Abstract
Background
Depression is a common and potentially debilitating illness worldwide. Attendance to routine childcare appointments is a key point of interest in the effort to improve the health and care for families facing depression.
Aim
To evaluate the association between maternal depression and offspring non-attendance to the Danish childcare and vaccination programme (CCP) for children from 0–5 years of age. The CCP consists of seven separate visits and several vaccinations. To investigate if exposure to recent and previous depression may affect attendance differently.
Design and setting
Population-based cohort study using Danish nationwide registers.
Method
Participants were all live-born children (n = 853 315) in Denmark in the period from 1 January 2000 until 31 August 2013, and their mothers. The outcome of interest was non-attendance of each one of the seven scheduled childcare visits and two vaccination entities in the CCP. Exposure was maternal (both previous and recent) depression. All information was obtained from Danish national registries.
Results
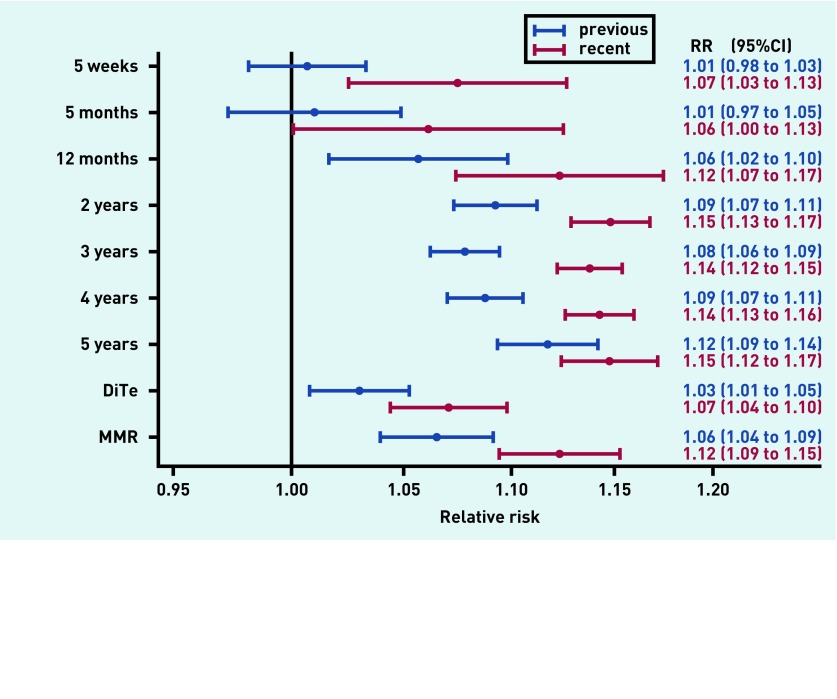
The risk of not attending CCP was higher for children of mothers with depression. For children of mothers with previous depression, the relative risk (RR) was 1.01 (95% confidence interval [CI] = 0.98 to 1.03) at the 5-week childcare visit, and 1.12 (95% CI = 1.09 to 1.14) at the 5-year childcare visit. For children of mothers with recent depression, the RR was 1.07 (95% CI = 1.03 to 1.13) at the 5-week visit, and 1.15 (95% CI = 1.13 to 1.17) at the 5-year visit. Furthermore, the risk of missing at least four of the seven childcare visits was higher for children of females with maternal depression (RR = 1.16, 95% CI = 1.13 to 1.19).
Conclusion
Maternal depression seems to compromise CCP attendance. These findings suggest a need for careful clinical attention to these vulnerable families, even years after a diagnosis of depression.
Keywords: child care, delivery of health care, depression, Denmark, general practice, maternal
INTRODUCTION
Depression is a common mental illness with a lifetime prevalence of 16–18%, and it progresses to a chronic state (depressive symptoms for >2 years) in 10–30% of affected individuals.1,2 The risk of depression among females is approximately twice that of males, a risk that increases further during and after pregnancy.2–5 The negative adverse effects of maternal depression on offspring development and behaviour have been studied extensively. Existing research has found that maternal depressive symptoms correlate with higher rates of insecure attachment between mother and child,6 emotional insensitivity, and negative parenting behaviour.7–10 All of these factors can lead to internalising and externalising behaviour problems in the children.11–13 Maternal depression has been found to be associated with increased childhood illnesses, lower immunisation rates, poorer cognitive development, and higher likelihood of underweight in the offspring.14–18 A British review described maternal depression as the mental disorder with the highest public health impact, and highlighted the importance of this topic in the global agenda.19
The long-term health consequences of growing up with a parent suffering from depression are less well studied. Raposa et al found that maternal depression during pregnancy was associated with increased health problems among offspring before age 5 years, greater health-related stress and poorer social adjustment at age 20 years, and difficulties with social functioning and higher rates of youth depressive symptoms at ages 22–25 years.20 These results imply a need for early identification of symptoms and development of interventions to reduce the negative trajectories for the offspring. Routine maternal depression screening during childcare visits has been found to be feasible, and provides opportunity in the consultation to address troublesome issues.21 In Denmark, routine maternal depression screening is not included in the childcare visit. The childcare visit includes an evaluation of the growth and welfare of the child, and also provides opportunity to detect, for example, signs of abuse, malnourishment, and obesity. The visits are performed by the GP and include physical examination of the child, evaluation of age-relevant milestones (motor and cognitive functions), and the child’s wellbeing and thriving in the family and in day care, as well as advice on nutrition and precautions. It remains unclear how often children of mothers with depression attend these visits. Some studies have found no association between maternal depression or anxiety and attendance to routine well-child visits and/or vaccinations,22–24 whereas others have found that children of mothers with depression or anxiety had a higher risk of either starting a vaccination programme late or not at all.25 Additionally, decreased odds of receiving age-appropriate well-child visits have been reported.26 To the authors’ knowledge, no previous study has explored the impact of recent depression compared to previous depression for contact to primary care.
