Abstract
Introduction: This study aimed to determine the bond strength of fiber post to composite core following surface treatment with Er,Cr:YSGG laser at different powers and sandblasting with and without thermocycling.
Methods: In this experimental study, 30 fiber posts (Glassix, Nordin, Switzerland) were randomly divided into 5 groups of sandblasting, no treatment and laser irradiation at 1, 1.5 and 2 W powers. Following composite filling and mounting, 1-mm thick sections were made for pushout bond strength testing. Half of the samples in each group were subjected to thermocycling (n=15). Two-way analysis of variance (ANOVA) was used to analyze the bond strength values. Pairwise comparisons were made using Tukey test (P<0.05).
Results: Effect of treatment method on push-out bond strength of fiber post to composite core was significant (P=0.017), while thermocycling had no significant effect on bond strength (P=0.964). Pairwise comparison of surface treatment methods revealed no significant difference in groups with and without thermocycling (P>0.05), but Er,Cr:YSGG laser irradiation with 1 W power yielded significantly higher bond strength than the control group (P=0.01).
Conclusion: Irradiation of Er,Cr:YSGG laser at 1 W power increased the bond strength of fiber post to composite core. Thermocycling slightly decreased the bond strength at the fiber postcore interface.
Keywords: Bond strength, Composite, Er, Cr:YSGG laser, Post
Introduction
Endodontically treated teeth exhibit lower fracture strength than sound teeth due to considerable loss of tooth structure. Fiber posts are extensively used to provide retention for the core in permanent restoration of endodontically treated teeth.1
Prefabricated fiber posts have shown promising clinical results in terms of durability for use in endodontically treated teeth with moderate amount of remaining coronal tooth structure. Fiber posts have gained increasing popularity as an alternative to the traditional casting post and core restorations.2-4 Prefabricated fiber posts adhesively bond to the root canal walls and provide retention for composite cores. Core build-up is done chairside and thus, eliminates the need for a laboratory fabrication step.5-7 Fiber posts are often made of silanized glass or quartz fibers in an epoxy- or methacrylate-based resin matrix. No chemical reaction occurs between the organic matrix of fiber posts and methacrylate present in the core build-up material.8-10 Despite several advantages of fiber posts over the conventional posts, bond to intracanal dentin and core material has always been challenging for the former group.3,11,12
Some surface treatment methods including mechanical and chemical treatments have been proposed to enhance the bond of fiber posts to substrates, with controversial results.13-15 The chemical bond between fibers and resin materials is enhanced by the application of silane coupling agent.16-19 Application of silane increases the wettability of post surface; thus, an intimate contact can be obtained between the two materials. On the other hand, micromechanical retention can be provided by abrasion with air born particles measuring 25-30 μ in size, via increasing the surface area and microporosity. Resin penetrates into the microporosities and forms resin tags, which result in micromechanical interlocking and enhance the retention of the core material.19 Since no general consensus has been reached for an ideal clinical bonding process, attempts have been made to find alternative chemical and mechanical techniques for surface treatment of fiber posts to achieve higher bond strength. Surface treatment with Er,Cr:YSGG laser is among the suggested techniques.
The Er,Cr:YSGG laser is well absorbed by the water and minerals present in the formulation of hydroxyapatite crystals. Due to the absorption of Er,Cr:YSGG laser wavelength in water, it has several applications for the gingival tissue and oral mucosa.20 Due to its numerous advantages, this laser is used as a safe and effective surface treatment modality to enhance the bond strength. Moreover, laser irradiated surfaces may provide a strong bond to restorative materials thanks to numerous porosities and the absence of a smear layer.21
Application of laser in dentistry is becoming increasingly popular. Arslan et al22 reported that Er:YSGG laser irradiation at 4.5 W power was more effective for increasing the bond strength of fiber-glass posts to composite core, compared to sandblasting. However, Tuncdemir et al showed that Er:YAG laser irradiation at different powers had no significant effect on the bond of quartz fiber posts to resin cements.23 Moreover, Kurtulmus-Yilmaz et al assessed the effect of Er,Cr:YSGG laser irradiation on bond strength of fiber posts to resin cores, and reported that application of this laser at 1 W and 1.5 W power enhanced the bond at the post-core interface.24
To the best of the authors’ knowledge, no previous study has evaluated the bond strength of fiber posts to composite core with/without thermocycling, and only one study was found on the effect of Er,Cr:YSGG laser irradiation on bond strength of fiber posts to composite cores, and it didn’t evaluated the effect of thermocycling on the results.24
Duration and method of aging are among other factors affecting the success of composite restorations. Thus, artificial aging must be performed to simulate the clinical setting. Thermocycling and water storage are among the well-accepted artificial aging protocols for simulation of clinical oral environment.6 Thermocycling has been extensively used in studies on composite restorations, to simulate aging of composite bond. In this method, samples are subjected to severe thermal changes. High temperature degrades the physico-chemical properties of composite and compromises its bond. Thermal changes decrease the number of unreacted double bonds on the surface or within the composite, and negatively affect the composite bond strength.2
This study sought to assess the effect of Er,Cr:YSGG laser irradiation on push-out bond strength of fiber post to composite core, in comparison with sandblasting and no surface treatment.
