Abstract
Background
Adverse childhood experiences (ACEs) are associated with multiple mental and physical health problems. Yet, mechanisms by which ACEs confer risk for specific problems are largely unknown. Children in foster care typically have multiple ACEs and high rates of negative sequelae, including delinquent behaviors. Mechanisms explaining this link have not been explored in this population. Impaired sleep has been identified as a potential mechanism by which ACEs lead to delinquency in adolescents, because inadequate sleep may lead to poor executive function and cognitive control – known risk factors for delinquency.
Methods
Interviews were conducted with 516 maltreated children in foster care, ages 9–11 years, and their caregivers regarding child exposure to ACEs, sleep problems, engagement in delinquent acts, symptoms of posttraumatic stress disorder, and current psychotropic medication use. ACEs data were also obtained from child welfare case records.
Results
After controlling for age, gender, race/ethnicity, placement type (residential, kin, foster), length of time in placement, posttraumatic stress symptoms, and current psychotropic medication use, sleep partially mediated the association between ACEs and delinquency.
Conclusions
Although delinquency is likely multiply determined in this population, improving sleep may be one important strategy to reduce delinquency.
Keywords: sleep, delinquency, child maltreatment, adverse childhood experiences, foster care
Adverse childhood experiences (ACEs) are potentially traumatic or highly stressful events that may result in physical and mental health problems (Anda et al., 2006). The link between ACEs and delinquency in adolescence has been established in community and trauma-exposed samples (Lansford et al., 2007; Maschi, Bradley, & Morgen, 2008; Stouthamer-Loeber, Loeber, Homish, & Wei, 2001). Children in foster care are at high risk for both ACEs and delinquency (Baglivio et al., 2016; Bruskas & Tessin, 2013; Ryan & Testa, 2005; Stein et al., 2001), yet the link between ACEs and delinquency in this population, and the mechanisms explaining this link, have not yet been examined (Moore & Ramirez, 2015). Sleep is one mechanism to consider. Sleep problems, which include difficulty falling or staying asleep and sleep disorders, are not uncommon during the transition from childhood to adolescence due to biological, psychological, and social changes to the sleep cycle (Mindell & Meltzer, 2008; Smaldone, Honig, & Byrne, 2007). Most research on sleep in the context of ACEs exposure and behavior problems, however, has been conducted with adolescents (e.g., Rubens, Fite, Cooley, & Canter, 2014). This study examines sleep problems, including sleeping more or less than others, sleep disruptions, and tiredness, as a potential mechanism by which ACEs are associated with delinquency in maltreated preadolescent children in foster care.
ACEs, Foster Care and Sleep Problems
Exposure to ACEs, including violence, parental conflict, and peer victimization, is associated with poor sleep in youth (El-Sheikh, Buckhalt, Mize, & Acebo, 2006; Lepore & Kliewer, 2013), and has been linked with sleep problems into adulthood (Gelaye et al., 2015; Kajeepeta, Gelaye, Jackson, & Williams, 2015). ACEs can trigger a psychological and biological response to stress, which results in the release of stress hormones such as corticotropin-releasing hormones (Lupien, McEwan, Gunnar, & Heim, 2009). These hormones elicit mental and physiological arousal responses (McEwen, 1998), which in turn lead to sleep disruptions (Buckley & Schatzberg, 2005). Chronic or repeated exposure to stressors can result in an overactive hypothalamic-pituitary-adrenal axis, making individuals more hypervigilant and alert, resulting in difficulty falling and staying asleep (Buckley & Schatzberg, 2005).
Despite the prevalence of ACEs among foster youth, little is known about the link between ACEs exposure and sleep problems in this population. Tininenko, Fisher, Bruce, and Pears (2010) found that young children in foster care had longer sleep latency than children from a community sample. Although a change in living situation because of a child’s entry into foster care could improve sleep onset and reduce sleep disruptions via providing a safer sleeping area and an improved sleep routine (Charuvastra & Cloitre, 2009), sleeping in a new place may also alter a child’s sleep associations and create or exacerbate sleep problems (LeBourgeois, Giannotti, Cortesi, Wolfson, & Harsh, 2005).
Sleep Problems and Delinquency
Research has also highlighted the association between sleep problems and externalizing problems, including delinquency (Clinkinbeard, Simi, Evans, & Anderson, 2011; Owens, Wang, Lewin, Skora, & Baylor, 2017; Pesonen et al., 2010; Rubens et al., 2014). In a sample of 6- to 11-year-olds, less sleep time was associated with an increase in conduct problems (Holley, Hill, & Stevenson, 2011). In a longitudinal examination of sleep and problem behaviors in twins, sleep problems, including difficulties falling asleep and frequent wakings, at ages 3–4 predicted conduct problems at age 7 (Gregory, Eley, O’Connor, & Plomin, 2004).
The link between sleep problems and delinquency may be due to the role of executive functioning in problem behavior. Poor quality sleep contributes to executive function deficits, or problems carrying out complex cognitive tasks, such as inhibition, planning, and reasoning (Meldrum, Barnes, & Hay, 2015). These deficits are associated with externalizing problems in youth (Peach & Gaultney, 2013): in a nationally-representative sample of adolescents, the association between sleep duration and delinquency was partially mediated by increased sensation seeking and decreased impulse control. Meldrum and colleagues (2015) noted an indirect effect of self-control in the link between sleep deprivation and delinquency in adolescents. Given the risk of delinquency in youth in foster care, examining how sleep problems contribute to delinquency in this population may inform intervention efforts.
Complicating Factors
One complicating factor in the relationship between ACEs, sleep, and delinquency is that sleep problems, such as nightmares, are a symptom of posttraumatic stress disorder (PTSD; American Psychiatric Association, 2013). Although not all ACEs are traumatic for every child, ~20% of children in foster care have significant PTSD symptoms (Kolko et al., 2010). Sleep problems may confer risk for PTSD (Koren, Arnon, Lavie, & Klein, 2002), and, for PTSD treatment to be most beneficial, sleep problems must be resolved (Galovski, Monson, Bruce, & Resick, 2009; Kovachy et al., 2013). However, sleep problems in individuals exposed to ACEs may not be fully explained by PTSD symptoms. Therefore, research isolating the impact of sleep problems when controlling for PTSD symptoms is needed.
