Abstract
HIV-associated histoplasmosis is mainly misdiagnosed for granulomatous diseases, such as tuberculosis. Nonetheless, malignancy-like lesions have been reported sporadically in HIV-infected patients. Although the main reported lesions are erosive or ulcerated, here a rare case of oral tumor is reported. This case raises the awareness of this presentation, and the importance of accurate identification in the laboratory. Performing systematic specific stains for fungal elements and culture on tissue samples ensures accurate differential diagnosis.
Keywords: Histoplasma capsulatum, Histoplasmosis, HIV, Oral, Differential diagnosis
1. Introduction
Histoplasma capsulatum is responsible for histoplasmosis, a deep systemic mycosis with worldwide distribution that can affect both immunocompetent and immunocompromised individuals [1]. Histoplasmosis is mainly an airborne disease. Disruption of soils contaminated by H. capsulatum aerosolizes microconidia which are eventually inhaled by a host [1].
Although it is mostly asymptomatic and spontaneously resolutive in immunocompetent persons, histoplasmosis is symptomatic and disseminated in 95% of HIV-infected patients with a CD4 count less than 200/mm³ [2]. In endemic areas, the pathophysicological mechanism that leads to disease remains debated (new infection or endogenous reactivation) [3].
During HIV infection, the evolution is highly variable, from extreme latency to fulminant forms [2]. The most frequent presentation is subacute, with symptoms evolving for over one or two months. The clinical presentation is misleading, with non-specific symptoms. Fever, fatigue and weight loss are almost constant. The presence of respiratory signs, and/or digestive signs, and/or superficial lymphadenopathies is frequent. Neurological, oral and cutaneous involvements are less frequent. For 10–20% of patients, the presentation is fulminant, similar to septic shock and rapidly fatal [4].
The diagnosis of histoplasmosis requires pathological investigations that are often invasive (bone marrow sample or tissue biopsy). Moreover, it is necessary that clinicians suspect the diagnosis when facing certain clinical situations, in order to ask for specific fungal investigations [4]. Among these are the direct examination of a fresh sample and fungal culture which remains the gold standard method despite its low sensitivity and the slow growth rate of the fungus in culture (up to six weeks) [1], [5]. Among non-culture-based diagnostic tests, serology is not very contributive in HIV-infected patients and molecular tools are not commercialized yet. However, robust enzyme immunoassays (EIAs) on urine, blood or bronchoalveolar lavage are being commercialized [6]. Recent developments in monoclonal antigen detection in urine and blood are promising since the most sensitive EIA developed to date has only been available in the USA [7]. Standard biological examinations are not specific but may orient clinicians.
While waiting for a mycological gold standard-based diagnosis, when clinical suspicion is high, clinicians have two options for treatment initiation according to disease severity: intravenous liposomal amphotericin B (L-AmB) for severe cases or oral itraconazole for non-severe cases [8]. Although L-Amb has shown its fungicidal activity and its efficacy on survival, it is nephrotoxic [9]. L-AmB or alternative lipid formulation of AmB at the same dosage are safer and may be preferred to Deoxycholate-AmB. Itraconazole is fungistatic and exposes to drug-drug interactions if the treatment of potential coinfections and or antiretroviral therapy need to be introduced at the same time. This is compounded by a reduced bioavailability during HIV infection, which makes reaching the recommended effective blood levels long and difficult [1].
Despite numerous publications on HIV-associated histoplasmosis, the true burden of HIV-associated histoplasmosis remains unknown in endemic areas [1], [10]. Nevertheless the disease may rank among the top causes of AIDS-related deaths in Latin America and probably accounts for thousands of deaths every year while being undiagnosed [11]. The disease has been stated a neglected disease because, even in endemic areas, physicians awareness seems insufficient and a few laboratories are able to perform the diagnosis [6], [10]. With no access to diagnostic tools or adapted antifungal therapy, one of the main issues is that histoplasmosis is probably often misdiagnosed for another disease, and therefore physicians do not ask for a fungal diagnosis and do not treat it with antifungals. Reported since the discovery of histoplasmosis, the main differential diagnosis of HIV-associated histoplasmosis is tuberculosis [12]. Malignancy-like clinical presentations also represent a challenging differential diagnosis requiring specific stainings and culture when performing a tumor biopsy in endemic or non-endemic areas. Regarding malignancy-like lesions of the mucous membrane caused by H. capsulatum gastrointestinal and oral involvements have been reported in non-HIV and in HIV-infected patients [13], [14], [15], [16], [17].
