Abstract
Parent-Child relationships have long-term effects on health, particularly later inflammation and depression. We hypothesized that these effects would be mediated by later romantic partner relationships and elevated stressors in young adulthood, helping promote chronic, low grade, inflammation as well as depressive symptoms, and driving their covariation. Provocatively, it has been proposed recently that youth experiencing harsher parenting may also develop a stronger association between inflammation and depressive symptoms in adulthood and altered effects of stressors on outcomes. In the current investigation we test these ideas using an 18-year longitudinal study of N = 413 African American youth that provides assessment of the parent-child relationship (at age 10), pro-inflammatory cytokine profile and depressive symptoms (at age 28), and potential mediators in early young adulthood (assessed at ages 21 and 24). As predicted, the effect of harsher parent-child relationships (age 10) on pro-inflammatory state and increased depressive symptoms at age 28 were fully mediated through young-adult stress and romantic partner relationships. In addition, beyond these mediated effects, parent-child relationships at age 10 moderated the concurrent association between inflammation and depressive symptoms, as well as the prospective association between romantic partner relationships and inflammation, and resulted in substantially different patterns of indirect effects from young adult mediators to outcomes. Results support theorizing that the association of depression and inflammation in young adulthood is conditional on earlier parenting, and suggest incorporating this perspective into models predicting long-term health outcomes.
Keywords: inflammation, depression, parenting, stress, cytokines
Parenting experiences during childhood have important implications for a range of physical health and mental health outcomes (Cicchetti & Toth, 2005; Luthar, 2006; Moffitt, et al., 2013; Waldinger & Schultz, 2016). The surprisingly durable effects of experiences during childhood and adolescence is consistent with mounting evidence that such experiences can become biologically embedded in a variety of ways (Brody et al., 2016; Hertzman, 2012 ), potentially allowing them to exert an influence over inflammatory processes and health outcomes many years later (Beach et al., 2015; 2016; Danese, et al., 2008). For African American youth growing up in challenging environments, some types of parenting may play a central protective role, protecting youth from the full impact of difficult rearing environments, and perhaps from difficulties associated with the transition to adulthood in resource poor environments (McLoyd, 1990). In particular, African American youth often confront a challenging transition to productive young adult roles challenging (Young, 2012). Many confront communities with limited resources, discriminatory hiring practices, and challenges that limit opportunities to obtain stable employment (Furstenberg, 2008; Osgood et al., 2005), and so experience additoonal discrimination and economic hardship (Chou et al., 2012; Phelan & Link, 2015). In such contexts, a history of warmer (and less harsh) parenting has been shown to decrease a range of long-term negative outcomes (Luthar, 2006; Brody et al., 2016) including hormonal, metabolic, inflammatory, and cardiovascular risk attributable to childhood and adolescent adversity (Brody, Yu, Beach, Kogan, Windle, & Philibert, 2014; Chen & Miller, 2013), decrease the accelerated aging that often accompanies SES related stressors (Brody et al., 2016; Geronimus, Hicken, Keene, & Bound, 2006), and enhance self-reported health in young adulthood (Beach, Lei, Brody et al., 2016; Danese, et al., 2008). Conversely, harsh parenting may promote inflammation and negative health outcomes (Ehrlich et al., 2015; Schofield, Conger, Gonzales, Merrick, 2016).
The body of research linking child-parent relationships to long-term physical health and mental health outcomes strongly suggests the value of attention to parent-child relationships as one foundation of developmental models that explain the emergence in early adulthood of pro-inflammatory and increased depressive proclivities. However, recent theorizing by Miller and Cole (2012) suggests the possibility of substantial expansion of mediational models linking parent-child relationships to young adult outcomes. Whereas previous models have focused on mediation of parenting effects through psychosocial changes and shifts in various behavioral proclivities, lifestyle choices, or circumstances associated with health outcomes (e.g. McEwen, et al., 1998; Kohen et al, 2002; Stock, et al., 2013; Gibbons, et al., 2014), or have examined direct effects on inflammation or pro-inflammatory propensities (Beach et al., 2016; Cole, 2013), Miller & Cole’s (2012) model suggests that parenting, through its effect on the experience of chronic stressors, may also play a role in changing the association between depression and inflammation (Miller & Cole, 2012). As a consequence, youth reared in less supportive and harsher home environments may be qualitatively different in the way inflammation and depression are associated with each other, and not just quantitatively different in overall level of inflammation and depression compared to peers receiving more supportive parenting. Stated differently, youths who experienced harsh parenting may be more likely to become depressed than their peers with more supportive parents, and more provocatively, Miller and Cole (2012) suggest that their depressive symptoms may be secondary to the effect of inflammation, an effect not present for their peers reared with warmer, less harsh parenting. Further, Miller and Cole (2012) suggest that the concurrent association of inflammation with depressive symptoms may be greater for youth with less warm, more harsh parents.
Several steps are required, however, before this provocative assertion can be fully accepted. Prior research has not examined likely proximal mediators of parenting effects on depressive symptoms and inflammation such as early young adult romantic partner relationships and experience of stressors in the transition to adulthood. It is possible, therefore, that psychosocial mediators such as increased propensity to encounter stressful experiences or problematic relationships with romantic partners during the transition to adulthood may account for some of parenting’s impact on inflammation and depressive symptoms later in young adulthood. These mediators may also help explicate their heightened association with each other for receiving harsher parenting. In addition, it is possible that the hypothesized reprogramming of the connection between inflammation and depressive symptoms is more parsimoniously explained as sensitization to particular stressors due to earlier life experiences, and not as a more general sensitization of inflammation and depression in response to stress. To explore these possibilities further, we provide background on each of the theoretical assertions, and then present an integrated model comprising the parts.
Parenting effects on Depression
There are a variety of reasons to expect that parenting experiences during childhood will contribute to increased depressive symptoms. A large body of evidence supports expectations of a link between parenting and later experiences of depressive symptoms (Blatt & Homann, 1992), and several mechanisms potentially explain this association. First, early stress may set the stage for more stress later on, or lead to stress sensitization, including increased severity and greater responsiveness to stress (e.g. Espejo, et al., 2007). Second, problems in early parenting experiences may lead to increased difficulty in later romantic and interpersonal relationships (e.g., Simons, et al., 2014; Eberhart & Hammen, 2006 ) which may in turn be related to depressive symptoms. Both models have strong potential implications for propensity for depressive symptoms in adulthood (Beach, 2014). Accordingly, African American youth who experience less supportive and more harsh parenting are predicted to experience increased stress during the transition to adulthood in multiple domains (cf. Luthar, 2006; Waldinger & Schultz, 2016), and decreased warmth and more harshness in romantic relationships (Simons et al., 2014) leading to, and potentially accounting for, increased risk for depressive symptoms.
Parenting effects on later inflammation
Several streams of theorizing and empirical work also suggest that parenting should be consequential for later inflammation. In particular, predictive-adaptive response (PAR) models (e.g., Cole, et al., 2011; Gluckman, Hanson & Spencer, 2005; Miller & Cole, 2012; Rickard & Lummaa, 2007) suggest that social adversity and perceived threat in childhood or early adolescence will lead to more inflammation in adulthood. This shift is labeled “adaptive” because it is a biological change that prepares youth for life in dangerous or difficult environments, thereby readying them for elevated risk of tissue damage and a context in which enhanced pro-inflammatory potential might be useful in enhancing survival, or at least would have been adaptive in our recent evolutionary past. At a mechanistic level, parenting can be seen as critical in the process leading to the shift to greater inflammation. Specifically, children raised by more warm and less harsh caregivers are likely to be shielded from some of the negative consequences associated with stress in childhood and adolescence. In turn, this decreased impact of stress should result in decreased desensitization of glucocorticoid receptors in the cells that regulate inflammation (cf. Marques, Silverman, & Sternberg, 2009; Raison & Miller, 2003; Rohleder, Marin, Ma, & Miller, 2009). Indeed, to the extent that supportive parenting helps to counter the impact of life stress for youth growing up in challenging environments, supportive parenting may be particularly consequential in predicting long-term biological consequences in such contexts. In contrast, parenting that is harsh may amplify inflammatory profiles later in life (Dube et al., 2009; Miller & Chen, 2010).
Parenting effects on inflammation through young adult romantic partnerships and stress
In adolescence, quality of relationships with one’s parents is more influential than any other single factor in predicting romantic relationship quality (Simons, Simons & Wallace, 2004), in part because they provide a template for youth regarding relationships and how to respond to interpersonal stress. The resulting patterns of warmth and hostility that youth enact in their own emerging relationships, in turn, influence the quality of their adult relationships (Conger et al., 2000; Bryant, 2006), with a strong direct connection between quality of parenting relationships in childhood and early adult experiences of romantic relationship hostility and warmth (Simons, Simons, Landor, Bryant, & Beach, 2014). In turn, relationship conflict and hostility have been found to prompt elevations in circulating interleukin (IL)-6 and tumor necrosis factor (TNF)-alpha (Kiecolt-Glaser et al., 2005), whereas supportive relationships predict improvements in physical health over time (Barr, Culatta, & Simons, 2013; Barr et al., 2016). Greater parental harshness may also influence the felt stressfulness and so the potential inflammatory impact of romantic partner hostility (Ehrlich, et al., 2015). Similarly, parenting relationships may forecast heightened experiences with stress in young adulthood (Beach et al., 2016) by presaging or contributing to difficulties in other social roles, and also by influencing the inflammatory effects of young adult stressors.
Stress and romantic partner relationship effects on depression and inflammation
Strong and substantial literatures have established the impact of romantic relationship problems and acute stressors on depressive symptoms. There is considerable support for concurrent and prospective connections between romantic relationship problems and depression at all stages of relationship development (Beach, 2014; Steinberg & Davila, 2008). For example, in a population-based sample in the Netherlands, intimate partner relational problems were associated with increased incidence of dysthymia and major depressive episodes (Overbeek et al., 2006), and in a population-based sample of more than 900 married adults who did not meet criteria for 12-month major depressive episode (MDE) at baseline, intimate partner relational problems were associated with a 2.7-fold increased risk for MDE during the following 12 months (Whisman & Bruce, 1999). At the same time, more recent research has found that married and cohabiting couples exhibit similar connections between problems in romantic relationships and depressive symptoms (Barr et al., 2013; Barr, Sutton, Simons, et al., 2016), suggesting broad generalizability of the effect to multiple relationship types. Similarly, for effects of stress on depression, a substantial literature indicates robust associations between stressful life events and depression (Brown & Harris, 1989; Hammen, 2006), an effect of discrimination on depression (Brody et al., 2006; Gibbons et al., 2004) and an effect of financial stress on depression (Conger, 2010). Parallel literatures indicate effects of stress on inflammation, including effects of discrimination and financial strain (Brody et al., 2014; 2015; Cutrona Abraham, Russel, et al., 2015; Simons, Lei, Beach et al., 2016). Similarly, a strong experimental literature links marital hostility to inflammation (Kiecolt-Glaser, et al., 2005; 2010).
