Abstract
Background: Burnout is a growing problem among healthcare professionals and may be mitigated and even prevented by measures designed to promote empathy and resilience.
Objectives: We studied the association between burnout and empathy in primary care practitioners in Lleida, Spain and investigated possible differences according to age, sex, profession, and place of practice (urban versus rural).
Methods: All general practitioners (GPs) and family nurses in the health district of Lleida (population 366 000) were asked by email to anonymously complete the Maslach Burnout Inventory (MBI) and the Jefferson Scale of Physician Empathy (JSPE) between May and July 2014. Tool consistency was evaluated by Cronbach’s α, the association between empathy and burnout by Spearman’s correlation coefficient, and the association between burnout and empathy and sociodemographic variables by the χ2 test.
Results: One hundred and thirty-six GPs and 131 nurses (52.7% response rate) from six urban and 16 rural practices participated (78.3% women); 33.3% of respondents had low empathy, while 3.7% had high burnout. The MBI and JSPE were correlated (P < .001) and low burnout was associated with high empathy (P < .05). Age and sex had no influence on burnout or empathy.
Conclusion: Although burnout was relatively uncommon in our sample, it was associated with low levels of empathy. This finding and our observation of lower empathy levels in rural settings require further investigation.
KEY MESSAGES.
More empathic primary care practitioners have lower burnout scores.
Practitioners working in rural areas have significantly lower levels of empathy than their urban counterparts have.
Interventions designed to foster attributes and skills such as empathy, resilience, and doctor–patient communication may help to reduce and prevent burnout.
Key words: Communication, empathy, primary care, family medicine, professionalism
Introduction
The doctor–patient relationship has undergone dramatic changes in recent years.[1] Increasing access to information, social changes, and patient-centred care has modified the role of practitioners and increased patient autonomy.[2] In response to these changes, the medical community has realized the importance of both increasing awareness among medical students and practitioners of the impact of doctors’ attitudes on clinical outcomes and patient satisfaction and of fostering the acquisition of necessary skills and strategies.[3] Communication skills, resilience, and empathic engagement are all important tools but it should not be forgotten that empathic practitioners are at greater risk of empathic stress (suffer with the suffering of others) and burnout.[4–6]
A study published by the European General Practice Research Network in 2008 reported that burnout was a common problem across Europe and a source of health problems among primary care practitioners.[7,8] Numerous studies have investigated the causes of burnout and proposed mechanisms to reduce this state of emotional, mental, and physical exhaustion,[9] and it has even been argued that burnout prevention should begin during college years.[10] Empathy refers to the ability to understand the experiences and feelings of another person and to communicate this understanding to them.[11] This attribute has been associated, either theoretically or empirically, with some factors such as respect, prosocial behaviour, moral reasoning, positive attitudes towards elderly people, the ability to create a good medical history, increased physician and patient satisfaction, and favourable clinical outcomes.[12] Preliminary reports by Hojat et al. [13] of a positive association between physician empathy and improved clinical outcomes (in their case diabetes control) have subsequently been confirmed in similar studies,[14] including recent work by our group that found a positive association between physician and nurse empathy and improved hypertension control (manuscript submitted for publication).
Fostering skills such as empathy and resilience among practitioners may improve work engagement, doctor–patient communication and satisfaction, and treatment adherence.[15] helping to reduce burnout and ultimately improve patient outcomes.[13,14] In a recent psycho-educational programme undertaken in Barcelona, Spain, a mindfulness intervention was seen to improve empathy and reduce burnout in primary care practitioners.[16]
The association between empathy and burnout has been investigated from numerous approaches and low empathy appears to be associated with high burnout, and in particular with certain components of burnout.[17,18] In 2014, a Canadian team found evidence that cognitive empathy may have a protective role in burnout among primary care practitioners but more studies are needed.[19] In a recent study, our group found high empathy to be significantly associated with low burnout, but we found no link to sick leave prescribing practices.[20]
The aim of this study was to determine the level of empathy and burnout among general practitioners (GPs) and family nurses in a large health district in Lleida, Spain, to investigate the association between these two states.
