Abstract
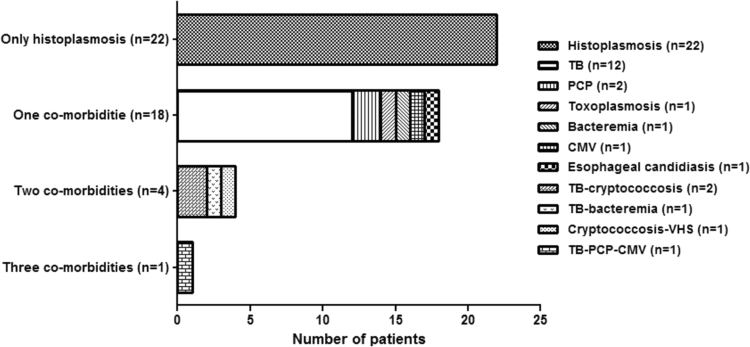
A total of 23/45 (51%) patients with AIDS and histoplasmosis from Medellín, Colombia had other infections. Tuberculosis was the most common (n = 16/23, 70%). Pneumocystosis and cryptococcosis were found in three patients each (13%), bacterial infection and cytomegalovirus occurred each in two patients (9%) while toxoplasmosis, herpes virus and esophageal candidiasis were recorded in one patient each (4%). Of all co-infected patients, 18/23 (78%) had one, four (17%) had two and one (4%) had three additional opportunistic infections.
Keywords: AIDS, Histoplasmosis, Histoplasma, Co-infection
1. Introduction
Histoplasmosis is a common infection in the Americas, although it is diagnosed in certain countries of Asia (China, India, Malaysia, Indonesia, Singapore, Thailand, Vietnam and Japan) and Africa (Democratic Republic of Congo, Congo, Liberia, Ivory Coast, Gambia, Uganda, Central African Republic, Guinea Bissau and Senegal) [1], [2], [3]. The clinical presentation depends partly on the concentration of infectious particles in the inoculum, as well as on the condition of the host's immune system at the time of infection [4], [5]. Highly susceptible populations are recognized and include individuals at the extremes of life, persons undergoing immunosuppressive therapy, solid organ recipients and, especially, patients infected with the human immunodeficiency virus (HIV) who have CD4 T cells counts below 150 per µL [4].
In persons living with HIV/AIDS (PLWHA), the mycosis often produces a severe clinical form of disease called progressive disseminated histoplasmosis (PDH), which has a high mortality if treatment is not initiated promptly [4], [5]. As has been previously reported, PDH symptoms are nonspecific, and among PLWHA, symptoms may be similar to those observed in other infectious diseases, thus complicating diagnosis and treatment [4], [6], [7], [8]. In Colombia and other endemic countries in the Americas, where access to antiretroviral therapy (ART) can be limited, histoplasmosis is a cause of high morbidity and mortality (up to 30%) in PLWHA [9].
2. Cases
An observational, cross-sectional study of patients with histoplasmosis was performed between May 2008 and August 2011 in a cohort of PLWHA from La Maria Hospital in Medellín, Colombia [8]. The diagnosis of histoplasmosis was made based on the guidelines of the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the Mycoses Study Group (EORTC/MSG) [10]. A diagnosis was considered proven if H. capsulatum was isolated from any of the following samples: blood, tissue, sterile fluids or respiratory specimens or by a positive histopathological analysis, with presence of intracellular yeasts, identified by Wright staining. A diagnosis was considered probable if H. capsulatum could not be isolated, but there was evidence of reactive serology such as presence of either H or M precipitin band or both bands by the immunodiffusion (ID) test and a titer of 1:32 or higher with histoplasmin antigen by the complement fixation (CF) test, or a positive antigenuria test [10]. Co-infections present in these patients were defined based on clinical, radiological and microbiological criteria.
