Abstract
The longevity of metal-on-polyethylene prosthetic hip joint bearings, in which a CoCrMo femoral head articulates with a polyethylene liner, is often limited by polyethylene wear and osteolysis caused by polyethylene wear particles. Current approaches to reduce polyethylene wear include improving the mechanical properties of the polyethylene liner, and/or manufacturing ultra-smooth articulating surfaces. In contrast, this experimental work shows that adding a patterned microtexture of concave “dimples” to a polished CoCrMo surface significantly reduces polyethylene wear by promoting the formation of an elastohydrodynamic lubricant film, which reduces contact between the CoCrMo and polyethylene bearing surfaces. Using a gravimetric method to measure polyethylene pin wear during pin-on-disc experiments, it was demonstrated that microtextured CoCrMo caused reduced polyethylene wear compared to polished CoCrMo surfaces. Wear was quantified for different polyethylene materials currently used in commercial prosthetic hip joint bearings, and for several microtexture geometries. It was also documented by correlating polyethylene wear with surface topography measurements that the patterned microtexture reduced contact between the articulating bearing surfaces.
1. Introduction
More than 300,000 total hip replacement (THR) surgeries are performed in the United States each year to treat degenerative joint diseases that cause pain and disability (2015 data). The most common type of prosthetic hip joint consists of a metal femoral head typically made from a cobalt chromium molybdenum (CoCrMo) alloy, articulating with a polyethylene acetabular liner consisting of (vitamin-E infused/cross-linked) ultra-high molecular weight polyethylene (UHMWPE). It is well-documented that the survivorship of these metal-on-polyethylene (MOP) prosthetic hip joints declines significantly after 15–20 years of use due in part to adhesive, and/or abrasive wear of the acetabular liner that articulates with the femoral head, and adverse immunological reaction to microscopic wear debris that causes inflammation and osteolysis, which weakens the implant to bone interface and may cause mechanical instability. Increasing longevity of prosthetic hip joints will reduce the need for complicated revision surgeries to replace implants or surgery postponement, which leaves the patient in pain and disability.
Research to increase longevity of prosthetic hip joints by reducing wear can be categorized into improving the mechanical properties of the polyethylene liner or improving the design of the femoral head/liner pairs. For example, the introduction of highly cross-linked polyethylene (HXPE), and subsequently the addition of anti-oxidant materials such as vitamin E to UHMWPE, has substantially reduced polyethylene wear. Alternatively, improvements in the design of the femoral head/liner pairs have focused on employing new materials and manufacturing ultra-smooth bearing surfaces, as indicated by the increased interest in ceramic-on-polyethylene (COP) and ceramic-on-ceramic (COC) prosthetic hip joints . Hard ceramic bearing surfaces can be polished to an average surface roughness that is an order of magnitude smaller than that of metal femoral heads, which may enable them to operate in the (elasto)hydrodynamic lubrication regime during a portion of the gait cycle, thus reducing friction and polyethylene wear. Ceramic materials are also less susceptible to abrasion and they exhibit improved hydrophilicity compared to CoCrMo and are biologically inert. As such, materials such as zirconia gain popularity but despite their attractive tribological properties, reports of in-vivo early osteolysis with a zirconia (ceramic) on polyethylene bearing have been documented.
In contrast with this existing research, reducing polyethylene wear by adding a patterned microtexture to polished CoCrMo material was investigated, in a CoCrMo / polyethylene bearing couple analogous to that used in MOP prosthetic hip joint bearings. The patterned microtexture forms a dense array of concave “dimples,” creating microhydrodynamic bearings that pressurize the joint fluid and increase the separation between the CoCrMo and polyethylene surfaces during articulation, thus reducing contact, friction, and polyethylene wear.
Surface texturing has been successfully used in a myriad of applications, resulting in a substantial reduction of friction and wear of bearing surfaces. A few researchers have experimentally studied the effect of surface texturing on prosthetic joint bearings to reduce friction and wear. Ito et al. used concave circular dimples (0.5 mm diameter, 0.1 mm depth, and 1.2 mm pitch) on a CoCrMo femoral head in a hip simulator, and reported that the friction coefficient and the UHMWPE wear was reduced by 36.2% and 69%, respectively, compared to using a smooth femoral head, in a 60 degree swing motion test (0.33 Hz, 1 million cycles). Sawano et al. performed pin-on-disc (POD) experiments to evaluate wear of UHMWPE pins articulating against textured CoCrMo alloy discs (0.3 to 4 μm diameter, 0.25 to 4.4 μm depth, and 0.1 mm pitch). They demonstrated that a 1 μm deep dimple reduced the UHMWPE wear by up to 61% compared to a smooth CoCrMo surface, and attributed this to wear particles being trapped within the dimples. Roy et al. performed POD experiments with a UHMWPE pin articulating with a textured CoCrMo disc, and found that circular dimples with 400 μm diameter, 30 μm depth, and 15% texture density reduced the friction coefficient and UHMWPE wear by 22% and 53%, respectively, compared to articulating with a smooth CoCrMo surface. However, testing was performed at 5–20 Hz, which exceeds the aproximately 1 Hz gait frequency. Cho et al. evaluated steel surfaces textured with circular dimples of 75 μm diameter, depth ranging between 20 and 75 μm, and texture density between 5 and 25% in a POD test with UHMWPE pins, and found a reduction of the friction coefficient between the textured discs and the UHMWPE pins independent of the dimple geometry. Chyr et al. used cylindrical surrogate CoCrMo femoral heads articulating with a cylindrical UHMWPE liner. They used a numerical lubrication model to optimize the microtexture geometry and density in terms of maximum lubricant film thickness, and then selected four candidate microtexture designs from the numerical results to use in experiments. Using a custom testing apparatus that implemented the primary kinematic and loading components of a hip, and with a reciprocating sliding motion to mimic gait, they found that adding the optimized microtexture designs to the smooth femoral head reduced friction drastically over almost the entire kinematic cycle.