How this fits in
Extant research in this area has yielded ambiguous results. To the authors’ knowledge, no previous study has included data from an entire country or explored the difference in impact of maternal recent and previous depression on attendance of routine childcare appointments. This study provides novel knowledge on the association between maternal depression and offspring attendance to routine childcare appointments, and reveals a link that could serve to improve the general welfare of both.
This study aims to explore attendance to the Danish routine childcare and vaccination programme (CCP), and to examine the potential association between attendance and exposure to maternal depression. Furthermore, the study aims to investigate whether exposure to recent and previous depression affects attendance differently.
METHOD
Study design
All information for this population-based cohort study was obtained through Danish national registries. All citizens in Denmark are assigned a unique personal identification number (PIN) at birth or immigration. This PIN was used to link information at the personal level from different national registries.
All children eligible for inclusion were live-born children with Danish residency born from 1 January 2000 to 31 August 2013 (n = 853 315). The children were linked to their mothers through the Danish Civil Registration System.27 Children or mothers who died, emigrated, or disappeared during follow-up were censored from the analysis after the date of departure, and children with an inactive PIN were excluded from all analyses (n = 3072). The children were followed until their sixth birthday or 31 December 2013, whichever came first. The main study thus included a total of 850 243 children and 517 107 mothers.
Exposure
Maternal depression was defined by the following three criteria:
one or more hospital admission owing to a main diagnosis of depression;
two or more outpatient contacts to a hospital owing to a main diagnosis of depression within 6 months;
reimbursement of two or more prescriptions of antidepressant medications within 6 months. (Box 1).
Box 1. Criteria for exposure, and description of exposure groups.
| Exposure measures | Criteria required for depression | Groups of depression |
|---|---|---|
| • Antidepressant medications | • ≥2 prescriptions reimbursed within 6 months | • Never (control group): not meeting any depression criteria in a 60-month period before date of childcare visit |
| • Admission to a hospital | • ≥1 admission to a hospital within 6 months scheduled childcare visit | • Previous: meeting at least one of the criteria from 6–60 months before |
| • Outpatient contact to a hospital | • ≥2 outpatient contacts to a hospital within 6 months childcare visit | • Recent: meeting at least one of the criteria during the 6 months before scheduled |
Information on hospitalisations and outpatient contacts was obtained from the Danish Psychiatric Central Research Register.28 The Danish Register of Medicinal Product Statistics provided the authors with information on the use of antidepressant drugs.29 The control group ‘never depressed’ was defined as not meeting any of the three depression criteria in the 60-month period before the date of the childcare visit. Exposure was divided into two groups: ‘previous depression’ when meeting at least one of the criteria during a period of 6–60 months before the relevant childcare visit, and ‘recent depression’ when meeting at least one of the criteria during the 6-month period before the relevant childcare visit (Box 1).
Outcomes
The primary outcome of interest was non-attendance to routine childcare visits. In Denmark, seven childcare visits are scheduled in general practice from age 0–5 years, and each is registered with a specific service code in the National Health Insurance Service Register (NHSR).30 All GP consultations are free of charge. Non-compliance was defined as no record of childcare visit during a specific compliance window.
The secondary outcome of interest was non-attendance to the recommended vaccination programme. Vaccination-specific codes were obtained from the NHSR. The Danish vaccination programme consists of two types of vaccination: diphtheria/tetanus/pertussis/polio (DiTe), and measles, mumps, and rubella (MMR).31
Vaccination for pneumococcus was introduced in 2007, and the codes for Haemophilus influenza changed during the study period. As these vaccines are administered simultaneously with the others mentioned above, they were ignored in further analyses.