Methods
Study design and participants
We performed a cross-sectional descriptive study with volunteer participants. In total, 507 GPs and family nurses working in 22 primary care centres in the health district of Lleida, Spain (population of >366 000) were contacted by email and asked to complete an anonymous empathy and burnout survey between May and July 2014; 267 (136 GPs and 131 nurses) agreed to participate (response rate, 52.7%).
Instruments and variables
Burnout was measured using the Spanish version of the Maslach Burnout Inventory, a widely used and validated 22-item scale that measures three domains: emotional exhaustion, depersonalization, and personal accomplishment.[21] Empathy was measured using the validated Spanish version of the Jefferson Scale of Physician Empathy (JSPE),[22] which is also a widely recognized scale, consisting of 20 items.[23] Both scales are rated using a seven-point Likert-type scale, with high scores indicating high burnout and high empathy. The following sociodemographic data were recorded: age, sex, profession (GP, paediatrician, or nurse), and place of practice, i.e., urban (centres located in the capital city) versus rural.
Data analysis
The initial analysis consisted of a descriptive study of the qualitative variables and scores on the MBI and JSPE. The reliability of the instruments was tested by calculating Cronbach α, which was 0.733 for the MBI and 0.748 for the JSPE. The Kolmogorov–Smirnov, Lilliefors and χ2 tests were used to test the normality of distribution of the questionnaire scores and choose the most appropriate correlation coefficient measure (Pearson correlation coefficient for normally distributed data and Spearman rank correlation coefficient for non-normally distributed data).
To analyse the association between sociodemographic variables and JSPE and MBI scores, we grouped the scores into three categories—low, moderate, and high—following a previously described system.[20] All the results were presented with 95% confidence intervals and rural settings were estimated using crude odds ratios. The results’ associations were compared using the χ2 test and effect sizes for differences between urban were disaggregated according to age, sex, profession, and place of practice. For the data analysis, descriptive means of frequency, percentages, and standard deviations were calculated using SPSS version 15.0.
Ethical and confidentiality aspects
The study was approved by the clinical research ethics committee of the Jordi Gol Institute for Research in Primary Care (IDIAP) number P14/034. Maintenance of confidentiality and anonymity of data conformed to the Spanish Data Protection Law 15/1999. All data were coded and accessible only to the primary care information system technician who cross-referenced the data. Because the database was anonymous, at no time could the researchers identify the study participants.
Results
Description of sample
The sample was composed by 136 GPs (50.9% of the sample) and 131 nurses (49.1%) with a median age of 48 years (31–65 years). There were 209 women (73.3%) and 58 men (16.8%). Six of the 22 health centres were urban and 16 were rural.[24] Table 1 summarizes the characteristics of the sample and their scores on the MBI and JSPE.
Table 1.
