Abstract
A key determinant of population health is the behavioral profile of a population. Nearly eighty percent of American adults enter older age having smoked cigarettes or been obese. It is unknown to what extent risky behaviors (e.g., smoking, poor diet and physical inactivity, excessive alcohol consumption) cumulatively are reducing U.S. health and life expectancy and what levels might be achievable in their absence. Using data from the Health and Retirement Study, we studied individuals aged 50+ who never smoked, were not obese, and consumed alcohol moderately. Compared to the U.S. population, those with a favorable behavioral profile have up to seven years longer life expectancy at age 50 and they experience up to six years postponement in the onset of disability. These results provide a benchmark for evaluating the massively damaging effects that behavioral risks have on health at older age and the importance of policy prioritization for behavioral-based interventions.
INTRODUCTION
Older Americans are living longer and are generally healthier than their predecessors.1,2 In aging societies, the health and functional ability of the elderly is of central policy significance. Nearly all high-income countries subsidize medical and hospice care for the elderly and a healthier older population is more capable of contributing to economic and social roles than an unhealthier one. Actuarial calculations informing Social Security’s future solvency rely heavily on the longevity expectations of those who will enter old age in the coming decades.3
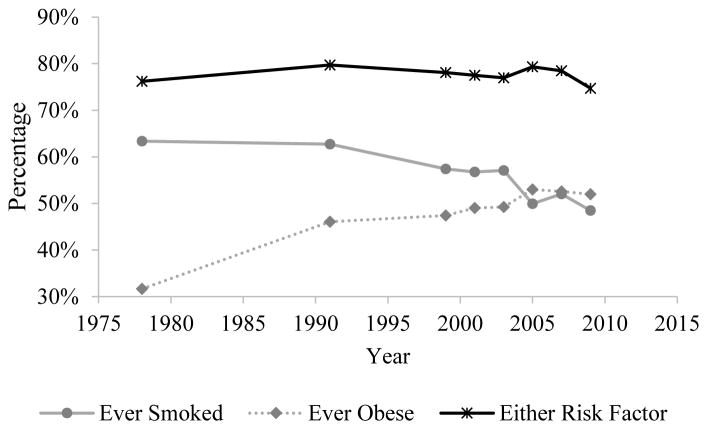
Research documents strong heterogeneity in healthy aging across individuals—that is individuals appear to “age” at different rates.4 Among the key determinants of this variation are health-related behaviors whose effects often are realized over the long-term and at older age (e.g., cigarette smoking, diet, physical activity). By ages 50–59, nearly 80% of American adults have either ever smoked or have been obese, a level that has remained remarkably stable since the 1970s (Exhibit 1). While the percentage of Americans who have smoked has been declining over time, the prevalence of obesity has increased markedly, potentially off setting health gains made from reductions in smoking.5,6
Exhibit 1.
Prevalence of ever smoking, ever obesity, and the presence of either risk factor among adults aged 50–59 in the U.S. National Health and Nutrition Examination Survey. Ever smoked is having smoked at least 100 cigarettes in lifetime based on respondent reports. Ever obese is ever having a BMI≥30 kg/m2 ascertained from a question asking about maximum lifetime body weight (excluding pregnancy). Prevalence of either risk factor is having reported ever smoking or having ever been obese.
Data Source: Author analysis of U.S. National Health and Nutrition Examination Survey II (1976–1980), III (1988–1994), and 1999–2010.
The combined prevalence of smoking and obesity suggests that these two behavioral factors are key determinants of healthy aging among older Americans (obesity being an indicator for dietary and physical activity behaviors). [An additional behavioral factor is excessive alcohol consumption. Recent estimates indicate that 1 in 10 deaths among adults ages 20–64 during 2006–2010 were attributable to excessive alcohol consumption.7] Because behavioral factors can be targeted by a wide range of policies, measuring their cumulative impact aids in the prioritization of such policies.
The massively damaging effects risky behaviors are having on population health is increasingly recognized by international bodies outside of the traditional health sector. In 2011, for example, the United Nations General Assembly held a high level meeting on non-communicable disease, of which behavioral interventions were a primary focus. This meeting was the first high-level meeting convened over a health issue since HIV/AIDS.
