Abstract
Objectives
Early determination of hospital discharge disposition status at an acute admission is extremely important for stroke management and the eventual outcomes of patients with stroke. We investigated the hospital discharge disposition of patients with stroke residing in Tennessee and developed a predictive tool for clinical adoption. Our investigational aims were to evaluate the association of selected patient characteristics with hospital discharge disposition status and predict such status at the time of an acute stroke admission.
Methods
We analyzed 127,581 records of patients with stroke hospitalized between 2010 and 2014. Logistic regression was used to generate odds ratios and 95% confidence intervals to examine the factor outcome association. An easy-to-use clinical predictive tool was built by using integer-based risk scores derived from coefficients of multivariable logistic regression.
Results
Among the 127,581 records of patients with stroke, 86,114 (67.5%) indicated home discharge and 41,467 (32.5%) corresponded to facility discharge. All considered patient characteristics had significant correlations with hospital discharge disposition status. Patients were at greater odds of being discharged to another facility if they were women; older; black; patients with a subarachnoid or intracerebral hemorrhage; those with the comorbidities of diabetes mellitus, heart disease, hypertension, chronic kidney disease, arrhythmia, or depression; those transferred from another hospital; or patients with Medicare as the primary payer. A predictive tool had a discriminatory capability with area under the curve estimates of 0.737 and 0.724 for derivation and validation cohorts, respectively.
Conclusions
Our investigation revealed that the hospital discharge disposition pattern of patients with stroke in Tennessee was associated with the key patient characteristics of selected demographics, clinical indicators, and insurance status. These analyses resulted in the development of an easy-to-use predictive tool for early determination of hospital discharge disposition status.
Keywords: discharge, prediction, risk score, statistical analysis, stroke management
Stroke is the fifth leading cause of death and a leading cause of long-term disability in the United States, where each year approximately 800,000 people experience a stroke, including 610,000 new and 185,000 recurrent strokes, at a cost of $34 billion.1,2 The state of Tennessee lies in the “Stroke Belt” of the United States and has the highest prevalence of stroke and its corresponding risk factors.3,4 Patients with significant physical, cognitive, and/or behavioral deficits after stroke often are referred for intensive rehabilitation. Early research suggests that the site for postacute stroke care (eg, inpatient rehabilitation facility [IRF], skilled nursing facility [SNF], home with/without home health [HH], or outpatient rehabilitation services) significantly affects 6-month functional outcomes in the domains of basic mobility, activities of daily living, and applied cognition. In a study in northern California, patients who went to an IRF postacute stroke had better functional outcomes than those who received care through an SNF, HH, or outpatient rehabilitation services.5 Yet clinicians and discharge planners continue to grapple with the lack of standardized assessment capable of predicting optimal postacute discharge resource allocation. Furthermore, the rehabilitation needs assessment and the subsequent insurance approval process can take days, thereby resulting in an unnecessary longer hospital stays and potentially exposing patients to hospital-acquired infections. Early determination of hospital discharge disposition, especially at an acute admission, if possible, can optimize acute stroke care at the hospital, help with prognostication, allow sufficient time for patients and their families to prepare for postacute stroke care, and provide sufficient time for finding the appropriate rehabilitation program and obtaining the requisite insurance approval.6 As such, early identification of discharge disposition may be extremely important for stroke management, decision support, and eventual outcomes for patients with stroke.
Although several studies have examined patient characteristics associated with hospital discharge disposition, the results of these studies are inconsistent.7–18 A literature review of 19 articles found that functional dependence, comorbidity, neurocognitive dysfunction, previous living circumstances, and marital status were significantly associated with other than home discharge for patients with stroke.18 The effect of age, sex, race, affected hemisphere, or availability of a caregiver on hospital discharge disposition was inconsistent across studies, however.18 Furthermore, few studies have proposed a discharge disposition predictive model for use in acute patients with stroke. A discharge disposition predictive model after acute stroke using the Taiwan Stroke Registry data with 21,575 patients with stroke was reported but lacked generalizability to populations outside Taiwan and used clinical parameters that may not be available at the time of a patient’s presentation with stroke.14 In the United States, the Northeast Cerebrovascular Consortium piloted a formal rehabilitation needs assessment with discharge referral prediction in the acute hospital setting. They determined that the sociodemographic characteristics, premorbid function, and Barthel Index activities of daily living score for patients with stroke discriminated between discharge home and inpatient rehabilitation (SNF and IRF).19
As such, our goal was to develop and validate a simple predictive tool for determining hospital discharge disposition status using easily available patient characteristics (sex, age, race, stroke type, comorbidity, source of admission, primary payer class, and secondary payer class) at the time of a patient’s presentation with acute stroke symptoms. To meet our goal, we evaluated the association of patient characteristics with hospital discharge disposition status based on the data provided by the Tennessee Department of Health through the Hospital Discharge Data System.