While several researchers have reported reduced friction and wear for a textured CoCrMo surface articulating with a smooth UHMWPE specimen, no systematic study is available that quantifies the polyethylene wear rate as a function of microtexture parameters. Such results are critical for translation to the clinic. Hence, the objective of this paper is to experimentally quantify wear between UHMWPE pins and smooth and microtextured CoCrMo discs, the same materials used in commercial prosthetic hip joints. Different microtexture designs and different types of polyethylene were evaluated, currently used in prosthetic hip joints, to evaluate the effect of bearing surface texture parameters on polyethylene wear. It is noted that pin-on-disc testing does not provide the same wear rates and mechanisms as implant simulator testing, but it is typically used as a comparative screening test.
2. Materials and methods
2.1 Specimens
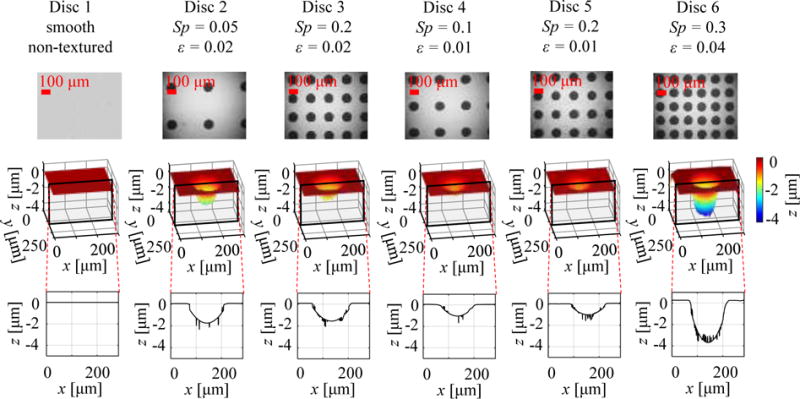
Laser surface texturing (LST) with a femtosecond laser ablation process was employed to manufacture five different patterned microtexture designs, selected based on our previous numerical optimization work on smooth CoCrMo (ASTMF1537-08) discs polished to Ra < 50 nm, identical to the surface quality of femoral heads of commercial MOP prosthetic hip joints. Table 1 identifies the different microtexture designs used in terms of the texture density Sp, which represents the fraction of the bearing surface covered by the microtexture features, and the texture aspect ratio ε, which is the ratio of depth and diameter of the spherical texture features. In addition, Table 1 shows a smooth non-textured CoCrMo disc used as benchmark specimen. An optical microscopy image, a white light interferometry image, and a cross-sectional view of the latter to illustrate the geometry of the microtexture feature and to demonstrate that the surface texturing does not affect the land area in between texture features, is shown for each CoCrMo disc.
Table 1.
CoCrMo discs with different microtexture geometry designs, identified by their texture density Sp and texture aspect ratio ε. Optical microscopy and white light interferometry (with cross-sectional profile) images are also provided for each.
|
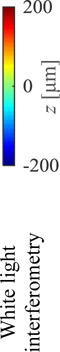
Three types of medical grade UHMWPE pins were evaluated, machined from ram-extruded bar stock: (1) standard UHMWPE (GUR 1050-ASTM F648-14), (2) highly cross-linked polyethylene with 75 kGy gamma radiation (HXPE-ASTM F648-14), and (3) vitamin-E infused polyethylene highly cross-linked polyethylene with 75 kGy gamma radiation (VEXPE UHMWPE-ASTM F-2695). Six pins of 9 mm diameter and 15 mm length were machined of each material type, with one flat and one hemispherical end (ASTM F732). The hemispherical end seats in a conical pin holder and ensures self-alignment of the flat end of the pin, finished to Ra < 1.5 μm, with the disc surface. Table 2 shows the surface topography of the articulating flat surface of a representative polyethylene pin of each material type, obtained with white light interferometry (Zygo NewView 5000), which reveals a shallow raised area in the center of the pin and concentric machining marks. A trace along the diameter of the pin further illustrates the scale of the surface topography. Table 2 also shows the average values for all six pins of each material type, of Ra, Rq, and Rt values, and the asperity density ns, mean radius of asperity summits Rs, and the standard deviation of asperity heights σs, derived from the white light interferometry data of the articulating surface, using an 8-nearest neighbor scheme . It was observed that the surface topography is almost independent of the material type, but that the articulating surfaces of the HXPE and VEXPE UHMWPE pins were slightly smoother than that of the regular UHMWPE surface, indicated by lower Ra, Rq, and Rt, and by lower ns, σs and higher Rs values.
