Summary
Background
Semitendinosus (ST) is widely used autograft in anterior cruciate ligament reconstructions (ACLR). Although tendon harvesting is a common procedure, some patients exhibit pain, cramping and dysfunctional at posterior thigh after the ACLR. The formation of the newly regenerated neotendon could be compromised by a new injury or too rapid rehabilitation. We present this clinical entity and the developed surgical technique and share our experience in treatment of these patients.
Methods
Ten patients underwent operation where the harvested, retracted and loose muscle (9 ST, 1 gracilis) was reattached again. The delay to the diagnosis and the outcome of the procedure were recorded. Cases were followed and magnetic resonance images (MRI) were included from 2 cases for the demonstration of postoperative healing.
Results
Six ST and the gracilis patients with prolonged symptoms had good results and returned to their normal activity level. Preoperative MRI showed increased signal intensity and edema of the harvested and retracted muscles as the sign of compromised healing of the neotendon. Postoperatively, these MRI findings were resolved.
Conclusions
In high activity level patients with chronic posterior thigh pain and cramping of the harvested muscle, the stabilization procedure of the poorly healed muscle belly could lead to beneficial outcome.
Level of evidence
IV. Case series.
Keywords: ACL reconstruction, hamstring, operative treatment, posterior thigh pain, tendon harvesting
Introduction
Anterior cruciate ligament reconstruction (ACLR) is a common operation1, where the semitendinosus (ST) tendon is widely used as an autogenous graft for the replacement of the torn ACL1, 2. The ST is known to regenerate relatively well after the harvesting, forming a so called neotendon3. However, sometimes the regeneration process of the neotendon is disturbed which causes pain, weakness and cramping to the posterior thigh4–9. The reasons for the compromised healing of the neotendon are not well described in the literature earlier, although the cause for chronic posterior thigh pain might be too early started and rapid progression in postoperative physiotherapy or a new injury to the posterior thigh after harvesting10. The tendon pathology can be seen using magnetic resonance imaging (MRI)11.
To our knowledge, no reports of operative treatment for posterior thigh pain after hamstring tendon harvest have been previously published. The main purpose of this study is to present this clinical entity and the developed surgical technique solving the problem with our experience in treatment of these patients.
Patients and methods
Altogether ten athletes (7 males and 3 females), who had experienced an injury to the harvested hamstring site after an ACLR, underwent the operative treatment (Tab. I). Before the operation, all the patients experienced pain, had a dysfunctional posterior thigh and were not able to rehabilitate the hamstring area. The clinical diagnosis was supported by T2-weighted MRI (excluding 2 of the cases with operative indication of cramping and painful clinical condition) and the preoperative findings were confirmed during the operation as a poorly regenerated neotendons as well as retracted ST (Fig. 1) and gracilis (Fig. 2) muscles. Also, patients were not able to participate in sports due to the posterior thigh pain preoperatively. Characteristics of the patients and the delay from injury to surgery are presented in Table I. Two MRI case examples were obtained to demonstrate the increased signal and edema of the harvested muscle (Fig. 3), the retraction of the harvested muscle after successful ACLR (Fig. 4) and disturbed regeneration of gracilis neotendon (Fig. 5), respectively. Two patients underwent peak torque force testing (Dcom 900, Diter Oy, Kaarina, Finland) during the rehabilitation. The study data was gathered retrospectively with informed consent from the patients as well as carried out according to international ethical and scientific standards with acceptance of local ethical committee12.
Table I.
