Abstract
Objective
This study was designed to explore the time trends in geographical variations of cervical cancer mortality in mainland China over the period 1973 to 2013, to provide subnational spatio-temporal patterns for targeted promotion of human papillomavirus vaccine in China.
Methods
Data were extracted from three national retrospective death surveys and cancer registry. The rate ratio (RR) was estimated for the aggregated data for seven geographical regions using generalized linear models to evaluate time trends in geographical disparities of cervical cancer mortality.
Results
There was a significant decrease in cervical cancer mortality in China from 1973–1975 to 2004–2005, but leveled off thereafter to 2011–2013. Compared to the period 1973–1975 the RR for the three last time periods were 0.33 [95% confidence interval (95% CI): 0.30–0.37] for 1990–1992, 0.21 (95% CI: 0.19–0.24) for 2004–2005 and 0.24 (95% CI: 0.22–0.26) for 2011–2013. Females living in the Northwest China and Central China have a high risk of mortality from cervical cancer compared to the nationwide, with the RR being 2.09 (95% CI: 1.83–2.38) and 1.26 (95% CI: 1.11–1.44) respectively, while the RRs for South China, Northeast China and Southwest China were below 1.00, indicating the lower death risk. Despite the mortality rate had increased slightly from 2004 to 2013, there was an encouraging sign that the geographical disparities in cervical cancer mortality had gradually narrowed over time across China.
Conclusions
Although cervical cancer mortality in China has reduced to very low levels, the high risk of cervical cancer in Northwest China and Central China is still noteworthy. Public health policies including the promotion of vaccine should be targeted to further reduction of geographical disparities in cervical cancer mortality.
Keywords: Cervical cancer, mortality, spatio-temporal, epidemiology, China
Introduction
As one of the most common gynecologic cancers, cervical cancer was estimated to cause 265,700 female deaths worldwide in 2012, and was the fourth leading cause of cancer mortality in women (1). The burden of cervical cancer was more severe in less developed countries, with standardized mortality rates about 2.5 times that of developed countries (8.3 to 3.3 per 100,000) (1). In China, there were 24,500 and 26,400 estimated death cases of cervical cancer in 2012 and 2013, with age-standardized mortality rate (ASMR) 2.64 and 2.62 per 100,000 respectively (2-4).
There was a large geographical variation in cervical cancer incidence and mortality rates worldwide. Incidence and mortality rates are the highest in sub-Saharan Africa, Latin America and the Caribbean, and Melanesia and the lowest in Western Asia, Australia/New Zealand, and Northern America (2,5). In Eastern, Middle, and Southern Africa, as well as Melanesia, cervical cancer is the leading cause of cancer death in females (2). There is very limited research on the geographical distribution of cervical cancer incidence or mortality in China. The only study and cancer atlas on the geographical distribution of cervical cancer was based on the First National Survey of Death Causes for the period 1973–1975 (6). However, it has been more than 40 years from the time which the study was carried out, resulting in the dilemma that there was no study on the latest geographical distribution of cervical cancer in China.
Globally, the age-standardized incidence rates for cervical cancer keep decreased from 1990 to 2015, the total incidence rate of cervical cancer would have decreased 26% due to the decreasing incidence rates after adjusted by population size and age structure from 2005 to 2015 (7). Compared three death surveys in 1973, 1992 and 2005, the mortality rates of cervical cancer kept declining in China (8,9). However, the mortality rate of cervical cancer from cancer registration in China had shown an increase since 2000s (4,10). During 2001–2013, the ASMR of cervical cancer increased by 5.7% per year, and the trend was significant (4). These studies are focusing on the nationwide and have some flaws, that is, either covering a short-term period or just a descriptive research.
Since the late 1970s, when the initiation of economic reforms in China began to lead to a rapid socioeconomic transformation and a shift from a predominately rural lifestyle to a more urban lifestyle, the distribution of cervical cancer in China might have shifted. To address these concerns, this study was designed to access the geographical variation and time trends in cervical cancer mortality from mid-1970s to early 2010s.
Materials and methods
Data sources
Cervical cancer mortality data were extracted from three national retrospective surveys on cause of death from 1973 to 2005 and the National Central Cancer Registry of China in 2011–2013. The data included the number and age of people dying from cervical cancer, and the corresponding population of each geographical area. The three surveys of cause of death in China have been described in detail in previous publications (11-13). Briefly, the First National Survey of Death Causes for the period 1973–1975 covered nearly all regions of mainland China (excluding Taiwan, Hong Kong, Macau, and 35 sparsely populated counties) (11). The Second National Retrospective Sampling Survey of Death Causes for the period 1990–1992 included 263 sample points (12). The Third National Retrospective Sampling Survey of Death Causes for the period 2004–2005 covered 213 counties/cities/districts (13). A total of 625 qualified cancer registries from 31 provinces were involved in 2011–2013 cancer report in China, the overall population coverage was 600 million (304 million males and 296 million females) (2-4,14).