Methods
Study Population
We used data from the Hospital Discharge Data System maintained by the Tennessee Department of Health. The purpose of the Hospital Discharge Data System is to collect and summarize hospital claims data and to analyze and compare charges for similar types of services.20 The dataset included all of the records of hospitalized patients with the principal diagnosis of stroke (International Classification of Diseases, Ninth Revision codes 430, 431, 433, 434, and 436). The dataset contains information on patient demographics, primary and secondary diagnoses, procedures performed, and insurance status.
Variables
We stratified age into three categories: 18 to 64 years, 65 to 74 years, and 75 years and older and stroke types were pooled into three categories: ischemic, subarachnoid hemorrhage, and intracerebral hemorrhage. We included diabetes mellitus, heart disease, hypertension, peripheral arterial disease, chronic kidney disease, hyperlipidemia, arrhythmia, and depression as comorbid conditions. Sources of patient referrals to hospital were grouped into home or a nonhealthcare facility, clinic or physician’s office, or another hospital. Health insurance was categorized into private insurance, Medicaid, Medicare managed, and Medicare fee-for-service. Discharge disposition status was defined as home discharge when patients were discharged home with or without HH care services and as facility discharge when patients were discharged to healthcare facilities such as an SNF, an intermediate care facility, IRF, and another short-term general hospital for inpatient care.20
Statistical Analyses
Demographic and clinical characteristics of patients with stroke with home discharge were first compared with facility discharge counterparts using Pearson χ2. To develop our predictive tool, we divided the whole dataset into a derivation cohort and a validation cohort. The derivation cohort consisted of records of patients with stroke hospitalized from 2010 through 2013 and the validation cohort consisted of records of patients with stroke hospitalized in 2014. Based on the derivation cohort, logistic regression was performed to estimate odds ratios (ORs) of patient characteristics associated with facility discharge. Both unadjusted and adjusted ORs with 95% confidence intervals (CIs) were considered. Next, coefficients from the multivariable logistic regression related to adjusted ORs were used to derive risk scores.21,22 A total risk score was calculated for each patient by adding corresponding risk scores.21,22 Following the logistic function, the predicted probability of facility discharge for each total risk score was given and compared with the observed counterpart. Eventually, an easy-to-use predictive tool was built by using the total risk score to predict the hospital discharge disposition status of each patients with stroke. We assessed the performance of such a predictive tool using the receiver operating characteristic (ROC) curve and the area under a ROC curve (AUC) with 95% CI. All of the statistical analyses were performed using Python version 2.7.12 (Python Software Foundation, Wilmington, DE). The institutional review board of the University of Tennessee at Chattanooga approved this research project.
Results
The original dataset for our investigation included 139,706 records of patients with the principal diagnosis of stroke, hospitalized from 2010 to 2014. We excluded 12,125 records (invalid or missing data: 1151, deceased/expired: 6855, discharged to hospice: 3185, discontinued care/court: 934). Of the remaining 127,581 records, 86,114 (67.5%) were related to home discharge and 41,467 (32.5%) corresponded to facility discharge (Table 1). All of the examined patient characteristics were significantly associated with hospital discharge disposition status (Table 1). The ratios of patients with stroke discharged to a facility compared with home remained stable during the study period (2010: 0.51, 2011: 0.54, 2012: 0.52, 2013: 0.54, 2014: 0.55).
Table 1.
Demographic and clinical characteristics of patients with stroke by hospital discharge disposition status in the complete dataset
| Characteristics | Home discharge, N = 86,114 (%) | Facility discharge, N = 41,467 (%) | P |
|---|---|---|---|
| Sex | <0.0001 | ||
| Male | 43,955 (51.0) | 18,708 (45.1) | |
| Female | 42,159 (49.0) | 22,759 (54.9) | |
| Age, y | <0.0001 | ||
| 18–64 | 36,136 (41.9) | 13,604 (32.8) | |
| 65–74 | 25,673 (29.8) | 9896 (23.9) | |
| ≥75 | 24,305 (28.3) | 17,967 (43.3) | |
| Race | <0.0001 | ||
