review and meta-analysis and reporting the score of each health-related quality of life domain/sub-scale assessed with the Short-Form 36 questionnaire
| Domains/subscales | Mean (95%CI) | I2 | P-value |
|---|---|---|---|
| Physical functioning (PF) | 57.36 (50.62 to 65.10) | 99.6% | 0.000 |
| Physical role physical functioning (PRF) | 49.77 (39.98 to 59.57) | 99.7% | 0.000 |
| Bodily pain (BP) | 56.60 (53.44 to 59.66) | 97.7% | 0.000 |
| General health perceptions (GHP) | 50.63 (47.75 to 53.50) | 98.5% | 0.000 |
| Vitality (VT) | 54.85 (51.72 to 57.98) | 98.5% | 0.000 |
| Social role functioning (SRF) | 63.02 (60.13 to 65.90) | 97.8% | 0.000 |
| Emotional role functioning (ERF) | 52.45 (42.86 to 62.04) | 99.8% | 0.000 |
| Mental health (MH) | 59.79 (55.60 to 63.98) | 99.0% | 0.000 |
Discussion
The current study examined HRQoL in Iranian elderly people, using SF-36, a questionnaire that comprehensively assess various aspects of health [39].
Concerning mean overall HRQoL, in our study it was lower than the value found by, studies done in other countries, especially in those economically developed [40–46]. In Australia, data from the “Dynamic Analyses to Optimise Ageing” (DYNOPTA) project have shown that SF-36 scores range from 60.04 to 82.16, depending on the sub-scale. Similar results have been reported in the United Kingdom [47], in New Zealand [48], and in China [49], among others. In Germany, SF-36 scores ranged from 59.46 to 88.74 for males and from 57.25 to 84.24 for females, depending on the domain [50]. On the other hand, scholars in Chile have found rather low values (ranging from 49.1 to 55.7 for males and from 43.8 to 53.3 for females) [51].
Differences in health programs and in access to healthcare services provided can explain this discrepancy, as well as cultural, social, and economic factors, among others [52].
Concerning the different dimensions/sub-scales of the SF-36 questionnaire (Additional file 1), the findings of this study showed that GHP, PRF, and ERF reported the lowest scores [43, 53, 54], probably due to poor healthcare services for elderly people compared with the general population and lack of adequate funds [55], together with both individual and societal factors, since HRQoL is a multidimensional construct [56]. A low HRQoL among the elderly could be improved by targeted programs of health promotion, prevention and delivery of high-quality services.
Low HRQoL is associated with higher mortality rate. In elderly people, lack of movement increases the risk of suffering from cardiovascular disease, cancer, and diabetes, among others. A correct diet, regular exercise and periodic check-ups can maintain and promote an active and healthy life [57–59]. Reduced societal interactions and communications, as well as ageing-related psychological and behavioral features can explain a decreased score in the GHP domain/sub-scale [43]. Low physical health due to changes in lifestyle, economic status and lack of appropriate welfare services also contribute to a reduced HRQoL. Presence of partner during ageing could be of great help to individual happiness, preventing isolation, depression and premature death [60].
On the other hand, in our study, SRF and MH reported the highest scores. This could be attributed to the particular status of elderly people in the Iranian society, in that respect for the elderly is a religious and societal tenet [61].
Decision- and policy-makers should allocate resources in improving access to healthcare services and mental training among the elderly [62, 63], as Iran’s population has grown rapidly in the last years and is now significantly ageing.
In the last years, Iran has done many remarkable efforts in implementing various programs for health promotion, even though focusing less on the elderly [64]. It should be an onus to improve and enhance HRQoL among the elderly subjects. Iran, like many other developing countries, has limited financial resources in the health sector [65] and HRQoL assessment can play a major role in a rational resources allocation.
The present study had some limitations that should be properly cited, with the most important being the high heterogeneity between studies probably caused by differences in study conditions. Further, there is a dearth of data concerning HRQoL in some provinces of Iran and in rural environments, since most studies have been conducted in urban areas and in large cities.
On the other hand, the present study has some strengths, in that it adds to the extant literature, being, for example, more comprehensive and exhaustive than the systematic review and meta-analysis carried out by Farajzadeh and collaborators [66], which was based on 21 studies, where ours is based on 25 primary researches [67].
Conclusion
The results of this study showed that HRQoL among healthy elderly Iranian individuals is generally low. Health policy-makers should put HRQoL among the elderly as a priority of their agenda, implementing ad hoc programs and providing social, economic and psychological support, as well as increasing the participation of old people in the community life and use their experience.