Data analysis
The basic geographical unit of analysis (building block) used in this study is province. We divided mainland China into seven geographical regions (Figure 1) in order to fit a spatio-temporal model. The ASMR was calculated using the direct standardization method (to the Segi standard population), for each province and geographical region and each of the four periods.
1.
Schematic diagram of the division of China into seven geographical regions.
The provincial level data were then aggregated into seven geographical regions. We used generalized linear models with a negative binomial error structure [to overcome over-dispersion (15)] to calculate rate ratio (RR) of death from cervical cancer for the aggregated data for geographical regions (with national average as a reference) after controlling for the other factors included in the model. A detailed description of the models can be found in our previous publications (16,17). Briefly, these analyses consisted of two models. First, we fitted a model with the main-effect variables of age group at death and region, stratified by the period (1973–1975, 1990–1992, 2004–2005 and 2011–2013) to test whether the effect of region was significant in each period. Then we fitted the second model with the variables of age group, region and period included to test whether the effect of period was significant and also to validate whether the effect of region was still significant after further adjustment for period. Lastly, we added an interaction term between geographical region and period to the second model, and then a likelihood ratio test was conducted to determine if this interaction was significant to see whether the geographical variation over period is significant.
All significance tests with P<0.05 were taken to indicate statistical significance. Statistical analyses were performed in R software (Version 3.4.1; R Foundation for Statistical Computing, Vienna, Austria).
Results
Mortality rate
From the mid-1970s to the early 2010s there was a decrease in cervical cancer mortality in China, as shown in Table 1. Average crude mortality rates decreased from 11.35 per 100,000 in 1973–1975, to 3.89 per 100,000 in 1990–1992, 2.89 per 100,000 in 2004–2005 and 3.89 per 100,000 in 2011–2013, and ASMR decreased from 14.47 per 100,000 in 1973–1975, to 4.29 per 100,000 in 1990–1992, 2.45 per 100,000 in 2004–2005 and 2.53 per 100,000 in 2011–2013.
1.
Death case, population, crude mortality rate (per 100,000) and age-standardized mortality rate (per 100,000) of cervical cancer in China, 1973–2013
| Region | Period | Death case | Person years (million) | Crude mortality rate | ASMR |
| ASMR, age-standardized mortality rate. | |||||
| North China | 1973–1975 | 21,167 | 135.93 | 15.57 | 18.65 |
| Northeast China | 1973–1975 | 9,506 | 127.08 | 7.48 | 11.22 |
| East China | 1973–1975 | 40,538 | 340.19 | 11.92 | 14.26 |
| Central China | 1973–1975 | 36,264 | 229.07 | 15.83 | 19.90 |
| South China | 1973–1975 | 5,121 | 104.71 | 4.89 | 6.10 |
| Southwest China | 1973–1975 | 14,979 | 210.49 | 7.12 | 9.36 |
| Northwest China | 1973–1975 | 12,026 | 81.98 | 14.67 | 21.03 |
| China | 1973–1975 | 139,601 | 1,229.44 | 11.35 | 14.47 |
| North China | 1990–1992 | 807 | 16.61 | 4.86 | 5.36 |
| Northeast China | 1990–1992 | 186 | 11.87 | 1.57 | 2.04 |
| East China | 1990–1992 | 2,031 | 50.35 | 4.03 | 4.09 |
| Central China | 1990–1992 | 1,246 | 30.62 | 4.07 | 4.50 |
| South China | 1990–1992 | 491 | 18.52 | 2.65 | 2.87 |
| Southwest China | 1990–1992 | 599 | 23.88 | 2.51 | 2.88 |
| Northwest China | 1990–1992 | 977 | 10.94 | 8.93 | 11.37 |
| China | 1990–1992 | 6,337 | 162.79 | 3.89 | 4.29 |
| North China | 2004–2005 | 374 | 11.07 | 3.38 | 2.63 |
| Northeast China | 2004–2005 | 161 | 8.58 | 1.88 | 1.52 |
| East China | 2004–2005 | 887 | 34.78 | 2.55 | 1.96 |
| Central China | 2004–2005 | 607 | 18.48 | 3.28 | 3.06 |