| White | 71,469 (82.9) | 33,114 (79.9) | |
| Black | 11,533 (13.4) | 7012 (16.9) | |
| Other | 3112 (3.7) | 1341 (3.2) | |
| Stroke type | <0.0001 | ||
| Ischemic | 78,774 (91.5) | 34,143 (82.3) | |
| Subarachnoid hemorrhage | 3184 (3.7) | 2383 (5.8) | |
| Intracerebral hemorrhage | 4156 (4.8) | 4941 (11.9) | |
| Comorbidity | <0.0001 | ||
| Diabetes mellitus | 21,353 (24.8) | 14,357 (34.6) | |
| Heart disease | 30,237 (35.1) | 21,205 (51.1) | |
| Hypertension | 48,877 (56.8) | 32,055 (77.3) | |
| Peripheral arterial disease | 5831 (6.8) | 2120 (5.1) | |
| Chronic kidney disease | 6004 (7.0) | 5322 (12.8) | |
| Hyperlipidemia | 27,892 (32.4) | 15,006 (36.2) | |
| Arrhythmia | 10,150 (11.8) | 10,766 (25.9) | |
| Depression | 4730 (5.5) | 3486 (8.4) | |
| Source of admission | <0.0001 | ||
| Nonhealthcare facility | 56,752 (65.9) | 30,788 (74.2) | |
| Clinic or physician’s office | 19,134 (22.2) | 1696 (4.1) | |
| Transfer from a hospital | 6014 (6.9) | 4544 (10.9) | |
| Other | 4214 (5.0) | 4439 (10.8) | |
| Primary payer class | <0.0001 | ||
| Medicare (not managed) | 40,441 (46.9) | 23,645 (57.0) | |
| Medicare (managed) | 14,172 (16.5) | 6740 (16.3) | |
| Medicaid | 633 (0.7) | 262 (0.6) | |
| Private insurance | 23,021 (26.7) | 7586 (18.3) | |
| Other | 7847 (9.2) | 3234 (7.8) | |
| Secondary payer class | <0.0001 | ||
| Medicare (not managed) | 6327 (7.3) | 3042 (7.3) | |
| Medicare (managed) | 2143 (2.5) | 1162 (2.8) | |
| Medicaid | 5725 (6.6) | 4302 (10.4) | |
| Private insurance | 24,133 (28.0) | 12,379 (29.9) | |
| Other | 47,786 (55.6) | 20,582 (49.6) |
The derivation and validation cohorts included 101,223 and 26,358 records, respectively (size ratio: 3.8:1). Based on both unadjusted and adjusted ORs, patient characteristics such as female sex; ages 75 years and older; black race; a subarachnoid or intracerebral hemorrhage; presence of diabetes mellitus, hypertension, heart disease, chronic kidney disease, arrhythmia, or depression; fee-for-service Medicare; and transfer from an outside hospital were associated with an increased risk of having a facility discharge (Table 2).
Table 2.
ORs of patient characteristics associated with facility discharge for patients with stroke (derivation cohort)
| Characteristics | Unadjusted OR | Adjusted OR | β |
|---|---|---|---|
| Sex | |||
| Male | 1.00 (Ref) | 1.00 (Ref) | 0 |
| Female | 1.27 (1.24–1.30) | 1.15 (1.12–1.19) | 0.1427 |
| Age, y | |||
| 18–64 | 1.00 (Ref) | 1.00 (Ref) | 0 |
| 65–74 | 1.02 (0.98–1.05) | 1.01 (0.96–1.06) | 0.0129 |
| ≥75 | 2.00 (1.94–2.06) | 1.81 (1.72–1.91) | 0.5955 |
| Race | |||
| White | 1.00 (Ref) | 1.00 (Ref) | 0 |
| Black | 1.31 (1.26–1.36) | 1.15 (1.11–1.20) | 0.1440 |
| Other | 0.92 (0.86–0.99) | 0.78 (0.73–0.85) | −0.2428 |
| Stroke type | |||
| Ischemic | 1.00 (Ref) | 1.00 (Ref) | 0 |
| Subarachnoid hemorrhage | 1.72 (1.62–1.83) | 2.34 (2.19–2.50) | 0.850 |
| Intracerebral hemorrhage | 2.78 (2.65–2.92) | 2.91 (2.76–3.07) | 1.068 |
| Comorbidity | |||
| Diabetes mellitus | 1.22 (1.19–1.26) | 1.29 (1.25–1.34) | 0.2563 |
| Heart disease | 1.14 (1.09–1.18) | 1.15 (1.11–1.20) | 0.1433 |
| Hypertension | 2.31 (2.23–2.39) | 1.90 (1.84–1.97) | 0.6438 |
| Peripheral arterial disease | 0.59 (0.55–0.62) | 0.68 (0.63–0.72) | −0.3922 |
| Chronic kidney disease | 1.37 (1.31–1.44) | 1.24 (1.18–1.30) | 0.2127 |
| Hyperlipidemia | 0.77 (0.75–0.79) | 0.83 (0.81–0.86) | −0.1815 |
| Arrhythmia | 2.08 (2.00–2.17) | 1.71 (1.64–1.79) | 0.5373 |
| Depression | 1.38 (1.30–1.45) | 1.35 (1.28–1.43) | 0.3024 |
| Source of admission | |||
| Nonhealthcare facility | 1.00 (Ref) | 1.00 (Ref) | 0 |
| Clinic or physician’s office | 0.16 (0.15–0.17) | 0.20 (0.19–0.21) | −1.6026 |
| Transfer from a hospital | 1.46 (1.39–1.53) | 1.18 (1.13–1.24) | 0.1684 |
| Other | 1.98 (1.89–2.07) | 1.73 (1.65–1.82) | 0.5485 |
| Primary payer class | |||
| Medicare (not managed) | 1.00 (Ref) | 1.00 (Ref) | 0 |
| Medicare (managed) | 0.80 (0.77–0.83) | 0.75 (0.72–0.79) | −0.2883 |
| Medicaid | 0.75 (0.64–0.88) | 0.71 (0.60–0.86) | −0.3362 |
| Private insurance | 0.56 (0.54–0.58) | 0.72 (0.68–0.75) | −0.3351 |
| Other | 0.71 (0.67–0.74) | 0.72 (0.67–0.77) | −0.3275 |
| Secondary payer class | |||
| Medicare (not managed) | 1.00 (Ref) | 1.00 (Ref) | 0 |
| Medicare (managed) | 1.17 (1.07–1.27) | 1.14 (1.04–1.26) | 0.1331 |
| Medicaid | 1.60 (1.50–1.71) | 1.67 (1.55–1.80) | 0.5148 |
| Private insurance | 1.10 (1.04–1.16) | 1.10 (1.04–1.17) | 0.0945 |
| Other | 0.92 (0.88–0.97) | 1.34 (1.26–1.42) | 0.2928 |
OR, odds ratio; ref, reference.
