Abstract
Allergic reactions to metals following joint arthroplasty represent a rare and poorly understood phenomenon. Much is still unknown regarding the natural history of this complication, and how it can best be prevented and managed. We present a case of a 68-year-old woman who underwent a left total knee arthroplasty for treatment of osteoarthritis. After an initial uneventful postoperative course, she developed a troublesome erythematous rash both around the incision site and over her trunk. Blood testing revealed no evidence of infection and clinically her prosthesis was functioning well. Skin patch testing revealed positive results for vanadium (+) and palladium (+). Her cutaneous symptoms are currently being managed conservatively and have shown a partial response to topical steroids. Revision surgery remains a long-term treatment option should conservative therapy fail; however, it would require a custom-made prosthesis as no standard tibial component is free from vanadium.
Keywords: orthopaedic and trauma surgery, osteoarthritic knww
Background
Cutaneous allergy to metals in the form of contact dermatitis is common, with nickel allergy alone thought to affect around 17% of women.1 In contrast, apparent cutaneous hypersensitivity reactions to metal prostheses are relatively rare. As the number of people undergoing arthroplasty continues to rise, potential allergic responses to metallic components of joint prostheses are of increasing concern yet remain poorly understood. Metal prosthesis allergy is believed to represent a T-cell-mediated, type IV hypersensitivity response in which metal ions generated from prosthesis corrosion form antigenic complexes with native proteins, which are recognised by the immune system.2 This process is analogous to contact dermatitis in which Langerhans cells in the skin act as specialised antigen-presenting cells (APCs) and trigger T lymphocytes and the subsequent allergic response following contact with an offending allergen. However, in comparison, the exact APC responsible for metal prosthesis hypersensitivity is unknown and the interplay between other immune cells or cytokines involved are not as clearly defined.2 3 Metal hypersensitivity following arthroplasty has been implicated in causing a range of clinical pictures, including local erythematous eczema around the incision site, widespread systemic skin manifestations, persistent synovitis leading to prolonged pain, and aseptic loosening.3 When protracted and refractory to conservative treatment, these symptoms can cause great morbidity and necessitate the need for revision surgery. While metals such as cobalt, nickel and chromium are most commonly implicated, we present an interesting case of local and systemic allergic reactions to vanadium and palladium following total knee arthroplasty (TKA).
Case presentation
A 68-year-old woman was referred for an orthopaedic opinion for increasing left knee pain. A year earlier, she had undergone left knee arthroscopy and excision of a medial meniscus tear.
Unfortunately, her symptoms failed to improve with subsequent conservative treatment. Plain radiographs revealed severe medial compartment osteoarthritis and she was listed for a TKA. The patient underwent an unremarkable TKA using a Genesis II system with an uncomplicated initial postoperative course. Following the procedure, the patient developed an erythematous rash with associated serous discharge over the incision, along with a more generalised itchy erythematous rash on the trunk and ocular pruritus (figures 1 and 2). She remained systemically well with no clinical evidence of infection and demonstrated a good, pain-free range of movement in her knee joint.