Methods
Thirty glass fiber posts (Glassix #3, Nordin, Switzerland) were used in this study to make all specimens. Based on the method of surface treatment, the posts were randomly divided into 5 groups. After cleaning the posts with alcohol, group 1 posts were subjected to 1 W Er,Cr:YSGG laser (Biolase, Waterlase, USA). Group 2 posts were subjected to 1.5 W Er,Cr:YSGG laser. Group 3 posts were subjected to 2 W Er,Cr:YSGG laser. Group 4 posts were sandblasted and group 5 posts had no treatment. For surface treatment with laser, laser was set on H mode and each fiber post was lased for 2 cycles with a swiping motion; each cycle of laser treatment took 40 seconds. Each laser power was used with 20 Hz frequency, 60% water, 40% air and Δt of 60 μs. Fiber posts in the sandblasting group were sandblasted with 50 μ Al2O3 particles at 2.8 bar pressure for 5 seconds from 10 mm distance.
After cleaning the posts by immersing in ultrasonic bath containing water for 4 minutes, silane (PULPDENT, Watertown, USA) was applied on all fiber posts and gently air-dried after 1 minute. Bonding agent (Single Bond, 3M ESPE, St. Paul, MN, USA) was then applied on the entire surface of fiber posts and each surface was cured for 20 seconds using a light curing unit with light intensity of 600 mW/cm2 (Woodpecker, Shanghai, China). The apical third of each post was placed in a surveyor and adjusted perpendicular to a glass slab. A cylindrical plexiglass mold measuring 8 mm in diameter and 2 mm in thickness was placed over the post surrounding its non-tapered zone in such a way that the post was approximately positioned at the center of the mold. After post placement, composite (P60, 3M ESPE, St. Paul, MN, USA) was applied to the mold in 2 mm increments and was cured for 20 seconds using the same light curing unit. Then, another mold was placed above the previous one and filled similarly. The procedure continued until the non-tapered zone of each post was completely filled. Next, the remaining tapered part of each post was cut. After that, all composite-post blocks were immersed in distilled water at 37°C for 24 hours. Finally, the composite_post blocks were mounted in epoxy resin and sectioned perpendicular to apical-coronal direction to 1-mm thickness using a Mecatome (Presi, France). By doing so, 5 samples were obtained of each composite-post blocks approximately, and a total of 30 samples for each groups. Half of the samples in each group were thermocycled (10 000 cycles, 5°C-55°C, 20 seconds of dwell time and 10 seconds of transfer time), while the other half were not (n = 15). Samples’ thickness was measured by a digital caliper and all samples were subjected to push-out bond strength tests by the universal testing machine (Zwick Roell, Ulm, Germany). The bond strength values were recorded in megapascals (MPa).
The samples were loaded by a cylindrical plunger with 0.8 mm diameter at the center of posts without contact with the surrounding core surfaces. Load was applied in an apical-coronal direction at a crosshead speed of 1 mm/min and continued until the post displacement. Maximum load at post displacement was measured in Newton and calculated and reported in MPa. The samples were then evaluated under a stereomicroscope (Nikon, Tokyo, Japan) to determine the mode of failure at ×40 magnification.
Five fiber posts (one of each group) were prepared and after the gold coating under sputter coater (SBC12, KYKY, China) for 30 minutes, they were evaluated under a scanning electron microscope (SEM) at ×500 magnification (EM3200, KYKY, China) and micrographs were captured for assessment of surface morphology.
The data were analyzed using SPSS version 21.0. Descriptive statistics were applied and the mean and standard deviation (SD) of push-out bond strength of fiber posts to composite core were reported for the five groups. Two-way analysis of variance
( ANOVA) was applied to assess the effect of surface treatment method and conduction of thermocycling on the results. Tukey test was used for pairwise comparisons of the groups. Type one error was considered as 0.05.
Results
The mean and SD of push-out bond strength of fiber posts to composite core, following sandblasting with and without thermocycling, were 15.76 ± 4.22 MPa and 16.56 ± 3.46 MPa, respectively. In the control group with and without thermocycling, these values were 12.59 ± 2.95 and 14.68 ± 2.16 MPa, respectively. These values in the 1 W, 1.5 W and 2 W laser groups with and without thermocycling were 17.02 ± 7.81 MPa and 18.3 ± 4.02 MPa, 14.19 ± 4.11 MPa and 15.18 ± 6.28 MPa and 14.83 ± 4.99 MPa and 15.11 ± 5.19 MPa, respectively (Table 1 and Figure 1).