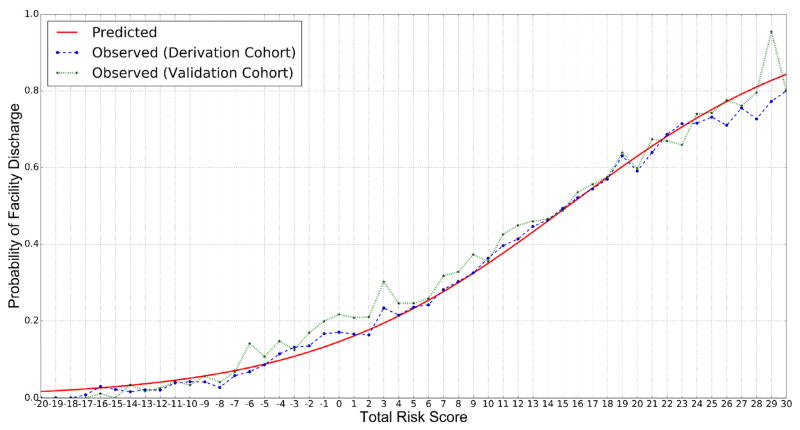
The range of the calculated risk scores for patient characteristics was from −14 to 9 (Table 3). The range of the total risk score for a given patient was from −20 to 39. The predicted probability of facility discharge increased with the total risk score following logistic function (Fig. 1), which means a patient with a higher total risk score had a higher chance of being discharged to a healthcare facility. Because the number of patients with total risk scores of >30 was small, only results corresponding to total risk scores from −20 to 30 were reported. Furthermore, the observed probabilities of facility discharge for both derivation and validation cohorts were consistent with the predicted counterpart (Fig. 1).
Table 3.
Risk scores of patient characteristics associated with facility discharge for stroke patients (the derivation cohort)
| Characteristics | Risk score | Simplified risk score |
|---|---|---|
| Sex | ||
| Male | 0 | 0 |
| Female | 1 | 1 |
| Age, y | ||
| 18–64 | 0 | 0 |
| 65–74 | 0 | 0 |
| ≥75 | 5 | 2 |
| Race | ||
| White | 0 | 0 |
| Black | 1 | 1 |
| Other | −2 | 0 |
| Stroke type | ||
| Ischemic | 0 | 0 |
| Subarachnoid hemorrhage | 7 | 2 |
| Intracerebral hemorrhage | 9 | 2 |
| Comorbidity | ||
| Diabetes mellitus | 2 | 1 |
| Heart disease | 1 | 1 |
| Hypertension | 6 | 2 |
| Peripheral arterial disease | −3 | 0 |
| Chronic kidney disease | 2 | 1 |
| Hyperlipidemia | −2 | 0 |
| Arrhythmia | 5 | 2 |
| Depression | 3 | 1 |
| Source of admission | ||
| Nonhealthcare facility | 0 | — |
| Clinic or physician’s office | −14 | — |
| Transfer from a hospital | 1 | — |
| Other | 5 | — |
| Primary payer class | ||
| Medicare (not managed) | 0 | — |
| Medicare (managed) | −3 | — |
| Medicaid | −3 | — |
| Private insurance | −3 | — |
| Other | −3 | — |
| Secondary payer class | ||
| Medicare (not managed) | 0 | — |
| Medicare (managed) | 1 | — |
| Medicaid | 4 | — |
| Private insurance | 1 | — |
| Other | 3 | — |
Fig. 1.
Predicted and observed probabilities of facility discharge for each total risk score. The predicted probability of facility discharge increased with the total risk score following logistic function. The observed probabilities of facility discharge for both derivation and validation cohorts were consistent with the predicted counterpart.
