Abstract
Objective
To examine the association between changes in waist-hip ratio (WHR), a measure of abdominal obesity, and age-related macular degeneration (AMD).
Methods
A total of 12 515 persons from a population-based cohort study, aged 45 to 64 years in 1987 to 1989, were followed up over 6 years. The percentage change in WHR during follow-up was ranked into sex-specific deciles; an increase in WHR was defined as the top 10% of change and a decrease in WHR as the bottom 10%. The association of increased or decreased WHR and presence of AMD at follow-up was determined using logistic regression adjusting for potential confounders.
Results
The average change in WHR was an increase of 2%, ranging from a decrease of 44% to an increase of 102%. A decrease in WHR of 3% or more was associated with 29% lower odds of any AMD (odds ratio = 0.71; 95% confidence interval, 0.52–0.97). This effect was most pronounced among obese participants at baseline, where a decrease in WHR was associated with 59% lower odds of AMD (odds ratio = 0.41; 95% confidence interval, 0.20–0.82).
Conclusions
Middle-aged persons who had a 3% or greater reduction in WHR over time were less likely to have AMD, particularly among those who were initially obese.
Age-related macular degeneration (AMD) is the leading cause of visual impairment among elderly persons. Despite advances in research, few modifiable risk factors for AMD have been identified. Although clear associations have been shown with smoking, associations with hypertension, cardiovascular disease, dyslipidemia, and dietary fat intake have not been consistent.1–4
The relationship between obesity and AMD has been the subject of several studies (Table 1), including cross-sectional and case-control studies5–7,15 and more recently longitudinal studies.8,9,11,12,14 Most of these have examined AMD associations with overweight and obesity defined by the body mass index (BMI) (calculated as weight in kilograms divided by height in meters squared).5,11 Some studies investigating the relationship between BMI and incident AMD have found no association9,13,16 or have found associations solely within specific population subgroups such as women.10
Table 1.
Summary of Studies on Body Mass Index, Waist-Hip Ratio, and Age-Related Macular Degeneration
| Study Population | Type of Study | Participants, No. (Age, y) |
Definition of BMI or WHR |
AMD Definition | Main Findings |
|---|---|---|---|---|---|
| Blue Mountains Eye Study, Australia5 | Population based, cross-sectional | 3654 (≥49) | Overweight: BMI ≥25 and <30; obesity: BMI ≥30 | Early and late AMD | OR=1.78 for early AMD and obesity |
| Age-Related Eye Disease Study6 | Clinic based, cross-sectional | 4519 | Increasing BMI | Neovascular AMD and central geographic atrophy | Increased BMI associated with increase in neovascular AMD |
| POLA study, ages 60–95y7 | Population based, cross-sectional | 2584 (60–95) | Obesity: BMI ≥30 | Soft drusen, late AMD, pigmentary abnormalities | OR=2.29 for late AMD and obesity |
| Beaver Dam Eye Study, United States8–10 | Population based, cross-sectional, and prospective cohort | 3722 (43–86) | Continuous BMI and WHR | Early and late AMD | BMI and WHR associated with increased early AMD in women in cross-sectional study; no relation of BMI to incident early or late AMD |
| Physicians’ Health Study, United States11 | Prospective cohort study of incidence | 21121 | Overweight: BMI ≥25 and <30; obesity: BMI ≥30 | Dry or neovascular AMD | RR=2.15 for dry AMD and obesity |
| Hospital-based retinal practice, United States12 | Longitudinal study of progression | 261 (≥60) | Overweight: BMI ≥25 and <30; obesity: BMI ≥30, WHR | Geographic atrophy and neovascular disease (combined) | BMI: RR=2.32 for overweight, RR=2.35 for obesity; WHR: RR=1.84 for highest tertilevs lowest tertile |
| Pooled data from 3 studies in Australia, United States, and Europe13 | Prospective cohort | 9523 (43–95) | Overweight: BMI ≥25 and <30; obesity: BMI ≥30 | Late AMD | No association |
| Clinical cohort with early or intermediate AMD, United States14 | Longitudinal study of incidence | 2506 | Obesity: BMI ≥30 | Neovascular AMD or central geographic atrophy | OR=1.93 for obesity and central geographic atrophy |
| Lithuania15 | Population based, case-control | 1403 (35–64) | Overweight: BMI ≥25 and <30; obesity: BMI ≥30 | AMD | AMD was associated with increased BMI in men |
| Israel16 | Population based, case-control | 130 (56–77) | Overweight: BMI ≥25 and <30; obesity: BMI ≥30 | No association |
Abbreviations: AMD, age-related macular degeneration; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); OR, odds ratio; POLA, Pathologies Oculaires Liées à l’Age; RR, relative risk; WHR, waist-hip ratio.
The waist-hip ratio (WHR) is a measure of central or abdominal obesity. There is now increasing evidence that WHR is a better predictor of diabetes and cardiovascular diseases than BMI.17 However, only 2 studies have investigated relationships between WHR and AMD,10,12 with one of them showing stronger relationships between WHR and AMD than between BMI and AMD.