Another complication is psychotropic medication use. Child welfare-involved children are 2–3 times more likely to be prescribed psychotropic medications than non-child-welfare involved children (Raghavan et al., 2005). Some medications, such as tricyclic antidepressants, can improve sleep (Wilson & Argyropoulos, 2005), and atypical antipsychotics can be sedating (Roth, Zorick, Sicklesteel, & Stepanski, 1981). Conversely, stimulants may increase sleep latency (Bricard & Boidein, 2001). Individual differences in response to medication (Burroughs, Maxey, & Levy, 2002) and classes of medication that confer variable sleep effects, including selective serotonin reuptake inhibitors (Wilson & Argyropoulos, 2005), can further complicate research with youth taking medication. Thus, sleep research conducted with children in foster care should account for the potential impact of medication use.
Finally, there are important demographic controls in this context. Differences in sleep quality have been found across racial/ethnic groups (Buckhalt, El-Sheikh, & Keller, 2007). PTSD symptoms are typically higher amongst females (Merikangas et al., 2010). Characteristics of the foster placement may impact sleep, given potential variations in sleep hygiene and perceived safety during sleep for children living in residential placements, versus with relatives, versus in traditional foster homes. Similarly, the longer a child spends in a certain placement, their sleep duration may increase due to increased comfort falling asleep in the new setting or to improved sleep routines (Charuvastra & Cloitre, 2009).
Current Study
The goal of this study was to determine if sleep problems, broadly, mediate the association between ACEs and delinquency in a sample of preadolescent children who recently entered the foster care system, while controlling for symptoms of PTSD, psychotropic medication use, and demographic factors (i.e., race/ethnicity, gender, age, placement type, length of stay in current placement). We expected an indirect effect of sleep on delinquency in the overall sample, as well as in a subsample of children not currently taking psychotropic medications.
Method
Participants
Participants included 516 maltreated preadolescents (M age =10.3 years, SD=.90) in out-of-home care and their foster caregivers. Participants were recruited for a randomized trial testing the Fostering Healthy Futures preventive intervention (Taussig, Culhane, & Hettleman, 2007), in a large, urban Western city. Children were recruited if they were between 9 and 11 years old and had been placed in out-of-home care within the preceding year in a participating county. Of those eligible, 91% were enrolled.
Child participants were 52.4% male and 76.1% ethnic/racial minority (47.2% Hispanic/Latino/a, 48.0% Caucasian, 27.2% African American/Black, 9.9% Native American, and 4.1% Asian/Pacific Islander; non-exclusive categories). Children were living in kinship care (52.2%), non-relative foster care (44.3%), and group homes/residential treatment centers (3.5%). They had been in foster care an average of 7.1 months (SD=3.5), and in their current placement an average of 6.0 months (SD=3.8) at the time of the interview.
Measures
Demographic Information
Child welfare records and caregiver and child interviews provided data on gender, ethnic/racial minority status, age, placement type (i.e., traditional foster care (living with non-family members), kinship care (living with family members), or in a residential treatment center), length of current placement, and current use of psychotropic medications (“Is the child currently taking any medications for behavioral or emotional problems?”).
Adverse Childhood Experiences
ACEs were assessed with a previously-developed 6-item measure (Raviv, Taussig, Culhane, & Garrido, 2010), comprised of: Physical Abuse; Sexual Abuse; Removal from a single parent household; Exposure to community violence; Number of caregiver transitions; and Number of school transitions. The first three ACEs were coded as “present” (1) or “absent” (0) following review of child welfare records. Community violence and transitions were assessed through child report and dichotomized: a score of 1 was assigned to scores in the upper quartile of the sample, and a score of 0 for all others (e.g., Appleyard et al., 2005). To determine community violence exposure, an adapted version of the Things I Have Seen and Heard scale (Richters & Martinez, 1993) was used. Children indicated the number of times in the past year they had seen or heard acts such as “guns being shot.” Responses ranged from never (0) to four or more times (4). The upper quartile included children with scores of 13.00 and higher (range=0–30.00, M=8.47, SD=6.70). Caregiver transitions were measured based on child report of the number of caregiver transitions since birth (range=1–11, M=2.79, SD=2.07). Children in the upper quartile had 4 or more transitions. For school transitions, children reported the number of school transitions they had experienced (range=0–29, M=3.22, SD=2.85), with 4 or more representing the upper quartile. Scores of 0 or 1 on each of the 6 indices were summed to form a composite. In this sample, ACE scores ranged from 0–5 (Figure 1), M=1.66, SD=1.11. Most children (77%) were exposed to at least one ACE.
Figure 1.
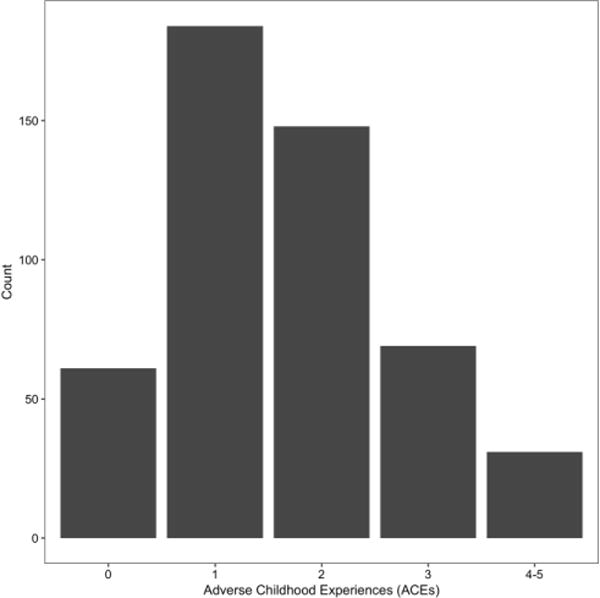
Adverse Childhood Experiences
Sleep
Sleep problems were measured using the Child Behavior Checklist (CBCL), a caregiver-report measure of child psychosocial functioning (Achenbach & Rescorla, 2001). Caregivers rate frequency of behaviors over the past 6 months on a scale (0=never, 1=sometimes, 2=often). Sleep problems were calculated in two ways due to lack of consensus in the field regarding the optimal CBCL-based measure of sleep problems. First, we used the sum of 7 sleep items on the CBCL showing convergent validity with validated sleep measures, with items including overtired without good reason, sleeps less than most kids (Becker, Ramsey, & Byars, 2015). The second measure of sleep problems was the CBCL item “trouble sleeping,” as this item is predictive of children’s overall sleep problems (Gregory et al., 2011). In the current sample, the 7-item measure ranged from 0–10, M=1.66, SD=1.97. Items on the 7-item scale do not typically result in an internally consistent measure of sleep functioning, because children often do not experience each of the different problems assessed. However, the entire scale is useful in predicting aspects of children’s psychosocial functioning (Becker et al., 2015). Internal consistency of the 7-item scale in this study was .54, consistent with Becker and colleagues, 2015. The 1-item measure scores in this sample ranged from 0–2, M=.27, SD=.58. Twenty percent of caregivers reported their foster child had “trouble sleeping” at least “sometimes.”