Among scientists, there is also long-standing interest in identifying maximum achievable levels of human health and longevity.8–10 One approach has been the study of “vanguard” populations — groups that exhibit exceptionally favorable health — such as select religious minorities (e.g., Seventh Day Adventists, Mormons) and scientific elites.11,12 A key vanguard population that to our knowledge has not been analyzed in this context is individuals who possess a favorable behavioral profile across multiple behaviors such as individuals who never smoked, are non-obese, and drink alcohol moderately. A vanguard population defined by a favorable behavioral profile will be drawn broadly from diverse socioeconomic and race/ethnic groups. Thus, the study of their health would be highly informative to understanding maximum achievable levels of health and longevity in large populations.
Against this backdrop, we evaluated the extent to which three major behavioral factors (cigarette smoking, obesity, and unhealthy alcohol consumption) influence the overall and disability-free life expectancy of Americans over age 50. Our contribution is two-fold. First, the focus on life expectancies provide straightforward policy-relevant metrics to assess the population-level effects of behavioral factors. Disability-free life expectancy, or how long an individual is expected to live without a disability, is particularly relevant because it conveys information on the functional capacity of older individuals.
Second, we analyzed sub-groups by behavioral profiles, in addition to addressing each risk factor separately. This approach allows us to assess the total effect of the three risk factors. We gave particular focus to individuals who have a low-risk profile (e.g., individuals who have never smoked, are not obese, and drink alcohol at healthy levels) as the study of these individuals provides insight into how much the three risk factors combined are holding back overall and disability-free life expectancy.
METHODS
Data
Data were from the U.S. Health and Retirement Study (HRS), a high-quality on-going longitudinal survey on health among middle- and older-aged Americans that began in 1992. The HRS is supported by the U.S. National Institute on Aging and the Social Security Administration and is conducted by the University of Michigan.13 Respondents were re-surveyed biannually with follow-up response levels consistently above 85%.14 Since 1998, the HRS has been nationally representative of non-institutionalized Americans aged 50+. After participants enroll in the study, the HRS follows them even if they become institutionalized. HRS data are linked to the U.S. National Death Index. We used the RAND HRS Data file, version N, which is an easy to use longitudinal data set based on the HRS data. It was developed at RAND with funding from the National Institute on Aging and the Social Security Administration.15
Our analytical sample included respondents aged 50–74 in 1998 (N=14,804). Disability transitions and deaths were modeled during 2000–2012. There were 4,305 deaths and 6,795 disability transitions over 153,991 person-years of follow-up (Supplementary Appendix 1 shows descriptive information on deaths and transitions across disability states).16
Measures
Disability was defined by a respondent report of a limitation in at least one of five activities of daily living (ADL): walking, dressing, bathing, getting in/out of bed, or eating. Respondents not reporting any limitations were considered disability-free.
Smoking categories were current, former, or never smoker with never smoker as the low-risk category. Weight status categories, based on Centers for Disease Control and Prevention definitions for adults, were obese (BMI≥30.0) and non-obese (BMI<30), with non-obese as the low-risk category. Because preliminary models indicated non-significant differences in risk between normal weight (BMI 20.0–24.9) and overweight (BMI 25.0–29.9) respondents in these two groups were combined in the non-obese category. Underweight respondents (BMI<18.5) were excluded from the low-risk non-obese group.
Alcohol consumption groups were non-drinker or irregular drinker, moderate drinker, and heavy drinker, with moderate drinker as the low-risk category.17,18 Moderate and heavy drinker categories were defined as drinking alcohol at least one day per week in addition to meeting a threshold for weekly number of drinks: moderate – less than 14 drinks per week for men and less than 7 drinks per week for women and heavy – 14 or more drinks per week for men and 7 or more drinks per week for women.19 Individuals who reported drinking alcohol less than one day per week (irregular drinkers), who represented about one-fifth of all drinkers, were classified with non-drinkers because preliminary analyses revealed higher mortality and disability risks in irregular drinkers compared to the low-risk moderate drinkers.
Low-risk Behavioral Profiles
We examined two low-risk behavioral (LRB) profiles: LRB 1 was individuals who never smoked and were non-obese. LRB 2 was individuals who never smoked, were non-obese, and were moderate alcohol consumers. Individuals at high-risk on multiple behaviors were also evaluated: (1) obese + ever-smoker and (2) obese + ever-smoker + non-moderate drinker.
Control variables were educational attainment (< high school (HS) completion, HS degree/GED/some college attendance, college graduate) and race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, non-Hispanic other race).
