Summary
Background
The aim of the study was to compare the mini-open to the classic open repair techniques for Achilles tendon ruptures.
Methods
We retrospectively evaluated at a minimum of 2 years follow-up 32 subcutaneous Achilles tendon ruptures; 17 underwent mini-open surgery (Group A) and 15 the open technique (Group B).
Results
No difference in Achilles Tendon Total Rupture Score and in modified Leppillahti score was observed. With respect to the contralateral side the width of the operated Achilles tendon was 4.07 mm thicker in Group A and 7.67 mm in Group B (p<.05); the calf circumference reduction was respectively 10 mm and 23.75 mm (p<.05). Iso-kinetic peak force measurement of the calf muscle strength showed a loss of 8.21% in Group A versus 17.25% in Group B (p <.05). The mean Patient Satisfaction Score was 96.76 in Group A and 88.67 in Group B (p<.01); respectively 82.3% vs 66.7% of patients were able to return to previous levels of sporting activity. There were two post-operative complications in Group B and one in Group A.
Conclusion
Mini-open technique minimizes the risk of complications, leads to an improved tendon healing process and functional recovery with higher patient satisfaction.
Level of evidence
IV.
Keywords: Achilles tendon, achilles tendon rupture, Achilles tendon repair, mini open technique, tenorrhaphy
Introduction
Subcutaneous rupture of Achilles tendon is a common lesion, accounting for approximately 35% of all tendon tears1 and for about 33.3% of foot traumas2. The prevalence is approximately 18 per 100,000 per year3 and the incidence has increased over the past decade, reflecting the greater prevalence of people who are involved in sports, with the highest incidence in men aged 30 to 50 years4. The left side is ruptured more commonly than the right side5. It is generally accepted that ruptures occurs in previously abnormal tendons6 and the mechanisms of injury include sudden forced plantar flexion of the foot, unexpected dorsiflexion of the foot, and violent dorsiflexion of a plantar flexed foot6. The appropriate treatment of acute complete Achilles tendon rupture remains controversial. The treatment choices include conservative management with casting and bracing7, open repair and percutaneous repair8,9. The main advantages of open repair over conservative management are decreased rates of re-rupture, less residual lengthening, less calf atrophy, better range of ankle movement and consequently resumption of a higher level of sporting activity and shorter time to return to work10. Maffulli et al. found increased clinical and functional outcomes after surgical repair compared to conservative treatment11. However, when conservative treatment included functional rehabilitation, it was equal to surgical treatment with regards to the incidence of re-rupture as reported by Zhang et al. in a recent systematic review of overlapping metanalyses12.
Nevertheless, surgical treatment is associated with an increased incidence of postoperative complications such as skin-tendon adhesions, infection, delayed healing of the surgical wound, sural nerve lesion, and suture granulomas13.
Percutaneous repair, first described by Ma and Griffith14, seems to bridge the gap by combining the advantages of both methods15,16. It is associated with a lower complication rate compared to open operative repair13 but it may be associated with a higher risk of re-rupture and sural nerve injury17.
However, several researchers have reported the absence of re-ruptures and nerve lesions4,18.
Percutaneous repair may not achieve satisfactory contact of the tendon stumps. Because of this, healing may be delayed and the original length of the tendon may not be accurately restored.
Therefore a minimally invasive surgery has been proposed by several Authors4,9, it allows precise visualisation and control the tendon ends while avoiding excessive dissection and disturbance of local vascularity, so minimizing nerve and wound healing problems.
In the literature, we could find only a few studies that compare the results of a minimally invasive technique to an open repair19. Moreover, to our knowledge, no previous study has compared the isokinetic evaluation in these two groups.
The aim of our study was to compare a minimally invasive repair to an open repair in terms of clinical-functional outcomes, and isokinetic measurement. Moreover we investigated the rate of re-rupture and development of complications, especially sensory disturbance and infections, between these two techniques of Achilles tendon repair. The hypothesis is that mini-open technique, thanks to the possibility of visualisation and control of the tendon ends and to the minor local vascular damage, has similar or better functional outcomes compared to open technique, avoiding extensive dissection, nerve and wound healing complications.
Materials and methods
A consecutive series of 32 traumatic subcutaneous acute Achilles tendon rupture in 29 patients, occurring between 2 and 8 cm proximal to the calcaneus tuberosity, were treated by the same team. In all cases, the diagnosis was based mainly on history and clinical examination (functional impairments, palpation of the gap, Thompson test) and confirmed by ultrasound examination.