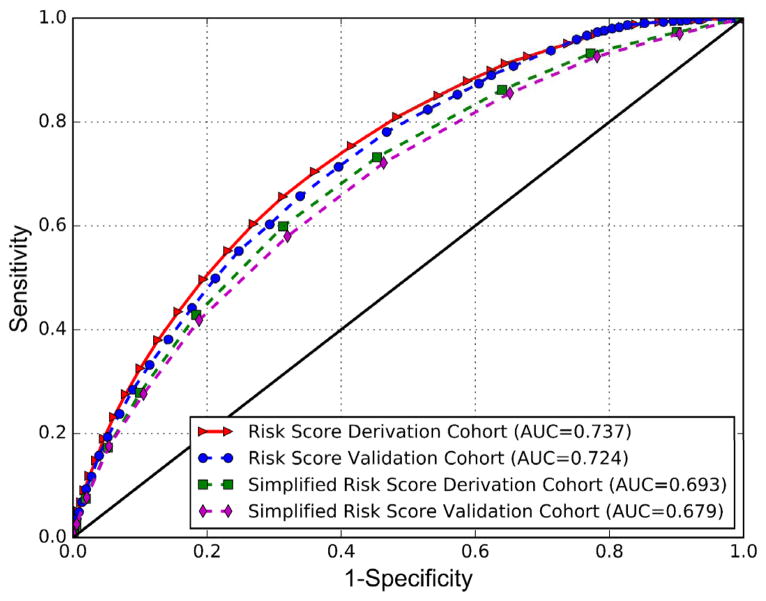
To confirm the usefulness of the easy-to-use predictive tool, ROC curves for both derivation and validation cohorts were plotted (Fig. 2). The corresponding AUCs of the derivation and validation cohorts were 0.737 (95% CI 0.734–0.740) and 0.724 (95% CI 0.718–0.730), respectively. We simplified risk scores further and considered only five patient characteristics (sex, age, race, stroke type, and comorbidity) and exploited only two positive integers (1 or 2) to represent risks (Table 3). When such simplified risk scores were applied, the AUCs of the derivation and validation cohorts were 0.693 (95% CI 0.689–0.696) and 0.679 (95% CI 0.673–0.686), respectively (Fig. 2).
Fig. 2.
Receiver operating characteristic curves of an easy-to-use predictive tool using risk scores or simplified risk scores. This predictive tool had a discriminatory capability to determine hospital discharge disposition status at an acute stroke admission. Risk scores were derived from coefficients of multivariable logistic regression related to adjusted odds ratio. Risk scores were further simplified using only 2 positive integers (1 or 2) to represent risks. AUC, area under the curve.
Discussion
In this study we developed and validated a discharge disposition predictive tool based on integer-based risk scores for patients hospitalized with a principal diagnosis of stroke. This easy-to-use tool had a significant discriminatory capability and used patient characteristics available at the time of a patient’s presentation to a hospital. The hospital discharge disposition results from multiple factors with mixed effects, so risk scores were derived from coefficients of multivariable logistic regression related to an adjusted OR. Based on the adjusted OR, the top five patient characteristics associated with a high risk of facility discharge were identified as an intracerebral hemorrhage, a subarachnoid hemorrhage, hypertension, ages 75 years and older, and arrhythmia.
We identified a strong correlation between hospital discharge disposition and the studied patient characteristics, which aligns with the findings of other investigators. We found that female patients with stroke in Tennessee were more likely than others to be discharged to a facility rather than home.9 A study mentioned that patients’ marital status and sex could play a role in institutionalization.23 One of the reasons that female patients are more likely to be discharged to a facility is that male caregivers are less experienced in providing care to their spouses in comparison with female caregivers. This also aligns with the fact that patients receiving inadequate support from their caregivers often are discharged to a facility or other institutions.24
Older patients also were more likely be discharged to a facility rather than home.9,14,25 In our study the probability of patients with stroke being discharged to a facility increased as their age increased. For example, for the age group of 75 years and older (OR 1.81, 95% CI 1.72–1.91), the probability of being discharged to a facility nearly doubled compared with the age group of younger than 64 years (OR 1.00, Reference). Because it is hard for them to take care of their own health,26 they must rely on systematic and careful management from the facility. Furthermore, as patients with stroke age, their caregivers may have a different condition and may be unable to provide adequate support for them.14
Patients with hemorrhagic stroke also were likely to be discharged to a facility rather than home. Compared with ischemic stroke, hemorrhagic stroke is much more severe because of a higher mortality rate and different medical procedures.27 As such, patients with hemorrhagic stroke need attentive care from institutions.
