Abstract
Several techniques have been proposed to prevent hypotension in obstetric patients. Ephedrine and phenylephrine are individually used to prevent maternal hypotension; however, each has its own drawbacks. Some researchers have reported that the infusion of combined ephedrine and phenylephrine immediately after spinal anesthesia for cesarean delivery reduces the incidence of maternal hypotension. Other studies have indicated that the combination is not superior to the infusion of an individual agent. The present study aimed to evaluate the effect of prophylactic infusion of ephedrine and phenylephrine before the induction of spinal anesthesia for cesarean section on maternal hemodynamic. In a randomized, double-blinded clinical trial study, 90 pregnant women that underwent elective cesarean delivery under spinal anesthesia were recruited. Before the spinal anesthesia, the infusion of combined ephedrine and phenylephrine during 15 minutes (study group) or serum NaCl 0.9% (placebo group) was performed. Hemodynamic parameters and fetal blood gas were recorded. The data were analyzed using the SPSS software, version 16.0. The results showed that hypotension and bradycardia after spinal anesthesia were less in the study group. The need for vasopressors and inotropes to treat hypotension, nausea, and vomiting were higher in the placebo group. First- and fifth-minute Apgar scores were higher in the study group. The prophylactic infusion of low-dose ephedrine and phenylephrine before spinal anesthesia for cesarean delivery can be used to decrease the frequency and severity of maternal hypotension and its side effects to the mother and neonate. Trial Registration Number: IRCT201401277013N6
Keywords: Cesarean Section, Anesthesia, Spinal, Hypotension, Ephedrine, Phenylephrine
What’s Known
The infusion of combined ephedrine and phenylephrine immediately after spinal anesthesia for cesarean section reduces the incidence of maternal hypotension and increases the PH of the fetal umbilical artery.
Some studies have demonstrated that such combination is not superior to the infusion of the individual agent.
What’s New
There are dissimilar results on the effect of combined ephedrine and phenylephrine versus the infusion of individual agent on the incidence of maternal hypotension and neonatal outcome in the spinal anesthesia for cesarean section.
In previous studies, the drugs were administered after spinal injection rather than before spinal anesthesia.
Introduction
Hypotension is the most common complication of neuraxial anesthesia in obstetric patients1 and its prevalence in cesarean section is about 50-90%.2,3 Maternal hypotension causes unpleasant symptoms such as nausea, vomiting, loss of consciousness, respiratory depression, and cardiac arrest. Hypotension may reduce placental perfusion and result in fetal acidosis and neurological injury.1-3 Several techniques have been proposed to prevent hypotension.1-4
Ephedrine has been used as the agent of choice in the prevention and treatment of hypotension following spinal anesthesia in pregnant women. However, recently, there have been concerns regarding its use because of complications such as supraventricular tachycardia, tachyphylaxis, and the probability of fetal acidosis.1-7 Phenylephrine (a strong α-agonist of sympathetic receptors) can be used for the prevention and treatment of maternal hypotension. It reduces the incidence of nausea and vomiting as well as fetal acidosis, but it may cause maternal bradycardia and decreased cardiac output. Therefore, the use of phenylephrine, especially for prophylaxis of hypotension, is uncommon.1,3,5,8,9 Combining drugs with different mechanisms of action lowers the amount of each drug, thus the undesired effects are minimized.10
The present study aimed to evaluate the effect of prophylactic infusion of a combined ephedrine and phenylephrine on maternal hemodynamic before the induction of spinal anesthesia for cesarean section. This topic was motivated by the fact that there have been no investigations evaluating the effect of vasopressors before spinal injection. In previous studies, the drugs were administered after spinal injection. Furthermore, there are dissimilar results on the infusion of combined ephedrine and phenylephrine after spinal anesthesia for cesarean section if maternal hypotension and fetal acidosis occur.5,6,11-13
Materials and Methods
The present randomized, double-blinded clinical trial was performed in Al-Zahra Hospital, Tabriz University of Medical Sciences (Tabriz, Iran) from May 2014 to February 2015. In total, 90 full-term pregnant women with ASA class I-II were recruited. The sample size was calculated using the incidence of hypotension as the primary outcome. A sample size of 42 pregnant women per group was required to achieve 80% power at 5% significance level to detect 40% difference in hypotension rate between the two groups. To allow for potential dropouts, 90 patients aged 18-40 years were recruited. Using the simple random method, the patients were randomly allocated into two groups (n=45 each), namely the study group and placebo group.
The inclusion criteria were full-term pregnant women, 18-40 years of age, ASA class I-II, and scheduled for elective cesarean section under spinal anesthesia. The exclusion criteria were pre-existing or pregnancy-induced hypertension (BP>140/90 mmHg), systemic or psychological diseases, known fetal abnormality, emergency cesarean section, any medical contraindication to spinal anesthesia, allergy to local anesthetics, and the use of vasopressors before the operation.