Description of sample, sociodemographic information, empathy and burnout depending on its place of practice.
| Urban (n = 111) |
Rural (n = 156) |
Crude effect (OR) |
||||
|---|---|---|---|---|---|---|
| n (%) | 95%CI | n (%) | 95%CI | OR (95%CI) | P | |
| Age (years) | ||||||
| 31–40 | 26 (23.4) | (15.5–31.3) | 34 (21.7) | (15.3–28.2) | 1 (ref.) | .915 |
| 41–50 | 40 (36.1) | (27.1–44.9) | 55 (35.2) | (27.7–42.7) | 1.05 (0.552.1) | .880 |
| >50 | 45 (40.5) | (31.4–49.6) | 67 (42.9) | (35.1–50.7) | 1.14 (0.6–2.1) | .689 |
| Profession | ||||||
| Nurse | 50 (45.1) | (35.7–54.3) | 81 (51.9) | (44.1–59.7) | 1 (ref.) | .409 |
| General practitioner | 50 (45.1) | (35.7–54.1) | 65 (41.6) | (33.9–49.4) | 0.8 (0.4–1.3) | .398 |
| Paediatrician | 11 (9.8) | (4.3–15.4) | 10 (6.4) | (2.5–10.2) | 0.56 (0.2–1.4) | .221 |
| Sex | ||||||
| Male | 21 (18.9) | (11.6–26.2) | 37 (23.7) | (17.1–30.3) | 1 (ref.) | .350 |
| Female | 90 (81.1) | (73.7–88.3) | 119 (76.2) | (69.6–82.9) | 0.75 (0.4–1.3) | |
| Empathy (JSPE) | ||||||
| Low | 27 (24.3) | (16.3–32.3) | 62 (39.7) | (32.0–47.4) | 1 (ref.) | .019 |
| Moderate | 38 (34.2) | (25.4–43.1) | 50 (32.1) | (24.7–39.3) | 0.57 (0.3–1.1) | .077 |
| High | 46 (41.4) | (32.2–50.6) | 44 (28.2) | (21.1–35.2) | 0.42 (0.2–0.7) | .005 |
| Burnout (MBI) | ||||||
| Low | 63 (56.7) | (47.5–65.9) | 94 (60.2) | (52.5–67.9) | 1 (ref.) | .776 |
| Moderate | 43 (38.7) | (29.6–47.8) | 57 (36.5) | (28.9–44.1) | 0.89 (0.5–1.4) | .648 |
| High | 5 (4.5) | (0.6–8.3) | 5 (3.2) | (0.4–5.9) | 0.67 (0.1–2.4) | .540 |
The crude effect estimates the effect of the urban/rural location over each variable, the reference group is noted using (ref.).
Burnout and empathy results
According to the overall MBI scores, 157 respondents (58.8%) had low burnout, 100 (37.5%) had moderate burnout, and 10 (3.7%) had high burnout. Eighty-nine respondents (33.3%) had low empathy, 88 (33%) had moderate empathy, and 90 (33.7%) had high empathy (Table 1) A summary of the correlation analysis between empathy and burnout scores and their dimensions is shown in Table 2.
Table 2.
Correlation coefficients for the Jefferson Scale of Empathy and the Maslach Burnout Inventory.
| Spearman correlation (P-value) | Emotional exhaustion | Depersonalization | Personal accomplishment | Empathy (JSPE) |
|---|---|---|---|---|
| Overall burnout score (MBI) | 0.7 (<.001) | 0.6 (<.001) | −0.5 (<.001) | −0.2 (<.001) |
| Emotional exhaustion | 0.4 (<.001) | −0.3 (<.001) | −0.1 (.037) | |
| Depersonalization | −0.4 (<.001) | −0.2 (<.001) | ||
| Personal accomplishment | 0.3 (<.001) |
Empathy and burnout in urban and rural practices
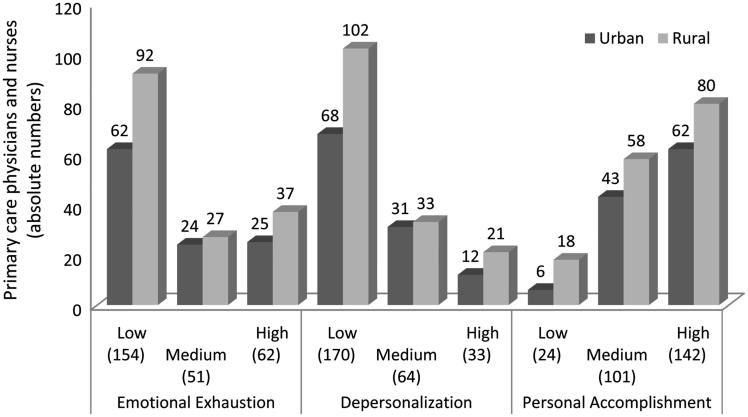
We observed a significant difference for empathy (P = .019) but not burnout levels according to place of work (urban versus rural): high empathy was more common in urban practices (41.4%), while low empathy was more common in rural practices (39.7%). No significant differences were found for age of respondents according to place of work. Figure 1 shows the distribution of burnout scores in the different domains of the MBI according to place of work. Emotional exhaustion and depersonalization scores were both lower in rural areas.
Figure 1.
Distribution of burnout scores according to the different domains of the Maslach Burnout Inventory and place of practice (urban versus rural).