Table 2.
White light interferometry image of the articulating surface of the UHMWPE pins, and average surface topography metrics of all pins
| Pin-type | UHMWPE GUR 1050 | HXPE | VEXPE UHMWPE |
|---|---|---|---|
|

|
|

|
| Ra [μm] | 1.312 | 0.869 | 0.874 |
| Rq [μm] | 1.816 | 1.531 | 1.325 |
| Rt [μm] | 197.651 | 181.585 | 135.389 |
| ns [1/μm2] | 0.491 | 0.098 | 0.112 |
| σs [μm] | 1.265 | 0.909 | 0.934 |
| Rs [μm] | 0.277 | 0.732 | 0.440 |
2.2 Wear testing apparatus
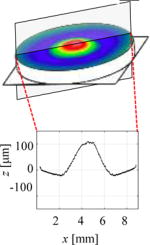
Figure 1 shows a schematic of the five-station POD tester developed at the University of Utah, which was employed to measure wear of the polyethylene pins when articulating with the CoCrMo discs under circular motion and static loading. A POD tester enables fast evaluation of a large number of material pairs (pin and disc) as a function of operating and environmental conditions. It is a well-established and widely accepted method in testing biomaterials, because experimental data is available to potentially benchmark with new results. Each station of the POD tester consists of a shaft supported by two linear bearings, driven by a closed-loop, velocity-controlled motor and gear mechanism, and loaded with deadweights (13 kg) to provide the desired contact pressure between the pin and disc. The eccentricity e determines the radius of the circular wear path. A sealed cup around each disc allows for lubrication during testing.
Figure 1.
Schematic of five-station pin-on-disc tester. Inset shows detail of polyethylene pin articulating with CoCrMo disc.
2.3 Testing procedure
The ASTM F732 standard was followed for wear testing, using a 10 mm diameter circular wear path of a polyethylene pin on a stationary CoCrMo disc. This results in a sliding distance of 31.4 mm per cycle, which falls within the in-vivo sliding distance that ranges between 8.6 and 33.6 mm measured for hips. Two million wear cycles were performed at a frequency of 1 Hz to approximate the frequency of human walking gait, a contact area of 63.6 mm2, and contact pressure of 2.0 MPa (ASTM F732). This contact area is much smaller than the physiological contact area in prosthetic hips, which ranges between 320 and 960 mm2. Saikko et al. suggested that contact pressure should not exceed 2.0 MPa in POD wear tests of prosthetic joint materials to best mimic in-vivo wear, although in-vivo contact pressure may be higher than 2 MPa. Filter-sterilized (1μm) bovine calf serum (Hyclone, Logan, UT) with 20 mg/ml protein concentration was used as lubricant, and the sliding interface between pin and disc is submerged at all time during the experiment. All polyethylene pins are pre-soaked for two weeks in the lubricant to reduce the fluid-sorption effect prior to testing, and one soak-control specimen is maintained for each experiment. Gravimetric methods were employed per ASTM F2025 to quantify polyethylene wear, at 80,000 cycle intervals, when all testing chambers were thoroughly cleaned and the lubricant was replaced. Weight measurements were repeated for each pin ten times using an analytical balance (Mettler Toledo ML 204, resolution = 0.1 mg, repeatability = 0.1 mg) and the average was reported. Wear debris size and shape was not analyzed in this work. All experiments were performed at room temperature.
2.4 Data analysis
A 3 × 6 (polyethylene material by disc microtexture) full factorial design was used to measure wear of all possible bearing pairs (different polyethylene materials and microtextured versus polished CoCrMo discs). To analyze the effect of each independent variable, results were grouped based on the polyethylene material and based on the disc microtexture. The null hypothesis defined that neither polyethylene material nor disc microtexture affected polyethylene wear and all bearing pairs wore at the same rate. To test this null hypothesis a student’s t-test was performed for two-tailed distributions with unequal variance between the groups. A p-value of 0.05 was considered statistically significant, as commonly used in other experimental studies of polyethylene wear of orthopedic materials. However, we report the actual p-values in the results and discussion section. Linear regression analysis was conducted to assess the relationship between the pin’s wear rate and average surface roughness of the pin’s bearing surface (Ra).