The Association of Inflammation and Depression
Because similar psychosocial and family precursors have been linked to both inflammation and depressive symptoms, there is reason to expect some relationship between them, at least for some individuals (Raison, et al., 2006). Less clear, however, is whether the association is stable across individuals, or only holds for some (Glassman & Miller, 2007; Miller & Cole, 2012; Miller, Chen, & Parker, 2011). If the association of depressive symptoms and inflammation is conditional, it is of particular interest to test the factors that may influence the magnitude of the association (Pasco, et al., 2013). Miller and Cole argue that depression and inflammation may co-vary more strongly for those who have experienced substantial childhood adversity (cf. Danese et al., 2008), a circumstance thought to amplify inflammatory cytokine signaling between the brain and the periphery (Irwin & Cole, 2011). As outlined above, harsh parenting in challenging contexts may predict a shift to a pro-inflammatory response set (Beach et al., 2015; 2016; Ehrlich et al., 2015), and to the extent that it does, it may also contribute to the development of increased covariation between depressive symptoms and inflammation in the manner described by Miller & Cole, (2012), and do so beyond its effects on likely psychosocial mediators such as future experience with stressors or with romantic partners.
Parenting Effects on African Americans
As outlined by Ehrlich et al. (2015), harsh vs. supportive parenting helps youth modulate biological reactions to stress, changing activity of the hypothalamic–pituitary–adrenal axis (Flinn & England, 1995; Miller, Chen, et al., 2011; Pendry & Adam, 2007) and, in turn, its biological impact on immune responses, particularly inflammation, desensitization of glucocorticoid receptors to cortisol, and programming of pro-inflammatory cells (monocytes and macrophages), allowing them greater opportunity to initiate and sustain overly prolonged inflammatory responses (e.g., Marques, Silverman, & Sternberg, 2009; Miller et al., 2008; Raison & Miller, 2003; Rohleder, Marin, Ma, & Miller, 2009), and giving rise to the chronic low-grade inflammation thought to be problematic with regard to long-term health outcomes (Raison & Miller, 2003). In the context of a chronic inflammatory state, pro-inflammatory effects may begin to drive some depressive symptomatology such as feelings of fatigue, sluggish cognitive functioning, and sleep dysregulation (Miller et al, 2009; Miller et al., 2008), leading to a shift in which inflammation increasingly drives depressive symptoms. For African American youth, the effect of childhood stressors on inflammation may be intensified (Geronimus, et al., 2006; 2010), increasing the importance of warm and supportive parenting. Supporting this view, Slopen et al (2010) compared the association of retrospective reports of early life adversity and five inflammatory markers (e.g., CRP, IL-6) in a sample of 177 African American and 822 White adults and found a relationship between adversity and all five biomarkers for the African Americans; however, none of the relationships was significant for the Whites. They concluded by calling for additional longitudinal studies with more African American participants.
Heuristic Model
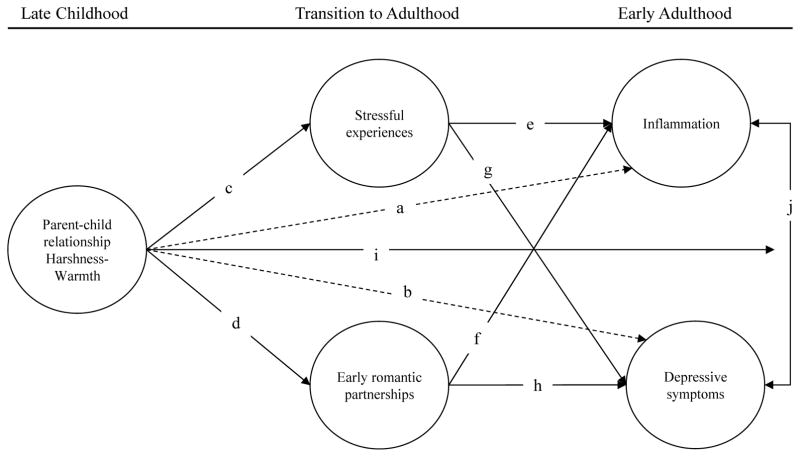
A model that comprises the foregoing elements can be seen in Figure 1. This model suggests that one way in which parent-child relationships influence later depression and inflammation is that parent-child experiences lower in warmth and higher in harshness may directly affect these outcomes (dotted lines a and b). Alternatively, the effect of parenting may be indirect, first influencing the level and experience of stress during early adulthood (path c) as well as influencing emerging romantic partner relationships (path d). In turn, experiences of stressors and behavior in close relationships may mediate parent-child relationships effects on depressive symptoms and inflammation (pathways c,e; d,h; c,g; d,f), driving their covariation. Additionally, the model suggests that, for the reasons outlined above, parenting may further influence the association of depressive symptoms and inflammation, leading those with more negative parent-child experiences to demonstrate a stronger than expected (positive) association between inflammation and depressive symptoms, whereas those with more positive parent-child experiences will show a weaker or negative association (pathway i). Accordingly, line “I” in the figure connecting parenting to outcome covariance (pathway “j”), portrays the hypothesis that even after accounting for all direct and mediated pathways, there will still be a significant moderating effect of the sort proposed by Miller and Cole (2012), indicating that parent-child harshness in childhood has the potential to increase the association of depressive symptoms and inflammation. To the extent this pathway is significant in the final model, it implies a substantial shift, contingent on parenting, in patterns of indirect effects and the extent to which inflammation may drive depressive symptoms.
Figure 1.
Theoretical model showing mediated pathways as well as hypothesized additional biological reprogramming of the association between inflammation and depressive symptoms due to the parent-child relationship.
Examining Pro-inflammatory Effects as a Ratio of Pro- to Anti-inflammatory Cytokines
In the current investigation we examine the ratio of pro to anti-inflammatory cytokines as our index of inflammatory activity. The relative balance between broadly pro-inflammatory cytokines such as TNF-alpha, and those with some or substantial anti-inflammatory properties such as IL-4 and IL-10, is notably altered in a pro-inflammatory direction in numerous inflammatory diseases. This alteration suggests that it is the ratio, rather than the level of either type in isolation, that is most strongly associated with illness. Specifically, because glucocorticoids inhibit production of pro-inflammatory cytokines, but stimulate production of anti-inflammatory cytokines, the effect of stressors and protective factors on long-term health may be captured best by examining the balance of pro vs. anti inflammatory cytokines (Elenkov & Chrousos, 2002) and this approach may provide critical insights into mechanisms underlying various diseases in humans. As described above, family context may influence this balance through its effect on the production of glucocorticoids, (i.e., hormones influencing the production of pro-inflammatory cytokines such as IL-12, TNF-alpha, and interferon (IFN)-gamma), as well as the production of anti-inflammatory cytokines such as IL-10 and IL-4. Thus, chronic stress in the absence of supportive relationships that help to regulate its effects may result in a pro-inflammatory ratio and so a heightened inflammatory response.
Adequate assessment of the balance of pro- and anti-inflammatory cytokines also requires assessment of multiple cytokines that reflect the broad complexity of the whole system. In the current investigation, we use a multiplex system to provide a more robust characterization of cytokine levels and to allow creation of a measure of the pro- to anti-inflammatory cytokine ratio.
Hypotheses
Parent-child relationships will be related to both depressive symptoms and inflammation. More harshness and less warmth in parent-child relationships will be associated with more inflammation and more depressive symptoms.
Parent-child relationships will be associated with early young-adult compound stress level and this will partially mediate its effects on inflammation and depressive symptoms.
Parent-child relationships will also predict warmth/hostility in early young adult romantic relationships and the quality of these romantic relationships will partially mediate parenting’s effects on inflammation and depressive symptoms later in young adulthood.
-
Jointly, early young-adult compound stress and early young adult romantic relationships will both significantly mediate the effects of parent-child relationship harshness and warmth on later young adult depressive symptoms and inflammation.
Direct effects will not account for the moderating effect of parent-child relationship valence on the association between inflammation and depressive symptoms.
-
Explication of the moderating effect of parent-child relationships will show differential strength of pathways from mediators to outcomes as a function of parenting.
In keeping with Miller and Cole (2012), there will be a stronger and more positive association between depressive symptoms and inflammation among those who experienced harsher parenting.
There will be substantially different patterns of indirect effects from young adult mediators to outcomes between those with a history of more harsh vs. more warm parent-child relationships.
Methods
Participants
The first wave of FACHS data was collected in 1997–1998 from 889 African American, fifth-grade children (467 from Iowa and 422 from Georgia), their primary caregiver, and a secondary caregiver when one was present in the home. Primary caregivers’ mean age was 37 (range 23 to 80 years), 93% were female, 84% were the target’s biological mothers, and 44% identified themselves as single parents. Their educational backgrounds were diverse, ranging from less than a high school diploma (19%) to a bachelor’s or advanced degree (9%).
Of the 889 targets interviewed at wave 1, 687 provided data at wave 5 (collected in 2007–2008), and 699 (79% of the original sample) provided data at wave 6 (collected in 2011–2012). Waves 5 and 6 were the assessments used to examine composite stress and romantic relationship quality in early young adulthood. In 2014–2015 a 7th wave of data collection was completed that included blood draws. Given the logistics of scheduling home visits by phlebotomists, only members of the sample residing in Georgia, Iowa, or a contiguous state were identified as eligible. After also excluding persons who were deceased, incarcerated, or otherwise unreachable, we were left with a pool of 545 individuals, 470 (86%) of whom agreed to be interviewed and to provide blood. Of these 413 have been assayed and were included in these analyses.
Analyses indicated that those individuals who did not participate in waves 6 and 7 did not differ significantly from those who participated with regard to wave 1 scores on caregivers’ education, household income, family structure, or neighborhood characteristics. Compared to wave 1, however, a higher percentage of those interviewed at waves 6 and 7 were female.
Procedures
The protocol and all study procedures were approved by the University Institutional Review Boards. To enhance rapport and cultural understanding, African American university students and community members served as field researchers to collect data from the families in their homes. Prior to data collection, the researchers received one month of training in the administration of the self-report instruments. The questions were administered in the respondent’s home and took on average about 2 hours to complete. In wave 1 the instruments were presented on laptop computers. Questions appeared in sequence on the screen, which both the researcher and participant could see. The researcher read each question aloud and the participant entered an anonymous response using a separate keypad. Some of the instruments administered in waves 5 – 7 included questions regarding illegal or potentially embarrassing activities. Hence, in an effort to further enhance anonymity, we used audio-enhanced, computer-assisted, self-administered interviews (ACASI). Using this procedure, the respondent sat in front of a computer and responded to questions as they are both presented visually on the screen and auditorily via earphones.