Association between empathy and burnout among nurses and GPs
Table 3 summarizes the relationship between empathy and burnout among nurses. We observed a significant association between high empathy and low burnout (P < .05). Moreover, this association was significant for two of the domains of the MBI: depersonalization and personal accomplishment. Table 4 shows the corresponding results for GPs. In this case, we also found an association between high burnout and low empathy, both overall and for depersonalization and personal accomplishment. The association between empathy and personal accomplishment was particularly significant, at P < .001.
Table 3.
Association between levels of empathy and burnout among family nurses. The negative 95% confidence intervals are due to approximation of the normal distribution of categorical variables and low sample size.
| Low empathy |
Moderate empathy |
High empathy |
|
|||||
|---|---|---|---|---|---|---|---|---|
| n (%) | 95%CI | n (%) | 95%CI | n (%) | 95%CI | n | P-value | |
| Burnout | 131 | .011 | ||||||
| Low | 23 (51.1) | (36.5–65.7) | 32 (71.1) | (57.8–84.3) | 31 (75.6) | (62.4–88.7) | ||
| Moderate | 21 (46.6) | (32.1–61.2) | 13 (28.8) | (15.6–42.1) | 10 (24.3) | (11.2–37.5) | ||
| High | 1 (2.2) | (–2.1–6.5) | 0 (0) | (0–0) | 0 (0) | (0–0) | ||
| Emotional exhaustion | 131 | .221 | ||||||
| Low | 23 (51.1) | (36.5–65.7) | 32 (71.1) | (57.8–84.35) | 27 (65.8) | (51.3–80.3) | ||
| Moderate | 12 (26.6) | (13.7–39.5) | 7 (15.5) | (4.9–26.1) | 7 (17.1) | (5.5–28.5) | ||
| High | 10 (22.2) | (10.1–34.3) | 6 (13.3) | (3.4–23.2) | 7 (17.1) | (5.5–28.5) | ||
| Depersonalization | 131 | .038 | ||||||
| Low | 25 (55.5) | (41.1–70.1) | 32 (71.1) | (57.8–84.3) | 33 (80.4) | (68.3–92.6) | ||
| Moderate | 17 (37.7) | (23.6–51.9) | 10 (22.2) | (10.1–34.3) | 6 (14.6) | (3.8–25.4) | ||
| High | 3 (6.6) | (–0.6–13.9) | 3 (6.6) | (–0.6–13.9) | 2 (4.8) | (–1.7–11.4) | ||
| Personal accomplishment | 131 | <.001 | ||||||
| Low | 5 (11.1) | (1.9–20.2) | 3 (6.6) | (–0.6–13.9) | 1 (2.4) | (–2.2–7.1) | ||
| Moderate | 24 (53.3) | (38.7–67.9) | 14 (31.1) | (17.5–44.6) | 9 (21.9) | (9.2–34.6) | ||
| High | 16 (35.5) | (21.5–49.5) | 28 (62.2) | (48.1–76.3) | 31 (75.6) | (62.4–88.7) | ||
Table 4.
Association between levels of empathy and burnout among general practitioners. The negative 95% confidence intervals are due to approximation of the normal distribution of categorical variables and low sample size.
