Abstract
Psychosis is a heterogeneous psychiatric condition for which a multitude of risk and protective factors have been suggested. This umbrella review aimed to classify the strength of evidence for the associations between each factor and psychotic disorders whilst controlling for several biases. The Web of Knowledge database was searched to identify systematic reviews and meta‐analyses of observational studies which examined associations between socio‐demographic, parental, perinatal, later factors or antecedents and psychotic disorders, and which included a comparison group of healthy controls, published from 1965 to January 31, 2017. The literature search and data extraction followed PRISMA and MOOSE guidelines. The association between each factor and ICD or DSM diagnoses of non‐organic psychotic disorders was graded into convincing, highly suggestive, suggestive, weak, or non‐significant according to a standardized classification based on: number of psychotic cases, random‐effects p value, largest study 95% confidence interval, heterogeneity between studies, 95% prediction interval, small study effect, and excess significance bias. In order to assess evidence for temporality of association, we also conducted sensitivity analyses restricted to data from prospective studies. Fifty‐five meta‐analyses or systematic reviews were included in the umbrella review, corresponding to 683 individual studies and 170 putative risk or protective factors for psychotic disorders. Only the ultra‐high‐risk state for psychosis (odds ratio, OR=9.32, 95% CI: 4.91‐17.72) and Black‐Caribbean ethnicity in England (OR=4.87, 95% CI: 3.96‐6.00) showed convincing evidence of association. Six factors were highly suggestive (ethnic minority in low ethnic density area, second generation immigrants, trait anhedonia, premorbid IQ, minor physical anomalies, and olfactory identification ability), and nine were suggestive (urbanicity, ethnic minority in high ethnic density area, first generation immigrants, North‐African immigrants in Europe, winter/spring season of birth in Northern hemisphere, childhood social withdrawal, childhood trauma, Toxoplasma gondii IgG, and non‐right handedness). When only prospective studies were considered, the evidence was convincing for ultra‐high‐risk state and suggestive for urbanicity only. In summary, this umbrella review found several factors to be associated with psychotic disorders with different levels of evidence. These risk or protective factors represent a starting point for further etiopathological research and for the improvement of the prediction of psychosis.
Keywords: Schizophrenia, psychosis, risk, environment, socio‐demographic factors, parental factors, perinatal factors, antecedents, ultra‐high‐risk state for psychosis, Black‐Caribbean ethnicity, urbanicity
Psychotic disorders like schizophrenia are among the world's leading causes of disability1. They have a mean incidence of 31.7 per 100,000 person‐years in England2 and a 12‐month prevalence of 1.1% among the US population3. Despite many decades of research, the etiology of these disorders remains undetermined4.
The model that has received most empirical support suggests that the etiology of psychotic disorders, schizophrenia for example, involves direct genetic and environmental risk factors along with their interaction5, 6. In reality, some of the risk factors that have been associated with psychotic disorders – such as family history of mental illness – include both a genetic and an environmental component, and hence a distinction between genetic and environmental risk factors may be spurious.
With this in mind, in this study we adopted a pragmatic approach and used the term “non‐purely genetic factors” to define socio‐demographic, parental, perinatal, later factors and antecedents7, 8, 9 that may increase (risk factors) or decrease (protective factors) the likelihood of developing psychotic disorders. The clinical importance of investigating these factors is threefold. First, they could potentially be used to advance the prediction of psychosis in populations at risk of developing the disorder10, 11. Second, some, albeit not all, of these factors may be potentially modifiable by preventive interventions4. Third, they could inform outreach campaigns targeting the general public to raise awareness of risk factors for psychosis and to promote mental health.
Numerous studies investigating the association between potential risk or protective factors and psychotic disorders have been published. The body of literature in this area is substantial, presumably due to the severe societal burden that is associated with these disorders and thus the urgent need to understand their causes. However, to date, for all of those factors, there is no conclusive evidence with respect to both the association itself and its direction (i.e., risk or protective), because published findings have often been conflicting.
Furthermore, some of these results have been found to be affected by several types of biases12, 13. These are particularly relevant to this area of research because experimental support for etiology, in the sense of randomized allocation to the above‐mentioned exposures13, is naturally lacking, and most evidence is based on observational studies. Finally, previously published literature did not generate clear hierarchies of evidence across those factors, rendering the overall interpretation of the findings particularly complex. In fact, until recently there were no stringent evaluation criteria by which to hierarchically stratify the robustness of the evidence whilst at the same time controlling for the presence of biases.
Umbrella reviews can overcome these problems by assessing the level of the evidence provided by systematic reviews and meta‐analyses14 for each risk or protective factor, through strict criteria that probe a standard list of potential biases. These criteria have been extensively validated in various areas of medicine, such as neurology, oncology, nutrition medicine, internal medicine, psychiatry, paediatrics, dermatology and neurosurgery15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33. In the current study, we applied the umbrella review approach to the published evidence on risk or protective factors for psychotic disorders.
Our umbrella review advances knowledge in the field of psychosis etiology, providing the first state‐of‐the‐art classification based on the robustness of associations between putative risk or protective factors and psychotic disorders, controlling at the same time for several biases. The use of classification criteria for levels of evidence can help overcome some of the ambiguity experienced by clinicians and researchers when confronted with conflicting meta‐analyses34 on complex topics and trying to base their decisions on them. Furthermore, our analysis will hopefully promote further etiological clinical research in psychosis, support the refinement of risk prediction in at‐risk populations, and inform future preventive strategies.
METHODS
The protocol of the study was registered on PROSPERO 2016: CRD42016054101.
Search strategy and selection criteria
An umbrella review (i.e., a systematic collection and assessment of multiple systematic reviews and meta‐analyses published on a specific research topic)35 was conducted. We searched the Web of Knowledge database (incorporating Web of Science and MEDLINE) to identify systematic reviews or meta‐analyses of observational studies that examined the association between a number of factors and psychotic disorders, published from 1965 to January 31, 2017. The search strategy used the keywords (“systematic review” OR “meta‐analysis”) and (“psychosis” OR “schizophrenia”). We then conducted a manual search of the reference lists of the retrieved articles.
Articles were initially screened on the basis of title and abstract reading. The full texts of potentially eligible articles were then independently scrutinized by two investigators (PFP, VRC), with no language restrictions. We selected systematic reviews or meta‐analyses of individual observational studies (case‐control, cohort, cross‐sectional and ecological studies) that examined the association between socio‐demographic, parental, perinatal, later factors or antecedents and any non‐organic psychotic disorder as defined by any edition of the ICD or the DSM, including a comparison group of non‐psychotic healthy controls, and reporting enough data to perform the analyses.
When data were incomplete, the corresponding author was contacted and invited to send additional information. When two articles presented overlapping datasets on the same factor, only the article with the largest dataset was retained for the main analysis. However, if the overlap was minimal, the articles were used conjointly, counting overlapping individual studies once only36, 37, 38, 39, 40, 41, 42, 43. Moreover, we also excluded articles that did not report quantitative data, and articles with an outcome other than the onset of an established psychotic disorder, such as those related to relapse, remission or treatment response.
Articles that investigated pure genetic markers of psychotic disorders were excluded, because they have been examined extensively elsewhere44, 45. Articles that investigated the association between biomarkers and psychotic disorders were not included, because this would have required specific methodological approaches and separate analyses. However, some putative biomarkers have been defined as antecedents (e.g., premorbid IQ38, 39, minor physical anomalies46, non‐right handedness47, dermatoglyphic abnormalities48 and neurological soft signs49) or perinatal factors (vitamin D50), and the relevant articles were therefore included.
The same inclusion/exclusion criteria were checked for each individual study comprised in every eligible meta‐analysis or systematic review. The Preferred Reporting Items for Systematic Reviews and Meta‐analyses (PRISMA) recommendations51 and the Meta‐analysis of Observational Studies in Epidemiology (MOOSE) guidelines52 were followed.
Data extraction
Data extraction was performed independently by at least two investigators. Any existing discrepancies were resolved in consensus meetings with two of the authors (VRC, PFP). Factors were extracted as defined in the corresponding meta‐analysis or systematic review. We did not combine similar factors if they were considered and analyzed separately by meta‐analyses/systematic reviews53. Similarly, we did not split factors into subgroups if they were considered as a whole54. When a meta‐analysis or systematic review reported both pooled results and results divided according to subgroups, pooled results were preferred, since they had a larger sample size.
Such a conservative approach was adopted to minimize the chance of introducing risk or protective factors that had not been defined by the corresponding articles, and that may have been too heterogeneous to allow meaningful interpretation. This approach also minimized the risk of artificially inflating the sample size and therefore biasing the hierarchical classification of the evidence. The exception was for analyses not based on individual‐level data, for which we specifically created new risk factors55, 56, as detailed in the statistical analysis section.
For descriptive purposes, risk/protective factors for psychotic disorders were clustered as previously suggested: socio‐demographic and parental factors, perinatal factors, later factors (i.e., factors intervening in the post‐perinatal period) and antecedents7, 8, 9. In line with previous definitions7, 8, antecedents were conceptualized as premorbid deviations in functioning and developmental milestones that could indicate an early expression of the disorder or active risk‐modifying mechanisms and processes involved in psychosis onset. Risk factors, instead, would indicate a passive exposure to environmental agents that could play a role in the development of psychosis. One could argue that this distinction remains arbitrary, since the exact timing and mechanisms involved in the etiology of psychotic disorders remain to be elucidated, but this issue is beyond the aim of this review.
Several variables were recorded: the type of factor studied, the first author of the paper, the year of publication, the type of psychotic diagnosis, and the measure of association between the factor and psychotic disorders (preferably unadjusted), with the corresponding 95% confidence interval (CI) and the sample size (where available). If studies contained several types of control groups, data from healthy controls were used. When data were reported only in graphic form, they were digitally measured and extracted using WebPlotDigitizer57. The methodological quality of included studies was assessed using the validated AMSTAR (A Measurement Tool to Assess Systematic Reviews) instrument58, 59, 60.
Statistical analysis
This umbrella review is composed of a number of meta‐analyses of the included articles conducted separately with a series of scripts in R61. The effect size measures of the association between each factor and psychotic disorders were: incidence rate ratio (IRR), odds ratio (OR), risk ratio (RR), and standardized mean difference (Hedges’ g) for continuous measures. Primarily, the effect size measure and its CI were used.
Since authors usually round off the measures, the first step was to “unround” them by estimating a more exact measure and CI, in which the (logarithm of the) lower and upper bounds were symmetrical around the (logarithm of the) measure. Subsequently, the variance was calculated from the standard formula for the CI. If two or more studies shared the non‐exposed sample, the size of this sample was divided equally between these studies. This approach minimized the dependence produced by the sharing of the non‐exposed sample, whilst allowing estimation of heterogeneity across the exposed samples62.
Some factors required special adjustments, such as: a) the transformation of measures other than OR into OR in factors where effect size was reported using different types of measures (to have a single outcome measure), and b) the combination of effect sizes for left and right nostrils in olfaction studies63, conservatively assuming a weak to moderate correlation (r=0.3)64. Ultimately, we used the “metainc” (IRR), “metabin” (RR and OR), or “metacont” (Hedges’ g) functions in the R “meta” package65 to calculate the meta‐analytic effect size and its p value, the CI, and the heterogeneity (summarized with the I2 statistic and the p value associated with the Q value). Resulting statistics were also used to calculate the prediction interval66.
A few specific adjustments were also adopted for age and gender, where IRRs were available for schizophrenia and affective psychosis separately, and stratified by 5 or 10‐year age ranges and gender2, 67. We combined schizophrenia and affective psychoses and then meta‐analyzed the IRR of each 10‐year age range (vs. other ages), and the IRR of males (vs. females, globally and within each 10‐year age range). Since age and gender were considered as basic factors and excluded by previous reviews on psychosis8, 9 and by umbrella reviews on other neuropsychiatric conditions23, 25, 27, these analyses were considered exploratory.
Alternative analyses were also conducted for latitude55 and gross national income per capita (GNI)56, when the prevalence rates were provided in a series of locations. Specifically, the incidence in each location was (logistic) regressed by the latitude or GNI, obtaining the OR of 10° increase in latitude or 10,000 USD increase in GNI. These results were also considered exploratory because they are based on ecological analyses rather than individual‐level data, and were traditionally excluded from previous umbrella reviews of risk factors23, 25, 27.
Complementary analyses included: a) an Egger test to assess small‐study effects that lead to potential reporting or publication bias68; b) a test of excess significance bias69 as described below, and c) an OR equivalent. The test of excess significance bias consisted of a binomial test to compare the observed vs. the expected number of studies yielding statistically significant results. This expected number was calculated as the sum of the statistical power of the studies, which was estimated using the standard t‐test formulas for Hedges’ g, and random simulations for OR, RR and IRR. Specifically, the statistical power of study A was estimated as the proportion of times in which a simulated study using binomial or Poisson random cases was considered “statistically significant”; the simulated studies had the same mean incidence and person‐times or sample sizes as study A (using the full sample sizes in case of sharing a sample), and the same effect size as the largest study in the meta‐analysis.
Small‐study effects and excess significance bias were claimed at one‐sided p values <0.05, as in previous studies27. In order to easily compare meta‐analyses using different outcome measures, OR equivalents were provided for the above measures. Given the low incidence of psychotic disorders, RR was assumed to be equivalent to OR, after checking that the difference between an OR and a RR of the same data was negligible. IRR was assumed to be equivalent to RR, and Hedges’ g was converted to OR using a standard formula70.
IRR, OR and RR greater than 1 or Hedges’ g greater than 0 indicated that the factor was associated with an increased likelihood of psychotic disorders. IRR, OR and RR lower than 1 or Hedges’ g lower than 0 indicated that the factor was associated with a reduced likelihood of psychotic disorders, i.e. it was protective.
The levels of evidence of the associations between putative risk (or protective) factors and psychotic disorders were classified in accordance with previous umbrella reviews23, 25, 27: convincing (class I) when number of cases >1000, p < 10−6, I2 < 50%, 95% prediction interval excluding the null, no small‐study effects, and no excess significance bias; highly suggestive (class II) when number of cases >1000, p < 10−6, largest study with a statistically significant effect, and class I criteria not met; suggestive (class III) when number of cases >1000, p<10−3, and class I‐II criteria not met; weak (class IV) when p < 0.05 and class I‐III criteria not met; non‐significant when p > 0.05.