To our knowledge, there has been no analysis of the association between changes in WHR, BMI, or weight with the presence of AMD to date. In the current study, we use longitudinal data from the Atherosclerosis Risk in Communities Study to examine the relationship between changes in WHR during a 6-year period and presence of AMD at the end of the 6-year period. Our hypothesis is that WHR, a measure of central obesity, and changes in WHR over time are associated with the prevalence of AMD.
METHODS
STUDY POPULATION
The Atherosclerosis Risk in Communities Study is a population-based cohort study that included 15 792 women and men aged 45 to 64 years at baseline in 1987 to 1989.18 Population samples were selected from 4 US communities. Of those examined at baseline, 86% of the survivors returned for the third examination 6 years after the baseline examination (1993–1995).
Our study population comprised persons who returned to the third examination, when retinal photography was first performed.4,19,20 Of the 12 887 who returned for this examination, we excluded 271 with no retinal photographs or with ungradable photographs, 30 without measurements of weight, height, waist circumference, or hip circumference, and, owing to small numbers, 38 whose race was neither black nor white and 42 black residents in Minneapolis, Minnesota, and Maryland, leaving 12 506 who provided data for this study. Characteristics of participants with and without gradable retinal photographs have been previously reported.19
Institutional review boards at each study site and at the Fundus Photograph Reading Center, University of Wisconsin, Madison, approved the study. Informed consent was obtained from all of the participants, and the study was conducted in accordance with the Declaration of Helsinki.
WHR, BMI, AND WAIST CIRCUMFERENCE
Waist and hip circumferences were determined by horizontal measurement of the maximum girth at the umbilicus and over the buttocks, respectively.
To analyze the relationship between change in WHR from baseline and the third examination and AMD at the third examination, we defined change in 2 ways: absolute and relative. Absolute change (in centimeters) was defined as the difference between WHR at baseline and WHR at the third examination. Relative change was defined as the percentage change in WHR between baseline and the third examination. For categorical comparisons, we wanted categories of decreased and increased WHR to contain a change of at least 3% based on current ideas of clinical significance.21 We divided change in WHR into sex-specific deciles; decreased WHR was defined for primary analyses as the bottom decile of percentage change (including change of −3% to −44%), increased WHR was defined as the top decile of percentage change (including change of 6% to 102%), and stable WHR was defined as the intermediate 8 deciles. Change in waist circumference was similarly defined.
Height and weight circumferences were measured with participants in scrub suits. For analysis by weight group, the population was divided into normal weight (BMI ≥18.5 and <25), overweight (BMI ≥25 and <30), and obese (BMI ≥30) groups.22 Owing to their small numbers (88 individuals), those with BMI less than 18.5 were not included in the analyses stratified by weight group. We defined changes in BMI in the same way as WHR.
RETINAL PHOTOGRAPHY AND AGE-RELATED MACULAR DEGENERATION
The retinal photography procedure and the assessment of AMD have been previously reported.4,20,23 Briefly, a 45° nonmydriatic retinal photograph centered on the region of the optic disc and the macula of 1 randomly selected eye of each participant was taken following 5 minutes of dark adaptation. Graders masked to subject identity evaluated the photographs at the University of Wisconsin, Madison, using a modification of the Wisconsin AMD grading system.24 The presence of soft drusen, retinal pigment epithelial depigmentation, increased retinal pigment, pure geographic atrophy, and signs of exudative macular degeneration were determined in the macular area circumscribed by the outermost circle of the grading grid.
Soft drusen were defined as those having a diameter larger than 63 µm. Retinal pigment epithelial depigmentation and increased retinal pigment associated with AMD (the presence of granules or clumps of gray or black pigment in or beneath the retina) were defined as present or absent/questionable. Early AMD was defined as the presence of soft drusen alone, retinal pigment epithelial depigmentation alone, or a combination of soft drusen with increased retinal pigment and/or retinal pigment epithelial depigmentation in the absence of late AMD. Late AMD was defined as the presence of signs of exudative AMD or pure geographic atrophy. Any AMD was defined as the presence of either early or late AMD.
Quality-control procedures were based on repeated assessment of photographs for 520 participants.19 In general, weighted κ of signs of AMD ranged from 0.67 to 0.81 for intragrader comparisons and 0.55 to 0.92 for intergrader comparisons.
OTHER RISK FACTORS
Participants were evaluated for cardiovascular risk factors at each examination.25 Patients were defined as having preexisting coronary heart disease if they had a history of acute myocardial infarction, silent infarction, or coronary revascularization procedures at baseline. Blood pressure was taken according to a standardized protocol with a random-zero sphygmomanometer, and the mean of the last 2 measurements was used.25 Blood was drawn after the patient had fasted overnight and processing was performed for total cholesterol, low-density lipoprotein cholesterol, triglycerides, glucose, and fibrinogen levels and white blood cell count as described elsewhere.25,26 Diabetes mellitus was defined as a fasting glucose level of 126 mg/dL or higher (to convert to millimoles per liter, multiply by 0.0555), a nonfasting glucose level of 200 mg/dL or higher, or a self-reported history of or treatment for diabetes. Education and cigarette smoking were ascertained from interview. Education was divided into basic (<12 years), intermediate (12–16 years), or advanced (17–21 years) levels. Participants were categorized as current, former, and never smokers, and years of smoking cigarettes were also recorded. Physical activity was characterized by sports and leisure activity indexes (scores within each index ranging from 0–5) described elsewhere.27,28
STATISTICAL ANALYSES
The crude distribution of potential confounders across categories of change in WHR was determined by analysis of variance. To analyze the cross-sectional relationship between WHR and AMD, logistic regression was performed on AMD at examination 3 using standardized values of WHR measured at examination 3 and confounders measured at examination 3. All of the analyses were adjusted for sex, age (continuously), race, and study center. A second set of models was additionally adjusted for smoking status, blood glucose level, systolic blood pressure, serum total cholesterol level, the presence of coronary heart disease or diabetes, physical activity level, fibrinogen level, and white blood cell count measured at baseline.