Of the 32 subcutaneous acute Achilles tendon ruptures, 17 underwent mini-open surgery (Group A); and 15 underwent surgery with the open technique (Group B). The first 15 ruptures were treated with open repair consecutively and the last 17 were treated with the mini-open repair. Three patients had rupture of the Achilles tendon in both legs but at different times, therefore the first side involved was treated with open surgery and the second side with mini-open surgery. All patients were eligible and then enrolled because none had the following exclusion criteria:
previous operating procedures or history of partial or complete rupture of the involved tendon;
combination with lower limb fractures;
systemic therapies that may lead to a pathological condition in the interested ankle as immunosuppressive treatment and systemic steroids13,20;
previous local therapy that might have weakened the tendon (local infiltration of anaesthetics or steroids in the Achilles tendon region);
diabetes, neurovascular and/or neurological diseases.
The mean age was 47.18 years (SD ±11.83; range 29–66) in Group A and 44.53 years (SD ±10.03; range 34–72) in Group B.
In Group A 82.3% of patients were males (14 of 17) while in Group B 93.3% (14 of 15); the right side was affected in 41.2% of cases in Group A (7 of 17) and in 26.7% of cases in Group B (4 of 15).
In 70.6% of patients in Group A (12 of 17) and in 73.3% in Group B (11 of 15) the rupture occurred during athletic activities.
The two groups were comparable in terms of demographic and clinical variables such as age, gender, injured side, type of trauma and time to surgery (Tab. I). All patients were evaluated at 2-years follow-up (range 23–26 months). Ethical approval was obtained from the local ethical review board. The study meets the ethical standards required by MLTJ21.
Table I.
Groups homogeneity through analysis of age, gender, side of lesion, type of trauma and time before surgery. Age and time values are expressed as the mean ± SD. A p < 0.05 has been considered significant.
| Variable | Mini | Open | p value |
|---|---|---|---|
| Age (years) | 47.18 ± 11.83 | 44.53 ± 10.03 | 0.50 |
| Gender (M - F) | 82.3% M (14 - 3) | 93.3% M (14 - 1) | 0.349 |
| Side (right - left) | 41.2% right (7 - 10) | 26.7% right (4 - 11) | 0.388 |
| Type of trauma (athletic - nonathletic) | 70.6% athletic (12 - 5) | 73.3% athletic (11 - 4) | 0.666 |
| Time before surgery (days) | 4.71 ± 2.97 | 7.47 ± 13.66 | 0.422 |
Operative techniques
The patient was placed in a prone position under general, spinal or peripheral nerve block anesthesia with the knees slightly flexed and a pneumatic tourniquet placed around the proximal part of the thigh. Before starting the procedure, the rupture and the diastasis (gap) were localized.
Mini open technique
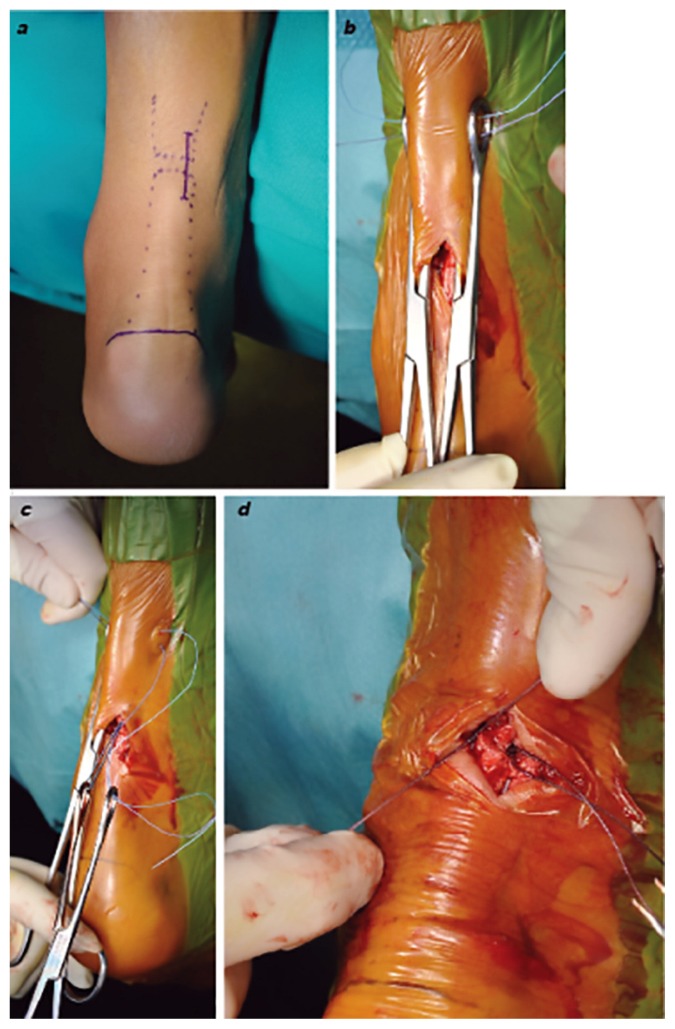
The mini open repair (Group A), using a modified Kakiuchi technique, started with a longitudinal medial paratendinous incision of 3.2 cm on average in length (Fig. 1a). The paratenon was incised and the proximal stump was identified.