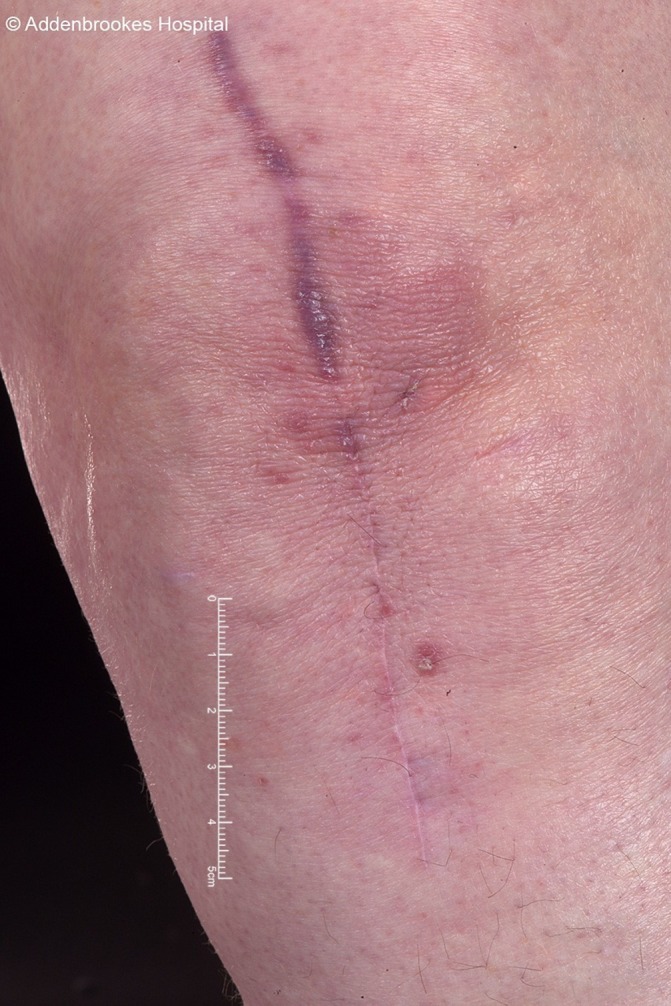
Figure 1.

Anterior aspect of knee 4 months following total knee arthroplasty
Figure 2.
Posterior chest 6 months following total knee arthroplasty.
Investigations
Serum blood testing revealed no evidence of infection, with white cell count, C reactive protein and erythrocyte sedimentation rate in the normal ranges along with negative viral and bacterial swabs results. Skin patch testing was performed, which revealed positive results for palladium chloride (+), vanadium chloride (+), gold sodium thiosulfate (+) and potassium dicyanoaurate (+). A skin biopsy of the affected area of the knee revealed mild chronic perivascular inflammation of the superficial dermis, and subsequent trace metal blood testing showed no elevation of serum cobalt, chromium, vanadium, palladium or gold levels.
Outcome and follow-up
Presently, the patient remains well, with an excellent pain-free range of motion from her TKA. Her rash is being managed by the dermatologists with topical steroids and has shown some improvement (figure 3). While the knee is functioning well, the patient is unsatisfied with her rash. If the rash becomes recalcitrant to treatment and the patient wants to proceed with revision, the implants will need to be custom made as no standard tibial component is free from vanadium other than the all polyethylene inserts, which are not available in the long-stem revision situation.
Figure 3.
Anterior aspect of knee after 2 months of topical steroid treatment.
Discussion
The causal link between arthroplasty and allergic responses is debated, with many conflicting pieces of research on the ability of metal prostheses to cause hypersensitivity reactions. Limitations of this work include this being only a single case of a potentially very rare metal allergy following TKA. More commonly, dermatitis is known to occur postoperatively secondary to swelling and the symptoms experienced by our patient could represent an epiphenomenon rather than a true allergy. However, the authors feel the persistence of symptoms following the resolution of swelling, the development of dermatitis at sites distant to the operation and the positive skin patch testing results to vanadium all add strength to metal allergy as the cause.