Here we report a rare case of oral HIV-associated histoplasmosis because it is important to reinforce awareness of physicians and dentists on fungal infections when facing a malignancy-like oral lesion.
2. Case
A 52 year-old man presented at the emergency department for fever and fatigue. He was a homeless man originating from Haïti and hab been living in French Guiana for over ten years. He was known for an advanced HIV infection diagnosed 7 years before when the patient presented with concomitant pulmonary tuberculosis and pneumocystosis. At the time of HIV infection diagnosis, the CD4 lymphocyte count and HIV viral load were at 57/mm3 and over 6 log10, respectively. The patient received six weeks of anti-tuberculosis therapy and cotrimoxazole for pneumocystosis before fleeing the hospital and interrupting medical follow up. Other past medical events were chronic obstructive pulmonary disease due to smoking, a negative hepatitis C serology, serological evidence of a past toxoplasmosis infection (IgM antibody negative and IgG antibody positive) and serological evidence of a resolved hepatitis B (HBs antigen negative, HBc antibody and HBs antibody positive).
Upon admission in the emergency department, the patient reported anorexia and a 15 kg weight loss over a period of a few months, and a recent dysphonia. There was no dyspnea. Fever was 38.5 °C, and there was a large burgeoning and necrotic ulceration of the base of the tongue and the anterior part of the soft palate pillars, with a whitish coating (Fig. 1). There were no lymphadenopathies, and the rest of the examination was without particularities.
Fig. 1.
Oral examination upon hospital admission.
