Abstract
Introduction
Rehabilitation measures for patients in the working age primarily aim at maintaining employability, restoring fitness for work or timely return to work (RTW). To facilitate RTW after long sick leave in Germany, both rehabilitation physicians' knowledge about the patients' workplace and communication between the rehabilitation physician and the occupational physician need to be improved. This research will record the experiences and attitudes of occupational physicians, rehabilitation physicians and general practitioners, as well as of rehabilitation patients, to indicate barriers and possibilities for improvement concerning the intersection between workplace and rehabilitation institution. As a previous literature review has shown, insufficient data on the experiences and attitudes of the stakeholders are available. Therefore, an exploratory qualitative approach was chosen.
Methods and analysis
8 focus group discussions will be conducted with occupational physicians, rehabilitation physicians, general practitioners and rehabilitation patients (2 focus groups with 6–8 interviewees per category). Qualitative content analysis will be used to evaluate the data, thus describing positive and negative experiences and attitudes, barriers and possibilities for improvement at the intersection of general and occupational medicine and rehabilitation with regard to the workplace. The data from the focus groups will be used to develop a standardised quantitative questionnaire for a survey of the medical groups and rehabilitation patients in a follow-up project.
Ethics and dissemination
The research will be undertaken with the approval of the Ethics Committee of the Medical Faculty and University Hospital of Tuebingen. The study participants’ consent will be documented in written form. The names of all study participants and all other confidential information data fall under medical confidentiality. The results will be published in a peer-reviewed medical journal independent of the nature of the results.
Keywords: QUALITATIVE RESEARCH, REHABILITATION MEDICINE, Interdisciplinary cooperation, Health services research, OCCUPATIONAL & INDUSTRIAL MEDICINE, Return to Work
Strengths and limitations of this study.
A strength of this qualitative study is that we will include the perspectives of both the main medical stakeholders (rehabilitation physicians, general practitioners, occupational health physicians) and the rehabilitants.
We will strive to attain a maximal structural heterogeneity of participants in the focus group discussions in order to reflect the diversity of ideas and perceptions within the study population.
A limitation of qualitative studies in general is that the results are not statistically generalisable or representative of the population as a whole.
A limitation of the study is that, owing to resource and time constraints, not all stakeholders who are directly or indirectly involved in rehabilitation (ie, relatives of patients, representatives of funding agencies) can be invited for additional focus group discussions.
Background
In the past decades, a steady increase in rehabilitation treatments has been observed in Germany.1 2 This increase is driven inter alia by demographic evolution, social objectives to extend retirement age, the changing spectrum of disease, an increase in chronic diseases and a changing workforce. For most members of society, the ability to work is the foundation of a self-determined and responsible existence. Rehabilitation links prevention, therapy and post-treatment care and aims to provide rapid and sustainable return to work (RTW) of the patient.
The rehabilitative healthcare system in Germany is an example of a highly segmented structure in which multiple protagonists fulfil different roles.1 The existing and still increasing relevancy of rehabilitation itself therefore underlines the importance of well-functioning intersections in the rehabilitation process as well.1–4
Intersections in complex social systems are points of transition where organisational responsibilities, specific occupational competencies and delivered services end and are in need of cooperative supplementation and continuation. In healthcare, these intersections can be characterised and potentially optimised by health services research.5–7 Such intersections also exist in German rehabilitation processes, due to often complex goals, as well as the German sectoral health service system.8 In this system, each sector acts according to its own goals and priorities. The rehabilitation process is thus rather challenging, since those involved are not always familiar with the specifics of every sector of the healthcare system. Furthermore, protagonists outside the healthcare system (eg, family and employers) also play an important role in the process.8
From a positivist stance, intersections are transition points between segments of care and thus constitute an opportunity for specialisation and performance refinement. Intersections can, however, also induce interference in the effective delivery of healthcare.
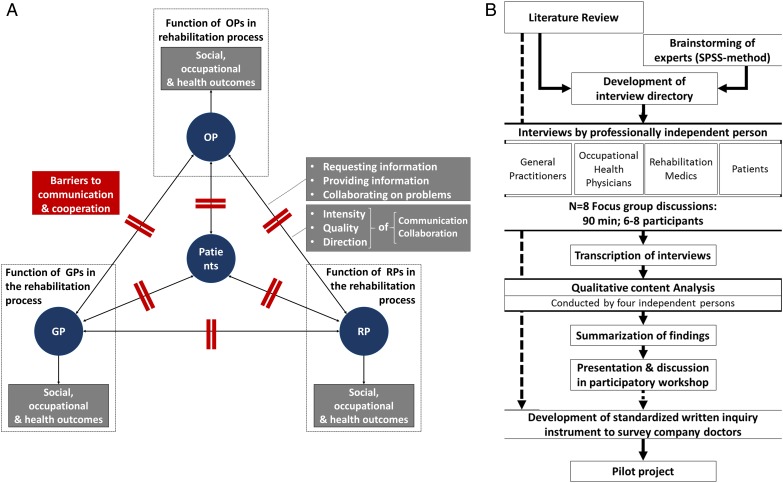
The main medical protagonists in the German rehabilitation system are general practitioners (GPs), rehabilitation physicians (RPs) and occupational health physicians (OPs).3 Each professional group fulfils a specific function in the rehabilitation process, which depends on or may be improved through collaboration and information flow to achieve social, occupational and health outcomes for the patients. Barriers to communication and cooperation between the protagonists may therefore lead to patients not receiving the best treatment possible.9
Figure 1A describes the intersections in the rehabilitation process between patients and the groups of medical stakeholders involved in our study.