In addition to the interview data, at Wave 7 participants were also asked to provide a blood sample. A certified phlebotomist drew five tubes of blood at each participant’s home. Two of the tubes were spun immediately to separate serum into 3 cryovials that were then frozen and stored in a −80° freezer until used for the analyses described below. At Wave 7, 63% of the participants had romantic partners. Participants designated as having a romantic partner indicated that they were in a committed relationship (i.e. not dating others), engaged, cohabiting, or married.
Procedure
Measures
Early Parenting
Parenting was assessed using target youth and parent reports when targets were 10.5, on average. The items for the scales were adapted from instruments developed for the Iowa Youth and Families Project (IYFP) (Conger et al., 1992). Hostility/harshness was assessed with eight items from the target and from the parent (e.g., How often did your [caregiver] push, grab, hit or shove you? How often does your [caregiver] insult or swear at you?), each followed by a 4-point scale, from 1 (never) to 4 (always). The parental-warmth measure included nine items, such as “How often in the last 12 months did your [caregiver] let you know [she/he] really cares about you?” each followed by a 4-point scale, from never to always. These items were recoded so that higher scores on all items indicated lack of parental warmth/greater harshness in early life. Scores from the target and the parent were standardized and then averaged to form a measure of the parent-child relationship. Coefficient alpha was .79 for the target, .85 for the parent. Primary caregiver and target reports were correlated significantly, r = .256, p < .001.
Composite stress
We examined three sources of stress at Waves 5 & 6 (when participants were 21 and 24 on average respectively): racial discrimination, financial stress, and negative life events. The racial discrimination scale consisted of 13 items (Landrine & Klonoff, 1996) that focused on the extent to which respondents experienced discriminatory events, ranging from 1 (never) to 4 (several times) during the preceding year (e.g., “How often has someone yelled a racial slur or racial insult at you just because you are African American?”). Cronbach’s alpha for the scale was .91. We also measured the occurrence of serious negative life events during the past year using a five-item scale (Conger & Elder, 1994). An example item is, “Were you seriously ill or injured in the past 12 months?” Two items assessed financial stress (Conger & Elder, 1994): “During the past 12 months, have you had (a) serious money problems or (b) not enough money?” Cronbach’s alpha was .71. In each case, the scale scores were normalized and the mean was calculated to create an overall composite stress measure. Factor analysis of the three standardized scale scores comprising the composite contextual stress measure produced factor loadings that were significant and in the expected direction (λ > .6). Using Nunnally’s (1978) reliability formula for composite variables, the reliability for the overall index was .95.
Romantic partnership warmth/hostility
The measure was comprised of two subscales at Waves 5 and 6. Responses ranged from 1 (never) to 4 (always). To assess warmth in the relationship, we asked three questions concerning the degree to which the partner displayed warm and supportive behaviors (e.g., helped do something important or showed affection) during the past month and three questions concerning the degree to which the respondent displayed the same behaviors toward their partner (Surjadi, Lorenz, Wickrama, & Conger, 2011). Alpha for the scale was .85 at wave 5 and .87 at wave 6. The other scale assessed relationship hostility using the Relationship Hostility Scale (Cui et al., 2005) to allow participants to report how often they had engaged in hostile, aggressive actions toward their romantic partner during the previous month and how often their partner had engaged in these behaviors. This 5-item scale consisted of items such as insult or swear at your romantic partner and shout or yell at your romantic partner. Alpha for the scale was .79 at wave 5 and .80 at wave 6. Actor reports of own and partner’s warm and hostile behaviors were combined so that couple-level relationship warmth and hostility included each respondent’s report of their own and their partner’s behavior. Our index was comprised of the couple-level standardized score on warmth minus the standardized score on hostility. Larger values indicate more positive, supportive relationships with less hostility.
Depressive symptoms
We used a nine item measure of depressive symptoms (UM-CIDI; Kessler 1994). Respondents were asked to report whether or not they experienced several symptoms of depression (e.g. “felt sad, empty, or depressed most of the day” and “lost interest in things”) for at least a two-week period in the past year. Responses ranged from 0 = No to 1 = Yes. All respondents were asked all 9 items, and items were summed to create a measure of depressive symptoms. Cronbach’s alpha for the scale was .85.
Control variables
Gender, diet, exercise, binge drinking, cigarette use, graduating high school, having health insurance, and being married or cohabiting were included as covariates in all multivariate analyses. Covariates have been linked to health and relationship outcomes and so were included to minimize risk of confounding the associations of interest. Gender was self-reported and was controlled in all analyses and examined in exploratory analyses as a potential source of differential response. Demographic controls were education level (0 = less than high school; 1 = high school or more) and married status (0; others; 1 = married/cohabited). Indicators of recent health status and health behavior were also controlled. These controls included health insurance status coded dichotomously (1 = respondent lacks health insurance). Exercise was measured with two items: On how many of the past 7 days did you exercise or participate in physical activity for at least 30 min that made you breathe hard such as running or riding a bicycle fast? And, on how many of the past 7 days did you exercise or participate in physical activity for at least 30 min that did not make you breathe hard, but was still exercise such as fast walking, slow bicycling, skating, pushing a lawn mower, or doing active household chores? The response categories ranged from 1 (0 days) to 5 (all 7 days). Scores on the two items were averaged to form the exercise measure. Healthful diet was assessed using two items that asked about frequency of fruit and vegetable consumption during the previous 7 days. Responses ranged from 1 (none) to 6 (more than once every day) and were averaged to form the healthful diet variable. Binge drinking was defined as the consumption of 3 or more drinks of alcohol (1 = never, 6 = several times per week). Respondents reported how many cigarettes they had smoked in the past 3 months (1 = I have not smoked in the last 3 months to 6 = A pack or more a day).
Assessment of Pro-inflammatory and Anti-inflammatory Cytokines
A certified phlebotomist drew five tubes of blood at each participant’s home. Two of the tubes were spun immediately to separate serum into 3 cryovials that were then frozen and stored in a −80° freezer until used for the analyses described below.
A traditional enzyme-linked immunosorbent assay (ELISA) was used to measure 17 cytokines. To assess the cytokines simultaneously, we used ELISA blood assays obtained with the Bio-Plex Pro™ Human Cytokine 17-Plex Immunoassay (Bio-Rad, Hercules, CA), a 1 × 96-well kit that includes coupled magnetic beads, detection antibodies, standards, assay buffer, wash buffer, sample diluent, standard diluent, detection antibody diluent, streptavidin-PE, a flat bottom plate, and sealing tape. The assay detects IL–1β, IL–2, IL–4, IL–5, IL–6, IL–7, IL–8, IL–10, IL–12, IL–13, IL–17, G–CSF, GM–CSF, IFN–γ, MCP–1, MIP–1β, and TNF–α. Using the 17-plex array, we randomly assigned aliquots of blood from participants to one of eight plates. Because IL–2, GM–CSF, and MCP–1 were present at undetectable levels in the vast majority of samples (≥ 95%) these cytokines were excluded from our index, leaving 14 cytokines to be included. Of the cytokines included, 3 are anti-inflammatory and 11 are pro-inflammatory (see formula below). Full names, intercorrelations, and mean levels for the 14 cytokines used in calculating ratio scores are provided in Supplemental table S1.
To correct for potential method variance reflecting plate effects rather than the variables of interest, we corrected the 14 cytokines for plate-to-plate variation using linear regression with the eight plates entered as categorical covariates. For all cytokines, we used the residuals after the removal of plate effects in subsequent analyses. Utilizing approaches recommended in the literature to enhance the distribution of scores for assays in which “normal” values are typically undetectable, cytokines with no detectable values were coded as 1, cytokines with detectable values below the upper quartile were coded as 2, and those equal to or above the value defining the upper quartile were coded as 3 (Conraads et al., 2006; Taylor et al;., 2013; van Kammen, McAllister-Sistilli, Kelley, Gurklis, & Yao, 1999).
To capture the relative balance of pro-inflammatory to anti-inflammatory activity, cytokines involved in pro-inflammatory responses were summed separately from cytokines involved in anti-inflammatory responses. The following equation was used to calculate the relative balance of pro-inflammatory (numerator) to anti-inflammatory (denominator) cytokines:
Using this ratio, higher scores indicated increasing dominance of the pro-inflammatory response. As expected, levels covaried across all pro- and anti-inflammatory cytokines, with an intraclass correlation of .74 between all cytokines.
Plan of Analysis
We first examined preliminary descriptive statistics and intercorrelations for all the primary study and control variables, setting the foundation for our specific hypotheses. Then we examined hypotheses in the order they were introduced above. In order to test the predictions regarding effects of the parent-child relationship on adult depressive symptoms and inflammation, we used Mplus 7.04 (Muthén & Muthén 2015) to examine hypothesized direct, mediated, and moderated effects. Because missing data might influence our findings, we use the last observation carried forward approach for imputing missing values. The mediated-moderation model available in Mplus 7.04 (Muthén & Muthén, 2015) was used to examine the extent to which the parent-child relationship (at baseline) indirectly influenced adult depressive symptoms and inflammation through young adult relationships and young adult composite stress, as well as whether the effect of association of adult depressive symptoms and inflammation was amplified by quality of the parent-child relationship. Given that unpartnered respondents had no score on relationship quality, we treated romantic partnership warmth/hostility as an internal moderator in order to lose no observations from the analyses. To do so, we first standardized the overall measure (warmth – hostility) to have a mean of 0 and a standard deviation of 1. Then, as instructed by Mirowsky (1999), we assigned all respondents who were not in a relationship a score of zero.
Finally, we tested the final model for sex differences in all pathways using the multiple group analysis option in Mplus, and, absent significant sex differences, we probed for moderation of all pathways from mediators to outcomes by parenting, again using Mplus. We follow-up this with an examination of differences in in indirect pathways from hypothesized mediators to outcomes. To assess goodness-of-fit, we used Steiger’s Root Mean Square Error of Approximation (RMSEA; Browne & Cudeck, 1992) and the comparative fit index (CFI; Bentler 1990). The CFI is truncated to range from 0 to 1 and values close to 1 indicate a very good fit (Bentler 1990). An RMSEA smaller than .05 indicates a close fit; an RMSEA between .05 and .08 suggests a reasonable fit (Browne and Cudeck 1992).
In all analyses, we include all individuals regardless of the presence of a romantic partner. Because the presence vs. absence of a partner may be consequential, this is explicitly modeled in our analyses even though it is not included explicitly in the heuristic model.
RESULTS
Table 1 presents means, standard deviations, and intercorrelations for all demographic and major study variables. As can be seen in Table 1, there are significant zero order correlations among early harsh parenting and inflammation, depressive symptoms, stress, and romantic relationship quality. In addition, inflammation is related to stress and romantic relationship quality, but not to depressive symptoms. As can also be seen, all control variables show significant or marginal associations with other variables in the model, suggesting the value of retaining them as controls in the analyses.
Table 1.