We also have found that African American/black patients were more likely than patients of other races to be discharged to facilities.9 This finding may be confounded by a lower socioeconomic status such as education, working status, and household income.28
Patients with stroke and diabetes mellitus,14 heart disease,29 hypertension, chronic kidney disease,30 arrhythmia,29 or depression were more likely than others to receive care from a variety of healthcare facilities. Based on the Tennessee hospital discharge data, the prevalence of hypertension among patients with stroke was high and consequentially led to an increased odds for discharge to another facility. This finding reflects the overall higher prevalence of hypertension among Tennessean adults compared with national estimates31,32 and highlights the need for early detection and control of this important risk factor within the state’s adult population.1,4,33 The OR of facility discharge for individuals with poststroke arrhythmia was high, even though the population was small (10,150; OR 1.71, 95% CI 1.64–1.79) compared with other major comorbidities such as diabetes mellitus (21,353; OR 1.29, 95% CI 1.25–1.34), heart diseases (30,237; OR 1.15, 95% CI 1.11–1.20), or hyperlipidemia (27,892; OR 0.83, 95% CI 0.81–0.86). This result suggests the need for further investigation on the correlation between arrhythmia and stroke.
In this article we presented a tool developed with a focus on clinical utility and the rapidity of discharge disposition determination. The predictive tool has important clinical implications because it may serve as a strong first assessment for acute stroke discharge disposition analysis in the acute hospital setting. As discussed in the comparison to two other models reported in the literature,14,34 our tool is simple, can be implemented by a healthcare provider with minimal training, and can provide guidance to care coordinators at the time of admission in preparing for an adequate discharge disposition. Early discharge planning is not only associated with decreased duration of acute hospitalization but also with improved patient-centered outcomes such as decreased readmission rate and duration.35 Furthermore, early patient transition to optimal discharge disposition reduces costs.36 European hospitals are studying early supported poststroke discharge and exploring key patient variables such as premorbid functional status and cognitive function.37 Likewise, our predictive tool can be used for future research to identify patient subsets that can benefit from early discharge to home.37
Our investigation is subject to at least two limitations. First, we did not have information about the functional status of the patients with stroke, subsequent to the stroke. The functional/behavioral measures such as the National Institutes of Health Stroke Scale (NIHSS), the Functional Independence Measure, the Barthel Index, and the Rankin Scale were not available through these hospital discharge data. Having access to any of these measures would have strengthened the final models in our analysis and would have further aided our assessment of stroke severity and its correlation with discharge disposition status.15,18,38 For example, others have shown that the NIHSS score at admission is a potential factor for discharge disposition prediction, in which the corresponding AUC can be as high as 0.84.14 The NIHSS score also has been used for risk adjustment to determine racial and ethnic differences in clinical outcomes.12 Our findings of selected sociodemographic, clinical, and insurance status being strongly associated with the prediction of hospital discharge disposition align well with the studies in which functional/behavioral measures are included, however.
A second limitation is that the Tennessee hospital discharge data did not allow us to differentiate stroke care among patients by primary hospital. This may be an important confounder for our findings because other investigators have shown significant variability in stroke outcomes by hospital facility, where teaching hospitals and certified stroke centers reported better stroke outcomes compared with community hospitals.39
In sum, our investigation of hospital discharge disposition in Tennessee suggests significant benefits and effectiveness in promoting both preclinical research and clinical utilization of stroke management and decision-making support. Proactive intervention, targeted treatment, and personalized care planning for patients with stroke can be enabled with the early determination of hospital discharge disposition at an acute stroke admission. Furthermore, our predictive tool, which is based on simple risk scores, may be an attractive and easily adoptable discharge risk tool for use by physicians or nurses in clinical practice, which may assist with an early discharge disposition prediction and become a standard procedure or health service in stroke management and decision support. Further study is required to determine whether our discharge disposition predictive tool may be expanded to predict discriminatively between SNF and IRF placement options and long-term patient outcomes.
Conclusions
The early determination of hospital discharge disposition status at an acute stroke admission is highly valuable for stroke management and can optimize a stroke system of care. Our study discovered the hospital discharge disposition pattern of patients with stroke in Tennessee and identified the top five patient characteristics associated with a high risk of facility discharge as being an intracerebral hemorrhage, a subarachnoid hemorrhage, hypertension, ages 75 years and older, and arrhythmia. Based on our findings, we developed an easy-to-use predictive tool using the derived integer-based risk scores. This tool can be adopted for an early and rapid determination by physicians or nurses in clinical practice.
Key Points.
Our study revealed the hospital discharge disposition pattern of stroke patients in Tennessee.
An easy-to-use predictive tool was built to determine hospital discharge disposition status of each patient with stroke at an acute stroke admission.
The top five patient characteristics associated with a high risk of facility discharge were identified as an intracerebral hemorrhage, a subarachnoid hemorrhage, hypertension, ages 75 years and older, and arrhythmia.
Acknowledgments
The research reported here was supported by National Institute of Biomedical Imaging and Bioengineering of the National Institutes of Health under award number R15EB015700. The work also was partially funded by the Tennessee Higher Education Commission. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
To purchase a single copy of this article, visit sma.org/smj-home. To purchase larger reprint quantities, please contact reprintsolutions@wolterskluwer.com.
J.S.C., Z.H., N.F., and M.S. have received compensation from the National Institutes of Health and the Tennessee Higher Education Commission. G.W.H. and R.Q. did not report any financial relationships or conflicts of interest.