Figure 1.
(A) Framework of cooperation between the stakeholders. Framework of cooperation, communication and information flow between the stakeholders involved in the qualitative study. The medical stakeholders (OPs, RPs and GPs) fulfil different functions in the rehabilitation system in order to achieve social, occupational or health outcomes. The professional groups interact in the process through collaboration and communication which can be characterised by its intensity, quality and the direction of interaction. The information flow and collaboration may be obstructed by barriers. (B) Flow chart of the study design. A literature search and the input of context experts were used to develop the interview guide used in the focus groups. A transcription of the focus group discussions will be used for quality content analysis and will be presented for content validation in a participatory workshop. GP, general practitioner; OP, occupational physician; RP, rehabilitation physician.
In the German rehabilitation system, GPs screen for patients, initiate and support the application process, provide preliminary medical information to the RPs, prepare the patients and are responsible for the postrehabilitation follow-up. The follow-up includes prescribing medication and treatments, issuing medical sickness certificates and evaluating the rehabilitation results. RPs are responsible for the rehabilitation treatment during the rehabilitation process, as well as for assessing the patients' ability to work and need for assisting devices. OPs functions with regard to the rehabilitation process include screening among employees, initiating or supporting the application process, providing RPs with information about the workplace as well as assessing, preparing and discussing the occupational reintegration. OPs can manage the provision of work accommodation (eg, assisting devices), determine the need and possibilities for retraining and job rotation and play a role in the evaluation of the rehabilitation treatment.3 10 11 To improve the intersection between work and rehabilitation, OPs in the German federal state Baden-Württemberg have the opportunity to support the introduction of rehabilitation measures through the local statutory pension insurance. Owing to this development, this federal state seems to be especially suitable to study the intersection of the medical rehabilitation process and the workplace.11
RPs, OPs and GPs complement each other with their specific abilities and institutional competences when it comes to reintegrating rehabilitation patients into the workforce. An intensive transfer of information between these medical groups concerning the entire rehabilitation process can help to approach the goals of the rehabilitation measures.8 12–14 OPs, GPs and RPs agree that an efficient cooperation at the intersections is necessary for successful medical rehabilitation and RTW. Therefore, cooperation and communication need to be strengthened, according to these protagonists.15–23
One intersection between the protagonists is the therapeutic strategy of graded RTW. The RP develops a scheme in which the patient starts to work with reduced working hours a day, based on his or her condition, which gradually are increased until the employee is able for a full RTW. Since this strategy needs the consent of the employee, the employer, the funding agency and the treating physician, it constitutes an intersection with the opportunity to link efforts of occupational healthcare and rehabilitation services. Studies found this intervention to be successful as a work rehabilitation strategy (ie, in regard to time to RTW).8 24–28
International literature reviews have revealed factors which had a positive influence on the occupational health of patients (eg, in regard to reduced sick leave and time to first RTW). The authors of these studies conclude that there is a moderate-to-strong evidence basis for interventions like: individualised rehabilitation adjusted for the demands of a specific workplace, providing work accommodations, early contact of the worker with the workplace and contact of the healthcare provider with the patients' workplace.24 29–35 In the German healthcare system, most of these aspects lie within the responsibility of OPs. Multidisciplinary RTW strategies as part of the rehabilitation treatment have been found to be successful in terms of occupational health outcomes.24 36–38 For the setting of the German rehabilitation process, studies have indicated that improved cooperation in the rehabilitation process, and especially the inclusion of OPs, is beneficial in improving the occupational health of patients.14 25–27 33
Barriers for successful RTW often include RPs' insufficient understanding of the patients’ workplace, as well as inadequate transfer of information between the RP and the occupational physician.8 9 14 23 39 40 Furthermore, privacy regulations require the communication between RPs and OPs to be authorised by the patients. Sometimes they are reluctant to give the necessary permission.22 39–41 So a deeper understanding of patients' attitudes towards OPs may be crucial to improve the RTW process.
However, although studies continue to show benefits of cooperating with OPs, other studies continue to draw the picture of a structural exclusion of OPs from the rehabilitation process. A low intensity of communication and cooperation between OPs and RPs has been shown in surveys from involving RPs,22 23 40 42 OPs23 40–42 and rehabilitants43 from Austria,23 the Netherlands,22 40 Belgium23 and Germany.41–43 Studies from Germany especially emphasised this structural exclusion of OPs from the rehabilitation process.41–43 In a survey among German OPs (n=293), 93% reported that only seldom cooperation with rehabilitation clinics took place.41 Other studies underlined the survey findings, for example, by stating that systematic communication between RPs and OPs would not take place on a regular basis or that OPs often receive information on their patients’ rehabilitation treatment months after the discharge, if at all.14
We conduct this study to better understand the discrepancy between the current structural exclusion of OPs from the rehabilitation process, and the possible benefits which improved cooperation with OPs would confer. The approach of this study is to survey both medical actors (OPs, RPs, GPs) and rehabilitation patients regarding their experiences, attitudes and perceived opportunities for improvement of the workplace–rehabilitation interface. The aim of this study is to determine the potential for improvement in the cooperation between OPs and RPs as well as between OPs and GPs. We also aim at determining the potential for a consequent improved RTW process overall.