To analyze the relationship between change in WHR, BMI, or waist circumference between baseline and the third examination and AMD at the third examination, we used sex-specific deciles of relative change as described earlier. The association between change in weight and AMD was analyzed using logistic regression with the stable weight group (deciles 2–9) as the reference group and presence or absence of AMD at the third examination as the outcome.
All of the analyses were adjusted for sex, age, race, and study center. A second set of models was additionally adjusted for baseline WHR, BMI, or waist circumference in the analyses of change in WHR, BMI, or waist circumference, respectively. A third set of models was also adjusted for baseline BMI or WHR, smoking status, years of cigarette smoking, change in smoking status during follow-up, serum glucose level, systolic blood pressure, serum total cholesterol level, the presence of coronary heart disease or diabetes, physical activity level, fibrinogen level, and white blood cell count, all measured at baseline. If one of the variables was used for stratification, it was no longer included in the model. Subgroup analyses were performed after stratifying by sex, age group, weight group, diabetes status, smoking status, and race. Interaction terms for each of the stratification variables with change in WHR were also tested in the logistic regression models. All of the analyses were performed using Stata/SE version 8.0 statistical software (Stata Corp, College Station, Texas).
RESULTS
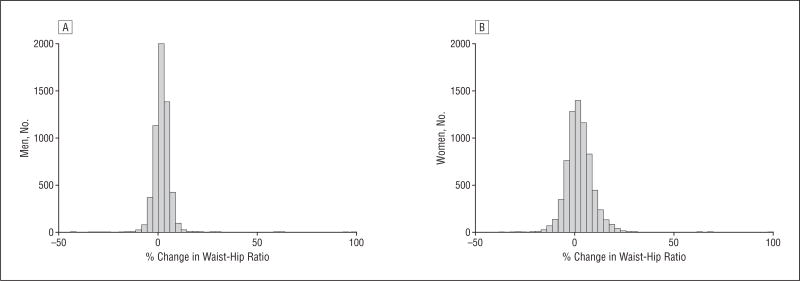
Between baseline and the third examination, the average change in WHR was an increase of 1% for men and 3% for women, ranging from a decrease of 44% to an increase of just more than 100% (Figure). Those whose WHRs decreased, increased, or remained stable differed according to race, education, baseline WHR, obesity prevalence, baseline coronary heart disease, diabetes prevalence, and baseline cardiovascular disease risk factors (Table 2). In general, the group with decreasing WHR had the highest baseline levels of cardiovascular risk factors, including BMI and WHR.
Figure.
Distribution of percentage change in waist-hip ratio between baseline and the third examination for men (A) and women (B).
Table 2.
Baseline Characteristics of Participants With Decreased, Increased, or Stable Waist-Hip Ratio Over 6 Years
| Change in WHR Over 6 ya | |||
|---|---|---|---|
|
|
|||
| Characteristic | Decrease (n=1250)b |
Stable (n=10 004) |
Increase (n=1252)b |
| Age, mean (SD), yc | 54.9 (5.8) | 54.0 (5.7) | 53.4 (5.8) |
| Male, % | 44.5 | 44.5 | 44.5 |
| African American, %c | 21.9 | 21.7 | 28.6 |
| High school education, %c | 77.2 | 80.4 | 80.4 |
| Current smoker, % | 19.2 | 17.4 | 18.8 |
| Prevalent coronary heart disease, % | 5.1 | 4.0 | 3.9 |
| Prevalent diabetes, %c | 19.6 | 15.0 | 11.8 |
| Serum glucose level, mean (SD), mg/dLc | 110.7 (41.8) | 106.1 (33.2) | 102.7 (31.5) |
| Systolic blood pressure, mean (SD), mm Hgc | 122.1 (18.7) | 119.8 (17.6) | 118.4 (16.7) |
| Diastolic blood pressure, mean (SD), mm Hg | 73.4 (11.3) | 73.3 (10.7) | 73.0 (10.6) |
| Total cholesterol level, mean (SD), mg/dLc | 216.8 (40.6) | 215.1 (41.3) | 209.5 (40.0) |
| Triglycerides level, mean (SD), mg/dLc | 141.7 (104.4) | 131.1 (86.6) | 113.0 (68.4) |
| Fibrinogen level, mean (SD), mg/dLc | 306.0 (65.7) | 298.5 (61.8) | 294.0 (62.1) |
| White blood cell count, mean (SD), cells/µLc | 6.2 (2.1) | 6.0 (1.8) | 6.1 (2.0) |
| WHR, mean (SD)c | 0.97 (0.08) | 0.93 (0.07) | 0.86 (0.08) |
| Obesity, %c,d | 33.1 | 26.5 | 18.9 |
| Percentage WHR change, mean (SD)c | −6.6 (3.7) | 1.9 (3.2) | 11.8 (7.0) |
Abbreviation: WHR, waist-hip ratio.