Biologically, lactate deshydrogenase (LDH) was elevated at 210 IU/l, albumin concentration was 26.7 mg/l, ferritine was 482 mg/l, C-reactive Protein (CRP) was 45 mg/l, creatinine awast 49 µmol/l, and liver enzymes were normal. The hematological results showed platelets at 215,000/mm3, hemoglobin at 9.3 g/dl, and white blood cells at 4 400/mm3. The CD4 lymphocyte count was 40/mm3 with a HIV viral load of 5.5 log10. The search for acid-fast bacilli was negative on 3 sputum samples (direct examination and culture) and in the blood cultures.
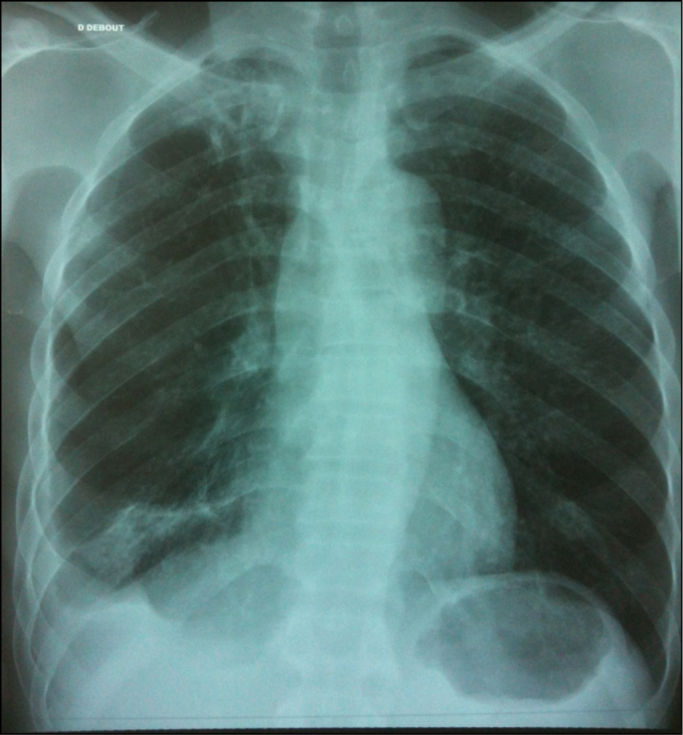
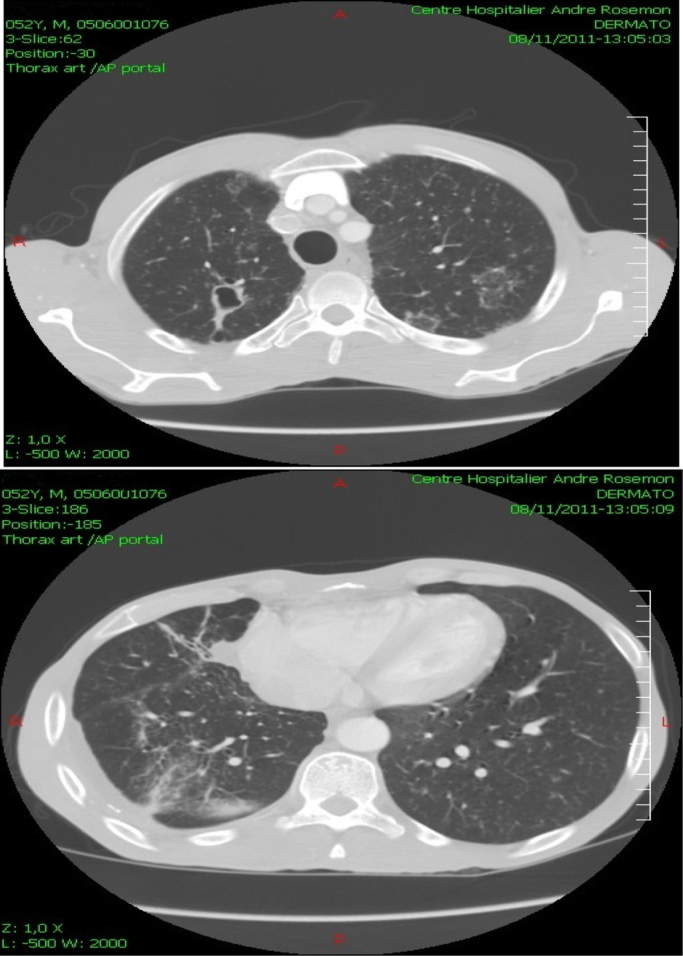
Radiologically, the chest Xray showed an interstitial syndrome suggestive of histoplasmosis with sequellae of the past tuberculosis (Fig. 2). Computed tomography showed an ulcerated lesion of the tongue and the oropharyngeal region (Fig. 3), right jugulo-carotidian lymphadenopathies, an aspect of pulmonary miliary, fibrotic sequelae associated with a localized bronchial dilatation of the right lung, and finally disseminated centrolobular emphysema (Fig. 4).
Fig. 2.
Chest X-Ray upon hospital admission.
Fig. 3.
Computed tomography of the pharyngeal region upon hospital admission (sagittal section).
Fig. 4.
Computed tomography of the thoracic region upon hospital admission (horizontal sections).
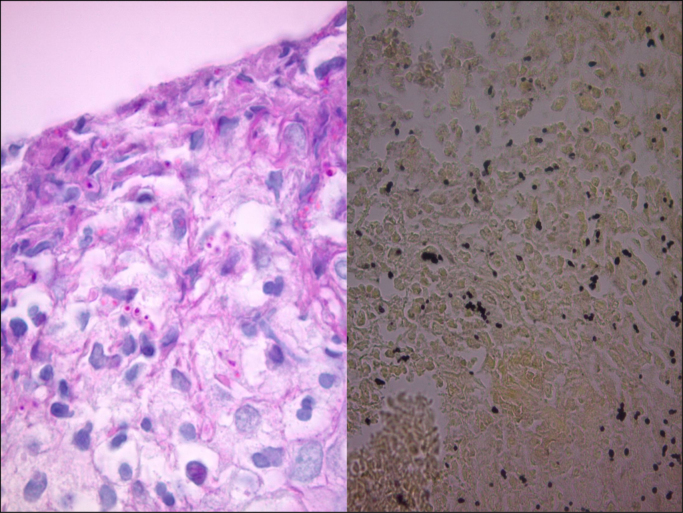
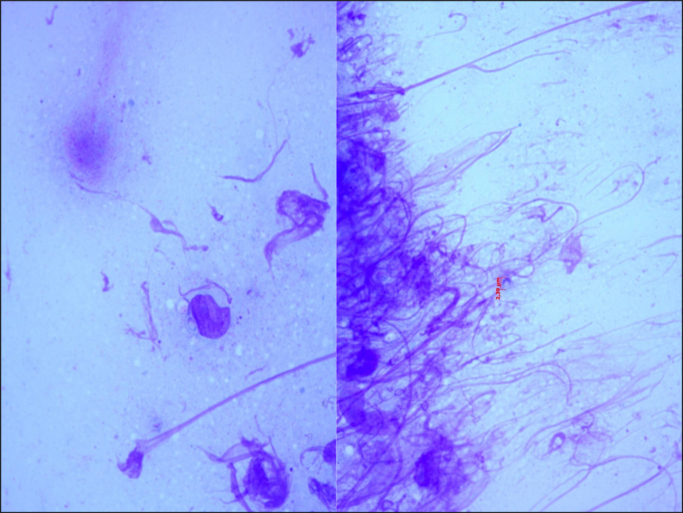
Multiple biopsies of the base of the tongue and of the amygdala lodges were performed. Pathological examination showed polymorphous granulomatous inflammation rich with histiocyte nests and lymphocytes, as well as the presence of intra-histiocytic yeasts of H. capsulatum (Fig. 5). The Acid-Fast Bacilli (AFB) smears were negative. Cytological examination of tissue smears and fungal culture at 25 °C confirmed the presence of H. capsulatum (Fig. 6).