3. Results and discussion
Figure 2 shows polyethylene wear as a function of the number of wear cycles for UHMWPE GUR 1050 (Fig. 2(a)), HXPE (Fig. 2(b)), and VEXPE UHMWPE (Fig. 2(c)) articulating with smooth (Disc 1) and microtextured (Disc 2–6) CoCrMo discs. The results show that the polished disc always causes higher polyethylene wear than the microtextured discs, independent of the polyethylene type. The microtexture creates microhydrodynamic bearings, which compress the lubricant between the pin and disc, slightly increasing the lubricant film thickness for a constant bearing load. Hence, the increased lubricant film thickness reduces contact between the pin and disc, which in turn reduces friction and wear, as our research group has shown previously. Specifically, it was observed that Disc 4 (Sp = 0.1, ε = 0.01) consistently yields the lowest polyethylene wear, which indicates that this microtexture design is the most optimal for wear reduction in this work. Consequently, since the smooth CoCrMo discs (Disc 1) do not have microhydrodynamic bearings, they result in higher polyethylene wear. Furthermore, it is noted that UHMWPE GUR 1050 polyethylene wears almost three times as much as the cross-linked polyethylene material, as expected, independent of the CoCrMo disc used.
Figure 2.
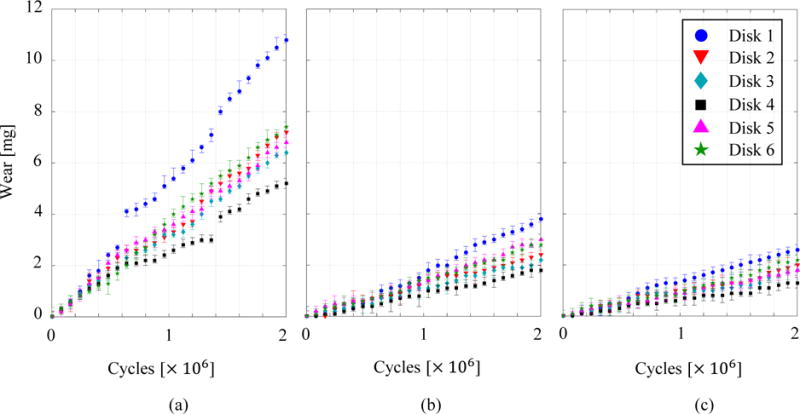
Polyethylene wear as a function of number of cycles for (a) UHMWPE GUR 1050, (b) HXPE, and (c) VEXPE UHMWPE, articulating with microtextured and polished CoCrMo discs. The data points show the average of ten wear measurements, whereas the error bars show the extreme wear measurement results.
Figure 3 shows polyethylene wear rate as a function of the number of wear cycles for UHMWPE GUR 1050 (Fig. 3(a)), HXPE (Fig. 3(b)), and VEXPE UHMWPE (Fig. 3(c)) articulating with smooth (Disc 1) and microtextured (Disc 2–6) CoCrMo discs. From Fig. 3 a break-in period was observed during which an elevated polyethylene wear rate occurs until approximately 600,000 wear cycles, after which the wear rate decreases, shown by changing slopes of the wear measurements documented in Fig. 2. This is likely due to machining marks or surface roughness peaks on the articulating surface of the polyethylene pin that are removed during the first thousands of wear cycles articulating with the CoCrMo disc. Also, it was observed that the wear rate of UHMWPE GUR 1050 increases after approximately 1.4 million wear cycles, likely due to the fatigue wear, based on the discontinuous wear versus number of cycles results shown in Fig. 2. A sub-surface crack may form due to contact pressure between the pin and disc, grows under cyclic loading, and eventually a wear particle separates from the polyethylene pin, which is observed as a discontinuous wear rate. Discontinuous wear rate results were observed with HXPE also, but not with VEXPE UHMWPE, which is likely due to the higher fatigue resistance of VEXPE UHMWPE compared to UHMWPE GUR 1050 and HXPE.
Figure 3.
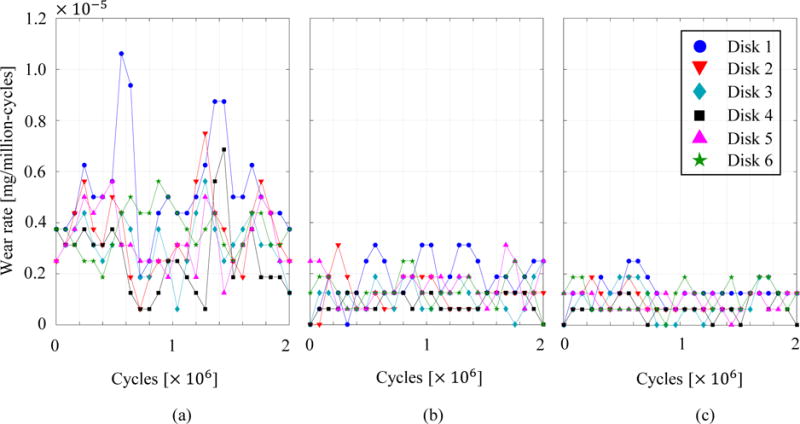
Polyethylene wear rate as a function of number of cycles for (a) UHMWPE GUR 1050, (b) HXPE, and (c) VEXPE UHMWPE, articulating with microtextured and polished CoCrMo discs
Table 3 lists the average wear rate in mg per million cycles (MC) for each combination of polyethylene and CoCrMo disc. The average wear of all experiments in this study with UHMWPE GUR 1050 is 3.65 mg/million-cycles after 2 million cycles (averaged over both smooth and textured discs), whereas the average wear for HXPE and VEXPE UHMWPE is 1.33 and 0.97 mg/million-cycles after 2 million cycles, respectively. Even though wear of HXPE and VEXPE UHMWPE is not significantly different (p = 0.059), the wear of UHMWPE GUR 1050 is significantly different from the other two materials (p = 0.001) for both UHMWPE GUR 1050 versus HXPE and versus VEXPE UHMWPE). HXPE and VEXPE UHMWPE wear significantly less than UHMWPE GUR 1050 pins due to their intrinsic resistance to shear stress resulting from cross-linking, which is well-known.