| Low empathy |
Moderate empathy |
High empathy |
|
|||||
|---|---|---|---|---|---|---|---|---|
| n (%) | 95%CI | n (%) | 95%CI | n (%) | 95%CI | n | P-value | |
| Burnout | 136 | .001 | ||||||
| Low | 15 (34.1) | (20.1–48.1) | 21 (48.8) | (33.9–63.7) | 35 (71.4) | (58.7–84.1) | ||
| Moderate | 25 (56.8) | (42.1–71.5) | 18 (41.8) | (27.1–56.6) | 13 (26.5) | (14.1–38.8) | ||
| High | 4 (9.1) | (0.6–17.5) | 4 (9.3) | (0.6–17.9) | 1 (2) | (–1.9–6) | ||
| Emotional exhaustion | 136 | .061 | ||||||
| Low | 21 (47.7) | (32.9–62.4) | 21 (48.8) | (33.9–63.7) | 30 (61.2) | (47.5–74.8) | ||
| Moderate | 6 (13.6) | (3.5–23.7) | 9 (20.9) | (8.7–33.1) | 10 (20.4) | (9.1–31.6) | ||
| High | 17 (38.6) | (24.2–53.1) | 13 (30.2) | (16.5–43.9) | 9 (18.3) | (7.5–29.2) | ||
| Depersonalization | 136 | .004 | ||||||
| Low | 17 (38.6) | (24.2–53.1) | 26 (60.4) | (45.8–75.1) | 37 (75.5) | (63.4–87.5) | ||
| Moderate | 15 (34.1) | (20.1–48.1) | 12 (27.9) | (14.5–41.3) | 4 (8.1) | (0.5–15.8) | ||
| High | 12 (27.2) | (14.1–40.4) | 5 (11.6) | (2.1–21.2) | 8 (16.3) | (5.9–26.6) | ||
| Personal accomplishment | 136 | <.001 | ||||||
| Low | 10 (22.7) | (10.3–35.1) | 3 (6.9) | (–0.6–14.5) | 2 (4.1) | (–1.4–9.6) | ||
| Moderate | 24 (54.5) | (39.8–69.2) | 21 (48.8) | (33.9–63.7) | 9 (18.3) | (7.5–29.2) | ||
| High | 10 (22.7) | (10.3–35.1) | 19 (44.1) | (29.34–59) | 38 (77.5) | (65.8–89.2) | ||
Discussion
Main findings
High empathy was significantly associated with low burnout in both GPs and nurses in a healthcare district with a registered population of over 366 000. While a third of practitioners had high empathy according to the JSPE, just 3.7% had high burnout scores on the MBI. Professionals working in rural practices were significantly less empathic that their colleagues in urban practices. No differences between empathy and burnout were observed according to age or sex.
Empathy, burnout and health care profession
Our findings add to the international literature on empathy and burnout in the healthcare profession.[7] Burnout is an increasingly recognized problem in this profession, and is a growing risk in countries and regions that have been hit by austerity measures and increasing demands on health services.[25] Stress, which is closely related to burnout, has been identified as the second largest cause of job absenteeism,[26] and high burnout rates of between 12% and 40% have been reported in certain settings.[27] Our observation of relatively low burnout (Table 1) rates in our series is a positive finding, and may be related to the high rates of empathy observed. However, further studies are needed to investigate this association. It should also be noted that burnout rates were considerably higher (23%) in the domain of emotional exhaustion (Table 3).
Empathy, burnout and place of work
Empathy levels were significantly higher in urban practices than in rural practices in our series as is described in Table 1 and Figure 1. This finding should be interpreted within the context of our study setting. Sixteen of the 22 centres analysed were rural, and rural centres in our district typically consist of multiple clinics, at some distance from each other, staffed by GPs and nurses who frequently work at more than one clinic. The lower empathy scores observed for rural GPs and nurses may reflect the fact that these practitioners need to cater on a daily basis to the diverse needs of different patient groups in different locations. This observation of lower empathy among rural practitioners could have important repercussions regarding stimulating research in this area to further clarify these findings and explore the reasons and to seek more evidence to justify the need for more resources in rural settings.
Empathy, burnout and sex
We found no significant differences between men and women for levels of empathy or burnout. Even though there was a predominance of women in all the age groups, our findings show a higher proportion of women in the younger age groups and a lower proportion in the older age groups. Women have been reported as being more empathic than men are,[28] but in our series, the balance observed between sexes is related to the characteristics of our region.
Empathy, burnout and profession
We expected to find higher empathy scores among family nurses than GPs as empathy is typically seen as an essential component of nursing care.[29] However, we did not observe those results. As can be seen in Tables 3 and 4, while we did observe higher rates of low empathy among nurses, the difference with GPs was not significant. We also found no significant differences between GPs and nurses for the level of burnout.
Strengths and limitations
The main limitation of this study is that it is a descriptive study of just a few of the variables that might intervene in the association between burnout and empathy. Future studies should explore additional factors related to personal characteristics, family responsibilities, society, and working environment that could influence both burnout and empathy. It would also be interesting to investigate causal relationships in future studies.
