Description
Case description
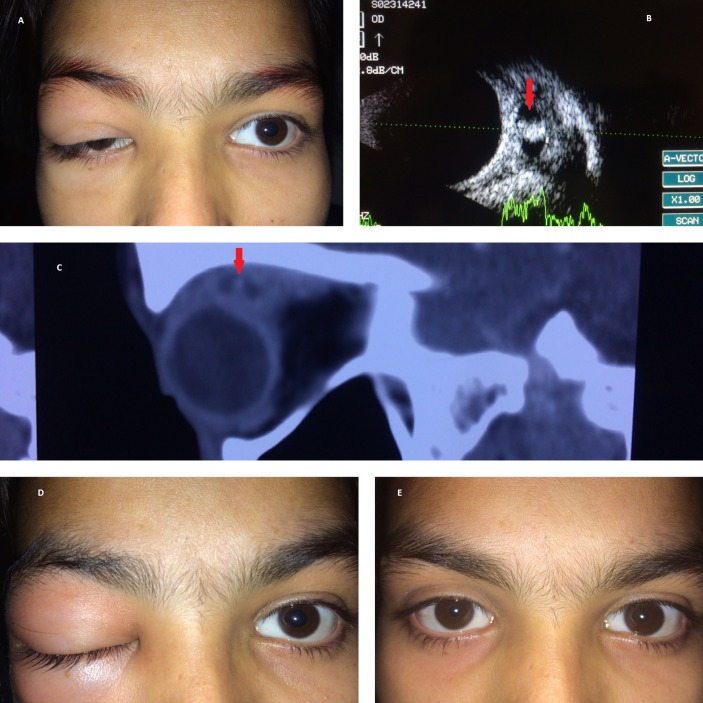
A 16-year-old girl presented with a 2-month history of recurrent (three episodes) right upper eyelid drooping and oedema (figure 1A). Examination showed fullness in the right upper eyelid along with elevation deficit. Visual acuity was 20/20 in each eye, and anterior and posterior segments were essentially within normal limits in both the eyes. To explain the cause, ultrasonography of the orbit for extraocular muscles revealed a large cyst in the superior rectus muscle along with a central hyperechoic spot corresponding to the scolex (figure 1B). Non-contrast CT of the orbit and brain revealed inflammatory thickening of the superior rectus muscle with the central cystic area harbouring the scolex without any intracranial foci (figure 1C). Based on the history and imaging findings a diagnosis of myocysticercosis was confirmed and the patient was started on tablet prednisolone 1mg/kg body weight from day 1 and tablet albendazole 15 mg/kg from day 3. The patient followed the protocol initially for 5 days and day 6 onwards she skipped the oral steroid medication and continued only with tablet albendazole for 3 days to present later with a predominant inflammatory swelling of the eyelid, chemosis and severe elevation deficit (figure 1D). The patient was counselled again about the importance of combined medication for successful treatment and better outcome; both the medications were continued with regular weekly follow-up. At around 2 weeks the scolex had disappeared on ultrasonography. Oral albendazole was continued for 4 weeks and oral steroids were tapered over a period of 4 weeks with complete recovery of ptosis in the right eye (figure 1E).
Figure 1.
(A) Initial clinical presentation with recurrent swelling and drooping of upper eyelid. (B) Ultrasonography of the superior rectus muscle showing a large cyst with a central high-amplitude spike corresponding to the scolex (red arrow). (C) Sagittal view of the non-contrast CT of the orbit showing inflammatory thickening of the superior rectus muscle with the cystic cavity having the central scolex (red arrow). (D) Inflammatory swelling of the right periorbital region after the patient skipped oral steroids. (E) Complete recovery of ptosis and inflammatory signs at the end of 4 weeks.
Discussion
A case of acquired ptosis with or without extraocular motility restriction having inflammatory signs should have a suspicion of extraocular myocysticercosis in endemic regions. Orbital ultrasonography and CT are able to define the muscle cyst and the scolex quite accurately in a majority of the cases.1 Successful treatment with the help of combined oral albendazole and prednisolone is proven by a number of studies.2 3 Albendazole mainly depletes the glycogen storage by inhibiting glucose uptake leading to death of the parasite, but subsequent to it there will be a release of toxins leading to severe inflammatory reaction; to tackle this oral steroids are given along with albendazole. In the present case, the patient was counselled about the need for combination medication before the beginning of the treatment but she defaulted and skipped oral steroids, which was indeed extremely necessary to counter the inflammation; but later with the guarded follow-up a favourable outcome was achieved. To conclude, in cases of extraocular muscle cysticercosis, a combination therapy with oral steroids and albendazole along with the appropriate dosage is necessary for a successful outcome. A close follow-up is preferred during the initial period to assess compliance to the treatment, detection of adverse events and management at the earliest.
Learning points.
Cases with extraocular myocysticercosis need thorough evaluation clinically as well as with appropriate imaging before the initiation of medical treatment.
A close follow-up during the initial period of treatment ensures compliance, early detection of complications and management.
Footnotes
Contributors: AS, SG, MSB and AP have evaluated the case in detail followed by appropriate medical management. AS, SG, MSB and AP after critically evaluating the educational value of the case wrote the report together.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Pujari A, Chawla R, Singh R, et al. . Ultrasound-B scan: an indispensable tool for diagnosing ocular cysticercosis. BMJ Case Rep 2017. doi: 10.1136/bcr-2017-219346 [Epub ahead of print 21 Apr 2017]. doi:10.1136/bcr-2017-219346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mohan K, Saroha V, Sharma A, et al. . Extraocular muscle cysticercosis: clinical presentations and outcome of treatment. J Pediatr Ophthalmol Strabismus 2005;42:28–33. [DOI] [PubMed] [Google Scholar]
- 3.Murthy R, Samant M. Extraocular muscle cysticercosis: clinical features and management outcome. Strabismus 2008;16:97–106. doi:10.1080/09273970802262506 [DOI] [PubMed] [Google Scholar]