Delinquency
Child report of delinquent acts was the sum of 5 questions from the Adolescent Risk Behaviors Scale, a compilation of widely-used measures of adolescent risk behaviors (Taussig, 2002). Children reported behaviors they had “chosen” and were not “forced” to do (i.e., shoplifting, purposely damaged or destroyed the property of others, set fire or tried to set fire to anything, carried a hidden weapon like a knife or gun, and went into a house or building to steal something). Behaviors were counted as present (1) or absent (0) if they had ever engaged in the behavior. Scores in this sample ranged from 0–5 (Figure 2), M=.48, SD=.81. At least one delinquent act was reported by 33.4% of children.
Figure 2.
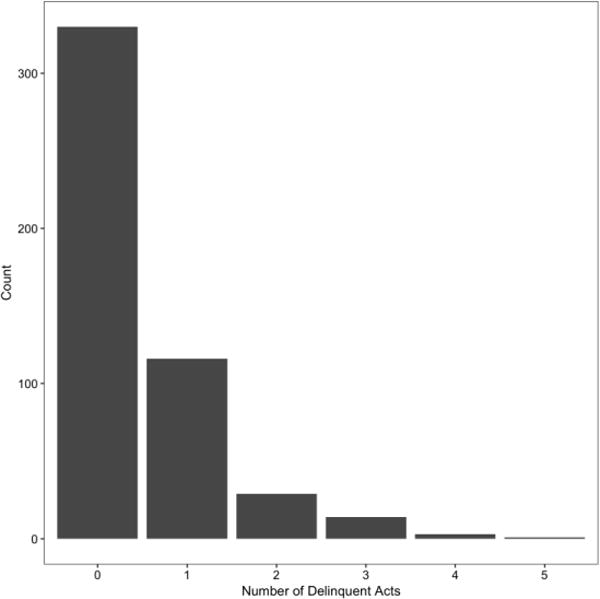
Delinquency
Trauma Symptoms
PTSD symptoms were measured using children’s mean raw score on the Trauma Symptom Checklist for Children (TSCC) posttraumatic stress (PTS) scale (Briere, 1996) which has evidenced good reliability (α=.83) and validity (Lanktree et al., 2008). The TSCC is a child self-report measure of PTS and related symptoms, asking questions in the present tense, i.e., “How often do each of these things happen to you?” on a 4-point scale from 0=“never” to 3=“almost all of the time.” The PTS scale measures avoidance of trauma triggers, hypervigilance, and re-experiencing phenomenon. The item assessing nightmares was deleted to reduce overlap with the sleep measure, yielding a 9-item scale. The internal consistency of the 9-item scale in this study was .85. Scores ranged from 0–27, M=7.89, SD=5.37.
Procedure
Children and caregivers were interviewed separately, and each were paid $40.00. Interviewers were trained graduate research assistants.
Ethical Considerations
Institutional review board approval from the University of Colorado School of Medicine, caregiver informed consent, and child assent were obtained prior to the interviews.
Data Analysis
Causal mediation analysis was performed to test whether sleep mediated the association between ACEs and delinquency within the potential outcomes framework, described in Imai, Keele, and Tingley (2010) and Imai, Keele, Tingley, and Yamamoto (2011). Because the potential outcomes framework is flexible enough to handle models of categorical variables, this approach allowed us to appropriately fit a Poisson regression model of the dependent variable, delinquency, which was measured as a count of distinct delinquent acts. In short, this framework requires fitting two statistical models, first a model of the mediator as a function of the predictor (“treatment”) variable and other covariates, and the second a model of the outcome as a function of the mediator, treatment, and other covariates. We then used these two models to obtain predicted values of the outcome (delinquency) under counterfactual treatment and mediator conditions to derive the estimated direct (ACEs on delinquency) and indirect (sleep on delinquency) effects.
The independent variable was number of ACEs. ACEs ranged from 0–5; however, categories 4 and 5 were collapsed due to a low frequency of children endorsing 4 (N=24, 4.75%) or 5 (N=5, 0.99%) ACEs. The mediator was caregiver report of sleep (both the 7- and 1-item scale in separate models). Both sleep measures evidenced right skew, which was improved by a natural log transformation. Control variables included PTSD symptoms, race/ethnicity, gender, current psychotropic medication use, age, placement type, and length of stay in the current placement.
Working in the potential outcomes framework, we first fit a linear regression model of the mediator, sleep, which allowed us to simulate counterfactual values of sleep under different levels of the IV (ACEs). We then fit a Poisson regression model of the outcome (delinquency), which was used to evaluate the direct effect of ACEs and the indirect effect of sleep on delinquency. Uncertainty in the direct and indirect effects was evaluated by estimating the mediator and outcome models on 1,000 bootstrap samples of the data (Imai et al., 2011). In other words, we used each set of bootstrapped coefficient estimates from the mediator model to produce predicted values for the mediator, sleep, under each treatment (ACEs=1, 2, 3, or 4–5) and then the control (ACEs=0) condition. We then produced predicted values of delinquency using the coefficient estimates from the outcome model, using the predicted values of sleep as the mediator, and holding the treatment value constant. This allowed us to estimate the mediating effect of sleep as the difference in the predicted value of delinquency when the mediator is at its predicted value under the treatment condition (number of ACEs), and when it is at its predicted value under the control (ACEs=0) condition. This process was repeated for each level of ACEs. Last, because the ACEs variable was ordinal, the method suggested by Imai, Keele, and Tingley (2010, p. 322) for evaluating average causal mediation effects with non-binary treatment variables was used. A custom program written for the R language (R Core Team 2016) implementing these methods adapted the source code for the “mediation” library (Tingley, Yamamoto, Hirose, Keele, & Imai, 2014).