Table 1. Descriptive Statistics for the Push-out Bond Strength of Fiber Posts to Composite Core in the 5 Groups With/Without Thermocycling and Pairwise Comparison .
| Group | Bond Strength | |
| Termocycling | No Termocycling | |
| Control | 12.59 (2.95)a | 14.68 (2.16)a |
| Sandblasting | 15.76 (4.22)a,b | 16.56 (3.46)a,b |
| Laser 1 W | 17.02 (7.81)b | 18.30 (4.02)b |
| Laser 1.5 W | 14.19 (4.11)a,b | 15.18 (6.28)a,b |
| Laser 2 W | 14.83 (4.99)a,b | 15.11 (5.19)a,b |
Different letter shows the statistically significant difference.
Figure 1.
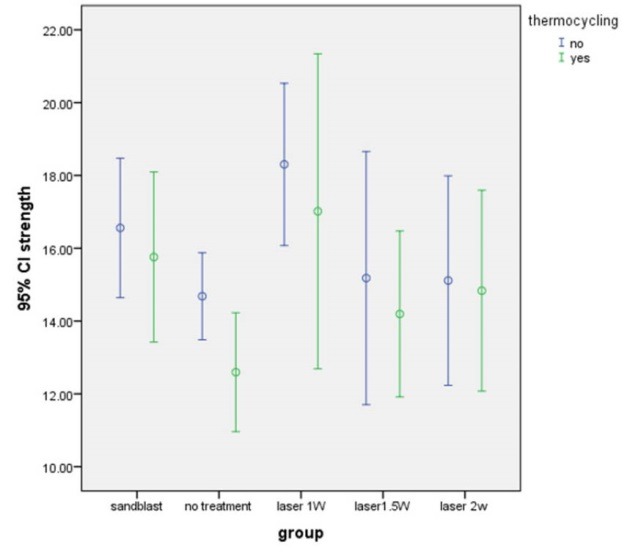
Push-out Bond Strength of Fiber Posts to Composite Core in the 5 Groups With and Without Thermocycling
Based on the results of two-way ANOVA, the effect of treatment method on push-out bond strength of fiber post to composite core was significant (P = 0.017) but thermocycling had no significant effect on bond strength (P = 0.17). The interaction effect of thermocycling and treatment method on bond strength was not significant neither (P = 0.96).
Considering the significant effect of different surface treatment methods on push-out bond strength of fiber posts to composite core, Tukey test was applied for pairwise comparisons of bond strength values. Based on Table 1, a significant difference was only found between the control (no surface treatment) and 1 W laser groups (P = 0.01), and no other significant difference was noted between different surface treatment groups in terms of bond strength of fiber post to composite core.
The frequency of failure modes is shown in Table 2. Overall, the frequency percentage of adhesive, cohesive within the core, cohesive within the post and mixed failures were found to be 87%, 5.33%, 2.67% and 5.33%, respectively.
Table 2. The Frequency of Modes of Failure in the 5 Surface Treatment Groups With and Without Thermocycling .
| Group | Thermocycling | Failure Pattern | |||
|
Adhesive
No. (%) |
Cohesive Within the Core
No. (%) |
Cohesive Within the Post
No. (%) |
Mixed
No. (%) |
||
| Control | Yes | 13 (86.87) | 1 (6.67) | 0 (0) | 1 (6.67) |
| No | 12 (80) | 2 (13.33) | 0 (0) | 1 (6.67) | |
| Sandblasting | Yes | 15 (100) | 0 (0) | 0 (0) | 0 (0) |
| No | 13 (86.87) | 1 (6.67) | 1 (6.67) | 0 (0) | |
| Laser 1 W | Yes | 15 (100) | 1 (6.67) | 0 (0) | 0 (0) |
| No | 12 (80) | 0 (0) | 1 (6.67) | 2 (13.33) | |
| Laser 1.5 W | Yes | 13 (86.67) | 0 (0) | 0 (0) | 2 (13.33) |
| No | 12 (80) | 1 (6.67) | 2 (13.33) | 0 (0) | |
| Laser 2 W | Yes | 12 (80) | 1 (6.67) | 0 (0) | 2 (13.33) |
| No | 14 (93.33) | 1 (6.67 | 0 (0) | 0 (0) | |
The micrographs of SEM analysis can be seen in Figure 2.
Figure 2.
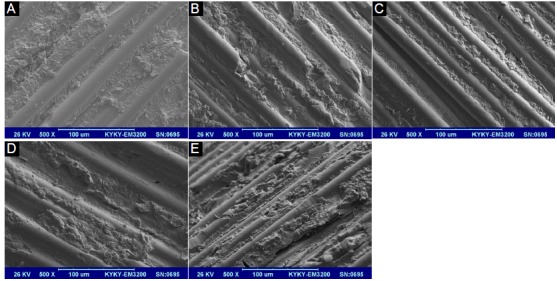
The SEM Micrographs (×500) of Fiber Post Surfaces in the 5 Groups of no Treatment (A), Sandblasting (B), 1 W Laser (C), 1.5 W Laser (D) and 2 W Laser (E).