Table 3.
Average wear rate for each combination of polyethylene and CoCrMo disc in milligram per million cycles
| Pin | Average wear rate [mg/MC]
|
|||||
|---|---|---|---|---|---|---|
| Disc 1 | Disc 2 | Disc 3 | Disc 4 | Disc 5 | Disc 6 | |
| UHMWPE GUR 1050 | 5.4 | 3.6 | 3.2 | 2.6 | 3.4 | 3.7 |
| HXPE | 1.9 | 1.2 | 1.1 | 0.9 | 1.5 | 1.4 |
| VEXPE UHMWPE | 1.3 | 1.0 | 0.9 | 0.6 | 0.9 | 1.1 |
This result was also independently confirmed in a blind study performed at DePuy Synthes using an AMTI Orthopod test machine and a Paul loading curve per ISO 14242.
Wear results were correlated with the surface topography measurements of the polyethylene articulating surface to demonstrate the effectiveness of microtexture in creating microhydrodynamic bearings that increase lubricant film thickness for constant bearing load and, thus, to show how the texture features reduce contact and wear. Figure 4 shows a typical example of the articulating surface of a UHMWPE GUR 1050 pin, before (Fig. 4(a)) and after the wear experiments with microtextured CoCrMo Disc 4 (Fig. 4(b)) and the polished CoCrMo Disc 1, respectively. These discs were chosen because they result in the lowest (Disc 4) and highest (Disc 1) polyethylene wear in our experiments. From Fig. 4 it was observed that the polyethylene surface that articulates with Disc 4 remains almost completely intact, apart from a few scratches, even still displaying the original machining marks after 2.0 million wear cycles. In contrast, the polyethylene surface that articulates with the polished Disc 1 displays two deep scratches on the surface and none of the original machining marks remain.
Figure 4.
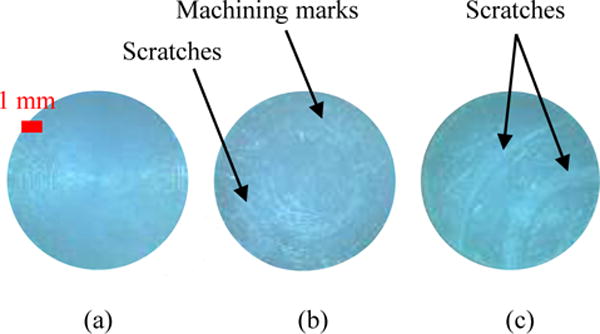
Surface topography of UHMWPE GUR 1050 (a) before a wear experiment, (b) after wear experiment with Disc 4, and (c) with Disc 1.
Surface topography of the articulating surface of the polyethylene pins was quantified before and after all wear experiments in this study. Figure 5 shows the average surface roughness (Ra) for UHMWPE GUR 1050 ((Fig. 5(a)), HXPE (Fig. 5(b)), and VEXPE UHMWPE (Fig. 5(c)) pins articulating with polished and microtextured discs. The correlation coefficient r between the increase of Ra (after – before wear experiment) and the corresponding wear was determined to be to be 0.82 for UHMWPE GUR 1050, 0.90 for HXPE, and 0.92 for VEXPE UHMWPE, respectively. This result substantiates that wear particles break away from the articulating surface and increase wear and surface roughness of the articulating surface. In agreement with the wear measurements shown in Fig. 2, it was observed that the polyethylene material articulating against the smooth CoCrMo disc (Disc 1) always displays the highest increase of Ra, independent of the polyethylene type. Correspondingly, it was also observed that the pin articulating against Disc 4, which resulted in the lowest wear, displayed the lowest Ra increase independent of the polyethylene material.
Figure 5.