| South China | 2004–2005 | 240 | 10.12 | 2.37 | 2.09 |
| Southwest China | 2004–2005 | 280 | 13.80 | 2.03 | 1.81 |
| Northwest China | 2004–2005 | 449 | 6.94 | 6.47 | 6.98 |
| China | 2004–2005 | 2,998 | 103.78 | 2.89 | 2.45 |
| North China | 2011–2013 | 1,498 | 45.75 | 3.27 | 2.01 |
| Northeast China | 2011–2013 | 1,280 | 26.27 | 4.87 | 2.88 |
| East China | 2011–2013 | 4,518 | 130.64 | 3.46 | 2.14 |
| Central China | 2011–2013 | 2,214 | 41.59 | 5.32 | 3.83 |
| South China | 2011–2013 | 844 | 24.70 | 3.42 | 2.59 |
| Southwest China | 2011–2013 | 622 | 16.18 | 3.84 | 2.58 |
| Northwest China | 2011–2013 | 536 | 10.84 | 4.94 | 3.84 |
| China | 2011–2013 | 11,512 | 295.98 | 3.89 | 2.53 |
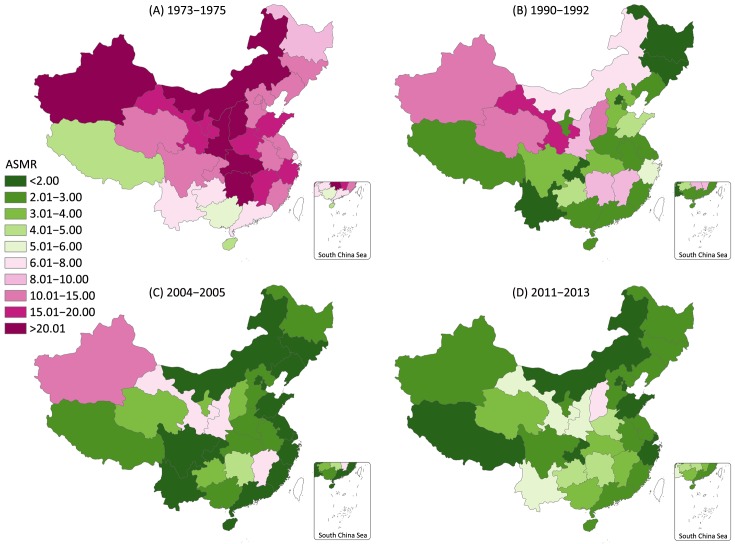
Values for the provincial ASMR estimates are presented in Supplementary Table S1. The overall ASMR of cervical cancer by province for the four periods is shown in Figure 2. In the period 1973–1975, Shanxi had the highest ASMR (29.67 per 100,000), followed by Inner Mongolia, Shaanxi, Hubei, Hunan and Xinjiang, while the provinces in Southwest China had lower rates, the lowest ASMR were observed in Tibet, Hainan and Guangxi. In the period 1990–1992, Gansu and Shanxi had the highest cervical cancer ASMR (15.17 per 100,000 and 14.46 per 100,000), while the ASMR for Jilin, Yunnan, Chongqing, Beijing and Heilongjiang fell below 2.00 per 100,000, with the remaining provinces ranged from 2.11 per 100,000 to 11.37 per 100,000. In 2004–2005, the only province with cervical cancer ASMR over 10.00 per 100,000 person-years was Xinjiang Uygur Autonomous Region (10.04 per 100,000), the second to fourth highest ASMR were observed in Gansu, Shaanxi and Jiangxi, while the mortality rates recorded in the other 26 provinces except Hunan were lower than 4.00 per 100,000, with 15 and 22 provinces having rates of less than 2.00 and 3.00 per 100,000 respectively. In 2011–2013, the areas with the highest cervical cancer ASMR were Shanxi province (7.46 per 100,000) and Gansu province (5.87 per 100,000), while the mortality rates recorded in the other 28 provinces except Tibet had relatively similar and lower mortality rate.
S1.
Age-standardized mortality rate (per 100,000) of cervical cancer by province as recorded during four periods in mainland China, 1973–1975, 1990–1992, 2004–2005 and 2011–2013
| Code | Region | 1973–1975 | 1990–1992 | 2004–2005 | 2011–2013 |
| 110000 | Beijing | 10.91 | 1.88 | 1.23 | 1.56 |
| 120000 | Tianjin | 13.07 | 2.31 | 1.89 | 1.61 |
| 130000 | Hebei | 14.98 | 3.26 | 2.82 | 2.59 |
| 140000 | Shanxi | 29.61 | 14.46 | 3.97 | 7.46 |
| 150000 | Inner Mongolia | 25.24 | 7.58 | 1.54 | 1.57 |
| 210000 | Liaoning | 11.94 | 2.47 | 1.03 | 2.99 |
| 220000 | Jilin | 12.10 | 1.62 | 1.86 | 2.71 |
| 230000 | Heilongjiang | 9.44 | 1.88 | 2.11 | 2.62 |
| 310000 | Shanghai | 7.87 | 2.11 | 0.91 | 1.78 |
| 320000 | Jiangsu | 13.12 | 2.84 | 1.18 | 2.22 |
| 330000 | Zhejiang | 15.83 | 5.55 | 1.91 | 1.96 |
| 340000 | Anhui | 11.78 | 2.51 | 2.69 | 2.57 |
| 350000 | Fujian | 11.63 | 2.95 | 1.66 | 2.08 |
| 360000 | Jiangxi | 17.39 | 8.33 | 6.10 | 3.97 |
| 370000 | Shandong | 18.56 | 4.76 | 1.24 | 1.81 |
| 410000 | Henan | 16.20 | 2.33 | 2.32 | 4.20 |
| 420000 | Hubei | 23.07 | 3.18 | 2.93 | 3.23 |
| 430000 | Hunan | 22.63 | 8.80 | 4.69 | 4.12 |
| 440000 | Guangdong | 6.33 | 2.93 | 1.88 | 2.24 |
| 450000 | Guangxi | 5.84 | 2.74 | 2.62 | 3.74 |
| 460000 | Hainan | 4.81 | 2.75 | 0.93 | 2.11 |
| 500000 | Chongqing | 11.43 | 1.85 | 1.06 | 1.78 |
| 510000 | Sichuan | 10.77 | 3.21 | 1.87 | 2.31 |
| 520000 | Guizhou | 6.92 | 4.39 | 3.74 | 4.09 |
| 530000 | Yunnan | 6.65 | 1.78 | 1.50 | 5.04 |
| 540000 | Tibet | 4.06 | 2.88 | 2.72 | 0.85 |
| 610000 | Shaanxi | 23.60 | 9.66 | 6.37 | 5.07 |
| 620000 | Gansu | 17.96 | 15.17 | 7.44 | 5.87 |
| 630000 | Qinghai | 10.08 | 11.37 | 3.58 | 3.55 |
| 640000 | Ningxia | 19.16 | 2.95 | 3.96 | 2.75 |
| 650000 | Xinjiang | 21.93 | 11.37 | 10.04 | 2.39 |
2.