Methods/design
On the basis of the Medical Research Council (MRC) recommendations,44 we will conduct an exploratory qualitative approach to analyse the need for improvement descriptively. Within the scope of our methods, we can identify what the stakeholders involved perceive as limiting and facilitating cooperation at the interfaces.
In a first phase of this project, a qualitative study using focus group discussions (FGDs) will be conducted and the derived data will be analysed using qualitative content analysis.45 In a second phase (which is not part of this study protocol), a standardised quantitative survey for OPs, GPs, RPs and rehabilitants will be developed and tested before implementation in a third phase as a follow-up project.
Research questions
Based on our framework of communication and cooperation between the protagonists involved in our study (figure 1A), the findings of the qualitative surveys of the groups noted above will be used to answer among others the following questions:
- Collaboration and communication:
- How do the medical parties experience and evaluate their cooperation?
- How do the participants experience the information flow between the stakeholders?
- How strong is the cooperation between OPs, RPs and GPs?
- What experiences do rehabilitation patients have with the intersection between OPs, RPs and GPs?
- Effects of communication and cooperation on patients' outcomes:
- How do the medical stakeholders perceive or expect the effect of lacking/improved communication and cooperation on rehabilitation outcomes?
- What do rehabilitants expect from the cooperation between OPs, RPs and GPs?
- Barriers to communication and cooperation:
- What kind of practical advice for the improvement of the intersections can be deduced from the subjective evaluations of the different stakeholders?
- What are the determinants of good cooperation?
- Does the cooperation between protagonists work better when OPs initiate the rehabilitation therapy?
- What opportunities for optimisation do the medical parties and the rehabilitation patients point out?
Work-related medical rehabilitation has gained importance in the German rehabilitation process in recent years, while only a few primary studies on the cooperation of the protagonists have been conducted during the same period.9 39 46 It is therefore possible that the cooperation and communication of protagonists have improved in recent years as well. Consequently, one research question will be:
What kind of changes in communication and cooperation between the main medical stakeholders have the participants experienced in recent years?
Study design
Owing to the scarcity in data, the chosen method for the first study is a qualitative research approach with the aim of gaining particularly detailed insights.47 Qualitative study designs are well established in health services research.48 Since early 2000, health services research in the field of occupational health gained further interest among researchers7 49 and qualitative methods have repeatedly been used successfully to answer research questions related to health and occupation.50–56
With the qualitative approach, the experiences of the respective groups are surveyed in FGDs.57 FGDs are established methods in health services research.58 59 Through thoroughly planned FGDs which are supported by guiding questions,60 perspectives and experiences on the topic can be determined, and insights on the attitudes and perspectives of OPs, RPs, GPs and rehabilitation patients can be gained.57 FGDs offer some advantages compared with individual interviews, for example, that ideas of individuals can be developed further through in-group processes or that group dynamics can generate new thinking about a topic.61–63 Since we aim to identify possibilities for improvement, we perceive these features as useful. To ensure a free and uninterrupted discussion, the four groups involved in the rehabilitation process will be interviewed separately.
The questions for discussions will be developed on the basis of literature reviews9 39 and brainstorming by an interdisciplinary team of scholars through a method that collects, tests, sorts and subsumes questions.64 In a second round, these key questions will be reflected and revised by the research team. This team consists of two occupational medicine scholars (both with experience as OPs), one OP, a rehabilitation researcher and a health services researcher. The guiding questions will be adjusted to appropriately address the different groups of actors or the rehabilitation patients, respectively. The content of the discussions is meant to record questions concerning experiences with and attitudes towards the cooperation of OPs, GPs and RPs in regard to rehabilitation measures for patients in working age and opportunities to optimise them.
A professionally independent person (ie, neither an OP, nor a RP nor a GP) with experience in conducting interviews and familiar with the research topic will lead the four FGDs. The moderator is not going to have any prior established relationship with the patients. Participants will be informed about the moderator's profession, about the aim of the study and about the independency in relation to the research project. We will inform about the moderator's credentials, profession and gender. The FGDs will be ∼90 min long and will be audio taped in their entirety. A complimentary video will be produced to make it easier to assign voices to discussion participants during transcription.
The participants will be notified in writing during the recruitment process that the FGDs are going to be recorded, that these recordings will be transcribed using pseudonyms, and finally evaluated.
The transcribed data of the FGDs will be evaluated using qualitative content analysis.45 This method involves four neutral persons to ensure an intersubjective correlation65 (quality assurance through communicative validation). Prior to the analysis, all persons involved in the analysis will record their expectations, preliminary assumptions, and their own experiences in written form so as not to predetermine the analysis through prior understanding.64 The resulting data will be evaluated using appropriate software (ie, MAXQDA).
The evaluation itself will be both inductive and deductive; inductive out of the material itself and deductive based on general prior knowledge and the guiding questions. First, the persons undertaking the analysis will read the transcript of one FGD separately and determine central themes. To ensure effective subjective understanding and to control for subjective blurring, the analysis will be validated by means of discussion between the two evaluators. The analysis of central themes will be performed sequentially in the first reading, for example, sentence by sentence, paragraph by paragraph. Repeated themes will be reflectively controlled in the ongoing analysis process, developed and finally brought together into categories. The content of the other focus group interviews will then be analysed using the previously developed category system, or the category system will be enhanced by new categories of content as they are encountered. The categories will be given definitions, coding rules and anchor examples to ensure proper assignment.45
In a final step, approaches to overcome or reduce the barriers and to improve the cooperation will be formulated, taking into account the experiences and wishes of the rehabilitation patients.