Finally, a sensitivity analysis was conducted for the factors classified as class I‐III by using only prospective studies (as defined in each meta‐analysis/systematic review or, when this was not provided, as defined by each individual study). Prospective studies allow one to address the temporality of the association, thus dealing with the problem of reverse causation that may affect, for example, case‐control studies23, 25, 27.
RESULTS
Database
Overall, 4,023 records were searched, 302 were screened and 55 articles were eligible2, 36, 37, 38, 39, 40, 41, 42, 43, 46, 47, 48, 49, 50, 53, 54, 55, 56, 63, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103, 104, 105, 106 (see Figure 1). The eligible articles were published between 1995 (when meta‐analyses in this field first became available)107 and 2017. All of the studies utilized a healthy control group except one, investigating the ultra‐high‐risk state98. This latter study used as controls help‐seeking individuals undergoing an ultra‐high‐risk assessment but not meeting the relevant criteria. The mental health status of this control group was not well defined.
Figure 1.
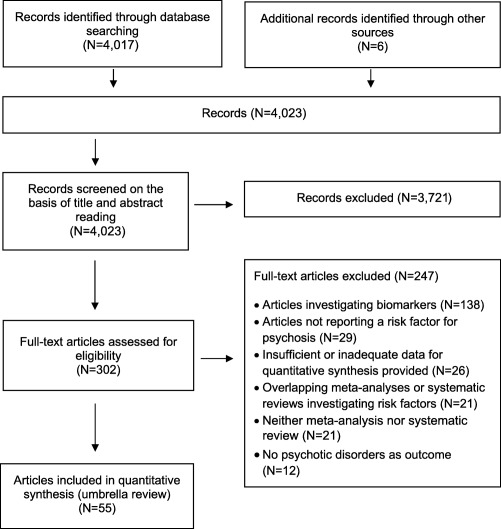
PRISMA flow chart
Overall, the 55 eligible meta‐analyses or systematic reviews, including 683 individual studies, reported on 170 putative risk/protective factors of psychotic disorders (Tables 1, 2, 3, 4). For paternal socio‐economic status73, neighbourhood‐level social deprivation74, pre‐pregnancy and pregnancy maternal obesity82, neonatal levels of vitamin D50, polluting agents (benzene, carbon monoxide, nitrogen dioxide, nitrogen oxides, tetrachloroethylene, traffic)84 and the ultra‐high‐risk state98, the studies did not provide a quantitative synthesis of individual findings, but reported adequate data to allow meta‐analyses.
Table 1.
Characteristics of meta‐analyses and systematic reviews studying the association between psychotic disorders and socio‐demographic and parental factors
| Study | Factors examined | k | Diagnosis | AMSTAR index |
|---|---|---|---|---|
| Bosqui et al71 | Ethnic minority in high ethnic density area; ethnic minority in low ethnic density area | 5, 5 | FEP, SZ, NAP, AP | 9/11 |
| Bourque et al53 | First generation immigrants; second generation immigrants | 12, 9 | SZ, NAP, AP | 10/11 |
| Torrey et al72 | Paternal age >35 years; paternal age >45 years; paternal age >55 years | 8, 7, 4 | SZ, NAP, AP | 3/11 |
| Kinney et al55 | Disadvantaged group; latitude | 2, 29 | SZ | 2/11 |
| Kirkbride et al2 | Age/gender; African ethnicity; Asian ethnicity; mixed ethnicity; other white ethnicity (all examined only in England) | 9, 4, 4, 2, 3 | FEP, SZ, NAP, AP | 11/11 |
| Kwok73 | Low paternal socio‐economic status | 9 | FEP, SZ, NAP | 6/11 |
| O'Donoghue et al74 | Neighbourhood level social deprivation | 3 | FEP | 8/11 |
| Rasic et al75 | Parental severe mental illness | 9 | FEP, SZ, NAP, AP | 6/11 |
| Saha et al56 | Gross national income per capita | 88 | SZ | 9/11 |
| Tortelli et al76 | Black‐Caribbean ethnicity in England | 7 | FEP, SZ, NAP, AP | 10/11 |
| van der Ven et al77 | North African immigrants in Europe | 5 | NAP | 9/11 |
| Vassos et al78 | Urbanicity | 8 | SZ, NAP | 6/11 |
k – number of studies for each factor, FEP – first episode of psychosis, SZ – schizophrenia, NAP – non‐affective psychosis other than schizophrenia, AP – affective psychosis, AMSTAR – A Measurement Tool to Assess Systematic Reviews
Table 2.
Characteristics of meta‐analyses and systematic reviews studying the association between psychotic disorders and perinatal factors
| Study | Factors examined | k | Diagnosis |
AMSTAR index |
|---|---|---|---|---|
| Cai et al40 | Gestational influenza | 6 | SZ, NAP, AP | 10/11 |
| Cannon et al37 | Anaemia in pregnancy; antepartum haemorrhage; asphyxia; baby detained in hospital; birth weight <2000 g; birth weight <2500 g; birth weight <2500 g + prematurity; breech delivery; caesarean section; cephalopelvic disproportion; congenital malformations; diabetes in pregnancy; emergency caesarean section; forceps/vacuum delivery; gestational age <37 weeks; gestational age >42 weeks; induction of labour; low Apgar score; non‐vertex presentation; placental abruption; preeclampsia; Rhesus incompatibility; small birth length; being small for gestational age; small head circumference; smoking in pregnancy; threatened premature delivery; urinary infection in pregnancy; uterine atony | 2, 4, 3, 2, 2, 4, 3, 3, 5, 2, 3, 2, 3, 6, 4, 3, 2, 2, 5, 2, 5, 2, 3, 5, 2, 1, 2, 2, 3 | SZ | 6/11 |
| Christesen et al50 | Neonatal vitamin D (<19.7 vs. 40.5‐50.9 nmol/L); neonatal vitamin D (19.7‐30.9 vs. 40.5‐50.9 nmol/L); neonatal vitamin D (30.9‐40.4 vs. 40.5‐50.9 nmol/L); neonatal vitamin D (>50.9 vs. 40.5‐50.9 nmol/L) | 1, 1, 1, 1 | SZ | 6/11 |
| Davies et al79 | Winter/spring season of birth in Northern hemisphere | 7 | SZ | 6/11 |
| Geddes & Lawrie81 | Obstetric complications | 10 | SZ | 6/11 |
| Geddes et al36 | Antepartum haemorrhage; birth weight <2500 g; caesarean section; congenital malformations; cord complications; forceps delivery; gestational age <37 weeks; incubator or resuscitation; labour >24 hours; non‐vertex presentation; preeclampsia; Rhesus incompatibility; rubella or syphilis; twin birth | 9, 9, 9, 7, 9, 9, 3, 8, 4, 9, 9, 7, 9, 9 | SZ | 4/11 |
| McGrath & Welham80 | Winter/spring season of birth in Southern hemisphere | 7 | SZ | 9/11 |
| Selten et al106 | Maternal stress during pregnancy | 4 | SZ | 5/11 |
| Selten & Termoshuizen41 | Gestational influenza | 7 | SZ, AP | 7/11 |
| Van Lieshout et al82 | Pre‐pregnancy and pregnancy maternal obesity | 4 | SZ, NAP | 10/11 |
k – number of studies for each factor, FEP – first episode of psychosis, SZ – schizophrenia, NAP – non‐affective psychosis other than schizophrenia, AP – affective psychosis, AMSTAR – A Measurement Tool to Assess Systematic Reviews
Table 3.
Characteristics of meta‐analyses and systematic reviews studying the association between psychotic disorders and later factors
| Study | Factors examined | k | Diagnosis |
AMSTAR index |
|---|---|---|---|---|
| Arias et al83 | BK virus; Borna disease virus; Chlamydia psittaci; Chlamydia trachomatis; cytomegalovirus; Epstein‐Barr virus; human endogenous retrovirus; human endogenous retrovirus type k115; human endogenous retrovirus type W; human herpes virus 2; influenza; JC virus; Toxocara spp; varicella zoster virus | 1, 8, 2, 2, 8, 3, 4, 1, 4, 5, 2, 1, 1, 4 | SZ | 8/11 |
| Attademo et al84 | Benzene; carbon monoxide; nitrogen dioxide; nitrogen oxides; tetrachloroethylene; traffic | 1, 1, 1, 1, 1, 1 | SZ | 2/11 |
| Beards et al85 | Adult life events | 6 | FEP, SZ, NAP, AP | 8/11 |
| Clancy et al86 | Epilepsy | 1 | SZ | 6/11 |
| Cunningham et al87 | Bullying | 1 | SZ, NAP | 7/11 |
| De Sousa et al88 | Parental communication deviance | 4 | SZ | 6/11 |
| Gurillo et al89 | Tobacco use | 5 | FEP, SZ, NAP, AP | 11/11 |
| Gutierrez‐Fernandez et al90 | Chlamydia pneumoniae; human herpes virus 1; human herpes virus 6 | 3, 11, 3 | SZ, NAP | 8/11 |
| Khandaker et al91 | Central nervous system infection during childhood | 2 | SZ, NAP | 10/11 |
| Linszen et al92 | Hearing impairment | 5 | SZ | 8/11 |
| Marconi et al93 | Heavy cannabis use | 2 | FEP, SZ, NAP | 7/11 |
| Molloy et al94 | Traumatic brain injury | 8 | SZ | 7/11 |
| Sutterland et al95 | Toxoplasma gondii IgG; Toxoplasma gondii IgM | 40, 15 | FEP, SZ | 9/11 |
| Varese et al54 | Childhood trauma | 20 | FEP, SZ, NAP, AP | 10/11 |
k – number of studies for each factor, FEP – first episode of psychosis, SZ – schizophrenia, NAP – non‐affective psychosis other than schizophrenia, AP – affective psychosis, AMSTAR – A Measurement Tool to Assess Systematic Reviews, Ig – immunoglobulin
Table 4.
Characteristics of meta‐analyses and systematic reviews studying the association between psychotic disorders and antecedents
| Study | Factors examined | k | Diagnosis |
AMSTAR index |
|---|---|---|---|---|
| Dickson et al96 | Motor function pre‐onset of psychosis; poor academic achievement pre‐onset of psychosis; poor mathematic academic achievement pre‐onset of psychosis | 4, 4, 3 | FEP, SZ, NAP | 7/11 |
| Filatova et al97 | Delay in grabbing object; delay in holding head up; delay in sitting unsupported; delay in standing unsupported; delay in walking unsupported | 3, 3, 4, 4, 5 | SZ, NAP | 9/11 |
| Fusar‐Poli et al98 | Ultra‐high‐risk state for psychosis | 9 | FEP | 9/11 |
| Golembo‐Smith et al48 | ATD angle; fingertip pattern asymmetry; fluctuating asymmetry A‐B ridge count; fluctuating asymmetry finger ridge count; total A‐B ridge count; total finger ridge count | 5, 4, 3, 3, 13, 13 | SZ | 6/11 |
| Hirnstein & Hugdahl47 | Non‐right handedness | 41 | SZ, NAP | 5/11 |
| Khandaker et al39 | Premorbid IQ | 5 | SZ, NAP | 8/11 |
| Kaymaz et al99 | Psychotic‐like experiences | 4 | FEP, SZ, NAP, AP | 10/11 |
| Koning et al100 | Dyskinesia in antipsychotic‐naïve schizophrenic patients; parkinsonism in antipsychotic‐naïve schizophrenic patients | 5, 3 | FEP, SZ | 5/11 |
| Matheson et al43 | Childhood social withdrawal | 5 | SZ, NAP | 8/11 |
| Moberg et al63 | Olfactory detection ability; olfactory identification ability; olfactory discrimination ability; olfactory memory ability; olfactory hedonics ability (pleasant odours); olfactory hedonics ability (unpleasant odours); olfactory hedonics ability (unspecified odours) | 18, 51, 8, 2, 9, 8, 7 | SZ, NAP | 9/11 |
| Neelam et al49 | Neurological soft signs | 7 | SZ, NAP | 8/11 |
| Ohi et al101 | Cooperativeness; harm avoidance; novelty seeking; persistence; reward dependence; self‐directedness; self‐transcendence | 7, 7, 7, 7, 7, 7, 7 | SZ | 4/11 |
| Ohi et al102 | Agreeableness; conscientiousness; extraversion; neuroticism; openness | 6, 7, 8, 8, 7 | SZ | 6/11 |
| Potvin & Marchand103 | Hypoalgesia | 9 | SZ | 5/11 |
| Tarbox & Pogue‐Geile42 | Childhood antisocial and externalizing behaviour; childhood social withdrawal and internalizing behaviour | 2, 6 | SZ, NAP | 3/11 |
| Ward et al104 | Extracranial size | 7 | SZ, NAP | 3/11 |
| Woodberry et al38 | Premorbid IQ | 11 | SZ | 7/11 |
| Xu et al46 | Minor physical anomalies | 14 | SZ | 4/11 |
| Yan et al105 | Trait anhedonia | 44 | SZ, NAP | 6/11 |
k – number of studies for each factor, FEP – first episode of psychosis, SZ – schizophrenia, NAP – non‐affective psychosis other than schizophrenia, AP – affective psychosis, AMSTAR – A Measurement Tool to Assess Systematic Reviews, ATD angle – dermatoglyphic feature that compares the length of the hand to the width
Summary of associations
The number of cases was greater than 1,000 for 48 factors (28.2%). One hundred three of the 170 analyzed factors (60.6%) presented a statistically significant effect (p<0.05) under the random‐effects model, but only 39 (22.9%) reached p<10−6. Fifty‐three factors (31.2%) presented a large heterogeneity (I2>50%), while for 28 (16.5%) the 95% prediction interval did not include the null. Additionally, the evidence for small‐study effects and excess significance bias was noted for 16 (9.4%) and 17 (10.0%) factors, respectively.