Discussion
Based on the results of this study, surface treatment method of fiber posts had a significant effect on their bond strength to composite core, but thermocycling had no such effect.
It has been documented that chemical composition (size, type, distribution and percentage of fibers) and surface topography of posts affect the post-resin core bond strength.23,25,26 In the current study, only one type of glass post (Glassix) was used to assess the effect of different surface treatment protocols on bond strength. Fiber posts have uniform, smooth surfaces limiting mechanical interlocking between the post surface and resin core.1 To obtain a bond between the methacrylate-based resin of the core material and resin matrix of the fiber post, fiber posts must undergo mechanical or chemical surface treatment to react with silane molecules.27 In the current study, samples were prepared with 1 W, 1.5 W and 2 W Er,Cr:YSGG laser, or by sandblasting plus silanization. On the other hand, thermocycling was performed for half the samples in each group, because in the clinical setting, bond strength is affected by chemical, thermal and mechanical factors in the oral cavity; however, in the current study, thermocycling had no significant effect on push-out bond strength of fiber posts to resin core. But, the bond strength values in the thermocycled samples were slightly lower than the values in the non-thermocycled samples. In the current study, the mean and SD of push-out bond strength of fiber posts to composite core following sandblasting with and without thermocycling was found to be 15.76 ± 4.22 MPa and 16.56 ± 3.46 MPa, respectively; the difference in bond strength between this method and other protocols was not significant.
It has been reported that sandblasting with Al2O3 particles may cause cracks in the post.28 Previous studies recommended mild sandblasting to prevent crack formation and minimize dimensional changes of fiber posts.29,30 Thus, in the current study, sandblasting was performed with 5μ Al2O3 particles at 2.8 bar pressure for 5 seconds from 10 mm distance.31 The SEM micrographs in the sandblasted group revealed irregular dugout areas of resin matrix all over the fiber posts.
The results of the current study showed that the mean and SD of push-out bond strength of fiber posts to composite core following 1 W, 1.5 W and 2 W laser irradiation with and without thermocycling were 17.02 ± 7.81 MPa and 18.3 ± 4.02, MPa, 14.19 ± 4.11 MPa and 15.18 ± 6.28 MPa and 14.83 ± 4.99 MPa and 15.11 ± 5.19 MPa, respectively. No significant difference was noted in the bond strength of 1.5 and 2 W laser groups and that of other groups; however, the bond strength of 1 W Er,Cr:YSGG laser group was significantly higher than that of no treatment group.
Laser irradiation is a safe and simple surface treatment method for some dental materials.32,33 Some recent studies evaluated the effects of different powers of Er:YAG laser on bond strength of fiber posts.22,23,33,34 Sipahi et al demonstrated that Er:YAG laser irradiation with 150 mJ power and 10 Hz frequency increased the bond strength of glass fiber posts34 but Tuncdemir et al reported that Er:YAG laser with the afore-mentioned parameters had no significant effect on push-out bond strength of quartz fiber posts.23 On the other hand, Arslan et al used Er:YAG laser with 150, 300 and 450 mJ powers and 10 Hz frequency for treatment of glass fiber posts and showed that Er:YAG laser irradiation at 450 mJ power increased the push-out22 and pull-out33 bond strength of fiber-post to resin core. Akin et al evaluated the bond strength of quartz fiber posts after different surface treatment methods and reported the highest bond strength in the sandblasted followed by the Er:YAG laser irradiated groups; these two methods significantly increased the bond strength of quartz fiber posts to resin cement.35 Moreover, Kriznar et al evaluated the micro-push-out bond strength of Multicore Flow resin material to 2 types of fiber posts following Er:YAG laser irradiation, and showed that Er:YAG laser irradiation negatively affected the bond strength of resin material to fiber posts.16 Controversial results of different studies may be attributed to factors such as type of fiber post and differences in laser parameters.
On the other hand, Er,Cr:YSGG laser used in the current study may have effects similar to those of Er:YAG laser since its wavelength (2.78 nm) is close to that of Er:YAG laser (2.94 nm).36 The efficacy of Er,Cr:YSGG laser for surface treatment of dentin,37,38 ceramics38 and composite resin39 has been previously evaluated. Kurtulmus-Yilmaz et al evaluated the effect of Er,Cr:YSGG laser on micro-push-out bond strength of fiber post to resin core, and showed that laser irradiation in 1 W and 1.5 W powers enhanced the bond strength, but 2 W laser irradiation had no such effect.24 Similarly, irradiation of 1 W laser in the current study improved the bond strength.