References
- 1.Clark ML, Gropen T. Advances in the stroke system of care. Curr Treat Options Cardiovasc Med. 2015;17:355. doi: 10.1007/s11936-014-0355-9. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. [Accessed October 12, 2016];Stroke facts. http://www.cdc.gov/stroke/facts.htm.
- 3.Centers for Disease Control and Prevention. [Accessed February 23, 2017];Prevalence of stroke—United States, 2006–2010. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6120a5.htm. Published May 25, 2012.
- 4.East Tennessee State University College of Public Health, the Tennessee Department of Health, and the American Heart/American Stroke Association. [Accessed June 27, 2017];Tennessee stroke registry report. 2014 https://www.etsu.edu/cph/biostat_epidemiology/documents/tsr_report_2014.pdf.
- 5.Chan L, Sandel ME, Jette AM, et al. Does postacute care site matter? A longitudinal study assessing functional recovery after a stroke. Arch Phys Med Rehabil. 2013;94:622–629. doi: 10.1016/j.apmr.2012.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luker JA, Bernhardt J, Grimmer KA, et al. A qualitative exploration of discharge destination as an outcome or a driver of acute stroke care. BMC Health Serv Res. 2014;14:193. doi: 10.1186/1472-6963-14-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen TA, Page A, Aggarwal A, et al. Social determinants of discharge destination for patients after stroke with low admission FIM instrument scores. Arch Phys Med Rehabil. 2007;88:740–744. doi: 10.1016/j.apmr.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 8.Kind AJ, Smith MA, Liou JI, et al. Discharge destination’s effect on bounce-back risk in black, white, and Hispanic acute ischemic stroke patients. Arch Phys Med Rehabil. 2010;91:189–195. doi: 10.1016/j.apmr.2009.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Freburger JK, Holmes GM, Ku LJ, et al. Disparities in postacute rehabilitation care for stroke: an analysis of the state inpatient databases. Arch Phys Med Rehabil. 2011;92:1220–1229. doi: 10.1016/j.apmr.2011.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bejot Y, Troisgros O, Gremeaux V, et al. Poststroke disposition and associated factors in a population-based study: the Dijon Stroke Registry. Stroke. 2012;43:2071–2077. doi: 10.1161/STROKEAHA.112.658724. [DOI] [PubMed] [Google Scholar]
- 11.Jaja BN, Saposnik G, Nisenbaum R, et al. Racial/ethnic differences in inpatient mortality and use of institutional postacute care following subarachnoid hemorrhage. J Neurosurg. 2013;119:1627–1632. doi: 10.3171/2013.7.JNS13544. [DOI] [PubMed] [Google Scholar]
- 12.Xian Y, Holloway RG, Smith EE, et al. Racial/ethnic differences in process of care and outcomes among patients hospitalized with intracerebral hemorrhage. Stroke. 2014;45:3243–3250. doi: 10.1161/STROKEAHA.114.005620. [DOI] [PubMed] [Google Scholar]
- 13.Van der Cruyssen K, Vereeck L, Saeys W, et al. Prognostic factors for discharge destination after acute stroke: a comprehensive literature review. Disabil Rehabil. 2015;37:1214–1227. doi: 10.3109/09638288.2014.961655. [DOI] [PubMed] [Google Scholar]
- 14.Tseng HP, Lin FJ, Chen PT, et al. Derivation and validation of a discharge disposition predicting model after acute stroke. J Stroke Cerebrovasc Dis. 2015;24:1179–1186. doi: 10.1016/j.jstrokecerebrovasdis.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 15.Nguyen VQ, PrvuBettger J, Guerrier T, et al. Factors associated with discharge to home versus discharge to institutional care after inpatient stroke rehabilitation. Arch Phys Med Rehabil. 2015;96:1297–1303. doi: 10.1016/j.apmr.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 16.Bell CL, LaCroix AZ, Desai M, et al. Factors associated with nursing home admission after stroke in older women. J Stroke Cerebrovasc Dis. 2015;24:2329–2337. doi: 10.1016/j.jstrokecerebrovasdis.2015.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dutrieux RD, van Eijk M, van Mierlo ML, et al. Discharge home after acute stroke: differences between older and younger patients. J Rehabil Med. 2016;48:14–18. doi: 10.2340/16501977-2045. [DOI] [PubMed] [Google Scholar]
- 18.Mees M, Klein J, Yperzeele L, et al. Predicting discharge destination after stroke: a systematic review. Clin Neurol Neurosurg. 2016;142:15–21. doi: 10.1016/j.clineuro.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 19.Stein J, Bettger JP, Sicklick A, et al. Use of a standardized assessment to predict rehabilitation care after acute stroke. Arch Phys Med Rehabil. 2015;96:210–217. doi: 10.1016/j.apmr.2014.07.403. [DOI] [PubMed] [Google Scholar]