By means of a qualitative approach, the different groups of actors will be surveyed about optimisation possibilities. The insights gained through all actors will be collected to create practical initial suggestions. Towards the end of the project, these suggestions will be introduced and discussed in a participatory workshop used for content validation. Representatives of OPs, RPs and GPs will be invited to participate in this expert workshop.
The study design is displayed in figure 1B.
Study population
To recruit the focus groups (n=6–8 interview partners), we will contact OPs from the address file of the Association of German factory and company doctors (Verband Deutscher Betriebs-und Werksärzte, VDBW). RPs and rehabilitation patients will be recruited from two institutions (Therapy Center Federsee, Bad Buchau; Rehabilitation Center Bad Duerrheim, Klinik Huettenbuehl). GPs will be contacted from the training-practice lists of the former General Medicine Department of the Medical Faculty, University of Tuebingen.
The FGDs with GPs and OPs will take place at the University Hospital of Tuebingen in our institute in Tuebingen. The FGDs with RPs and rehabilitants will take place in the respective clinic and for RPs in the context of the regularly held meetings for continuing education.
Election and invitation of the study population
For each group, participants as diverse as possible will be selected in accordance with the principle of maximal structural variation,66 to represent the heterogeneity of the research field as accurately as possible. Table 1 shows the constituency of the four collectives.
Table 1.
Planned composition of the four collectives for the focus group interviews
| Two focus groups per category, participants per focus group: n=6–8 | |
|---|---|
| General practitioners |
|
| OPs |
|
| RPs | Rehabilitation centre 1
|
| Rehabilitation patients | Rehabilitation centre 1:
|
Small-sized and medium-sized enterprise based on the EU definition (Commission Recommendation of 6 May 2003 concerning the definition of micro-sized, small-sized and medium-sized enterprises (2003/361/EC)).
EU, European Union; OP, occupational physician; RP, rehabilitation physician.
Election and invitation of GPs
For the group of GPs, primary care physicians, that is, office-based GPs and internists, supporting the work of the Department of General Medicine will be contacted. During the recruitment of the groups, equal representation must be ensured for both sexes, as well as both rural and urban geographic regions. Doctors from practices near to a larger occupational physician service (urban vs rural regions), as well as doctors from practices whose practice is not close to a large company and its particular occupational health service (urban vs rural regions) will be recruited. Furthermore, there will be a differentiation between doctors from individual and group practices. If several GPs will be available, the choice will be determined by the number of rehabilitation patients in care, the size of the practice (number of patients insured through statutory healthy insurance), as well as the years of experience as a GP. If feasible, GPs who also work as OPs will not be included. The invitation of the GPs will be conducted via email out of medical practices associated with the Department for General Medicine in the Medical Faculty of the University of Tuebingen. The GPs will be invited to participate in the FGDs, which will be conducted at the annual advanced training session for GPs at the University Department of Tuebingen.
Election and invitation of OPs
For the group of OPs, we will recruit those who are specialised in company medicine or occupational medicine and who work primarily as OPs. During the creation of the groups, it must be ensured that both sexes and both rural and urban regions will be represented equally. Furthermore, it will be differentiated between (1) OPs working for one business and those working for several businesses; (2) OPs employed by an occupational service provider and those working independently; and (3) OPs with other duties of occupational medicine. If several OPs are available, the choice will be determined by the years of experience as OP.
The OPs will be contacted via telephone. OPs will be informed about the aims of the study, the FGDs and privacy regulations. Unrelated to any actual participation in the study, structural data on the candidate will be recorded for the sampling. The persons not interested in partaking in the study will be asked for their consent to save and use the mostly structural data obtained during the telephone conversation for the study.
Election and invitation of RPs and rehabilitants
One focus group of RPs will be recruited from a medical rehabilitation centre that is specialised on internal, orthopaedic and psychosomatic diseases. The psychosomatic focus includes neurotic, stress-related, somatoform and affective disorders (including depression). Among the physicians specialised in orthopaedic rehabilitation, we will differentiate between the concept of occupational orthopaedic rehabilitation and psychosomatic orthopaedic rehabilitation.
For the other focus group with RPs, RPs will be recruited from a rehabilitation centre that is specialised on diseases in the musculoskeletal system and the respiratory system. For the choice of participating physicians, it will be ensured that the different medical indication groups (musculoskeletal disorders, mental disorders and internal diseases) of both clinics will be represented, that both sexes are represented equally and that doctors with as many different medical specialties as possible can be recruited. Furthermore, RPs with comparatively long professional experience in rehabilitation will be given preference. Using a short survey, a research assistant will conduct the first phone contact to record the characteristics used later for sampling.
