Abstract
Background: Evidence from epidemiological and experimental studies illustrates the beneficial impact of healthy lifestyle behaviours on cardiovascular risk.
Objectives: To assess the effectiveness of primary care health education interventions designed to promote healthy lifestyles on physical activity levels and cardiovascular risk.
Methods: A computer-aided search on PubMed and Scopus was performed to identify relevant studies published from January 2000 to October 2016. Two authors independently selected studies for inclusion and extracted data, including intervention characteristics and outcome measures, namely physical activity and cardiovascular risk or risk factors.
Results: Of the 212 identified studies, 15 met the inclusion criteria. The 15 studies enrolled 6727 participants; the sample size varied between 74 and 878 adults. Fourteen studies assessed physical activity by questionnaire and only one study used accelerometry. Eight of the 15 studies showed improvements in the physical activity levels after the intervention, ranging from 5% to 26% in those where significant changes between groups were detected. Most studies reported significant positive effects of the health education interventions on cardiovascular risk factors, mainly on lipid profile, blood pressure and cardiovascular risk score.
Conclusion: The health education interventions, in primary care, seem to improve daily physical activity, cardiovascular risk factors and risk score.
Keywords: Systematic reviews and meta-analyses, health education, prevention, general practice/family medicine, general
KEY MESSAGES
Health education interventions increase daily physical activity levels.
Primary care interventions focusing on healthy lifestyles improve cardiovascular risk score, lipid profile and blood pressure
Introduction
The mortality attributed to cardiovascular diseases (CVD) has fallen considerably in the last decades; nonetheless, it remains the major cause of premature death in Europe and worldwide [1]. The most recommended management strategy to reduce cardiovascular risk and cope with modifiable cardiovascular risk factors, including sedentary behaviour, overweight/obesity and hypertension [1], is the change of unhealthy lifestyle behaviours [2–5]. Primary healthcare interventions, by preventing and modifying CVDs risk factors [6], are a frontline strategy to fulfil this purpose. However, many barriers hamper the implementation of the recommended ‘high-risk’ approach, such as health professionals’ difficulties to assimilate multiple risk factors into an accurate assessment of cardiovascular risk [7]. Indeed, the adherence to the guidelines and lifestyle counselling is less than optimal and often abandoned by primary caregivers [7,8].
Lifestyle and health education programmes tend to be multidisciplinary with self-care components tailored to individual risk factors [9]. The beneficial impact of healthy lifestyle behaviours on cardiovascular risk was demonstrated in a three-year randomized trial in the primary care setting [10].
Health education refers to the improvement of individual, group, institutional, community and systemic strategies to expand health knowledge, attitudes, skills and behaviours [11]. It aims to enhance health literacy, and behaviour and lifestyles changes conducive to health through the educational process [11]. Usually, these programmes use different channels (mobile applications, face-to-face, text messaging, internet based tools, written educational materials such as flyers and booklets) to empower individuals to adopt healthy lifestyles [11].
Previous reviews on this topic [2–5,12], focusing on a specific tool to deliver the intervention (e.g. text messaging, face-to-face interventions), were conducted. In contrast, the present review is broader by not focusing on intervention tools but by highlighting the intervention features (intervention design) that make it most likely to increase daily physical activity (PA). In the present review, we provide a critical review of the literature linking healthy lifestyles, cardiovascular risk and/or risk factors and PA in primary care, and to discuss the impact of those interventions on PA. Having in mind the importance of PA, the aim of this review is to analyse the effectiveness of health education interventions for change of lifestyle, with particular emphasis on PA and cardiovascular risk, in primary care.
Methods
Databases and search strategy
We used preferred reporting items for systematic reviews and meta-analysis statement (PRISMA) standards to systematically search PubMed and Scopus for studies in the English language that evaluated the effects of health education interventions focused on change of lifestyle in primary care, on humans, published from January 2000 to October 2016 [13]. The search terms were: (counselling OR education OR intervention OR health promotion) AND (primary care) AND (cardiovascular risk) AND (physical activity OR healthy lifestyles) AND (randomized controlled trials). Reference lists of studies identified by electronic searches were then searched to identify further articles relating to the topic of the review and to ensure that appropriate articles were obtained. In addition, to avoid retrieval bias, we manually searched the reference lists of landmark studies and background articles on this topic to look for any relevant citations that electronic searches might have missed.