A sizeable proportion of evidence describing metal allergy following arthroplasty comes from anecdotal reports of cutaneous reactions and/or synovitis following joint replacement that resolved after revision surgery to non-allergic metal implants. Gao et al reported a case of localised eczema over the surgical scar, which later progressed to widespread dermatitis and pruritus following a TKA.4 The symptoms were resistant to antihistamine and corticosteroid therapies, with subsequent skin patch testing highly positive to chromium (++++). The TKA was revised to a non–chromium-containing alloy with resolution of eczema, dermatitis and pruritus. Similar cases of apparent allergic responses to nickel,5 6 chromium7 and palladium,5 with resolution of symptoms following revision, have also been reported. Allergic responses to vanadium implants appear to be even more uncommon. Asemota et al reported two patients who developed dermatitis and chronic pain, respectively, following spinal fusion.8 Skin patch testing suggested an allergic reaction to palladium, vanadium and nickel. There was a similar resolution of symptoms following implant removal. A comparable clinical picture has also been reported in cases of persistent synovitis following chromium–cobalt-containing knee arthroplasties.9 However, the relationship between documented metal allergy and/or positive patch test results and developing an allergic reaction following arthroplasty is not straightforward. To begin with, as previously mentioned, contact allergy to metal is relatively common, with around 17% of women and 3% of men allergic to nickel, and 1%–3% demonstrating allergic responses to cobalt and chromium.1 In contrast, allergic responses to metallic joint implants represent an uncommon phenomenon, occurring in an estimated 0.1%.10 The exact reason for this is disparity is unknown, but differences in the type of APC and its response to metals in skin versus deep joint tissues has been postulated.11 Furthermore, numerous reports in the literature exist of patients with documented metal allergy doing well with implants containing the offending metals.12 13 Thienpont and Berger described a patient with a history of contact dermatitis and positive patch test results to nickel, chromium and cobalt who went on to receive a cobalt–chromium TKA.12 The patient experienced no symptoms of pain or dermatitis and at 2 year follow-up no evidence of osteolysis, loosening or implant failure was present. Similar findings have been reported in a case series by Carlsson and Möller in which 18 patients with patch test positive allergic responses to chromium, cobalt or nickel received joint implants containing these metals. After a mean follow-up of 6.3 years, none of the patients suffered symptoms of dermatitis or pain attributable to allergy.13 Taken together, the evidence from case reports/series alone paints a confusing picture in which a small number of patients with cutaneous hypersensitivity to metals develop a prolonged allergic reaction to joint prosthesis metals.
The effect of intra-articular metal on the immune system is complex and poorly understood, and whether the above-described complications represent the development of new metal allergies or the exacerbation of pre-existing ones is unknown. Investigating this, one study measured metal sensitivity using skin patch testing and lymphocyte transformation tests preoperatively and postoperatively in 72 patients prior to hip or knee arthroplasty. The authors found five patients developed a new sensitivity to a metal contained in their joint prosthesis; however, interestingly, none developed symptoms of rash or dermatitis.14 Others have reported similar findings,15 and it appears that even when apparent allergic reactions following arthroplasty do occur, the outcome is highly variable. For example, Niki et al reported 5/24 patients who underwent TKA with positive modified lymphocyte stimulation tests to metals developed eczema postoperatively; of these, one had spontaneous resolution of symptoms, two showed partial response to medical therapy, while two required revision surgery (with successful resolution of symptoms).16
Perhaps what is of more clinical relevance is whether an allergy to metals has any effect on implant function in the form of aseptic loosening. Current opinion on aseptic loosening is that particles generated from prosthesis wear and corrosion slowly accumulate in the joint and trigger an inflammatory response. This response leads to osteolysis and bone resorption around the prosthesis and, ultimately, loosening of the component.17 Whether some individuals experience a more allergic, exaggerated response to these wear particles and subsequent accelerated prosthesis loosening is controversial. Granchi et al used patch testing on 94 patients: 20 awaiting TKA, 27 with well-functioning TKAs and 47 with evidence of loosening.18 The authors found a statistically significant increase in positive skin patch results in patients with both stable (48.1%) and loose (59.5%) TKAs compared with those awaiting arthroplasty (20.0%). While loosening of components was associated with the highest portion of positive skin patch results, statistically skin patch testing was unable to differentiate between stable and failing implants and the authors concluded metal sensitisation as a cause of TKA failure was unlikely.16 In a systematic review on the subject, the same authors showed similar findings, with positive test results to metal hypersensitivity increasing both postoperatively versus preoperatively (OR 1.52, 95% CI 1.06 to 2.31) and in failed versus stable implants (OR 2.76, 95% CI 1.14 to 6.70).19 It must be noted, however, that this review included hip arthroplasties and metal-on-metal implants, which are generally considered to convey a greater risk of metal sensitisation due to metallosis.