Following the recommendations of Ho, Imai, King, & Stuart (2007) and Imai et al. (2011), the analysis was preceded by a matching procedure, using propensity scores, where children with 0 ACEs were matched on age, gender, minority status, placement type, and length of stay in their current placement with children with 1 ACE, 2 ACEs, 3 ACEs, and then 4–5 ACEs. The goal was to ensure that children at each level of ACEs exposure (1–4) were similar in demographic characteristics and placement to children without exposure to any of the measured ACEs. Ten children were excluded due to matching (conducted using the “MatchIt” library in R; Ho, Imai, King, & Stuart, 2011). Missing data were rare, given that interviews were conducted in person. Only 0.25% of the data for the variables used in this analysis were missing. Due to the small amount of missing data, and because Little’s MCAR test conducted in SPSS v23 determined that the data were missing completely at random, listwise deletion was used. Following the matching procedure and listwise deletion, N=493. The mediation analysis was conducted twice - once using the entire sleep scale of the CBCL as the mediator, and once using the single “trouble sleeping” item of the CBCL as the mediator. Finally, MANOVA was used to determine if there were differences between children taking psychotropic medication and children not taking medication on the variables in the mediation models that would indicate a need to re-run analyses on the subset of children not taking medication.
Results
Table 1 contains zero-order correlations between key variables. The mediation analysis indicated that sleep partially mediated the direct effect of ACEs on delinquency. The 7-item measure of sleep problems was significant at the p<.05 level. The 1-item measure was not significant (see Models 1–2 in Table 2 for direct and indirect effects). In Model 1, the log of the 7-item sleep problems variable was the mediator. In Model 2, the log of the 1-item sleep problems variable was the mediator. The MANOVA indicated significant differences between children currently taking psychotropic medication (N=76, 14.7%) and children who were not (N=440, 85.3%; Wilks’ Lambda F=5.66, df=7,497, p=.01, η2=.07). Children taking medication were more likely to engage in delinquency (F=11.85, p=.01, η2=.02), exhibited more sleep problems (F=19.70, p=.01, η2=.04), and experienced more ACEs (F=7.31, p=.01, η2=.01) and PTSD symptoms (F=8.90, p=.01, η2=.02) than children not taking medication. Thus, mediation analyses were also conducted in a sample restricted to children who were not currently taking psychotropic medication (Models 3 and 4). These models were identical (respectively) to Models 1 and 2, except they were only conducted with children not taking medication.
Table 1.
Correlations
| Delinquency | ACEs | PTSD | Age | Gender | Ethnicity | Medication | Sleep(7-item) | Sleep (1-item) | Placement Length | Kinship Care | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| ACEs | 0.23* | ||||||||||
| PTSD | 0.19* | 0.18* | |||||||||
| Age | 0.22* | 0.16* | −0.09 | ||||||||
| Gender | 0.19* | 0.05 | −0.09 | 0.05 | |||||||
| Ethnicity | −0.03 | −0.12* | 0.05 | −0.01 | −0.05 | ||||||
| Medication | 0.12* | 0.09* | 0.11* | −0.01 | 0.07 | 0.03 | |||||
| Sleep (7-item) | 0.09* | 0.12* | 0.08 | −0.02 | −0.01 | 0.02 | 0.18* | ||||
| Sleep (1-item) | 0.12* | 0.09 | 0.09 | −0.03 | 0.03 | 0.02 | 0.14* | 0.61* | |||
| Placement Length | 0.02 | −0.06 | 0.09 | −0.05 | −0.02 | −0.02 | 0.07 | −0.03 | −0.056 | ||
| Kinship Care | −0.14* | −0.13* | −0.03 | −0.01 | −0.02 | −0.03 | −0.15* | −0.08 | −0.13* | 0.14* | |
| Residential Care | 0.08 | 0.02 | −0.01 | −0.01 | 0.15* | 0.07 | 0.24* | −0.01 | 0.02 | −0.01 | −0.17* |
Note. ACEs=adverse childhood experiences; PTSD=posttraumatic stress symptoms.
p<.05. Gender: Male=1; Minority=1; Placement: Kinship=1, Foster=0, Residential=1, Foster=0. 7-item sleep measure: nightmares, overtired without good reason, sleeps less than most kids, sleeps more than most kids during day and/or night, talks or walks in sleep, trouble sleeping, wets the bed. 1-item sleep measure=trouble sleeping.
Table 2.
Effect of ACEs and Sleep on Delinquency
| Model | # of ACEs | Avg Direct Effect – ACEs on # of Delinquent Acts | Avg Indirect Effect – Sleep on # of Delinquent Acts |
|---|---|---|---|
| 1 | 1 | 0.061** | 0.006** |
| 2 | 0.133** | 0.012** | |
| 3 | 0.220** | 0.018** | |
| 4–5 | 0.325** | 0.025** | |
| 2 | 1 | 0.063** | 0.004* |
| 2 | 0.138** | 0.007* | |
| 3 | 0.227** | 0.010* | |
| 4–5 | 0.327** | 0.014* | |
| 3 | 1 | 0.062** | 0.007** |
| 2 | 0.130** | 0.014** | |
| 3 | 0.222** | 0.022** | |
| 4–5 | 0.317** | 0.028** | |
| 4 | 1 | 0.062** | 0.004* |
| 2 | 0.137** | 0.008* | |
| 3 | 0.232** | 0.012* | |
| 4–5 | 0.341** | 0.017* |
Note. ACEs=Adverse childhood experiences.
p<.10,
p<.05.
Figure 3 shows the average mediation effect of sleep problems alongside the average direct effect of ACEs in Model 1 (visuals for Models 2–4 are indistinguishable, thus not shown). The mediator and outcome models are summarized in Table 3. The direct effect of ACEs (shaded light gray in Figure 3) was substantial. Namely, children with one ACE would be expected to engage in .061 more delinquent acts than children with none of the measured ACEs. For children with two ACEs, the expected increase in delinquent acts relative to children with no ACEs was approximately 0.133. The expected increase in delinquent acts for children with three ACEs over children with no ACEs was approximately 0.220. Finally, when children had experienced 4–5 ACEs, the expected increase in number of delinquent acts was approximately 0.325. Because the average value of delinquent acts observed in the sample was .48, the direct effect of ACEs on number of delinquent acts was large in magnitude.
Figure 3.