Statistical Analysis
We produced two sets of metrics. The first was the mean age of first incident disability conditional on being non-disabled at age 50. The second was life expectancy in disabled and non-disabled states. We measured overall life expectancy, disabled life expectancy, and disability-free life expectancy, all from age 50. We used multinomial logistic regression models to estimate age- and sex-specific transition probabilities across the states of non-disabled, disabled, and dead. We used the estimated transition probabilities in structured matrix population models to estimate life expectancies at age 50 in the various states (disabled, non-disabled, overall) and mean age of first incident disability. Matrix population models are extensions of multi-state life table techniques.20
Supplementary Appendix 2 describes the regression and matrix population models and Supplementary Appendix 3 provides coefficients from the regression models.16
Standard errors were estimated using bootstrap procedures. All analyses were conducted using Stata 14. Statistical code is available by request.
Study Limitations
A limitation is that we were unable to account for the wide number of behavioral factors that affect health. We relied on three behavioral factors that have been shown to have the largest impact on life expectancy in high-income countries. Obesity is an imperfect marker of lifelong dietary practices and physical activity. Sufficient detailed dietary histories are rarely available in health surveys and is not available in our data. The data we use does contain information on physical activity levels. However, physical activity levels will simultaneously be a cause and consequence of health rendering it difficult to infer reliable estimates of the effect of physical activity on health. We were also unable to observe disability incidence for individuals prior to entering our risk set at ages 50–74, thus the estimated mean age at first onset of disability does not account for disability incidence occurring prior to study entry and the actual mean age of disability incidence will be lower than what we show.
While our study provides novel insight into potential health gains from adopting low-risk behaviors, our study did not address the role of genetic factors, which may simultaneously influence both the presence of a risk factor and its damaging effects.21 For example, a similar set of genes may increase both the risk of becoming obese, given a certain diet, and the negative metabolic consequences of obesity.22 In addition, people who refrain from risky behavior may be likely to have other health-promoting traits (e.g., optimistic outlook), and our study did not account for this selection.
STUDY RESULTS
Descriptive Characteristics
At study onset, 13% of women and 10% of men were disabled. Approximately 26% of the sample were obese, 62% ever smokers, and 73% non/irregular or heavy drinkers. Twenty-seven percent of the sample were non-obese never-smokers (LRB1). Women (33%) were more likely than men (20%) to be in this low-risk category. Seven percent of the sample were non-obese never-smokers who drink moderately (LRB 2), with equal percentages of men and women. Supplementary Appendix 4 provides a table of sample characteristics at baseline in 1998.16 While individuals from all educational levels were represented among the LRBs, those with higher levels of education were more likely to be LRBs than others (Supplementary Appendix 5 shows the educational distribution for the behavioral groups).16
Disability Onset
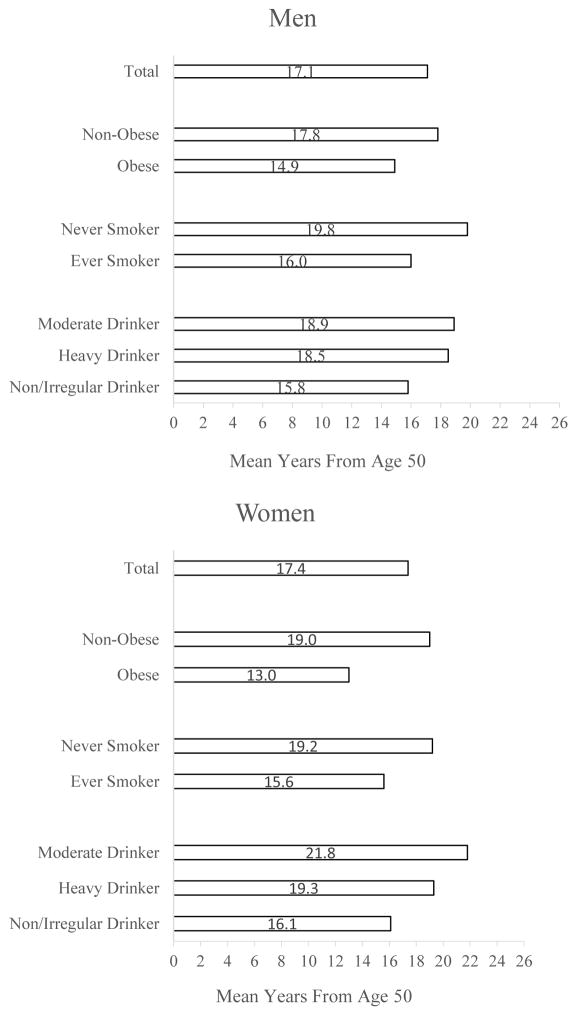
As expected, each behavioral risk factor was associated with early disability onset (Exhibit 2). Compared to the average for the entire population, obesity stood out as being the most consequential. On average, obese men became disabled at age 64.9 years, and obese women at age 63.0 years, a penalty of 3 years for men and 6 years for women when compared to their non-obese counterparts.. LRB 1 men and women had a mean age of first incident disability above age 70, 3.5 years longer than the total population. LRB 2 men and women displayed the longest postponement with a mean age of first disability incidence of 72.1 for men and 75.2 for women. Supplementary Appendix 6 shows mean age of first disability incidence since age 50 by behavioral profile.16
Exhibit 2.