Figure 1 a–d.
a) The longitudinal medial paratendinous skin incision used mini-open technique; b) two ring forceps are positioned between the paratenon and the proximal part of the Achilles tendon, and two no. 2 non-absorbable sutures are passed through the tendon, one more proximally and one more distally inside the ring of the forceps; c) withdrawing the two ring-forceps, the sutures are pulled back inside the surgical site; d) the tendon after the knots are tight, covering the knots with paratenon prevents contact with the fascia or subcutaneous tissues.
Pulling the proximal tendon stump with forceps, two ring-forceps were introduced with one branch under the fascia between the tendon and the paratenon and the other branch over the skin, one medially and one laterally. Careful positioning of the lateral forceps is necessary to avoid sural nerve injuries. Two no. 2 non-absorbable sutures (Ti-Cron Covidien®) were transversely passed through the proximal enlargement of the tendon, one more proximally and one more distally inside the ring of the forceps (Fig. 1b). The two ring-forceps were then slowly withdrawn. This maneuver resulted in the sutures sliding to a peritendinous position, and thus the tendon itself was the only tissue held by the sutures (Fig. 1c). Traction was applied to the two suture pairs to ensure that they were firmly anchored in the tendon, and they were individually clamped to avoid confusion.
The same maneuvers were performed in the distal stump. With the foot in the same equinus position of the uninjured side, the more proximal suture with the more distal suture and the less proximal with the less distal suture were tied (Fig. 1d). The knots in the sutures were covered with paratenon to prevent contact with the fascia or subcutaneous tissues and the cut ends of the paratenon and fascia were sutured in separate layers with absorbable sutures. Suturing of the skin was then performed.
Open technique
For the open repair a longitudinal midline incision of 9.4 cm on average in length was made preserving the lesser saphenous and sural nerve. The paratenon was carefully dissected and the rupture was identified. The tendon was repaired using the Krackow end-to-end method with no. 5 non absorbable suture (Ti-Cron Covidien ® Dub, Ireland) and a fine interrupted suture of the ends with an absorbable 2-0 suture (Safil Braun® Am Aesculap-Platz 78532 Tuttlingen). The paratenon was sutured with absorbable 2-0 and the cutis with a 2-0 interrupted suture.
Postoperative rehabilitation protocol
Different rehabilitation protocols are described in literature22, we used the same no-weight bearing protocol for both groups. A below-knee cast at 25° to 30° plantar flexion was maintained for 4 weeks. During the first 4 weeks, the patient was at rest without weight bearing. At the fifth week the cast was removed and replaced with a walker boot that allowed a range of motion from 0 to 30° plantar flexion. At the sixth week, partial load was permitted of up to 25 Kg and progressively up to full load. After 8 weeks, full load was reached and the orthosis was abandoned, a heel lift was maintained in patients’ shoes. A more intensive program of ankle motion, isometric, and proprioceptive exercises was then progressively instituted with raising on toes or heels allowed 12 weeks after the operation and full activities recommended 6 months after the surgery. Stretching of the calf muscle was avoided until 12 weeks post-op.
Clinical evaluation
Patients were recalled to the hospital for the 2-year follow up clinical assessment, and a battery of clinical and instrumental measures were performed. The clinical assessment included the measurement of the incision length and the differences in Achilles tendon width and calf circumference between operated and contralateral legs23. The Achilles Tendon Total Rupture Score (ATRS), the scoring method of Leppilahti and a modified scoring method of Leppilahti et al. were used. In the modified scoring method of Leppilhati, we combined the results of the isokinetic test with those of two functional tests (toe walk and heel walk) instead of using the isokinetic strength scoring scale alone for the item that can evaluate the muscle strength. An overall score of 90–100 rates as excellent, 75–85 is good, 60–70 is fair and less than 55 is poor. Furthermore, the ability to return to previous level of activity was investigated.
Isokinetic assessment
A blinded therapist unaware of the repair technique performed evaluated concentric plantar flexion and dorsiflexion peak forces registered by means of isokinetic dynamometer (Technogym® REV 7000 VX)24 with five successive cycles at an angular velocity of 30 °/s after 10 cycles of warm-up. All patients were verbally encouraged to achieve a maximal effort during testing. The percent difference in peak torque was calculated using unaffected side as reference. The percentage difference in peak torque values between the uninjured and injured sides was calculated for the plantar flexion and dorsiflexion of the ankle.