Correlations, means, and standard deviations among the study variables (n = 413)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Inflammation | — | ||||||||||||
| 2. Depressive symptoms | .044 | — | |||||||||||
| 3. Stressful experiences | .186** | .230** | — | ||||||||||
| 4. Romantic relationship | −.157** | −.152** | −.256** | — | |||||||||
| 5. Harsh parenting | .120* | .108* | .188** | −.189** | — | ||||||||
| 6. Health insurance | .074 | .052 | .003 | .085† | .022 | — | |||||||
| 7. Healthful diet | .099* | −.007 | .106* | .089† | −.039 | .118* | — | ||||||
| 8. Exercise | .122* | −.034 | .147** | .028 | .089† | .042 | .158** | — | |||||
| 9. Binge drinking | .029 | .206** | .180** | −.144** | .094† | .034 | −.003 | .127** | — | ||||
| 10. Cigarette use | .000 | .101* | .096† | −.054 | −.039 | −.067 | −.079 | .047 | .170** | — | |||
| 11. High school | .086† | .008 | .034 | .062 | −.056 | .243** | .121* | .052 | .154** | −.123* | — | ||
| 12. Married/cohabited | .062 | −.102* | −.074 | .093† | .024 | .058 | −.001 | .030 | −.063 | −.058 | .020 | — | |
| 13. Males | −.076 | −.152** | .084† | −.041 | .083† | −.115* | −.171** | .150** | .110* | .071 | −.066 | .008 | — |
|
| |||||||||||||
| Mean | 3.740 | 1.685 | .000 | −.015 | −.001 | .821 | 6.559 | 4.966 | 1.889 | 1.860 | .915 | .257 | .380 |
| SD | .779 | 2.154 | .854 | .968 | .652 | .384 | 2.423 | 2.305 | 1.247 | 1.555 | .279 | .437 | .486 |
p ≤ .01;
p ≤.05;
p<.10 (two-tailed tests); N = 413.
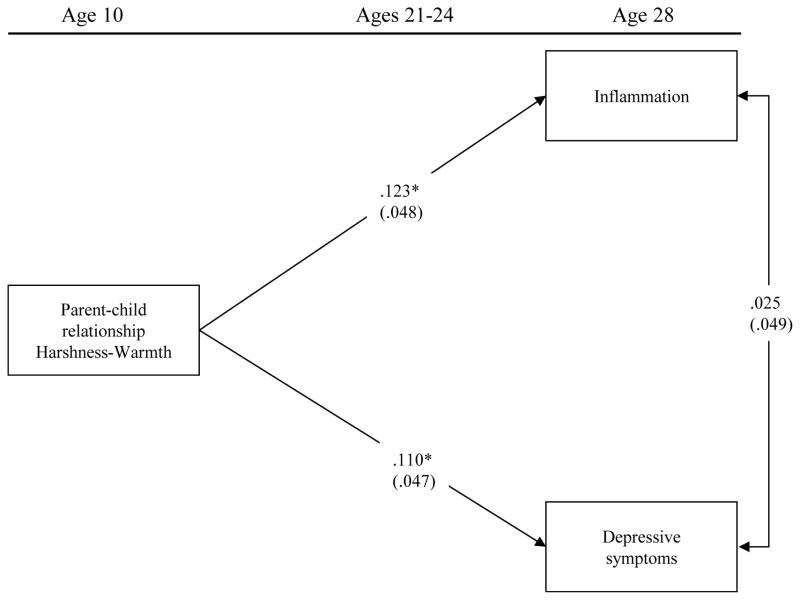
H1: Parent-child relationship at baseline (age 10) will be related to both depressive symptoms and inflammation even after controlling for the impact of control variables
As can be seen in Figure 2, controlling for gender, insurance, diet, exercise, binge drinking, cigarette use, high school, and marital status, the parent-child relationship continued to be significantly correlated with both depressive symptoms (b = .110, p = .020) and pro-inflammatory tendencies (b = .123, p = .011) in adulthood, increasing both, and indicating that the association is robust to covariates. However, despite a common source of influence, symptoms of depressive symptoms and pro-inflammatory tendencies in adulthood were not significantly associated with each other (b = .025, ns).
Figure 2. Direct pathways from parenting to inflammation and depressive symptoms.
Model is saturated. Values are standardized parameter estimates and standard errors are in parentheses. Gender, insurance, diet, exercise, binge drinking, cigarette use, high school, and married or cohabited are controlled in these analyses. N = 413.
**p ≤ .01; *p ≤.05; †p<.10 (two-tailed tests).
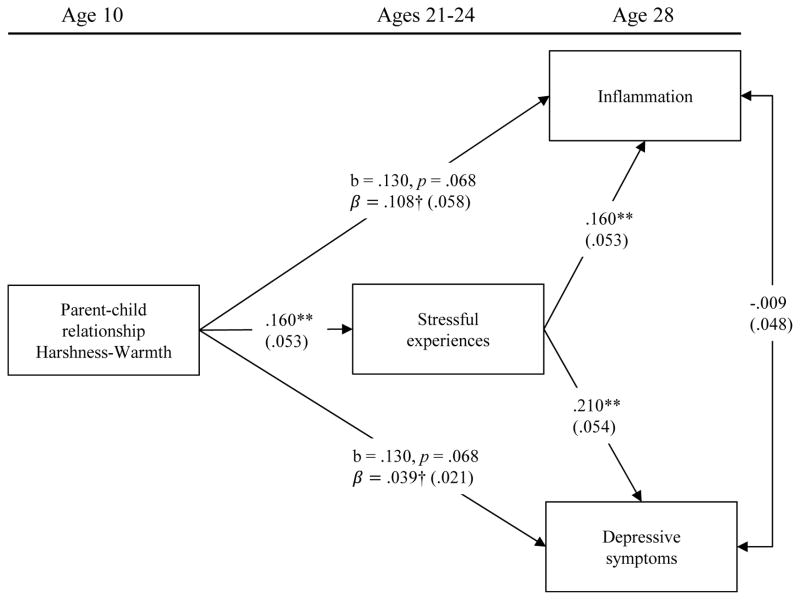
H2: The parent-child relationship will be associated with early young-adult compound stress level and this will partially mediate its direct effects on inflammation and depressive symptoms
Results of our examination of mediation of parent-child relationship effects on adult depressive symptoms and inflammation through young adult stress can be seen in Figure 3. As predicted, there was evidence of a significant effect of the parent-child relationship on young adult composite stress (b = .160, p = .001). Direct pathways from the parent-child relationship to depressive symptoms and inflammation were marginal after including the hypothesized mediator and so were constrained to be equal. Pathways from composite stress to both adult pro-inflammatory state and adult depressive symptoms were significant (b = .160, p = .001, and b = .210, p < .001, respectively), suggesting a significant indirect effect of parenting on outcomes through the association with young adult composite stress. Using bootstrapping methods with 1,000 replications, the test of the indirect effect of the parent-child relationship on inflammation through composite young adult stress was significant [IE = .028, 95% CI = (.009, .062), accounting for 20.59% portion of the total variance]. Likewise, using bootstrapping methods with 1,000 replications, the test of the indirect effect of the parent-child relationship on depressive symptoms through composite stress was significant [IE = .037, 95%CI (.013, .073), accounting for 48.68% of the total variance].
Figure 3. Indirect pathways from parenting to inflammation and depressive symptoms through later composite stress, with direct paths constrained to be equal.
Chi-square = .633, df = 1, p = .426; CFI = 1.000; RMSEA = .000. Values are standardized parameter estimates and standard errors are in parentheses. Gender, insurance, diet, exercise, binge drinking, cigarette use, high school, and married or cohabited are controlled in these analyses. Because direct effects are constrained, unstandardized b’s are provided in addition to the standardized parameters. N = 413. [indirect effect on inflammation = .028, 95%CI (.009, .062), 20.588% of the total variance]. [indirect effect on depression = .037, 95%CI (.013, .073), 48.684% of the total variance].
**p ≤ .01; *p ≤.05; †p<.10 (two-tailed tests).
There was no evidence of multicollinearity among the variables in the model. Diagnostic VIF scores for all variables were below 10, ranging from 1.02 to 1.16, indicating no evidence of multicollinearity among the study variables.
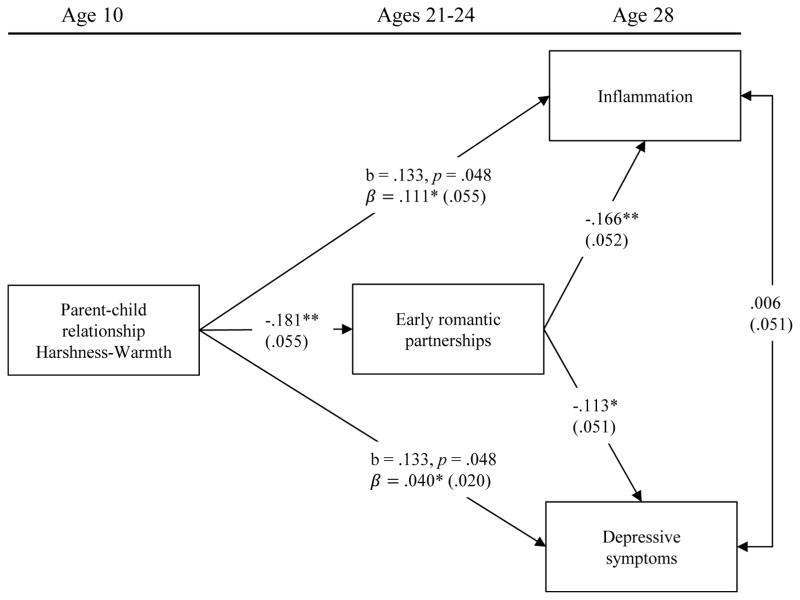
H3: The parent-child relationship will be associated with the balance of warmth and hostility in early young adult romantic relationships and this will mediate its direct effects on inflammation and depressive symptoms
Results of our examination of mediation of the parent-child relationship on adult depressive symptoms and inflammation through young adult romantic relationships can be seen in Figure 4. As predicted, there was evidence of a significant effect of harsh parenting on the warmth and hostility of young adult romantic relationships (b = −.181, p = .001). In turn, there were significant pathways from romantic relationships to both adult pro-inflammatory state (b = −.166, p = .001) and adult depressive symptoms (b = −.113, p = .027), again suggesting a significant indirect effect of parenting on outcomes, but this time through the association with young adult romantic relationships. Using bootstrapping methods with 1,000 replications, the test of the indirect effect of the parent-child relationship on inflammation through supportive-hostile romantic partner relationship was significant [IE = .030, 95%CI (.009, .076), accounting for 21.277% of the total variance]. Likewise, using bootstrapping methods with 1,000 replications, the test of the indirect effect of the parent-child relationship on depressive symptoms through young-adult romantic partner relationships was significant [IE = .020, 95%CI (.003, .050), accounting for 32.786% of the total variance], p < .05]. Supplemental analyses conducted to examine effects separately for romantic partner warmth (See Figure S2) and hostility (See Figure S3) indicate that effects are parallel for the two components and so supports treating them as a combined variable.