Patients with 8-hour fast did not receive premedication. Standard monitoring was established in the operating room, women rested in the supine position with left uterine displacement, and baseline blood pressure, SpO2, and HR were measured and recorded. Then, two 18-gauge intravenous cannulas were sited. Each patient received a 10 mL/kg IV infusion of Ringer’s solution for 15 minutes before spinal anesthesia. At the same time (i.e. during the administration of serum) and before spinal anesthesia, the infusion of 20 mL automated syringe was started in patients with the rate of 60 mL/h. The syringe in group 1 (study group, n=45) contained ephedrine 10 mg plus phenylephrine 125 mcg that had reached 15 mL with normal saline serum (NaCl 0.9%). In group 2 (placebo group, n=45) it contained only 15 mL of normal saline serum. The infusion rate of study solutions was adjusted according to the systolic blood pressure (SBP). This rate was maintained if SBP remained within 90-105% of the baseline. The rate of infusion was 30 mL/h if SBP increased within 105-120% of the baseline. The infusion was stopped if SBP increased to more than 120% of the baseline value and restarted at 60 mL/h if SBP decreased back to 90-105% of the baseline.
The dosage of vasopressors was chosen based on the study by Saravanan et al.13 All infusion solutions were prepared previously and labeled with code numbers. The patients as well as the medical student and nurses, who infused the solution and monitored vitals and other clinical signs throughout the operation, were blinded to the solutions. After the completion of fluid infusions, all patients received spinal anesthesia in a sitting position from L3-4 or L4-5 interspaces using a 25-gauge Quincke needle with 10 mg bupivacaine 0.5% (2 mL) and 15 µg fentanyl (1 cc; 10 µg). The total drug volume was 3.5 mL. Immediately after spinal anesthesia, all patients were positioned in the supine position with left uterine displacement. The operation began after the sensory block at dermatome T4. Oxygen was administered at the rate of 3 lit/min by a face mask until the umbilical cord was clamped. Oxytocine 20 U in Ringer’s solution was administered after the clamping of the cord. Blood pressure was controlled every 2 minutes after spinal anesthesia until delivery and then every 5 minutes throughout the operation. Moreover, HR and SpO2 were controlled throughout anesthesia. Sensory block was monitored to obtain a T4-5 level of anesthesia. After delivery and clamping of the umbilical cord, 1 mL of blood was drawn from the umbilical artery for neonatal blood gas analysis. Any decrease of about 20% from baseline in BP after spinal anesthesia was treated with 100 mg phenylephrine (if associated with tachycardia) or 5 mg ephedrine otherwise. Bradycardia (maternal HR<50 beats/min) was treated with 0.5 mg atropine if it was not associated with hypotension. The incidence of hypotension, maximal hypotension, duration of hypotension, total dose of injected vasopressors, and neonatal outcome parameters (first- and fifth-minute Apgar scores and PH of the umbilical artery) were recorded. The occurrence of nausea or vomiting was recorded on a four-point scale (0=none, 1=mild nausea, 2=nausea requiring treatment, 3=vomiting). Nausea or vomiting with a score of ≥2 was treated with 5-10 mg IV metoclopramide if untreated by vasopressors. Other collected data included the duration of operation and anesthesia (time of sensory block), total IV fluid administration, cause of cesarean, gravidity, and side effects (maternal unconsciousness and respiratory depression). Two surgeons were responsible for the operations. An anesthesiologist was responsible for the anesthesia and patient monitoring, and the other anesthesiologist and an intern were responsible for recording patient information and completing the questionnaires.
Data were analyzed using descriptive statistical methods (mean±SD), frequency, and percentage. Mean difference tests for independent samples were used for quantitative variables and Chi-squared test or Fisher’s exact test for qualitative variables. All data were analyzed using the SPSS software (version 16.0) and P≤0.05 were considered statistically significant.
The present study is registered (number: IRCT201401277013N6) on the website of Iranian clinical trials (IRCT; http://www.irct.ir) and approved by the Research Ethics Committee of Tabriz University of Medical Sciences. Written informed consent was obtained from the patients.
Results
At the end of the study, the data for 90 patients were collected (45 patients in the study group and 45 patients in the placebo group). There was no significant difference in patients’ demographic data between the groups. There was no significant difference in patients’ gravidity, cause of cesarean section, duration of operation and anesthesia, dermatomal sensory level, and duration of sensory block. Maternal baseline mean arterial pressure (MAP) and HR values were not different between the two groups (P=0.9 and P=0.8, respectively). Maternal side effects of spinal anesthesia and treatments are presented in table 1.
Table 1.