Selection criteria for studies
All studies retrieved from our search needed to meet the following inclusion criteria: randomized controlled trials; adult human subjects in primary prevention; submitted to a health education intervention, as defined in the introduction, aiming to enhance health literacy, and the adoption of healthy lifestyles; with PA as endpoint, regardless of being the primary or secondary endpoint. Studies were excluded on the basis of the following: review papers; letters or editorial articles; studies not involving a health education intervention; studies involving interventions with supervised exercise sessions; studies with children and adolescents and those only involving individuals aged over 65 years.
Study selection
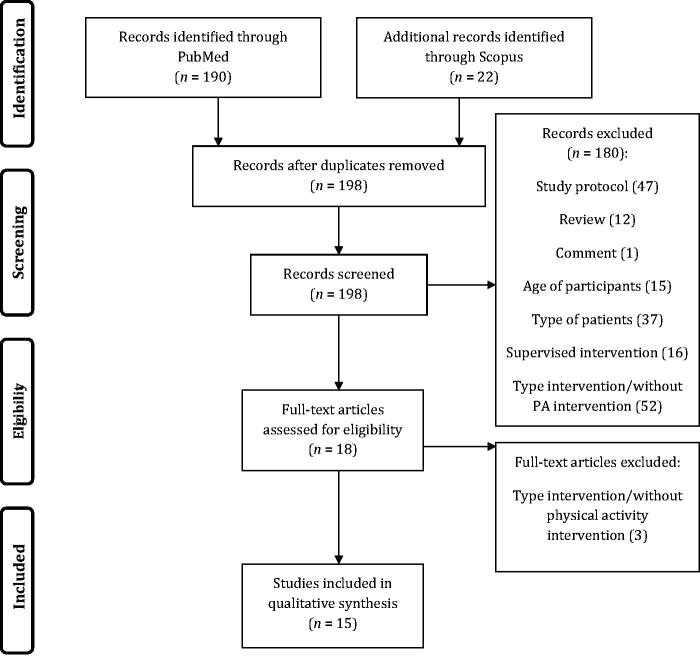
Two authors determined whether studies fulfilled the criteria for inclusion in this review through screening titles, abstracts, and keywords of the studies identified in the electronic search. When both authors failed to reach an agreement, the full text of the respective study was obtained and analysed to establish suitability. All studies classified as relevant by either of the authors were retrieved. Then, a standardized form was used to determine the eligibility for inclusion in the review based on the information within the full paper. A third author resolved disagreements. Figure 1 shows the process of the study identification and selection.
Figure 1.
Study identification and selection flow diagram.
Data extraction and methodological quality assessment
Two authors independently extracted data relevant to the review using a customized form. Data were extracted for study design, population, type and characteristics of the intervention, and outcomes, namely PA and cardiovascular risk or risk factors. Two authors using the PEDro scale independently assessed the methodological quality of each study. A third author resolved disagreements. The PEDro scale comprises 10 items that relate to internal validity and interpretability [14]. The scale provides an overall indication of RCT quality in a scale of 0 to 10. A study was rated as having ‘high’ methodological quality if it attained six points or more; the PEDro scale is a valid and reliable measure of the methodological quality of clinical trials [14,15].
Results
A total of 212 studies were identified in the electronic databases search. After reviewing the title and abstract, 13 papers were excluded by being duplicates (i.e. coming from the two different databases). Of the remaining 198 papers, 184 were further discarded due to the following reasons: comprised supervised exercise interventions (n = 16), the studies did not assess a measure of PA and type of intervention (n = 56), enrolled participants with established disease (for instance ankylosing spondylitis) (n = 36), review papers (n = 12), comments (n = 1), participants were children or old adults (n = 15), or pregnant women (n = 1), papers describing the study protocol for a randomized controlled trial (n = 47) (Figure 1). Therefore, only 15 studies were included in this review (Table 1). One study was excluded from the review because it has two publications of the same study [16].
Table 1.