Because our findings are largely based on survey responses, there is also a risk that the participants’ answers might have been affected by response and social desirability bias, particularly in the case of the JSPE, as empathy is considered a ‘socially desirable’ attribute, and this test reflects professional attitudes more than empathy as a global meaning.[30] However, some of this bias will have been offset by our use of widely recognized and validated instruments.
Another limitation of the study is that we were unable to analyse in detail the demographic characteristics of the different centres included due to the anonymous nature of our study.
Our study, however, also has certain strengths. Apart from being the first study in the field to investigate the association between empathy and burnout among GPs and family nurses in a large healthcare district, the main strength of our study is the large sample size, which enhances the reliability of our results and constitutes a positive factor towards continuing to explore the association between empathy, burnout, and clinical outcomes in primary care. We believe that our sample is representative of the primary care practitioners in our health district. The response rate (52.7%) was relatively high for a primary care setting and an almost identical number of GPs and nurses answered the survey.[31] The proportion of female respondents reflects the predominance of women in primary care in our district; in the year of the study, 58% of GPS and 92% of nurses were women
It also adds to the yet limited body of knowledge in this area and provides a reference point for comparison with other regions in Spain and worldwide.
Implications
The relatively low overall levels of burnout and high rates of empathy detected by our study are reassuring, but the higher rates of burnout detected in certain domains of the MBI indicate the need for further investigation, as does the detection of lower empathy among rural practitioners. Moreover, the association observed between high empathy and low burnout adds weight to the theory that interventions aimed at improving empathic engagement and resilience among healthcare practitioners can help to reduce burnout, improve physician and patient satisfaction, and ultimately enhance clinical outcomes. However, a broader view of the mental and emotional health of primary care practitioners, together with the implementation of measures to detect and promote awareness of burnout and to highlight the importance of attributes such as empathy and resilience, should be a priority for health institutions.
Conclusion
Although burnout was relatively uncommon in our sample, it was associated with low levels of empathy. This finding and our observation of lower empathy levels in rural settings requires further investigation.
Acknowledgements
The authors should like to thank all the primary care professionals who participated in this study for their dedication and time.
Declaration of interest
The authors declare no conflict of interest. The authors alone are responsible for the content and writing of the paper.
Funding Statement
Sociedad Española de Medicina Familiar y Comunitaria [3000 €]
References
- 1.Merriel SW, Salisbury C, Metcalfe C, et al. Depth of the patient–doctor relationship and content of general practice consultations: Cross-sectional study. Br J Gen Pract. 2015;65:e545–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ridd M, Shaw A, Lewis G, et al. The patient–doctor relationship: A synthesis of the qualitative literature on patients’ perspectives. Br J Gen Pract. 2009;59:e116–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Esquerda M, Yuguero O, Viñas J, et al. The medical empathy, is it born or is it done? Evolution of the empathy in medical students. Aten Primaria 2016;48:8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chiu C, Feuz MA, McMahan RD, et al. ‘Doctor, make my decisions’: Decision control preferences, advance care planning, and satisfaction with communication among diverse older adults. J Pain Symptom Manage 2016;51:33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lundberg KL. What are internal medicine residents missing? A communication needs assessment of outpatient clinical encounters. Patient Educ Couns. 2014;96:376–380. [DOI] [PubMed] [Google Scholar]
- 6.Tei S, Becker C, Kawada R, et al. Can we predict burnout severity from empathy-related brain activity? Transl Psychiatry. 2014;3:4(e393). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Soler JK, Yaman H, Esteva M, et al. Burnout in European family doctors: The EGPRN study. Fam Pract. 2008;25:245–265. [DOI] [PubMed] [Google Scholar]