Fig. 5.
LEFT: Tongue biopsy with Histoplasma capsulatum yeasts colored in fuchsia (Periodic-Acid-Schiff, ×40), RIGHT: Tongue biopsy with Histoplasma capsulatum yeasts colored in black (Gommori-Grocott, silver staining, ×20).
Fig. 6.
Tissue smears with cells of the base of the tongue, showing intra cellular yeasts of Histoplasma Capsulatum (May-Grumwald-Giemsa, ×100).
Bronchial fibroscopy with bronchoalveolar lavage was also performed showing white secretions on the right side, and areas of anthracosis. Samples microbiological analyses were all negative, notably regarding Koch Bacilli (smear and culture) and histoplasmosis (direct examination and culture).
Histoplasmosis immunodiffusion serology and RT-PCR, available on site, were not performed. Antigen detection for histoplasmosis was not available and not realized.
The final diagnosis was disseminated histoplasmosis, associated with oral candidiasis, in an HIV patient with severe immunosuppression. The patient was treated with itraconazole at a dose of 100 mg, 3 tablets morning and evening for 3 consecutive days, followed by 2 tablets morning and evening daily. The initial evolution was favorable with a marked reduction of the lesions after one week of treatment (Fig. 7). Complete healing with ad integrum restitution of the oral cavity was obtained after 6 months of itraconazole 400 mg daily in association with antiretroviral therapy.
Fig. 7.
Oral examination showing a marked decreased of the lesion after one week of antifungal therapy with itraconazole.
3. Discussion
Oral presentations are commonly described in the literature among immunocompetent or immunosuppressed individuals, with highly variable frequencies (<10% to 60%) [15]. Nevertheless, they are not frequent in areas where physician awareness, good access to mycology laboratories and antifungal therapy converge to an early diagnosis and treatment [15].
HIV-associated histoplasmosis is the first AIDS-defining condition in French Guiana, where HIV prevalence exceeds 1% since the 1990's [18]. In the past ten years we observed a sharp decline in mortality together with a stable number of new cases [18]. As for mortality we observed a sharp decline in the incidence trends for muco-cutaneous presentations of HIV-associated histoplasmosis [15]. It used to represent a large proportion of diagnosed cases since it was first described by dermatologists looking for leishmaniasis [15]. To date, cutaneous presentations are scarce but oral mucosal presentations although rare have remained stable over time (unpublished data).
It is commonly described that oral involvement occurs at the late stage of histoplasmosis and HIV infection [15]. Regarding HIV infection, in almost all published series, the CD4 count at the time of oral histoplasmosis diagnosis was <70/mm3 [15]. Regarding histoplasmosis infection, oral involvement is often associated with involvement of another organ in the context of a progressive disseminated form of the disease [15]. However, authors have considered potential primary oral lesions, which may heal spontaneously [13]. Although the presence of H. capsulatum couldn’t be documented at the pulmonary level in our patient, the literature describes a frequent association between oral and pulmonary forms of histoplasmosis [13], [15]. Hence, in HIV-infected patients, oral involvement seems to represent the late expression of the progressive spread of H. capsulatum infection through the reticuloendothelial system.