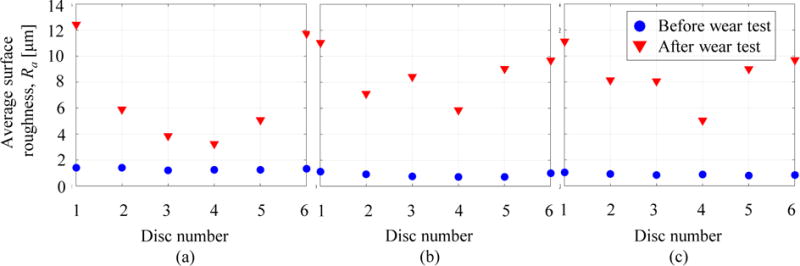
Average surface roughness Ra before and after wear testing for (a) UHMWPE GUR 1050, (b) HXPE, and (c) VEXPE UHMWPE
The primary limitations of the wear experiments documented in this paper are intrinsic to POD testing, and have been documented by others. Although POD testing enables quick evaluation of a large number of material pairs, the overly simplified flat-on-flat geometry does not represent the complex human joint geometry and articulation. Furthermore, the POD tester has a limited number of degrees-of-freedom (DOF) compared to the human joint, which affects the interface kinematics and how the material pair is loaded. For instance, the static loading implemented in this work neglects the dynamic in-vivo loading of the human joint. Also, the pin does not rotate about its own center axis and, thus, uni-directional sliding is used, as opposed to multi-directional sliding [50], which is generally considered to better mimic in-vivo kinematics. This work provides a relative comparison of polyethylene wear when articulating with microtextured and non-textured CoCrMo surfaces, without attempting to compare wear to previously published studies.
4. Conclusion
Polyethylene wear was reduced by adding a patterned microtexture of concave “dimples” to a polished CoCrMo disc, analogous to the surface finish and material of the femoral head of an MOP prosthetic hip bearing. Based on pin-on-disc wear measurements with a circularly rotating polyethylene pin on a CoCrMo disc, polyethylene wear was observed to be lower in all cases measured for microtextured compared to non-textured bearings. Combining wear with surface topography measurements demonstrated that the microtexture reduced wear by increasing the lubricant film thickness, which in turn decreased contact between the two articulating surfaces. Specifically, it was concluded that Disc 4 (Sp = 0.1, ε = 0.01) consistently yielded the lowest polyethylene wear, in-line with numerical optimization of the microtexture performed in earlier work.
Highlights.
Microtexture reduces polyethylene wear when articulating with CoCr discs
Microtexture reduces polyethylene wear independent of polyethylene material type
Surface roughness correlates with wear
Acknowledgments
A.B. and B.R. acknowledge support from the National Institutes of Health, National Institute of Arthritis and Musculoskeletal and Skin Diseases under grant 1R03AR066826-01A1.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Foran JRH. Website of the American Academy of Orthopaedic Surgeons. August 2015 [Online] Available: http://orthoinfo.aaos.org/topic.cfm?topic=A00377 [Accessed 11 April 2017]
- 2.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 3.Dumbleton J. Wear and its measurement for joint prosthesis materials. Wear. 1978;49(2):297. [Google Scholar]
- 4.Cooper J, Dowson D, Fisher J. Macroscopic and microscopic wear mechanisms in ultra-high molecular weight polyethylene. Wear. 1993;378:162–164. [Google Scholar]
- 5.Fisher J. Wear of ultra-high molecular weight polyethylene in total artificial joints. Curr Orthop. 1994;8(3):164. [Google Scholar]
- 6.Wang A, Essner A, Polineni V, Stark C, Dumbleton J. Lubrication and wear of ultra-high molecular weight polyethylene in total joint replacements. Tribol Int. 1998;31(1–3):17. [Google Scholar]
- 7.Jasty M, Smith E. Wear particles of total joint replacements and their role in periprosthetic osteolysis. Curr Opin Rheumatol. 1992;4(2):204. doi: 10.1097/00002281-199204000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Harris W. Wear and Periprosthetic Osteolysis: The Problem. Clin Orthop Relat Res 393: 66 (2001. 2001;393:66–70. doi: 10.1097/00003086-200112000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Dumbleton J, Manley M, Edidin A. A literature review of the association between wear rate and osteolysis in total hip arthroplasty. J Arthroplasty. 2002;17(5):649–661. doi: 10.1054/arth.2002.33664. [DOI] [PubMed] [Google Scholar]
- 10.Harris W. Conquest of a worldwide human disease: particle-induced periprosthetic osteolysis. Clin Orthop Relat Res. 2004;429:39–42. doi: 10.1097/01.blo.0000149821.72760.39. [DOI] [PubMed] [Google Scholar]
- 11.Marshall A, Ries M, Paprosky W. How prevalent are implant wear and osteolysis, and how has the scope of osteolysis changed since 2000? J Am Acad Orthop Surg 16: S1 (2008) 2008;16(Suppl 1):S1–6. doi: 10.5435/00124635-200800001-00003. [DOI] [PubMed] [Google Scholar]