- 8.Wurm W, Vogel K, Holl A, et al. Depression-burnout overlap in physicians. PLoS One. 2016. 1;11:e0149913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Decety J, Fotopoulou A.. Why empathy has a beneficial impact on others in medicine: Unifying theories. Front Behav Neurosci. 2015;14:457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boissy A, Windover AK, Bokar D, et al. Communication skills training for physicians improves patient satisfaction. J Gen Intern Med. 2016;31:755–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hojat M, Gonella JS, Nasca TJ, et al. Physician empathy: Definition, components, measurement and relationship to gender and specialty. Am J Psychiatry 2002;159:1563–1569. [DOI] [PubMed] [Google Scholar]
- 12.Kelley JM, Kraft-Todd G, Schapira L, et al. The influence of the patient–clinician relationship on healthcare outcomes: A systematic review and meta-analysis of randomized controlled trials. PLoS One. 2014;9:e94207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hojat M, Louis D, Markham F, et al. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86:359–364. [DOI] [PubMed] [Google Scholar]
- 14.Del Canale S, Louis DZ, Maio V, et al. The relationship between physician empathy and disease complications: An empirical study of primary care physicians and their diabetic patients in Parma, Italy. Acad Med. 2012;87:1243–1249. [DOI] [PubMed] [Google Scholar]
- 15.Derksen F, Bensing J, Lagro-Janssen A.. Effectiveness of empathy in general practice: A systematic review. Br J Gen Pract. 2013;63:e76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Montero-Marin J, Tops M, Manzanera R, et al. Mindfulness, resilience, and burnout subtypes in primary care physicians: The possible mediating role of positive and negative affect. Front Psychol. 2015;6:1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gleichgerrcht E, Decety J.. Empathy in clinical practice: how individual dispositions, gender, and experience moderate empathic concern, burnout, and emotional distress in physicians. PLoS One 2013;8:e61526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brazeau C, Schroeder R, Rovi S, et al. Relationships between medical student burnout, empathy, and professionalism climate. Acad Med. 2010;85:S33–S36. [DOI] [PubMed] [Google Scholar]
- 19.Lamothe M, Boujut E, Zenasni F, et al. To be or not to be empathic: The combined role of empathic concern and perspective taking in understanding burnout in general practice. BMC Fam Pract. 2014;15:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yuguero O, Esquerda M, Marsal JR, et al. Association between sick leave prescribing practices and physician burnout and empathy. PLoS One. 2015;10:e0133379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Álvarez Gallego E, Fernández Ríos L.. [The burnout syndrome or professional burnout]. Rev Asoc Esp Neuropsiq. 2001;21:257–65. Spanish. [Google Scholar]
- 22.Alcorta-Garza A, González-Guerrero JF, Tavitas-Herrera S.. [Validation of Jefferson scale of empathy among Mexican medical students]. Salud Mental. 2005;28:57–63. Spanish. [Google Scholar]
- 23.Hojat M, Gonnella JS, Nasca Tj.. The Jefferson scale of physician empathy: Further psychometric data and differences by gender and speciality at item level. Acad Med. 2002:7:S58–S60. [DOI] [PubMed] [Google Scholar]
- 24.Generalitat de Catalunya. Departament de Salut. Executive memory of the Health Region of Lleida. 2014;12–15. [Google Scholar]
- 25.Heras-Mosteiro J, Legido-Quigley H, Sanz-Barbero B, et al. Health care austerity measures in times of crisis: The perspectives of primary health care physicians in Madrid, Spain. Int J Health Serv. 2016;28pii: 0020731415625251. [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 26.Solberg IB, Tómasson K, Aasland O, et al. Cross-national comparison of job satisfaction in doctors during economic recession. Occup Med (Lond). 2014;64:595–600. [DOI] [PubMed] [Google Scholar]
- 27.Peckam C. Medscape physician lifestyle report 2016: Bias and burnout. [cited 2016 Sept 1] Available from: http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#1. [Google Scholar]
- 28.Moya Albiol L. Empathy (in Spanish). Plataforma Editorial. Valencia 2013. [Google Scholar]
- 29.Moghaddasian S, Lak Dizaji S, Mahmoudi M.. Nurses empathy and family needs in the intensive care units. J Caring Sci. 2013;2:197–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Petek M, Selic P.. Assessing empathic attitudes in medical students: The re-validation of the Jefferson scale of empathy student version report. Zdrav Var. 2015;54:282–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Perreten N, Domínguez-Berjón F, Astray J, et al. Response rates in three opinion surveys performed through online questionnaires in the health setting. Gac Sanit. 2012;26:477–479. [DOI] [PubMed] [Google Scholar]