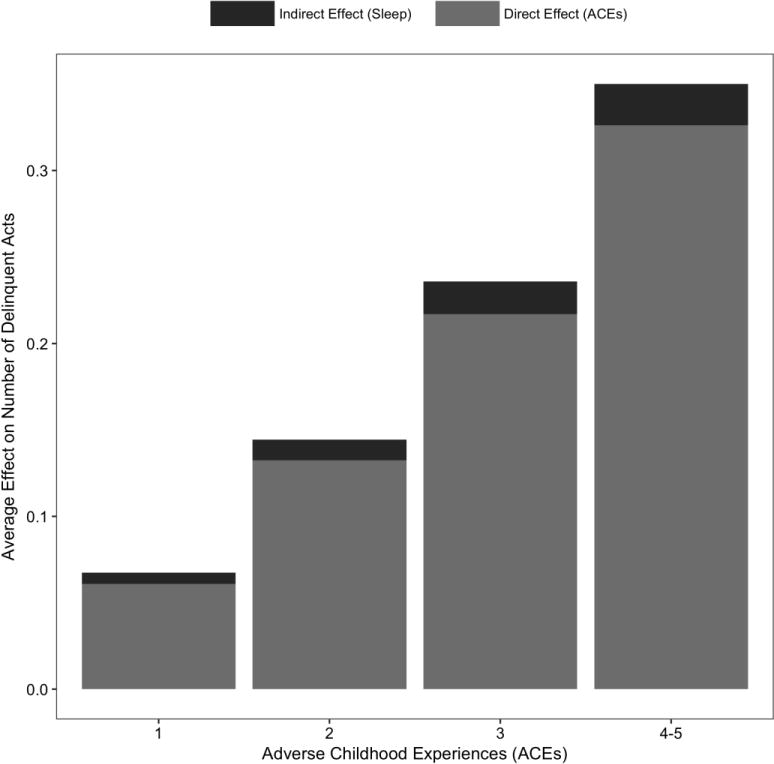
Effect of ACEs and Sleep on Delinquency.
Table 3.
Regression Models
| Linear Regression of Mediator (Sleep)
| ||||
|---|---|---|---|---|
| B | SE | p | β | |
| ACEs | 0.064 | 0.030 | 0.030* | 0.102 |
| PTSD | 0.006 | 0.006 | 0.322 | 0.046 |
| Age | −0.024 | 0.034 | 0.484 | −0.032 |
| Male | −0.014 | 0.061 | 0.823 | −0.010 |
| Minority | 0.039 | 0.071 | 0.584 | 0.025 |
| Medication | 0.401 | 0.100 | 0.001* | 0.186 |
| Kinship Care | −0.075 | 0.062 | 0.226 | −0.056 |
| Residential Care | −0.316 | 0.202 | 0.119 | −0.072 |
| Placement Length | −0.006 | 0.008 | 0.427 | −0.036 |
|
| ||||
| Poisson Regression of Outcome (Delinquency)
| ||||
| B | SE | p | β | |
| Sleep | 0.237 | 0.099 | 0.016* | 0.198 |
| ACEs | 0.167 | 0.063 | 0.008* | 0.221 |
| PTSD | 0.064 | 0.012 | 0.001* | 0.426 |
| Age | 0.394 | 0.078 | 0.001* | 0.438 |
| Male | 0.711 | 0.146 | 0.001* | 0.440 |
| Minority | −0.207 | 0.167 | 0.214 | −0.109 |
| Medication | 0.189 | 0.185 | 0.307 | 0.073 |
| Kinship Care | −0.318 | 0.143 | 0.026* | −0.197 |
| Residential Care | 0.268 | 0.321 | 0.404 | 0.051 |
| Placement Length | 0.013 | 0.017 | 0.443 | 0.060 |
Note. ACEs=adverse childhood experiences; PTSD=posttraumatic stress symptoms.
p<.05. Gender: Male=1; Minority=1; Placement: Kinship=1, Foster=0; Residential=1, Foster=0. 7-item sleep measure: nightmares, overtired without good reason, sleeps less than most kids, sleeps more than most kids during day and/or night, talks or walks in sleep, trouble sleeping, wets the bed. 1-item sleep measure=trouble sleeping.
The average mediation effects, shown in the darker shaded regions of Figure 3, were smaller in magnitude compared to the large direct effect of ACEs, but likewise increased as the value of ACEs increased. Specifically, for children with one ACE, the mediating effect of sleep problems was approximately 0.006. Given the estimated direct effect when ACEs=1 of 0.061, the overall effect on delinquency at this level was approximately 0.067, of which the mediating effect of sleep problems accounted for about 8.9% of the overall effect of ACEs on delinquency. For children with two ACEs, the mediating effect of sleep problems was estimated to be 0.012, implying a total effect on delinquent acts of 0.145, of which the mediating effect accounted for 8.3% of the overall effect of ACEs. For children with three ACEs and then four-five ACEs, the respective estimated average mediation effects were 0.018 and 0.025, and these effects accounted for approximately 7.6% and 7.1% of the total effects of ACEs on delinquent events at these levels of ACEs. In sum, sleep problems accounted for about 7–9% of the large effect of ACEs on delinquent acts across levels of ACEs exposure.
Discussion
This study investigated the mediating role of sleep problems in the association between ACEs and delinquency among a sample of maltreated preadolescents in foster care. Over 30% of youth reported engaging in at least one delinquent act, and over 20% of caregivers reported that their foster children had trouble sleeping. Sleep problems partially mediated the large association between ACEs and delinquency, even when controlling for several potential confounds and after restricting the sample to children not currently taking psychotropic medications. Only the 7-item measure, however, yielded statistically significant results in either the full sample of children or the sample of children not currently taking psychotropic medication.
Sleep problems accounted for a small portion of the effect of ACEs on delinquency. This is not surprising given decades of research demonstrating that delinquency is multi-determined (Huizinga, Esbensen, & Weiher, 1991). Improving sleep problems for preadolescents in foster care may be one avenue for preventing or reducing delinquency, particularly if addressing sleep problems is a component of broad intervention efforts. It may be especially important to intervene during preadolescence with high-risk children, including children in foster care, because delinquency often emerges during adolescence (Moffitt, 1993). Research shows that addressing sleep problems in youth with externalizing problems could influence future problem behavior. Bootzin and Stevens (2005) found that addressing insomnia in adolescents receiving substance abuse treatment resulted in a significant decline in substance use one year later. Exploring sleep interventions for youth in foster care, and assessing their impact on behavior problems, is an important future direction.
Sleep problems remained associated with delinquency even after controlling for PTSD symptoms. This finding makes sense given research suggesting that significant sleep problems, when present, may need to be treated as an additional, separate concern for children receiving PTSD treatment to ensure long-term maintenance of treatment gains (Galovski et al., 2009). Additionally, children who were currently taking psychotropic medications had higher ACEs, PSTD symptoms, and delinquency rates. Interestingly, sleep problems retained a significant indirect effect in the subset of children not currently taking medication. Finally, main effects in the regression (Table 3) indicated that children in kinship homes were less likely than children in foster homes to engage in delinquency. Research examining aspects of the sleep environment across foster care settings will be an important future direction.