- 12.Ong K, Lau E, Suggs J, Kurtz S, Manley M. Risk of subsequent revision after primary and revision total joint arthroplasty. Clin Orthop Rel Res. 2010;468:3070–3076. doi: 10.1007/s11999-010-1399-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whittaker J, Dharmarajan R, Toms A. The management of bone loss in revision total knee replacement. J Bone Joint Surg Br. 2008;90(8):981–7. doi: 10.1302/0301-620X.90B8.19948. [DOI] [PubMed] [Google Scholar]
- 14.McKellop H, Shen F, Lu B, Campbell P, Salovey R. Development of an extremely wear-resistant ultra high molecular weight polyethylene for total hip replacements. J Orthop Res 17:157(1999) 1999;17(2):157–67. doi: 10.1002/jor.1100170203. [DOI] [PubMed] [Google Scholar]
- 15.McKellop H, Shen F, Lu B, Campbell P, Salovey R. Effect of sterilization method and other modifications on the wear resistance of acetabular cups made of ultra-high molecular weight polyethylene. A hip-simulator study. J Bone Joint Surg Am. 2000;82-A(12):1708–25. doi: 10.2106/00004623-200012000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Muratoglu O, Bragdon C, O’Connor D, Jasty M, Harris W. A novel method of cross-linking ultra-high-molecular-weight polyethylene to improve wear, reduce oxidation, and retain mechanical properties. J Arthroplasty. 2001;16(2):149–160. doi: 10.1054/arth.2001.20540. [DOI] [PubMed] [Google Scholar]
- 17.Heisel C, Silva M, Rosa MD, Schmalzried T. Short-term in vivo wear of cross-linked polyethylene. J Bone Joint Surg Am 86: 748 (2004) 2004;86-A(4):748–51. doi: 10.2106/00004623-200404000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Kurtz S, Patel J. The Clinical Performance of Highly Cross-linked UHMWPE in Hip Replacements. in UHMWPE Biomaterials Handbook, Elsevier. 2015:57–71. [Google Scholar]
- 19.Kurtz S, Gawel H, Patel J. History and Systematic Review of Wear and Osteolysis Outcomes for First-generation Highly Crosslinked Polyethylene. Clinical Orthopaedics and Related Research. 2011;469(8):2262–77. doi: 10.1007/s11999-011-1872-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Davidson J, Mishra A, Poggie R, Wert JJ. Sliding friction and UHMWPE wear comparison between cobalt alloy and zirconia surfaces. Trans Orthop Res Soc. 1992;211(1):404. [Google Scholar]
- 21.Wang K. The use of titanium for medical applications in the USA. Mater Sci Eng. 1996;213(1–2):134–137. [Google Scholar]
- 22.Piconi C, Maccauro G. Zirconia as a ceramic biomaterial. Biomater. 1999;20(1):1–25. doi: 10.1016/s0142-9612(98)00010-6. [DOI] [PubMed] [Google Scholar]
- 23.Agarwal A, Dahotre NB. Mechanical properties of laser engineering composite boride coating on steel: a nanoindentation approach. Metall Mater Trans. 2000;31 A:401. [Google Scholar]
- 24.Yang Y, Ong J, Tian J. Deposition of highly adhesive ZrO2 coating on Ti and CoCrMo implant materials using plasma spraying. Biomater. 2003;24(4):619–627. doi: 10.1016/s0142-9612(02)00376-9. [DOI] [PubMed] [Google Scholar]
- 25.Sychterz C, E C, Jr, Young A, H R, Jr, Engh C. Comparison of in vivo wear between polyethylene liners articulating with ceramic and cobalt-chrome femoral heads. J Bone Jt Surg B. 2000;82(7):948–951. doi: 10.1302/0301-620x.82b7.9885. [DOI] [PubMed] [Google Scholar]
- 26.Rahaman M, Yao A, Bal B, Garino J, Ries M. Ceramics for prosthetic hip and knee joint replacement. J Am Ceram Soc. 2007;90(7):1965–1988. [Google Scholar]
- 27.Hamadouche M, Madi F, Kerboull L, Courpied JP, Kerboull M. Early femoral osteolysis following Charnley-Kerboull total hip arthroplasty combining a 22-mm zirconia head on polyethylene. Rev Chir Orthop Reparatrice Appar Mot. 2005;91(5):439–45. doi: 10.1016/s0035-1040(05)84361-2. [DOI] [PubMed] [Google Scholar]
- 28.Etsion I. State-of-the-art in laser surface texturing. J Tribol. 2005;127(1):248–253. [Google Scholar]
- 29.Ito H, Kaneda K, Yuhta T, Nishimura I, Yasuda K, Matsuno T. Reduction of polyethylene wear by concave dimples on the frictional surface in artificial hip joints. J Arthroplasty. 2000;15(3):332–338. doi: 10.1016/s0883-5403(00)90670-3. [DOI] [PubMed] [Google Scholar]
- 30.Sawano H, Warisawa S, Ishihara S. Study on long life of artificial joints by investigating optimal sliding surface geometry for improvement in wear resistance. Precis Eng. 2009;33(4):492–498. [Google Scholar]
- 31.Roy T, Choudhury D, Ghosh S, Mamat AB, Pingguan-Murphy B. Improved friction and wear performance of micro dimpled ceramic-on-ceramic interface for hip joint arthroplasty. Ceram Int. 2015;41(1):681–690. [Google Scholar]