A standardized data collection form was developed in Microsoft Access consisting of variables for clinical findings, laboratory testing, treatment and outcome. For statistical analysis, absolute and relative frequencies were calculated and tested for normality. To identify statistical association, we used the Chi2 test, Student t-test or Mann-Whitney U test. In order to identify differences among histoplasmosis patients with and without co-infections, statistical associations were defined by a p value less than 0.05. All analyses were performed using the software EPIDAT 3.1 and STATA 8.0.
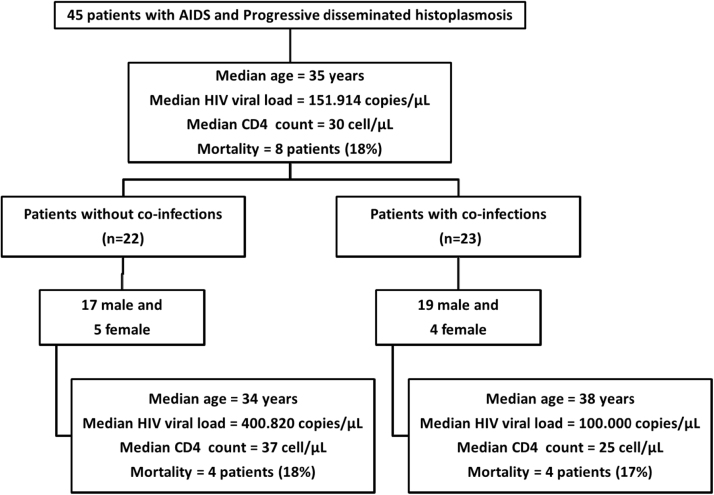
A total of 45 patients with AIDS and PDH were identified, 30 (67%) were classified as proven cases and 15 (33%) as probable cases. At the time of enrollment in the study, patients with histoplasmosis had the following clinical characteristics: a median CD4 cell concentration of 30 per µL (Range [R] = 3–540 cells per µL); and a median viral load of 151,914 copies per µL (R = 40-6.678,540 copies per µL) (Fig. 1); median body temperature was 37.4 °C (R = 36–39 °C); median body mass index was 18.04 (R = 12.3–24.8). A total of 39 (87%) patients with histoplasmosis had weight loss at enrollment and 18 (40%) had a Karnofsky score under 30. Gastrointestinal manifestations were present in 38 (84%) patients. Patients also had pulmonary manifestations (75%), neurological abnormalities (64%), lymphadenopathies (58%), and skin (49%) and oral mucosal lesions (44%). A total of 8 (18%) patients died.
Fig. 1.
Study flow chart of analyzed subjects. General characteristics of 45 patients with AIDS and progressive disseminated histoplasmosis (PDH). In 22 (49%) patients no other opportunistic infection was reported at time of diagnosis of PDH; presence of co-infections were reported in the remaining 23 (51%) patients with AIDS and PDH.
Co-infections were diagnosed in 23 of the 45 patients (51%) There were 19 males (83%) and 4 females (17%) with a median age of 38 years (R = 21–55 years). The median CD4 T cell count was 25 cells per µL (R = 3–330 cells per µL) and the HIV viral load was 100,000 copies per µL (R = 266-6.678,540 copies per µL). No statistically significant differences among patients with nd without co-infections were found (Fig. 1). There was also no statistically significant differences in mortality among patients with and without co-infections (Fig. 1).
Of the 23 patients presenting with histoplasmosis and other infections, 18 (78%) had one additional opportunistic infection, 4 patients (17%) had two, and one patient (4%) had 3 additional infections (Fig. 2). Tuberculosis (TB) was found in 16 of 23 patients (70%) and was the main co-infection followed by pneumocystosis and cryptococcosis diagnosed in 3 of 23 patients each (13%). Bacterial infections (Salmonella) and Cytomegalovirus (CMV) occurred in 2 patients each (9%), while 1 patient exhibited concomitant toxoplasmosis, herpes virus and esophageal candidiasis. It is important to note that all 4 patients presenting with either bacterial disease or CMV infection died.