Mean age of first disability incidence from age 50 by behavioral risk factor.
Data Source: Author analysis of U.S. Health and Retirement Survey, 1998
Notes: Total is entire sample. Obesity is defined as BMI≥30.0 kg/m2. Ever smoker includes former and current smokers. Moderate drinking are individuals who drink and consume <14 drinks/week (men) and <7 drinks/week (women). Heavy drinking is ≥14 drinks/week (men) and ≥7 drinks/week (women).
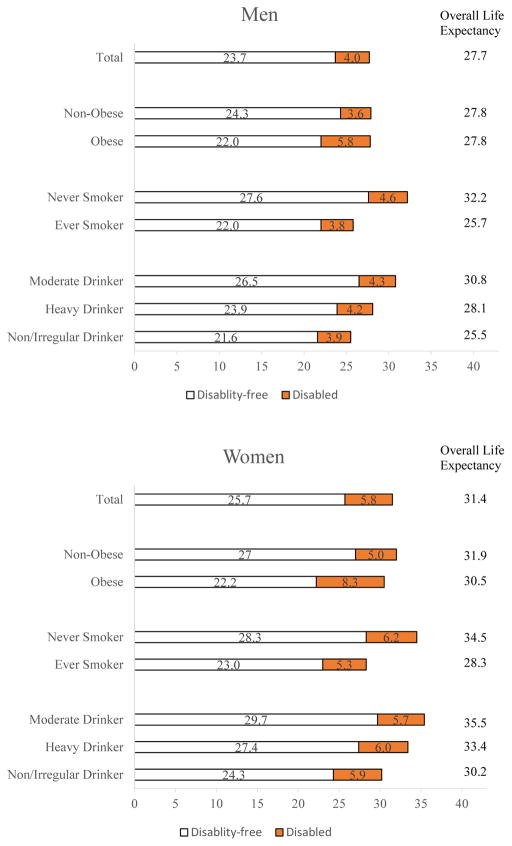
Life Expectancies
Life expectancy for the total population at age 50 was 27.7 years for men and 31.4 years for women, which translates into a life expectancy of 77.7 years for men and 81.4 years for women (Exhibit 3). Our life expectancy estimates were similar to U.S. life expectancy from 2005 National Vital Statistics data.23 Women spent more years of life disabled than men, 5.8 years compared to 4.0 years for men. Obesity had a moderate effect on overall life expectancy, and a more substantial effect on disability-free life expectancy. Non-obese men lived 2.3 years longer disability-free compared to obese men, and non-obese women lived 4.8 years longer disability-free than non-obese women. The non-obese also spent less time disabled compared to the obese, 2.2 years less for men and 3.3 years less for women.
Exhibit 3.
Overall, disability-free, and disabled life expectancy at age 50, by behavioral risk factor. Data Source: Author analysis of U.S. Health and Retirement Study (1998–2012)
Notes: X-axis represents number of years from age 50. Total is entire analytical sample from HRS. Obesity is defined as BMI≥30.0 kg/m2. Ever smoker includes former and current smokers. Moderate drinking are individuals who drink and consume <14 drinks/week (men) and <7 drinks/week (women). Heavy drinking is ≥14 drinks/week (men) and ≥7 drinks/week (women).