An inherent difficulty in investigating any causal relationship between known metal contact allergy and arthroplasty-related complications of dermatitis, synovitis and/or aseptic loosening is the lack of preoperative information on contact allergy. There is currently no definitive evidence that preoperative screening questionnaires or skin patch testing is beneficial.
To overcome this, an interesting study was carried out in 2015 by a Danish group in which data from 46 407 patients listed on the Danish knee arthroplasty register was cross-linked with 27 020 patients registered in the Copenhagen contact allergy database.20 A total of 327 patients had undergone both patch testing and TKA, 253 of these before the arthroplasty procedures. In contrast to the above studies, their results revealed a lower (non-significant) prevalence of metal allergy in patients who underwent revision surgery versus those with stable TKAs (13% vs 16%). Together, these studies suggest metallic joint implants can sensitise an individual to various metals in some cases. The clinical significance of sensitisation to metals is much more uncertain, and whether an increase in a positive allergy test results directly translates to an increased likelihood of allergic dermatitis post-arthroplasty is unknown. Similarly, while metal hypersensitivity may be involved in prosthesis loosening, a causal effect has not been proven currently, and any increased hypersensitivity seen in failing implants may be secondary to loosening, as opposed to being its cause.
Conclusion
Our current understanding of the pathogenesis and clinical significance of allergic responses to joint arthroplasty is incomplete, a fact reflected by the wide range of differing, sometimes contradictory evidence that is currently available. The temporal association observed in numerous case reports of arthroplasty, onset of symptoms and resolution following revision strongly implies the role of allergic responses to prosthesis components. However, it appears such an allergic reaction represents a rare response that occurs in an unpredictable way. The current literature suggests many cases of dermatitis or eczema following arthroplasty will resolve spontaneously or respond well to topical and/or systemic medical therapies. In cases refractory to conservative treatment, revision surgery can be offered; however, patients must be counselled on the uncertain success of any such procedure in resolving symptoms and must carefully weigh up the risks involved in revision arthroplasty.
Learning points.
Allergic reactions to metallic arthroplasty components represent an uncommon but difficult-to-manage complication.
Diagnosis should be considered only after more sinister causes of rash/persistent pain (infection, component loosening, malrotation etc) have been excluded.
There is no current evidence to support preoperative screening via skin patch testing or questionnaires prior to arthroplasty.
The natural history of joint prosthesis allergy remains poorly understood. Cutaneous symptoms should initially be treated conservatively with medical therapy. In resistant/refractory cases, revision arthroplasty containing hypoallergenic compounds can be offered; however, the patient must be carefully counselled regarding the risk versus benefits of revision arthroplasty.
Footnotes
Contributors: FP was the main author writing this case report. RC contributed to the design and writing the discussion of the article. AR contributed in the writing of the case presentation and editing. AV was the operating surgeon who oversaw the design, editing and final review of the case report.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Thyssen JP, Menné T. Metal allergy—a review on exposures, penetration, genetics, prevalence, and clinical implications. Chem Res Toxicol 2010;23:309–18. 10.1021/tx9002726 [DOI] [PubMed] [Google Scholar]