Studies of the effects of health education intervention in physical activity.
| Reference | PEDro score | Participants | Intervention |
PA assessment | PA results/conclusions | ||
|---|---|---|---|---|---|---|---|
| Type/provider | Follow-up | ||||||
| Azar et al., 2016 [17] | 8/10 | 74 participants Immediate Group: 37 (22 women); 59.6 ± 11.9 years Delayed group: 37 (22 women); 59.8 ± 10.5 years |
24 weekly face-to-face groups videoconference + seven in-person group based PA Physicians, nutritionists, exercise physiologists and lifestyle coaches |
Six m | Stanford seven-day PA recall | Change from baseline to three m, mean (95% CI): Immediate group: 652.8 (236.8–1068.7) Delayed group: 103.6 (–294.8–501.9) Between-group difference: 549.2 (–26.8–1125.2) |
No changes in PA in either group at three and six months |
| Griffin et al.,2014 [27] | 8/10 | 478 participants with T2DM. IG: 239 (89 women), 59.5 ± 7.5 years CG: 239 (91 women), 59.8 ± 7.5 years |
Intensive treatment plus a theory-based behaviour change intervention: 1 h introductory meeting + six 30 min meetings + four brief phone calls Lifestyle facilitators |
12 m | Four days accelerometry and Norfolk PA questionnaire | IG: 90.0 ± 55.1–95.2 ± 55.7 MET- h/week CG: 78.6 ± 48.0 to 80.1 ± 49.5 MET-h/week |
PA improved in both groups. No significant differences between groups at one year in PA both objectively and subjectively measured. |
| Reid et al., 2014 [29] | 7/10 | 426 family members of patients with CAD. IG: 211 (128 women), 52.0 ± 11.9 years CG: 215 (133 women), 51.1 ± 11.3 years |
17 counselling sessions (one face-to-face +16 telephone); weekly for the first 12 weeks and then at weeks 16, 20, 26, 39 and 52 Health educator |
12 m | Modified Godin leisure-time exercise questionnaire | IG: 91.7 ± 102.5 to 142.5 ± 122.0 min/week CG: 88.7 ± 99.7 to 118.6 ± 109.1 min/week |
The IG showed higher PA levels than the CG. |
| Lakerveld et al.,2013 [24] | 8/10 | 622 adults at risk for T2DM and CVDs. IG: 314 (178 women), 43.6 ± 5.1 years CG: 308 (185 women), 43.4 ± 5.5 years |
Cognitive behavioural program: six 30-min counselling sessions + three-monthly sessions by phone for one year + health brochures Practice nurses |
12 m | SQUASH questionnaire | Values are median (Q1;Q3) of moderate PA: IG: 56 (19–150) to 52 (21–138) MET min/day CG: 47 (19–120) to 56 (26–126) MET min/day |
No changes in PA |
| Hardcastle et al.,2013 [22] | 7/10 | 334 participants with CVDs risk factors. IG: 203 (n of women n/a), 50.1 ± 0.7 years CG: 131, 50.4 ± 1.0 years |
Standard exercise and nutrition information plus up to five face-to-face motivational interviewing sessions PA specialist, registered dietitian |
Six m | IPAQ | Walking time: IG: 996.1 ± 1116.6 to 1195.54 ± 1277.6 METmin/week CG: 1242.5 ± 1432.7 to 1050.5 ± 1344.4 METmin/week |
The IG significantly increased walking time. |
| Cochrane et al.,2012 [19] | 8/10 | 601 participants with Framingham score ≥20%. IG:236 (32 women), 63.3 ± 6.4 years CG: 365 (36 women), 63.9 ± 6.5 years |
NHS health check service + support for lifestyle change based on the motivational interview/counselling model Lifestyle coach |
Support upto 12 m | General practice PA questionnaire | Mean PA score: IG: 2.07–2.81 CG: 2.65–2.80 |
PA scores improved in both the CG (NHS health check only group) and the IG (NHS health check plus additional lifestyle support) |
| Harris et al., 2012 [20] | 7/10 | 699 participants either aged 56–64 years or 40–55 years with hypertension or dyslipidaemia. IG: 384 (232 women), mean age n/a CG: 315 (169 women) |
Brief lifestyle advice and motivational counselling: one individual session + four 1.5-h sessions over the first three months and a further two follow-up sessions at six and nine months. GP, nurses and practice managers |
Nine m | The brief PA assessment tool | PA score: IG: 3.71, 4.59 and 4.60 CG: 3.38, 3.89 and 4.09 |
PA increased to a greater extent in the IG both at six and nine months |
| Parra-Medina et al., 2011 [8] | 9/10 | 266 women with hypertension or diabetes. IG: 136, mean age n/a CG: 130 |
Theory-based lifestyle intervention targeting PA and dietary fat intake: tailored telephone counselling and tailored newsletters Primary care providers and nurses |
12 m | CHAMPS Questionnaire | Odds ratios (95%CI) of increasing leisure-time moderate-to-vigorous PA: IG: 3.82 (1.41, 10.30) (at 6 months) 1.76 (0.62, 5.0) (at 12 months) |