Classification of level of evidence of associations between socio‐demographic and parental, perinatal, later factors or antecedents and psychotic disorders
Among the 170 factors, one socio‐demographic factor (Black‐Caribbean ethnicity in England: OR=4.87, 95% CI: 3.96‐6.00) and one antecedent (ultra‐high‐risk state: OR=9.32, 95% CI: 4.91‐17.72) presented a convincing level of association (class I: >1000 cases, p < 10−6, no evidence of small‐study effects or excess significance bias, 95% prediction interval not including the null, and no large heterogeneity).
For six factors there was highly suggestive evidence for association (class II: >1000 cases, p<10−6, largest study with a statistically significant effect, and class I criteria not met). These were two socio‐demographic and parental factors (ethnic minority in low ethnic density area: OR=3.71; and second generation immigrants: OR=1.68); none of the perinatal and later factors; and four antecedents (minor physical anomalies: OR=5.30; trait anhedonia: OR=4.41; olfactory identification ability: OR=0.19; and premorbid IQ: OR=0.47).
There was suggestive evidence for association (class III) for nine further factors: four socio‐demographic and parental factors (North‐African immigrants in Europe: OR=2.22; urbanicity: OR=2.19; ethnic minority in high ethnic density area: OR=2.11; and first generation immigrants: OR=2.10); one perinatal factor (winter/spring season of birth in Northern hemisphere: OR=1.04); two later factors (childhood trauma: OR=2.87; and Toxoplasma gondii IgG: OR=1.82); and two antecedents (childhood social withdrawal: OR=2.91; and non‐right handedness: OR=1.58). There was either weak (class IV) or no evidence of association with psychotic disorders for all other factors (see Tables 5, 6, 7, 8).
Table 5.
Level of evidence for the association of socio‐demographic and parental factors and psychotic disorders
| Factor | k | Random‐effects measure, ES (95% CI) | Features used for classification of level of evidence | eOR | CE | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | p random‐effects | I2 (p) | PI (95% CI) | SSE/ESB | LS | |||||
| Black‐Caribbean ethnicity in England76 | 9 | IRR, 4.87 (3.96‐6.00) | 3,446 | 2.8 × 10−50 | 38% (0.12) | 2.95‐8.03 | No/No | Yes | 4.87 | I |
| Ethnic minority in low ethnic density area71 | 5 | IRR, 3.71 (2.47‐5.58) | 1,328 | 3.1 × 10−10 | 70% (0.09) | 0.95‐14.43 | Yes/No | Yes | 3.71 | II |
| Second generation immigrants53 | 26 | IRR, 1.68 (1.42‐1.92) | 28,753 | 7.6 × 10−10 | 77% (<0.001) | 0.92‐3.06 | No/No | Yes | 1.68 | II |
| North African immigrants in Europe77 | 12 | IRR, 2.22 (1.58‐3.12) | 2,577 | 4.2 × 10−6 | 65% (0.001) | 0.77‐6.41 | No/NA | Yes | 2.22 | III |
| Urbanicity78 | 8 | OR, 2.19 (1.55‐3.09) | 45,791 | 8.9 x 10−5 | 99% (<0.001) | 0.62‐7.77 | No/No | Yes | 2.19 | III |
| Ethnic minority in high ethnic density area71 | 5 | IRR, 2.11 (1.39‐3.20) | 1,328 | 4.3 × 10−4 | 58% (0.04) | 0.57‐7.81 | No/No | Yes | 2.11 | III |
| First generation immigrants53 | 42 | IRR, 2.10 (1.72‐2.56) | 25,063 | 1.9 × 10−13 | 89% (<0.001) | 0.75‐5.89 | No/Yes | No | 2.10 | III |
| Parental severe mental illness75 | 9 | RR, 5.94 (2.99‐11.79) | 90 | 3.5 × 10−7 | 0% (0.85) | 2.60‐13.59 | No/No | Yes | 5.94 | IV |
| Black African ethnicity in England2 | 4 | IRR, 4.72 (3.30‐6.77) | 452 | 2.3 × 10−17 | 49% (0.12) | 1.25‐17.82 | No/NA | Yes | 4.72 | IV |
| Asian ethnicity in England2 | 6 | IRR, 2.83 (1.59‐5.05) | 613 | 4.2 × 10−4 | 55% (0.05) | 0.53‐15.00 | No/Yes | No | 2.83 | IV |
| Other white ethnicity in England2 | 3 | IRR, 2.62 (1.35‐5.10) | 274 | 0.004 | 87% (<0.001) | 0.93‐21.88 | No/NA | Yes | 2.62 | IV |
| Paternal age >45 years72 | 4 | OR, 2.36 (1.35‐4.11) | 392 | 0.003 | 0% (0.66) | 0.69‐8.01 | No/Yes | No | 2.36 | IV |
| Disadvantaged vs. advantaged groups55 | 3 | RR, 2.27 (1.21‐4.27) | 532 | 0.010 | 69% (0.04) | 0‐2016.72 | No/No | Yes | 2.27 | IV |
| Mixed ethnicity in England2 | 3 | IRR, 2.19 (1.08‐4.44) | 330 | 0.030 | 0% (0.41) | 0.02‐14.53 | No/NA | No | 2.19 | IV |
| Low paternal socio‐economic status73 | 9 | OR, 1.30 (1.02‐1.65) | 15,922 | 0.032 | 94% (<0.001) | 0.58‐2.90 | No/No | Yes | 1.30 | IV |
| Paternal age >35 years72 | 9 | OR, 1.22 (1.06‐1.41) | 2,181 | 0.007 | 30% (0.18) | 0.89‐1.67 | No/Yes | No | 1.22 | IV |
| Neighbourhood level social deprivation74 | 3 | OR, 1.64 (0.83‐3.23) | 5,560 | 0.156 | 88% (<0.001) | 0‐5961.52 | No/No | No | 1.64 | ns |
| Paternal age >55 years72 | 7 | OR, 1.21 (0.82‐1.78) | 57 | 0.341 | 47% (0.07) | 0.45‐3.22 | No/No | No | 1.21 | ns |
k – number of samples for each factor, ES – effect size, N – number of cases, PI – prediction interval, CI – confidence interval, SSE – small‐study effect, ESB – excess significance bias, LS – largest study with significant effect, eOR – equivalent odds ratio, CE – class of evidence, IRR – incidence rate ratio, OR – odds ratio, RR – relative risk, NA – not assessable, ns – not significant
Table 6.
Level of evidence for the association of perinatal factors and psychotic disorders
| Factor | k |
Random‐effects measure, ES (95% CI) |
Features used for classification of level of evidence | eOR | CE | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | p random‐effects | I2 (p) | PI (95% CI) | SSE/ESB | LS | |||||
| Winter/spring season of birth in Northern hemisphere79 | 27 | OR, 1.04 (1.02‐1.06) | 115,010 | 2.1 × 10−6 | 0% (0.99) | 1.02‐1.06 | No/No | Yes | 1.04 | III |
| Diabetes in pregnancy37 | 2 | OR, 10.12 (1.84‐55.72) | 243 | 0.008 | 0% (0.69) | NA | NA/NA | No | 10.12 | IV |
| Emergency caesarean section37 | 3 | OR, 3.36 (1.48‐7.63) | 825 | 0.004 | 0% (0.92) | 0.02‐685.69 | No/No | No | 3.36 | IV |
| Birth weight <2000 g37 | 2 | OR, 2.46 (1.11‐5.46) | 507 | 0.027 | 0% (0.85) | NA | NA/NA | Yes | 2.46 | IV |
| Congenital malformations36, 37 | 10 | OR, 2.31 (1.29‐4.13) | 1,080 | 0.005 | 0% (0.99) | 1.16‐4.57 | No/Yes | Yes | 2.31 | IV |
| Incubator or resuscitation36 | 8 | OR, 2.12 (1.29‐3.47) | 438 | 0.003 | 0% (0.85) | 1.14‐3.92 | No/No | No | 2.12 | IV |
| Neonatal vitamin D (<19.7 vs. 40.5‐50.9 nmol/L)50 | 1 | RR, 2.11 (1.28‐3.49) | 424 | 0.004 | NA (1.00) | NA | NA/NA | Yes | 2.11 | IV |
| Neonatal vitamin D (30.9‐40.4 vs. 40.5‐50.9 nmol/L)50 | 1 | RR, 2.10 (1.30‐3.40) | 424 | 0.003 | NA (1.00) | NA | NA/NA | Yes | 2.10 | IV |
| Threatened premature delivery37 | 2 | OR, 2.05 (1.02‐4.10) | 314 | 0.043 | 0% (0.56) | NA | NA/NA | Yes | 2.05 | IV |
| Neonatal vitamin D (19.7‐30.9 vs. 40.5‐50.9 nmol/L)50 | 1 | RR, 2.02 (1.27‐3.19) | 424 | 0.003 | NA (1.00) | NA | NA/NA | Yes | 2.02 | IV |
| Pre‐pregnancy and pregnancy maternal obesity82 | 4 | OR, 1.99 (1.26‐3.14) | 305 | 0.003 | 27% (0.24) | 0.47‐8.50 | No/No | No | 1.99 | IV |
| Uterine atony37 | 3 | OR, 1.93 (1.35‐2.76) | 836 | 3.3 × 10−4 | 0% (0.37) | 0.19‐19.78 | No/No | Yes | 1.93 | IV |
| Obstetric complications81 | 10 | OR, 1.84 (1.25‐2.70) | 373 | 0.002 | 25% (0.21) | 0.80‐4.22 | Yes/Yes | No | 1.84 | IV |
| Neonatal vitamin D (>50.9 vs. 40.5‐50.9 nmol/L)50 | 1 | RR, 1.71 (1.04‐2.80) | 424 | 0.033 | NA (1.00) | NA | NA/NA | Yes | 1.71 | IV |
| Antepartum haemorrhage36, 37 | 14 | OR, 1.63 (1.12‐2.38) | 1,489 | 0.011 | 6% (0.38) | 0.92‐2.89 | No/No | No | 1.63 | IV |
| Birth weight <2500 g36, 37 | 13 | OR, 1.57 (1.20‐2.07) | 1,815 | 0.001 | 0% (0.45) | 1.16‐2.14 | No/Yes | Yes | 1.57 | IV |
| Small head circumference37 | 2 | OR, 1.41 (1.00‐1.97) | 762 | 0.048 | 0% (0.58) | NA | NA/NA | No | 1.41 | IV |
| Placental abruption37 | 2 | OR, 4.54 (0.32‐64.63) | 314 | 0.264 | 72% (0.05) | NA | NA/NA | No | 4.54 | ns |
| Rhesus incompatibility36, 37 | 9 | OR, 1.96 (0.88‐4.33) | 1,097 | 0.098 | 0% (0.98) | 0.75‐5.11 | No/NA | No | 1.96 | ns |
| Asphyxia37 | 3 | OR, 1.95 (0.77‐4.97) | 1,122 | 0.160 | 76% (0.01) | 0‐108727 | No/No | Yes | 1.95 | ns |
| Forceps delivery36 | 9 | OR, 1.67 (0.90‐3.08) | 554 | 0.103 | 42% (0.08) | 0.34‐8.15 | Yes/No | Yes | 1.67 | ns |
| Rubella or syphilis36 | 9 | OR, 1.64 (0.47‐5.71) | 567 | 0.435 | 0% (0.099) | 0.37‐7.39 | No/No | No | 1.64 | ns |
| Twin birth36 | 9 | OR, 1.53 (0.79‐2.97) | 558 | 0.208 | 0% (0.45) | 0.69‐3.40 | Yes/No | No | 1.53 | ns |
| Gestational age <37 weeks36, 37 | 7 | OR, 1.35 (0.99‐1.84) | 1,502 | 0.057 | 0% (0.66) | 0.90‐2.03 | Yes/No | No | 1.35 | ns |
| Being small for gestational age37 | 5 | OR, 1.34 (0.82‐2.19) | 1,436 | 0.240 | 58% (0.04) | 0.28‐6.41 | No/No | Yes | 1.34 | ns |
| Smoking in pregnancy37 | 1 | OR, 1.29 (0.72‐2.31) | 76 | 0.393 | NA (1.00) | NA | NA/NA | No | 1.29 | ns |
| Birth weight <2500 g and prematurity37 | 4 | OR, 1.25 (0.52‐3.00) | 959 | 0.610 | 65% (0.03) | 0.03‐46.31 | No/No | Yes | 1.25 | ns |
| Anaemia in pregnancy37 | 3 | OR, 1.22 (0.46‐3.28) | 528 | 0.688 | 56% (0.10) | 0‐ 41770 | No/No | No | 1.22 | ns |
| Maternal stress during pregnancy106 | 5 | RR, 1.16 (0.94‐1.43) | 4,412 | 0.166 | 71% (0.01) | 0.60‐2.25 | No/No | No | 1.16 | ns |
| Low Apgar score37 | 2 | OR, 1.13 (0.69‐1.84) | 405 | 0.622 | 0% (0.67) | NA | NA/NA | No | 1.13 | ns |
| Preeclampsia36, 37 | 15 | OR, 1.07 (0.78‐1.46) | 2,277 | 0.690 | 22% (0.20) | 0.53‐2.15 | No/No | Yes | 1.07 | ns |
| Forceps/vacuum delivery37 | 7 | OR, 1.07 (0.81‐1.42) | 1,888 | 0.643 | 34% (0.16) | 0.55‐2.09 | No/No | Yes | 1.07 | ns |
| Cord complications36 | 9 | OR, 1.06 (0.47‐2.39) | 549 | 0.894 | 0% (0.54) | 0.40‐2.83 | No/No | No | 1.06 | ns |
| Small birth length37 | 3 | OR, 1.05 (0.86‐1.30) | 929 | 0.619 | 0% (0.91) | 0.28‐4.03 | No/No | No | 1.05 | ns |
| Baby detained in hospital37 | 3 | OR, 1.04 (0.59‐1.86) | 976 | 0.883 | 76% (0.01) | 0‐903.90 | No/No | Yes | 1.04 | ns |
| Winter/spring season of birth in Southern hemisphere80 | 7 | OR, 1.03 (0.88‐1.19) | 15,023 | 0.738 | 16% (0.30) | 0.77‐1.37 | No/NA | No | 1.03 | ns |
| Influenza during pregnancy40, 41 | 14 | OR, 0.99 (0.91‐1.08) | 7,620 | 0.867 | 46% (0.03) | 0.79‐1.24 | No/No | No | 0.99 | ns |
| Non‐vertex presentation36, 37 | 15 | OR, 0.99 (0.75‐1.31) | 2,272 | 0.953 | 6% (0.38) | 0.65‐1.51 | No/No | No | 0.99 | ns |
| Gestational age >42 weeks37 | 3 | OR, 0.97 (0.48‐1.95) | 1,193 | 0.933 | 42% (0.18) | 0‐1000 | No/No | No | 0.97 | ns |
| Caesarean section36, 37 | 15 | OR, 0.95 (0.71‐1.28) | 1,920 | 0.734 | 0% (0.46) | 0.68‐1.32 | No/No | No | 0.95 | ns |
| Breech delivery37 | 3 | OR, 0.95 (0.49‐1.84) | 470 | 0.879 | 0% (0.78) | 0.01‐68.26 | No/No | No | 0.95 | ns |
| Urinary infection in pregnancy37 | 3 | OR, 0.90 (0.44‐1.84) | 690 | 0.776 | 29% (0.24) | 0‐498.73 | No/No | No | 0.90 | ns |
| Induction of labor37 | 3 | OR, 0.82 (0.53‐1.28) | 528 | 0.387 | 24% (0.26) | 0.02‐35.30 | No/No | No | 0.82 | ns |
| Cephalopelvic disproportion37 | 2 | OR, 0.60 (0.18‐1.99) | 243 | 0.407 | 0% (0.48) | NA | NA/NA | No | 0.60 | ns |
| Labour >24 hours36 | 4 | OR, 0.84 (0.39‐1.78) | 266 | 0.643 | 20% (0.28) | 0.09‐8.11 | No/No | No | 0.84 | ns |
k – number of samples for each factor, ES – effect size, N – number of cases, PI – prediction interval, CI – confidence interval, SSE – small‐study effect, ESB – excess significance bias, LS – largest study with significant effect, eOR – equivalent odds ratio, CE – class of evidence, IRR – incidence rate ratio, OR – odds ratio, RR – relative risk, NA – not assessable, ns – not significant
Table 7.