Never-smokers had a substantially longer overall and disability-free life expectancy compared to ever-smokers but experienced a longer time living with a disability. Compared to heavy drinkers and non/irregular drinkers, moderate drinkers exhibited the longest overall and disability-free life expectancies.
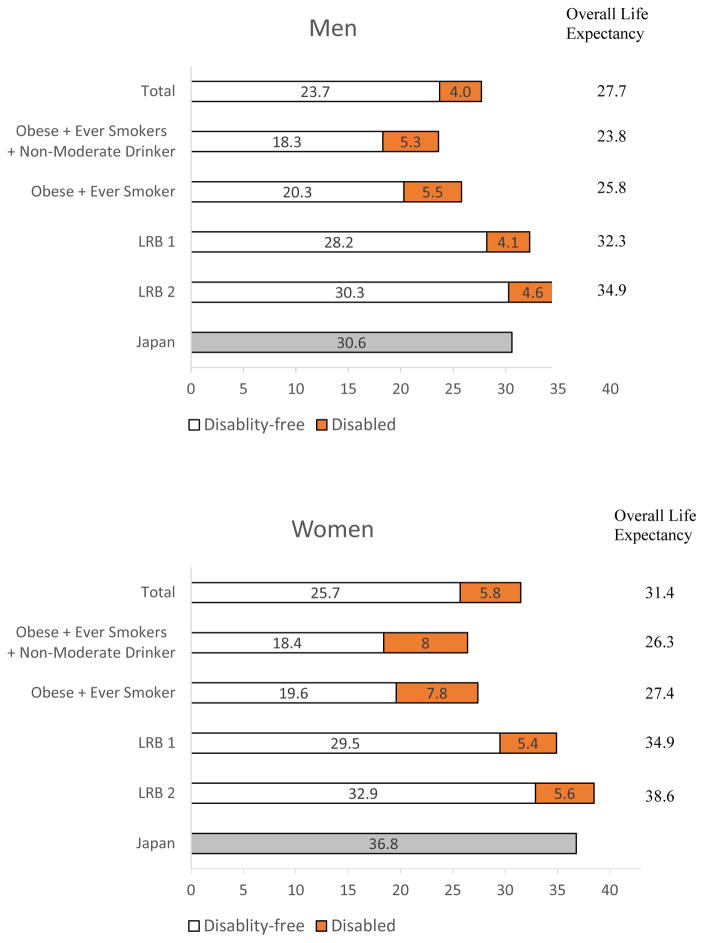
The life expectancy advantages of the LRB populations is shown in Exhibit 4. LRB men and women a 4 (LRB 1) to 7 (LRB 2) years longer than the total population. Importantly, nearly all of this advantage was due to a longer disability-free life. Thus, LRB populations not only live longer, they do so in disabled-free state. In contrast, obese, ever-smoking, non-moderate drinkers lived four to five years less overall than the total population and five to seven years less in a disability-free state. The difference is greater comparing the best to the worst profiles. For example, a 50-year-old woman who never smoked, was never obese, and drinks moderately will live an extra 12 years, on average, than the same-age obese woman who ever smoked and does not drink moderately. The difference in life expectancy between the two categories was 11.1 years for men.
Exhibit 4.
Overall, disability-free, and disabled life expectancy at age 50 by behavioral profile. Data Sources: Author analysis of U.S. Health and Retirement Study (1998–2012). Human Mortality Database (Japan, 2005).
Notes: X-axis represents number of years from age 50. Total is entire analytical sample from HRS. LRB 1 represents non-obese never smokers and LRB 2 represents non-obese, never smokers, and moderate drinkers. Shaded grey bar for Japan indicates overall life expectancy at age 50 in 2005 as published in the Human Mortality Database.49
The exceptional profile of the LRB populations is further borne out through a comparison with life expectancy in 2005 in Japan, a nation known for the long lives of its citizens (Exhibit 4). Life expectancy at age 50 for the U.S. total population lagged behind life expectancy in Japan by three years for men and five years for women. With the exception of LRB 1 women, the other three LRB groups had a longer total life expectancy compared to Japan. Supplementary Appendix 7 provides 95% confidence intervals for all estimates shown in Exhibits 3–4.16
Additional Findings
In our sample, the dominant smoking group was former smokers (41% of the total sample) and it is relevant to ask whether individuals who quit early in life can still experience a long and disabled-free life. In separate analyses (data not shown), we found that non-obese individuals who quit smoking ten or more years prior to survey entry and drank alcohol moderately had total and healthy life expectancies only one year shorter than non-obese never-smokers who drank alcohol moderately (LRB2).