This is the first known study to show that ACEs may confer risk for sleep problems, which then may confer risk for delinquency, in children in foster care. This is key because a child’s entry into foster care often presents an opportunity for receipt of health-focused services. Sleep problems may be ameliorated by improving sleep conditions and sleep hygiene, by increasing adult supervision of children’s sleep, and by addressing medical issues that may be causing or exacerbating sleep problems (Mindell & Meltzer, 2008).
With behavioral interventions consistently shown to improve sleep problems in youth (Meltzer & Mindell, 2014), and incremental changes in sleep problems having a significant impact on externalizing problems (e.g., Holley et al., 2011), incorporating sleep interventions into services may enhance care. Providers should screen for sleep problems to create a more comprehensive intervention plan. Factors unique to foster care that might influence sleep quality, including changes to the sleep environment due to moving homes and the degree of perceived safety in the new sleep setting, are important considerations. Although there are no known sleep interventions developed for foster care, if providers focus on assessing and intervening with sleep issues with children in care, it could be one cost-effective method to prevent delinquency.
Findings should be interpreted considering study limitations. The sleep measure may be an underestimate of sleep problems, because it was based solely on caregiver report. Foster caregivers, who may not have had children in their homes or residential settings for long, might not be fully aware of children’s sleep problems. Studies have found low correspondence between parent- and child-reported sleep problems (Paavonen et al., 2000) and between parent-reported sleep quality and disruptions compared to actigraphy (Dayyat, Spruyt, Molfese, & Gozal, 2011). Additionally, while the sleep measure used is a valid screening tool for sleep problems, it is not a diagnostic measure (Becker et al., 2015). Including comprehensive diagnostic tools when assessing sleep problems among youth in foster care is warranted to help target specific sleep interventions. Similarly, all children had a documented history of maltreatment and were likely exposed to various unmeasured ACEs (Raviv et al., 2010). Thus, the current measure of ACEs may also be an underestimate.
Our delinquency measure also had limitations. We defined delinquency as engagement in law-breaking behaviors. Other studies have defined delinquency more broadly, asking preadolescents, for example, whether they have “lied to parents about where they have been” or “done…dangerous things just for fun” alongside inquiring about law-breaking behaviors (Hirschfield & Gasper, 2001). However, because conduct problems do not fully account for the development of delinquency (Frick, Cornell, Barry, Bodin, & Dane, 2003), we employed a stricter definition. Indeed, rates of delinquency within our sample (33% engaged in at least one delinquent act) are consistent with those found in other samples measuring delinquency in preadolescence (e.g., Loeber, Stouthamer-Loeber, & Van Kammen, 1989).
Another limitation was the lack of measures of home environment. Home environment predicts both delinquency (Sullivan, 2006) and sleep problems (Spilsbury et al., 2005), making it an important consideration when studying how sleep affects delinquency. However, because many children in this sample had not lived in their current placement for long, and because of the vast differences in “home” environments between residential, kinship, and foster placements, traditional measures of home environment were not used. Determining whether the sleep problems identified in this study reflect poor home environments (e.g., lack of routines, lack of caregiver attunement to child needs) is an important future direction.
Finally, analysis of cross-sectional data limits the ability to examine the mediating effect temporally. Therefore, whether early ACEs were associated with later sleep problems and if sleep problems were associated with later delinquency was not examined. Longitudinal analysis is needed to determine whether sleep problems act as a true causal mediator. Similarly, studies to promote the understanding of how sleep problems during preadolescence influence the developmental trajectory of delinquency will be important.
When examining how sleep problems affect the developmental trajectory of delinquency, it will also be helpful to know what types of sleep problems are most strongly associated with delinquency, the differential impact of various types of adversity, and other characteristics of children whose delinquent behaviors are highly associated with sleep problems. Understanding how sleep interacts with other risk factors for delinquency, such as substance use, peer deviance, and adult supervision (Shader, 2001) will also further the field, as will evaluating whether addressing sleep problems helps reduce delinquency.
Conclusions
Determining risk factors for delinquency in children in foster care is vital given the well-established link between foster care placement and later juvenile justice involvement (Baglivio et al., 2016). Placement in foster care is an opportunity to ameliorate risk factors such as sleep problems. Findings from this study indicate that it is prudent to assess for sleep problems in this population, to help foster caregivers establish good sleep hygiene, and to systematically implement treatment plans that include a focus on sleep.
Key Points.
ACEs are associated with sleep problems in youth.
Adverse childhood experiences (ACEs) and sleep problems pose risk for delinquency.
We test whether sleep mediates the association between ACEs and delinquency in preadolescents in foster care, a group at high risk for ACEs, delinquency, and sleep problems.
Sleep partially mediated the direct effect of ACEs on delinquency.
Improving sleep may be one important strategy to reduce delinquency in this at-risk population.
Acknowledgments
The Developmental Psychobiology Research Group, T32 MH015442, funded E.H.’s effort. The research was principally supported by National Institute of Mental Health grants (K01 MH01972, R21 MH067618, R01 MH076919, H.T., PI) and the Kempe Foundation, Pioneer Fund, Daniels Fund, and Children’s Hospital Colorado Research Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors wish to thank Marko Klasnja for statistical consultation and Horace P. Hambrick, for psychotropic medication consultation. The authors have declared that they have no competing or potential conflicts of interest.