- 32.Cho M, Choi H-J. Optimization of Surface Texturing for Contact Between Steel and Ultrahigh Molecular Weight Polyethylene Under Boundary Lubrication. Tribol Lett. 2014;56(3):409–422. [Google Scholar]
- 33.Chyr A, Qiu M, Speltz JW, Jacobsen RL, Sanders AP, Raeymaekers B. A patterned microtexture to reduce friction and increase longevity of prosthetic hip joints. Wear. 2014;315(1–2):51–57. doi: 10.1016/j.wear.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Qiu M, Minson BR, Raeymaekers B. The effect of texture shape on the friction coefficient and stiffness of gas-lubricated parallel slider bearings. Tribol Int. 2013;67:278–288. [Google Scholar]
- 35.ASTM International. West Conshohocken; PA: 2008. ASTM F1537-08, “Standard Specification for Wrought Cobalt-28Chromium-6Molybdenum Alloys for Surgical Implants (UNS R31537, UNS R31538, and UNS R31539)”. www.astm.org. [Google Scholar]
- 36.ASTM International. West Conshohocken; PA: 2014. ASTM F648-14, “Standard Specification for Ultra-High-Molecular-Weight Polyethylene Powder and Fabricated Form for Surgical Implants”. www.astm.org. [Google Scholar]
- 37.ASTM International. West Conshohocken; PA: 2012. ASTM F2695-12, “Standard Specification for Ultra-High Molecular Weight Polyethylene Powder Blended With Alpha-Tocopherol (Vitamin E) and Fabricated Forms for Surgical Implant Applications”. www.astm.org. [Google Scholar]
- 38.ASTM International. West Conshohocken; PA: 2011. ASTM F732-00(2011), “Standard Test Method for Wear Testing of Polymeric Materials Used in Total Joint Prostheses”. www.astm.org. [Google Scholar]
- 39.Pawar G, Pawlus P, Etsion I, Raeymaekers B. The effect of determining topography parameters on analyzing elastic contact between isotropic rough surfaces. J Tribol. 2013;135(1) [Google Scholar]
- 40.Bennett D, Humphreys L, O’Brien S, Kelly C, Orr J, Beverland D. The influence of wear paths produced by hip replacement patients during normal walking on wear rates. J Orthop Res. 2008;26(9):1210–7. doi: 10.1002/jor.20583. [DOI] [PubMed] [Google Scholar]
- 41.Murray M, Drought A, Kory R. Walking patterns of normal men. Journal of Bone and Joint surgery. 1964 jbjs.org. [PubMed]
- 42.Michael H, Catledge S, Konovalov V, Clem W, Chowdhury S, Etheridge B, Stanishevsky A, Lemons J, Vohra Y, Eberhardt A. Preliminary Tribological Evaluation of Nanostructured Diamond Coatings against Ultra-High Molecular Weight Polyethylene. J Biomed Mater Res B Appl Biomater. 2008;85(1):140–8. doi: 10.1002/jbm.b.30926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Saikko V. Effect of Contact Pressure on Wear and Friction of Ultra-High Molecular Weight Polyethylene in Multidirectional Sliding. Proceedings of the Institution of Mechanical Engineers, Part H: Journal of Engineering in Medicine. 2006;220(7):723–31. doi: 10.1243/09544119JEIM146. [DOI] [PubMed] [Google Scholar]
- 44.Saikko V. Effect of Lubricant Protein Concentration on the Wear of Ultra-High Molecular Weight Polyethylene Sliding Against a CoCr Counterface. J Tribol. 2003;125(3):638–642. [Google Scholar]
- 45.ASTM International. West Conshohocken; PA: 2012. ASTM F2025-06(2012), “Standard Practice for Gravimetric Measurement of Polymeric Components for Wear Assessment”. www.astm.org. [Google Scholar]
- 46.Oral E, Christensen SD, Malhi AS, Wannomae KK, Muratoglu OK. Wear resistance and mechanical properties of highly crosslinked UHMWPE dopped with vitamin-E. J Arthroplasty. 2006;21(4):580–591. doi: 10.1016/j.arth.2005.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Qiu M, Delic A, Raeymaekers B. The Effect of Texture Shape on the Load-Carrying Capacity of Gas-Lubricated Parallel Slider Bearings. Tribology Letters. 2012;48(3):315–327. [Google Scholar]
- 48.Qiu M, Chyr A, Sanders AP, Raeymaekers B. Designing prosthetic knee joints with bio-inspired bearing surfaces. Tribology International. 2014;77:106–110. doi: 10.1016/j.triboint.2014.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Blau P. Society of Tribologists and Lubrication Engineers Annual Meeting and Exhibition. Lake Buena Vista; United States; 2014. The use and misuse of the pin-on-disk wear test. [Google Scholar]
- 50.Wang A, Polineni VK, Essner A, Sokol M, Sun D, Stark C, Dumbleton J. The significance of nonlinear motion in the wear screening of orthopaedic implant materials. Journal of Testing and Evaluation. 1997;25(2):239–245. [Google Scholar]