SI conversion factors: To convert glucose to millimoles per liter, multiply by 0.0555. To convert total cholesterol to millimoles per liter, multiply by 0.0259. To convert triglycerides to millimoles per liter, multiply by 0.0113. To convert fibrinogen to micromoles per liter, multiply by 0.0294. To convert white blood cell count to ×109/L, multiply by 0.001.
From baseline to the third examination.
Decrease and increase in WHR are defined as the bottom and top sex-specific deciles, respectively, of percentage change in WHR over the 6-year follow-up.
Indicates significant differences between categories by analysis of variance, P<.05.
Indicates body mass index (calculated as weight in kilograms divided by height in meters squared) of 30 or higher.
There was a positive cross-sectional relationship between WHR at examination 3 and presence of AMD at examination 3 (Table 3). After full multivariate adjustment, the increased odds of any AMD associated with a 1-SD increase in WHR was 14% (95% confidence interval [CI], 1.02–1.27). An association was seen with all forms of AMD analyzed. There was no association between BMI at examination 3 and presence of AMD (odds ratio [OR] = 1.02 per 1-SD increase; 95% CI, 0.92–1.12).
Table 3.
Cross-sectional Association of Waist-Hip Ratio and Age-Related Macular Degeneration at the Third Examination
| OR (95% CI) of AMD, Per 1-SD Change in WHR at Third Examination |
||||
|---|---|---|---|---|
|
|
||||
| AMD Subtype | Participants, No. |
Participants at Risk, No. |
Adjusted for Age, Sex, Race, and Centera |
Multivariate-Adjustedb |
| Any AMD | 608 | 12 506 | 1.09 (1.00–1.20) | 1.14 (1.02–1.27) |
| Early AMD | 591 | 12 506 | 1.08 (0.99–1.19) | 1.11 (1.00–1.24) |
| Late AMD | 17 | 12 506 | 1.37 (1.00–1.90) | 1.36 (1.02–1.83) |
| Soft drusen | 504 | 12 506 | 1.07 (0.96–1.18) | 1.09 (0.96–1.22) |
| RPE abnormalities | 293 | 12 506 | 1.14 (1.01–1.30) | 1.20 (1.04–1.39) |
Abbreviations: AMD, age-related macular degeneration; CI, confidence interval; OR, odds ratio; RPE, retinal pigment epithelium; WHR, waist-hip ratio.
Adjusted in logistic regression models.
Adjusted additionally for body mass index (calculated as weight in kilograms divided by height in meters squared), smoking status, years of cigarette smoking, systolic blood pressure, prior coronary heart disease, diabetes, total cholesterol level, high-density lipoprotein cholesterol level, and serum glucose level measured at examination 3 and fibrinogen level, white blood cell count, and physical activity level measured at baseline.
There was a slight increase in the prevalence of AMD across the WHR relative change categories, with 50 cases of AMD (4%) in the group with decreasing WHR, 495 cases (5%) in the group with stable WHR, and 63 cases (5%) in the group with increasing WHR. There was no significant association between continuous change in WHR (OR = 1.09 per 1-SD change; 95% CI, 0.99–1.19) and the presence of AMD after full multivariate adjustment.
Having a decrease in WHR was associated with 29% lower odds of any AMD in the total population (Table 4). Such a decrease was associated with lower odds of early AMD and soft drusen but not with retinal pigment epithelial pigmentary abnormalities. We were unable to analyze late AMD as there were no cases within the decrease group and only 4 within the increase group. No factors for which the variables were adjusted appreciably altered the associations observed (Table 4).
Table 4.
Change in Waist-Hip Ratio Between Baseline and the Third Examination and Age-Related Macular Degeneration at the Third Examination
| OR (95% CI) of AMD | |||||
|---|---|---|---|---|---|
|
|
|||||
| WHR Change | Participants, No. |
Participants at Risk, No. |
Adjusted for Age, Sex, Race, and Centera |
Multivariate-Adjustedb | Multivariate-Adjustedc |
| Any AMD | |||||
| Decreased | 50 | 1250 | 0.74 (0.55–1.00) | 0.71 (0.53–0.97) | 0.71 (0.52–0.97) |
| Stable | 495 | 10004 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Increased | 63 | 1252 | 1.09 (0.83–1.42) | 1.16 (0.87–1.53) | 1.11 (0.82–1.49) |
| Early AMD | |||||
| Decreased | 50 | 1250 | 0.77 (0.57–1.04) | 0.74 (0.55–1.00) | 0.74 (0.54–1.01) |
| Stable | 482 | 10004 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Increased | 59 | 1252 | 1.04 (0.79–1.38) | 1.10 (0.83–1.47) | 1.05 (0.77–1.42) |
| Soft drusen | |||||
| Decreased | 44 | 1250 | 0.79 (0.58–1.09) | 0.78 (0.56–1.07) | 0.78 (0.56–1.08) |
| Stable | 410 | 10004 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Increased | 50 | 1252 | 1.04 (0.77–1.40) | 1.08 (0.79–1.47) | 1.00 (0.72–1.39) |
| RPE abnormalities | |||||
| Decreased | 30 | 1250 | 0.98 (0.67–1.45) | 0.90 (0.60–1.33) | 0.89 (0.59–1.34) |
| Stable | 230 | 10004 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Increased | 33 | 1252 | 1.24 (0.85–1.79) | 1.41 (0.96–2.07) | 1.39 (0.93–2.07) |
Abbreviations: AMD, age-related macular degeneration; CI, confidence interval; OR, odds ratio; RPE, retinal pigment epithelium; WHR, waist-hip ratio.