In patients with rupture of Achilles tendon of both legs the percentage difference in peak torque values was calculated by comparing the side treated with the open technique to the side treated with the mini-open technique.
Patients subjective outcomes
The Patient Satisfaction Score was used to quantify the subjective outcomes of both groups after surgery. Patients were asked to mark a line from 0 to 100 about how they felt and how good their recovery was, compared to what they expected.
Statistical analysis
All statistical tests were performed using SPSS Statistics V22.0. Primary outcome variables included: I) mean thickness difference between operated and contralateral Achilles tendons [mm]; II) calf circumference reduction of the operated with respect to contralateral leg [mm]; III) ATRS score; IV) average loss on isokinetic peak force of ankle plantar flexion (%), and V) ankle dorsi-flexion (%).
Outcome variables normality distribution was investigated using the Shapiro-Wilk Test. Since data normality was ascertained for all variables (i.e., p-value> 0.05), parametric tests were employed, and all data are presented as mean ± standard deviation. Outcome variables in the two groups were compared by means of independent samples t-tests. Since five t-tests were performed, i.e., one for each outcome variable, Bonferroni correction has been applied and p-values<0.01 were considered as significant (i.e., 0.05/5=0.01).
The Kruskal Wallis test for the comparison of ordinal variables was used to investigate group differences dealing with the results of Leppilahti score and Leppilahti modified score.
Results
Primary outcome measures such as tendon thickness differences, calf circumference reduction and isokinetic peak force of ankle plantar flexion proved to be statistically different for the two groups, whereas the ATRS score, and the ankle dorsi-flexion isokinetic peak force were not statistically different.
Clinical evaluation
The mean thickness difference between operated and contralateral Achilles tendons was 4.1 mm (SD± 0.8) in group A and 7.7 mm (SD± 3.7) in Group B(t-test p=.007) (Fig. 2A). The calf circumference reduction of the operated with respect to contralateral leg was −1.0 cm (SD± 0.59) in Group A and −2.4 cm (SD± 1.4) in Group B (t-test p=.006) (Fig. 2B). As expected, due to the used technique, incision length was statistically significantly shorter for Group A with respect to Group B, with a mean incision length of 33±6 mm and 94±29 mm respectively (t-test p-value<.001).
Figure 2 A–E.
Histograms representing means along standard deviation for the five principal outcomes. Black column represent the open technique group and grey columns represent the mini-open surgery group. ATRS, Achilles Tendon Total Rupture Score.
No significant difference could be detected using the ATRS score and the modified scoring method of Leppillahti.
The ATRS score was 92.71 (SD± 13.00; range 55–100) in Group A and 89.25 (SD± 12.89; range 59–100) in Group B (Fig. 2C). According to the modified scoring method of Leppillahti in Group A 47% (8 of 17) of patients were graded excellent, 35% (6 of 17) good, 18% (3 of 17) fair; in Group B 33% (5 of 15) of patients were graded excellent, 47% (7 of 15) good, 13% (2 of 15) fair and 7% (1 of 15) poor; the results using Kruskall Wallis test of the Leppilahti modified score of the two groups were not statistically significant.
A statistically significant difference was instead found using the Leppilahti score (Kruskall Wallis p-value< 0.001), indeed in Group A there were more excellent results than in Group B: in Group A there were 14 excellent results, while in group B there were only 2, the good results are respectively 2 vs 9 and the poor results were 1 vs 4.
The 82.3% (14 of 17) of patients in Group A and the 66.7% (10 of 15) in Group B were able to return to previous levels of activity or sport.
Isokinetic assessment
Isokinetic peak force measurement of ankle plantar flexion showed an average loss of 8.48 % (SD± 8.05) in Group A versus 16.63 % (SD± 8.75) in Group B of the calf muscle strength compared to the normal side with a statistically significant difference in favour of group A (t-test p =.022) (Fig. 2D). The isokinetic peak force measurement of ankle dorsiflexion was on average reduced by 5.70% (SD± 13.19) in Group A versus 6.60% (SD± 12.35) in Group B of the tibialis anterior compared to the normal side (Fig. 2E); in this case with the numbers available, no significant difference could be detected (t-test p=0.860).
Isokinetic tests in bilateral rupture were analyzed separately. The peak force measurement of ankle dorsiflexion was on average reduced by 11.7% in the Achilles tendon treated with Open technique compared to Mini-open one. The peak force measurement of ankle plantar flexion showed an average loss of 16.47% in the tendon treated with Open technique compared to the Mini-open one.
Subjective outcome
A statistically significant difference was found in Patient Satisfaction Score between the two groups: 96.76 in Group A (range, 90–100) and 88.67 in Group B (range, 60–100) (t-test p=0.016).