We also explored whether the life expectancies at age 50 changed over the period of study. We split the data into two periods – 1998–2004 and 2005–2010 – and compared life expectancy at age 50 across the two periods. For the total sample, life expectancy at age 50 increased by about 0.60 years, about one-third of this time disability-free and two-thirds with disability. Results were similar for the two low risk behavior groups. However, our analysis was likely underpowered to distinguish differences in trends across these subgroups.
DISCUSSION
Sizeable segments of the U.S. population exhibit advantageous behavioral profiles, but little is known about how long they live because prior research is limited to studying the effect of single health behaviors on life expectancy. Studying the effect of multiple health behaviors exercised simultaneously provides new insight into levels of health that are achievable without novel life-extending medical technologies.
We analyzed non-disabled and disabled life expectancy for low-risk behavioral groups, one consisting of respondents who were not obese and never smoked and a similar group whose members also drank alcohol moderately. Compared to the average American, these two low-risk groups had a 4–7 year advantage in life expectancy at age 50 and experienced substantially postponed onset of disability. Strikingly, these populations also experienced a disability-free life expectancy similar to or longer than the overall life expectancy of the average American. A methodological advantage of our study was that longitudinal data were used to estimate transition probabilities, avoiding the biases arising from cross-sectional approaches.24
Risk Factor Prevention
Our findings are best interpreted in the context of population-level risk factor prevention, namely, the potential health gains realizable if more Americans adopted a low-risk behavioral profile.
The findings of our study do demonstrate what is being achieved by a sizeable segment of Americans and may be potentially achievable for many others. The low-risk behavioral groups have a life expectancy comparable to other exceptionally long-lived populations. Montez and Hayward25 examined populations defined by a combination of race, childhood health, socioeconomic adversities, and educational attainment and found that the most advantaged groups—those with favorable childhood health, no socioeconomic adversity, and high educational achievement—had life expectancies of 82 years for men and 86 years for women, similar to our estimates for the low-risk groups. Immigrant populations also exhibit exceptionally high longevity attributed in part to positive health selection (i.e., “the healthy migrant effect” and normative traits that may refrain them from engaging in risky behaviors. Mehta et al.26 showed that, during 2000–2010, U.S. immigrants had a life expectancy of 84 years for men and 87 years for women. Neither study accounted explicitly for behavioral factors.
Role of Behavioral Change
Our approach did not lend itself to estimating the benefits of behavioral change among individuals already having a risk factor. However, our study provides some indications of the sizeable benefits achievable through behavioral change. We found that individuals who quit smoking 10 years or more prior to our study experienced an exceptionally long disabled-free life if they also are at low-risk on other behavioral factors. This finding is consistent with prior findings illustrating that quitting smoking and other favorable behavioral changes, even in late-life, enhances longevity.27 Similarly, an emerging body of evidence suggests that obesity exhibits “duration” effects in that reducing the length of time obese may be associated with improved health.28
Disability Postponement
Our study of the low-risk behavioral groups suggest that these exceptional groups experience substantial disability postponement compared to others. The benefit to society is that postponement will defer disability-associated healthcare costs into older ages and enable opportunities for individuals to work longer. Nonetheless, our findings also indicate that low-risk groups live a similar number of disabled years compared to the total population. In other words, we did not find evidence of a “compression” of disability among the low-risk groups.