Covariates
A Danish register-based study revealed that several factors are associated with lower participation in the CCP.32 These risk factors included household income, the parents’ occupational and educational level, and the number of older siblings. Information on maternal age at birth and parity was obtained from the Danish Civil Registration System.27 From Statistics Denmark, the authors received information on maternal cohabitation status, income, and education.30 Furthermore, the authors included information on maternal mental comorbidity, including drug abuse, alcoholism, eating disorders, schizophrenia, dementia, and bipolar disorder. These were identified using the algorithm developed by Prior et al.33 Paternal depression, defined by the same criteria as maternal depression, was also included as a covariate. Participants with missing values in any of the covariates were included in the analyses by adding an ‘unknown’ category to the categorical variables. In the multivariate analyses, adjustments were made dynamically, as the covariates for a child can change between two childcare visits. The covariates were measured 5 years before the start of the compliance windows. This was incorporated to minimise residual confounding and to ensure that covariates were measured before exposure to prevent them from acting as intermediaries in the causal chain.
Statistical analysis
To assess the timing of the exposure, maternal depression was categorised into three groups — never depressed, previous depression, and recent depression. The compliance windows were made asymmetrical, as a right-skewed distribution was seen for child age at the childcare visits; CCP that is, the children tended to be older than the scheduled age when attending the CCP. To maximise the possibility of attendance, the windows were defined as widely as possible without overlap. Poisson regression with robust variance estimation (sandwich estimator) was used in the analyses.34 Analyses were run separately for each of the seven childcare visits and the two vaccination groups. Crude analyses are presented with adjustments for calendar year, as the authors found a time trend in childbirths and attendance rates.
To assess whether maternal depression was associated with repeated absence from childcare visits, Poisson regression with robust variance was performed to determine the risk of missing at least 50% of the scheduled visits (that is, missing four or more visits). In this analysis, exposure was defined as ‘never’ versus ‘ever’ (previous or recent depression), and the authors included data for children born in 2000–2008 to ensure comprehensive follow-up.
Sensitivity analyses
Females admitted to a hospital with depression tend to have more severe depression than females treated with antidepressant medications in primary health care. Hence, in one sub-analysis, exposure was restricted to include mothers treated only with medications, and mothers treated through hospital admission or outpatient contacts, regardless of medication use.
Antidepressant medications may be prescribed for other illnesses and mental illnesses other than depression. From 2004 and onwards, Danish physicians could indicate a diagnosis when prescribing certain medicines. In a sub-analysis, the authors included only prescriptions containing the indication code ‘depression’. Participants in this analysis were children born in 2006–2013 and their mothers.
RESULTS
The overall numbers of children in each exposure group at all visits/vaccinations are shown in Table 1. Depression was, in both groups, associated with shorter education, lower income, more divorces, and a greater number of other mental conditions in addition to depression (Table 2). The authors found an unequal distribution of missing values across the three exposure categories. Sub-analyses revealed that the main part of these missing values belonged to mothers without residency in Denmark. These mothers do not appear in the Danish registries, which may explain why most were ‘never’ depressed. Sub-analyses including only children of mothers with residency in Denmark at least 5 years before birth did not alter the final results.
Table 1.
Non-attendance of CCP childcare visits and vaccinationsa
| Childcare visit | Compliance windows | Depression categories | Children in the study, n | Children missing CCP, n | Non-attendance, % |
|---|---|---|---|---|---|
| 5 weeks | 3 weeks to 3.9 months | Never | 795 597 | 116 871 | 15 |
| Previous | 42 754 | 5375 | 13 | ||
| Recent | 11 892 | 1502 | 13 | ||
| Total | 850 243 | 123 748 | 15 | ||
|
| |||||
| 5 months | 4 months to 10.9 months | Never | 764 443 | 54 289 | 7 |
| Previous | 37 930 | 2744 | 7 | ||
| Recent | 14 330 | 1061 | 7 | ||
| Total | 816 703 | 58 094 | 7 | ||
|
| |||||
| 12 months | 11 months to 22.9 months | Never | 708 354 | 51 102 | 7 |
| Previous | 29 982 | 2482 | 8 | ||
| Recent | 20 360 | 1780 | 9 | ||
| Total | 758 696 | 55 364 | 7 | ||
|
| |||||
| 2 years | 23 months to 34.9 months | Never | 645 074 | 169 894 | 26 |
| Previous | 25 588 | 8373 | 33 | ||
| Recent | 27 057 | 9186 | 34 | ||
| Total | 697 719 | 187 453 | 27 | ||
|
| |||||
| 3 years | 35 months to 46.9 months | Never | 580 206 | 195 855 | 34 |
| Previous | 25 500 | 10 520 | 41 | ||
| Recent | 28 192 | 11 929 | 42 | ||
| Total | 633 898 | 218 304 | 34 | ||
|
| |||||
| 4 years | 47 months to 58.9 months | Never | 517 572 | 164 308 | 32 |
| Previous | 24 515 | 9130 | 37 | ||
| Recent | 28 896 | 10 995 | 38 | ||
| Total | 570 983 | 184 433 | 32 | ||
|
| |||||
| 5 years | 59 months to 6 years | Never | 453 635 | 88 209 | 19 |
| Previous | 25 127 | 6486 | 26 | ||
| Recent | 27 909 | 7062 | 25 | ||
| Total | 506 671 | 101 757 | 20 | ||
|
| |||||
| DiTe | 11 months to 21 months | Never | 716 622 | 153 965 | 21 |
| Previous | 30 526 | 6702 | 22 | ||
| Recent | 20 678 | 4723 | 23 | ||
| Total | 767 826 | 165 390 | 22 | ||
|
| |||||
| MMR | 14 months to 24 months | Never | 701 134 | 115 719 | 17 |
| Previous | 28 802 | 5405 | 19 | ||
| Recent | 23 019 | 4594 | 20 | ||
| Total | 752 955 | 125 718 | 17 | ||
The number of children in all exposure categories at each visit. Since the mother can change status from one visit to the next, some children will also alter status in the depression categories. CCP = the Danish childcare and vaccination programme. DiTe = diphtheria/tetanus/pertussis vaccination. MMR = measles, mumps, and rubella vaccination.