Acknowledgements
The authors are grateful to the reviewers for their constructive comments, which improved the manuscript.
Funding
Not applicable.
Availability of data and materials
Not applicable. This study is a systematic review and we used a primary data, but all data are archived according to the Swedish Act concerning the Ethical Review of Research Involving Humans to attain confidentiality. Data are therefore not publicly available but are available from the corresponding author upon reasonable request.
Abbreviations
- BP
Bodily pain
- CI
Confidence intervals
- ERF
Emotional role functioning
- GHP
General health perceptions
- HRQoL
Health-related quality of life
- MCS
Mental Component Summary
- MeSH
Medical Subject Headings
- MH
Mental health
- PCS
Physical Component Summary
- PF
Physical functioning
- PRF
Physical role functioning
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROs
Patient-reported outcomes
- SF-36
The Short-Form 36
- SID
Scientific Information Database
- SRF
Social role functioning
- STROBE
STrengthening the Reporting of OBservational studies in Epidemiology
- VT
Vitality
- WOS
Web of Science
Additional file
Pooled scores of each health-related quality of life domain/sub-scale assessed with the Short-Form 36 questionnaire. (DOCX 99 kb)
Authors’ contributions
Study design: MB, ST, Collected data: ST, MB, MB, MTM, MS, Data analysis: MB, MB, Final revision and grammar editing: NLB, AA, MM. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12955-018-0845-7) contains supplementary material, which is available to authorized users.
Contributor Information
Sogand Tourani, Email: sogandtourani@yahoo.com.
Masoud Behzadifar, Email: masoudbehzadifar@gmail.com.
Mariano Martini, Email: mariano.yy@gmail.com.
Aidin Aryankhesal, Email: aryankhesal.a@iums.ac.ir.
Masood Taheri Mirghaed, Email: masood.mirghaed@gmail.com.
Morteza Salemi, Email: morsal59@gmail.com.
Meysam Behzadifar, Email: m_behzadifar67@yahoo.com.
Nicola Luigi Bragazzi, Email: robertobragazzi@gmail.com.
References
- 1.Global elderly care in crisis. Lancet. 2014;383(9921):927. [DOI] [PubMed]
- 2.Danial Z, Motamedi MH, Mirhashemi S, Kazemi A, Mirhashemi AH. Ageing in iran. Lancet. 2014;384(9958):1927. doi: 10.1016/S0140-6736(14)62278-9. [DOI] [PubMed] [Google Scholar]
- 3.Couzner L, Ratcliffe J, Lester L, Flynn T, Crotty M. Measuring and valuing quality of life for public health research: application of the ICECAP-O capability index in the Australian general population. Int J Public Health. 2013;58(3):367–376. doi: 10.1007/s00038-012-0407-4. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. (WHO). Measuring quality of. life. 1997; Available from: http://www.who.int/mental_health/media/68.pdf
- 5.Saxena S, Carlson D, Billington R, Orley J. The WHO quality of life assessment instrument (WHOQOL-Bref): the importance of its items for cross-cultural research. Qual Life Res 2001;10(8):711–721. [DOI] [PubMed]
- 6.Harrefors C, Savenstedt S, Axelsson K. Elderly people's perceptions of how they want to be cared for: an interview study with healthy elderly couples in northern Sweden. Scand J Caring Sci. 2009;23(2):353–360. doi: 10.1111/j.1471-6712.2008.00629.x. [DOI] [PubMed] [Google Scholar]
- 7.Netuveli G, Blane D. Quality of life in older ages. Br Med Bull. 2008;85:113–126. doi: 10.1093/bmb/ldn003. [DOI] [PubMed] [Google Scholar]
- 8.Tanjani PT, Motlagh ME, Nazar MM, Najafi F. The health status of the elderly population of Iran in 2012. Arch Gerontol Geriatr. 2015;60(2):281–287. doi: 10.1016/j.archger.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 9.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ. 2007;85(11):867–872. doi: 10.2471/BLT.07.045120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thabane L, Mbuagbaw L, Zhang S, Samaan Z, Marcucci M, Ye C, et al. A tutorial on sensitivity analyses in clinical trials: the what, why, when and how. BMC Med Res Methodol. 2013;13(92) [DOI] [PMC free article] [PubMed]
- 13.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vahdani Nia MS, Goshtasebi A, Montazeri A, Maftoon F. Health-related quality of life in an elderly population in Iran: a population-based study. Payesh. 2005;4(2):113–120. [Google Scholar]