In contrast, those with multiple behavioral risk factors not only have a short life but also experience an extended time disabled, underscoring the large negative effects of risky behavioral factors. Of note is that we found obesity to be strongly associated with years lived with a disability, a finding that has been reported in at least one previous study and is especially concerning given obesity’s rising prevalence since at least the early 1980s.29 As evidenced in our Exhibit 1 and some previous analyses of the National Health and Nutrition Examination Survey (NHANES),30 the rising trend of obesity may have levelled during the early and mid 2000s. However, we believe that it is premature to infer that the long-term rise in obesity has ended. For example, between 2005–2006 and 2013–2014 the prevalence of obesity among American adult women showed significant increases according to analyses of NHANES data.31
Policy Considerations
As aging nations grapple with the social, economic, and fiscal consequences of a growing elderly population, a key variable is the future health status of the older population.32 Our findings indicate that the high prevalence of risky behaviors poses a formidable challenge to achieving even larger improvements in population health. Optimistically, evidence supports that population-level behavioral profiles can be responsive to large-scale and high-level policy efforts with some of the most convincing evidence coming from anti-smoking campaigns.33 The Affordable Care Act made a major step forward in federal support for prevention through its establishment of the Prevention and Public Health Fund of which behavioral improvement is a core focus. Financial “sticks” through taxation of cigarettes, alcohol, and potentially beverages and foods associated with obesity also enjoy a solid evidence base.34 The success of these and other policies in helping people to maintain a healthy body weight and refrain from smoking and heavy alcohol consumption will largely define whether the future of aging in the U.S. is healthy or disabled.
Supplementary Material
Acknowledgments
Both authors contributed equally to this work and are listed in alphabetical order by last name. This research was supported by the National Institute on Aging (NIA) (Grant No. R01AG040212; principal investigator: Samuel Preston), and pilot funding from the NIA supported the Network on Life Course Health Dynamics and Disparities in 21st Century America (Grant No. NIA R24AG045061; http://isr.umich.edu/nlchdd/). Mikko Myrskylä was supported by the European Research Council (Grant No. 336475). The authors thank Daniel Schneider for his excellent statistical support. The viewpoints expressed reflect those of the authors and not necessarily those of any funding body or affiliated institution. [Published online July 19, 2017.]
References
- 1.Cutler DM, Landrum MB. Dimensions of Health in the Elderly Population. National Bureau of Economic Research; 2011. [accessed 13 Feb 2017]. http://www.nber.org/papers/w17148. [Google Scholar]
- 2.Kramarow E, Lubitz J, Lentzner H, Gorina Y. Trends In The Health Of Older Americans, 1970–2005. Health Aff (Millwood) 2007;26:1417–1425. doi: 10.1377/hlthaff.26.5.1417. [DOI] [PubMed] [Google Scholar]
- 3.Board of Trustees. The 2015 Annual Report of the Board of Trustees of the Federal Old-Age Survivors Insurance and Federal Disability Insurance Trust Funds. U.S. Government Publishing Office; 2015. https://www.ssa.gov/oact/tr/2015/tr2015.pdf. [Google Scholar]
- 4.Lowsky DJ, Olshansky SJ, Bhattacharya J, Goldman DP. Heterogeneity in Healthy Aging. J Gerontol A Biol Sci Med Sci. 2014;69:640–649. doi: 10.1093/gerona/glt162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Preston SH, Stokes A, Mehta NK, Cao B. Projecting the effect of changes in smoking and obesity on future life expectancy in the United States. Demography. 2014;51:27–49. doi: 10.1007/s13524-013-0246-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stewart ST, Cutler DM, Rosen AB. Forecasting the effects of obesity and smoking on U.S. life expectancy. N Engl J Med. 2009;361:2252–2260. doi: 10.1056/NEJMsa0900459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stahre M. Contribution of Excessive Alcohol Consumption to Deaths and Years of Potential Life Lost in the United States. Prev Chronic Dis. 2014:11. doi: 10.5888/pcd11.130293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manton KG, Stallard E, Tolley HD. Limits to human life expectancy: evidence, prospects, and implications. Popul Dev Rev. 1991;17:603. [Google Scholar]
- 9.Oeppen J, Vaupel JW. Broken limits to life expectancy. Science. 2002;296:1029–1031. doi: 10.1126/science.1069675. [DOI] [PubMed] [Google Scholar]
- 10.Olshansky SJ, Carnes BA, Cassel C. In search of Methuselah: estimating the upper limits to human longevity. Science. 1990;250:634–640. doi: 10.1126/science.2237414. [DOI] [PubMed] [Google Scholar]
- 11.Andreev EM, Jdanov D, Shkolnikov VM, Leon DA. Long-term trends in the longevity of scientific elites: Evidence from the British and the Russian academies of science. Popul Stud. 2011;65:319–334. doi: 10.1080/00324728.2011.603428. [DOI] [PubMed] [Google Scholar]
- 12.Enstrom JE, Breslow L. Lifestyle and reduced mortality among active California Mormons, 1980–2004. Prev Med. 2008;46:133–136. doi: 10.1016/j.ypmed.2007.07.030. [DOI] [PubMed] [Google Scholar]
- 13.Health and Retirement Study, public use dataset. Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740). Ann Arbor, MI, (2016).