Table 2.
Maternal characteristics at the 5-week childcare visita
| Never depressed | Previous depression | Recent depression | Total | P-value | |
|---|---|---|---|---|---|
| n (%) | 795 597 (93.6) | 42 754 (5.0) | 11 892 (1.4) | 850 243 | |
|
| |||||
| Year of birth, n (column %) | |||||
| 2000–2004 | 308 532 (38.8) | 9562 (22.4) | 2032 (17.1) | 320 126 | |
| 2005–2008 | 236 869 (29.8) | 13 540 (31.7) | 3867 (32.5) | 254 276 | |
| 2009–2013 | 250 196 (31.4) | 19 652 (46.0) | 5993 (50.4) | 275 841 | <0.001 |
|
| |||||
| Age of mother, mean (SD) | 30.6 (4.8) | 30.5 (5.2) | 31.3 (5.0) | 30.6 (4.9) | <0.001 |
|
| |||||
| Parity, n (column %) | |||||
| 1 | 350 925 (44.1) | 19 912 (46.6) | 5316 (44.7) | 376 153 | |
| 2 | 299 219 (37.6) | 14 021 (32.8) | 4208 (35.4) | 317 448 | |
| 3 | 108 916 (13.7) | 6121 (14.3) | 1657 (13.9) | 116 694 | |
| +4 | 36 537 (4.6) | 2700 (6.3) | 711 (6.0) | 39 948 | <0.001 |
|
| |||||
| Education, n (column %) | |||||
| ≤10 years | 198 891 (25.0) | 17 572 (41.1) | 4170 (35.1) | 220 633 | |
| >10 and ≤15 years | 389 956 (49.0) | 18 051 (42.2) | 5382 (45.3) | 413 389 | |
| >15 years | 142 546 (17.9) | 5613 (13.1) | 1890 (15.9) | 150 049 | |
| Unknownb | 64 204 (8.1) | 1518 (3.6) | 450 (3.8) | 66 172 | <0.001 |
|
| |||||
| Income decile, n (column %) | |||||
| Low | 286 508 (36.0) | 17 498 (40.9) | 4592 (38.6) | 308 598 | |
| Moderate | 352 020 (44.2) | 20 366 (47.6) | 5848 (49.2) | 378 234 | |
| High | 113 798 (14.3) | 4367 (10.2) | 1216 (10.2) | 119 381 | |
| Unknownb | 43 271 (5.4) | 523 (1.2) | 236 (2.0) | 44 030 | <0.001 |
|
| |||||
| Civil status, n (column %) | |||||
| Widow | 500 (0.1) | 40 (0.1) | 9 (0.1) | 549 | |
| Divorced | 14 719 (1.9) | 1325 (3.1) | 363 (3.1) | 16 407 | |
| Married | 127 794 (16.1) | 7142 (16.7) | 2025 (17.0) | 136 961 | |
| Unmarried | 602 013 (75.7) | 33 524 (78.4) | 9198 (77.3) | 644 735 | |
| Unknownb | 50 571 (6.4) | 723 (1.7) | 297 (2.5) | 51591 | <0.001 |
|
| |||||
| Mental comorbidities (Yes), n (column %)c | 2583 (0.3) | 996 (2.3) | 411 (3.5) | 3990 | <0.001 |
The covariates for this analysis are measured 5 years before the visit in order to avoid the covariates being intermediate factors. One way Anova (analysis of variance) and Kruskal-Wallis test is used to generate P-values.
Unknown represents missing data.
Mental comorbidities include drug abuse, alcoholism, eating disorders, schizophrenia, dementia, and bipolar disorder. SD = standard deviation.