Figure 4. Indirect pathways from parenting to inflammation and depressive symptoms through romantic partner relationships, with direct paths constrained to be equal.
Chi-square = 1.522, df = 1, p = .217; CFI = .994; RMSEA = .036. Values are standardized parameter estimates and standard errors are in parentheses. Gender, insurance, diet, exercise, binge drinking, cigarette use, high school, and married or cohabited are controlled in these analyses. Because direct effects are constrained, unstandardized b’s are provided in addition to the standardized parameters. N = 413. [indirect effect on inflammation = .030, 95%CI (.009, .076), 21.277% of the total variance]. [indirect effect on depression = .020, 95%CI (.003, .050), 32.786% of the total variance].
**p ≤ .01; *p ≤.05; †p<.10 (two-tailed tests).
Again, there was no evidence of multicollinearity among the variables in the model. Diagnostic VIF scores for all variables were below 10, ranging from 1.01 to 1.06, indicating no evidence of multicollinearity among the study variables.
H4: a) Jointly, early young-adult compound stress and early young adult romantic relationships will fully mediate direct effects of the parent-child relationship on later young adult depressive symptoms and inflammation
Because both hypothesized sets of mediational pathways were independently significant, we examined their joint effects. As can be seen in Figure 5, both indirect pathways through composite stress remained significant overall [for inflammation, IE = .023, 95% CI = (.006, .056); for depressive symptoms (IE = .034, 95% CI = (.011, .073)). However, only one indirect pathway through young adult romantic relationships remained significant. The indirect pathway to inflammation was significant [IE = .027, 95% CI = (.007, .074)], but the indirect pathway to depressive symptoms was no longer significant.
Figure 5. Full model showing indirect pathways from parenting to outcomes with both mediators and direct pathways from parenting to inflammation and depressive symptoms constrained to be equal.
Chi-square = 8.120, df = 4, p = .087; CFI = .976; RMSEA = .050. Values are standardized parameter estimates and standard errors are in parentheses. Gender, insurance, diet, exercise, binge drinking, cigarette use, high school, and married or cohabited are controlled in these analyses. Because direct effects are constrained, unstandardized b’s are provided in addition to the standardized parameters.N = 413. [indirect effect on inflammation through stress = .023, 95%CI (.006, .056), 20.000% of the total variance]. [indirect effect on depression through stress = .034, 95%CI (.011, .073), 47.887% of the total variance]. [indirect effect on inflammation through romantic partner = .027, 95%CI (.007, .074), 23.478% of the total variance].
**p ≤ .01; *p ≤.05; †p<.10 (two-tailed tests).
Because the difference in chi-square models is itself distributed as a chi-square with degrees of freedom equal to the difference of the nested models, we more stringently tested the hypothesis of full mediation though young adult composite stress and young adult romantic relationship by constraining the direct pathways from parenting to depressive symptoms and inflammation to be zero rather than simply constraining them to be equal. This resulted in a non-significant change in chi-square ( , NS), supporting full mediation of parenting effects on outcomes.
H4b.) Even after fully accounting for the associations due to direct and mediated impacts, early harsh parenting will demonstrate a moderating effect on the relationship between depressive symptoms and inflammation
We also introduced a moderated pathway to test the hypotheses that early harsh parenting would alter the association of inflammation and depressive symptoms even after controlling the effect of shared mediators. As can be seen in Figure 5, the parent-child relationship was a significant moderator (b = .163, p = .001), indicating that there is a different association between depressive symptoms and inflammation as a function of the parent-child relationship experiences that is not explained by the mediated effects.
Using the multiple group analysis option in Mplus we examined the extent to which findings varied by sex. This procedure compares the Chi Square for each path when it is constrained to be equal for males and females versus when it is free to differ. Table 2 shows that the change in Chi Square was not significant for any of the paths in the final structural model presented in Figure 5, indicating no significant sex differences in the pathways examined. Accordingly, we further probed the moderating effect of parenting using the full sample.
Table 2.
Comparison of the paths in figure 5 showing no significant difference for males and females.
| Paths | ΔChi Square | df | p-value |
|---|---|---|---|
| Parent-child relationship → Stressful experiences | .468 | 1 | .494 |
| Parent-child relationship → Inflammation | .197 | 1 | .657 |
| Parent-child relationship → Depressive symptoms | .269 | 1 | .604 |
| Parent-child relationship → Early romantic partnerships | .059 | 1 | .808 |
| Stressful experiences → Inflammation | .693 | 1 | .405 |
| Stressful experiences → Depressive symptoms | 2.759 | 1 | .097 |
| Early romantic partnerships → Inflammation | 2.502 | 1 | .114 |
| Early romantic partnerships → Depressive symptoms | 2.285 | 1 | .131 |
| Depressive symptoms → Inflammation | .005 | 1 | .944 |
| Parent-child relationship × Depressive symptoms → Inflammation | 2.026 | 1 | .155 |
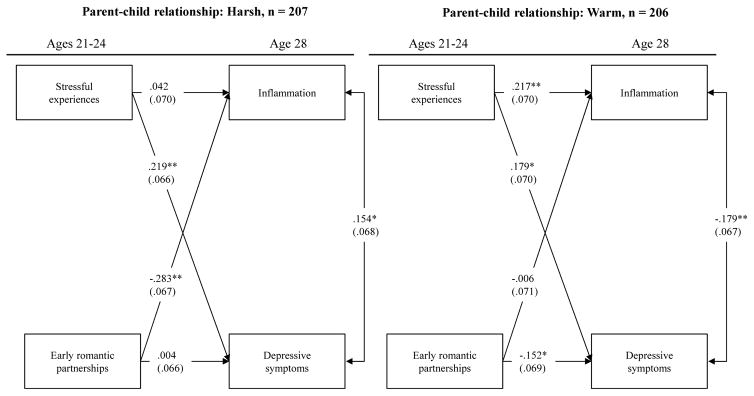
H5: a. Explication of the moderating effect will show differential pathways from mediators to outcomes as a function of the parent-child relationship
To further clarify the implications of the significant moderating effect of the parent-child relationship on the strength of the association between inflammation and depressive symptoms, we contrasted those above the median on harsh parenting at baseline with those at or below the median. The differing patterns of association can be seen in Figure 6, and the significance of pathway differences for harsh vs. warm parenting groups are identified in Table 3. There was a significant association between composite stress and depressive symptoms for both the high harshness (b = .219, p = .001) and high warmth (b = .179, p = .010) groups, and the strength of this association did not differ significantly between the two groups. However, the effect of romantic partner warmth/hostility was significant only for the high early parenting stress group (b = −.283, p < .001) and not for the low harsh parenting group (b = −.006, NS), resulting in a significant difference in this pathway between the two groups ( , p = .009). There also were significant associations between stress and inflammation for the warm (low harsh) parenting group (b = .217, p = .002) as well as between romantic partner problems and depressive symptoms (b = .179, p = .010), and these were not significant for the harsh parenting group, but in neither case is was there a significant difference, ( and 2.598, respectively, NS).
Figure 6. Comparison of Direct and indirect pathways among those above and below the median on experiences of Harsh parenting.
Model is saturated. Values are standardized parameter estimates and standard errors are in parentheses. Gender, insurance, diet, exercise, binge drinking, cigarette use, high school, and married or cohabited are controlled in these analyses. N = 413.
**p ≤ .01; *p ≤.05; †p<.10 (two-tailed tests).
Table 3.
Comparison of the paths for the parent-child relationship high and low in Figure 6
| Paths | Δ Chi-Square | df | p-value |
|---|---|---|---|
| Stress → Inflammation | 2.976 | 1 | .085 |
| Stress → Depression | 0.424 | 1 | .515 |
| Supportive-hostile RP behavior → Inflammation | 6.885 | 1 | .009 |
| Supportive-hostile RP behavior → Depression | 2.598 | 1 | .107 |
| Inflammation ↔ Depression | 11.437 | 1 | .001 |
| Mediated Pathways | |||
| RP relationship → Inflammation → Depression | 18.454 | 2 | .00009 |
| RP relationship → Depression → Inflammation | 14.292 | 2 | .0008 |
| stress → Inflammation → Depression | 14.546 | 2 | .0007 |
| stress → Depression → Inflammation | 12.117 | 2 | .002 |
H5b. There will be a stronger positive association between depressive symptoms and inflammation among those who experienced more harsh parenting than among those who experienced more warm parenting
To test the hypothesis that harsh parenting changed the association between inflammation and depressive symptoms we examined the link for those above the median with those at or below the median on harsh parenting. As can be seen in Figure 6, the associations are substantially different for those high in harsh parenting for whom the association is positive (b = .154, p = .023) compared to those with high Warmth, for whom the association is negative (b = −.179, p = .008). In both cases the association is significant, albeit in opposite directions. The difference between the two pathways was also significant, ( , p = .001).
H5c. There will be substantially different patterns of indirect effects from young adult mediators to outcomes between those with harsh parent-child relationships compared to those with warm parent-child relationships
To test the hypothesis that parenting might change indirect pathways to outcomes by increasing the effect of inflammation on depressive symptoms, we examined all four indirect effect pathways from hypothesized mediators to outcomes. As can be seen in the bottom half of Table 3, all indirect paths differed significantly between the two groups, with models treating inflammation as the mediator being most strongly divergent. Using bootstrap methods with 1,000 replications, the test of the indirect effect of romantic partner relationships on depressive symptoms through inflammation was significantly different for those above vs. below the median on parental harshness [For those above the median (Harsh), IE = −.041, 95%CI (−.113, −.006), 47.13% of the total variance. For those below the median (Warm), IE = .004, 95%CI (−.021, .026), 0.65% of the total variance]. Likewise, the test of the indirect effect of composite stress on depressive symptoms through inflammation was significantly different. [For those above the median (Harsh), IE = .006, 95%CI (−.010, .043), 2.74% of the total variance. For those below the median (Warmth), IE = −.038, 95%CI (−.086, −.007), 14.90% of the total variance.]. Also, significantly different were indirect effects on depression through inflammation. The indirect effect of romantic partner relationships on inflammation through depressive symptoms was significantly different for those above vs. below the median [For those above the median (Harsh), IE = .001, 95%CI (−.020, .037), 0.351% of the total variance. For those below the median (Warm), IE = 45.902, 95%CI (−.003, .077), 0.65% of the total variance]. In addition, the test of the indirect effect of composite stress on inflammation through depressive symptoms was significantly different for those above vs. below the median [For those above the median (Harsh), IE = .035, 95%CI (.003, .101), 83.33% of the total variance. For those below the median (Warmth), IE = −.033, 95%CI (−.083, −.001), 11.66% of the total variance.]