We focused on the particular medical rehabilitation centres in order to include patients' suffering from, and physicians working on, disorders most relevant for in-house medical rehabilitation, which are: musculoskeletal disorders (reason of treatment in 34% of all female patients and 31% of all male patients), internal diseases (including oncological, cardiovascular, gastrointestinal, endocrine diseases; 25% among female patients, 30% among male patients), as well as mental disorders (21% among female patients, 13% among male patients).1
Criteria for the choice of rehabilitation patients are an age range of 20–60 years, the intention to gain full occupation after rehabilitation, either new or existing, as well as being in a stationary rehabilitation setting for the first time. Furthermore, the equal representation of sexes and indicators for the rehabilitation treatment (functional restriction and diagnosis) will be ensured in the recruitment process.
Rehabilitation patients will be referred by their attending physicians, who will be in turn previously informed about the study and selected for inclusion. The patients will be informed and asked for their participation in the study. The attending physicians are going to fill out the protocol ‘first contact phone call rehabilitation patient’.
The focus group of rehabilitation patients will meet towards the end of the stationary rehabilitation treatment on weeknights after the daily programmes in both clinics. The patients will be asked to participate in a telephone survey 3 months after the end of their rehabilitation treatment.
Ethics and dissemination
The participation in the study will be voluntary. The consent of the participants can be withdrawn at any given time without a statement of reasons and without detriment in medical care. The nature and scope of the research will be explained to the study participants in written and oral form before onset of the study. Their consent will be documented by their signature on the consent form. The video tapes are going to be destroyed after the pseudonymisation is completed. The patients will additionally be assured that neither participation nor non-participation will be of any detriment to them. In addition, audio tapes will be destroyed no later than 10 years after publication of the study. Until this date, the tapes will remain sealed and only available to the persons involved in this research.
Results from the study will be published, independent of the nature of the results, in scientific peer-reviewed journals, in the PhD theses of the author (JS) and at conferences. Authorship will be granted only to those who fulfil the authorship criteria recommended by the International Committee of Medical Journal Editors. We will report the results using the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist.67
Conclusion
This qualitative study will use FGDs with OPs, RPs and GPs, as well as rehabilitation patients to explore experiences and attitudes in order to describe barriers and possibilities for improvement concerning the intersection between the workplace and rehabilitation institutions. We want to better understand the discrepancy between sustained expression of support for improved cooperation,16 18–20 22 23 the possible benefits of improved cooperation with OPs24 25 37 and the persisting structural exclusion of OPs from the rehabilitation process.9
This qualitative study is part of a larger mixed-method research project. In a first phase, blind spots in the knowledge about the issue are identified through a scoping review,9 which also forms the basis of the key questions for the FGDs. This qualitative project phase will be preceded by a third phase, in which we will use a representative survey of a broadened spectrum of stakeholders in order to quantify and differentiate enhancing and hindering (structural) factors. The findings of this exploratory mixed-method project could lead to intervention projects, which would then be developed, introduced and evaluated in larger follow-up projects.
Supplementary Material
Footnotes
Acknowledgements: The authors thank Dr Martina Michaelis, Christine Preiser for her assistance with the development of the interview guide, and to Lisa Peterson for translation services and language check.
Contributors: SV-M, JS, RK, GK and MAR contributed to the publication in the following way. SV-M and MAR were involved in development of the study design as a whole; GK and RK were involved in critical review of the study design as a whole; SV-M, MAR and JS were involved in development of the theoretical background and review of literature; SV-M and MAR were involved in development of research questions; SV-M and MAR were involved in development of interview guide; SV-M, GK and RK were involved in development of inclusion and exclusion strategy for participants; SV-M, JS, GK and RK were involved in election and invitation of participants; JS, SV-M and MAR were involved in development of strategy for data analysis; SV-M was involved in obtaining approval by the ethics committee; JS was involved in drafting the manuscript; SV-M, MAR, RK and GK were involved in critical revision of the manuscript. SV-M, JS, MAR, RK and GK were involved in final approval of the version and agreement to be accountable for all aspects of the work.
Funding: The study is part of the Junior Program of the Network for Health Services Research of the federal state of Baden-Württemberg (Versorgungsforschung Baden-Württemberg), which is funded by the federal state's Ministry for Scholarship, Research, and Art (Ministerium für Wissenschaft, Forschung und Kunst) and the Ministry for Labor, Social Order, Family, Women and Senior Citizens (Ministerium für Arbeit und Sozialordnung, Familie, Frauen und Senioren). The costs of this study will be funded by this programme up to €40 000, while the rest will be funded by the Institute of Occupational and Social Medicine and Health Services Research, University Hospital and Faculty of Medicine Tuebingen. The work of the Institute of Occupational and Social Medicine and Health Services Research is supported by an unrestricted grant of the employers' association of the metal and electric industry Baden-Württemberg (Südwestmetall).
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: The research will be undertaken in accordance with the bylaws for medical practitioners of the Doctoral Association (Landesärztekammer) of the federal state of Baden-Württemberg and the declaration of Helsinki in their respective current versions. The study design will be given to the Ethics Committee of the Medical Faculty and University Hospital of Tuebingen for review before the onset of the study. The names of all study participants and all other confidential information fall under medical confidentiality and the regulations of the German Federal Data Protection Act (Bundesdatenschutzgesetz, BDSG).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All data relating to the study protocol are included in this paper. The results of the study will be published as soon as the project is completed.