Maternal side effects of spinal anesthesia and the required treatments
| Side effect | Study group (n=45) | Placebo group (n=45) | P value |
|---|---|---|---|
| Hypotension | 7 (15.5%) | 32 (71.1%) | <0.001 |
| Bradycardia | 0 (0%) | 6 (13.3%) | 0.01 |
| Nausea and vomiting | 4 (8.8%) | 10 (22.2%) | 0.05 |
| Consciousness decline | 0 | 0 | - |
| Ventilation depression | 0 | 0 | - |
| Unrest | 2 (4.4%) | 3 (6.6%) | 0.5 |
| Treatment | |||
| Ephedrine | 4 (8.8%) | 31 (68.8%) | <0.001 |
| Phenylephrine | 1 (2.2%) | 5 (11.1%) | 0.03 |
| Atropine | 0 | 6 (13.3%) | 0.01 |
| Metoclopramide | 0 | 4 (8.9%) | 0.03 |
| Midazolam | 3 (6.6%) | 3 (6.6%) | 0.66 |
| Support of ventilation | 0 | 0 | - |
Number (percent)
Hypotension and bradycardia after spinal anesthesia were less in the study group. The patients of the study group were less and late hypotensive (P=0.04) than those of the placebo group and returned to normal blood pressure faster (P=0.02). The need for phenylephrine and ephedrine (for the treatment of hypotension) and atropine (for the treatment of bradycardia) was higher in the placebo group. Nausea and vomiting were significantly more frequent in the placebo group.
Neonatal outcomes are shown in table 2. First- and fifth-minute Apgar scores were higher in the study group. Umbilical arterial PH showed no significant differences between the two groups. CONSORT flowchart is shown in figure 1.
Table 2.
Neonatal outcomes of the study and placebo groups
| Outcome | Study group (n=45) | Placebo group (n=45) | P value |
|---|---|---|---|
| Apgar in 1st min | 8.79±1.41 | 7.73±1.05 | 0.001 |
| Apgar in 5th min | 9.71±0.6 | 9.09±1.14 | 0.04 |
| PH of umbilical artery | 7.31±0.08 | 7.29±1.51 | 0.08 |
Mean±SD
Figure 1.
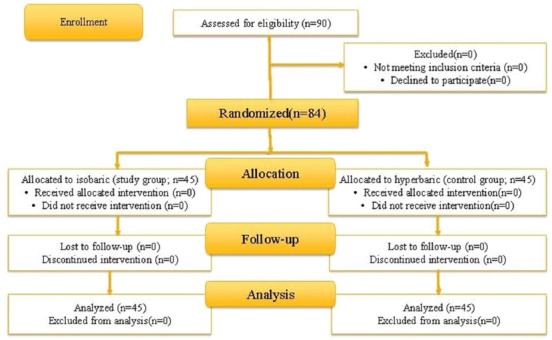
CONSORT flowchart of patients enrolled in the study
Discussion
The results of the present study indicated that the prophylactic infusion of low doses of ephedrine (10 mg) and phenylephrine (125 µg) before spinal anesthesia for cesarean section, caused a significant decrease in the frequency and severity of maternal hypotension, need for vasoactive drugs, nausea, vomiting, need for antiemetic drug, and an increase in the Apgar score of neonates. A study showed that ephedrine could not always prevent hypotension and nausea during spinal anesthesia without effects on maternal tachycardia and fetal acidosis.8 There are also studies that examined the effect of prophylactic intravenous ephedrine with different doses on reducing the rate of hypotension; nevertheless, several cases showed hypertension.2,6 In the present study, due to the use of low-dose medications, hypertension was not observed more than in the placebo group. Aragao et al. used intramuscular injection of combined ephedrine and phenylephrin.3 The rate of hypotension in their study group was 45%, while it was 15.5% in our study, indicating that our approach may be more effective.
In the present study, the neonatal Apgar scores in the first and fifth minutes were higher in the study group than the placebo group. These results were consistent with those of several other studies that had confirmed the effect of ephedrine and phenylephrine infusion on the improvement of fetal oxygenation.1-3,7 Nevertheless, unlike the results of some other studies,7 we observed no significant difference in the PH of the umbilical artery. Previous studies demonstrate that the use of combined method is not superior to the individual use of ephedrine or phenylephrine in preventing or treating hypotension. In most studies, vasopressors were administered immediately after the induction of spinal anesthesia. However, we infused vasopressors 15 minutes before the induction of spinal anesthesia for a preemptive effect. In addition, we used lower doses of drugs than previous studies.13 Therefore, the side effects of vasopressors were fewer in our study. The main limitation of the present study was the low sample size. A higher number of patients would help to achieve results that are more accurate.
Conclusion
The present study indicated that the prophylactic infusion of low doses of ephedrine and phenylephrine before spinal anesthesia for cesarean section might result in a significant decrease in the frequency and severity of maternal hypotension, need for vasoactive drugs, nausea, vomiting, need for antiemetic drug, and an increase in the Apgar score of neonates.