Complications
In Group A there was 1 patient (6%) who had a late heel ulcer secondary to boot wear; in Group B there were 3 patients (20%) who had complications: there was one deep infection which required irrigation and debridement, one superficial infection treated with antibiotic therapy and one sural nerve lesion.
Discussion
Subcutaneous rupture of Achilles tendon is a frequent lesion but, despite its high incidence, the optimal management of Achilles tendon ruptures remains a topic of active debate25: in fact, open operative treatment of acute Achilles tendon ruptures reduces the risk of re-rupture compared to non-operative treatment (3.5 vs 12.6%; RR 0.27) but has the drawback of a significantly higher risk of other complications (34.1 vs 2.7%; RR 10.60), including wound infection26. These complications may be reduced by performing surgery percutaneously27, however, re-rupture, tendon elongation, and sural nerve entrapment are all reported complications in percutaneous repair 28; while Miniopen surgery methods provide satisfactory exposure of the rupture without markedly compromising the circulation29.
Our study shows a statistically significant superiority of the mini open technique compared to the open one in terms of clinical evaluation (calf circumference, tendon width and Leppillathi score), instrumental measurement (isokinetic peak force measurement of ankle plantar flexion) and subjective outcome.
In particular, we treated a sub group of the three patients with bilateral rupture of Achilles tendon with the two different techniques. In these cases a direct evaluation between the two techniques could be done on the same patient. Measuring objective parameters, it’s important to see that difference in isokinetic peak force of calf muscle and of tibialis anterior strength could be found in favor of mini-open technique. These results are very important because a lot of previous studies show a permanent plantar flexion deficit after Achilles tendon rupture30,31.
Bressel et al.32 found a reduction of 17% in maximal voluntary plantar flexor torque of the involved side compared to the uninvolved. This difference continued in time, also after two years as found by Möller et al.33. The inferior material properties of a scarred Achilles tendon may influence the more global structural properties of the intact muscle tendon unit. A disorganized tissue arrangement34 and an increased content of type III rather than type I collagen35 in the repaired tendon after long-term healing influences the stiffness, strength and viscoelastic behaviour of tendon36.
Moreover as peak torque generated by a muscle is closely related to its cross-sectional area37, the difference reported between limbs and between the two groups may be related to the differences found in calf circumference. Although circumference measurements may give insight into the cross-sectional area of a muscle group, the relative amount of bone, fat and muscle cannot be discerned and therefore this should be interpreted with caution.
Tendon width and maximum calf circumference are among the most studied parameters after Achilles tendon rupture. Previous studies found permanent calf muscle atrophy and increased tendon width after Achilles tendon rupture38. Bressel et al.32 found a reduction of 5% in calf circumference of the involved side compared to the uninvolved.
There are also better outcomes in ATRS score, in Leppillathi modified score and in returning to previous sporting level but due to the limited number of patients a statistically significant difference was not found. Minor incidence of complications was found in group A and in particular there were no sural nerve lesions or deep infections. Also Tejwani et al.26 found in their study statistically significant differences in terms of wound complication and nerve injury rates in favour of mini open technique.
Vadalà et al.39 and Keller et al.40 found good outcomes using two different mini-open techniques that can be considered similar to ours and these results are encouraging us to go on with our technique instead of a conventional open approach.
Klein et al.19 have recently made a retrospective study comparing an open technique and a mini open technique to treat Achilles ruptures: it shows a shorter time between surgical intervention and full return to activity in patients treated with mini open technique.
The relatively limited sample size of the two groups has to be considered a limit in particular concerning the results of ATRS score, the modified scoring method of Leppillahti, where better outcomes are found in mini-open group, but a statistically significant difference couldn’t be proven. Moreover in our retrospective study the lack of a nonsurgical group should be considered another important limit also considering recent interesting results with conservative treatment in Achilles tendon rupture41.
Finally, another limit of the study is the retrospective design, indeed the tendon size and calf circumference before injury are lacking. Further prospective studies are required to confirm our findings. However this is the first study to compare isokinetic assessment in Achilles rupture treated with open technique vs mini-open technique.
Conclusion
Considering our experience, the mini-open technique compared to open surgery has obtained better results in terms of tendon width (p<.05), muscle mass and strength recovery of plantarflexion (p<.05) and patient satisfaction (p<.01). No differences were found in terms of clinical outcomes.
Acknowledgements
The Authors thank Dr. Marta Gandolla for his assistance with statistical analysis and manuscript review. The Authors declare that they have no conflict of interest or funding.