References
- 1.Deutsche Rentenversicherung (DRV). [Rehabilitation report 2015]. Berlin: DRV, 2015. [Google Scholar]
- 2.Bundesministerium für Arbeit und Soziales [Federal Ministry for work and social affairs] (BMAS), ed. [Statement of the scientific expert group RehaFutur on the future of vocational rehabilitation in Germany. Research report F393] Bonn: BMAS, 2009. [Google Scholar]
- 3.Pfaff H, Janßen C, Kowalski C, et al. . Ärzte und Betriebe: [Joint for health—a new concept for improved health care. Final report of the project: “physicians and companies as cooperation partners (ÄrBeK)”]. Gütersloh, Germany: Bertelsmann Stiftung, 2009. (cited 13 April 2016). http://www.bertelsmann-stiftung.de/cps/rde/xbcr/bst/Kurzfassung_Abschlussbericht.pdf [Google Scholar]
- 4.Bethge M, Bartel S. [Update 2015 of the working group “Rehabilitation and Work” of the German Society for Rehabilitation Sciences]. Rehabilitation 2016;55:63–5. 10.1055/s-0042-100230 [DOI] [PubMed] [Google Scholar]
- 5.Lohr KN, Steinwachs DM. Health services research: an evolving definition of the field. Health Serv Res 2002;37:7–9. [PubMed] [Google Scholar]
- 6.Agency for Healthcare Research and Quality (AHRQ). AHRQ website [internet]. Rockville, USA: AHRQ, 2010. (cited 12 December 2010). http://www.ahrq.gov/fund/minortrg.htm (accessed 11/13 2009). [Google Scholar]
- 7.Deitchman S, Dembe AE, Himmelstein J. Advent of occupational health services research. Am J Ind Med 2001;40:291–4. 10.1002/ajim.1103 [DOI] [PubMed] [Google Scholar]
- 8.Loisel P, Buchbinder R, Hazard R, et al. . Prevention of work disability due to musculoskeletal disorders: the challenge of implementing evidence. J Occup Rehabil 2005;15:507–24. 10.1007/s10926-005-8031-2 [DOI] [PubMed] [Google Scholar]
- 9.Völter-Mahlknecht S, Rieger MA. [Patient care at the interface between rehabilitation and occupational health physicians—a systematic literature review focusing health care organization]. Dtsch Med Wochenschr 2014;139:1609–14. [DOI] [PubMed] [Google Scholar]
- 10.Panter W. [Medical and vocational rehabilitation form the perspective of occupational health physicians]. Heidelberg, Germany: ECOmed Medizin, 2012:55–72. [Google Scholar]
- 11. DRV Baden-Württemberg. [BÄR occupation physician guided rehabilitation] [Internet]. Dtsch. Rentenversicher. [cited 2016 Apr 13]. https://www.deutsche-rentenversicherung.de/BadenWuerttemberg/de/Inhalt/Allgemeines/Downloads/Reha-Projekte/Flyer-BAER.pdf?__blob=publicationFile&v=3.
- 12.Moßhammer D, Natanzon I, Manske I, et al. . Cooperation between general practitioners and occupational health physicians in Germany: how can it be optimised? A qualitative study. Int Arch Occup Environ Health 2014;87:137–46. 10.1007/s00420-013-0845-1 [DOI] [PubMed] [Google Scholar]
- 13.Moßhammer D, Michaelis M, Mehne J, et al. . General practitioners’ and occupational health physicians’ views on their cooperation: a cross-sectional postal survey. Int Arch Occup Environ Health 2016;89:449–59. 10.1007/s00420-015-1084-4 [DOI] [PubMed] [Google Scholar]
- 14.Schwarze M, Spallek M, Korallus C, et al. . Advantages of the JobReha discharge letter: an instrument for improving the communication interface in occupational rehabilitation. Int Arch Occup Environ Health 2013;86:699–708. 10.1007/s00420-012-0805-1 [DOI] [PubMed] [Google Scholar]
- 15.de Bono AM. Communication between an occupational physician and other medical practitioners—an audit. Occup Med Oxf Engl 1997;47:349–56. 10.1093/occmed/47.6.349 [DOI] [PubMed] [Google Scholar]
- 16.Buijs P, van Amstel R, van Dijk F. Dutch occupational physicians and general practitioners wish to improve cooperation. Occup Environ Med 1999;56:709–13. 10.1136/oem.56.10.709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Friesen MN, Yassi A, Cooper J. Return-to-work: the importance of human interactions and organizational structures. Work Read Mass 2001;17:11–22. [PubMed] [Google Scholar]
- 18.Edlund C, Dahlgren L. The physician's role in the vocational rehabilitation process. Disabil Rehabil 2002;24:727–33. 10.1080/09638280210124310 [DOI] [PubMed] [Google Scholar]
- 19.Jakobsson B, Schüldt Håård U, Bergroth A, et al. . Improved cooperation in vocational rehabilitation with systematic rehabilitation group meetings. Disabil Rehabil 2002;24:734–40. 10.1080/09638280210124329 [DOI] [PubMed] [Google Scholar]
- 20.Beaumont D. Rehabilitation and retention in the workplace—the interaction between general practitioners and occupational health professionals: a consensus statement. Occup Med Oxf Engl 2003;53:254–5. 10.1093/occmed/kqg064 [DOI] [PubMed] [Google Scholar]
- 21.Beaumont D. The interaction between general practitioners and occupational health professionals in relation to rehabilitation for work: a Delphi study. Occup Med Oxf Engl 2003;53:249–53. 10.1093/occmed/kqg066 [DOI] [PubMed] [Google Scholar]