Conflict of Interest: None declared.
References
- 1.Chestnut DH, Wong CA, Tsen LC, Kee WDN, Beilin Y, Mhyre J. Chestnut's Obstetric Anesthesia:Principles and Practice E-Book. Elsevier Health Sciences. 2014 [Google Scholar]
- 2.Metzger A, Eisen I, Todris L, Etchin A, Kuit J. Maternal hypotension during elective cesarean section and short-term neonatal outcome. American Journal of Obstetrics & Gynecology. 2010;202(1):56.e1–e5. doi: 10.1016/j.ajog.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 3.Aragao FF, Aragao PW, Martins CA, Salgado FN, Barroqueiro ES. Comparison of metaraminol, phenylephrine and ephedrine in prophylaxis and treatment of hypotension in cesarean section under spinal anesthesia. Rev Bras Anestesiol. 2014;64(5):299–306. doi: 10.1016/j.bjan.2013.07.014. [DOI] [PubMed] [Google Scholar]
- 4.Ngan Kee WD. Prevention of maternal hypotension after regional anaesthesia for cesarean section. Current Opinion in Anaesthesiology. 2010;23(3):304–9. doi: 10.1097/ACO.0b013e328337ffc6. [DOI] [PubMed] [Google Scholar]
- 5.Ng F, Karmakar M, Ngan Kee WD, Lee A, Gin T. A randomized double-blinded comparison of phenylephrine and ephedrine infusion combination to maintain blood pressure during spinal anesthesia for cesarean section delivery:The effects on fetal acid-base status and hemodynamic control. Anesthesia and Analgesia. 2008;107(4):1295–302. doi: 10.1213/ane.0b013e31818065bc. [DOI] [PubMed] [Google Scholar]
- 6.Ngan Kee WD, Khaw K, Tan P, Ng F, Karmakar M. Placental transfer and fetal metabolic effects of phenylephrine and ephedrine during spinal anesthesia for cesarean section. Anesthesiology. 2009;111:506–12. doi: 10.1097/ALN.0b013e3181b160a3. [DOI] [PubMed] [Google Scholar]
- 7.Adigun TA, Amanor-Boadu SD, Soyannwo OA. Comparison of intravenous ephedrine with phenylephrine for the maintenance of arterial blood pressure during elective caesarean section under spinal anaesthesia. Afr J Med Med Sci. 2010;39(1):13–20. [PubMed] [Google Scholar]
- 8.Magalhaes E, Goveia CS, de Araujo Ladeira LC, Nascimento BG, Kluthcouski SM. Ephedrine versus phenylephrine:prevention of hypotension during spinal block for cesarean section and effects on the fetus. Rev Bras Anestesiol. 2009;59(1):11–20. doi: 10.1590/s0034-70942009000100003. [DOI] [PubMed] [Google Scholar]
- 9.Ngan Kee WD, Lee A, Khaw KS, Ng FF, Karmakar MK, Gin T. A randomized double-blinded comparison of phenylephrine and ephedrine infusion combinations to maintain blood pressure during spinal anesthesia for cesarean delivery:the effects on fetal acid-base status and hemodynamic control. Anesth Analg. 2008;107(4):1295–302. doi: 10.1213/ane.0b013e31818065bc. [DOI] [PubMed] [Google Scholar]
- 10.Das S, Mukhopadhyay S, Mandal M, Mandal S, Basu SR. A comparative study of infusions of phenylephrine, ephedrine and phenylephrine plus ephedrine on maternal haemodynamics in elective caesarean section. Indian J Anaesth. 2011;55(6):578–83. doi: 10.4103/0019-5049.90612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loughrey JP, Yao N, Datta S, Segal S, Pian-Smith M, Tsen LC. Hemodynamic effects of spinal anesthesia and simultaneous intravenous bolus of combined phenylephrine and ephedrine versus ephedrine for cesarean delivery. Int J Obstet Anesth. 2005;14(1):43–7. doi: 10.1016/j.ijoa.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 12.Bhattarai B, Bhat SY, Upadya M. Comparison of bolus phenylephrine, ephedrine and mephentermine for maintenance of arterial pressure during spinal anesthesia in cesarean section. JNMA J Nepal Med Assoc. 2010;49(177):23–8. [PubMed] [Google Scholar]
- 13.Saravanan S, Kocarev M, Wilson RC, Watkins E, Columb MO, Lyons G. Equivalent dose of ephedrine and phenylephrine in the prevention of post-spinal hypotension in Caesarean section. Br J Anaesth. 2006;96(1):95–9. doi: 10.1093/bja/aei265. [DOI] [PubMed] [Google Scholar]