The basic characteristics of the patients undergoing the reattachment of the harvested muscle including the subjective results of the procedure.
| Cases (n.) | Sex | Age (years) | Injured side | Sports | Delay from the injury to the reattachment | Muscle | Result |
|---|---|---|---|---|---|---|---|
| 1.*† | Female | 18 | Right | Javelin | 2 months | ST | Good |
| 2. | Female | 24 | Right | Horse riding | 14 months | ST | Good |
| 3. | Male | 25 | Left | Running | 7 months | ST | Fair |
| 4. † | Female | 25 | Left | Football | 3 weeks | ST | Good |
| 5. | Male | 27 | Right | Football | 6 months | ST | Good |
| 6. | Male | 28 | Left | Football | 18 months | ST | Poor |
| 7. | Male | 32 | Right | Floorball | 10 years | ST | Good |
| 8. | Male | 33 | Left | Floorball | 5 months | ST | Good |
| 9. | Male | 35 | Right | Football | 10 months | ST | Poor |
| 10.** | Male | 27 | Right | Ice hockey | 36 months | gracilis | Good |
A case example. MR images showing pre- and postoperative changes of the harvested ST with control MR image from an asymptomatic control (Figures 3 and 4).
A case example. The peek torque forces of the hamstrings after the reattachment of harvested ST were recorded.
A case example. MR images showing preoperative changes of the harvested gracilis (Figure 5).
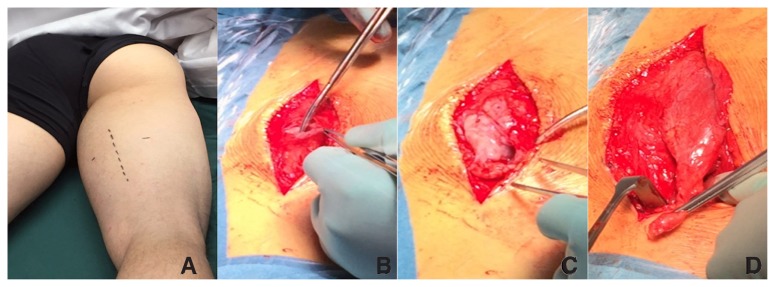
Figure 1 A–D.
Perioperative images showing: A) the line of skin incision; B) vertical fasciotomy to identify cramping and painful ST muscle belly seen on MRI; C) proximal stump of the rectracted ST with notably pathological musculature; D) debrided ST muscle belly drawn towards its original place
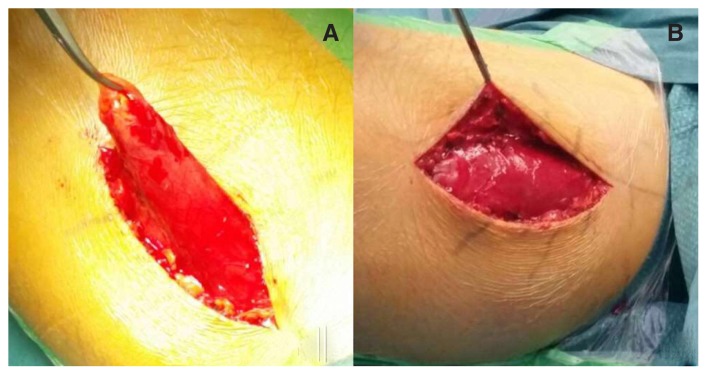
Figure 2 A, B.
A) Intraoperative images demonstrating harvested and retracted gracilis muscle belly without proper neotendon; B). The gracilis muscle has been tightened and sutured to the nearby adductors.
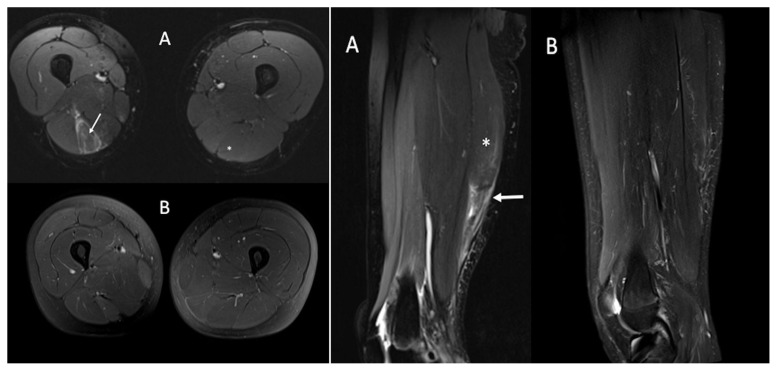
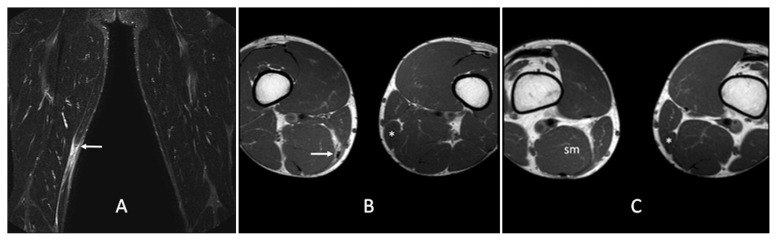
Figure 3 A, B.