Level of evidence for the association of later factors and psychotic disorders
| Factor | k |
Random‐effects measure, ES (95% CI) |
Features used for classification of level of evidence | eOR | CE | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | p random‐effects | I2 (p) | PI (95% CI) | SSE/ESB | LS | |||||
| Childhood trauma54 | 20 | OR, 2.87 (2.07‐3.98) | 2,363 | 2.5 × 10−14 | 77% (<0.001) | 0.75‐11.01 | No/Yes | No | 2.87 | III |
| Toxoplasma gondii IgG95 | 42 | OR, 1.82 (1.51‐2.18) | 8,796 | 2.1 × 10−10 | 78% (<0.001) | 0.68‐4.88 | Yes/Yes | No | 1.82 | III |
| Toxocara spp83 | 1 | OR, 41.61 (9.71‐178.32) | 98 | 5.1 × 10−7 | NA (1.00) | NA | NA/NA | Yes | 41.61 | IV |
| Chlamydia psittaci83 | 2 | OR, 29.05 (8.91‐94.69) | 82 | 2.2 × 10−8 | 0% (0.71) | NA | NA/NA | Yes | 29.05 | IV |
| Human endogenous retrovirus type W83 | 5 | OR, 19.78 (6.50‐60.22) | 256 | 1.4 × 10−7 | 33% (0.20) | 1.05‐372.34 | No/No | Yes | 19.78 | IV |
| Parental communication deviance88 | 4 | g, 1.35 (0.97‐1.73) | 74 | 2.3 × 10−12 | 0% (0.41) | 0.51‐2.19 | No/No | No | 11.55 | IV |
| Chlamydia pneumoniae90 | 3 | OR, 6.02 (2.86‐12.66) | 116 | 2.1 × 10−6 | 0% (0.57) | 0.05‐745.30 | No/No | Yes | 6.02 | IV |
| Traffic84 | 1 | RR, 5.55 (1.63‐18.87) | 29 | 0.006 | NA (<0.001) | NA | NA/NA | Yes | 5.55 | IV |
| Adult life events85 | 6 | OR, 5.34 (3.84‐7.43) | 317 | 2.1 × 10−23 | 3% (0.39) | 3.22‐8.87 | No/No | Yes | 5.34 | IV |
| Heavy cannabis use93 | 2 | OR, 5.17 (3.64‐7.36) | 748 | 6.3 × 10−20 | 42% (0.18) | NA | NA/NA | Yes | 5.17 | IV |
| Benzene84 | 1 | RR, 3.20 (1.01‐10.12) | 29 | 0.048 | NA (1.00) | NA | NA/NA | Yes | 3.20 | IV |
| Tobacco use89 | 6 | RR, 2.19 (1.36‐3.53) | 8,488 | 0.001 | 99% (<0.001) | 0.38‐12.50 | No/No | Yes | 2.19 | IV |
| Borna disease virus83 | 21 | OR, 1.94 (1.30‐2.91) | 1,919 | 0.001 | 36% (0.05) | 0.65‐5.81 | No/No | Yes | 1.94 | IV |
| Traumatic brain injury94 | 8 | OR, 1.49 (1.09‐2.05) | 9,653 | 0.013 | 78% (<0.001) | 0.57‐3.89 | Yes/No | No | 1.49 | IV |
| Human herpes virus 283 | 5 | OR, 1.44 (1.14‐1.81) | 901 | 0.002 | 0% (0.97) | 0.99‐2.09 | No/No | Yes | 1.44 | IV |
| Chlamydia trachomatis83 | 2 | OR, 4.39 (0.03‐587.92) | 82 | 0.554 | 85% (0.01) | NA | NA/NA | No | 4.39 | ns |
| Human endogenous retrovirus83 | 4 | OR, 3.64 (0.72‐18.37) | 128 | 0.117 | 36% (0.19) | 0.01‐1019 | No/No | Yes | 3.64 | ns |
| Tetrachloroethylene84 | 1 | RR, 3.41 (0.48‐24.24) | 4 | 0.219 | NA (1.00) | NA | NA/NA | No | 3.41 | ns |
| Carbon monoxide84 | 1 | RR, 3.07 (0.96‐9.82) | 29 | 0.059 | NA (1.00) | NA | NA/NA | No | 3.07 | ns |
| Epilepsy86 | 1 | OR, 3.06 (0.31‐29.95) | 4 | 0.337 | NA (1.00) | NA | NA/NA | No | 3.06 | ns |
| Nitrogen oxides84 | 1 | RR, 2.02 (0.74‐5.53) | 29 | 0.171 | NA (1.00) | NA | NA/NA | No | 2.02 | ns |
| Central nervous system infection during childhood91 | 2 | RR, 1.99 (0.31‐12.78) | 2,369 | 0.466 | 80% (0.02) | NA | NA/NA | No | 1.99 | ns |
| Epstein‐Barr virus83 | 3 | OR, 1.98 (0.23‐16.85) | 55 | 0.532 | 0% (0.81) | 0‐2121495 | No/No | No | 1.98 | ns |
| Nitrogen dioxide84 | 1 | RR, 1.91 (0.70‐5.19) | 29 | 0.205 | NA (1.00) | NA | NA/NA | No | 1.91 | ns |
| Hearing impairment92 | 5 | OR, 1.64 (0.85‐3.15) | 597 | 0.141 | 76% (0.002) | 0.18‐15.17 | No/No | Yes | 1.64 | ns |
| Toxoplasma gondii IgM95 | 15 | OR, 1.24 (0.97‐1.59) | 2,867 | 0.083 | 2% (0.43) | 0.91‐1.70 | No/No | No | 1.24 | ns |
| Human herpes virus 190 | 11 | OR, 1.24 (0.98‐1.58) | 1,117 | 0.074 | 5% (0.39) | 0.87‐1.78 | No/No | No | 1.24 | ns |
| Cytomegalovirus83 | 8 | OR, 1.20 (0.65‐2.20) | 171 | 0.558 | 0% (1.00) | 0.56‐2.56 | No/No | No | 1.20 | ns |
| Varicella zoster virus83 | 4 | OR, 1.17 (0.16‐8.58) | 69 | 0.878 | 0% (0.99) | 0.01‐92.93 | No/No | No | 1.17 | ns |
| BK virus83 | 1 | OR, 1.05 (0.02‐55.41) | 20 | 0.979 | NA (1.00) | NA | NA/NA | No | 1.05 | ns |
| JC virus83 | 1 | OR, 1.05 (0.02‐55.41) | 20 | 0.979 | NA (1.00) | NA | NA/NA | No | 1.05 | ns |
| Human endogenous retrovirus type k11583 | 1 | OR, 0.89 (0.43‐1.84) | 178 | 0.753 | NA (1.00) | NA | NA/NA | No | 0.89 | ns |
| Influenza83 | 2 | OR, 0.87 (0.05‐15.48) | 33 | 0.925 | 0% (0.92) | NA | NA/NA | No | 0.87 | ns |
| Human T‐lymphotropic virus 183 | 2 | OR, 0.57 (0.20‐1.62) | 209 | 0.294 | 0% (0.87) | NA | NA/NA | No | 0.57 | ns |
| Bullying87 | 1 | OR, 0.38 (0.13‐1.10) | 30 | 0.075 | NA (1.00) | NA | NA/NA | No | 0.38 | ns |
| Human herpes virus 690 | 3 | OR, 0.34 (0.05‐2.42) | 55 | 0.284 | 0% (0.71) | 0‐106440 | No/No | No | 0.34 | ns |
k – number of samples for each factor, ES – effect size, N – number of cases, PI – prediction interval, CI – confidence interval, SSE – small‐study effect, ESB – excess significance bias, LS – largest study with significant effect, eOR – equivalent odds ratio, CE – class of evidence, IRR – incidence rate ratio, OR – odds ratio, RR – relative risk, Ig – immunoglobulin, NA – not assessable, ns – not significant
Table 8.