Crude regression analysis showed that exposed children had a higher risk of non-attendance, both in terms of childcare visits and vaccinations (Figure 1). Adjustments generally attenuated the association. Exposure to recent maternal depression was associated with a statistically significantly higher risk of non-attendance of up to 16%, depending on the specific childcare visit. Exposure to previous maternal depression was also associated with a statistically significantly higher risk in the analyses for 2-year, 3-year, 4-year, and 5-year follow-up. A vague trend towards higher risk of non-attendance was seen with increasing age of the child. The risk of not receiving vaccination was highest for the MMR vaccination (Figure 1).
Figure 1.
Relative risk of not attending the Danish childcare and vaccination programme (CCP) visits. Reference group is ‘never depressed’ mothers. The adjusted analysis includes the covariates maternal age at birth (sextiles), maternal education (three groups), maternal income (deciles), cohabitation status (four groups), calendar year (indicator variables), paternal depression (three groups), maternal mental comorbidities (indicator for any of six diagnoses), parity (four groups). See groups in Table 2.
Defining maternal depression solely by reimbursement of prescriptions for antidepressant drugs did not alter the results considerably (results not shown).
Defining maternal depression solely by hospitalisations or outpatient contacts broadened the confidence intervals (CIs), as a lower number was exposed. The patterns of associations were the same, but the association between depression and early visits (up to 12 months) was no longer significant, and the difference in risk between recent and previous depression was not statistically significant (results not shown).
In one sensitivity analysis, the authors included only reimbursements with the depression-specific prescription code, but these results did not differ markedly from the original analysis (results not shown). However, the CIs broadened due to the smaller sample size, and some of the results fell below the threshold of significance.
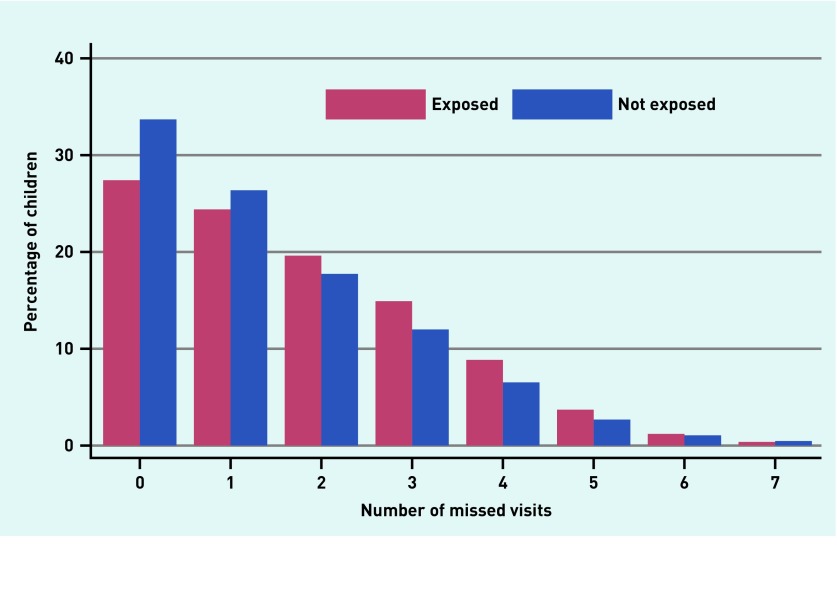
Children of mothers with depression attended fewer childcare visits compared to children of mothers without depression. A total of 34% of the unexposed children attended all childcare visits, whereas the corresponding figure was 27% for the exposed children (Figure 2). In the adjusted analyses, children of mothers with depression had a 12% higher risk of missing >50% of the childcare visits (that is, more than four out of seven visits) compared to children of mothers without depression during childhood, relative risk (RR) 1.16, 95% CI = 1.13 to 1.19).
Figure 2:
Percentage of children with 0–7 missed visits for exposed and non-exposed. Exposed: children of mothers with either previous or recent depression. Not exposed: children of mothers with no registered diagnosis of depression during the previous 60 months.
DISCUSSION
Summary
Children of mothers with depression were less likely to attend childcare visits and the vaccination programme. Recent depression yielded the highest risk of non-attendance, but exposure to previous depression also affected the attendance significantly. Furthermore, exposure to depression was associated with a significantly higher risk of missing more than 50% of the childcare visits during childhood.