The IG showed higher total and leisure-time moderate-to-vigorous PA at 6 months but not at 12 months |
| Koelewijn-Van Loon et al., 2009 [23] | 7/10 | 589 patients eligible for cardiovascular risk management. IG: 304 (174 women), 56 ± 10 years CG: 285 (151 women), 58 ± 10 years |
2 face-to-face consultations (15-20 min) + 10 min telephone consultation (or a face-to face consultation) Nurses |
12 w | CHAMPS Questionnaire | Moderate or vigorousintensity PA: IG: 405 ± 343 to 460 ± 362 min/week CG: 447 ± 345 to 449 ± 365 min/week |
No changes in PA |
| Holmen et al.,2014 [28] | 7/10 | 151 Diabetic participants FTA Group: 51 (17 women); 58.6 ± 11.8 years FTA-HC: 50 (25 women); 57.4 ± 12.1 years CG: 50 (20 women); 55.9 ± 12.2 years |
FTA Group: mobile phone with self-management system FTA-HC group: five phone based conversations (20 min) during four months for health counselling with motivational interviewing based on the transtheoretical model. Nurses |
12 m | HeiQ questionnaire | FTA group: 2.78 (2.52, 3.04) to 2.82 (2.60, 3.05) FTA-HC: 2.78 (2.57, 2.99) to 2.81 (2.57, 3.04) CG: 2.71 (2.51, 2.92) to 2.81 (2.58, 3.04) |
No changes in PA |
| Armit et al., 2009 [25] | 6/10 | 136 participants not meeting PA recommendations (82 women). IG (ES): 45 (31 women), mean age n/a IG (ES + P): 45 (27 women) CG: 46 (24 women) |
ES: GP usual care +30 min PA counselling based on the transtheoretical model. ES + P: as for ES group, with goal setting (steps/day) and self-monitoring focusing on a pedometer GP and Exercise scientists |
12 w (24 w follow-up) | Active Australia PA questionnaire | Odds ratios (95% CI) for meeting the National Physical Activity Guidelines IG (ES + P): 2.39 (1.01, 5.64) IG (ES): 1.14 (.47, 2.76) |
PA improved in all groups. At week 24, the ES + P group were more likely to report meeting PA guidelines than the CG |
| Davies et al., 2008 [26] | 7/10 | 824 patients with T2DM. IG: 437 (47 women), 59 years (SD n/a) CG: 387 43 women), 60 years |
Six-hour structured group health education programme focused on lifestyle factors, such as food choices and PA Registered healthcare professionals |
12 m | IPAQ | No IPAQ data is reported. | The IG showed greater increase in PA at four months |
| Wister et al., 2007 [9] | 8/10 | 315 participants with a Framingham score ≥10% IG: 157 (86 women), 55.8 ± 5.5 years CG: 158 (98 women), 55.1 ± 5.2 years |
Report card showing person’s risk profile + telehealth-guided self-care management system at every six months Lifestyle counsellors |
12 m | Five-point ordinal scale | Difference between baseline and one year, mean (95% CI): IG: 0.17 (–0.06–0.40) CG: 0.16 (–0.08–0.40) |
No differences between groups |
| Hardcastle et al., 2008 [21] | 7/10 | 334 participants with CVDs risk factors IG: 203 (n of women n/a), 50.1 ± 0.7 years CG: 131, 50.4 ± 0.9 years |
Patient-centred counselling intervention that incorporated standard exercise and nutrition information + up to five face-to-face motivational interviewing sessions PA specialists, registered dietician |
Six m | IPAQ | Baseline and follow-up changes: IG: 198 ± 63 Met min/week walking CG: –145 ± 109 Met-min/week walking IG: 245 ± 104 Met min/week total PA CG: –122 ± 158 Met min/week total PA |
The IG significantly increased walking and total PA when compared to the CG |
| Elley et al., 2003 [18] | 5/10 | 878 sedentary participants. IG: 451 (301 women), 57.2 ± 10.8 years CG: 427 (281 women), 58.6 ± 11.5 years |
A prompt card, stating the stage of change, + oral and written advice by GP in the consultation + at least three telephone calls (lasting 10–20 min) over the next three months GP and practice nurse |
Three m | Three-month PA recall questionnaire | Mean changes (95% CI): IG: 54.6 (41.4–68.4) min/week CG: 16.8 (6.0–32.4) min/week |
The IG showed greater increase in PA during leisure time and total energy expenditure than the CG |
CAD: coronary artery disease; CG: control group; CHAMPS: community healthy activities model programme for seniors; CVDs: cardiovascular diseases; ES: exercise scientist group; GP: general practitioner; IG: intervention group; IPAQ: international physical activity questionnaire; HeiQ: health education impact questionnaire; n/a: not available; PA: physical activity; P: pedometer; m: months; SD: standard deviation; SQUASH: short questionnaire to assess health enhancing physical activity; T2DM: type 2 diabetes mellitus; w: weeks; FTA: few touch application; FTA HC: few touch application with health counselling.