Fig. 2.
Distribution of co-infections observed in 45 patients with AIDS and progressive disseminated histoplasmosis (PDH). In 22 patients no other opportunistic infection was reported at time of diagnosis of PDH (49%). In the remaining 23 patients with co-infections (51%), 18 (78%) had 1 additional opportunistic disease, 4 patients (17%) had 2, and 1 patient (4%) had 3 different opportunistic diseases.
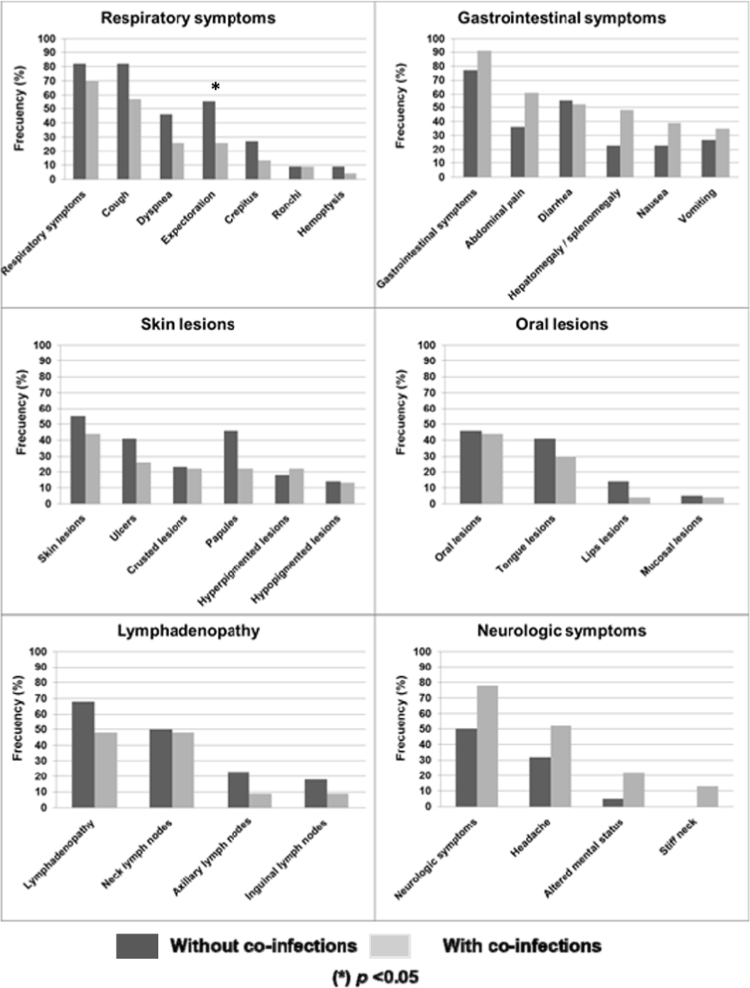
When we compared clinical manifestations grouped by systems among patients with and without co-infections, we observed differences in the presence of lymphadenopathy and neurological symptoms. All other variables analyzed did not show differences between the two groups (Fig. 3).
Fig. 3.
Clinical findings recorded in 45 AIDS patients with histoplasmosis, with or without co-infection.