Adjusted in logistic regression models.
Adjusted additionally for baseline WHR.
Adjusted additionally for baseline smoking status, years of cigarette smoking, change in smoking status during follow-up, baseline body mass index (calculated as weight in kilograms divided by height in meters squared), systolic blood pressure, prior coronary heart disease, diabetes, total cholesterol level, triglycerides level, serum glucose level, plasma fibrinogen level, white blood cell count, and physical activity level.
Decrease and increase in WHR are defined as the bottom and top sex-specific deciles, respectively, of percentage change in WHR over the 6-year follow-up.
Among persons who were obese at baseline, a decrease in WHR was associated with 59% lower odds of AMD (OR = 0.41; 95% CI, 0.20–0.82) (Table 5). There was no relationship between a decrease in WHR and a decreased risk of AMD in those who were overweight or normal weight at baseline. However, there was no significant interaction between WHR change category and baseline weight group (P =.23). No factors for which the variables were adjusted appreciably altered the associations observed (Table 5).
Table 5.
Change in Waist-Hip Ratio Between Baseline and the Third Examination and Age-Related Macular Degenerationat the Third Examination Stratified by Baseline Weight
| OR (95% CI) of AMD | |||||
|---|---|---|---|---|---|
|
|
|||||
| WHR Change | Participants, No. |
Participants at Risk, No. |
Adjusted for Age, Sex, Race, and Centera |
Multivariate-Adjustedb | Multivariate-Adjustedc |
| Obese | |||||
| Decreased | 9 | 414 | 0.39 (0.20–0.77) | 0.38 (0.19–0.77) | 0.41 (0.20–0.82) |
| Stable | 137 | 2649 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Increased | 9 | 236 | 0.83 (0.41–1.65) | 0.85 (0.41–1.76) | 0.85 (0.41–1.78) |
| Overweight | |||||
| Decreased | 23 | 453 | 0.87 (0.56–1.36) | 0.87 (0.55–1.37) | 0.83 (0.52–1.34) |
| Stable | 208 | 4075 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Increased | 22 | 489 | 0.95 (0.60–1.49) | 0.94 (0.59–1.51) | 0.95 (0.58–1.54) |
| Normal weight | |||||
| Decreased | 18 | 373 | 1.00 (0.60–1.66) | 0.92 (0.55–1.54) | 0.96 (0.57–1.61) |
| Stable | 147 | 3212 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Increased | 31 | 517 | 1.42 (0.95–2.12) | 1.61 (1.06–2.45) | 1.45 (0.93–2.27) |
Abbreviations: AMD, age-related macular degeneration; CI, confidence interval; OR, odds ratio; WHR, waist-hip ratio.
Adjusted in logistic regression models.
Adjusted additionally for baseline WHR.
Adjusted additionally for baseline smoking status, years of cigarette smoking, change in smoking status during follow-up, baseline body mass index (calculated as weight in kilograms divided by height in meters squared), systolic blood pressure, prior coronary heart disease, diabetes, total cholesterol level, triglycerides level, serum glucose level, plasma fibrinogen level, white blood cell count, and physical activity level.
Decrease and increase in WHR are defined as the bottom and top sex-specific deciles, respectively, of percentage change in WHR over the 6-year follow-up.
There was no large significant relationship between an increase in WHR over time and increased odds of AMD (Table 4). Stratification by weight category suggested that an increase in WHR was associated with increased odds of any AMD in individuals with normal weight (Table 5), although this was not statistically significant in the fully adjusted model (P = .09).
Analyses were also performed in subgroups defined by sex, diabetes, race, and smoking status. A decrease in WHR was significantly associated with lower odds of having AMD compared with those with stable WHR in women (OR = 0.63;95%CI, 0.40–0.98) and nonsmokers (OR = 0.60; 95% CI, 0.46–0.93). However, no interaction terms between change in WHR, so defined, and sex, diabetes, race, or smoking status were found to be significant.
When categories were defined by absolute change in WHR, the same trends seen earlier were observed (data not shown). After adjustment for age, sex, race, and center, a decrease in WHR was associated with decreased odds of AMD in the total population (OR = 0.74; 95% CI, 0.55–1.00). In the obese subpopulation, the fully adjusted OR for AMD was 0.59 (95% CI, 0.33–1.06).