References
- 1.Józsa L, Kvist M, Bálint BJ, Reffy A, Järvinen M, Lehto M, et al. The role of recreational sport activity in Achilles tendon rupture. A clinical, pathoanatomical, and sociological study of 292 cases. Am J Sports Med [Internet] 2016 Sep 27;17(3):338–343. doi: 10.1177/036354658901700305. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2729483. [DOI] [PubMed] [Google Scholar]
- 2.Wicks MH, Harbison JS, Paterson DC. Tendon injuries about the foot and ankle in children. Aust N Z J Surg [Internet] 2016 Sep 27;50(2):158–161. doi: 10.1111/j.1445-2197.1980.tb06656.x. 1980 Apr. Available from: http://www.ncbi.nlm.nih.gov/pubmed/6930233. [DOI] [PubMed] [Google Scholar]
- 3.Leppilahti J, Puranen J, Orava S. Incidence of Achilles tendon rupture. Acta Orthop Scand [Internet] 2016 Sep 27;67(3):277–279. doi: 10.3109/17453679608994688. 1996 Jun. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8686468. [DOI] [PubMed] [Google Scholar]
- 4.Assal M, Jung M, Stern R, Rippstein P, Delmi M, Hoffmeyer P. Limited open repair of Achilles tendon ruptures: a technique with a new instrument and findings of a prospective multicenter study. J Bone Joint Surg Am [Internet] 2016 Sep 27;84-A(2):161–170. 2002 Feb. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11861720. [PubMed] [Google Scholar]
- 5.Hattrup SJ, Johnson KA. A review of ruptures of the Achilles tendon. Foot Ankle [Internet] 2016 Sep 27;6(1):34–38. doi: 10.1177/107110078500600107. 1985 Aug. Available from: http://www.ncbi.nlm.nih.gov/pubmed/3899877. [DOI] [PubMed] [Google Scholar]
- 6.Arner O, Lindholm A. Subcutaneous rupture of the Achilles tendon; a study of 92 cases. Acta Chir Scand Suppl [Internet] 2016 Sep 27;116(Supp 239):1–51. 1959. Available from: http://www.ncbi.nlm.nih.gov/pubmed/13660721. [PubMed] [Google Scholar]
- 7.Weber M, Niemann M, Lanz R, Müller T. Nonoperative treatment of acute rupture of the achilles tendon: results of a new protocol and comparison with operative treatment. Am J Sports Med [Internet] 2017 Jun 2;31(5):685–691. doi: 10.1177/03635465030310050901. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12975187. [DOI] [PubMed] [Google Scholar]
- 8.Amlang MH, Christiani P, Heinz P, Zwipp H. [Percutaneous technique for Achilles tendon repair with the Dresden Instruments]. Unfallchirurg. 2005;108(7):529–536. doi: 10.1007/s00113-005-0938-8. [DOI] [PubMed] [Google Scholar]
- 9.Kakiuchi M. A combined open and percutaneous technique for repair of tendo Achillis. Comparison with open repair. J Bone Joint Surg Br [Internet] 2016 Sep 27;77(1):60–63. 1995 Jan. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7822398. [PubMed] [Google Scholar]
- 10.Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. Surgical Versus Nonsurgical Treatment of Acute Achilles Tendon Rupture. J Bone Jt Surgery-American Vol [Internet] 2017 Mar 30;94(23):2136–2143. doi: 10.2106/JBJS.K.00917. 2012 Dec 5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23224384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maffulli G, Buono AD, Richards P, Oliva F, Maffulli N. Conservative, minimally invasive and open surgical repair for management of acute ruptures of the Achilles tendon: a clinical and functional retrospective study. Muscle, Ligaments Tendons J [Internet] 2017 May 27;7(1):46–52. doi: 10.11138/mltj/2017.7.1.046. Available from: http://www.mltj.org/index.php?PAGE=articolo_dett&ID_ISSUE=950&id_article=8048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang H, Tang H, He Q, Wei Q, Tong D, Wang C, et al. Surgical Versus Conservative Intervention for Acute Achilles Tendon Rupture: A PRISMA-Compliant Systematic Review of Overlapping Meta-Analyses. Medicine (Baltimore) [Internet] 2017 Mar 30;94(45):e1951. doi: 10.1097/MD.0000000000001951. 2015 Nov. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00005792-201511110-00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chiodo CP, Wilson MG. Current concepts review: acute ruptures of the achilles tendon. Foot ankle Int [Internet] 2016 Sep 27;27(4):305–313. doi: 10.1177/107110070602700415. 2006 Apr. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16624224. [DOI] [PubMed] [Google Scholar]
- 14.Ma GW, Griffith TG. Percutaneous repair of acute closed ruptured achilles tendon: a new technique. Clin Orthop Relat Res [Internet] 2016. Sep 27, pp. 247–255. 1977 Oct. Available from: http://www.ncbi.nlm.nih.gov/pubmed/340096. [PubMed]