Discussion
As expected, we found strong support for the hypothesis that some effects of the parent-child relationship on later inflammation and depression were mediated by early young-adult behavioral proclivities. In particular, due to the association of greater parental harshness and less warmth with later increased likelihood to experience elevated levels of composite stress and decreased warmth - hostility in romantic partner relationships in early young adulthood, the main effect associations with inflammation and depressive symptoms were fully explained. Indeed, the main effects from parenting to depression and inflammation could be constrained to be zero in the final model without producing significant deterioration in model fit. Accordingly, the mediational model presented in figure 5 is consistent with a broad prior literature linking parenting to later experiences of stress, as well as with the hypothesis that the parent-child relationship lays the groundwork for development of adult romantic partner relationships. Although this model fits the data well, there was one tell-tale oddity. Surprisingly, despite having a number of predictors in common, depressive symptoms and inflammation were not significantly correlated in adulthood (age 28). In keeping with hypotheses put forward by Cole and Miller (2012) we wondered if this might reflect higher-order changes attributable to the parent-child relationship in which widespread reprogramming of direction and magnitude of effects between depressive symptoms and inflammation occurred.
Consistent with hypotheses put forward by Cole and Miller (2012), the parent-child relationship also moderated the association of inflammation and depressive symptoms in adulthood. The non-significant association between depressive symptoms and inflammation in adulthood observed for the sample as a whole masked two significant correlations in the sub-populations formed by considering separately those with more versus less harsh parenting in childhood. Among those who had harsher parenting experiences, the association between inflammation and depression was significant and positive, indicating that greater inflammation was associated with greater depressive symptoms. However, among those with warmer parent-child relationships, the association was significant and negative, indicating that greater inflammation was associated with fewer depressive symptoms. This pattern suggests substantial shifts in associations among harsh parenting, inflammation, and depressive symptoms, and provides initial support for the hypothesis that parenting may be particularly consequential for understanding adult pro-inflammatory tendencies (Ehrlich, et al., 2015), as well as supporting Miller and Cole’s (2012) hypothesis that there may be two relatively distinct populations comprising the general population with each showing differing patterns of association between inflammation and depressive symptoms.
Our examination of mediators also allowed us to examine prospective effects of stress on depressive symptoms and inflammation as well as prospective effects of romantic relationships on depressive symptoms and inflammation, potentially adding to previous theorizing. We found that both composite stress in early young adulthood and romantic partner relationship quality served as mediators of parenting’s effect on inflammation and depressive symptoms. However, when considered jointly, the indirect pathway from parenting to depressive symptoms through romantic partner relationship quality became non-significant, suggesting that some apparent effects on depression that might be attributed to relationship quality when it is considered alone may be better thought of as effects of composite stress, highlighting the potential for stress and relationship quality to influence each other as well as depressive symptoms. Equally interesting is the possibility that examination of subpopulations would show other interesting patterns of indirect effects. The indirect effect of romantic partner relationship quality on depression through inflammation is particularly pronounced among those with more harsh parent-child relationships, and is made all the more interesting because the effect of romantic relationship quality on inflammation remained robust to the inclusion of composite stressor effects even in the overall model, suggesting that its effect on inflammation is as strong overall as the effect of the composite stress variable comprised of financial stress, discrimination, and recent negative life events. Overall then, the results are consistent with the expectation that the Miller and Coles (2012) model will highlight new facets of the relationship between depressive symptoms and inflammation, substantially expanding mediational models that link experiences in adulthood with later depressive and inflammatory outcomes.
Of particular interest, the introduction of likely mediators of parenting’s effect on inflammation and depressive symptoms did not account for moderation of their association by parental harshness. Expected mediating pathways were found, but so were significant shifts in underlying associations due to parenting experiences. Accordingly, at this level the Miller and Cole (2012) hypothesis was strongly supported. Looking at specific pathways, however, we found that the prospective pathways between composite stress and inflammation for those with harsher parenting was marginal, and was stronger among those reared in “warmer” parenting contexts. This is inconsistent with a broad “stress-sensitivity” effect due to harsh parenting. Conversely, the prospective association of romantic partner relationship and inflammation was significantly different between the two groups, with those experiencing harsher parenting demonstrating a significantly stronger (inverse) association between warmth in the romantic partner relationship and elevated inflammation. This finding is in the direction that would be expected based on Miller and Cole (2012) and may suggest that, at least when attention is focused on the sensitizing effects of harsh parenting, there may be sensitization primarily to later interpersonal events, including difficulties in romantic partner relationships, and perhaps there is not a tendency toward a more generalized heightened stress-sensitivity.
Consistent with predictions by Miller and Cole (2012) we also observed a substantial shift in the pattern of indirect pathways from stressors to outcomes as a function of differing parent-child relationship experiences. Consistent with theorizing, differences in indirect effects were most prominent for those in which stressor effects on depression were mediated through inflammation, suggesting a role for inflammation in driving depressive symptoms. The indirect effect of romantic partner relationship quality on depressive symptoms through inflammation was significantly greater for those who had experienced harsher parenting. Conversely, the indirect effect of composite stress on depression through inflammation was significantly stronger for those who had experienced warmer relationships with parents, but the effect countered rather than amplified the direct effect of composite stress on depressive symptoms. That is, it appears those with warmer parenting histories were afforded additional protection against depressive symptoms in response to external stressors, and it is a protection not afforded to those with harsher parenting.
Limitations
Although our study overcame some limitations of past research and addressed a novel and exciting theoretical issue, it also suffered from several shortcomings. First, the dataset is limited in its ability to probe effects across childhood. Our data set begins at age 10, and it would be of considerable interest to examine parenting relationships at even earlier ages. Many versions of the PAR model emphasize the importance of programming that occurs at even earlier ages (e.g., Miller, Chen, Parker, 2011), and it may be that early experience with harsh parenting and harsh environments before age 10 is even more consequential than that measured at age 10. However, this also can also be seen as making the current investigation somewhat conservative. Most current theorizing would hypothesize even larger effects if parenting were assessed at younger ages. In addition, because of the relatively strong stability of both context and parenting across childhood, it may be that our assessments at age 10 proved to be relatively strong predictors in part because they actually captured considerable variance in earlier parenting experiences. A second limitation is that we were not able to link our assessment of inflammation in adulthood to a later increased risk for illness in middle age or beyond. At the last wave of data collection, our respondents were only 28 years of age. Consequently, they have not yet entered the age of risk for onset of the chronic diseases of aging. As we have noted, however, prior research has established a link between inflammation and onset of chronic illness, and recently Simons et al. (2016) found that inflammation completely mediated the impact of socioeconomic strain on the development of chronic illness. Accordingly, an important future direction will be to link parenting to chronic diseases of aging as these emerge, as well as to other specific illnesses, or precursors to illness, and to show that these effects are mediated by inflammation.
Conclusions and Implications for Future Directions
Our study findings might be viewed as containing a combination of encouragement and caution for those interested in parenting’s role in health and for PAR theorists. On the one hand, it appears clear that parenting relationships must be considered when investigating the impact of adverse events and negative context on children. A warm relationship with a parent provides considerable beneficial effect on life trajectory, and also appears consequential for the programming of biological reactions to future stressors and the manner in which inflammation and depressive symptoms influence each other. The cautionary note is that the reprogramming that occurs may not unfold in exactly the way that current models suggest, and it may be necessary to add measures of young adult and later adult relationships to better capture some of the variables likely to drive problematic shifts in inflammation and to promote chronic depressive symptoms in the context of chronic inflammation. Given the complex nature of inflammatory processes, of course, it is likely that other markers of inflammation or other ways of combining those markers could lead to somewhat different conclusions. However, because inflammation is an important marker of health, it will be useful and important to further probe the current results and examine additional biological correlates in future investigations.
It may be taken as somewhat bad news, however, that a “harsher” parenting style has such long lasting effects on an individual’s risk for elevated inflammation and depressive symptoms (and their relationship to each other). Early negative parenting elevates both inflammation and depressive symptoms during adulthood and increases the likelihood that problems in adult relationships with a romantic partner will amplify inflammation still further, indirectly amplifying depressive symptoms. This finding suggests, at a minimum, that most interventions focused on relationship quality begin too late. Ideally we would begin our efforts to prevent later romantic relationship problems by helping build warm, supportive parent-child relationships. The current results suggest that if we missed this window of opportunity we might still focus on enhancing early adult relationships because these may be the more proximal mediators of some of the lasting effects of parenting. These early relationships may be quite consequential for understanding the “weathering” process and its attendant implications for health across adulthood. Underscoring the value of an increased relationship focus is that there is a stronger effect of young adult relationships on inflammation for those with a history of harsher parenting, suggesting that to the extent that effective relationship interventions are developed and offered at this stage of life, they may prove particularly consequential for inflammation and health among those at greater risk.
There also may be clinical implications of the current findings related to rethinking and modifying current “marital models” of depression (Beach et al., 1990). The current results suggest that those at greater risk for relationship problems, i.e. those with a history of harsher parenting experiences, are also more likely to show a pattern of concomitant inflammation, and substantially stronger indirect effects from romantic relationship hostility to inflammation and then to depressive symptoms. If so, it may be that inflammatory processes are helping to drive or maintain their depressive symptoms, and better understanding this mechanism may result in improved intervention. For example, depressed persons whose depressive symptoms are being driven by relationship hostility may be less responsive to standard pharmacological intervention (Hepgul et al., 2016). If confirmed in work with clinical or treatment seeking populations, this would suggest the value of considering alternative pharmacotherapy for such cases, perhaps combining marital therapy or other interpersonally focused intervention with pharmacological agents that have enhanced anti-inflammatory activity.
Supplementary Material
Acknowledgments
This research was supported by Award Number R01 HL8045 from the National Heart, Lung, and Blood Institute, Award Number R01 HD080749 from the National Institute of Child Health and Human Development, and P30 DA027827 from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily reflect the official views of the National Institutes of Health or any agencies that comprise it.
Contributor Information
Steven R. H. Beach, Center for Family Research, University of Georgia
Man Kit Lei, Center for Family Research, University of Georgia.
Ronald L. Simons, Department of Sociology, University of Georgia
Ashley B. Barr, Department of Sociology, SUNY Buffalo
Leslie G. Simons, Department of Sociology, University of Georgia
Katherine Ehrlich, Center for Family Research, University of Georgia.