Analysis of the relationship of percentage change in BMI with AMD demonstrated a relationship similar to that with WHR (data not shown), although the relationship with a large decrease in weight was generally weaker. There was no relationship between decreases in BMI and AMD in the total population (OR = 0.99; 95% CI, 0.74–1.32). In the obese subpopulation, there were decreased odds of 50% (95% CI, 0.27–0.89). A similar relationship with change in waist circumference, similarly defined, was also observed (data not shown), although the only significant association was that between a decrease in waist circumference and AMD in the obese subpopulation (OR = 0.34; 95% CI, 0.16–0.71).
COMMENT
In this middle-aged population, a decrease in WHR over a 6-year period, defined as the bottom decile of percentage change in WHR, was associated with a reduced prevalence of AMD. This effect was particularly apparent among persons who were obese at baseline, with a 61% decrease in the odds of AMD associated with a reduction in WHR over time. While there was a trend to suggest that increases in WHR were also associated with an increased prevalence of AMD, this relationship was not statistically significant.
Our findings suggest a role of weight loss in preventing the development of AMD, adding to existing literature on the increased risk of AMD associated with higher BMI and WHR (Table 1). Prospective data from the Physicians’ Health Study, for example, demonstrated that the 15-year incidence for visually significant dry AMD was highest in obese men and lowest in men with normal BMI while controlling for age and smoking.11 The mechanisms linking higher body weight with AMD are still unclear. Prior studies have suggested that oxidative stress may be one such mechanism.29–31 Other risk factors for AMD, including physical inactivity,32 hypertension, and hyperlipidemia, are also associated with obesity, suggesting that these associations may reflect shared risk factors. However, associations between WHR and AMD were independent of these risk factors.
Our finding of a reduction in WHR related to decreased odds of prevalent AMD is consistent with studies showing that weight loss leads to improvements in cardiovascular risk factors, including diabetes and hypertension.33–36 Studies have further suggested that the beneficial effects of weight loss are most apparent among the overweight or obese,34,35 which supports the stronger association we found for AMD in persons who were obese. One problem with analyzing observational weight loss data is that unintentional weight loss is often caused by illness, leading to an association between weight loss and ill health or mortality. Studies specifically analyzing intentional weight loss have generally found it to be beneficial for health.35 In our study, we did not have data to differentiate intentional weight loss, so it is possible that the true beneficial effects observed are underestimated. However, including only individuals free of coronary heart disease and diabetes at baseline had little effect on the results.
The finding that weight gain (both absolute and relative changes) was not significantly associated with an increased risk of AMD was somewhat unexpected. There was a suggestion of increased AMD risk among persons with normal weight at baseline. This was also seen in another study where substantial weight gain was significantly associated with increased cardiovascular risk only in younger men with normal weight.34
Three observations deserve comment. First, the relationship with AMD was stronger when weight loss was defined according to WHR rather than BMI. Waist-hip ratio is now considered a better measure of abdominal obesity and thus cardiovascular risk.17 Second, there is evidence that relative weight change is a better indicator of metabolic risk than absolute change.21 While we found the same trends when comparing absolute and relative WHR changes, only the relationships with relative change were statistically significant. Third, because the relationships were not continuous, weight change was analyzed categorically. We defined increases and decreases in weight as the sex-specific top and bottom deciles of percentage weight change (as the most extreme changes present in sufficient numbers to provide adequate power) vs the intermediate 8 deciles as the reference group. The percentage changes contained within these deciles were 3% to 44% loss and 6% to 102% gain in WHR. In a recent article, Stevens et al21 suggested that weight maintenance be defined as a change of less than 3% of body weight. Within the 6-year follow-up in this study, approximately one-third of participants increased their WHR by 3% or more. Nevertheless, a repeated analysis using a ±3% cutoff for WHR change showed no significant associations. It will be important to repeat these findings in other studies as the extremes of weight change examined here may not be applicable to other populations.
The primary limitation of this study is that we were restricted to measuring the occurrence rather than incidence of AMD. Thus, we cannot conclude on the causative nature of improvements in WHR with lower risk of AMD. Additional studies analyzing the effect of improvements in WHR and the incidence of AMD are thus necessary. A second limitation is that retinal photography was performed in only 1 eye for each participant. Consequently, the AMD prevalence we found may be lower than the true prevalence, weakening observed effects. A third limitation is that uncontrolled confounding remains a possible explanation of the observed relationships. Finally, in this middle-aged population, there were insufficient numbers to analyze late AMD.
In conclusion, we show that a reduction in WHR in middle-aged persons, particularly those who were initially obese, may be associated with a decrease in the likelihood of prevalent AMD. With increasing prevalence of obesity, these results should be confirmed in future studies as reduction in risk of AMD may be an additional benefit of reducing weight, especially in obese and overweight patients.
Acknowledgments
Funding/Support: The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts N01-HC-55015, N01-HC-55016, N01-HC-55018, N01-HC-55019, N01-HC-55020, N01-HC-55021, and N01-HC-55022. Additional support was provided by a VicHealth Research Fellowship (Dr Peeters) and the National Heart Foundation, Australia (Dr Wong).
Additional Contributions: We thank the staff and participants in the Atherosclerosis Risk in Communities Study for their important contributions.
Footnotes
Financial Disclosure: None reported.