- 15.Maffulli N, Longo UG, Oliva F, Ronga M, Denaro V. Minimally Invasive Surgery of the Achilles Tendon. Orthop Clin North Am [Internet] 2017 Jul 15;40(4):491–498. doi: 10.1016/j.ocl.2009.05.006. 2009 Oct. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0030589809000376. [DOI] [PubMed] [Google Scholar]
- 16.McClelland D, Maffulli N. Percutaneous repair of ruptured Achilles tendon. J R Coll Surg Edinb [Internet] 2017 Jul 15;47(4):613–618. 2002 Aug. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12363186. [PubMed] [Google Scholar]
- 17.Wong J, Barrass V, Maffulli N. Quantitative review of operative and nonoperative management of achilles tendon ruptures. Am J Sports Med [Internet] 2016 Sep 27;30(4):565–575. doi: 10.1177/03635465020300041701. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12130412. [DOI] [PubMed] [Google Scholar]
- 18.Hockenbury RT, Johns JC. A biomechanical in vitro comparison of open versus percutaneous repair of tendon Achilles. Foot Ankle [Internet] 2016 Sep 27;11(2):67–72. doi: 10.1177/107110079001100202. 1990 Oct. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2265811. [DOI] [PubMed] [Google Scholar]
- 19.Klein EE, Weil L, Baker JR, Weil LS, Sung W, Knight J. Retrospective analysis of mini-open repair versus open repair for acute Achilles tendon ruptures. Foot Ankle Spec [Internet] 2016 Sep 27;6(1):15–20. doi: 10.1177/1938640012463052. 2013 Feb. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23064474. [DOI] [PubMed] [Google Scholar]
- 20.Turati M, Glard Y, Afonso D, Griffet J, Bigoni M. Osteochondral alteration in a child treated with levetiracetam: A rare case of juvenile osteochondritis dissecans of the talar head. J Pediatr Orthop Part B. 2017;26(2) doi: 10.1097/BPB.0000000000000354. [DOI] [PubMed] [Google Scholar]
- 21.Padulo J, Oliva F, Frizziero A, Maffulli N. Muscles, Ligaments and Tendons Journal - Basic principles and recommendations in clinical and field science research: 2016 update. MLTJ. 2016;6(1):1–5. doi: 10.11138/mltj/2016.6.1.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maffulli N, Tallon C, Wong J, Lim KP, Bleakney R. Early weightbearing and ankle mobilization after open repair of acute midsubstance tears of the achilles tendon. Am J Sports Med [Internet] 2017 Jul 15;31(5):692–700. doi: 10.1177/03635465030310051001. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12975188. [DOI] [PubMed] [Google Scholar]
- 23.Todorov A, Schaub F, Blanke F, Heisterbach P, Sachser F, Gösele A, et al. Clinical assessment is sufficient to allow outcome evaluation following surgical management of Achilles tendon ruptures. Muscles Ligaments Tendons J [Internet] 2017 Jul 15;5(2):68–72. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26261784. [PMC free article] [PubMed] [Google Scholar]
- 24.Bigoni M, Gorla M, Guerrasio S, Brignoli A, Cossio A, Grillo P, et al. Shoulder evaluation with isokinetic strength testing after arthroscopic rotator cuff repairs. J Shoulder Elbow Surg [Internet] 2016 Oct 6;18(2):178–183. doi: 10.1016/j.jse.2008.09.002. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19111477. [DOI] [PubMed] [Google Scholar]
- 25.Freedman BR, Gordon JA, Soslowsky LJ. The Achilles tendon: fundamental properties and mechanisms governing healing. Muscles Ligaments Tendons J [Internet] 2017 Jul 15;4(2):245–255. 2014 Apr. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25332943. [PMC free article] [PubMed] [Google Scholar]
- 26.Tejwani NC, Lee J, Weatherall J, Sherman O. Acute achilles tendon ruptures: a comparison of minimally invasive and open approach repairs followed by early rehabilitation. Am J Orthop (Belle Mead NJ) [Internet] 2016 Sep 27;43(10):E221–225. 2014 Oct. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25303448. [PubMed] [Google Scholar]
- 27.Khan RJK, Fick D, Keogh A, Crawford J, Brammar T, Parker M. Treatment of acute achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am [Internet] 2016 Sep 27;87(10):2202–2210. doi: 10.2106/JBJS.D.03049. 2005 Oct. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16203884. [DOI] [PubMed] [Google Scholar]