Level of evidence for the association of antecedents and psychotic disorders
| Factor | k |
Random‐effects measure, ES (95%CI) |
Features used for classification of level of evidence | eOR | CE | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | p random‐effects | I2 (p) | PI (95% CI) | SSE/ESB | LS | |||||
| Ultra‐high‐risk state for psychosis98 | 9 | RR, 9.32 (4.91 to 17.72) | 1,226 | 9.5 × 10−12 | 0% (0.91) | 4.30 to 20.24 | No/No | No | 9.32 | I |
| Minor physical anomalies46 | 14 | g, 0.92 (0.61 to 1.23) | 1,212 | 5.8 × 10−9 | 91% (<0.001) | −0.34 to 2.18 | No/Yes | Yes | 5.30 | II |
| Trait anhedonia105 | 44 | g, 0.82 (0.72 to 0.92) | 1,601 | 9.2 × 10−57 | 43% (0.002) | 0.37 to 1.27 | No/Yes | Yes | 4.41 | II |
| Olfactory identification ability63 | 55 | g, −0.91 (–1.05 to −0.78) | 1,703 | 4.0 × 10−41 | 67% (<0.001) | −1.72 to −0.10 | Yes/Yes | Yes | 0.19 | II |
| Premorbid IQ38, 39 | 16 | g, −0.42 (−0.52 to −0.33) | 4,459 | 1.1 × 10−18 | 73% (<0.001) | −0.70 to −0.14 | No/No | Yes | 0.47 | II |
| Childhood social withdrawal42, 43 | 15 | g, 0.59 (0.33 to 0.85) | 1,810 | 6.4 × 10−6 | 93% (<0.001) | −0.44 to 1.62 | No/No | Yes | 2.91 | III |
| Non‐right handedness47 | 41 | OR, 1.58 (1.35 to 1.86) | 2,652 | 2.0 × 10−8 | 21% (0.12) | 0.99 to 2.54 | No/No | No | 1.58 | III |
| Neurological soft signs49 | 8 | g, 1.83 (1.28 to 2.38) | 564 | 7.7 × 10−11 | 93% (<0.001) | −0.15 to 3.81 | Yes/No | Yes | 27.59 | IV |
| Neuroticism102 | 8 | g, 1.20 (0.88 to 1.52) | 430 | 2.7 × 10−13 | 73% (<0.001) | 0.18 to.21 | No/No | Yes | 8.76 | IV |
| Harm avoidance101 | 7 | g, 0.98 (0.78 to 1.18) | 384 | 4.5 × 10−21 | 48% (0.07) | 0.43 to 1.53 | No/No | Yes | 5.92 | IV |
| Parkinsonism in antipsychotic‐naïve schizophrenic patients100 | 3 | OR, 5.33 (1.75 to 16.23) | 84 | 0.003 | 0% (0.81) | 0 to 7310 | No/No | Yes | 5.33 | IV |
| Psychotic like experiences99 | 4 | RR, 3.84 (2.55 to 5.79) | 118 | 1.2 × 10−10 | 0% (0.65) | 1.56 to 9.45 | No/No | No | 3.84 | IV |
| Dyskinesia in antipsychotic‐naïve schizophrenic patients100 | 5 | OR, 3.59 (1.53 to 8.42) | 189 | 0.003 | 0% (0.75) | 0.90 to 14.32 | No/No | Yes | 3.59 | IV |
| Self‐transcendence101 | 7 | g, 0.61 (0.48 to 0.75) | 384 | 7.8 × 10−19 | 0% (0.67) | 0.43 to 0.79 | No/No | Yes | 3.03 | IV |
| Antisocial and externalizing behaviour42 | 3 | g, 0.48 (0.22 to 0.74) | 68 | 3.1 × 10−4 | 36% (0.20) | −1.97 to 2.93 | No/No | Yes | 2.39 | IV |
| Delay in walking unsupported97 | 5 | g, 0.48 (0.27 to 0.68) | 368 | 4.3 × 10−6 | 81% (<0.001) | −0.27 to 1.22 | Yes/NA | Yes | 2.37 | IV |
| Hypoalgesia103 | 9 | g, 0.46 (0.13 to 0.79) | 204 | 0.006 | 64% (0.005) | −0.57 to 1.49 | No/No | No | 2.31 | IV |
| Extracranial size104 | 7 | g, 0.27 (0.05 to 0.50) | 192 | 0.018 | 15% (0.31) | −0.15 to 0.70 | No/No | Yes | 1.64 | IV |
| Delay in standing unsupported97 | 4 | g, 0.25 (0.12 to 0.39) | 307 | 2.6 × 10−4 | 48% (0.12) | −0.26 to 0.76 | Yes/NA | No | 1.58 | IV |
| Delay in sitting unsupported97 | 4 | g, 0.19 (0.05 to 0.33) | 386 | 0.006 | 48% (0.12) | −0.33 to 0.70 | Yes/NA | No | 1.41 | IV |
| Delay in holding head up97 | 3 | g, 0.13 (0.01 to 0.24) | 352 | 0.029 | 0% (0.91) | −0.61 to 0.86 | Yes/NA | No | 1.26 | IV |
| Olfactory memory ability63 | 2 | g, −1.62 (–2.24 to −1.01) | 67 | 2.0 × 10−7 | 56% (0.13) | NA | NA/NA | Yes | 0.05 | IV |
| Self‐directedness101 | 7 | g, −0.96 (–1.10 to −0.82) | 384 | 7.7 × 10−42 | 0% (0.75) | −1.14 to −0.78 | No/No | Yes | 0.17 | IV |
| Extraversion102 | 8 | g, −0.90 (–1.05 to −0.75) | 430 | 3.6 × 10−32 | 5% (0.38) | −1.13 to −0.67 | No/No | Yes | 0.20 | IV |
| Olfactory discrimination ability63 | 8 | g, −0.88 (–1.16 to −0.60) | 226 | 4.1 × 10−10 | 45% (0.07) | −1.61 to −0.15 | No/No | Yes | 0.20 | IV |
| Olfactory hedonics ability (pleasant odours)63 | 10 | g, −0.76 (−0.99 to −0.54) | 298 | 2.5 × 10−11 | 38% (0.10) | −1.34 to −0.19 | No/No | Yes | 0.25 | IV |
| Conscientiousness102 | 7 | g, −0.68 (−0.92 to −0.44) | 399 | 2.2 × 10−8 | 51% (0.05) | −1.33 to −0.04 | No/No | Yes | 0.29 | IV |
| Olfactory detection ability63 | 18 | g, −0.63 (−0.94 to −0.32) | 498 | 5.9 × 10−5 | 80% (<0.001) | −1.92 to 0.66 | Yes/Yes | No | 0.32 | IV |
| Motor function pre‐onset of psychosis96 | 4 | g, −0.56 (−0.73 to −0.38) | 152 | 4.1 × 10−10 | 0% (0.60) | −0.94 to −0.17 | No/No | Yes | 0.36 | IV |
| Olfactory hedonics ability (unspecified odours)63 | 7 | g, −0.51 (−0.78 to −0.24) | 142 | 2.1 × 10−4 | 21% (0.26) | −1.06 to 0.05 | No/No | No | 0.40 | IV |
| Agreeableness102 | 6 | g, −0.47 (−0.88 to −0.07) | 375 | 0.022 | 81% (<0.001) | −1.82 to 0.88 | No/No | Yes | 0.42 | IV |
| Cooperativeness101 | 7 | g, −0.47 (−0.60 to −0.33) | 384 | 7.9 × 10−12 | 0% (0.88) | −0.64 to −0.29 | Yes/Yes | Yes | 0.43 | IV |
| Reward dependence101 | 7 | g, −0.43 (−0.56 to −0.30) | 384 | 2.7 × 10−10 | 0% (0.43) | −0.61 to −0.26 | No/No | Yes | 0.46 | IV |
| Openness102 | 7 | g, −0.40 (−0.67 to −0.13) | 399 | 0.003 | 62% (0.01) | −1.18 to 0.38 | No/Yes | No | 0.49 | IV |
| Olfactory hedonics ability (unpleasant odours)63 | 9 | g, −0.35 (−0.53 to −0.17) | 244 | 1.3 × 10−4 | 0% (0.79) | −0.57 to −0.13 | No/No | No | 0.53 | IV |
| Persistence101 | 7 | g, −0.24 (−0.39 to −0.08) | 384 | 0.003 | 22% (0.26) | −0.56 to 0.09 | No/No | No | 0.65 | IV |
| Total A‐B ridge count48 | 13 | g, −0.15 (−0.28 to −0.02) | 979 | 0.027 | 46% (0.35) | −0.53 to 0.23 | No/No | No | 0.76 | IV |
| Fluctuating asymmetry A‐B ridge count48 | 4 | g, 0.74 (−0.65 to 2.13) | 241 | 0.295 | 98% (<0.001) | −6.00 to 7.49 | No/Yes | Yes | 3.84 | ns |
| Fluctuating asymmetry finger ridge count48 | 4 | g, 0.31 (−0.50 to 1.12) | 233 | 0.448 | 94% (<0.001) | −3.54 to 4.17 | No/No | Yes | 1.76 | ns |
| Fingertip pattern asymmetry48 | 5 | g, 0.25 (−0.08 to 0.59) | 249 | 0.138 | 66% (0.02) | −0.85 to 1.35 | No/No | Yes | 1.58 | ns |
| Poor general academic achievement pre‐onset of psychosis96 | 4 | g, 0.20 (−0.12 to 0.51) | 1,007 | 0.219 | 93% (<0.001) | −1.25 to 1.65 | No/No | Yes | 1.43 | ns |
| ATD angle48 | 5 | g, 0.16 (−0.02 to 0.34) | 261 | 0.083 | 0% (0.54) | −0.13 to 0.46 | No/No | No | 1.34 | ns |
| Poor mathematic academic achievement pre‐onset of psychosis96 | 3 | g, 0.11 (−0.24 to 0.47) | 136 | 0.527 | 63% (0.06) | −3.77 to 3.99 | No/No | Yes | 1.23 | ns |
| Delay in grabbing object97 | 3 | g, 0.05 (−0.07 to 0.17) | 351 | 0.440 | 14% (0.31) | −0.90 to 1.00 | Yes/NA | No | 1.09 | ns |
| Novelty seeking101 | 7 | g, −0.31 (−0.68 to 0.05) | 384 | 0.092 | 85% (<0.001) | −1.56 to 0.93 | No/No | No | 0.57 | ns |
| Total finger ridge count48 | 13 | g, −0.12 (−0.29 to 0.04) | 935 | 0.149 | 65% (0.001) | −0.69 to 0.44 | No/Yes | No | 0.80 | ns |
k – number of samples for each factor, ES – effect size, N – number of cases, PI – prediction interval, CI – confidence interval, SSE – small study effect, ESB – excess significance bias, LS – largest study with significant effect, eOR – equivalent odds ratio, CE – class of evidence, IRR – incidence rate ratio, OR – odds ratio, RR – relative risk, ATD angle – dermatoglyphic feature that compares the length of the hand to the width, NA – not assessable, ns – not significant
Exploratory analyses
Results of the exploratory analyses on the association between age and gender strata (total of 23 strata) showed a main effect for male gender (males vs. females: IRR=1.34, 95% CI: 1.05‐1.71, class IV). There was also a main effect for 15‐35 year‐old age (25‐34 year‐old vs. other: IRR=1.45, 95% CI: 1.29‐1.63, class II; 20‐29 year‐old vs. other: IRR=2.43, 95% CI: 1.58‐3.74, class IV; 15‐24 year‐old vs. other: IRR=1.46, 95% CI: 1.14‐1.87, class IV). Age older than 35 was found to be a protective factor (60‐69 year‐old vs. other: IRR=0.26, 95% CI: 0.14‐0.51, class IV; 55‐64 year‐old vs. other: IRR=0.30, 95% CI: 0.17‐0.51, class IV; 50‐59 year‐old vs. other: IRR=0.50, 95% CI: 0.27‐0.93, class IV; 40‐49 year‐old vs. other: IRR=0.54, 95% CI: 0.35‐0.83, class IV; 35‐44 year‐old vs. other: IRR=0.80, 95% CI: 0.70‐0.93, class IV).
There was also weak (class IV) association between psychotic disorders and male gender for 15‐40 year‐old age (male vs. female within 20‐29 year‐old: IRR=2.19, 95% CI: 1.69‐2.84; male vs. female within 15‐24 year‐old: IRR=1.98, 95% CI: 1.62‐2.41; male vs. female within 30‐39 year‐old: IRR=1.72, 95% CI: 1.22‐2.41; male vs. female within 25‐34 year‐old: IRR=1.60, 95% CI: 1.26‐2.03). The other ten strata were all not associated with psychotic disorders.
Additional exploratory analyses on latitude (per 10°)55and GNI per capita (per 10,000 USD)56 found significant associations, with ORs of 1.22 and 0.80, respectively. Although these factors include >1000 patients and have a p<0.001, it was not possible to apply the classification of the evidence.
Classification of level of evidence of associations between socio‐demographic and parental, perinatal, later factors or antecedents and psychotic disorders after sensitivity analysis
A sensitivity analysis was not possible for four of the associations categorized as class I‐III in the overall analysis (winter/spring season of birth in Northern hemisphere, olfactory identification ability, trait anhedonia and minor physical anomalies), because they did not include any prospective studies.
Within class I factors, only ultra‐high‐risk state maintained the same level of evidence, whereas Black‐Caribbean ethnicity in England downgraded to a weak (class IV) level of evidence. Equally, all other available class II and III factors were downgraded either to a weak (ethnic minority in low ethnic density area, North‐African immigrants in Europe, childhood trauma, ethnic minority in high ethnic density area, childhood social withdrawal, first and second generation immigrants, Toxoplasma gondii IgG, and premorbid IQ) or a non‐significant (non‐right handedness) level of evidence, except urbanicity, that remained a class III risk factor (Table 9).
Table 9.
Sensitivity analysis for the associations of socio‐demographic and parental, perinatal, later factors, antecedents and psychotic disorders within individual prospective studies of class I‐III factors
| Factor | CE | k |
Random‐effects measure, ES (95% CI) |
Features used for classification of level of evidence | eOR | CES | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N > 1000 | p random‐effects | I2 (p) | PI (95% CI) | SSE/ESB | LS | ||||||
| Ultra‐high‐risk state for psychosis98 | I | 9 | RR, 9.32 (4.91 to 17.72) | Yes | 9.5 × 10−12 | 0% (0.91) | 4.30 to 20.24 | No/No | No | 9.32 | I |
| Urbanicity78 | III | 8 | OR, 2.19 (1.55 to 3.09) | Yes | 8.9 × 10−6 | 99% (<0.001) | 0.62 to 7.77 | No/No | Yes | 2.19 | III |
| Black‐Caribbean ethnicity in England76 | I | 7 | IRR, 5.54 (4.50 to 6.82) | No | 4.9 × 10−59 | 0% (0.48) | 4.22 to 7.27 | No/No | Yes | 5.54 | IV |
| Ethnic minority in low ethnic density area71 | II | 3 | IRR, 4.27 (1.89 to 9.68) | No | 4.9 × 10−4 | 82% (0.004) | 0 to 75335 | Yes/No | Yes | 4.27 | IV |
| North African immigrants in Europe77 | III | 8 | IRR, 3.20 (2.36 to 4.35) | No | 1.0 × 10−13 | 21% (0.27) | 1.73 to 5.94 | No/NA | Yes | 3.20 | IV |
| Childhood trauma54 | III | 4 | OR, 2.52 (1.27 to 5.02) | Yes | 0.009 | 71% (0.016) | 0.14 to 46.01 | No/Yes | No | 2.52 | IV |
| Ethnic minority in high ethnic density area71 | III | 3 | IRR, 2.51 (1.10 to 5.71) | No | 0.028 | 70% (0.037) | 0 to 28153 | No/No | Yes | 2.51 | IV |
| Childhood social withdrawal42, 43 | III | 11 | g, 0.43 (0.14 to 0.71) | Yes | 0.003 | 94% (<0.001) | −0.63 to 1.48 | No/No | Yes | 2.16 | IV |
| First generation immigrants53 | III | 12 | IRR, 1.83 (1.40 to 2.38) | No | 9.6 × 10−6 | 0% (0.82) | 1.35 to 2.47 | No/Yes | No | 1.83 | IV |
| Second generation immigrants53 | II | 10 | IRR, 1.45 (1.05 to 2.01) | Yes | 0.023 | 76% (<0.001) | 0.54 to 3.95 | Yes/No | No | 1.45 | IV |
| Toxoplasma gondii IgG95 | III | 7 | OR, 1.28 (1.06 to 1.55) | Yes | 0.012 | 22% (0.26) | 0.86 to 1.91 | Yes/No | No | 1.28 | IV |
| Premorbid IQ38, 39 | III | 9 | g, −0.43 (–0.64 to −0.22) | No | 5.2 × 10−5 | 62% (0.007) | −1.04 to 0.18 | No/No | Yes | 0.46 | IV |
| Non‐right handedness47 | III | 1 | OR, 1.83 (0.62 to 5.39) | No | 0.273 | NA | NA | NA/NA | No | 1.83 | ns |
| Minor physical anomalies46 | II | NC | NC | NC | NC | NC | NC | NC | NC | NC | NC |
| Olfactory identification ability63 | II | NC | NC | NC | NC | NC | NC | NC | NC | NC | NC |
| Trait anhedonia105 | II | NC | NC | NC | NC | NC | NC | NC | NC | NC | NC |
| Winter/spring season of birth in Northern hemisphere79 | III | NC | NC | NC | NC | NC | NC | NC | NC | NC | NC |
CE – class of evidence, k – number of samples for each factor within prospective studies, ES – effect size, CI – confidence interval, N – number of cases, PI – prediction interval, SSE – small study effect, ESB – excess significance bias, LS – largest study with significant effect, eOR – equivalent odds ratio, CES – class of evidence after sensitivity analysis, RR – relative risk, OR – odds ratio, IRR – incidence rate ratio, NA – not assessable, Ig – immunoglobulin, ns – non‐significant, NC – not calculable (no prospective studies to be analyzed)
DISCUSSION
To our knowledge, this is the first umbrella review of risk and protective factors for psychotic disorders that includes a robust hierarchical classification of the published evidence. Overall, 55 meta‐analyses or systematic reviews, with a total of 683 individual studies and 170 socio‐demographic and parental, perinatal, later factors or antecedents of psychotic disorders, were included. There was convincing evidence (class I) for only two factors, which were the ultra‐high‐risk state for psychosis and Black‐Caribbean ethnicity in England. However, six other factors were characterized by highly suggestive evidence (class II), and another nine by suggestive evidence (class III). Sensitivity analyses that limited data to prospective studies indicated that ultra‐high‐risk state and urbanicity showed the largest evidence of association (class I and class III, respectively) with psychotic disorders.