Provincial cervical cancer age-standardized morality rates (ASMR) of mainland China during four periods, excluding Taiwan, Hong Kong and Macau, China. (A) 1973–1975, the First National Survey of Death Causes; (B) 1990–1992, the Second National Sampling Survey of Death Causes; (C) 2004–2005, the Third National Survey of Death Causes; (D) 2011–2013, the 625 qualified cancer registries.
The ASMR of cervical cancer by geographical region for four periods is shown in Table 1. Overall, the census carried out in 1973–1975 covered much more death cases in every region than the other three sample periods, at the same time, ASMR in every region was always much higher than those in the other three periods. Women living in Northwest China had the highest ASMR across all four periods, followed by Central China for period 1973–1975, 2004–2005 and 2011–2013 and North China for period 1990–1992, while women living in the coastal provinces having the lower mortality rates, and the lowest rates were observed in South China, Northeast China, Northeast China and North China for period 1973–1975, 1990–1992, 2004–2005 and 2011–2013, respectively. These patterns of variation are similar to those by province but are smaller in magnitude and more stable.
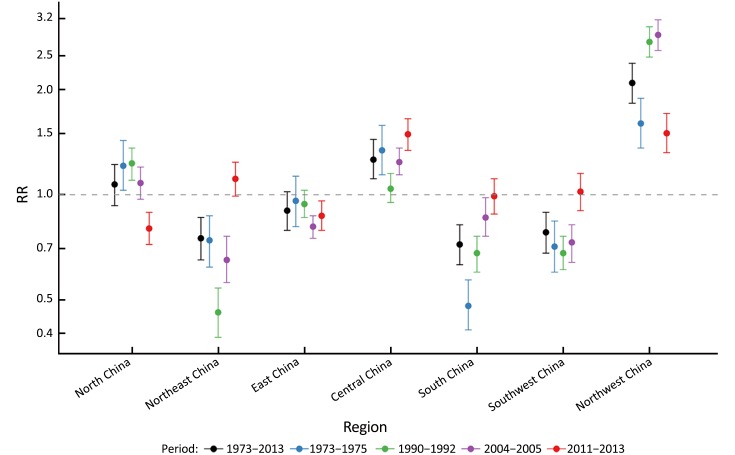
Geographical disparities
Estimates of the RR for cervical cancer death across the seven geographical regions over the whole period and four sub-periods are shown in Figure 3. Values of these RR estimates and P-values for the effect of region are presented in Supplementary Table S2. The variation in cervical cancer mortality was significant (P<0.0001) between the seven geographical regions for each of the study periods. Compared with national average of each period in China, women living in Northwest China had a much higher risk of mortality from cervical cancer for all four study periods, with the RR being 1.60 (95% CI: 1.36–1.89) in 1973–1975, 2.74 (95% CI: 2.48–3.03) in 1990–1992, 2.87 (95% CI: 2.59–3.17) in 2004–2005 and 1.50 (95% CI: 1.32–1.71) in 2011–2013. South China, Northeast China and Southwest China had a lower risk of cervical cancer death in the first three periods, on the contrary, these areas had an elevated risk of death in 2011–2013 with the RR being 0.99 (95% CI: 0.88–1.11), 1.11 (95% CI: 0.99–1.24) and 1.02 (95% CI: 0.90–1.15) respectively. After adjusted by study period and age structure, the RR for Northwest China and Central China were 2.09 (95% CI: 1.83–2.38) and 1.26 (95% CI: 1.11–1.44) respectively, while the RR for South China, Northeast China and Southwest China were significantly below 1.00, indicating the lower risk of death using the national average risk as reference.
3.
Rate ratio (RR, log measure in Y-axis) for mortality from cervical cancer in China by geographical regions for the entire period from 1973 to 2013 and the sub-period 1973–1975, 1990–1992, 2004–2005 and 2011–2013 with national average being the reference (1.00) (bars around the point estimate are the 95% confidence intervals).