References
- 1.van Leeuwen R, Klaver CC, Vingerling JR, Hofman A, de Jong PT. Epidemiology of age-related maculopathy: a review. Eur J Epidemiol. 2003;18(9):845–854. doi: 10.1023/a:1025643303914. [DOI] [PubMed] [Google Scholar]
- 2.Cheung N, Liao D, Islam FM, Klein R, Wang JJ, Wong TY. Is early age-related macular degeneration related to carotid artery stiffness? the Atherosclerosis Risk in Communities Study. Br J Ophthalmol. 2007;91(4):430–433. doi: 10.1136/bjo.2006.106054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wong TY, Mitchell P. The eye in hypertension. Lancet. 2007;369(9559):425–435. doi: 10.1016/S0140-6736(07)60198-6. [published correction appears in Lancet. 2007;369(9579):2078] [DOI] [PubMed] [Google Scholar]
- 4.Wong TY, Klein R, Sun C, et al. Atherosclerosis Risk in Communities Study. Age-related macular degeneration and risk for stroke. Ann Intern Med. 2006;145(2):98–106. doi: 10.7326/0003-4819-145-2-200607180-00007. [DOI] [PubMed] [Google Scholar]
- 5.Smith W, Mitchell P, Leeder SR, Wang JJ. Plasma fibrinogen levels, other cardiovascular risk factors, and age-related maculopathy: the Blue Mountains Eye Study. Arch Ophthalmol. 1998;116(5):583–587. doi: 10.1001/archopht.116.5.583. [DOI] [PubMed] [Google Scholar]
- 6.Age-Related Eye Disease Study Research Group. Risk factors associated with age-related macular degeneration: a case-control study in the age-related eye disease study: Age-Related Eye Disease Study Report number 3. Ophthalmology. 2000;107(12):2224–2232. doi: 10.1016/s0161-6420(00)00409-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Delcourt C, Michel F, Colvez A, Lacroux A, Delage M, Vernet MH, POLA Study Group Associations of cardiovascular disease and its risk factors with age-related macular degeneration: the POLA study. Ophthalmic Epidemiol. 2001;8(4):237–249. doi: 10.1076/opep.8.4.237.1613. [DOI] [PubMed] [Google Scholar]
- 8.Klein R, Klein BE, Jensen SC. The relation of cardiovascular disease and its risk factors to the 5-year incidence of age-related maculopathy: the Beaver Dam Eye Study. Ophthalmology. 1997;104(11):1804–1812. doi: 10.1016/s0161-6420(97)30023-2. [DOI] [PubMed] [Google Scholar]
- 9.Klein R, Klein BE, Tomany SC, Cruickshanks KJ. The association of cardiovascular disease with the long-term incidence of age-related maculopathy: the Beaver Dam Eye Study. Ophthalmology. 2003;110(4):636–643. doi: 10.1016/S0161-6420(02)01448-3. [corrected and republished in Ophthalmology. 2003;110(6):1273-1280] [DOI] [PubMed] [Google Scholar]
- 10.Klein BE, Klein R, Lee KE, Jensen SC. Measures of obesity and age-related eye diseases. Ophthalmic Epidemiol. 2001;8(4):251–262. doi: 10.1076/opep.8.4.251.1612. [DOI] [PubMed] [Google Scholar]
- 11.Schaumberg DA, Christen WG, Hankinson SE, Glynn RJ. Body mass index and the incidence of visually significant age-related maculopathy in men. Arch Ophthalmol. 2001;119(9):1259–1265. doi: 10.1001/archopht.119.9.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seddon JM, Cote J, Davis N, Rosner B. Progression of age-related macular degeneration: association with body mass index, waist circumference, and waist-hip ratio. Arch Ophthalmol. 2003;121(6):785–792. doi: 10.1001/archopht.121.6.785. [DOI] [PubMed] [Google Scholar]
- 13.Tomany SC, Wang JJ, Van Leeuwen R, et al. Risk factors for incident age-related macular degeneration: pooled findings from 3 continents. Ophthalmology. 2004;111(7):1280–1287. doi: 10.1016/j.ophtha.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 14.Clemons TE, Milton RC, Klein R, Seddon JM, Ferris FL., III Age-Related Eye Disease Study Research Group. Risk factors for the incidence of advanced age-related macular degeneration in the Age-Related Eye Disease Study (AREDS): AREDS report No. 19. Ophthalmology. 2005;112(4):533–539. doi: 10.1016/j.ophtha.2004.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paunksnis A, Cimbalas A, Cerniauskiene LR, et al. Early age-related maculopathy and risk factors of cardiovascular disease in middle-aged Lithuanian urban population. Eur J Ophthalmol. 2005;15(2):255–262. doi: 10.1177/112067210501500213. [DOI] [PubMed] [Google Scholar]
- 16.Moeini HA, Masoudpour H, Ghanbari H. A study of the relation between body mass index and the incidence of age related macular degeneration. Br J Ophthalmol. 2005;89(8):964–966. doi: 10.1136/bjo.2005.066241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Welborn TA, Dhaliwal SS, Bennett SA. Waist-hip ratio is the dominant risk factor predicting cardiovascular death in Australia. Med J Aust. 2003;179(11–12):580–585. doi: 10.5694/j.1326-5377.2003.tb05704.x. [DOI] [PubMed] [Google Scholar]