- 15.Nejati V, Ashayeri H. Health related quality of life in the elderly in Kashan. IJPCP. 2008;14(1):56–61. [Google Scholar]
- 16.Tajvar M, Arab M, Montazeri A. Determinants of health-related quality of life in elderly in Tehran, Iran. BMC Public Health. 2008;8(323) [DOI] [PMC free article] [PubMed]
- 17.Abbasimoghadam MA, Dabiran S, Safdari R, Djafarian K. Quality of life and its relation to sociodemographic factors among elderly people living in Tehran. Geriatr Gerontol Int. 2009;9(3):270–275. doi: 10.1111/j.1447-0594.2009.00532.x. [DOI] [PubMed] [Google Scholar]
- 18.Farhadi A, Foroughan M, Mohammadi F. The quality of life among rural elderlies a cross-sectional study. Salmand. 2011;6(2):38–46. [Google Scholar]
- 19.Abdoli B, Modaberi S, Comparison SP. Of the quality of life for healthy active and sedentary elderly and with osteoarthritis. Annals of. Biol Res. 2012;3(5):2337–2342. [Google Scholar]
- 20.Agha nouri A, Mahmoudi M, Salehi H, Jafarian K. Quality of life in the elderly people covered by health centers in the urban areas of Markazi Province. Iran Salmand. 2012;6(4):20–29. [Google Scholar]
- 21.Heydari J, S K, Shahhosseini Z. Health-related quality of life of elderly living in nursing home and homes in a district of Iran: implications for policy makers. Indian J Sci Technol 2012;5(5):2782–2787.
- 22.Salehi L, Salaki S, Alizadeh L. Health-related quality of life among elderly member of elderly centers in Tehran. IRJE. 2012;8(1):14–20. [Google Scholar]
- 23.Zahmatkeshan N, Bagherzadeh R, Akaberian S, Yazdankhah MR, Mirzaei K, Yazdanpanah S, et al. Assessing quality of life and related factors in Bushehr,s elders. J Fasa Univ Med Sci. 2012;2(1):53–58. [Google Scholar]
- 24.Abdollahi F, Mohammadpour RA. Health related quality of life among the elderly living in nursing home and homes. J Mazandaran Univ Med Sci. 2013;23(104):20–25. [Google Scholar]
- 25.Darvishpoor Kakhki A, Saeedi JA. Factors related to health-related quality of life (HRQoL) of elderly people in Tehran. 2013;23(82):8–16. [Google Scholar]
- 26.Heravi-Karimooi M, Rejeh N, Montazeri A. Health-related quality of life among abused and non-abused elderly people: a comparative study. Payesh. 2013;12(5):479–488. [Google Scholar]
- 27.Mohammadiannia M, Foroughan M, Rassafiani M, Hosseinzadeh S. Visual functioning and its relations with quality of life in the older people using governmental outpatient clinics Services in the City of Boushehr. Salmand. 2013;7(4):16–26. [Google Scholar]
- 28.SalariLak S, Gorginkaraji L, Amiri S. Quality of life in elderly population in Kamyaran district, 2009. J Urmia Univ Med Sci. 2013;24(1):24–29. [Google Scholar]
- 29.Ghaderi D, Mostafaee A. A study on the relationship between religious orientations and quality of life among elderly men living in nursing homes and those living with their families in Tabriz. Salmand. 2014;9(1):14–21. [Google Scholar]
- 30.Hedayati HR, Hadi N, Mostafavi L, Akbarzadeh A, Montazeri A. Quality of life among nursing home residents compared with the elderly at home. Shiraz E-Med J. 2014;15(4):e22718. doi: 10.17795/semj22718. [DOI] [Google Scholar]
- 31.Hekmatpou D, Jahani F, Behzadi F. Study the quality of life among elderly women in arak in 2013. AMUJ. 2014;17(2):1–8. [Google Scholar]
- 32.Naseh L, Shaikhy R, Rafii F. Quality of life and its related factors among elderlies living in nursing homes. IJN. 2014;27(87):67–78. [Google Scholar]
- 33.Rakhshani T, Shojaiezadeh D, Lankarani KB, Rakhshani F, Kaveh MH, Zare N. The association of health-promoting lifestyle with quality of life among the Iranian elderly. Iran Red Crescent Med J. 2014;16(9):e18404. doi: 10.5812/ircmj.18404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jadidi A, Farahaninia M, Janmohammadi S, Haghani H. The relationship between spiritual well-being and quality of life among elderly people. Holist Nurs Pract. 2015;29(3):128–135. doi: 10.1097/HNP.0000000000000081. [DOI] [PubMed] [Google Scholar]