S2.
Mortality rate ratio of cervical cancer by geographical regions from 1973 to 2013
| Period | Region | RR (95% CI) |
| RR, rate ratio; 95% CI, 95% confidence interval. | ||
| 1973–1975 | North China | 1.21 (1.03–1.43) |
| 1973–1975 | Northeast China | 0.74 (0.62–0.87) |
| 1973–1975 | East China | 0.96 (0.81–1.13) |
| 1973–1975 | Central China | 1.34 (1.14–1.58) |
| 1973–1975 | South China | 0.48 (0.41–0.57) |
| 1973–1975 | Southwest China | 0.71 (0.60–0.84) |
| 1973–1975 | Northwest China | 1.60 (1.36–1.89) |
| 1990–1992 | North China | 1.23 (1.10–1.36) |
| 1990–1992 | Northeast China | 0.46 (0.39–0.54) |
| 1990–1992 | East China | 0.94 (0.86–1.03) |
| 1990–1992 | Central China | 1.04 (0.95–1.15) |
| 1990–1992 | South China | 0.68 (0.60–0.76) |
| 1990–1992 | Southwest China | 0.68 (0.61–0.76) |
| 1990–1992 | Northwest China | 2.74 (2.48–3.03) |
| 2004–2005 | North China | 1.08 (0.97–1.20) |
| 2004–2005 | Northeast China | 0.65 (0.56–0.76) |
| 2004–2005 | East China | 0.81 (0.75–0.87) |
| 2004–2005 | Central China | 1.24 (1.14–1.36) |
| 2004–2005 | South China | 0.86 (0.76–0.98) |
| 2004–2005 | Southwest China | 0.73 (0.64–0.82) |
| 2004–2005 | Northwest China | 2.87 (2.59–3.17) |
| 2011–2013 | North China | 0.80 (0.72–0.89) |
| 2011–2013 | Northeast China | 1.11 (0.99–1.24) |
| 2011–2013 | East China | 0.87 (0.79–0.96) |
| 2011–2013 | Central China | 1.49 (1.34–1.65) |
| 2011–2013 | South China | 0.99 (0.88–1.11) |
| 2011–2013 | Southwest China | 1.02 (0.90–1.15) |
| 2011–2013 | Northwest China | 1.50 (1.32–1.71) |
| 1973–2013 | North China | 1.07 (0.93–1.22) |
| 1973–2013 | Northeast China | 0.75 (0.65–0.86) |
| 1973–2013 | East China | 0.90 (0.79–1.02) |
| 1973–2013 | Central China | 1.26 (1.11–1.44) |
| 1973–2013 | South China | 0.72 (0.63–0.82) |
| 1973–2013 | Southwest China | 0.78 (0.68–0.89) |
| 1973–2013 | Northwest China | 2.09 (1.83–2.38) |
Time trends
Consistent with the results of ASMR by geographical region over time, the effect of study period was significant with P<0.0001 after adjusting for age and region effects, confirming that the decreasing trend in the mortality of cervical cancer was significant. After adjusting for age and region effects, the RR for study period were 0.33 (95% CI: 0.30–0.37) for 1990–1992, 0.21 (95% CI: 0.19–0.24) for 2004–2005 and 0.24 (95% CI: 0.22–0.26) for 2011–2013, compared with the first death survey in 1973–1975.
The interaction between geographical region and study period was also significant (P<0.0001), indicating that the geographical differential in cervical cancer mortality had narrowed over time.
Discussion
In this study, we analyzed the long-term cervical cancer data systematically and identified three important patterns. First, the overall mortality rate for cervical cancer decreased significantly during the period 1973–2005, but leveled off thereafter. The national ASMR of cervical cancer declined by 70.4% from the mid-1970s to early 1990s and then by 83.1% and 82.5% to the mid-2000s and early 2010s respectively. The general downward trend from mid-1970s to mid-2000s was confirmed by Chinese local publications (9). An upward trend from mid-2000s to early 2010s was moderate compared with the result from the data based on cancer registry only, which showed that the ASMR of cervical cancer in the mainland China increased (5.7% per year) from 2000 to 2013 (4). After adjusting for age and region effects, the RR for the three later study periods were lower than 1.00, which confirmed that the cervical cancer death risk had generally declined in China over the past 40 years across China. However, the higher RR in 2011–2013 than 2004–2005 demonstrated that beginning in 2004, cervical cancer mortality rates might have uplifted (P>0.05), and this situation may require the implementation of effective measures to reduce the mortality rate in Chinese women.
Secondly, geographical variations in cervical cancer mortality rates were observed for each study period from 1973–1975 to 2011–2013 in mainland China. In general, the cervical cancer mortality rates of Northwest China, including Xinjiang, Gansu and Shaanxi provinces, together with Shanxi province were higher than those in other provinces of China. While the provinces in Southwest China and Northeast China, as well as all coastal provinces had a relatively lower ASMR from cervical cancer. These geographical disparities of cervical cancer mortality were confirmed by the following statistical models and all the differences were significant (P<0.001). The general patterns we reported are similar to findings from previous cross-sectional descriptive studies (18), while our study covers a long period and also further extends these findings by fitting a series of models to quantify this variation and to test whether the geographical variation was significant.