The studies had a mean methodological quality score of 7.2 out of 10, ranging from 5 to 9 on the PEDro scale (Table 1). Lack of blinding was the most evident methodological flaw in the studies. Failure to conceal allocation was another general methodological limitation.
The 15 studies enrolled a total of 6727 participants; the sample size ranged from 74 to 878 adults [17,18]. Among these studies, seven enrolled adults eligible for CVDs risk assessment or presenting at least one cardiovascular risk factor [16,19–23], one enrolled adults at risk of diabetes or CVDs, two studies encompassed sedentary participants, three included participants with diabetes, or adults with hypertension or diabetes [8], and another study included family members of patients with coronary artery disease [18,24,26–29].
The health education interventions were delivered in several ways, including face-to-face sessions [19–22,26], by telephone [8,9,28], group sessions and a combination of face-to-face, telephone, and group sessions [16–18,23,24–27,29]. The method most used was face-to-face sessions plus telephone. There were differences between the frequency of sessions and the length of the interventions. Interventions varied in length from six hours to 12 months [8,19,24,26–29].
Regarding the methodology used to assess PA, the great majority of studies used a questionnaire. Only one study used an objective measure (accelerometry) together with the Norfolk Physical Activity Questionnaire [27]. The international physical activity questionnaire (IPAQ) and the community healthy activities model programme for seniors (CHAMPS) questionnaire were used in three studies each [8,21,22,23,26]. The other eight studies used different questionnaires (Table 1).
Lifestyle outcomes
Behavioural outcomes included PA, diet, alcohol consumption and smoking status. Significant improvements in the PA levels of the interventional group (IG) compared with the control group (CG) were reported in eight studies (Table 1) [8,18,20–22,25,26,29]. Armit et al. showed an increase in PA at weeks 12 and 24 with no significant group differences; nonetheless, at week 24, the group receiving behaviour change advice plus a pedometer was more likely to report meeting PA guidelines than the CG group [25]. Additionally, three studies found a significant increase in the PA levels of both groups. In these studies, the CG also received an intervention, i.e. they received more than the usual care [19,24,27]. In the Cochrane et al. study the CG received the NHS health check plus the usual general practitioner care [19]; Lakerveld et al. provided the CG with brochures with information and guidelines with regard to healthy PA levels, a healthy diet and, if relevant, smoking cessation [24]; in the study of Griffin et al. the CG received an intensive treatment which included among other features dietary counselling, more frequent contacts with the general practitioner and theory-based education [27]. Only four studies reported a lack of significant effects of the intervention on PA levels [9,17,23,28].
Dietary intake was reported in 10 studies [8,19–24,27–29]. Harris et al. reported a daily enhancement in the number of portions of fruit and vegetable consumed in the IG at six months, but showed no significant differences at 12 months [20]. Koelewijn-Van Loon et al. showed a significantly lower intake of fat in the IG and a significantly higher percentage of participants meeting the recommendations for vegetable intake than in the control group [23]. Hardcastle et al. described a lower fat intake at six and 18 months [22].
Smoking and alcohol consumption were measured in eight studies [16,19,20,23,24,26,27,29]. Only Davies et al. reported a decrease in smoking status in the intervention group at eight and 12 months follow-up compared with the control group [26].