3. Discussion
Among this cohort of PLWHA who were identified as having progressive disseminated histoplasmosis, over half had an additional opportunistic infections [11]. This is higher than those reported in Panama (25%), French Guiana (37–42%), Argentina (42%) and Brazil (43%). However, tuberculosis was the most frequently reported opportunistic infection in all these countries [12], [13], [14], [16], [17]
It is clear from these results that in this patient population, there is a serious challenge in differentiating clinical signs and symptoms which might help determine the presence of additional co-infections. This highlights the importance of looking for co-infections in such patients, and of studying the organs most frequently clinically involved. It is, moreover, important to emphasize that signs and symptoms must be correlated with laboratory diagnostics. Proper diagnostic procedures should be done whenever there is any suspicion of histoplasmosis or other infections. Rapid diagnosis will reduce the time to treatment and reduce mortality [8], [16], [17], [18], [19]
Bacteremia and CMV disease were frequent in patients who died, although only 4 patients presented these co-infections, and had TB. In these 4 patients it is difficult to be sure that the direct cause of death was either the bacteremia or CMV disease, because these patients were severely ill [15], [17]
As a final note, these persons living with HIV/AIDS had important abnormalities in their immune status which, together with the non-specificity of clinical signs and symptoms, indicate that the one should be concerned and suspect other opportunistic infections that may be present simultaneously. Appropriate laboratory tests need to be used in order to promptly confirm correct diagnoses and provide appropriate therapies.
Conflict of interest
None. The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the CDC.
Ethical form
Please note that this journal requires full disclosure of all sources of funding and potential conflicts of interest. The journal also requires a declaration that the author(s) have obtained written and signed consent to publish the case report from the patient or legal guardian(s). The statements on funding, conflict of interest and consent need to be submitted via our Ethical Form that can be downloaded from the submission site www.ees.elsevier.com/mmcr. Please note that your manuscript will not be considered for publication until the signed Ethical Form has been received.
Acknowledgements
The authors express their appreciation to the medical doctors of the HIV and pneumology services in La Maria Hospital, Carlos A. Agudelo, Carlos A. Restrepo, Diego A. Molina, Carolina Muñoz, Lucía Correa, Fernando Bedoya, Alejandra Medina, Federico Rodriguez, Luisa Orozco and Juliana Marin. Our thanks also go to the laboratory diagnosis staff of the Medical and Experimental Mycology group (CIB), Catalina de Bedout, Alejandra Zuluaga, Karen Arango, Yorlady Valencia, Luisa Lopez and Angela Tabares.
This work was supported in part by Colciencias, Bogotá, Colombia via the young investigators and innovators program Virginia Gutierrez de Pineda, the Corporación para Investigaciones Biológicas (CIB), Medellín, Colombia, the Fondo de Investigaciones de la Universidad del Rosario (FIUR), Bogota, Colombia and the Mycotic Diseases Branch at the Centers for Disease Control and Prevention (CDC), Atlanta, USA.
References
- 1.Colombo A.L., Tobon A., Restrepo A., Queiroz-Telles F., Nucci M. Epidemiology of endemic systemic fungal infections in Latin America. Med Mycol. 2011;49:785–798. doi: 10.3109/13693786.2011.577821. [DOI] [PubMed] [Google Scholar]
- 2.Knox K.S., Hage C.A. Histoplasmosis. Proc. Am. Thorac. Soc. 2010;7:169–172. doi: 10.1513/pats.200907-069AL. [DOI] [PubMed] [Google Scholar]
- 3.Bahr N.C., Antinori S., Wheat L.J., Sarosi G.A. Histoplasmosis infections worldwide: thinking outside of the Ohio River valley. Curr. Trop. Med Rep. 2015;2:70–80. doi: 10.1007/s40475-015-0044-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deepe G.S. Histoplasma capsulatum. In: Bennett J.E., Dolin R., Blaser M.J., editors. Principles and Practice of Infectious Diseases. Elsevier; Philadelphia, USA: 2015. pp. 2949–2962. [Google Scholar]