Overall, our umbrella review indicates that, although a large number of risk factors for psychotic disorders have been evaluated in multiple studies, reviews and meta‐analyses, the number of those that have suggestive or stronger support is far more limited. This is consistent with previous findings about the etiology of other neuropsychiatric conditions where umbrella reviews have been performed, such as dementia, Parkinson's disease, amyotrophic lateral sclerosis, multiple sclerosis and bipolar disorder16, 23, 25, 26, 27.
Although the past two decades have clearly shown that the ultra‐high‐risk state is substantially associated with an increased risk of psychosis11, 108, 109, this result should be interpreted with caution. Firstly, this state is the closest antecedent of psychosis by definition, with onset of the disorder occurring from within a few months of ultra‐high‐risk diagnosis110. Indeed, some ultra‐high‐risk individuals already present with severe symptoms, including short‐lived psychotic episodes111, 112, affective symptoms113 and impaired functioning114. Secondly, the ultra‐high‐risk state is intrinsically heterogeneous10, 115, including different subgroups115 and varying diagnostic operationalizations116. Furthermore, from an epidemiological perspective, it is a spurious condition, characterized by the accumulation of a number of risk factors117 which enrich the risk in an uncontrolled manner118, 119, 120, 121, 122.
Ethnic minority status and urbanicity may better represent true risk factors, contributing to the development of psychotic disorders through increased socio‐environmental adversities123. In fact, the effect of both factors on the risk of developing psychotic disorders may be explained (mediated) by environmental exposures at an individual level, such as substance use, social isolation, social defeat, social fragmentation, and discrimination124. Interestingly, many of these exposures appear to share a common factor of social stress and defeat125, 126, and have been – mostly indirectly – associated with various neurobiological sequelae of potential relevance to psychotic disorders127, such as alterations in the hypothalamic‐pituitary‐adrenal axis128, 129, inflammation130, altered brain functioning131, 132, reduced brain volumes133, and neurochemical dysfunctions126, 134, 135. However, studies to directly assess the correlations between these factors (e.g., urbanicity) and neurobiological alterations in psychotic disorders have only just started to emerge133, 136. Until the exact mechanisms that lead to an increased risk of psychosis are determined, the requirement for biological or psychological plausibility for these factors cannot be fully met. Importantly, future research is required to clarify the contextual specifics of ethnic minority status and urbanicity, because their effects may also be modulated by geographical location or predominant population factors, rather than having universal value.
Several other factors beyond the ultra‐high‐risk state, ethnic minority status, and urbanicity provided a highly suggestive or a suggestive level of evidence of association with psychotic disorders, mostly confirming the role that perinatal factors (winter/spring season of birth in Northern hemisphere) or later factors/antecedents (childhood trauma and childhood social withdrawal, Toxoplasma gondii IgG, minor physical anomalies, trait anhedonia, low olfactory identification ability, low premorbid IQ, and non‐right handedness) might have in psychosis onset. At the same time, a number of the explored factors showed only weak evidence of association with psychotic disorders. Some of these factors, such as heavy cannabis use and obstetric complications, were expected to have stronger evidence. However, weak findings in these areas may simply indicate that there are not yet enough data. Our umbrella review also identified only a few putative protective factors, indicating that the vast majority of available studies have focused on the adverse or negative end of several factors. Future research is required to actively seek unstudied protective factors that are not reciprocal to risk factors, such as specific characteristics of the individual, family or wider environment that improve the likelihood of positive outcomes137.
This study has several conceptual implications. On an etiopathological level, our findings corroborate the notion that psychotic disorders can be related to adversities in an individual's social milieu, whereby environmental exposures during critical developmental periods impact brain, neurocognition, affect, and social cognition13, 138. It is also apparent that most of these factors are likely not specific to psychosis, but also associated with other mental disorders139. From a transdiagnostic perspective, the current study can provide a benchmark for comparing the magnitude of association of these factors with other non‐psychotic mental disorders. On a risk prediction level, these results may substantially advance our ability to prognosticate the onset of psychosis in populations at risk, paralleling the recent advancements observed in genetics.
In this latter area, the availability of robust meta‐analytical evidence of associations between genetic loci and psychotic disorders – provided by the genome‐wide association study (GWAS) meta‐analysis conducted by the Schizophrenia Working Group of the Psychiatric Genomics Consortium44 – has ultimately led to the development of polygenic risk scores to assess the en masse genetic effect of several loci140. Polygenic risk scores have been used to predict case‐control status at the time of a first‐episode psychosis, explaining approximately 9% of the variance140. The small proportion of variance explained indicates that the use of polygenic risk scores in clinical routine would be unwarranted44 without first boosting them with other non‐purely genetic factors.
To date, the integration of multiple non‐purely genetic factors into “polyrisk” scores has been limited by the lack of established and robust a priori knowledge on their association with psychotic disorders139. The current umbrella review attempted to fill this knowledge gap by providing the most robust estimates of association (ORs) between several non‐purely genetic risk (or protective) factors and psychotic disorders. Assessing these predictive factors may offer some logistic advantages over more complex measurements that are based on cognitive, imaging, central or peripheral measures. Simple demographic factors have already been used to develop an individualized risk estimation tool to predict psychosis onset in at‐risk individuals in clinical practice141.
Recently, geneticists have advocated the development of polyrisk scores encompassing socio‐demographic, parental, perinatal, later factors, antecedents, and genetic risk profiling139, 142. Such an approach may ultimately reveal new, clinically useful predictors, because even the risk factors that we found to be weakly associated with psychotic disorders may eventually contribute to the predictive accuracy of the model, as previously observed for genetic associations44. The current umbrella review lays the groundwork for testing the predictive accuracy of integrated polyrisk scores in independent samples139.
Finally, on a pragmatic level, the current stratification of evidence can be used by clinicians, policy makers and regulatory bodies to inform and strategically target outreach campaigns, to promote the prevention of mental disorders in the youth population, and to raise awareness of risk factors for psychotic disorders.
This study also has some limitations. First, association is not necessarily causation. Reverse causation is a particular concern13, and thus establishing the temporality of the association is critical. It is possible that some of the later factors and antecedents are actually characteristics of psychotic disorders themselves or secondary to their appearance. To specifically address these problems and the effect of temporality, we conducted a sensitivity analysis restricted to individual studies with prospective designs.
A second limitation is that the umbrella review approach may favour the selection of more commonly and readily studied factors, since they are more likely to be included in a meta‐analysis. We cannot exclude the possibility that some promising factors, despite having sufficient data, do not have a corresponding eligible meta‐analysis, such as mood and anxiety disorders143, 144, 145, personality disorders146, attachment147, alcohol and psychoactive substances148, 149, 150, 151, sleep dysfunction152, homelessness153 or pervasive developmental disorders154. However, this possibility is becoming less likely in the current era, with meta‐analyses being performed massively, to the point that for several topics multiple meta‐analyses are available155, 156. In any case, for most putative risk or protective factors that are difficult to study (or uncommonly studied), the current grade of evidence is unlikely to be remarkable, given the limited data.
A third limitation is that the definition of healthy control groups employed by each meta‐analysis/systematic review or, when this was not provided, by each individual study, may not be entirely accurate. Moreover, some of the factors included in this umbrella review may be better conceptualized as risk markers, because they may be the result of different interacting risk factors. The ultra‐high‐risk state98, ethnicity76 and immigration status53, 77 are prototypical examples of risk markers, and their limitations have already been addressed above.
Another caution is that the categories of socio‐demographic and parental, perinatal, later factors, and antecedents7, 8, 9 were used only for descriptive purposes. As noted in the Methods section, these categories may actually overlap to some extent. Finally, the relevance of epigenetic risk factors, and the interaction between environmental and genetic factors in psychotic disorders, remains to be elucidated157.
In conclusion, we found several factors to be associated with psychotic disorders at different levels of evidence. These factors represent a starting point of knowledge that can be used to advance etiological research and improve the prediction of psychosis.
ACKNOWLEDGEMENTS
This study was supported in part by the National Institute for Health Research Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King's College London, by a 2017 Medical Research Council Confidence in Concept grant to P. Fusar‐Poli, and by Instituto de Salud Carlos III and FEDER grants (CP14/00041 and PI14/00292) to J. Radua. The funders had no influence on the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The views expressed are those of the authors and not necessarily those of the funders. J. Radua and V. Ramella‐Cravaro contributed equally to this work.
REFERENCES
- 1. Global Burden of Disease Study Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990‐2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:743‐800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kirkbride JB, Errazuriz A, Croudace TJ et al. Incidence of schizophrenia and other psychoses in England, 1950–2009: a systematic review and meta‐analyses. PLoS One 2012;7:e31660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cloutier M, Aigbogun MS, Guerin A et al. The economic burden of schizophrenia in the United States in 2013. J Clin Psychiatry 2016;77:764‐71. [DOI] [PubMed] [Google Scholar]
- 4. Fusar‐Poli P, McGorry PD, Kane J. Improving outcomes of first‐episode psychosis: an overview. World Psychiatry 2017;16:251‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. van Os J, Rutten BPF, Poulton R. Gene‐environment interactions in schizophrenia: review of epidemiological findings and future directions. Schizophr Bull 2008;34:1066‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Howes OD, Murray RM. Schizophrenia: an integrated sociodevelopmental‐cognitive model. Lancet 2014;383:1677‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Matheson SL, Shepherd AM, Laurens KR et al. A systematic meta‐review grading the evidence for non‐genetic risk factors and putative antecedents of schizophrenia. Schizophr Res 2011;133:133‐42. [DOI] [PubMed] [Google Scholar]
- 8. Laurens KR, Luo L, Matheson SL et al. Common or distinct pathways to psychosis? A systematic review of evidence from prospective studies for developmental risk factors and antecedents of the schizophrenia spectrum disorders and affective psychoses. BMC Psychiatry 2015;15:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dean K MR. Environmental risk factors for psychosis. Dialogues Clin Neurosci 2005;7:69‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fusar‐Poli P. The Clinical High‐Risk State for Psychosis (CHR‐P), Version II. Schizophr Bull 2017;43:44‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fusar‐Poli P, Schultze‐Lutter F. Predicting the onset of psychosis in patients at clinical high risk: practical guide to probabilistic prognostic reasoning. Evid Based Ment Health 2016;19:10‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ioannidis JP, Munafo MR, Fusar‐Poli P et al. Publication and other reporting biases in cognitive sciences: detection, prevalence, and prevention. Trends Cogn Sci 2014;18:235‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. van Os J, Kenis G, Rutten BPF. The environment and schizophrenia. Nature 2010;468:203‐12. [DOI] [PubMed] [Google Scholar]
- 14. Aromataris E, Fernandez R, Godfrey CM et al. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Health 2015;13:132‐40. [DOI] [PubMed] [Google Scholar]
- 15. Dinu M, Pagliai G, Casini A et al. Mediterranean diet and multiple health outcomes: an umbrella review of meta‐analyses of observational studies and randomised trials. Eur J Clin Nutr (in press). [DOI] [PubMed] [Google Scholar]
- 16. Bortolato B, Kohler CA, Evangelou E et al. Systematic assessment of environmental risk factors for bipolar disorder: an umbrella review of systematic reviews and meta‐analyses. Bipolar Disord 2017;19:84‐96. [DOI] [PubMed] [Google Scholar]
- 17. Kyrgiou M, Kalliala I, Markozannes G et al. Adiposity and cancer at major anatomical sites: umbrella review of the literature. BMJ 2017;356:j477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dragioti E, Karathanos V, Gerdle B et al. Does psychotherapy work? An umbrella review of meta‐analyses of randomized controlled trials. Acta Psychiatr Scand 2017;136:236‐46. [DOI] [PubMed] [Google Scholar]