A) Axial MR images show clear preoperative edema compared to contralateral side around the harvested semitendinosus (white arrow) indicating poorly recovered and retracted muscle belly (*); B) The muscle edema has resolved after operative treatment.
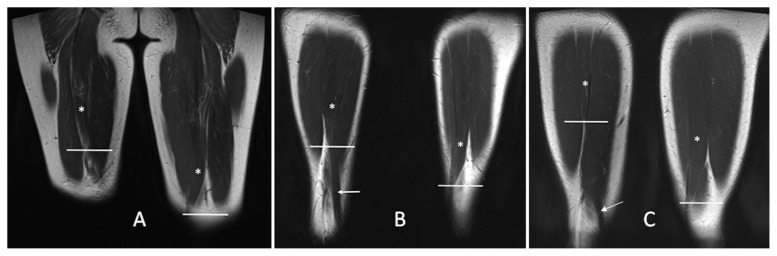
Figure 4 A–C.
The ST muscle rectraction compared between ACLR patients with one who had posterior thigh pain (preoperative coronal MR image, A) and asymptomatic random controls (B, C). The lines mark the end of semitendinosus muscles (*). The white arrows (B, C) demonstrate regenerated ST neotendons. Notably, the rectration of the muscle belly seems apparent in both groups compared to the unoperated side: 107mm (A), 47mm (B) and 62mm (C).
Figure 5.
Poorly recovered gracilis muscle after autograft harvesting. A) Coronal MR image of the thighs. The arrow marks the end of retracted gracilis muscle belly; B) At upper level the retracted gracilis muscle is visible in axial MR images (arrow); C) More distally the muscle is absent from the medial side of the semimembranousus muscle (sm). On the contralateral side normal gracilis muscle is seen (*).
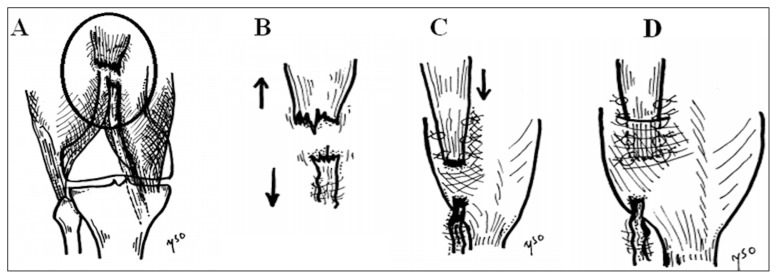
Surgical technique
In surgery, the patient was positioned prone, and a pillow was placed under the foot to hold the knee in a slight 10 to 15° flexion. A vertical incision was done over the preoperatively marked injured area. Usually, the retracted and painful ST muscle belly is quite easily palpated when the patient flexes the knee against resistance. A fasciotomy was first done in a line of skin incision. After the fasciotomy, the harvested ST was identified. The distal head of ST muscle was carefully liberated from adhesions and pulled towards its original insertion. When the tonus of the retracted ST was restored back near to normal, it was attached to the underneath located semimembranosus muscle. However, it is important to avoid over-tightening the semitendinosus in the process, which can be evaluated by knee extension-flexion movements and measuring the amount of retraction from preoperative MRIs. The symptomatic harvested gracilis muscle was operated using the same principles. The surgical technique is shown in Figures 1 and 2 as well as illustrated in Figure 6.