Cardiovascular risk outcomes
All studies used physiological outcomes to assess the effects of the health education interventions. They measured HbA1c [26], fasting blood glucose [20,29], blood pressure [19–22,25,26,29],, lipid profile [19–22,26,29], body mass index [9,19,20,29], waist circumference [9,19,20,29], body weight [19,20,21,22,26], heart score [23,26], Framingham score [9,18,19], and type 2 diabetes mellitus risk score [24].
Davies et al. showed reductions in body weight compared with control groups with a decrease of 3.1% at four months and 3.2% at 12 months [26]. The effects of health education interventions on waist circumference were significant in two studies and not significant in other two studies [9,19,20,29]. In some studies, risk factors, such as high cholesterol levels and blood pressure [19,20,25,29], did not improve during the study period [20,22,23,26,29]. However, other studies showed a significant decreased in blood pressure [9,21,22], total cholesterol and triglycerides after the intervention [9,21,22,26].
Regarding the heart score, Davies et al. reported a greater improvement in the IG in comparison to the CG [26]. Wister et al. also reported a decrease in the Framingham risk score of 3.1% [9] and Cochrane et al. reported a decrease of 2.98% [19].
Discussion
Main findings
Despite the differences between studies in the methods and instruments used to assess PA, the available evidence suggests that health education interventions are successful in the modification of PA levels in primary prevention. Despite the use of different indicators, in several reviewed studies where PA changes were statistically significant, the improvement ranged from 5% to 16% [19,20,22,27,29]. Moreover, another study reported odds for increasing PA in the intervention group of 3.82 [8], while in another study the odds to reach the PA recommendations was 2.39 [25]. Overall, the health education interventions seem to have positive repercussions on cardiovascular risk factors, mainly on lipid profile, blood pressure and cardiovascular risk score.
Strengths and limitations
Most the studies included in this review showed high methodological quality and, with two exceptions [8,25], have conducted an a priori power analysis to determine the sample size. In the majority of the studies, PA was assessed using different questionnaires, which may have limited the observation of the real impact of the interventions. Self-reported PA measures have low sensitivity, high variance, are less accurate, and frequently overestimate the PA levels [30]. Moreover, some of the questionnaires do not stratify PA by intensity levels (light, moderate, vigorous or very vigorous), precluding the analysis of the PA by intensities. Objective data is needed to measure sedentary time and/or the time spent in sedentary behaviours (sitting, TV viewing, time in bed rest) because it has been questioned whether the accomplishment of the recommended amount of daily physical activity time at moderate-to-vigorous intensities is sufficient to overcome long periods of sedentary behaviours, and yet protect the individuals against cardiovascular risk factors [31].
Most studies in this review did not consider the influence of environmental factors such as seasonal changes in daily physical activity. This cannot be disregarded when studying the long-term effects of health education interventions in the modification of PA levels since it was already shown there are significant differences in the amount and patterns of PA between winter and other seasons [32,33].
One limitation of this review is potential publication bias, as it included only articles published in English.
Interpretation
The studies that showed significant changes in PA have adopted face-to-face, at least one session, plus remote interventions and used motivational techniques for behavioural change such as motional interviewing sessions. Interventions incorporating cognitive behavioural strategies, including goal-setting, self-monitoring, face-to-face contacts, feedback and reinforcement are more likely to induce changes [34]. Despite assuming that the PA behaviour of the individuals might be influenced by these intervention characteristics, we cannot assume that this is the most effective delivery method because these common methodological traits were not substantially different from some of the studies not reporting changes in PA after the intervention.
In addition to the improvements in PA, several cardiovascular risk factors and risk score were positively change by the interventions, which make it clinically important. Indeed, even small but sustained lifestyle changes can substantially reduce cardiovascular risk, morbidity and mortality [34].
Implications for further research
In most studies, the sample was mixed gender cohorts. Therefore, future studies should include sub-analysis by gender to ascertain whether between-gender differences exist. They should also include measures of the time spent at different PA intensities, namely at moderate-to-vigorous PA, and sedentary behaviours, because sedentary time has been consistently related to deleterious health outcomes [35]. Environmental factors should be monitored, and PA contexts (occupational, leisure-time physical activity) must be differentiated. Since motivation or self-determination for exercise is an intra-personal correlate or determinant for the behavioural changes [36], future studies should report motivation levels or states of self-determination at baseline and how these features change throughout the interventions. Furthermore, future studies should also report the effect sizes, thereby enabling the appreciation of the magnitude in the differences between groups, and therefore, how effective the interventions are.