Strengths and limitations
A major strength of the present study was that it included the entire birth population in Denmark from 1997–2013 and had virtually complete follow-up, owing to the valid information in the Danish registries. Therefore, selection bias is unlikely to have been introduced.27–30,35,36
A potential limitation was that depression was only defined by medication or hospital contacts, such that females with depression with no medication prescriptions and no hospital contact would be categorised in the control group as ‘never depressed’. More GPs may now prefer non-pharmacological treatment. Additionally, some females may have difficulties complying with medical treatment. This information was not available for the present study, which might have introduced misclassification and could have biased the results towards no association, but does not explain the findings of higher non-attendance in the exposed group. Random misclassifications cannot be entirely excluded in a register-based study. To minimise this, the authors required the mother to reimburse at least two prescriptions for antidepressant medication within 6 months in order to be considered exposed in the analyses. Antidepressant medication could also be prescribed for anxiety and other illnesses. The sensitivity analysis, which included only information on reimbursement of antidepressants with the depression-specific prescription code, did not alter the overall results. The completeness of the services registered is generally regarded as high.27–30,35,36 However, a recent study found discrepancies between register data and medical records, which revealed an underestimation of the coverage of the MMR vaccination.37 Although relevant, it is unlikely that this misclassification is dependent on the exposure groups. Consequently, this cannot explain the authors’ findings of a higher risk of non-compliance in the exposed group.
Comparison with existing literature
Existing literature on maternal depression and offspring varies in quality and findings. A structured literature search yielded six relevant articles on well-child visits. Andersen et al30 and Goldman et al24 found no significant association between maternal depression and offspring attendance to routine childcare. Both studies were based on considerably smaller cohorts and shorter follow-up (first year of the child’s life). In addition, their designs (data collection based on questionnaires) were prone to recall bias and selection bias, which the authors themselves also acknowledge. Farr et al performed a cohort study in Portland and found no difference in the attendance to well-child visits and vaccination programmes, but they reported slightly higher use of emergency visits for infants of mothers with prenatal and postpartum depression or anxiety.22 Their definition of vaccination status was similar to the one in this study. However, they dichotomised the attendance to well-child visits into less than five visits or five or more visits. The study provided no record of previous maternal depression which might have affected the results. Minkovitz et al performed a study with a design similar to the present study.26 Follow-up was extended to 3 years of age and the outcome to six childcare visits. They found that children of mothers reporting depressive symptoms had decreased odds of receiving age-appropriate well-child visits and vaccinations. Turner et al added the perspective that children of mothers with mental disabilities generally attended vaccinations late or not at all, despite strong intentions to have the child vaccinated.25 To the authors’ knowledge, no previous studies have explored the difference between recent and previous depression for non-attendance in childcare visits.
In line with the present study, Sills et al found parental depression to be associated with a lower attendance to planned well-child visits, although only statistically significant among adolescents.38 The setting in their study was Kaiser Permanente, which is a health insurance system in the US. This system provides care for a large population and offers a broad spectrum of valid information, but it is still not generalisable to an entire nation. Among many structural differences, the population at Kaiser Permanente is younger, better educated, and wealthier than the average Danish population.39 Furthermore, Sills et al did not adjust for socioeconomic status, which has been shown to affect attendance.32
Alternative diagnoses may pollute the exposure group. Nevertheless, the results presented indicate that either depression is responsible for the majority of the risk, or people with other conditions treated with antidepressant medications behave similarly. Furthermore, the sub-analyses suggest that even mild cases of depression are also associated with higher risk of non-attendance to routine childcare visits.
When a mother is ill with depression, contacts without incitement (such as childhood illnesses) may have low priority. The core symptoms of depression are suppressed motivation, reduced energy, and low mood. The authors interpret the finding that recent depression impairs the compliance to all childcare visits as a sign of impaired parental energy. They found it of great interest that previous maternal depression affects the attendance significantly. A possible explanation could be that cognition and memory can be affected even years after recovery. Previous depression did not seem to significantly affect attendance to the first three visits. Important features mark the first year of a child’s life. Communication is non-verbal, which requires emotional sensitivity from parents in the interpretation of symptoms. In mothers with previous depression, parental insecurity might prompt the mother to attend the early visits but, as the child ages, the symptoms of depression may dominate increasingly, and persistent effort cannot be exercised. Previous research has implied that maternal depression is associated with both physical and psychological adverse effects in offspring.19
Implications for research and practice
The present study shows that maternal depression impairs attendance to routine childcare, even years after a diagnosis. This is important knowledge for GPs. Well childcare and pregnancy programmes are important aspects in public health care. Children of depressed mothers are at greater risk of adverse consequences and thus require increased attention in childcare. Two aspects of the present findings require special consideration. First, mothers known to have depression may benefit from proactive attention from health personnel and the social network. Second, GPs may consider non-attendance at childcare visits as a potential concern, and maternal depression should be considered as a potential reason. Routine childcare visits form part of a comprehensive scheme based on continuous contact between the GP and the mother from conception, during pregnancy, and through the first 5 years of the child’s life. It may be beneficial to explore the history of mental health when assessing these pregnant women and their children to ensure that extra support is provided to the ones that need it the most.
Future research could include designs that are capable of exploring the reasons behind non-attendance in routine childcare visits.