Oral mucosal manifestations are mainly represented by erosive or plaque-like lesions, ulcerations or ulcero-vegetative or nodular-ulcerative lesions. Localizations are mainly the lips, palate, gingiva, tongue and pharynx [13], [15], [16]. Any chronic oropharyngeal lesions, solitary or not, requires performing biopsies so that pathologists can rule out malignancies and microbiologists can rule out infectious diseases. If malignancies are the most common etiologies, notably squamous cell carcinoma, infectious diseases such as tuberculosis, syphilis, cytomegalovirus, paracoccidioidiomycosis, histoplasmosis or talaromycosis must be evoked by physicians facing an oral mucosal lesion in HIV-infected individuals [13], [15], [16].
Certain diagnoses rely on direct examination and fungal culture together with the required confirmatory culture (i.e. conversion of the mold cultured into the yeast phase of H. capsulatum) [1]. In the absence of fungal culture, there is a consensus that diagnostic may rely only on histology performed with specific stains for fungal elements (Periodic-acid Schiff and Gomori-Grocott methenamine silver) [1], [5]. Still confusion with C. glabrata, T. marneffei, Leishmania, Trypanosoma and other staining artifacts may persist if the clinical picture and the past medical history are not joined to the request [18]. In our report, although no confirmatory subculture was performed, we identified the mold phase of H. capsulatum from clinical samples and we feel confident with the diagnostic of histoplasmosis because of the local epidemiology and the complete healing after several months of itraconazole.
Oral presentations of HIV-associated histoplasmosis are not associated with a poor prognosis since mortality at one month was not shown to be higher than other presentations of the disease [15]. Hence, greater mortality at six months or more may be linked to the patients’ immune deficiency. Indeed, the vital prognosis of these patients seems to be linked to the level of immunosuppression, and not to the late stage of H. capsulatum infection. Despite oral presentations occurring in patients at the very late HIV stages with low CD4 counts, introducing oral itraconazole seems to be a good strategy in the absence of organ failure or concomitant opportunistic infections. But, physicians must pay attention to drug-drug interactions when introducing antiretroviral therapy (notably efavirenz) [1].
This report highlights the importance of including infectious diseases, notably fungal diseases such as histoplasmosis as a potential differential diagnosis when facing an oral mucosal lesion resembling a tumor. The capacity of physicians to suspect the diagnosis, to prescribe specific fungal investigations, and to start promptly antifungal therapy are key elements in patient care. In addition, physicians should not differ initiation of antiretroviral therapy since the patient prognosis is at risk considering the advanced stage of HIV infection [1].
Acknowledgements
We acknowledge an Investissement d'Avenir grant of the Agence Nationale de la Recherche (CEBA ANR-10-LABX-25-01). AA and TC draft the manuscript.
TC, JD, AR, CA and PC managed the patient, the diagnosis and revise the manuscript.
Acknowledgments
Conflict of interest
There are none.
Ethical form
Authors declared that they have obtained a written and signed consent from the patient to use his medical files in the context of biomedical research. Plus, a specific oral consent to take pictures and publish the case report was obtained from the patient.