Thirdly, the geographical disparities of cervical cancer mortality were found to have narrowed over time. The narrowing geographical disparities were likely to be caused by different level of decline over time by region. ASMR showed a more rapid decrease from 1973 to 2013 in the North China (–16.64 per 100,000, 9.28 times) and Northwest China (–17.19 per 100,000, 5.48 times), while in the Southwest China and South China the decline were moderate (–6.78 per 100,000, 3.63 times for Southwest China and –3.51 per 100,000, 2.36 times for South China).
The decreasing trends in cervical cancer mortality from 1973 to 2005 can be explained by a reduction in the prevalence of human papillomavirus (HPV) infection, mass screening and improved treatment, as well as a reduction in the population’s exposure to risk factors. It’s believed that HPV infection plays a key role in cervical cancer occurrence, the decreased prevalence of high-risk HPV was observed in several Chinese populations (19,20). Variations in the other risk factors such as smoking, sexual behaviors and personal hygiene, may also provide a reasonable explanation for the temporal trends of cervical cancer in China (21). Secondary prevention for cervical cancer, including screening in high-risk populations and early detection, early diagnosis and early treatment, probably played an important role in the downward trend of cervical cancer mortality in China (19,20). High-risk women in China have been screened extensively for early detection of cervical cancer since the 1960’s (22), and more than 10 million women from all 31 provinces of mainland China were covered every year recently (23). Improvements in treatment may be another important factor in the decline of mortality, as the increase in the survival rate for cervical cancer (24).
HPV infection, especially the high-risk HPV infection is recognized as the most important risk factor for cervical cancer, it was estimated that as much as 99.4% (95% CI: 97.7%–100%) death can be attributable to HPV infection in China (25). Given this fact, it is reasonable to attribute geographical disparities in cervical cancer mortality to the variation in HPV prevalence. Several nationwide studies had confirmed the higher HPV infection rate was observed in the region with a heavy burden of cervical cancer in China, while the lower HPV infection rate was detected in the areas with prosperous economy and more robust healthcare system (26). Consistent with the cervical cancer mortality, the prevalence of high-risk HPV in rural women was also higher than that in urban women (26,27). Other risk factors, such as socioeconomic status, educational level, smoking, sexual behaviors and personal hygiene, are likely to increase the occurrence of cervical cancer by increasing the risk of HPV infection indirectly (21). In Northwest China and Shanxi province, the lagging behind hygienic condition and economic level might be one of the reasons leading to higher mortality of cervical cancer.
Although the cervical cancer mortality rate in China had increased slightly from 2004 to 2013, there was an encouraging sign that the geographical disparities in cervical cancer mortality had gradually narrowed over time across China. This trend toward a narrower geographical disparity might be the results from continuous improvement in socioeconomic status and health conditions, and the large population cervical cancer screening in China (23). The Northwest China experienced a rapid economic growth during the past 40 years, the better living conditions and educations are available these days for women. Moreover, in recent years, cervical cancer screening in high-risk areas and rural areas not only reached the purpose of early diagnosis and early treatment, but also raised women’s awareness of self-protection from HPV infection. All this may have contributed to a notable decrease in the cervical cancer death risk among women in high-risk areas, maintaining these former high-risk areas at a lower mortality as it in other low-risk areas.
Our study may have some limitations. First, we use aggregate results of sampling sites as a provincial mortality estimate in 1990–1992, 2004–2005 and 2011–2013, the provincial mortality rates reported here may be an overestimate or underestimate for that province. Second, since of the data were extracted from the national death cause survey during 1973 to 2005, while the data for 2011–2013 came from the cancer registry, the results with these two sources may be not comparable. Despite these limitations, this study provides the most reliable results on the temporal and spatial patterns of cervical cancer mortality in China as far as we known, which can be used to update cervical cancer prevention strategy in China.