- 20.Hospital Discharge Data System User Manual. Chattanooga: Tennessee Department of Health; 2011. [Google Scholar]
- 21.Sullivan LM, Massaro JM, D’Agostino RB. Presentation of multivariate data for clinical use: the Framingham Study risk score functions. Stat Med. 2004;23:1631–1660. doi: 10.1002/sim.1742. [DOI] [PubMed] [Google Scholar]
- 22.Wu C, Hannan EL, Walford G, et al. A risk score to predict in-hospital mortality for percutaneous coronary interventions. J Am Coll Cardiol. 2006;47:654–660. doi: 10.1016/j.jacc.2005.09.071. [DOI] [PubMed] [Google Scholar]
- 23.Kelly-Hayes M, Wolf P, Kannel W, et al. Factors influencing survival and need for institutionalization following stroke: the Framingham Study. Arch Phys Med Rehabil. 1988;69:415–418. [PubMed] [Google Scholar]
- 24.de Pablo P, Losina E, Phillips CB, et al. Determinants of discharge destination following elective total hip replacement. Arthritis Rheum. 2004;51:1009–1017. doi: 10.1002/art.20818. [DOI] [PubMed] [Google Scholar]
- 25.Osborne J, Langefeld CD, Moomaw CJ, et al. Abstract ns20: discharge disposition after intracerebral hemorrhage. Stroke. 2015;46:ANS20. [Google Scholar]
- 26.Wang SY, Zhao Y, Zang XY. Continuing care for older patients during the transitional period. Chin Nurs Res. 2014;1:5–13. [Google Scholar]
- 27.Andersen KK, Olsen TS, Dehlendorff C, et al. Hemorrhagic and ischemic strokes compared: stroke severity, mortality, and risk factors. Stroke. 2009;40:2068–2072. doi: 10.1161/STROKEAHA.108.540112. [DOI] [PubMed] [Google Scholar]
- 28.Bettger JP, Zhao X, Bushnell C, et al. The association between socioeconomic status and disability after stroke: findings from the Adherence eValuation After Ischemic stroke Longitudinal (AVAIL) registry. BMC Public Health. 2014;14:281. doi: 10.1186/1471-2458-14-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stineman MG, Kwong PL, Bates BE, et al. Development and validation of a discharge planning index for achieving home discharge after hospitalization for acute stroke among those who received rehabilitation services. Am J Phys Med Rehabil. 2014;93:217–230. doi: 10.1097/PHM.0b013e3182a92bfb. [DOI] [PubMed] [Google Scholar]
- 30.El Husseini N, Fonarow GC, Smith EE, et al. Renal dysfunction is associated with poststroke discharge disposition and in-hospital mortality: findings from Get With The Guidelines-Stroke. Stroke. 2017;48:327–334. doi: 10.1161/STROKEAHA.116.014601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tennessee Department of Health. [Accessed February 23, 2017];High blood pressure facts. https://www.tn.gov/assets/entities/health/attachments/HBP.pdf.
- 32.Centers for Disease Control and Prevention. [Accessed February 23, 2017];Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. https://www.cdc.gov/nchs/products/databriefs/db133.htm. Published October 2013.
- 33.Centers for Disease Control and Prevention. [Accessed June 27, 2017];Vital signs: avoidable deaths from heart disease, stroke, and hypertensive disease-United States, 2001–2010. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6235a4.htm. Published September 6, 2013.
- 34.Ouellette DS, Timple C, Kaplan SE, et al. Predicting discharge destination with admission outcome scores in stroke patients. NeuroRehabilitation. 2015;37:173–179. doi: 10.3233/NRE-151250. [DOI] [PubMed] [Google Scholar]
- 35.Fox MT, Persaud M, Maimets I, et al. Effectiveness of early discharge planning in acutely ill or injured hospitalized older adults: a systematic review and meta-analysis. BMC Geriatr. 2013;13:70. doi: 10.1186/1471-2318-13-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beech R, Rudd AG, Tilling K, et al. Economic consequences of early inpatient discharge to community-based rehabilitation for stroke in an inner-London teaching hospital. Stroke. 1999;30:729–735. doi: 10.1161/01.str.30.4.729. [DOI] [PubMed] [Google Scholar]
- 37.Mas MÀ, Inzitari M. A critical review of Early Supported Discharge for stroke patients: from evidence to implementation into practice. Int J Stroke. 2015;10:7–12. doi: 10.1111/j.1747-4949.2012.00950.x. [DOI] [PubMed] [Google Scholar]
- 38.Meyer MJ, Pereira S, McClure A, et al. A systematic review of studies reporting multivariable models to predict functional outcomes after post-stroke inpatient rehabilitation. Disabil Rehabil. 2015;37:1316–1323. doi: 10.3109/09638288.2014.963706. [DOI] [PubMed] [Google Scholar]
- 39.Bettger JP, Thomas L, Liang L, et al. Hospital variation in functional recovery after stroke. Circ Cardiovasc Qual Outcomes. 2017;10(1) doi: 10.1161/CIRCOUTCOMES.115.002391. pii: e002391. [DOI] [PubMed] [Google Scholar]