- 28.Cetti R, Christensen SE, Ejsted R, Jensen NM, Jorgensen U. Operative versus nonoperative treatment of Achilles tendon rupture. A prospective randomized study and review of the literature. Am J Sports Med [Internet] 2016 Sep 27;21(6):791–799. doi: 10.1177/036354659302100606. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8291628. [DOI] [PubMed] [Google Scholar]
- 29.Mukundan C, El Husseiny M, Rayan F, Salim J, Budgen A. “Mini-open” repair of acute tendo Achilles ruptures-the solution? Foot Ankle Surg [Internet] 2016 Sep 27;16(3):122–125. doi: 10.1016/j.fas.2009.07.005. 2010 Sep. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20655011. [DOI] [PubMed] [Google Scholar]
- 30.Jacobs D, Martens M, Van Audekercke R, Mulier JC, Mulier F. Comparison of conservative and operative treatment of Achilles tendon rupture. Am J Sports Med [Internet] 2016 Sep 27;6(3):107–111. doi: 10.1177/036354657800600302. Available from: http://www.ncbi.nlm.nih.gov/pubmed/655329. [DOI] [PubMed] [Google Scholar]
- 31.Cetti R, Henriksen LO, Jacobsen KS. A new treatment of ruptured Achilles tendons. A prospective randomized study. Clin Orthop Relat Res [Internet] 2016. Sep 27, pp. 155–165. 1994 Nov. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7955677. [PubMed]
- 32.Bressel E, McNair PJ. Biomechanical behavior of the plantar flexor muscle-tendon unit after an Achilles tendon rupture. Am J Sports Med [Internet] 2016 Sep 27;29(3):321–326. doi: 10.1177/03635465010290031201. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11394603. [DOI] [PubMed] [Google Scholar]
- 33.Möller M, Lind K, Movin T, Karlsson J. Calf muscle function after Achilles tendon rupture. A prospective, randomised study comparing surgical and non-surgical treatment. Scand J Med Sci Sports [Internet] 2016 Sep 27;12(1):9–16. doi: 10.1034/j.1600-0838.2002.120103.x. 2002 Feb. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11985760. [DOI] [PubMed] [Google Scholar]
- 34.Best TM, Collins A, Lilly EG, Seaber AV, Goldner R, Murrell GA. Achilles tendon healing: a correlation between functional and mechanical performance in the rat. J Orthop Res [Internet] 2016 Sep 27;11(6):897–906. doi: 10.1002/jor.1100110617. 1993 Nov. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8283336. [DOI] [PubMed] [Google Scholar]
- 35.Russell JE, Manske PR. Collagen synthesis during primate flexor tendon repair in vitro. J Orthop Res [Internet] 2016 Sep 27;8(1):13–20. doi: 10.1002/jor.1100080103. 1990 Jan. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2293627. [DOI] [PubMed] [Google Scholar]
- 36.Liu SH, Yang RS, al-Shaikh R, Lane JM. Collagen in tendon, ligament, and bone healing. A current review. Clin Orthop Relat Res [Internet] 2016. Sep 27, pp. 265–278. 1995 Sep. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7671527. [PubMed]
- 37.Wickiewicz TL, Roy RR, Powell PL, Edgerton VR. Muscle architecture of the human lower limb. Clin Orthop Relat Res [Internet] 2016. Sep 27, pp. 275–283. 1983 Oct. Available from: http://www.ncbi.nlm.nih.gov/pubmed/6617027. [PubMed]
- 38.Wredmark T, Carlstedt C. Tendon elongation and muscle function after repair of Achilles tendon rupture. J Med Sci … [Internet] 2016 Sep 2; 1992. Available from: http://onlinelibrary.wiley.com/doi/10.1111/j.1600-0838.1992.tb00334.x/abstract. [Google Scholar]
- 39.Vadalà A, Lanzetti RM, Ciompi A, Rossi C, Lupariello D, Ferretti A. Functional evaluation of professional athletes treated with a mini-open technique for achilles tendon rupture. Muscles Ligaments Tendons J [Internet] 2016 Sep 27;4(2):177–181. 2014 Apr. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25332932. [PMC free article] [PubMed] [Google Scholar]
- 40.Keller A, Ortiz C, Wagner E, Wagner P, Mococain P. Mini-open tenorrhaphy of acute Achilles tendon ruptures: medium-term follow-up of 100 cases. Am J Sports Med [Internet] 2016 Sep 27;42(3):731–736. doi: 10.1177/0363546513511418. 2014 Mar. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24318611. [DOI] [PubMed] [Google Scholar]
- 41.Olsson N, Silbernagel KG, Eriksson BI, Sansone M, Brorsson A, Nilsson-Helander K, et al. Stable surgical repair with accelerated rehabilitation versus nonsurgical treatment for acute Achilles tendon ruptures: a randomized controlled study. Am J Sports Med [Internet] 2017 Mar 30;41(12):2867–2876. doi: 10.1177/0363546513503282. 2013 Dec. Available from: http://journals.sagepub.com/doi/10.1177/0363546513503282. [DOI] [PubMed] [Google Scholar]