Acknowledgements
We thank Prof. Xue Qin Yu for method guidance. This work was supported by Ministry of Science and Technology of China (Grant No. 2014FY121100).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108. <DOI: 10.3322/caac.21262> <PMID: 25651787>] [DOI] [PubMed] [Google Scholar]
- 2.Chen W, Zheng R, Zuo T, et al. National cancer incidence and mortality in China, 2012. Chin J Cancer Res. 2016;28:1–11. doi: 10.3978/j.issn.1000-9604.2016.02.08. [Chen W, Zheng R, Zuo T, et al. National cancer incidence and mortality in China, 2012. Chin J Cancer Res 2016;28:1-11. <DOI: 10.3978/j.issn.1000-9604.2016.02.08> <PMID: 27041922>] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen W, Zheng R, Zhang S, et al. Cancer incidence and mortality in China in 2013: an analysis based on urbanization level. Chin J Cancer Res. 2017;29:1–10. doi: 10.21147/j.issn.1000-9604.2017.01.01. [Chen W, Zheng R, Zhang S, et al. Cancer incidence and mortality in China in 2013: an analysis based on urbanization level. Chin J Cancer Res 2017;29:1-10. <DOI: 10.21147/j.issn.1000-9604.2017.01.01> <PMID: 28373748>] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen W, Zheng R, Zhang S, et al. Cancer incidence and mortality in China, 2013. Cancer Lett. 2017;401:63–71. doi: 10.1016/j.canlet.2017.04.024. [Chen W, Zheng R, Zhang S, et al. Cancer incidence and mortality in China, 2013. Cancer Lett 2017;401:63-71. <DOI: 10.1016/j.canlet.2017.04.024> <PMID: 28476483>] [DOI] [PubMed] [Google Scholar]
- 5.M. Ervik, F. Lam, J. Ferlay, et al. Cancer Today, International Agency for Research on Cancer. Lyon, France. Available online: http://gco.iarc.fr/today
- 6.The Editoral Committee for the Atlas of Cancer Mortality in the People’s Republic of China. Atlas of cancer mortality in the People’s Republic of China. Beijing: China Map Press, 1979.
- 7.Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3:524–48. doi: 10.1001/jamaoncol.2016.5688. [Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol 2017;3:524-48. <DOI: 10.1001/jamaoncol.2016.5688> <PMID: 27918777>] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang L, Huangpu XM, Zhang SW, et al. Changes of mortality rate for cervical cancer during 1970’s and 1990’s periods in China. Zhongguo Yi Xue Ke Xue Yuan Xue Bao (in Chinese) 2003;25:386–90. [Yang L, Huangpu XM, Zhang SW, et al. Changes of mortality rate for cervical cancer during 1970’s and 1990’s periods in China. Zhongguo Yi Xue Ke Xue Yuan Xue Bao (in Chinese) 2003;25:386-90. <PMID: 12974079>] [PubMed] [Google Scholar]
- 9.Zhao FH, Hu SY, Zhang SW, et al. Cervical cancer mortality in 2004-2005 and changes during last 30 years in China. Zhonghua Yu Fang Yi Xue Za Zhi (in Chinese) 2010;44:408–12. [Zhao FH, Hu SY, Zhang SW, et al. Cervical cancer mortality in 2004-2005 and changes during last 30 years in China. Zhonghua Yu Fang Yi Xue Za Zhi (in Chinese) 2010;44:408-12.] [PubMed] [Google Scholar]
- 10.Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–32. doi: 10.3322/caac.21338. [Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115-32. <DOI: 10.3322/caac.21338> <PMID: 26808342>] [DOI] [PubMed] [Google Scholar]
- 11.The National Cancer Control Office of the Ministry of Health. China cancer death survey. Beijing: People’s Medical Publishing House, 1980.
- 12.National Office for Cancer Prevention and Control. China cancer death survey (1990-1992). Beijing: People’s Medical Publishing House, 2008.
- 13.Chen Z. The third national retrospective sampling survey of death causes in China. Beijing: China Union Medical University Press, 2008.
- 14.Chen W, Zheng R, Zeng H, et al. Annual report on status of cancer in China, 2011. Chin J Cancer Res. 2015;27:2–12. doi: 10.3978/j.issn.1000-9604.2015.01.06. [Chen W, Zheng R, Zeng H, et al. Annual report on status of cancer in China, 2011. Chin J Cancer Res 2015;27:2-12. <DOI: 10.3978/j.issn.1000-9604.2015.01.06> <PMID: 25717220>] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lindén A, Mäntyniemi S. Using the negative binomial distribution to model overdispersion in ecological count data. Ecology. 2011;92:1414–21. doi: 10.1890/10-1831.1. [Lindén A, Mäntyniemi S. Using the negative binomial distribution to model overdispersion in ecological count data. Ecology 2011;92:1414-21. <PMID: 21870615>] [DOI] [PubMed] [Google Scholar]
- 16.Xia C, Yu XQ, Zheng R, et al. Spatial and temporal patterns of nasopharyngeal carcinoma mortality in China, 1973-2005. Cancer Lett. 2017;401:33–8. doi: 10.1016/j.canlet.2017.04.016. [Xia C, Yu XQ, Zheng R, et al. Spatial and temporal patterns of nasopharyngeal carcinoma mortality in China, 1973-2005. Cancer Lett 2017;401:33-8. <DOI: 10.1016/j.canlet.2017.04.016> <PMID: 28450159>] [DOI] [PubMed] [Google Scholar]
- 17.Xia C, Kahn C, Wang J, et al. Temporal trends in geographical variation in breast cancer mortality in China, 1973-2005: an analysis of nationwide surveys on cause of death. Int J Environ Res Public Health 2016;13.