Figure 6.
Schematic drawing of the surgical technique. The poorly regenerated neotendon (A) is visualized in MRI. The extent of the retraction varies (B). The distal head of the harvested ST muscle belly is drawn towards its anatomical place and sutured to the SM (C). Alternatively, the harvested ST muscle can be stabilized by embedding it into the SM muscle itself (D).
Rehabilitation
The rehabilitation program after the operation was similar to the protocol after primary ACLR which highlights the progressive recovery to full knee function taking the hamstring donor site in consideration10. After the operation, the patient was allowed to start light walking, first with the help of crutches. After one to two weeks, full weight bearing was allowed. Active stretching of the hamstrings was avoided for four to six weeks. Light aqua training was started after three weeks and stationary bike training after three to four weeks. Light running was commenced eight weeks after the surgery. Heavier strength training was started gradually in the guidance of physiotherapist according to the patient’s progress, normally after two months from the operation.
Results
The patients and the outcomes of the surgery are listed in Table I. The outcome was rated good in 7 patients (ST n=6; gracilis=1). The median age of the patients was 27 years. The patients with good results were either asymptomatic or suffered only mild symptoms after the rehabilitation, and they could return to their pre-injury level of sports in 3–4 months. One athlete rated as a fair outcome had mild pain and discomfort after the rehabilitation. Two patients were evaluated as poor outcome due to pain and weakness during sports still after the rehabilitation. One of them ended up in a second operation at six months after the first one (Patient no. 6). The median delay from injury to surgery in ST patients with good results was 5.5 months. The patients with inferior outcomes were operated at 7, 10 and 18 months from the initial injury of the posterior thigh, respectively. In the case examples, MRI showed poorly regenerated ST (Fig. 3A) and gracilis (Fig. 5) neotendon after a successful ACLR. After the operation, the increased signal was disappeared (Fig. 3B).
In Patient no. 1 and 4, the peak torque forces were determined and were compared to the unoperated contralateral side 9-months postoperatively in both cases. In patient 1, the operated right side showed a flexion deficit (79%) while the peak force in extension was 102% and the ratio of flexion/extension strength was 78%. Despite of the inferior flexion strength compared to the unoperated side, the patient’s operated posterior thigh was painless and functioning well. In patient 4, the strength of the operated left side was improved equal to the unoperated right side after 9-month rehabilitation.
Discussion
A posterior thigh pain could be a troublesome adverse event to an athlete recovering from successful ACLR. In the present case-series, we demonstrate that the retracted, cramping and painful harvested muscle can be seen in MRI as increased signal and muscle edema, whereas Tadokoro et al. previously showed the actual retraction of the harvested muscle3. The posterior thigh pain seems to be more associated with an abnormal function of the loose and unstable harvested ST muscle, which can be operated by stabilizing the muscle belly for better function and especially pain-free motion. In addition, this poorly recovered muscle belly can be visualized as increased signal and edema in MRI.
Based on the recent systematic review by Suijkerbuijk et al., the regeneration of hamstring neotendon remains unclear13. Although the ACLR done with hamstring autograft is a common procedure, and the muscle morphology of ST seems to recover after the harvesting14, the failed regeneration of neotendon during rehabilitation is poorly recognized. Our case examples exhibit early phase postoperative hamstring pain, in which the regeneration process of the neotendon was disturbed during the rehabilitation of ACLR by an early traumatic injury or too early started hamstring rehabilitation, thus impairing the regeneration process of the neotendon. Interestingly, we reattached one gracilis muscle belly at the time of 36-months after initial injury of the neotendon. The gracilis muscle belly had the same cramping and chronic pain symptoms during sports activities. The reattachment of the gracilis muscle belly to adductors resolved the symptoms of the patient and the overall outcome of the surgery was good.