Gene H. Brody, Center for Family Research, University of Georgia
Robert A. Philibert, Department of Psychiatry, Carver School of Medicine, University of Iowa
References
- Barr AB, Culatta E, Simons RL. Romantic relationships and health among African American young adults: Linking patterns of relationship quality over time to changes in physical and mental health. Journal of Health and Social Behavior. 2013;54:369–385. doi: 10.1177/0022146513486652. http://dx.doi.org/10.1177/0022146513486652. [DOI] [PubMed] [Google Scholar]
- Barr AB, Sutton TE, Simons LG, Wickrama KAS, Lorenz FO. Romantic Relationship Transitions and Changes in Health among Rural, White Young Adults. Journal of Family Psychology. 2016;30:832–842. doi: 10.1037/fam0000207. doi: http://dx.doi.org/10.1037/fam0000207. [DOI] [PubMed] [Google Scholar]
- Beach SRH. The Couple and Family Discord Model of Depression: Updates and Future Directions. In: Agnew Christopher R, South Susan C., editors. Interpersonal Relationships and Health: Social and Clinical Psychological Mechanisms. Oxford University Press; 2014. pp. 133–155. [Google Scholar]
- Beach SRH, Lei MK, Brody GH, Miller GE, Chen E, Mandara J, Philibert RA. Smoking in young adulthood among African Americans: Interconnected effects of supportive parenting in early adolescence, pro-inflammatory epitype, and young adult stress. Development and Psychopathology. doi: 10.1017/S0954579416000961. Published online: 20 October 2016. First View. DOI: http://dx.doi.org/10.1017/S0954579416000961. [DOI] [PMC free article] [PubMed]
- Beach SRH, Lei MK, Brody GH, Dogan MV, Philibert RA. Higher Levels of Protective Parenting are Associated with Better Young Adult Health: Exploration of Mediation through Epigenetic Influences on Pro-Inflammatory Processes. Frontiers in Psychology. 2015;6:676. doi: 10.3389/fpsyg.2015.00676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach SRH, Lei MK, Brody GH, Kim S, Barton AW, Dogan MV, Philibert RA. Parenting, SES-risk, and later Young Adult Health: Exploration of opposing indirect effects via DNA methylation. Child Development. 2016;87(1):111–121. doi: 10.1111/cdev.12486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Blatt SJ, Homann E. Parent-child interaction in the etiology of dependent and self-critical depression. Clinical Psychology Review. 1992;12(1):47–91. [Google Scholar]
- Brody GH, Chen YF, Murry VM, Simons RL, Ge X, Gibbons FX, Gerrard M, Cutrona CE. Perceived Discrimination and the Adjustment of African American Youths: A Five-Year Longitudinal Analysis With Contextual Moderation Effects. Child Development. 2006;77(3):1170–1189. doi: 10.1111/j.1467-8624.2006.00927.x. [DOI] [PubMed] [Google Scholar]
- Brody GH, Miller GE, Yu T, Beach SRH, Chen E. Supportive family environments ameliorate the link between racial discrimination and epigenetic aging: A replication across two longitudinal cohorts. Psychological Science. 2016;27(4):530–541. doi: 10.1177/0956797615626703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Yu T, Beach SRH. Resilience to Adversity and the Early Origins of Disease. Development and Psychopathology. 2016;28(4pt2):1347–1365. doi: 10.1017/S0954579416000894. speical issue on Epigenetics: Development, Psychopathology, Resilience, and Preventive Intervention. DOI: https://doi.org/10.1017/S0954579416000894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Yu T, Beach SRH, Kogan SM, Windle M, Philibert RA. Harsh parenting and adolescent health: A longitudinal analysis with genetic moderation. Health Psychology. 2014;33(5):401–409. doi: 10.1037/a0032686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Yu T, Miller GE, Chen C. Discrimination, racial identity, and cytokine levels among African-American adolescents. Journal of Adolescent Health. 2015;56:496–501. doi: 10.1016/j.jadohealth.2015.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological Methods and Research. 1992;21:230–258. [Google Scholar]
- Brown GW, Harris TO. Social origins of depression: A study of psychiatric disorder in women. London: Routledge; 1989. [Google Scholar]
- Bryant CM. Pathways linking early experiences and later relationship functioning. In: Crouter AC, Booth A, editors. Romance and Sex in Adolescence and Emerging Adulthood: Risks and Opportunities. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 2006. pp. 103–111. [Google Scholar]
- Chen E, Miller GE. Socioeconomic status and health: Mediating and moderating factors. Annual Review of Clinical Psychology. 2013;9:723–749. doi: 10.1146/annurev-clinpsy-050212-185634. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. Child maltreatment. Annual Review of Clinical Psychology. 2005;1:409–438. doi: 10.1146/annurev.clinpsy.1.102803.144029. [DOI] [PubMed] [Google Scholar]
- Chou T, Asnaani A, Hofmann SG. Perception of racial discrimination and psychopathology across three U.S. ethnic minority groups. Cultural Diversity and Ethnic Minority Psychology. 2012;18(1):74–81. doi: 10.1037/a0025432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole SW. Social Regulation of Human Gene Expression: Mechanisms and Implications for Public Health. American Journal of Public Health. 2013;103(Suppl 1):S84–S92. doi: 10.2105/AJPH.2012.301183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole SW, Conti G, Arevalo JMG, Ruggiero AM, Heckman JJ, Suomi SJ. Transcriptional modulation of the developing immune system by early life social adversity. Proceedings of the National Academy of Sciences. 2012;109:20578–20583. doi: 10.1073/pnas.1218253109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger RD, Conger KJ, Elder GH, Lorenz FO, Simons RL, Whitbeck LB. A family process model of economic hardship and adjustment of early adolescent boys. Child development. 1992;63(3):526–541. doi: 10.1111/j.1467-8624.1992.tb01644.x. [DOI] [PubMed] [Google Scholar]
- Conger RD, Cui M, Bryant GM, Elder GH. Competence in early adult romantic relationships. Journal of Personality and Social Psychology. 2000;79:224–237. doi: 10.1037//0022-3514.79.2.224. http://dx.doi.org/10.1037/0022-3514.79.2.224. [DOI] [PubMed] [Google Scholar]
- Conger RD, Conger KJ, Marin MJ. Socioeconomic status, family processes, and individual development. Journal of Marriage and Family. 2010;72(3):685–704. doi: 10.1111/j.1741-3737.2010.00725.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger RD, Elder GH., Jr . Families in troubled times: The Iowa Youth and Families Project. In: Conger RD, Elder GH Jr, editors. Families in troubled times: Adapting to change in rural America. Hawthorne, NY: Aldine de Gruyter; 1994. pp. 57–78. [Google Scholar]
- Conraads VM, Denollet J, De Clerck LS, Stevens WJ, Bridts C, Vrints CJ. Type D personality is associated with increased levels of tumour necrosis factor (TNF)-α and TNF-α receptors in chronic heart failure. International Journal of Cardiology. 2006;113:34–38. doi: 10.1016/j.ijcard.2005.10.013. [DOI] [PubMed] [Google Scholar]
- Cui M, Lorenz F, Conger R, Melby J, Bryant C. Observer, self-, and partner reports of hostile behaviors in romantic relationships. Journal of Marriage and Family. 2005;67:1169–1181. doi: 10.1111/j.1741-3737.2005.00208.x. [DOI] [Google Scholar]
- Curtis S, Dunkel CS, Mathes EW, Kesselring SN, Decker ML, Kelts DJ. Parenting influence on the development of life history strategy. Evolution & Human Behavior. 2015;36(5):374–378. DOI: http://dx.doi.org/10.1016/j.evolhumbehav.2015.02.006. [Google Scholar]
- Cutrona CE, Abraham WT, Russel DW, Beach SRH, Burzette R, Gibbons FX, Gerrard M, Monik M, Philibert RA. Financial Strain, Inflammatory Factors, and Hemoglobin A1C Levels in African-American women. British Journal of Health Psychology. 2015;20(3):662–79. doi: 10.1111/bjhp.12120. [DOI] [PubMed] [Google Scholar]
- Danese A, Moffitt TE, Pariante CM, Ambler A, Poulton R, Caspi A. Elevated inflammation levels in depressed adults with a history of childhood maltreatment. Archives of General Psychiatry. 2008;65:409–415. doi: 10.1001/archpsyc.65.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, Croft JB. Cumulative childhood stress and autoimmune diseases in adults. Psychosom Med. 2009;71:243e250. doi: 10.1097/PSY.0b013e3181907888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eberhart N, Hammen C. Interpersonal predictors of onset of depression during the transition to adulthood. Personal Relationships. 2006;13:195–206. [Google Scholar]
- Ehrlich KB, Miller GE, Rohleder N, Adam EK. Trajectories of relationship stress and inflammatory processes in adolescence. Development and Psychopathology. 2015;28:127–138. doi: 10.1017/S0954579415000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elenkov IJ, Chrousos GP. Stress hormones, proinflammatory and anti-inflammatory cytokines, and autoimmunity. Annals of the New York Academy of Science. 2002;966:290–303. doi: 10.1111/j.1749-6632.2002.tb04229.x. [DOI] [PubMed] [Google Scholar]
- Espejo E, Hammen C, Connolly N, Brennan P, Najman J, Bor W. Stress sensitization and adolescent depressive severity as a function of childhood adversity: A link to anxiety disorders. Journal of Abnormal Child Psychology. 2007;35:287–299. doi: 10.1007/s10802-006-9090-3. [DOI] [PubMed] [Google Scholar]
- Flinn MV, England BG. Childhood stress and family environment. Current Anthropology. 1995;36:854–866. doi: 10.1086/204444. [DOI] [Google Scholar]
- Furstenberg FF. The intersections of social class and the transition to adulthood. New Directions for Child and Adolescent Development. 2008;2008(119):1–10. doi: 10.1002/cd.205. [DOI] [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States. American Journal of Public Health. 2006;96:826–833. doi: 10.2105/ajph.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Hicken MT, Pearson JA, Seashols SJ, Brown KL, Cruz TD. Do US Black women experience stress-related accelerated biological aging? A novel theory and first population-based test of Black-White differences in telomere length. Human Nature. 2010;21:19–38. doi: 10.1007/s12110-010-9078-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons FX, Gerrard M, Cleveland MJ, Wills TA, Brody G. Perceived discrimination and substance use in African American parents and their children: A panel study. Journal of Personality and Social Psychology. 2004;86(4):517–529. doi: 10.1037/0022-3514.86.4.517. [DOI] [PubMed] [Google Scholar]
- Gibbons FX, Kingsbury JH, Weng C, et al. Effects of perceived racial discrimination on health status and health behavior: A differential mediation hypothesis. Health Psychology. 2014;33(1):11–19. doi: 10.1037/a0033857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glassman AH, Miller GE. Where there is depression, there is inflammation. sometimes! Biological Psychiatry. 2007;62:280–281. doi: 10.1016/j.biopsych.2007.05.032. [DOI] [PubMed] [Google Scholar]
- Gluckman PD, Hanson MA, Spencer HG. Predictive adaptive responses and human evolution. Trends in Ecology and Evolution. 2005;20(10):537–533. doi: 10.1016/j.tree.2005.08.001. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress generation in depression: reflections on origins, research, and future directions. Journal of Clinical Psychology. 2006;62(9):1065–1082. doi: 10.1002/jclp.20293. doi:210.1002/JCLP.20293. [DOI] [PubMed] [Google Scholar]