- 18.Shi JF, Canfell K, Lew JB, et al. The burden of cervical cancer in China: synthesis of the evidence. Int J Cancer. 2012;130:641–52. doi: 10.1002/ijc.26042. [Shi JF, Canfell K, Lew JB, et al. The burden of cervical cancer in China: synthesis of the evidence. Int J Cancer 2012;130:641-52. <DOI: 10.1002/ijc.26042> <PMID: 21387308>] [DOI] [PubMed] [Google Scholar]
- 19.de Sanjose S, Quint WG, Alemany L, et al. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010;11:1048–56. doi: 10.1016/S1470-2045(10)70230-8. [de Sanjose S, Quint WG, Alemany L, et al. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol 2010;11:1048-56. <DOI: 10.1016/S1470-2045(10)70230-8> <PMID: 20952254>] [DOI] [PubMed] [Google Scholar]
- 20.Zhao FH, Lin MJ, Chen F, et al. Performance of high-risk human papillomavirus DNA testing as a primary screen for cervical cancer: a pooled analysis of individual patient data from 17 population-based studies from China. Lancet Oncol. 2010;11:1160–71. doi: 10.1016/S1470-2045(10)70256-4. [Zhao FH, Lin MJ, Chen F, et al. Performance of high-risk human papillomavirus DNA testing as a primary screen for cervical cancer: a pooled analysis of individual patient data from 17 population-based studies from China. Lancet Oncol 2010;11:1160-71. <DOI: 10.1016/S1470-2045(10)70256-4 > <PMID: 21075054>] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jiang J, Pang H, Liu B, et al. Effects of active, passive, and combined smoking on cervical cancer mortality: a nationwide proportional mortality study in Chinese urban women. Cancer Causes Control. 2015;26:983–91. doi: 10.1007/s10552-015-0580-x. [Jiang J, Pang H, Liu B, et al. Effects of active, passive, and combined smoking on cervical cancer mortality: a nationwide proportional mortality study in Chinese urban women. Cancer Causes Control 2015;26:983-91. <DOI: 10.1007/s10552-015-0580-x> <PMID: 25898822>] [DOI] [PubMed] [Google Scholar]
- 22.Yang DW, Yao JF, Xing SF, et al. Mass cytologic screening for cervical carcinoma in China. A review of 7,735,057 reported cases. Acta Cytol. 1985;29:341–4. [Yang DW, Yao JF, Xing SF, et al. Mass cytologic screening for cervical carcinoma in China. A review of 7,735,057 reported cases. Acta Cytol 1985;29:341-4. <PMID: 3859133>] [PubMed] [Google Scholar]
- 23.Wang B, He M, Chao A, et al. Cervical cancer screening among adult women in China, 2010. Oncologist. 2015;20:627–34. doi: 10.1634/theoncologist.2014-0303. [Wang B, He M, Chao A, et al. Cervical cancer screening among adult women in China, 2010. Oncologist 2015;20:627-34. <DOI: 10.1634/theoncologist.2014-0303> <PMID: 25956407>] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zeng H, Zheng R, Guo Y, et al. Cancer survival in China, 2003-2005: a population-based study. Int J Cancer. 2015;136:1921–30. doi: 10.1002/ijc.29227. [Zeng H, Zheng R, Guo Y, et al. Cancer survival in China, 2003-2005: a population-based study. Int J Cancer 2015;136:1921-30. <DOI: 10.1002/ijc.29227> <PMID: 25242378>] [DOI] [PubMed] [Google Scholar]
- 25.Islami F, Chen W, Yu XQ, et al. Cancer deaths and cases attributable to lifestyle factors and infections in China, 2013. Ann Oncol. 2017;28:2567–74. doi: 10.1093/annonc/mdx342. [Islami F, Chen W, Yu XQ, et al. Cancer deaths and cases attributable to lifestyle factors and infections in China, 2013. Ann Oncol 2017;28:2567-74. <DOI: 10.1093/annonc/mdx342> <PMID: 28961829>] [DOI] [PubMed] [Google Scholar]
- 26.Li J, Huang R, Schmidt JE, et al. Epidemiological features of Human Papillomavirus (HPV) infection among women living in Mainland China. Asian Pac J Cancer Prev. 2013;14:4015–23. doi: 10.7314/apjcp.2013.14.7.4015. [Li J, Huang R, Schmidt JE, et al. Epidemiological features of Human Papillomavirus (HPV) infection among women living in Mainland China. Asian Pac J Cancer Prev 2013;14:4015-23. <PMID: 23991946>] [DOI] [PubMed] [Google Scholar]
- 27.Zhao FH, Lewkowitz AK, Hu SY, et al. Prevalence of human papillomavirus and cervical intraepithelial neoplasia in China: a pooled analysis of 17 population-based studies. Int J Cancer. 2012;131:2929–38. doi: 10.1002/ijc.27571. [Zhao FH, Lewkowitz AK, Hu SY, et al. Prevalence of human papillomavirus and cervical intraepithelial neoplasia in China: a pooled analysis of 17 population-based studies. Int J Cancer 2012;131:2929-38. <DOI: 10.1002/ijc.27571> <PMID: 22488743>] [DOI] [PMC free article] [PubMed] [Google Scholar]