- 5.Goodwin R.A., Loyd J.E., Des Prez R.M. Histoplasmosis in normal hosts. Med. (Baltim.). 1981;60:231–266. doi: 10.1097/00005792-198107000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Kauffman C.A. Histoplasmosis: a clinical and laboratory update. Clin. Microbiol. Rev. 2007;20:115–132. doi: 10.1128/CMR.00027-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kauffman C.A. Diagnosis of histoplasmosis in immunosuppressed patients. Curr. Opin. Infect. Dis. 2008;21:421–425. doi: 10.1097/QCO.0b013e328306eb8d. [DOI] [PubMed] [Google Scholar]
- 8.Caceres D.H., Tobón A.M., Cleveland A.A., Scheel C.M., Berbesi D.Y., Ochoa J. Clinical and laboratory profile of persons living with human immunodeficiency virus/acquired immune deficiency syndrome and histoplasmosis from a Colombian hospital. Am. J. Trop. Med Hyg. 2016;95:918–924. doi: 10.4269/ajtmh.15-0837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cáceres D.H., Gómez B.L., Restrepo A., Tobón A.M. Histoplasmosis and AIDS: clinical and laboratory risk factors associated with the disease's prognosis. Infectio. 2012;16:44–50. [Google Scholar]
- 10.De Pauw B., Walsh T.J., Donnelly J.P., Stevens D.A., Edwards J.E., Calandra T. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin. Infect. Dis. 2008;46:1813–1821. doi: 10.1086/588660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sterling T.R., Chaisson R.E. General clinical manifestations of human immunodeficiency virius infection (including the acute retroviral syndrome and oral cutaneous, rinal, ocular, metabolic and cardiac diseases) In: Bennett J.E., Dolin R., Blaser M.J., editors. Principles and practice of infectious diseases. Elsevier; Philadelphia, USA: 2015. pp. 1541–1557. [Google Scholar]
- 12.Gutierrez M.E., Canton A., Sosa N., Puga E., Talavera L. Disseminated histoplasmosis in patients with AIDS in Panama: a review of 104 cases. Clin. Infect. Dis. 2005;40:1199–1202. doi: 10.1086/428842. [DOI] [PubMed] [Google Scholar]
- 13.Mora D.J., dos Santos C.T., Silva-Vergara M.L. Disseminated histoplasmosis in acquired immunodeficiency syndrome patients in Uberaba, MG, Brazil. Mycoses. 2008;51:136–140. doi: 10.1111/j.1439-0507.2007.01459.x. [DOI] [PubMed] [Google Scholar]
- 14.Corti M.E., Negroni R., Esquivel P., Villafañe M.F. Histoplasmosis diseminada en pacientes con SIDA: análisis epidemiológico, clínico, microbiológico e inmunológico de 26 pacientes. Enf. Emerg. 2004;6:8–15. [Google Scholar]
- 15.Agudelo C.A., Restrepo C.A., Molina D.A., Tobón A.M., Kauffman C.A., Murillo C. Tuberculosis and histoplasmosis co-infection in AIDS patients. Am. J. Trop. Med. Hyg. 2012;6:1094–1098. doi: 10.4269/ajtmh.2012.12-0292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huber F., Nacher M., Aznar C., Pierre-Demar M., El Guedj M., Vaz T. AIDS-related Histoplasma capsulatum var. capsulatum infection: 25 years experience of French Guiana. AIDS. 2008;22:1047–1053. doi: 10.1097/QAD.0b013e3282ffde67. [DOI] [PubMed] [Google Scholar]
- 17.Adenis A., Nacher M., Hanf M., Basurko C., Dufour J., Huber F. Tuberculosis and histoplasmosis among human immunodeficiency virus-infected patients: a comparative study. Am. J. Trop. Med. Hyg. 2014;90:216–223. doi: 10.4269/ajtmh.13-0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nacher M., Adenis A., Mc Donald S., Do Socorro Mendonca Gomes M., Singh S., Lopes Lima I. Disseminated histoplasmosis in HIV-infected patients in South America: a neglected killer continues on its rampage. PLoS Negl. Trop. Dis. 2013;7:e2319. doi: 10.1371/journal.pntd.0002319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scheel C.M., Gómez B.L. Diagnostic methods for histoplasmosis: focus on endemic countries with variable infrastructure levels. Curr. Trop. Med. Rep. 2014;1:129–137. doi: 10.1007/s40475-014-0020-0. [DOI] [PMC free article] [PubMed] [Google Scholar]