- 35.Babak A, Daneshpajouhnejad P, Davari S, Aghdak P, Pirhaji O, Jahangiri P. Quality of life among the elderly under the protection of health and treatment centers in Isfahan Province, Iran, and its relationship with depression and body mass index. J Isfahan Med Sch. 2016;34(393):885–892. [Google Scholar]
- 36.Farzianpour F, Arab M, Foroushani AR, Zali Mehran EM. Evaluation of the criteria for quality of life of elderly health care centers in Tehran Province. Iran Glob J Health Sci. 2016;8(7):68–76. doi: 10.5539/gjhs.v8n7p68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shirvani M, Heidari M. Quality of life in postmenopausal female members and non-members of the elderly support association. J Menopausal Med. 2016;22(3):154–160. doi: 10.6118/jmm.2016.22.3.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hajian-Tilaki K, Heidari B, Hajian-Tilaki A. Health related quality of life and its socio-demographic determinants among Iranian elderly people: a population based cross-sectional study. J Caring Sci. 2017;6(1):39–47. doi: 10.15171/jcs.2017.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tsai SY, Chi LY, Lee CH, Chou P. Health-related quality of life as a predictor of mortality among community-dwelling older persons. Eur J Epidemiol. 2007;22(1):19–26. doi: 10.1007/s10654-006-9092-z. [DOI] [PubMed] [Google Scholar]
- 40.Bartsch LJ, Butterworth P, Byles JE, Mitchell P, Shaw J, Anstey KJ. Examining the SF-36 in an older population: analysis of data and presentation of Australian adult reference scores from the dynamic analyses to optimise ageing (DYNOPTA) project. Qual Life Res. 2011;20(8):1227–1236. doi: 10.1007/s11136-011-9864-0. [DOI] [PubMed] [Google Scholar]
- 41.Capuron L, Moranis A, Combe N, Cousson-Gelie F, Fuchs D, De Smedt-Peyrusse V. Vitamin E status and quality of life in the elderly: influence of inflammatory processes. Br J Nutr. 2009;102(10):1390–1394. doi: 10.1017/S0007114509990493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.García EL, Banegas JR, Pérez-Regadera AG, Cabrera RH, Rodríguez-Artalejo F. Social network and health-related quality of life in older adults: a population-based study in Spain. Qual Life Res. 2005;14(2):511–520. doi: 10.1007/s11136-004-5329-z. [DOI] [PubMed] [Google Scholar]
- 43.Lima MG, Barros MB, César CL, Goldbaum M, Carandina L, Ciconelli RM. Health related quality of life among the elderly: a population-based study using SF-36 survey. Cad Saude Publica. 2009;25(10):2159–2167. doi: 10.1590/S0102-311X2009001000007. [DOI] [PubMed] [Google Scholar]
- 44.Miranda LC, Soares SM, Silva PA. Quality of life and associated factors in elderly people at a reference center. Cien Saude Colet. 2016;21(11):3533–3544. doi: 10.1590/1413-812320152111.21352015. [DOI] [PubMed] [Google Scholar]
- 45.Mishra GD, Gale CR, Sayer AA, Cooper C, Dennison EM, Whalley LJ, et al. How useful are the SF-36 sub-scales in older people? Mokken scaling of data from the HALCyon programme. Qual Life Res. 2011;20(7):1005–1010. doi: 10.1007/s11136-010-9838-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tsai SY, Chi LY, Lee LS, Chou P. Health-related quality of life among urban, rural, and island community elderly in Taiwan. J Formos Med Assoc. 2004;103(3):196–204. [PubMed] [Google Scholar]
- 47.Walters SJ, Munro JF, Brazier JE. Using the SF-36 with older adults: a cross-sectional community-based survey. Age Ageing. 2001;30(4):337–343. doi: 10.1093/ageing/30.4.337. [DOI] [PubMed] [Google Scholar]
- 48.Stephens C, Alpass F, Baars M, Towers A, Stevenson B. SF-36v2 norms for new Zealanders aged 55-69 years. N Z Med J. 2010;123(1327):47–57. [PubMed] [Google Scholar]
- 49.Wang R, Wu C, Zhao Y, Yan X, Ma X, Wu M, et al. Health related quality of life measured by SF-36: a population-based study in shanghai, China. BMC Public Health. 2008;8(292) [DOI] [PMC free article] [PubMed]
- 50.Kurth BM, Ellert U. The SF-36 questionnaire and its usefulness in population studies: results of the German health interview and examination survey 1998. Soz Praventivmed. 2002;47(4):266–277. doi: 10.1007/BF01326408. [DOI] [PubMed] [Google Scholar]