- 19. Markozannes G, Tzoulaki I, Karli D et al. Diet, body size, physical activity and risk of prostate cancer: an umbrella review of the evidence. Eur J Cancer 2016;69:61‐9. [DOI] [PubMed] [Google Scholar]
- 20. Belbasis L, Savvidou MD, Kanu C et al. Birth weight in relation to health and disease in later life: an umbrella review of systematic reviews and meta‐analyses. BMC Med 2016;14:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Belbasis L, Stefanaki I, Stratigos AJ et al. Non‐genetic risk factors for cutaneous melanoma and keratinocyte skin cancers: an umbrella review of meta‐analyses. J Dermatol Sci 2016;84:330‐9. [DOI] [PubMed] [Google Scholar]
- 22. Papageorgiou PN, Deschner J, Papageorgiou SN. Effectiveness and adverse effects of deep brain stimulation: umbrella review of meta‐analyses. J Neurol Surg A Cent Eur Neurosurg 2017;78:180‐90. [DOI] [PubMed] [Google Scholar]
- 23. Bellou V, Belbasis L, Tzoulaki I et al. Systematic evaluation of the associations between environmental risk factors and dementia: an umbrella review of systematic reviews and meta‐analyses. Alzheimers Dement 2017;13:406‐18. [DOI] [PubMed] [Google Scholar]
- 24. Carvalho AF, Kohler CA, Fernandes BS et al. Bias in emerging biomarkers for bipolar disorder. Psychol Med 2016;46:2287‐97. [DOI] [PubMed] [Google Scholar]
- 25. Bellou V, Belbasis L, Tzoulaki I et al. Environmental risk factors and Parkinson's disease: an umbrella review of meta‐analyses. Parkinsonism Relat Disord 2016;23:1‐9. [DOI] [PubMed] [Google Scholar]
- 26. Belbasis L, Bellou V, Evangelou E. Environmental risk factors and amyotrophic lateral sclerosis: an umbrella review and critical assessment of current evidence from systematic reviews and meta‐analyses of observational studies. Neuroepidemiology 2016;46:96‐105. [DOI] [PubMed] [Google Scholar]
- 27. Belbasis L, Bellou V, Evangelou E et al. Environmental risk factors and multiple sclerosis: an umbrella review of systematic reviews and meta‐analyses. Lancet Neurol 2015;14:263‐73. [DOI] [PubMed] [Google Scholar]
- 28. Tsilidis KK, Kasimis JC, Lopez DS et al. Type 2 diabetes and cancer: umbrella review of meta‐analyses of observational studies. BMJ 2015;350:g7607. [DOI] [PubMed] [Google Scholar]
- 29. Theodoratou E, Tzoulaki I, Zgaga L et al. Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta‐analyses of observational studies and randomised trials. BMJ 2014;348:g2035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tonelli AR, Zein J, Adams J et al. Effects of interventions on survival in acute respiratory distress syndrome: an umbrella review of 159 published randomized trials and 29 meta‐analyses. Intensive Care Med 2014;40:769‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ioannidis JP, Zhou Y, Chang CQ et al. Potential increased risk of cancer from commonly used medications: an umbrella review of meta‐analyses. Ann Oncol 2014;25:16‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Doufas AG, Panagiotou OA, Ioannidis JP. Concordance of sleep and pain outcomes of diverse interventions: an umbrella review. PLoS One 2012;7:e40891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Contopoulos‐Ioannidis DG, Ioannidis JP. Claims for improved survival from systemic corticosteroids in diverse conditions: an umbrella review. Eur J Clin Invest 2012;42:233‐44. [DOI] [PubMed] [Google Scholar]
- 34. Fleischhacker WW. A meta view on meta‐analyses. JAMA Psychiatry 2017;74:684‐5. [DOI] [PubMed] [Google Scholar]
- 35. Ioannidis JPA. Integration of evidence from multiple meta‐analyses: a primer on umbrella reviews, treatment networks and multiple treatments meta‐analyses. CMAJ 2009;181:488‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Geddes JR, Verdoux H, Takei N et al. Schizophrenia and complications of pregnancy and labor: an individual patient data meta‐analysis. Schizophr Bull 1999;25:413‐23. [DOI] [PubMed] [Google Scholar]
- 37. Cannon M, Jones PB, Murray RM. Obstetric complications and schizophrenia: historical and meta‐analytic review. Am J Psychiatry 2002;159:1080‐92. [DOI] [PubMed] [Google Scholar]
- 38. Woodberry KA, Giuliano AJ, Seidman LJ. Premorbid IQ in schizophrenia: a meta‐analytic review. Am J Psychiatry 2008;165:579‐87. [DOI] [PubMed] [Google Scholar]
- 39. Khandaker GM, Barnett JH, White IR et al. A quantitative meta‐analysis of population‐based studies of premorbid intelligence and schizophrenia. Schizophr Res 2011;132:220‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cai L, Wan CL, He L et al. Gestational influenza increases the risk of psychosis in adults. Med Chem 2015;11:676‐82. [DOI] [PubMed] [Google Scholar]
- 41. Selten J‐P, Termorshuizen F. The serological evidence for maternal influenza as risk factor for psychosis in offspring is insufficient: critical review and meta‐analysis. Schizophr Res 2017;183:2‐9. [DOI] [PubMed] [Google Scholar]
- 42. Tarbox SI, Pogue‐Geile MF. Development of social functioning in preschizophrenia children and adolescents: a systematic review. Psychol Bull 2008;134:561‐83. [DOI] [PubMed] [Google Scholar]
- 43. Matheson SL, Vijayan H, Dickson H et al. Systematic meta‐analysis of childhood social withdrawal in schizophrenia, and comparison with data from at‐risk children aged 9‐14 years. J Psychiatr Res 2013;47:1061‐8. [DOI] [PubMed] [Google Scholar]
- 44. Schizophrenia Working Group of the Psychiatric Genomics Consortium . Biological insights from 108 schizophrenia‐associated genetic loci. Nature 2014;511:421‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. O'Dushlaine C, Rossin L, Lee PH et al. Psychiatric genome‐wide association study analyses implicate neuronal, immune and histone pathways. Nat Neurosci 2015;18:199‐209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Xu T, Chan RCK, Compton MT. Minor physical anomalies in patients with schizophrenia, unaffected first‐degree relatives, and healthy controls: a meta‐analysis. PLoS One 2011;6:e24129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hirnstein M, Hugdahl K. Excess of non‐right‐handedness in schizophrenia: meta‐analysis of gender effects and potential biases in handedness assessment. Br J Psychiatry 2014;205:260‐7. [DOI] [PubMed] [Google Scholar]
- 48. Golembo‐Smith S, Walder DJ, Daly MP et al. The presentation of dermatoglyphic abnormalities in schizophrenia: a meta‐analytic review. Schizophr Res 2012;142:1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Neelam K, Garg D, Marshall M. A systematic review and meta‐analysis of neurological soft signs in relatives of people with schizophrenia. BMC Psychiatry 2011;11:139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Christesen HT, Elvander C, Lamont RF et al. The impact of vitamin D in pregnancy on extraskeletal health in children: a systematic review. Acta Obstet Gynecol Scand 2012;91:1368‐80. [DOI] [PubMed] [Google Scholar]
- 51. Moher D, Liberati A, Tetzlaff J et al. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006‐12. [DOI] [PubMed] [Google Scholar]
- 52. Stroup DF, Berlin JA, Morton SC et al. Meta‐analysis of observational studies in epidemiology ‐ a proposal for reporting. JAMA 2000;283:2008‐12. [DOI] [PubMed] [Google Scholar]
- 53. Bourque F, van der Ven E, Malla A. A meta‐analysis of the risk for psychotic disorders among first‐ and second‐generation immigrants. Psychol Med 2011;41:897‐910. [DOI] [PubMed] [Google Scholar]
- 54. Varese F, Smeets F, Drukker M et al. Childhood adversities increase the risk of psychosis: a meta‐analysis of patient‐control, prospective‐ and cross‐sectional cohort studies. Schizophr Bull 2012;38:661‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kinney DK, Teixeira P, Hsu D et al. Relation of schizophrenia prevalence to latitude, climate, fish consumption, infant mortality, and skin color: a role for prenatal vitamin D deficiency and infections? Schizophr Bull 2009;35:582‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Saha S, Chant D, Welham J et al. A systematic review of the prevalence of schizophrenia. PLoS Med 2005;2:413‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Rohatgi A. WebPlotDigitizer 3.10. arohatgi.info/WebPlotDigitizer/.
- 58. Shea BJ, Grimshaw JM, Wells GA et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 2007;7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Shea BJ, Bouter LM, Peterson J et al. External validation of a measurement tool to assess systematic reviews (AMSTAR). PLoS One 2007;2:e1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Pieper D, Mathes T, Eikermann M. Can AMSTAR also be applied to systematic reviews of non‐randomized studies? BMC Res Notes 2014;7:609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. R Development Core Team . R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing, 2011. [Google Scholar]
- 62. Higgins JPT, Green S. (eds). Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration, 2011. [Google Scholar]
- 63. Moberg P, Kamath V, Marchetto D et al. Meta‐analysis of olfactory function in schizophrenia, first‐degree family members, and youths at‐risk for psychosis. Schizophr Bull 2014;40:50‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Rubia K, Alegria AA, Cubillo AI et al. Effects of stimulants on brain function in attention‐deficit/hyperactivity disorder: a systematic review and meta‐analysis. Biol Psychiatry 2014;76:616‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Schwarzer G. Meta: an R package for meta‐analysis. R News 2007;7:40‐5. [Google Scholar]
- 66. Higgins JPT, Thompson SG, Spiegelhalter DJ. A re‐evaluation of random‐effects meta‐analysis. J R Stat Soc A Stat 2009;172:137‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Jackson D, Kirkbride J, Croudace T et al. Meta‐analytic approaches to determine gender differences in the age‐incidence characteristics of schizophrenia and related psychoses. Int J Methods Psychiatr Res 2013;22:36‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Egger M, Smith GD, Schneider M et al. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Ioannidis JPA, Trikalinos TA. An exploratory test for an excess of significant findings. Clin Trials 2007;4:245‐53. [DOI] [PubMed] [Google Scholar]
- 70. Chinn S. A simple method for converting an odds ratio to effect size for use in meta‐analysis. Stat Med 2000;19:3127‐31. [DOI] [PubMed] [Google Scholar]
- 71. Bosqui TJ, Hoy K, Shannon C. A systematic review and meta‐analysis of the ethnic density effect in psychotic disorders. Soc Psychiatry Psychiatr Epidemiol 2014;49:519‐29. [DOI] [PubMed] [Google Scholar]
- 72. Torrey EF, Buka S, Cannon TD et al. Paternal age as a risk factor for schizophrenia: how important is it? Schizophr Res 2009;114:1‐5. [DOI] [PubMed] [Google Scholar]
- 73. Kwok W. Is there evidence that social class at birth increases risk of psychosis? A systematic review. Int J Soc Psychiatry 2014;60:801‐8. [DOI] [PubMed] [Google Scholar]
- 74. O'Donoghue B, Roche E, Lane A. Neighbourhood level social deprivation and the risk of psychotic disorders: a systematic review. Soc Psychiatry Psychiatr Epidemiol 2016;51:941‐50. [DOI] [PubMed] [Google Scholar]
- 75. Rasic D, Hajek T, Alda M et al. Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: a meta‐analysis of family high‐risk studies. Schizophr Bull 2014;40:28‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Tortelli A, Errazuriz A, Croudace T et al. Schizophrenia and other psychotic disorders in Caribbean‐born migrants and their descendants in England: systematic review and meta‐analysis of incidence rates, 1950–2013. Soc Psychiatry Psychiatr Epidemiol 2015;50:1039‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. van der Ven E, Veling W, Tortelli A et al. Evidence of an excessive gender gap in the risk of psychotic disorder among North African immigrants in Europe: a systematic review and meta‐analysis. Soc Psychiatry Psychiatr Epidemiol 2016;51:1603‐13. [DOI] [PubMed] [Google Scholar]
- 78. Vassos E, Pedersen CB, Murray RM et al. Meta‐analysis of the association of urbanicity with schizophrenia. Schizophr Bull 2012;38:1118‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Davies G, Welham J, Chant D et al. A systematic review and meta‐analysis of Northern Hemisphere season of birth studies in schizophrenia. Schizophr Bull 2003;29:587‐93. [DOI] [PubMed] [Google Scholar]
- 80. McGrath JJ, Welham JL. Season of birth and schizophrenia: a systematic review and meta‐analysis of data from the Southern Hemisphere. Schizophr Res 1999;35:237‐42. [DOI] [PubMed] [Google Scholar]
- 81. Geddes JR, Lawrie SM. Obstetric complications and schizophrenia: a meta‐analysis. Br J Psychiatry 1995;167:786‐93. [DOI] [PubMed] [Google Scholar]
- 82. Van Lieshout RJ, Taylor VH, Boyle MH. Pre‐pregnancy and pregnancy obesity and neurodevelopmental outcomes in offspring: a systematic review. Obes Rev 2011;12:e548‐59. [DOI] [PubMed] [Google Scholar]
- 83. Arias I, Sorlozano A, Villegas E et al. Infectious agents associated with schizophrenia: a meta‐analysis. Schizophr Res 2012;136:128‐36. [DOI] [PubMed] [Google Scholar]
- 84. Attademo L, Bernardini F, Garinella R et al. Environmental pollution and risk of psychotic disorders: a review of the science to date. Schizophr Res 2017;181:55‐9. [DOI] [PubMed] [Google Scholar]
- 85. Beards S, Gayer‐Anderson C, Borges S et al. Life events and psychosis: a review and meta‐analysis. Schizophr Bull 2013;39:740‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Clancy MJ, Clarke MC, Connor DJ et al. The prevalence of psychosis in epilepsy; a systematic review and meta‐analysis. BMC Psychiatry 2014;14:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Cunningham T, Hoy K, Shannon C. Does childhood bullying lead to the development of psychotic symptoms? A meta‐analysis and review of prospective studies. Psychosis 2015;8:48‐59. [Google Scholar]
- 88. de Sousa P, Varese F, Sellwood W et al. Parental communication and psychosis: a meta‐analysis. Schizophr Bull 2014;40:756‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Gurillo P, Jauhar S, Murray RM et al. Does tobacco use cause psychosis? Systematic review and meta‐analysis. Lancet Psychiatry 2015;2:718‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Gutierrez‐Fernandez J, de Dios Luna del Castillo J, Mananes‐Gonzalez S et al. Different presence of Chlamydia pneumoniae, herpes simplex virus type 1, human herpes virus 6, and Toxoplasma gondii in schizophrenia: meta‐analysis and analytical study. Neuropsychiatr Dis Treat 2015;11:843‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Khandaker GM, Zimbron J, Dalman C et al. Childhood infection and adult schizophrenia: a meta‐analysis of population‐based studies. Schizophr Res 2012;139:161‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Linszen MMJ, Brouwer RM, Heringa SM et al. Increased risk of psychosis in patients with hearing impairment: review and meta‐analyses. Neurosci Biobehav Rev 2016;62:1‐20. [DOI] [PubMed] [Google Scholar]