Footnotes
Conflict of interest statement: No conflicts declared.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont; 2001. [Google Scholar]
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, Giles WH. The enduring effects of abuse and related adverse experiences in childhood. European Archives of Psychiatry and Clinical Neuroscience. 2006;256:174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appleyard K, Egeland B, Dulmen MH, Sroufe LA. When more is not better: The role of cumulative risk in child behavior outcomes. Journal of Child Psychology and Psychiatry. 2005;46:235–245. doi: 10.1111/j.1469-7610.2004.00351.x. [DOI] [PubMed] [Google Scholar]
- Baglivio MT, Wolff KT, Piquero AR, Bilchick S, Jackowski K, Epps N. Maltreatment, child welfare, and recidivism in a sample of deep-end crossover youth. Journal of Youth and Adolescence. 2016;45:625–654. doi: 10.1007/s10964-015-0407-9. [DOI] [PubMed] [Google Scholar]
- Becker SP, Ramsey RR, Byars KC. Convergent validity of the child behavior checklist sleep items with validated sleep measures and sleep disorder diagnoses in children and adolescents referred to a sleep disorders center. Sleep Medicine. 2015;16(1):79–86. doi: 10.1016/j.sleep.2014.09.008. [DOI] [PubMed] [Google Scholar]
- Bricard C, Boidein F. Prescribing Ritalin in combined modality management of hyperactivity with attention deficit. Encephale. 2001;27:435–443. [PubMed] [Google Scholar]
- Briere J. Trauma Symptom Checklist for Children (TSCC) professional manual. Odessa, FL: Psychological Assessment Resources; 1996. [Google Scholar]
- Bruskas D, Tessin DH. Adverse childhood experiences and psychosocial well-being of women who were in foster care as children. The Permanente Journal. 2013;17:e131–e141. doi: 10.7812/TPP/12-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckhalt JA, El-Sheikh M, Keller P. Children’s sleep and cognitive functioning: Race and socioeconomic status as moderators of effects. Child Development. 2007;78:213–31. doi: 10.1111/j.1467-8624.2007.00993.x. [DOI] [PubMed] [Google Scholar]
- Buckley TM, Schatzberg AF. On the interactions of the hypothalamic-pituitary- adrenal (HPA) axis and sleep: Normal HPA axis activity and circadian rhythm, exemplary sleep disorders. The Journal of Clinical Endocrinology & Metabolism. 2005;90:3106–3114. doi: 10.1210/jc.2004-1056. [DOI] [PubMed] [Google Scholar]
- Burroughs VJ, Maxey RW, Levy RA. Racial and ethnic differences in response to medicines: Towards individualized pharmaceutical treatment. Journal of the National Medical Association. 2002;94(10):1–26. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2594139/pdf/jnma00329-0002.pdf. [PMC free article] [PubMed] [Google Scholar]
- Charuvastra A, Cloitre M. Safe enough to sleep: Sleep disruptions associated with trauma, posttraumatic stress, and anxiety in children and adolescents. Child and Adolescent Psychiatric Clinics of North America. 2009;18:877–891. doi: 10.1016/j.chc.2009.04.002. [DOI] [PubMed] [Google Scholar]
- Clinkinbeard SS, Simi P, Evans MK, Anderson AL. Sleep and delinquency: Does the amount of sleep matter? Journal of Youth and Adolescence. 2011;40:916–930. doi: 10.1007/s10964-010-9594-6. [DOI] [PubMed] [Google Scholar]
- Dayyat EA, Spryut K, Molfese DL, Gozal D. Sleep estimates in children: Parental versus actigraphic assessments. Nature and Science of Sleep. 2011:115–123. doi: 10.2147/NSS.S25676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Buckhalt JA, Mize J, Acebo C. Marital conflict and disruption of children’s sleep. Child Development. 2006;77:31–43. doi: 10.1111/j.1467-8624.2006.00854.x. [DOI] [PubMed] [Google Scholar]
- Galovski TE, Monson C, Bruce SE, Resick PA. Does cognitive-behavioral therapy for PTSD improve perceived health and sleep impairment? Journal of Traumatic Stress. 2009;22:19–204. doi: 10.1002/jts.20418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelaye B, Kajeepeta S, Zhong QY, Borba CP, Rondon MB, Sánchez SE, Williams MA. Childhood abuse is associated with stress-related sleep disturbance and poor sleep quality in pregnancy. Sleep Medicine. 2015;16:1274–1280. doi: 10.1016/j.sleep.2015.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregory AM, Eley TC, O’Connor TG, Plomin R. Etiologies of associations between childhood sleep and behavioral problems in a large twin sample. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43:744–751. doi: 10.1097/01.chi/0000122798.47863.a5. [DOI] [PubMed] [Google Scholar]
- Gregory AM, Cousins JC, Forbes EE, Trubnick L, Ryan ND, Axelson DA, Dahl RE. Sleep items in the child behavior checklist: A comparison with sleep diaries, actigraphy, and polysomnography. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50:499–507. doi: 10.1016/j.jaac.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho DE, Imai K, King G, Stuart EA. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Political Analysis. 2007;15:199–236. [Google Scholar]
- Ho DE, Imai K, King G, Stuart EA. MatchIt: Nonparametric preprocessing for parametric causal inference. Journal of Statistical Software. 2011;42:1–28. https://www.unifr.ch/appecon/assets/files/Mastercourses/policy%20and%20impact%20/matchit-package-for-r-detailed-description.pdf. [Google Scholar]
- Holley S, Hill CM, Stevenson J. An hour less sleep is a risk factor for childhood conduct problems. Child: Care, Health and Development. 2011;37:563–570. doi: 10.1111/j.1365-2214.2010.01203.x. [DOI] [PubMed] [Google Scholar]
- Huizinga D, Esbensen FA, Weiher AW. Are there multiple paths to delinquency? Journal of Criminal Law & Criminology. 1991;82:83–118. [Google Scholar]
- Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychological Methods. 2010;15:309–334. doi: 10.1037/a0020761. [DOI] [PubMed] [Google Scholar]
- Imai K, Keele L, Tingley D, Yamamoto T. Unpacking the black box of causality: Learning about causal mechanisms from experimental and observational studies. American Political Science Review. 2011;105:765–789. [Google Scholar]
- Kajeepeta S, Gelaye B, Jackson CL, Williams MA. Adverse childhood experiences are associated with adult sleep disorders: a systematic review. Sleep Medicine. 2015;16:320–330. doi: 10.1016/j.sleep.2014.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolko DJ, Hurlburt MS, Zhang J, Barth RP, Leslie LK, Burns BJ. Posttraumatic stress symptoms in children and adolescents referred for child welfare investigation: A national sample of in-home and out-of-home care. Child Maltreatment. 2010;15:48–63. doi: 10.1177/1077559509337892. [DOI] [PubMed] [Google Scholar]
- Koren D, Arnon I, Lavie P, Klein E. Sleep complaints as early predictors of posttraumatic stress disorder: A 1-year prospective study of injured survivors of motor vehicle accidents. American Journal of Psychiatry. 2002;159:855–857. doi: 10.1176/appi.ajp.159.5.855. [DOI] [PubMed] [Google Scholar]