- 51.Lera L, Fuentes-García A, Sánchez H, Albala C. Validity and reliability of the SF-36 in Chilean older adults: the ALEXANDROS study. Eur J Ageing. 2013;10(2):127–134. doi: 10.1007/s10433-012-0256-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dickson VV, Howe A, Deal J, MM MC. The relationship of work, self-care and quality of life in a sample of older working adults with cardiovascular disease. Heart Lung. 2011;41(1):5–14. doi: 10.1016/j.hrtlng.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 53.Lam CLK, Gandek B, Ren XS, Chan MS. Tests of scaling assumptions and construct validity of the Chinese (HK) version of the SF-36 health survey. J Clin Epidemiol. 1998;51(11):1139–1147. doi: 10.1016/S0895-4356(98)00105-X. [DOI] [PubMed] [Google Scholar]
- 54.Wyss K, Wagner AK, Whiting D, Mtasiwa DM, Tanner M, Gandek B, et al. Validation of the Kiswalhili version of the SF-36 health survey in a representative sample of an urban population in Tanzania. Qual Life Res. 1999;8(1–2):111–120. doi: 10.1023/A:1026431727374. [DOI] [PubMed] [Google Scholar]
- 55.Skarupski KA, Mendes de Leon CF, Bienias JL, Scherr PA, Zack MM, Moriarty DG, et al. Black-white differences in health- related quality of life among older adults. Qual Life Res. 2007;16(2):287–296. doi: 10.1007/s11136-006-9115-y. [DOI] [PubMed] [Google Scholar]
- 56.Hambleton P, Keeling S, McKenzie M. The jungle of quality of life: mapping measures and meanings for elders. Australas J Ageing. 2009;28(1):3–6. doi: 10.1111/j.1741-6612.2008.00331.x. [DOI] [PubMed] [Google Scholar]
- 57.Drewnowski A, Evans WJ. Nutrition, physical activity, and quality of life in older adults: summary. J Gerontol A Biol Sci Med Sci. 2001;56(2):89–94. doi: 10.1093/gerona/56.suppl_2.89. [DOI] [PubMed] [Google Scholar]
- 58.Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med 2016;4:2050312116671725. [DOI] [PMC free article] [PubMed]
- 59.Thompson WW, Zack MM, Krahn GL, Andresen EM, Barile JP. Health-related quality of life among older adults with and without functional limitations. Am J Public Health. 2012;102(3):496–502. doi: 10.2105/AJPH.2011.300500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ferrucci L, Giallauria F, Guralnik JM. Epidemiology of aging. Radiol Clin N Am. 2008;46(4):643–652. doi: 10.1016/j.rcl.2008.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Aghamolaei T, Tavafian SS, Zare S. Health related quality of life in elderly people living in Bandar Abbas, Iran: a population-based study. Acta Med Iran. 2010;48(3):185–191. [PubMed] [Google Scholar]
- 62.Roe B, Beech R, Harris M, Beech B, Russell W, Gent D, et al. Improving quality of life for older people in the community: findings from a local partnerships for older people project innovation and evaluation. Prim Health Care Res Dev. 2011;12(3):200–213. doi: 10.1017/S1463423611000053. [DOI] [PubMed] [Google Scholar]
- 63.Goharinezhad S, Maleki M, Baradaran HR, Ravaghi H. Futures of elderly care in Iran: a protocol with scenario approach. Med J Islam Repub Iran. 2016;30:416. [PMC free article] [PubMed] [Google Scholar]
- 64.Lankarani KB, Alavian SM, Peymani P. Health in the Islamic Republic of Iran, challenges and progresses. Med J Islam Repub Iran. 2013;27(1):42–49. [PMC free article] [PubMed] [Google Scholar]
- 65.Naghavi M. Health transition in Iran. Irje. 2006;13(1):13–25. [Google Scholar]
- 66.Farajzadeh M, Ghanei Gheshlagh R, Sayehmiri K. Health related quality of life in Iranian elderly citizens: a systematic review and meta-analysis. Int J Community Based Nurs Midwifery. 2017;5(2):100–111. [PMC free article] [PubMed] [Google Scholar]
- 67.Tourani S, Aryankhesal A, Behzadifar M. Improving the search strategy of systematic reviews and meta-analysis. Int J Community Based Nurs Midwifery. 2017;5(4):417–418. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable. This study is a systematic review and we used a primary data, but all data are archived according to the Swedish Act concerning the Ethical Review of Research Involving Humans to attain confidentiality. Data are therefore not publicly available but are available from the corresponding author upon reasonable request.