- Hepgul N, Cattaneo A, Agarwal K, Baraldi S, Borsini A, Bufalino C, … Pariante CM. Transcriptomics in Interferon-α-Treated Patients Identifies Inflammation-, Neuroplasticity- and Oxidative Stress-Related Signatures as Predictors and Correlates of Depression. Neuropsychopharmacology. 2016;41(10):2502–2511. doi: 10.1038/npp.2016.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hertzman C. Putting the concept of biological embedding in historical perspective. PNAS. 2012;109(Suppl 2):17160–17167. doi: 10.1073/pnas.1202203109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin MR, Cole SW. Reciprocal regulation of the neural and innate immune systems. Nature Reviews Immunology. 2011;11:625–632. doi: 10.1038/nri3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Loving TJ, Stowell JR, Malarkey WB, Leme-show S, Dickinson SL, et al. Hostile marital interactions, proinflammatory cytokine production, and wound healing. Archives of General Psychiatry. 2005;62:1377–1384. doi: 10.1001/archpsyc.62.12.1377. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Gouin J, Hantsoo L. Close relationships, inflammation, and health. Neuroscience & Biobehavioral Reviews. 2010;35:33–38. doi: 10.1016/j.neubiorev.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohen DE, Brooks–Gunn J, Leventhal T, Hertzman C. Neighborhood income and physical and social disorder in canada: Associations with young children’s competencies. Child Development. 2002;73(6):1844–1860. doi: 10.1111/1467-8624.t01-1-00510. [DOI] [PubMed] [Google Scholar]
- Landrine H, Klonoff EA. The Schedule of Racist Events: A measure of racial discrimination and a study of its negative physical and mental health consequences. Journal of Black Psychology. 1996;22:144–168. doi: 10.1177/00957984960222002. [DOI] [Google Scholar]
- Lanquillon S, Krieg JC, Bening-Abu-Shach U, Vedder H. Cytokine production and treatment response in major depressive disorder. Neuropsychopharmacology. 2000;22(4):370–379. doi: 10.1016/S0893-133X(99)00134-7. [DOI] [PubMed] [Google Scholar]
- Luthar SS. Resilience in development: A synthesis of research across five decades. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology: Risk, Disorder, and Adaptation. New York: Wiley; 2006. pp. 740–795. [Google Scholar]
- Marques AH, Silverman MN, Sternberg EM. Glucocorticoid dysregulations and their clinical correlates: From receptors to therapeutics. Annals of the New York Academy of Sciences. 2009;1179:1–18. doi: 10.1111/j.1749-6632.2009.04987.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- McLoyd VC. The Impact of Economic Hardship on Black Families and Children: Psychological Distress, Parenting, and Socioemotional Development. Child Development. 1990;61(2):311–346. doi: 10.1111/j.1467-8624.1990.tb02781.x. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, Sze J, Marin T, Arevalo JMG, Doll R, et al. A genomic fingerprint of chronic stress in humans: Blunted glucocorticoid and increased NF-kB signaling. Biological Psychiatry. 2008;64:266–272. doi: 10.1016/j.biopsych.2008.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: Moving toward a model of behavioral and biological mechanisms. Psychological Bulletin. 2011;137:959–997. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Lachman ME, Chen E, Gruenewald TL, Karlamangla AS, Seeman TE. Pathways to resilience: Maternal nurturance as a buffer against the effects of childhood poverty on metabolic syndrome at midlife. Psychological Science. 2011;22(12):1591–1599. doi: 10.1177/0956797611419170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Cole SW. Clustering of depression and inflammation in adolescents previously exposed to childhood adversity. Biological Psychiatry. 2012;72(1):34–40. doi: 10.1016/j.biopsych.2012.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AH, Maletic V, Raison CL. Inflammation and its discontents: The role of cytokines in the pathophysiology of major depression. Biological Psychiatry. 2009;65:732–741. doi: 10.1016/j.biopsych.2008.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirowsky J. Analyzing associations between mental health and social circumstances. In: Aneshensel CS, Phelan JC, editors. Handbook of the sociology of mental health. New York, NY: Plenum; 1999. pp. 105–123. [Google Scholar]
- Moffitt TE the Klaus-Grawe 2012 Think Tank. Childhood exposure to violence and lifelong health: Clinical intervention science and stress biology research join forces. Development and Psychopathology. 2013;25(4 pt 2):1619–1634. doi: 10.1017/S0954579413000801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus version 7/04: Base program and combination add-on. Los Angeles, CA: Muthen & Muthen; 2015. [Google Scholar]
- Nunnally JC. Psychometric theory. New York, NY: McGraw-Hill; 1978. [Google Scholar]
- Osgood DW, Foster EM, Flanagan C, Ruth GR, editors. On Your Own without a Net: The Transition to Adulthood for Vulnerable Populations. Chicago: University of Chicago Press; 2005. [Google Scholar]
- Overbeek G, Vollebergh W, de Graaf R, Scholte R, de Kemp R, Engels R. Longitudinal associations of marital quality and marital dissolution with the incidence of DSM–III–R disorders. Journal of Family Psychology. 2006;20:284–291. doi: 10.1037/0893-3200.20.2.284. [DOI] [PubMed] [Google Scholar]
- Papakostas GI, Shelton RC, Kinrys G, Henry ME, Bakow BR, Lipkin SH, Pi B, Thurmond L, Bilello JA. Assessment of a multi-assay, serum-based biological diagnostic test for major depressive disorder: A Pilot and Replication Study. Molecular Psychiatry. 2011;18(3):332–9. doi: 10.1038/mp.2011.166. [DOI] [PubMed] [Google Scholar]
- Pasco JA, Moylan S, Allen NB, Stuart AL, Hayley AC, Byrne ML, Maes M. So depression is an inflammatory disease, but where does the inflammation come from? BMC Medicine. 2013;11:200. doi: 10.1186/1741-7015-11-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pendry P, Adam EK. Associations between parents’ marital functioning, maternal parenting quality, maternal emotion and child cortisol levels. International Journal of Behavioral Development. 2007;31(3):218–231. [Google Scholar]
- Phelan JC, Link BG. Is Racism a Fundamental Cause of Inequalities in Health? Annual Review of Sociology. 2015;41(1):311–330. doi: 10.1146/annurev-soc-073014-112305. [DOI] [Google Scholar]
- Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends in Immunology. 2006;27:24–31. doi: 10.1016/j.it.2005.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raison CL, Miller AH. When not enough is too much: The role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. American Journal of Psychiatry. 2003;160:1554–1565. doi: 10.1176/appi.ajp.160.9.1554. [DOI] [PubMed] [Google Scholar]
- Rickard IJ, Lummaa V. The predictive adaptive response and metabolic syndrome: challenges for the hypothesis. Trends in Endocrinology and Metabolism. 2007;18(3):94–99. doi: 10.1016/j.tem.2007.02.004. [DOI] [PubMed] [Google Scholar]
- Rohleder N, Marin TJ, Ma R, Miller GE. Biologic cost of caring for a cancer patient: Dysregulation of pro- and anti-inflammatory signaling pathways. Journal of Clinical Oncology. 2009;27:2909–2915. doi: 10.1200/JCO.2008.18.7435. [DOI] [PubMed] [Google Scholar]
- Schofield TJ, Conger RD, Gonzales JE, … Merrick MT. Harsh parenting, physical health, and the protective role of positive parent-adolescent relationships. Social Science & Medicine. 2016;157:18–26. doi: 10.1016/j.socscimed.2016.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott KM, Von Korff M, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, … Kessler RC. The association of childhood adversities and early onset mental disorders with adult onset chronic physical conditions. Archives of General Psychiatry. 2011;68(8):838–844. doi: 10.1001/archgenpsychiatry.2011.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons RL, Simons LG, Wallace LE. Families, delinquency and crime: Linking society’s most basic institution to antisocial behavior. New York, NY: Oxford University Press; 2004. [Google Scholar]
- Simons LG, Simons RL, Landor AM, Bryant CM, Beach SRH. Factors linking childhood experiences to adult romantic relationships among African Americans. Journal of Family Psychology. 2014;28(3):368–379. doi: 10.1037/a0036393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons RL, Lei MK, Bearch SRH, Philibert RA, Cutrona CE, Gibbons FX, Barr A. Economic hardship and biological weathering: The epigenetics of aging in a U.S. sample of black women. Social Science and Medicine. 2016;150:192–200. doi: 10.1016/j.socscimed.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons RL, Lei MK, Beach SRH, Barr AB, Simons LG, Gibbons FX, Philibert RA. Unpublished manuscript. University of Georgia; 2016. Discrimination, Segregation, and Chronic Inflammation: Testing the Weathering Explanation for the Poor Health of Black Americans. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Lewis TT, Gruenewald TL, Mujahid MS, Ryff CD, Albert MA, Williams DR. Early life adversity and inflammation in African Americans and whites in the midlife in the united states survey. Psychosomtic Medicine. 2010;72(7):694–701. doi: 10.1097/PSY.0b013e3181e9c16f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg SJ, Davila J. Adolescent romantic functioning and depression: The moderating role of parental emotional availability. Journal of Clinical Child and Adolescent Psychology. 2008;37:350–362. doi: 10.1080/15374410801955847. [DOI] [PubMed] [Google Scholar]
- Stock ML, Gibbons FX, Peterson LM, Gerrard M. The effects of racial discrimination on the HIV-risk cognitions and behaviors of black adolescents and young adults. Health Psychology. 2013;32(5):543. doi: 10.1037/a0028815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surjadi FF, Lorenz FO, Wickrama KAS, Conger RD. Parental support, partner support, and the trajectories of mastery from adolescence to early adulthood. Journal of Adolescence. 2011;34(4):619–628. doi: 10.1016/j.adolescence.2010.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor BD, Holzman CB, Fichorova RN, Tian Y, Jones NM, Fu W, Senagore PK. Inflammation biomarkers in vaginal fluid and preterm delivery. Human Reproduction. 2013;28(4):942–952. doi: 10.1093/humrep/det019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Kammen DP, McAllister-Sistilli CG, Kelley ME, Gurklis JA, Yao JK. Elevated interleukin-6 in schizophrenia. Psychiatry Research. 1999;87:129–136. doi: 10.1016/s0165-1781(99)00053-0. [DOI] [PubMed] [Google Scholar]
- Waldinger RJ, Schulz MS. The Long Reach of Nurturing Family Environments: Links With Midlife Emotion-Regulatory Styles and Late-Life Security in Intimate Relationships. Psychological Science. 2016;27(11):1443–1450. doi: 10.1177/0956797616661556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whisman MA, Bruce ML. Marital distress and incidence of major depressive episode in a community sample. Journal of Abnormal Psychology. 1999;108:674–678. doi: 10.1037//0021-843X.108.4.674. [DOI] [PubMed] [Google Scholar]
- Young JR. Underemployment in Urban and Rural America, 2005–2012. Carsey Institute; 2012. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.