Conclusion
The current research provides evidence that health education interventions are successful in the modification of PA levels in primary prevention. The health education interventions seem to have also a positive impact on cardiovascular risk factors, mainly on lipid profile, blood pressure and cardiovascular risk score.
Supplementary Material
Funding Statement
The European Regional Development Fund through the Operational Competitiveness Program, and the Portuguese Foundation for Science and Technology (FCT) supported this study and the research unit CIAFEL within the projects FCOMP-01-0124-FEDER-020180 (Reference FCT: PTDC/DES/122763/2010) and UID/DTP/00617/2013, respectively. iBiMED is a research unit supported by the Portuguese Foundation for Science and Technology (REF: UID/BIM/04501/2013) and FEDER/Compete2020 funds.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Perk J, De Backer G, Gohlke H, et al. . European guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J. 2012;33:1635–1701. [DOI] [PubMed] [Google Scholar]
- 2.Orrow G, Kinmonth AL, Sanderson S, et al. . Effectiveness of physical activity promotion based in primary care: Systematic review and meta-analysis of randomised controlled trials. Br Med J. 2012;344:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foster C, Richards J, Thorogood M, et al. . Remote and web 2.0 interventions for promoting physical activity. Cochrane Database Syst Rev. 2013;9:CD010395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richards J, Thorogood M, Hillsdon M, et al. . Face-to-face versus remote and web 2.0 interventions for promoting physical activity. Cochrane Database Syst Rev. 2013;9:CD010393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Richards J, Hillsdon M, Thorogood M, et al. . Face-to-face interventions for promoting physical activity. Cochrane Database Syst Rev. 2013;9:CD010392. [DOI] [PubMed] [Google Scholar]
- 6.Eriksson KM, Westborg CJ, Eliasson MC.. A randomized trial of lifestyle intervention in primary healthcare for the modification of cardiovascular risk factors. Scand J Public Health. 2006;34:453–461. [DOI] [PubMed] [Google Scholar]
- 7.van Steenkiste B, van der Weijden T, Stoffers HE, et al. . Improving cardiovascular risk management: A randomized, controlled trial on the effect of a decision support tool for patients and physicians. Eur J Cardiovasc Prev Rehabil. 2007;14:44–50. [DOI] [PubMed] [Google Scholar]
- 8.Parra-Medina D, Wilcox S, Salinas J, et al. . Results of the Heart Healthy and Ethnically Relevant Lifestyle trial: a cardiovascular risk reduction intervention for African American women attending community health centers. Am J Public Health. 2011;101:1914–1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wister A, Loewen N, Kennedy-Symonds H, et al. . One-year follow-up of a therapeutic lifestyle intervention targeting cardiovascular disease risk. CMAJ. 2007;177:859–865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eriksson MK, Franks PW, Eliasson M. A 3-year randomized trial of lifestyle intervention for cardiovascular risk reduction in the primary care setting: the Swedish Björknäs study. PLoS One. 2009;4:e5195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization Health education: theoretical concepts, effective strategies and core competencies: a foundation document to guide capacity development of health educators. Cairo: WHO Regional Office for the Eastern Mediterranean; [Internet] 2012. Available from: http://applications.emro.who.int/dsaf/EMRPUB_2012_EN_1362.pdf [cited 2016 Oct 28]. [Google Scholar]
- 12.Buchholz SW, Wilbur J, Ingram D, et al. . Physical activity text messaging interventions in adults: a systematic review. Worldviews Evid Based Nurs. 2013;10:163–173. [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, et al. . Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surg. 2010;8:336–341. [DOI] [PubMed] [Google Scholar]
- 14.Maher CG, Sherrington C, Herbert RD, et al. . Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–721. [PubMed] [Google Scholar]
- 15.Elkins MR, Moseley AM, Sherrington C, et al. . Growth in the Physiotherapy Evidence Database (PEDro) and use of the PEDro scale. Br J Sports Med. 2013;47:188–189. [DOI] [PubMed] [Google Scholar]
- 16.Koelewijn-van Loon MS, van der Weijden T, Ronda G, et al. . Improving lifestyle and risk perception through patient involvement in nurse-led cardiovascular risk management: A cluster-randomized controlled trial in primary care. Prev Med. 2010;50:35–44. [DOI] [PubMed] [Google Scholar]