Despite of the good regeneration rate, there are several possible morbidities, such as muscle atrophy, impaired muscle strength and restricted deep knee flexion associated with hamstring tendon harvesting4. Previously the posterior thigh pain after hamstring autograft harvest has been associated with the retraction of the harvested muscle based on computed tomography findings3. The MR images, which were obtained before and after the surgery when the patients exhibit resolution of symptoms and have returned to their pre-activity level, showed clear decline in signal and edema around the harvested muscle belly with beneficial patient outcome. Therefore, based on this case-series, more attention should be given to the reattachment and the stabilization procedure of the poorly regenerated neotendon and the harvested muscle to secure it from harmful motion which could generate clinical symptoms and muscle pathologies seen on MRI11.
The ST tendon is known to regenerate on average in 6–12 months after surgery, forming a neotendon, which resembles the native tendon9,15,16. The regeneration of the neotendon is crucial for stabilizing the muscle belly and recovering the function of the harvested muscle. The ST muscle may retract towards its origin which usually happens in early phase after surgery17. Based on Authors clinical experience, the extent of the muscle retraction might correlate with the symptoms. Smaller retractions seem to be relatively common even in asymptomatic patients, but in patients with more severe retractions, symptoms could begin to occur. Based on our clinical experience, the higher retraction of harvested muscle seems to associate with disturbed neotendon regeneration and leading to an unstable muscle belly (Fig. 4). An early trauma during rehabilitation could commence more retraction to the harvested muscle itself.
The decision making for surgical treatment could be challenging. Earlier Lempainen et al. have shown that after rapid diagnosis of the complete tears in the distal parts of the ST, high level athletes could Return - to - Play in 5 months6. Therefore, we presume that athletes could also benefit from the reattachment of the retracted and symptomatic muscle when the conservative treatment seems to be insufficient. The Authors recommendation is that the surgical treatment should be considered for a typical patient, who suffers from severe pain as well as a loss of hamstring muscle function. These patients are usually athletes, who will most likely benefit from trying to restore the muscle function as close to normal and as early as possible. In clinical practice, we have started the gradual hamstring trainings at 2-months after ACLR with good results. The limitations of this study include the relatively small number of patients and a lack of comparison group. Also, the population in this study were active professional or recreational athletes, thus very committed to follow the instructions and treatment plan after surgery and not representative of common population.
This is the first published study focusing on the surgical treatment of the posterior thigh pain after a successful ACLR. The main findings of this study were that the recovery after the stabilization of harvested muscle is often good and most of the patients could return to their pre-injury level of sports. In conclusion, the surgical reattachment of the retracted muscle belly could lead to overall good results and a near-tonormal muscle function can be expected.
Footnotes
Conflicts of interest
The Authors declare no conflicts of interest for this study.
References
- 1.Shaerf DA, Pastides PS, Sarraf KM, Willis-Owen C. Anterior cruciate ligament reconstruction best practice: A review of graft choice. World Journal of Orthopedics. 2013;5(1):23–29. doi: 10.5312/wjo.v5.i1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chechik O, Amar E, Khashan M, Lador R, Eyal G, Gold A. An international survey on anterior cruciate ligament reconstruction practices. Int Orthop. 2012;37(2):201–206. doi: 10.1007/s00264-012-1611-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tadokoro K, Matsui N, Yagi M, Kuroda R, Kurosaka M, Yoshiya S. Evaluation of Hamstring Strength and Tendon Regrowth after Harvesting for Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2004;32(7):1644–1650. doi: 10.1177/0363546504263152. [DOI] [PubMed] [Google Scholar]