- 22.van Amstel R, Buijs P. [Open to improvements—medical specialists on the cooperation with occupational health physicians in the sociomedical supervision]. Hoofddorp: TNO Arbeid, 2000. Report No.: 1070110. [Google Scholar]
- 23.Rijkenberg A. The communication between occupational health physicians and specialists in physical medicine & rehabilitation—the situation in two different countries [a thesis submitted for the degree of: “Master in Occupational Health (MOH)”]. Antwerp, Belgium: Department of Epidemiology and Social Medicine, University of Antwerp, Belgium, 2012. [Google Scholar]
- 24.van Vilsteren M, van Oostrom SH, de Vet HCW, et al. . Workplace interventions to prevent work disability in workers on sick leave. Cochrane Database Syst Rev 2015;(10):CD006955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bethge M. Effects of graded return-to-work: a propensity-score-matched analysis. Scand J Work Environ Health 2016;42:273–9. 10.5271/sjweh.3562 [DOI] [PubMed] [Google Scholar]
- 26.Schneider U, Linder R, Verheyen F. Long-term sick leave and the impact of a graded return-to-work program: evidence from Germany. Eur J Health Econ 2016;17:629–43. 10.1007/s10198-015-0707-8 [DOI] [PubMed] [Google Scholar]
- 27.Schneider U, Linder R, Verheyen F. Long-term sick leave and graded return to work: what do we know about the follow-up effects? Health Policy 2016;120:1193–201. 10.1016/j.healthpol.2016.09.001 [DOI] [PubMed] [Google Scholar]
- 28.Seing I, MacEachen E, Ståhl C, et al. . Early-return-to-work in the context of an intensification of working life and changing employment relationships. J Occup Rehabil 2015;25:74–85. 10.1007/s10926-014-9526-5 [DOI] [PubMed] [Google Scholar]
- 29.Waddell G, Burton AK. Occupational health guidelines for the management of low back pain at work: evidence review. Occup Med Oxf Engl 2001;51:124–35. 10.1093/occmed/51.2.124 [DOI] [PubMed] [Google Scholar]
- 30.Carroll C, Rick J, Pilgrim H, et al. . Workplace involvement improves return to work rates among employees with back pain on long-term sick leave: a systematic review of the effectiveness and cost-effectiveness of interventions. Disabil Rehabil 2010;32:607–21. 10.3109/09638280903186301 [DOI] [PubMed] [Google Scholar]
- 31.Williams RM, Westmorland M. Perspectives on workplace disability management: a review of the literature. Work Read Mass 2002;19:87–93. [PubMed] [Google Scholar]
- 32.Steenstra IA, Anema JR, Bongers PM, et al. . The effectiveness of graded activity for low back pain in occupational healthcare. Occup Environ Med 2006;63:718–25. 10.1136/oem.2005.021675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bethge M, Müller-Fahrnow W. [Effectiveness of an intensified inpatient rehabilitation for musculoskeletal disorders: systematic review and meta analysis]. Rehabilitation 2008:200–9. [DOI] [PubMed] [Google Scholar]
- 34.Franche RL, Cullen K, Clarke J, et al. . Workplace-based return-to-work interventions: a systematic review of the quantitative literature. J Occup Rehabil 2005;15:607–31. 10.1007/s10926-005-8038-8 [DOI] [PubMed] [Google Scholar]
- 35.Krause N, Dasinger LK, Neuhauser F. Modified work and return to work: a review of the literature. J Occup Rehabil 1998;8:113–39. 10.1023/A:1023015622987 [DOI] [Google Scholar]
- 36.Cancelliere C, Donovan J, Stochkendahl MJ, et al. . Factors affecting return to work after injury or illness: best evidence synthesis of systematic reviews. Chiropr Man Ther 2016;24:32 10.1186/s12998-016-0113-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kamper SJ, Apeldoorn AT, Chiarotto A, et al. . Multidisciplinary biopsychosocial rehabilitation for chronic low back pain. Cochrane Database Syst Rev 2014;(9):CD000963 10.1002/14651858.CD000963.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Durand M-J, Corbière M, Coutu M-F, et al. . A review of best work-absence management and return-to-work practices for workers with musculoskeletal or common mental disorders. Work Read Mass 2014;48:579–89. [DOI] [PubMed] [Google Scholar]
- 39.Rijkenberg AM, van Sprundel M, Stassijns G. [Collaboration between occupational physicians and other specialists including insurance physicians]. Versicherungsmedizin 2013;65:140–5. [PubMed] [Google Scholar]
- 40.Vroeijenstijn-Nguyen X, Brenner R. [Contact between occupational health physicians and rehabilitation physicians—todays reality for a better future?]. Tijdschr Bedr Verzek 2007;2:59–62. 10.1007/BF03074510 [DOI] [Google Scholar]
- 41.Seidel H, Neuner R, Schochat T. [Occupational health physician and medical rehabilitation—a survey among occupational health physicians in Baden-Württemberg]. Arbeitsmedizin Sozialmedizin Umweltmed 2003;38:228–34. [Google Scholar]
- 42.Müller E, Mehrer L, Faust T, et al. . [Occupation-linked care of patients with musculoskeletal disorders: results of a survey among General practitioners, orthopedists, occupational health physicians and within rehabilitation]. DRV Schriften 2013;101:146–7. [Google Scholar]