- Kovachy B, O’Hara R, Hawkins N, Gershon A, Primeau MM, Carrion V. Sleep Disturbance in Pediatric PTSD: Current Findings and Future Directions. Journal of Clinical Sleep Medicine. 2013;9:501–510. doi: 10.5664/jcsm.2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanktree CB, Gilbert AM, Briere J, Taylor N, Chen K, Maida CA, Saltzman WR. Multi-informant assessment of maltreated children: Convergent and discriminant validity of the TSCC and TSCYC. Child Abuse & Neglect. 2008;32:621–625. doi: 10.1016/j.chiabu.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Lansford JE, Miller-Johnson S, Berlin LJ, Dodge KA, Bates JE, Pettit GS. Early physical abuse and later violent delinquency: A prospective longitudinal study. Child Maltreatment. 2007;12:233–245. doi: 10.1177/1077559507301841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebourgeois MK, Giannotti F, Cortesi F, Wolfson A, Harsh J. The relationship between reported sleep hygiene and sleep quality in Italian and American adolescents. Annals of the New York Academy of Sciences. 2004;1021(1):352–354. doi: 10.1196/annals.1308.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lepore SJ, Kliewer W. Violence exposure, sleep disturbance, and poor academic performance in middle school. Journal of Abnormal Child Psychology. 2013;41:1179–1189. doi: 10.1007/s10802-013-9709-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupien SJ, McEwan BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour, and cognition. Nature Reviews: Neuroscience. 2009;10:434–445. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- Maschi T, Bradley CA, Morgen K. Unraveling the link between trauma and delinquency: The mediating role of negative affect and delinquent peer exposure. Youth Violence and Juvenile Justice. 2008;6:136–157. [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- Meldrum RC, Barnes JC, Hay CJ. Sleep deprivation, low self-control, and delinquency: A test of the strength model of self-control. Journal of Youth and Adolescence. 2015;44:465–477. doi: 10.1007/s10964-013-0024-4. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mindell JA, Meltzer LJ. Behavioral sleep disorders in children and adolescents. Annals of the Academy of Medicine Singapore. 2008;37:722–728. [PubMed] [Google Scholar]
- Moffitt TE. Adolescence-limited and life-course persistent antisocial behavior: A developmental taxonomy. Psychological Review. 1993;100:674–701. [PubMed] [Google Scholar]
- Moore KA, Ramirez AN. Adverse childhood experience and adolescent well-being: Do protective factors matter? Child Indicators Research. 2015;9:299–316. [Google Scholar]
- Owens J, Wang G, Lewin D, Skora E, Baylor A. Association between short sleep duration and risk behavior factors in middle school students. Sleep. 2017;40 doi: 10.1093/sleep/zsw004. [DOI] [PubMed] [Google Scholar]
- Paavonen EJ, Aronen ET, Moilanen I, Piha J, Rasanen E, Almqvist F. Sleep problems of school-aged children: A complementary view. Acta Paediatr. 2000;89:223–228. doi: 10.1080/080352500750028870. [DOI] [PubMed] [Google Scholar]
- Peach HD, Gaultney JF. Sleep, impulse control, and sensation-seeking predict delinquent behavior in adolescents, emerging adults, and adults. Journal of Adolescent Health. 2013;5:293–299. doi: 10.1016/j.jadohealth.2013.03.012. [DOI] [PubMed] [Google Scholar]
- Core Team R. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2016. [Google Scholar]
- Raghavan R, Zima BT, Andersen RM, Liebowitz AA, Schuster MA, Landsverk J. Psychotropic medication use in a national probability sample of children in the child welfare system. Journal of Child and Adolescent Psychopharmacology. 2005;15:97–106. doi: 10.1089/cap.2005.15.97. [DOI] [PubMed] [Google Scholar]
- Raviv T, Taussig HN, Culhane SE, Garrido EF. Cumulative risk exposure and mental health symptoms among maltreated youth placed in out-of-home care. Child Abuse & Neglect. 2010;34:742–751. doi: 10.1016/j.chiabu.2010.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richters JE, Martinez P. The NIMH community violence project: I. Children as victims of and witnesses to violence. Psychiatry. 1993;56:7–21. doi: 10.1080/00332747.1993.11024617. [DOI] [PubMed] [Google Scholar]
- Roth T, Zorick F, Sicklesteel J, Stepanski E. Effects of benzodiazepines on sleep and wakefulness. British Journal of Clinical Pharmacology. 1981;11:31S–35S. doi: 10.1111/j.1365-2125.1981.tb01836.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubens SL, Fite PJ, Cooley JL, Canter KS. The role of sleep in the relation between community violence exposure and delinquency among Latino adolescents. Journal of Community Psychology. 2014;42:723–734. [Google Scholar]
- Ryan JP, Testa MF. Child maltreatment and juvenile delinquency: Investigating the role of placement and placement instability. Children and Youth Services Review. 2005;27:227–249. [Google Scholar]
- Shader M. Risk factors for delinquency: An overview. Washington, DC: Office of Juvenile Justice and Delinquency Prevention; 2001. [Google Scholar]
- Smaldone A, Honig JC, Byrne MW. Sleepless in America: Inadequate sleep and relationships to health and well-being of our nation’s children. Pediatrics. 2007;119(Suppl1):S29–37. doi: 10.1542/peds.2006-2089F. [DOI] [PubMed] [Google Scholar]
- Stein BD, Zima BT, Elliott MN, Burnam A, Shahinfar A, Leavitt LA. Violence exposure among school-age children in foster care: Relationship to distress symptoms. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:588–594. doi: 10.1097/00004583-200105000-00019. http://dx.doi.org.proxy.library.umkc.edu/10.1097/00004583-200105000-00019. [DOI] [PubMed] [Google Scholar]
- Stouthamer-Loeber M, Loeber R, Homish DL, Wei E. Maltreatment of boys and the development of disruptive and delinquent behavior. Development and Psychopathology. 2001;13:941–955. [PubMed] [Google Scholar]
- Taussig HN. Risk behaviors in maltreated youth placed in foster care: A longitudinal study of protective and vulnerability factors. Child Abuse and Neglect. 2002;26:1179–1199. doi: 10.1016/s0145-2134(02)00391-5. [DOI] [PubMed] [Google Scholar]
- Taussig H, Culhane S, Hettleman D. Fostering healthy futures: An innovative prevention program for preadolescent maltreated youth in foster care. Child Welfare. 2007;86:113–131. [PMC free article] [PubMed] [Google Scholar]
- Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. Mediation: R package for causal mediation analysis. Journal of Statistical Software. 2014;59:1–38. [Google Scholar]
- Tininenko JR, Fisher PA, Bruce J, Pears KC. Sleep disruption in young foster children. Child Psychiatry and Human Development. 2010a;41:409–424. doi: 10.1007/s10578-010-0177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tininenko JR, Fisher PA, Bruce J, Pears KC. Associations between sleep and intattentive/hyperactive problem behavior among foster and community children. Journal of Developmental and Behavioral Pediatrics. 2010b;31:668–674. doi: 10.1097/DBP.0b013e3181f1773b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson S, Argyropoulos S. Antidepressants and sleep: A qualitative review of the literature. CNS Drugs. 2005;65:927–947. doi: 10.2165/00003495-200565070-00003. [DOI] [PubMed] [Google Scholar]