- 4.Papalia R, Franceschi F, D’Adamio S, Diaz Balzani L, Maffulli N, Denaro V. Hamstring Tendon Regeneration After Harvest for Anterior Cruciate Ligament Reconstruction: A Systematic Review. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2015;31(6):1169–1183. doi: 10.1016/j.arthro.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 5.Cross MJ, Roger G, Kujawa P, Anderson IF. Regeneration of the semitendinosus and gracilis tendons following their transection for repair of the anterior cruciate ligament. Am J Sports Med. 1992;20(2):221–223. doi: 10.1177/036354659202000223. [DOI] [PubMed] [Google Scholar]
- 6.Lempainen L, Sarimo J, Mattila K, Heikkilä J, Orava S. Distal tears of the hamstring muscles: review of the literature and our results of surgical treatment. Br J Sports Med. 2006;41(2):80–83. doi: 10.1136/bjsm.2006.031211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakamae A, Ochi M, Deie M, Adachi N. Unsuccessful regeneration of the semitendinosus tendon harvested for anterior cruciate ligament reconstruction: Report of two cases. Orthopaedics & Traumatology: Surgery & Research. 2012;98(8):932–935. doi: 10.1016/j.otsr.2012.07.011. [DOI] [PubMed] [Google Scholar]
- 8.Järvinen TLN, Järvinen TAH, Penttilä T, Harilainen A, Sandelin J, Paakkala T. Failed regrowth of the harvested semitendinosus tendon: A rare complication of tendon harvest after anterior cruciate ligament reconstruction. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2003;19(4):1–3. doi: 10.1053/jars.2003.50120. [DOI] [PubMed] [Google Scholar]
- 9.Nikolaou VS, Efstathopoulos N, Wredmark T. Hamstring tendons regeneration after ACL reconstruction: an overview. Knee Surgery, Sports Traumatology, Arthroscopy. 2007;15(2):153–160. doi: 10.1007/s00167-006-0160-4. [DOI] [PubMed] [Google Scholar]
- 10.Adams D, Logerstedt D, Hunter-Giordano A, Axe MJ, Snyder-Mackler L. Current Concepts for Anterior Cruciate Ligament Reconstruction: A Criterion-Based Rehabilitation Progression. J Orthop Sports Phys Ther. 2012;42(7):601–614. doi: 10.2519/jospt.2012.3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hodgson RJ, O’Connor PJ, Grainger AJ. Tendon and ligament imaging. Br J Radiol. 2012;85(1016):1157–1172. doi: 10.1259/bjr/34786470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Padulo J, Oliva F, Frizziero A, Maffulli N. Muscles, Ligaments and Tendons Journal - Basic principles and recommendations in clinical and field science research: 2016 update. MLTJ. 2016;6(1):1–5. doi: 10.11138/mltj/2016.6.1.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Suijkerbuijk MAM, Reijman M, Lodewijks SJM, Punt J, Meuffels DE. Hamstring Tendon Regeneration After Harvesting. Am J Sports Med. 2015;43(10):2591–2598. doi: 10.1177/0363546514562169. [DOI] [PubMed] [Google Scholar]
- 14.Karagiannidis E, Kellis E, Galanis N, Vasilios B. Semitendinosus muscle architecture during maximum isometric contractions in individuals with anterior cruciate ligament reconstruction and controls. Muscles, Ligaments and Tendons Journal. 2017;7(1):147–151. doi: 10.11138/mltj/2017.7.1.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Åhlén M, Lidén M, Movin T, Papadogiannakis N, Rostgård-Christensen L, Kartus J. Histological Evaluation of Regenerated Semitendinosus Tendon a Minimum of 6 Years After Harvest for Anterior Cruciate Ligament Reconstruction. Orthopaedic Journal of Sports Medicine. 2014;2(9) doi: 10.1177/2325967114550274. 23259 67114550274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carofino B, Fulkerson J. Medial Hamstring Tendon Regeneration Following Harvest for Anterior Cruciate Ligament Reconstruction: Fact, Myth, and Clinical Implication. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2005;21(10):1257–1265. doi: 10.1016/j.arthro.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 17.Burks RT, Crim J, Fink BP, Boylan DN, Greis PE. The Effects of Semitendinosus and Gracilis Harvest in Anterior Cruciate Ligament Reconstruction. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2005;21(10):1177–1185. doi: 10.1016/j.arthro.2005.07.005. [DOI] [PubMed] [Google Scholar]