- 2.Goodman SB. Wear particles, periprosthetic osteolysis and the immune system. Biomaterials 2007;28:5044–8. 10.1016/j.biomaterials.2007.06.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lachiewicz PF, Watters TS, Jacobs JJ. Metal hypersensitivity and total knee arthroplasty. J Am Acad Orthop Surg 2016;24:106–12. 10.5435/JAAOS-D-14-00290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gao X, He RX, Yan SG, et al. Dermatitis associated with chromium following total knee arthroplasty. J Arthroplasty 2011;26:665.e13–665.e16. 10.1016/j.arth.2010.06.002 [DOI] [PubMed] [Google Scholar]
- 5.Bergschmidt P, Bader R, Mittelmeier W. Metal hypersensitivity in total knee arthroplasty: revision surgery using a ceramic femoral component—a case report. Knee 2012;19:144–7. 10.1016/j.knee.2011.01.001 [DOI] [PubMed] [Google Scholar]
- 6.Syed F, Jenner E, Faisal M, et al. Patellofemoral joint replacement and nickel allergy: an unusual presentation. Case Rep Orthop 2015;2015:1–4. 10.1155/2015/635082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomsen M, Rozak M, Thomas P. Pain in a chromium-allergic patient with total knee arthroplasty: disappearance of symptoms after revision with a special surface-coated TKA—a case report. Acta Orthop 2011;82:386–8. 10.3109/17453674.2011.579521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asemota E, Scheman AJ, Brod BA. Hypersensitivity reactions to metallic implants containing vanadium. Dermatitis 2016;27:387–8. 10.1097/DER.0000000000000229 [DOI] [PubMed] [Google Scholar]
- 9.Thakur RR, Ast MP, McGraw M, et al. Severe persistent synovitis after cobalt–chromium total knee arthroplasty requiring revision. Orthopedics 2013;36:e520–4. 10.3928/01477447-20130327-34 [DOI] [PubMed] [Google Scholar]
- 10.Merritt K, Rodrigo JJ. Immune response to synthetic materials. Clin Orthop Relat Res 1996;326:71–9. 10.1097/00003086-199605000-00009 [DOI] [PubMed] [Google Scholar]
- 11.Middleton S, Toms A. Allergy in total knee arthroplasty: a review of the facts. Bone Joint J 2016;98-B:437–41. 10.1302/0301-620X.98B4.36767 [DOI] [PubMed] [Google Scholar]
- 12.Thienpont E, Berger Y. No allergic reaction after TKA in a chrome–cobalt–nickel-sensitive patient: case report and review of the literature. Knee Surg Sports Traumatol Arthrosc 2013;21:636–40. 10.1007/s00167-012-2000-z [DOI] [PubMed] [Google Scholar]
- 13.Carlsson A, Möller H. Implantation of orthopaedic devices in patients with metal allergy. Acta Derm Venereol 1989;69:62–6. [PubMed] [Google Scholar]
- 14.Frigerio E, Pigatto PD, Guzzi G, et al. Metal sensitivity in patients with orthopaedic implants: a prospective study. Contact Dermatitis 2011;64:273–9. 10.1111/j.1600-0536.2011.01886.x [DOI] [PubMed] [Google Scholar]
- 15.Kitagawa A, Chin T, Tsumura N, et al. Metal sensitivity in patients before and after total knee arthroplasty (TKA): comparison between ceramic surfaced oxidized zirconium and cobalt–chromium implants. Hypersensitivity 2013;1:3 10.7243/2052-594X-1-3 [DOI] [Google Scholar]
- 16.Niki Y, Matsumoto H, Otani T, et al. Screening for symptomatic metal sensitivity: a prospective study of 92 patients undergoing total knee arthroplasty. Biomaterials 2005;26:1019–26. 10.1016/j.biomaterials.2004.03.038 [DOI] [PubMed] [Google Scholar]
- 17.Abu-Amer Y, Darwech I, Clohisy JC. Aseptic loosening of total joint replacements: mechanisms underlying osteolysis and potential therapies. Arthritis Res Ther 2007;9(Suppl 1):S6 10.1186/ar2170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Granchi D, Cenni E, Tigani D, et al. Sensitivity to implant materials in patients with total knee arthroplasties. Biomaterials 2008;29:1494–500. 10.1016/j.biomaterials.2007.11.038 [DOI] [PubMed] [Google Scholar]
- 19.Granchi D, Cenni E, Giunti A, et al. Metal hypersensitivity testing in patients undergoing joint replacement: a systematic review. J Bone Joint Surg Br 2012;94:1126–34. 10.1302/0301-620X.94B8.28135 [DOI] [PubMed] [Google Scholar]
- 20.Münch HJ, Jacobsen SS, Olesen JT, et al. The association between metal allergy, total knee arthroplasty, and revision: study based on the Danish knee arthroplasty register. Acta Orthop 2015;86:378–83. 10.3109/17453674.2014.999614 [DOI] [PMC free article] [PubMed] [Google Scholar]