High (2 W) power laser may destruct fibers and compromise the homogeneity and integrity of posts, which can eventually decrease the ability of posts to bond to silane and resin core material. Higher laser powers can cause severe physical damage to fiber posts, and the generated heat in this process may adversely affect the chemical composition of composite and compromise the quality of bond of fiber posts to composite core.24 In the current study, SEM micrographs of 1.5 and 2 W laser treated groups revealed areas of resin matrix and fiber dugout; however, in 1 W laser treated group, only resin matrix had been dugout in some areas between fibers, and the fibers remained intact.
Er,Cr:YSGG laser wavelength is in the infrared spectrum. Laser beams are aimed at the target organs via a fiber-optic system. In this laser, photons are reinforced in a medium of heterogeneous crystals. The laser emits photons at 2780 nm wavelength in 140 μs pulse and 10-50 Hz frequency. Laser irradiation of soft and hard tissues is a complex topic due to complicated interactions of laser energy, water and tissues.40 When tissues react to laser energy, the resultant outcome will be determined by the wavelength of laser, optical characteristics of tissue, duration of irradiation, laser energy and rate of laser absorption by the tissue. Laser absorption plays a major role in conversion of laser light energy to heat, sound or chemical energy between atoms and molecules in the target organ. Thus, the required laser energy to achieve a desired outcome would be variable depending on the type of target tissue.40
Chemical affinity between the two components is also an important determinant of bond strength.41 The surface of fiber posts is so polymerized that they are no longer capable of reacting or bonding to free radicals.42 The bond strength of composite resins to fiber posts is often limited due to chemical heterogeneity between methacrylate-based resins and epoxy resins in the post.43 Also, the composition of resin polymer matrix in the post can affect the ability of adhesive to penetrate between the fibers and provide adequate micromechanical retention.10 The main component in the composition of resin can also affect the bond to fiber posts.44 On the other hand, it seems that the surface roughness created by the manufacturer and the modifications made in the epoxy resin matrix of the post for bond to Bis-GMA also decrease the efficacy of surface treatments to enhance the bond strength.11
Based on the results of the current study, 10 000 cycles of thermocycling (equals to one year of clinical service),45 had no significant effect on bond strength of fiber posts to composite core; although it slightly (but not significantly) decreased the bond strength. Considering the necessity of simulation of clinical setting in in-vitro studies, we performed thermocycling as a standard method of artificial aging.6
In the current study, push-out loads were applied to samples to prevent creation of heterogeneous stresses in them. Some researchers believe that push-out bond strength testing is more reliable than the microtensile test for measurement of bond strength of fiber posts to radicular dentin46 because the push-out test highly resembles an actual shear test and provides a more reliable and accurate estimation of bond strength compared to the conventional shear test.47 The only shortcoming of the push-out strength test is unequal stress distribution in thick samples; this problem can be eliminated by slicing the samples to obtain thin sections.46 Goracci et al compared the efficacy of microtensile and push-out tests for accurate assessment of bond strength of fiber posts cemented in the post space, and showed that push-out test was more accurate than the microtensile test for measurement of bond strength of cemented fiber posts.46 In the push-out technique, all prepared samples can be used and the dispersion of results would be lower; whereas in microtensile test, numerous primary fractures occur in the samples and the results would have high dispersion.46
In the current study, 87% of the failures were of adhesive type and occurred at the fiber post-resin core interface in different surface treatment groups.
In the current study, 10 000 thermal cycles (corresponding to approximately one year of clinical service) had no significant effect on bond strength; the effect of longer duration of aging on bond strength must be evaluated in future studies.
In vitro studies cannot completely simulate the oral clinical conditions. In the oral cavity, restored teeth are exposed to numerous variables; they are constantly exposed to moisture, thermal alterations and variations in pH due to a variety of diets. Moreover, they are exposed to bacteria and different enzymes and are subjected to masticatory forces. All these factors have undeniable effects on the bond strength of fiber posts to composite core, and may compromise the clinical service of posts. Thus, the effect of these parameters on bond strength of posts to composite core can be an interesting topic for future studies.
Our in vitro assessment of surface treatment effect of fiber posts with Er,Cr:YSGG laser on their bond to composite core with and without thermocycling by all its limitations, revealed that irradiation of Er,Cr:YSGG laser with 1 W power effectively enhanced the bond strength of fiber posts to composite core, and thermocycling slightly (but not significantly) decreased the bond strength at the post-core interface.
Conflict of Interests
The authors declare no conflict of interest.
Ethical Considerations
Since this research is an experimental study, there is no ethical consideration.
Please cite this article as follows: Hashemikamangar SS, Hasanitabatabaee M, Kalantari S, Gholampurdehaky M, Ranjbaromrani L, Ebrahimi H. Bond strength of fiber posts to composite core: effect of surface treatment with Er,Cr:YSGG laser and thermocycling. J Lasers Med Sci. 2018;9(1):36-42. doi:10.15171/jlms.2018.09.