- 18.ARIC Investigators. The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. Am J Epidemiol. 1989;129(4):687–702. [PubMed] [Google Scholar]
- 19.Hubbard LD, Brothers RJ, King WN, et al. Methods for evaluation of retinal microvascular abnormalities associated with hypertension/sclerosis in the Atherosclerosis Risk in Communities Study. Ophthalmology. 1999;106(12):2269–2280. doi: 10.1016/s0161-6420(99)90525-0. [DOI] [PubMed] [Google Scholar]
- 20.Wong TY, Tikellis G, Sun C, Klein R, Couper DJ, Sharrett AR. Age-related macular degeneration and risk of coronary heart disease: the Atherosclerosis Risk in Communities Study. Ophthalmology. 2007;114(1):86–91. doi: 10.1016/j.ophtha.2006.06.039. [DOI] [PubMed] [Google Scholar]
- 21.Stevens J, Truesdale KP, McClain JE, Cai J. The definition of weight maintenance. Int J Obes (Lond) 2006;30(3):391–399. doi: 10.1038/sj.ijo.0803175. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Geneva, Switzerland: World Health Organization; 1997. [PubMed] [Google Scholar]
- 23.Klein R, Clegg L, Cooper LS, et al. Prevalence of age-related maculopathy in the Atherosclerosis Risk in Communities Study. Arch Ophthalmol. 1999;117(9):1203–1210. doi: 10.1001/archopht.117.9.1203. [DOI] [PubMed] [Google Scholar]
- 24.Klein R, Davis MD, Magli YL, Segal P, Klein BE, Hubbard L. The Wisconsin age-related maculopathy grading system. Ophthalmology. 1991;98(7):1128–1134. doi: 10.1016/s0161-6420(91)32186-9. [DOI] [PubMed] [Google Scholar]
- 25.National Heart, Lung, and Blood Institute. Atherosclerosis Risk in Communities Study: Operations Manual No. 2: Cohort Component Procedures, Version 2.0. Chapel Hill: ARIC Coordinating Center, School of Public Health, University of North Carolina; 1988. [Google Scholar]
- 26.Duncan BB, Schmidt MI, Chambless LE, Folsom AR, Carpenter M, Heiss G. Fibrinogen, other putative markers of inflammation, and weight gain in middle-aged adults: the ARIC study. Obes Res. 2000;8(4):279–286. doi: 10.1038/oby.2000.33. [DOI] [PubMed] [Google Scholar]
- 27.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36(5):936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 28.Brancati FL, Kao WH, Folsom AR, Watson RL, Szklo M. Incident type 2 diabetes mellitus in African American and white adults: the Atherosclerosis Risk in Communities Study. JAMA. 2000;283(17):2253–2259. doi: 10.1001/jama.283.17.2253. [DOI] [PubMed] [Google Scholar]
- 29.Zarbin MA. Current concepts in the pathogenesis of age-related macular degeneration. Arch Ophthalmol. 2004;122(4):598–614. doi: 10.1001/archopht.122.4.598. [DOI] [PubMed] [Google Scholar]
- 30.Kopitz J, Holz FG, Kaemmerer E, Schutt F. Lipids and lipid peroxidation products in the pathogenesis of age-related macular degeneration. Biochimie. 2004;86(11):825–831. doi: 10.1016/j.biochi.2004.09.029. [DOI] [PubMed] [Google Scholar]
- 31.Roth F, Bindewald A, Holz FG. Key pathophysiologic pathways in age-related macular disease. Graefes Arch Clin Exp Ophthalmol. 2004;242(8):710–716. doi: 10.1007/s00417-004-0976-x. [DOI] [PubMed] [Google Scholar]
- 32.Knudtson MD, Klein R, Klein BE. Physical activity and the 15-year cumulative incidence of age-related macular degeneration: the Beaver Dam Eye Study. Br J Ophthalmol. 2006;90(12):1461–1463. doi: 10.1136/bjo.2006.103796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wannamethee SG, Shaper AG. Weight change and duration of overweight and obesity in the incidence of type 2 diabetes. Diabetes Care. 1999;22(8):1266–1272. doi: 10.2337/diacare.22.8.1266. [DOI] [PubMed] [Google Scholar]
- 34.Wannamethee SG, Shaper AG, Walker M. Overweight and obesity and weight change in middle aged men: impact on cardiovascular disease and diabetes. J Epidemiol Community Health. 2005;59(2):134–139. doi: 10.1136/jech.2003.015651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wannamethee SG, Shaper AG, Lennon L. Reasons for intentional weight loss, unintentional weight loss, and mortality in older men. Arch Intern Med. 2005;165(9):1035–1040. doi: 10.1001/archinte.165.9.1035. [DOI] [PubMed] [Google Scholar]
- 36.Stevens VJ, Obarzanek E, Cook NR, et al. Trials for the Hypertension Prevention Research Group. Long-term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II. Ann Intern Med. 2001;134(1):1–11. doi: 10.7326/0003-4819-134-1-200101020-00007. [DOI] [PubMed] [Google Scholar]