Funding
The study was supported by an unrestricted grant from the Lundbeck Foundation (grant number: R155-2012-11280) and by the Program for Clinical Research Infrastructure (PROCRIN), which was established by the Lundbeck Foundation and the Novo Nordisk Foundation, and is administered by Danish Regions.
Ethical approval
Not applicable.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.The Danish Health Authority National klinisk retningslinje for non-farmakologisk behandling af unipolar depression. [Danish national clinical guideline for non-pharmacological therapies for unipolar depression] 2016. https://sundhedsstyrelsen.dk/da/nyheder/2016/~/media/0216564BB8AA4D40B7DBAF21E9ACF403.ashx (accessed 18 Dec 2017).
- 2.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 3.Munk-Olsen T, Laursen TM, Pedersen CB, et al. New parents and mental disorders. JAMA. 2006;296(21):2582–2589. doi: 10.1001/jama.296.21.2582. [DOI] [PubMed] [Google Scholar]
- 4.Weissman MM, Bland MC, Canino MJ, et al. Cross-national epidemiology of major depression and bipolar disorder. JAMA. 1996 doi: 10.1001/jama.1996.03540040037030. [DOI] [PubMed] [Google Scholar]
- 5.Angst J, Gamma A, Gastpar M, et al. Gender differences in depression. Epidemiological findings from the European DEPRES I and II studies. Eur Arch Psychiatry Clin Neurosci. 2002 doi: 10.1007/s00406-002-0381-6. [DOI] [PubMed] [Google Scholar]
- 6.Campbell SB, Brownell CA, Hungerford A, et al. The course of maternal depressive symptoms and maternal sensitivity as predictors of attachment security at 36 months. Dev Psychopathol. 2004;16(2):231–252. doi: 10.1017/s0954579404044499. [DOI] [PubMed] [Google Scholar]
- 7.Davalos DB, Yadon CA, Tregellas HC. Untreated prenatal maternal depression and the potential risks to offspring: a review. Arch Womens Ment Health. 2012;15(1):1–14. doi: 10.1007/s00737-011-0251-1. [DOI] [PubMed] [Google Scholar]
- 8.Cookson H, Granell R, Joinson C, et al. Mothers’ anxiety during pregnancy is associated with asthma in their children. J Allergy Clin Immunol. 2009 doi: 10.1016/j.jaci.2009.01.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marcus SM. Depression during pregnancy: rates, risks, and consequences — Motherisk update 2008. Can J Clin Pharmacol. 2009;16(1):e15–22. [PubMed] [Google Scholar]
- 10.Hammerton G, Zammit S, Mahedy L, et al. Pathways to suicide-related behavior in offspring of mothers with depression: The role of offspring psychopathology. J Am Acad Child Adolesc Psychiatry. 2015;54(5):385–393. doi: 10.1016/j.jaac.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Susman EJ, Trickett PK, Iannotti RJ, et al. Child-rearing patterns in depressed, abusive, and normal mothers. Am J Orthopsychiatry. 1985;55(2):237–251. doi: 10.1111/j.1939-0025.1985.tb03438.x. [DOI] [PubMed] [Google Scholar]
- 12.Cummings EM, Davies PT. Maternal depression and child development. J Child Psychol Psychiatry. 1994;35(1):73–112. doi: 10.1111/j.1469-7610.1994.tb01133.x. [DOI] [PubMed] [Google Scholar]
- 13.Leis JA, Heron J, Stuart EA, Mendelson T. Associations between maternal mental health and child emotional and behavioral problems: Does prenatal mental health matter? J Abnorm Child Psychol. 2014 doi: 10.1007/s10802-013-9766-4. [DOI] [PubMed] [Google Scholar]
- 14.Rahman A, Iqbal Z, Bunn J, et al. Impact of maternal depression on infant nutritional status and illness. Arch Gen Psychiatry. 2004 doi: 10.1001/archpsyc.61.9.946. [DOI] [PubMed] [Google Scholar]
- 15.Patel V, Prince M. Maternal psychological morbidity and low birth weight in India. Br J Psychiatry. 2006;188(3):284–285. doi: 10.1192/bjp.bp.105.012096. [DOI] [PubMed] [Google Scholar]
- 16.Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010 doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adewuya AO, Ola BO, Aloba OO, et al. Impact of postnatal depression on infants’ growth in Nigeria. J Affect Disord. 2008 doi: 10.1016/j.jad.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 18.Black MM, Baqui AH, Zaman K, et al. Maternal depressive symptoms and infant growth in rural Bangladesh. Am J Clin Nutr. 2009 doi: 10.3945/ajcn.2008.26692E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Atif N, Lovell K, Rahman A. Maternal mental health: The missing “m” in the global maternal and child health agenda. Semin Perinatol. 2015 doi: 10.1053/j.semperi.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 20.Raposa E, Hammen C, Brennan P, Najman J. The long-term effects of maternal depression: early childhood physical health as a pathway to offspring depression. J Adolesc Health. 2014 doi: 10.1016/j.jadohealth.2013.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olson AL, Dietrich AJ, Prazar G, Hurley J. Brief maternal depression screening at well-child visits. Pediatrics. 2006 doi: 10.1542/peds.2005-2346. [DOI] [PubMed] [Google Scholar]