References
- 1.Balbosh A, Kern M. Effect of surface treatment on retention of glass-fiber endodontic posts. J Prosthet Dent. 2006;95(3):218–223. doi: 10.1016/j.prosdent.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Fredriksson M, Astback J, Pamenius M, Arvidson K. A retrospective study of 236 patients with teeth restored by carbon fiber-reinforced epoxy resin posts. J Prosthet Dent. 1998;80(2):151–157. doi: 10.1016/s0022-3913(98)70103-9. [DOI] [PubMed] [Google Scholar]
- 3.Monticelli F, Grandini S, Goracci C, Ferrari M. Clinical behavior of translucent-fiber posts: a 2-year prospective study. Int J Prosthodont. 2003;16(6):593–596. [PubMed] [Google Scholar]
- 4.Malferrari S, Monaco C, Scotti R. Clinical evaluation of teeth restored with quartz fiber-reinforced epoxy resin posts. Int J Prosthodont. 2003;16(1):39–44. [PubMed] [Google Scholar]
- 5.Robbins JW. Guidelines for the restoration of endodontically treated teeth. J Am Dent Assoc. 1990;120(5):558. doi: 10.14219/jada.archive.1990.0087. [DOI] [PubMed] [Google Scholar]
- 6.Gutmann JL. The dentin-root complex: anatomic and biologic considerations in restoring endodontically treated teeth. J Prosthet Dent. 1992;67(4):458–467. doi: 10.1016/0022-3913(92)90073-j. [DOI] [PubMed] [Google Scholar]
- 7.Schwartz RS, Robbins JW. Post placement and restoration of endodontically treated teeth: a literature review. J Endod. 2004;30(5):289–301. doi: 10.1097/00004770-200405000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Kallio TT, Lastumaki TM, Vallittu PK. Bonding of restorative and veneering composite resin to some polymeric composites. Dent Mater. 2001;17(1):80–86. doi: 10.1016/s0109-5641(00)00064-6. [DOI] [PubMed] [Google Scholar]
- 9.Lastumaki TM, Lassila LV, Vallittu PK. The semi-interpenetrating polymer network matrix of fiber-reinforced composite and its effect on the surface adhesive properties. J Mater Sci Mater Med. 2003;14(9):803–809. doi: 10.1023/a:1025044623421. [DOI] [PubMed] [Google Scholar]
- 10.Mannocci F, Sherriff M, Watson TF, Vallittu PK. Penetration of bonding resins into fibre-reinforced composite posts: a confocal microscopic study. Int Endod J. 2005;38(1):46–51. doi: 10.1111/j.1365-2591.2004.00900.x. [DOI] [PubMed] [Google Scholar]
- 11.Bouillaguet S, Troesch S, Wataha JC, Krejci I, Meyer JM, Pashley DH. Microtensile bond strength between adhesive cements and root canal dentin. Dent Mater. 2003;19(3):199–205. doi: 10.1016/s0109-5641(02)00030-1. [DOI] [PubMed] [Google Scholar]
- 12.Ferrari M, Cagidiaco MC, Grandini S, De Sanctis M, Goracci C. Post placement affects survival of endodontically treated premolars. J Dent Res. 2007;86(8):729–734. doi: 10.1177/154405910708600808. [DOI] [PubMed] [Google Scholar]
- 13.Vano M, Goracci C, Monticelli F. et al. The adhesion between fibre posts and composite resin cores: the evaluation of microtensile bond strength following various surface chemical treatments to posts. Int Endod J. 2006;39(1):31–39. doi: 10.1111/j.1365-2591.2005.01044.x. [DOI] [PubMed] [Google Scholar]
- 14.Faria MI, Gomes E, Messias DC, Silva Filho JM, Souza Filho CB, Paulino SM. Tensile strength of glass fiber posts submitted to different surface treatments. Braz Dent J. 2013;24(6):626–629. doi: 10.1590/0103-6440201302365. [DOI] [PubMed] [Google Scholar]
- 15.Soares CJ, Santana FR, Pereira JC, Araujo TS, Menezes MS. Influence of airborne-particle abrasion on mechanical properties and bond strength of carbon/epoxy and glass/bis-GMA fiber-reinforced resin posts. J Prosthet Dent. 2008;99(6):444–454. doi: 10.1016/s0022-3913(08)60106-7. [DOI] [PubMed] [Google Scholar]
- 16.Kriznar I, Jevnikar P, Fidler A. Effect of Er:YAG laser pretreatment on bond strength of a composite core build-up material to fiber posts. Lasers Med Sci. 2015;30(2):733–740. doi: 10.1007/s10103-013-1412-4. [DOI] [PubMed] [Google Scholar]