- 43.Lüdemann A. [Communication and communication structure between occupational health physicians and rehabilitation clinics] [Dissertation]. Lübeck, Germany: Medical Faculty, University Lübeck, 2006. [Google Scholar]
- 44.Campbell M, Fitzpatrick R, Haines A, et al. . Framework for design and evaluation of complex interventions to improve health. BMJ 2000;321:694–6. 10.1136/bmj.321.7262.694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mayring P. Qualitative content analysis: theoretical foundation, basic procedures and software solution [internet]. Klagenfurt, Austria, 2014. Available from: http://nbn-resolving.de/urn:nbn:de:0168-ssoar-395173 [Google Scholar]
- 46.Moßhammer D, Manske I, Grutschkowski P, et al. . [Intersections in the health care service provision of GPs and OPs—a literature review]. Arbeitsmed Sozialmed Umweltmed 2011;46:301–7. [Google Scholar]
- 47.Flick U. An introduction to qualitative research. 5th edn Los Angeles: Sage Publications Ltd., 2014. [Google Scholar]
- 48.Clarke A. Focus group interviews in health-care research. Prof Nurse 1999;14:395–7. [PubMed] [Google Scholar]
- 49.Rudolph L, Deitchman S, Dervin K. Integrating occupational health services and occupational prevention services. Am J Ind Med 2001;40:307–18. 10.1002/ajim.1105 [DOI] [PubMed] [Google Scholar]
- 50.Brohan E, Henderson C, Wheat K, et al. . Systematic review of beliefs, behaviours and influencing factors associated with disclosure of a mental health problem in the workplace. BMC Psychiatry 2012;12:11 10.1186/1471-244X-12-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wells M, Williams B, Firnigl D, et al. . Supporting “work-related goals” rather than “return to work” after cancer? A systematic review and meta-synthesis of 25 qualitative studies. Psychooncology 2013;22:1208–19. [DOI] [PubMed] [Google Scholar]
- 52.Stergiou-Kita M, Grigorovich A, Tseung V, et al. . Qualitative meta-synthesis of survivors’ work experiences and the development of strategies to facilitate return to work. J Cancer Surviv 2014;8:657–70. 10.1007/s11764-014-0377-z [DOI] [PubMed] [Google Scholar]
- 53.Banning M. Employment and breast cancer: a meta-ethnography. Eur J Cancer Care (Engl) 2011;20:708–19. 10.1111/j.1365-2354.2011.01291.x [DOI] [PubMed] [Google Scholar]
- 54.MacEachen E, Kosny A, Scott-Dixon K, et al. . Workplace health understandings and processes in small businesses: a systematic review of the qualitative literature. J Occup Rehabil 2010;20:180–98. 10.1007/s10926-009-9227-7 [DOI] [PubMed] [Google Scholar]
- 55.MacEachen E, Clarke J, Franche RL, et al. , Workplace-based Return to Work Literature Review Group. Systematic review of the qualitative literature on return to work after injury. Scand J Work Environ Health 2006;32:257–69. 10.5271/sjweh.1009 [DOI] [PubMed] [Google Scholar]
- 56.Andersen MF, Nielsen KM, Brinkmann S. Meta-synthesis of qualitative research on return to work among employees with common mental disorders. Scand J Work Environ Health 2012;38:93–104. 10.5271/sjweh.3257 [DOI] [PubMed] [Google Scholar]
- 57.Krueger RA, Casey MA. Focus groups: a practical guide for applied research. Thousand Oaks, USA: SAGE Publications, 2014. [Google Scholar]
- 58.Bender DE, Ewbank D. The focus group as a tool for health research: issues in design and analysis. Health Transit Rev 1994;4:63–80. [PubMed] [Google Scholar]
- 59.Wong LP. Focus group discussion: a tool for health and medical research. Singapore Med J 2008;49:256–60; quiz 261. [PubMed] [Google Scholar]
- 60.Morgan DL. Focus groups as qualitative research. Sage Publications; 1988.
- 61.Leung F-H, Savithiri R. Spotlight on focus groups. Can Fam Physician 2009;55:218–9. [PMC free article] [PubMed] [Google Scholar]
- 62.Mansell I, Bennett G, Northway R, et al. . The learning curve: the advantages and disadvantages in the use of focus groups as a method of data collection. Nurse Res 2004;11:79–88. 10.7748/nr2004.07.11.4.79.c6217 [DOI] [PubMed] [Google Scholar]
- 63.Tuckett AG, Stewart DE. Collecting qualitative data: part II. Group discussion as a method: experience, rationale and limitations [corrected]. Contemp Nurse 2004;16:240–51. [DOI] [PubMed] [Google Scholar]
- 64.Helfferich C. [The quality of qualitative data. Manual for performing qualitative interviews]. Wiesbaden, Germany: Verlag für Sozialwissenschaften, 2008. [Google Scholar]
- 65.Lucius-Hoene G, Deppermann A. [Reconstruction of a narrative identity. Working book on the analysis of narrative interviews]. Wiesbaden, Germany: Verlag für Sozialwissenschaften, 2004. [Google Scholar]
- 66.Kleining G. Umriss zu einer Methodologie Qualitativer Sozialforschung. Köln Z Für Soziol Sozialpsychologie 1982;34:224–53. [Google Scholar]
- 67.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.