- 93. Marconi A, Di Forti M, Lewis CM et al. Meta‐analysis of the association between the level of cannabis use and risk of psychosis. Schizophr Bull 2016;42:1262‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Molloy C, Conroy RM, Cotter DR et al. Is traumatic brain injury a risk factor for schizophrenia? A meta‐analysis of case‐controlled population‐based studies. Schizophr Bull 2011;37:1104‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Sutterland AL, Fond G, Kuin A et al. Beyond the association. Toxoplasma gondii in schizophrenia, bipolar disorder, and addiction: systematic review and meta‐analysis. Acta Psychiatr Scand 2015;132:161‐79. [DOI] [PubMed] [Google Scholar]
- 96. Dickson H, Laurens KR, Cullen AE et al. Meta‐analyses of cognitive and motor function in youth aged 16 years and younger who subsequently develop schizophrenia. Psychol Med 2012;42:743‐55. [DOI] [PubMed] [Google Scholar]
- 97. Filatova S, Koivumaa‐Honkanen H, Hirvonen N et al. Early motor developmental milestones and schizophrenia: a systematic review and meta‐analysis. Schizophr Res 2017;188:13‐20. [DOI] [PubMed] [Google Scholar]
- 98. Fusar‐Poli P, Cappucciati M, Rutigliano G et al. At risk or not at risk? A meta‐analysis of the prognostic accuracy of psychometric interviews for psychosis prediction. World Psychiatry 2015;14:322‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Kaymaz N, Drukker M, Lieb R et al. Do subthreshold psychotic experiences predict clinical outcomes in unselected non‐help‐seeking population‐based samples? A systematic review and meta‐analysis, enriched with new results. Psychol Med 2012;42:2239‐53. [DOI] [PubMed] [Google Scholar]
- 100. Koning JPF, Tenback DE, van Os J et al. Dyskinesia and Parkinsonism in antipsychotic‐naive patients with schizophrenia, first‐degree relatives and healthy controls: a meta‐analysis. Schizophr Bull 2010;36:723‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Ohi K, Hashimoto R, Yasuda Y et al. Personality traits and schizophrenia: evidence from a case‐control study and meta‐analysis. Psychiatry Res 2012;198:7‐11. [DOI] [PubMed] [Google Scholar]
- 102. Ohi K, Shimada T, Nitta Y et al. The Five‐Factor Model personality traits in schizophrenia: a meta‐analysis. Psychiatry Res 2016;240:34‐41. [DOI] [PubMed] [Google Scholar]
- 103. Potvin S, Marchand S. Hypoalgesia in schizophrenia is independent of antipsychotic drugs: a systematic quantitative review of experimental studies. Pain 2008;138:70‐8. [DOI] [PubMed] [Google Scholar]
- 104. Ward KE, Friedman L, Wise A et al. Meta‐analysis of brain and cranial size in schizophrenia. Schizophr Res 1996;22:197‐213. [DOI] [PubMed] [Google Scholar]
- 105. Yan C, Cao Y, Zhang Y et al. Trait and state positive emotional experience in schizophrenia: a meta‐analysis. PLoS One 2012;7:e40672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Selten JP, Cantor‐Graae E, Nahon D et al. No relationship between risk of schizophrenia and prenatal exposure to stress during the Six‐Day War or Yom Kippur War in Israel. Schizophr Res 2003;63:131‐5. [DOI] [PubMed] [Google Scholar]
- 107. O'Rourke K. An historical perspective on meta‐analysis: dealing quantitatively with varying study results. J Roy Soc Med 2007;100:579‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Fusar‐Poli P, Borgwardt S, Bechdolf A et al. The psychosis high‐risk state: a comprehensive state‐of‐the‐art review. JAMA Psychiatry 2013;70:107‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Fusar‐Poli P, Rutigliano G, Stahl D et al. Long‐term validity of the At Risk Mental State (ARMS) for predicting psychotic and non‐psychotic mental disorders. Eur Psychiatry 2017;42:49‐54. [DOI] [PubMed] [Google Scholar]
- 110. Kempton MJ, Bonoldi I, Valmaggia L et al. Speed of psychosis progression in people at ultra‐high clinical risk: a complementary meta‐analysis. JAMA Psychiatry 2015;72:622‐3. [DOI] [PubMed] [Google Scholar]
- 111. Fusar‐Poli P, Cappucciati M, De Micheli A et al. Diagnostic and prognostic significance of brief limited intermittent psychotic symptoms (BLIPS) in individuals at ultra high risk. Schizophr Bull 2017;43:48‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Fusar‐Poli P, Cappucciati M, Bonoldi I et al. Prognosis of brief psychotic episodes: a meta‐analysis. JAMA Psychiatry 2016;73:211‐20. [DOI] [PubMed] [Google Scholar]
- 113. Falkenberg I, Valmaggia L, Byrnes M et al. Why are help‐seeking subjects at ultra‐high risk for psychosis help‐seeking? Psychiatry Res 2015;228:808‐15. [DOI] [PubMed] [Google Scholar]
- 114. Fusar‐Poli P, Rocchetti M, Sardella A et al. Disorder, not just state of risk: meta‐analysis of functioning and quality of life in people at high risk of psychosis. Br J Psychiatry 2015;207:198‐206. [DOI] [PubMed] [Google Scholar]
- 115. Fusar‐Poli P, Cappucciati M, Borgwardt S et al. Heterogeneity of psychosis risk within individuals at clinical high risk: a meta‐analytical stratification. JAMA Psychiatry 2016;73:113‐20. [DOI] [PubMed] [Google Scholar]
- 116. Fusar‐Poli P, Cappucciati M, Rutigliano G et al. Towards a standard psychometric diagnostic interview for subjects at ultra high risk of psychosis: CAARMS versus SIPS. Psychiatry J 2016;2016:7146341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Fusar‐Poli P, Tantardini M, De Simone S et al. Deconstructing vulnerability for psychosis: meta‐analysis of environmental risk factors for psychosis in subjects at ultra high‐risk. Eur Psychiatry 2017;40:65‐75. [DOI] [PubMed] [Google Scholar]
- 118. Fusar‐Poli P, Rutigliano G, Stahl D et al. Deconstructing pretest risk enrichment to optimize prediction of psychosis in individuals at clinical high risk. JAMA Psychiatry 2016;73:1260‐7. [DOI] [PubMed] [Google Scholar]
- 119. Fusar‐Poli P, Schultze‐Lutter F, Cappucciati M et al. The dark side of the moon: meta‐analytical impact of recruitment strategies on risk enrichment in the clinical high risk state for psychosis. Schizophr Bull 2016;42:732‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Fusar‐Poli P, Schultze‐Lutter F, Addington J. Intensive community outreach for those at ultra high risk of psychosis: dilution, not solution. Lancet Psychiatry 2016;3:18. [DOI] [PubMed] [Google Scholar]
- 121. Fusar‐Poli P, Palombini E, Davies C et al. Why transition risk to psychosis is not declining at the OASIS ultra high risk service: the hidden role of stable pretest risk enrichment. Schizophr Res (in press). [DOI] [PubMed] [Google Scholar]
- 122. Fusar‐Poli P. Why ultra high risk criteria for psychosis prediction do not work well outside clinical samples and what to do about it. World Psychiatry 2017;16:212‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Kirkbride J, Hameed Y, Ankireddypalli G et al. The epidemiology of first‐episode psychosis in early intervention in psychosis services: findings from the Social Epidemiology of Psychoses in East Anglia [SEPEA] Study. Am J Psychiatry 2017;174:143‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Heinz A, Deserno L, Reininghaus U. Urbanicity, social adversity and psychosis. World Psychiatry 2013;12:187‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Selten J‐P, van Os J, Cantor‐Graae E. The social defeat hypothesis of schizophrenia: issues of measurement and reverse causality. World Psychiatry 2016;15:294‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Mizrahi R. Social stress and psychosis risk: common neurochemical substrates? Neuropsychopharmacology 2016;41:666‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Holtzman CW, Trotman HD, Goulding SM et al. Stress and neurodevelopmental processes in the emergence of psychosis. Neuroscience 2013;249:172‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Steinheuser V, Ackermann K, Schonfeld P et al. Stress and the city: impact of urban upbringing on the (re)activity of the hypothalamus‐pituitary‐adrenal axis. Psychosom Med 2014;76:678‐85. [DOI] [PubMed] [Google Scholar]
- 129. Mewes R, Reich H, Skoluda N et al. Elevated hair cortisol concentrations in recently fled asylum seekers in comparison to permanently settled immigrants and non‐immigrants. Transl Psychiatry 2017;7:e1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Powell ND, Sloan EK, Bailey MT et al. Social stress up‐regulates inflammatory gene expression in the leukocyte transcriptome via beta‐adrenergic induction of myelopoiesis. Proc Natl Acad Sci USA 2013;110:16574‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Akdeniz C, Tost H, Streit F et al. Neuroimaging evidence for a role of neural social stress processing in ethnic minority‐associated environmental risk. JAMA Psychiatry 2014;71:672‐80. [DOI] [PubMed] [Google Scholar]
- 132. Lederbogen F, Kirsch P, Haddad L et al. City living and urban upbringing affect neural social stress processing in humans. Nature 2011;474:498‐501. [DOI] [PubMed] [Google Scholar]
- 133. Haddad L, Schafer A, Streit F et al. Brain structure correlates of urban upbringing, an environmental risk factor for schizophrenia. Schizophr Bull 2015;41:115‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Selten JP, Booij J, Buwalda B et al. Biological mechanisms whereby social exclusion may contribute to the etiology of psychosis: a narrative review. Schizophr Bull (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Egerton A, Howes OD, Houle S et al. Elevated striatal dopamine function in immigrants and their children: a risk mechanism for psychosis. Schizophr Bull 2017;43:293‐301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Frissen A, van Os J, Habets P et al. No evidence of association between childhood urban environment and cortical thinning in psychotic disorder. PLoS One 2017;12:e0166651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Keskinen E, Marttila R, Koivumaa‐Honkanen H et al. Search for protective factors for psychosis ‐ a population‐based sample with special interest in unaffected individuals with parental psychosis. Early Interv Psychiatry (in press). [DOI] [PubMed] [Google Scholar]
- 138. Millan MJ, Andrieux A, Bartzokis G et al. Altering the course of schizophrenia: progress and perspectives. Nat Rev Drug Discov 2016;15:485‐515. [DOI] [PubMed] [Google Scholar]
- 139. Uher R, Zwicker A. Etiology in psychiatry: embracing the reality of poly‐gene‐environmental causation of mental illness. World Psychiatry 2017;16:121‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Vassos E, Di Forti M, Coleman J et al. An examination of polygenic score risk prediction in individuals with first episode psychosis. Biol Psychiatry 2016;81:470‐7. [DOI] [PubMed] [Google Scholar]
- 141. Fusar‐Poli P, Rutigliano G, Stahl D et al. Development and validation of a clinically based risk calculator for the transdiagnostic prediction of psychosis. JAMA Psychiatry 2017;74:493‐500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Iyegbe C, Campbell D, Butler A et al. The emerging molecular architecture of schizophrenia, polygenic risk scores and the clinical implications for GxE research. Soc Psychiatry Psychiatr Epidemiol 2014;49:169‐82. [DOI] [PubMed] [Google Scholar]
- 143. Hartley S, Barrowclough C, Haddock G. Anxiety and depression in psychosis: a systematic review of associations with positive psychotic symptoms. Acta Psychiatr Scand 2013;128:327‐46. [DOI] [PubMed] [Google Scholar]
- 144. Mishara AL, Fusar‐Poli P. The phenomenology and neurobiology of delusion formation during psychosis onset: Jaspers, Truman symptoms, and aberrant salience. Schizophr Bull 2013;39:278‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Achim AM, Maziade M, Raymond E et al. How prevalent are anxiety disorders in schizophrenia? A meta‐analysis and critical review on a significant association. Schizophr Bull 2011;37:811‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Newton‐Howes G, Tyrer P, North B et al. The prevalence of personality disorder in schizophrenia and psychotic disorders: systematic review of rates and explanatory modelling. Psychol Med 2008;38:1075‐82. [DOI] [PubMed] [Google Scholar]
- 147. Gumley AI, Taylor HEF, Schwannauer M et al. A systematic review of attachment and psychosis: measurement, construct validity and outcomes. Acta Psychiatr Scand 2014;129:257‐74. [DOI] [PubMed] [Google Scholar]
- 148. Large M, Sharma S, Compton MT et al. Cannabis use and earlier onset of psychosis. Arch Gen Psychiatry 2011;68:555‐61. [DOI] [PubMed] [Google Scholar]
- 149. Murray RM, Quigley H, Quattrone D et al. Traditional marijuana, high‐potency cannabis and synthetic cannabinoids: increasing risk for psychosis. World Psychiatry 2016;15:195‐204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Bramness JG, Rognli EB. Psychosis induced by amphetamines. Curr Opin Psychiatry 2016;29:236‐41. [DOI] [PubMed] [Google Scholar]
- 151. Roncero C, Ros‐Cucurull E, Daigre C et al. Prevalence and risk factors of psychotic symptoms in cocaine‐dependent patients. Actas Esp Psiquiatr 2012;40:187‐97. [PubMed] [Google Scholar]
- 152. Reeve S, Sheaves B, Freeman D. The role of sleep dysfunction in the occurrence of delusions and hallucinations: a systematic review. Clin Psychol Rev 2015;42:96‐115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Folsom D, Jeste DV. Schizophrenia in homeless persons: a systematic review of the literature. Acta Psychiatr Scand 2002;105:404‐13. [DOI] [PubMed] [Google Scholar]
- 154. Padgett FE, Miltsiou E, Tiffin PA. The co‐occurrence of nonaffective psychosis and the pervasive developmental disorders: a systematic review. J Intellect Dev Disabil 2010;35:187‐98. [DOI] [PubMed] [Google Scholar]
- 155. Ioannidis JP. The mass production of redundant, misleading, and conflicted systematic reviews and meta‐analyses. Milbank Q 2016;94:485‐514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Siontis KC, Hernandez‐Boussard T, Ioannidis JP. Overlapping meta‐analyses on the same topic: survey of published studies. BMJ 2013;347:f4501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Millan MJ. An epigenetic framework for neurodevelopmental disorders: from pathogenesis to potential therapy. Neuropharmacology 2013;68:2‐82. [DOI] [PubMed] [Google Scholar]