- 17.Aksornmuang J, Foxton RM, Nakajima M, Tagami J. Microtensile bond strength of a dual-cure resin core material to glass and quartz fibre posts. J Dent. 2004;32(6):443–450. doi: 10.1016/j.jdent.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 18.Matinlinna JP, Lassila LV, Ozcan M, Yli-Urpo A, Vallittu PK. An introduction to silanes and their clinical applications in dentistry. Int J Prosthodont. 2004;17(2):155–164. [PubMed] [Google Scholar]
- 19.Goracci C, Raffaelli O, Monticelli F, Balleri B, Bertelli E, Ferrari M. The adhesion between prefabricated FRC posts and composite resin cores: microtensile bond strength with and without post-silanization. Dent Mater. 2005;21(5):437–444. doi: 10.1016/j.dental.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 20.Harashima T, Kinoshita JI, Kimura Y. et al. Morphological comparative study on ablation of dental hard tissues at cavity preparation by Er: YAG and Er, Cr: YSGG lasers. Photomedicine and Laser Therapy. 2005;23(1):52–5. doi: 10.1089/pho.2005.23.52. [DOI] [PubMed] [Google Scholar]
- 21.Hossain M, Nakamura Y, Yamada Y, Murakami Y, Matsumoto K. Microleakage of composite resin restoration in cavities prepared by Er,Cr:YSGG laser irradiation and etched bur cavities in primary teeth. J Clin Pediatr Dent. 2002;26(3):263–268. doi: 10.17796/jcpd.26.3.q8747j711g425582. [DOI] [PubMed] [Google Scholar]
- 22.Arslan H, Barutcigil C, Yilmaz CB, Ceyhanli KT, Topcuoglu HS. Push-out bond strength between composite core buildup and fiber-reinforced posts after different surface treatments. Photomed Laser Surg. 2013;31(7):328–333. doi: 10.1089/pho.2013.3478. [DOI] [PubMed] [Google Scholar]
- 23.Tuncdemir AR, Yildirim C, Guller F, Ozcan E, Usumez A. The effect of post surface treatments on the bond strength of fiber posts to root surfaces. Lasers Med Sci. 2013;28(1):13–18. doi: 10.1007/s10103-012-1053-z. [DOI] [PubMed] [Google Scholar]
- 24.Kurtulmus-Yilmaz S, Cengiz E, Ozan O, Ramoglu S, Yilmaz HG. The effect of Er,Cr:YSGG laser application on the micropush-out bond strength of fiber posts to resin core material. Photomed Laser Surg. 2014;32(10):574–581. doi: 10.1089/pho.2014.3780. [DOI] [PubMed] [Google Scholar]
- 25.Cekic-Nagas I, Sukuroglu E, Canay S. Does the surface treatment affect the bond strength of various fibre-post systems to resin-core materials? J Dent. 2011;39(2):171–179. doi: 10.1016/j.jdent.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 26.Elsaka SE. Influence of chemical surface treatments on adhesion of fiber posts to composite resin core materials. Dent Mater. 2013;29(5):550–558. doi: 10.1016/j.dental.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 27.Kulunk S, Kulunk T, Yenisey M. Effects of different surface pre-treatments on the bond strength of adhesive resin cement to quartz fiber post. Acta Odontol Scand. 2012;70(6):547–554. doi: 10.3109/00016357.2011.629623. [DOI] [PubMed] [Google Scholar]
- 28.Valandro LF, Yoshiga S, de Melo RM. et al. Microtensile bond strength between a quartz fiber post and a resin cement: effect of post surface conditioning. J Adhes Dent. 2006;8(2):105–111. [PubMed] [Google Scholar]
- 29.D’Arcangelo C, D’Amario M, Vadini M, De Angelis F, Caputi S. Influence of surface treatments on the flexural properties of fiber posts. J Endod. 2007;33(7):864–867. doi: 10.1016/j.joen.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 30.Kern M, Thompson VP. Sandblasting and silica coating of a glass-infiltrated alumina ceramic: volume loss, morphology, and changes in the surface composition. J Prosthet Dent. 1994;71(5):453–461. doi: 10.1016/0022-3913(94)90182-1. [DOI] [PubMed] [Google Scholar]
- 31.Yenisey M, Kulunk S. Effects of chemical surface treatments of quartz and glass fiber posts on the retention of a composite resin. J Prosthet Dent. 2008;99(1):38–45. doi: 10.1016/s0022-3913(08)60007-4. [DOI] [PubMed] [Google Scholar]
- 32.Spohr AM, Borges GA, Junior LH, Mota EG, Oshima HM. Surface modification of In-Ceram Zirconia ceramic by Nd:YAG laser, Rocatec system, or aluminum oxide sandblasting and its bond strength to a resin cement. Photomed Laser Surg. 2008;26(3):203–208. doi: 10.1089/pho.2007.2130. [DOI] [PubMed] [Google Scholar]