References
- 1.Adenis A.A., Aznar C., Couppie P. Histoplasmosis in HIV-infected patients: a review of new developments and remaining Gaps. Curr. Trop. Med. Rep. 2014;1:119–128. doi: 10.1007/s40475-014-0017-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kauffman C.A. Histoplasmosis: a clinical and laboratory update. Clin. Microbiol Rev. 2007;20(1):115–132. doi: 10.1128/CMR.00027-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hanf M., Adenis A., Couppie P., Carme B., Nacher M. HIV-associated histoplasmosis in French Guiana: recent infection or reactivation? AIDS. 2010;24(11):1777–1778. doi: 10.1097/QAD.0b013e32833999c9. [DOI] [PubMed] [Google Scholar]
- 4.Wheat J. Endemic mycoses in AIDS: a clinical review. Clin. Microbiol. Rev. 1995;8(1):146–159. doi: 10.1128/cmr.8.1.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Pauw B., Walsh T.J., Donnelly J.P., Stevens D.A., Edwards J.E., Calandra T. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin. Infect. Dis. 2008;46(12):1813–1821. doi: 10.1086/588660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Falci D.R., Hoffmann E.R., Paskulin D.D., Pasqualotto A.C. Progressive disseminated histoplasmosis: a systematic review on the performance of non-culture-based diagnostic tests. Braz. J. Infect. Dis. 2016 doi: 10.1016/j.bjid.2016.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Couppie P., Aznar C., Carme B., Nacher M. American histoplasmosis in developing countries with a special focus on patients with HIV: diagnosis, treatment, and prognosis. Curr. Opin. Infect. Dis. 2006;19(5):443–449. doi: 10.1097/01.qco.0000244049.15888.b9. [DOI] [PubMed] [Google Scholar]
- 8.Wheat L.J., Freifeld A.G., Kleiman M.B., Baddley J.W., McKinsey D.S., Loyd J.E. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2007;45(7):807–825. doi: 10.1086/521259. [DOI] [PubMed] [Google Scholar]
- 9.Johnson P.C., Wheat L.J., Cloud G.A., Goldman M., Lancaster D., Bamberger D.M. Safety and efficacy of liposomal amphotericin B compared with conventional amphotericin B for induction therapy of histoplasmosis in patients with AIDS. Ann. Int. Med. 2002;137(2):105–109. doi: 10.7326/0003-4819-137-2-200207160-00008. [DOI] [PubMed] [Google Scholar]
- 10.Nacher M., Adenis A., Mc Donald S., Do Socorro Mendonca Gomes M., Singh S., Lopes Lima I. Disseminated histoplasmosis in HIV-infected patients in South America: a neglected killer continues on its rampage. PLoS Negl. Trop. Dis. 2013;7(11):e2319. doi: 10.1371/journal.pntd.0002319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.neglected histoplasmosis in Latin America G Disseminated histoplasmosis in Central and South America, the invisible elephant: the lethal blind spot of international health organizations. AIDS. 2016;30(2):167–170. doi: 10.1097/QAD.0000000000000961. [DOI] [PubMed] [Google Scholar]
- 12.Adenis A., Nacher M., Hanf M., Basurko C., Dufour J., Huber F. Tuberculosis and Histoplasmosis among Human Immunodeficiency Virus-Infected Patients: a Comparative Study. Am. J. Trop. Med. Hyg. 2014 doi: 10.4269/ajtmh.13-0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klein I.P., Martins M.A.T., Martins M.D., Carrard V.C. Diagnosis of HIV infection on the basis of histoplasmosis-related oral ulceration. Spec. Care Dent. 2016;36(2):99–103. doi: 10.1111/scd.12147. [DOI] [PubMed] [Google Scholar]
- 14.Hernández S.L., López de Blanc S.A., Sambuelli R.H., Roland H., Cornelli C., Lattanzi V. Oral histoplasmosis associated with HIV infection: a comparative study. J. Oral. Pathol. Med. 2004;33(8):445–450. doi: 10.1111/j.1600-0714.2004.00183.x. [DOI] [PubMed] [Google Scholar]
- 15.Couppie P., Clyti E., Nacher M., Aznar C., Sainte-Marie D., Carme B. Acquired immunodeficiency syndrome-related oral and/or cutaneous histoplasmosis: a descriptive and comparative study of 21 cases in French Guiana. Int. J. Dermatol. 2002;41(9):571–576. doi: 10.1046/j.1365-4362.2002.01590.x. [DOI] [PubMed] [Google Scholar]
- 16.Antonello V.S., Zaltron V.F., Vial M. Oliveira FMd, Severo LC. Oropharyngeal histoplasmosis: report of eleven cases and review of the literature. Rev. da Soc. Bras. De. Med. Trop. 2011;44:26–29. doi: 10.1590/s0037-86822011000100007. [DOI] [PubMed] [Google Scholar]
- 17.Weed L.A., Parkhill E.M. The diagnosis of histoplasmosis in ulcerative disease of the mouth and pharynx. Am. J. Clin. Pathol. 1948;18(2):130. doi: 10.1093/ajcp/18.2.130. [DOI] [PubMed] [Google Scholar]
- 18.Adenis A., Nacher M., Hanf M., Vantilcke V., Boukhari R., Blachet D. HIV-associated histoplasmosis early mortality and incidence trends: from neglect to priority. PLoS Negl. Trop. Dis. 2014;8(8):e3100. doi: 10.1371/journal.pntd.0003100. [DOI] [PMC free article] [PubMed] [Google Scholar]