- 22.Farr SL, Dietz PM, Rizzo JH, et al. Health care utilisation in the first year of life among infants of mothers with perinatal depression or anxiety. Paediatr Perinat Epidemiol. 2013 doi: 10.1111/ppe.12012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anderson LN, Campbell MK, daSilva O, et al. Effect of maternal depression and anxiety on use of health services for infants. Can Fam Physician. 2008;54(12):1718–1719.e5. [PMC free article] [PubMed] [Google Scholar]
- 24.Goldman SL, Owen MT. The impact of parental trait anxiety on the utilization of health care services in infancy: a prospective study. J Pediatr Psychol. 1994 doi: 10.1093/jpepsy/19.3.369. [DOI] [PubMed] [Google Scholar]
- 25.Turner C, Boyle F, O’Rourke P. Mothers’ health post-partum and their patterns of seeking vaccination for their infants. Int J Nurs Pract. 2003;9(2):120–126. doi: 10.1046/j.1322-7114.2003.00410.x. [DOI] [PubMed] [Google Scholar]
- 26.Minkovitz CS, Strobino D, Scharfstein D, et al. Maternal depressive symptoms and children’s receipt of health care in the first three years of life. Pediatrics. 2005 doi: 10.1542/peds.2004-0341. [DOI] [PubMed] [Google Scholar]
- 27.Thygesen LC, Kjaer Ersbøll A. Danish population-based registers for public health and health-related welfare research: Introduction to the supplement. Scand J Public Health. 2011 doi: 10.1177/1403494811409654. [DOI] [PubMed] [Google Scholar]
- 28.Thygesen LC, Daasnes C, Thaulow I, Brønnum-Hansen H. Introduction to Danish (nationwide) registers on health and social issues: Structure, access, legislation, and archiving. Scand J Public Health. 2011 doi: 10.1177/1403494811399956. [DOI] [PubMed] [Google Scholar]
- 29.Kildemoes HW, Sørensen HT, Hallas J. The Danish National Prescription Registry. Scand J Public Health. 2011 doi: 10.1177/1403494810394717. [DOI] [PubMed] [Google Scholar]
- 30.Andersen JS, De Fine Olivarius N, Krasnik A. The Danish National Health Service Register. Scand J Public Health. 2011 doi: 10.1177/1403494810394718. [DOI] [PubMed] [Google Scholar]
- 31.The Danish Health Authority Børnevaccinationsprogrammet. Årsrapport 2014. [The child vaccination programme in Denmark. Annual report 2014] 2014. https://www.sst.dk/da/udgivelser/2016/boernevaccinations_programmet-aarsrapport-2014 (accessed 18 Dec 2017).
- 32.Søndergaard G, Biering-Sørensen S, Ishøy Michelsen S, et al. Non-participation in preventive child health examinations at the general practitioner in Denmark: a register-based study. Scand J Prim Health Care. 2008;26(1):5–11. doi: 10.1080/02813430801940877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prior A, Fenger-Grøn M, Larsen KK, et al. The association between perceived stress and mortality among people with multimorbidity: a prospective population-based cohort study. Am J Epidemiol. 2016 doi: 10.1093/aje/kwv324. [DOI] [PubMed] [Google Scholar]
- 34.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004 doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 35.Schmidt M, Pedersen L, Sørensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. 2014 doi: 10.1007/s10654-014-9930-3. [DOI] [PubMed] [Google Scholar]
- 36.Pedersen CB. The Danish Civil Registration System. Scand J Public Health. 2011 doi: 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- 37.Holt N, Mygind A, Bro F. Danish MMR vaccination coverage is considerably higher than reported. Dan Med J. 2017;64(2) pii: A5345. [PubMed] [Google Scholar]
- 38.Sills MR, Shetterly S, Xu S, et al. Association between parental depression and children’s health care use. Pediatrics. 2007 doi: 10.1542/peds.2006-2399. [DOI] [PubMed] [Google Scholar]
- 39.Frølich A, Diderichsen F, Graetz I, et al. Hvad kan det danske sundhedsvæsen lære af Kaiser Permanente? En sammenligning mellem den amerikanske forsikringsinstitution Kaiser Permanente og det danske sundhedsvæsen [What can the Danish healthcare system learn from Kaiser Permanente? A comparison between the American research institution Kaiser Permanente and the Danish healthcare system] University Press of Southern Denmark; 2011. [Google Scholar]