- 33.Arslan H, Kurklu D, Ayranci LB. et al. Effects of post surface treatments including Er:YAG laser with different parameters on the pull-out bond strength of the fiber posts. Lasers Med Sci. 2014;29(5):1569–1574. doi: 10.1007/s10103-013-1485-0. [DOI] [PubMed] [Google Scholar]
- 34.Sipahi C, Piskin B, Akin GE, Bektas OO, Akin H. Adhesion between glass fiber posts and resin cement: evaluation of bond strength after various pre-treatments. Acta Odontol Scand. 2014;72(7):509–515. doi: 10.3109/00016357.2013.875586. [DOI] [PubMed] [Google Scholar]
- 35.Akin GE, Akin H, Sipahi C, Piskin B, Kirmali O. Evaluation of surface roughness and bond strength of quartz fiber posts after various pre-treatments. Acta Odontol Scand. 2014;72(8):1010–1016. doi: 10.3109/00016357.2014.939710. [DOI] [PubMed] [Google Scholar]
- 36.Hossain M, Nakamura Y, Yamada Y, Kimura Y, Matsumoto N, Matsumoto K. Effects of Er,Cr:YSGG laser irradiation in human enamel and dentin: ablation and morphological studies. J Clin Laser Med Surg. 1999;17(4):155–159. doi: 10.1089/clm.1999.17.155. [DOI] [PubMed] [Google Scholar]
- 37.Garbui BU, de Azevedo CS, Zezell DM, Aranha AC, Matos AB. Er,Cr:YSGG laser dentine conditioning improves adhesion of a glass ionomer cement. Photomed Laser Surg. 2013;31(9):453–460. doi: 10.1089/pho.2013.3546. [DOI] [PubMed] [Google Scholar]
- 38.Kursoglu P, Motro PF, Yurdaguven H. Shear bond strength of resin cement to an acid etched and a laser irradiated ceramic surface. J Adv Prosthodont. 2013;5(2):98–103. doi: 10.4047/jap.2013.5.2.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cho SD, Rajitrangson P, Matis BA, Platt JA. Effect of Er,Cr:YSGG laser, air abrasion, and silane application on repaired shear bond strength of composites. Oper Dent. 2013;38(3):E1–9. doi: 10.2341/11-054-l. [DOI] [PubMed] [Google Scholar]
- 40.Rizoiu I, Kohanghadosh F, Kimmel AI, Eversole LR. Pulpal thermal responses to an erbium,chromium: YSGG pulsed laser hydrokinetic system. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86(2):220–223. doi: 10.1016/s1079-2104(98)90128-7. [DOI] [PubMed] [Google Scholar]
- 41.Boschian Pest L, Cavalli G, Bertani P, Gagliani M. Adhesive post-endodontic restorations with fiber posts: push-out tests and SEM observations. Dent Mater. 2002;18(8):596–602. doi: 10.1016/s0109-5641(02)00003-9. [DOI] [PubMed] [Google Scholar]
- 42.Bell AM, Lassila LV, Kangasniemi I, Vallittu PK. Bonding of fibre-reinforced composite post to root canal dentin. J Dent. 2005;33(7):533–539. doi: 10.1016/j.jdent.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 43.Monticelli F, Toledano M, Tay FR, Sadek FT, Goracci C, Ferrari M. A simple etching technique for improving the retention of fiber posts to resin composites. J Endod. 2006;32(1):44–47. doi: 10.1016/j.joen.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 44.Salameh Z, Papacchini F, Ounsi HF, Goracci C, Tashkandi E, Ferrari M. Adhesion between prefabricated fiber-reinforced posts and different composite resin cores: a microtensile bond strength evaluation. J Adhes Dent. 2006;8(2):113–117. [PubMed] [Google Scholar]
- 45.Xie C, Han Y, Zhao XY, Wang ZY, He HM. Microtensile bond strength of one- and two-step self-etching adhesives on sclerotic dentin: the effects of thermocycling. Oper Dent. 2010;35(5):547–555. doi: 10.2341/10-025-l. [DOI] [PubMed] [Google Scholar]
- 46.Goracci C, Tavares AU, Fabianelli A. et al. The adhesion between fiber posts and root canal walls: comparison between microtensile and push-out bond strength measurements. Eur J Oral Sci. 2004;112(4):353–361. doi: 10.1111/j.1600-0722.2004.00146.x. [DOI] [PubMed] [Google Scholar]
- 47.Drummond JL, Sakaguchi RL, Racean DC, Wozny J, Steinberg AD. Testing mode and surface treatment effects on dentin bonding . J Biomed Mater Res. 1996;32(4):533–541. doi: 10.1002/(SICI)1097-4636(199612)32:4<533::AID-JBM6>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]