- 14.Health and Retirement Study. [accessed 10 May 2016];Sample Size and Response Rates. 2011 http://hrsonline.isr.umich.edu/sitedocs/sampleresponse.pdf.
- 15.RAND HRS Data, Version N. Produced by the RAND Center for the Study of Aging, with funding from the National Institute on Aging and the Social Security Administration. Santa Monica, CA.
- 16.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 17.Thun MJ, Peto R, Lopez AD, Monaco JH, Henley SJ, Heath CWJ, et al. Alcohol Consumption and Mortality among Middle-Aged and Elderly U.S. Adults. N Engl J Med. 1997;337:1705–1714. doi: 10.1056/NEJM199712113372401. [DOI] [PubMed] [Google Scholar]
- 18.Gaziano JM, Gaziano TA, Glynn RJ, Sesso HD, Ajani UA, Stampfer MJ, et al. Light-to-moderate alcohol consumption and mortality in the physicians’ health study enrollment cohort. J Am Coll Cardiol. 2000;35:96–105. doi: 10.1016/s0735-1097(99)00531-8. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services, U.S. Department of Agriculture. Dietary Guidelines for Americans, 2015–2020. [Google Scholar]
- 20.Caswell H. Applications of Markov chains in demography. In: Langville Stewart WJ., editor. MAM2006: Markov Anniversary Meeting. Boson Books; Raleigh, North Carolina, USA: 2006. [Google Scholar]
- 21.Thorgeirsson TE, Geller F, Sulem P, Rafnar T, Wiste A, Magnusson KP, et al. A variant associated with nicotine dependence, lung cancer and peripheral arterial disease. Nature. 2008;452:638–642. doi: 10.1038/nature06846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Walley AJ, Blakemore AIF, Froguel P. Genetics of obesity and the prediction of risk for health. Hum Mol Genet. 2006;15:R124–R130. doi: 10.1093/hmg/ddl215. [DOI] [PubMed] [Google Scholar]
- 23.Arias E, Rostron BL, Tejada-Vera B. United States life tables, 2005. Natl Vital Stat Rep Cent Dis Control Prev Natl Cent Health Stat Natl Vital Stat Syst. 2010;58:1–132. [PubMed] [Google Scholar]
- 24.Guillot M, Yu Y. Estimating health expectancies from two cross-sectional surveys: The intercensal method. Demogr Res. 2009;21:503–534. doi: 10.4054/DemRes.2009.21.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Montez JK, Hayward MD. Cumulative childhood adversity, educational attainment, and active life expectancy among U.S. adults. Demography. 2014;51:413–435. doi: 10.1007/s13524-013-0261-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mehta NK, Elo IT, Engelman M, Lauderdale DS, Kestenbaum BM. Life Expectancy among U.S.-born and Foreign-born Older Adults in the United States: Estimates from Linked Social Security and Medicare Data. Demography. 2016 doi: 10.1007/s13524-016-0488-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rizzuto D, Orsini N, Qiu C, Wang H-X, Fratiglioni L. Lifestyle, social factors, and survival after age 75: population based study. The BMJ. 2012;345:e5568. doi: 10.1136/bmj.e5568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mehta NK. International Encyclopedia of the Social & Behavioral Sciences. Elsevier; Oxford: 2015. Obesity and Mortality; pp. 75–81. [Google Scholar]
- 29.Reuser M, Bonneux LG, Willekens FJ. Smoking kills, obesity disables: a multistate approach of the US Health and Retirement Survey. Obesity. 2009;17:783. doi: 10.1038/oby.2008.640. [DOI] [PubMed] [Google Scholar]
- 30.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. Jama. 2010;303:235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 31.Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA. 2016;315:2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harper S. Economic and social implications of aging societies. Science. 2014;346:587–591. doi: 10.1126/science.1254405. [DOI] [PubMed] [Google Scholar]
- 33.Cutler D. Ethnic Disparities in Aging Health. National Academy of Sciences; 2002. Behavioral Health Interventions: What Works and Why? [Google Scholar]
- 34.Preston SH. Commentary: When People Behave Badly. Epidemiology. 2014;25:191–193. doi: 10.1097/EDE.0000000000000049. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.