- 17.Azar KM, Koliwad S, Poon T, et al. . The Electronic CardioMetabolic Program (eCMP) for patients with cardiometabolic risk: A randomized controlled trial. J Med Internet Res. 2016;18:e134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elley CR, Kerse N, Arroll B, et al. . Effectiveness of counselling patients on physical activity in general practice: Cluster randomised controlled trial. Br Med J. 2003;326:793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cochrane T, Davey R, Iqbal Z, et al. . NHS health checks through general practice: Randomised trial of population cardiovascular risk reduction. BMC Public Health. 2012;12:944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harris MF, Fanaian M, Jayasinghe UW, et al. . A cluster randomised controlled trial of vascular risk factor management in general practice. Med J Aust. 2012;197:387–393. [DOI] [PubMed] [Google Scholar]
- 21.Hardcastle S, Taylor A, Bailey M, et al. . A randomised controlled trial on the effectiveness of a primary health care based counselling intervention on physical activity, diet and CHD risk factors. Patient Educ Couns. 2008;70:31–39. [DOI] [PubMed] [Google Scholar]
- 22.Hardcastle SJ, Taylor AH, Bailey MP, et al. . Effectiveness of a motivational interviewing intervention on weight loss, physical activity and cardiovascular disease risk factors: A randomised controlled trial with a 12-month post-intervention follow-up. Int J Behav Nutr Phys Act. 2013;10:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koelewijn-van Loon MS, van der Weijden T, van Steenkiste B, et al. . Involving patients in cardiovascular risk management with nurse-led clinics: A cluster randomized controlled trial. CMAJ. 2009;181:E267–E274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lakerveld J, Bot SD, Chinapaw MJ, et al. . Motivational interviewing and problem solving treatment to reduce type 2 diabetes and cardiovascular disease risk in real life: A randomized controlled trial. Int J Behav Nutr Phys Act. 2013;10:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Armit CM, Brown WJ, Marshall AL, et al. . Randomized trial of three strategies to promote physical activity in general practice. Prev Med. 2009;48:156–163. [DOI] [PubMed] [Google Scholar]
- 26.Davies MJ, Heller S, Skinner TC, et al. . Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. Br Med J. 2008;336:491–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Griffin SJ, Simmons RK, Prevost AT, et al. . Multiple behaviour change intervention and outcomes in recently diagnosed type 2 diabetes: the ADDITION-Plus randomised controlled trial. Diabetologia.2014;57:1308–1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holmen H, Torbjornsen A, Wahl AK, et al. . A mobile health intervention for self-management and lifestyle change for persons with type 2 diabetes, part 2: One-year results from the Norwegian randomized controlled trial RENEWING HEALTH. JMIR Mhealth uHealth. 2014;2:e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reid RD, McDonnell LA, Riley DL, et al. . Effect of an intervention to improve the cardiovascular health of family members of patients with coronary artery disease: A randomized trial. CMAJ. 2014;186:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dyrstad SM, Hansen BH, Holme IM, et al. . Comparison of self-reported versus accelerometer-measured physical activity. Med Sci Sports Exerc. 2014;46:99–106. [DOI] [PubMed] [Google Scholar]
- 31.Garber CE, Blissmer B, Deschenes MR, et al., American College of Sports Medicine position stand . Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359. [DOI] [PubMed] [Google Scholar]
- 32.Buchowski MS, Choi L, Majchrzak KM, et al. . Seasonal changes in amount and patterns of physical activity in women. J Phys Act Health. 2009;6:252–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tucker P, Gilliland J.. The effect of season and weather on physical activity: A systematic review. Public Health. 2007;121:909–922. [DOI] [PubMed] [Google Scholar]
- 34.Artinian NT, Fletcher GF, Mozaffarian D, et al. . Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: A scientific statement from the American Heart Association. Circulation. 2010;122:406–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:S76–S99. [DOI] [PubMed] [Google Scholar]
- 36.Ingledew DK, Markland D.. The role of motives in exercise participation. Psychol Health. 2008;23:807–828. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.