Abstract
Since the advent of direct acting antiviral (DAA) agents, chronic hepatitis C virus (HCV) treatment has evolved at a rapid pace. In contrast to prior regimen involving ribavirin and pegylated interferon, these newer agents are highly effective, well-tolerated, have shorter course of therapy and safer essentially in all HCV patients including those with advanced liver disease and following liver transplantation. Clinicians caring for HCV-infected patients on the liver transplant (LT) waitlist are often faced with a dilemma whether to treat HCV infection before or after liver transplantation. Sustained virological response (SVR) rates following HCV treatment may improve hepatic function sufficiently enough to negate the need for LT in certain patients. On the other hand, the decrease in MELD without improvement in quality of life in certain patients may lead to delay or dropout from potentially curative LT surgery list. In this context, our review focuses on the approach to and optimal timing of DAA-based treatment of HCV infection in LT candidates in the peri-transplant period.
Keywords: Hepatitis C virus, Direct-acting antiviral therapy, Liver transplantation, Purgatory Model for End-stage liver disease, Sustained virological response
Core tip: Optimal timing of antiviral therapy for hepatitis C virus (HCV) infection in liver transplant candidates using second generation direct-acting antivirals is debated. Available evidence lacks conviction if the viral eradication is beneficial in all HCV patients before liver transplantation. We aim to review the current literature to better delineate the appropriate timing of HCV treatment in the era of direct-acting antiviral agents.
INTRODUCTION
Chronic hepatitis C virus (HCV) infection continues to be a major cause of chronic liver disease in the United States (US) despite the overall decline in the incidence in recent years. Based on current estimates, 2.7 to 3.5 million persons are infected with chronic HCV (1.0%-1.5% of US population) and HCV-related liver disease accounts for more than 15000 deaths annually[1-3]. With 30% of all adult liver transplant surgeries performed annually in patients with HCV-related end-stage liver disease, HCV continues to be the leading indication for liver transplantation (LT) in the US[4,5]. However, with the introduction of second generation direct-acting antiviral (DAA) agents five years ago, the paradigm of HCV treatment landscape has shifted dramatically. With a very favorable safety profile and high rates of sustained virological response (SVR) of over 95%, the newer and all-oral DAA-based regimens have provided an unprecedented opportunity to cure HCV. Although HCV-disease burden remains substantial at the moment, it is estimated that, within next decade, most patients with HCV in clinical practice will likely have attained SVR[6]. Furthermore, SVR can forestall the progression of liver disease with subsequent reduction in liver-related complications including hepatocellular carcinoma (HCC), hepatic decompensation, and both liver related as well as all-cause mortality[7]. Although the newer DAA-based therapy has been highly effective, the optimal timing of HCV treatment in LT candidates is unclear and remains a subject of much debate. Achieving SVR following a DAA-based therapy in LT candidates with HCV-related cirrhosis may result in decrease in the Model for End-Stage Liver Disease (MELD) score without a significant improvement in quality of life due to persistence of end-stage liver disease-related complications (a concept of ‘MELD purgatory’)[8,9]. Furthermore, the improvement in MELD score may result in removal of these candidates from transplant waitlist thus reducing the likelihood of undergoing LT and potentially contributing to waitlist mortality. In addition to examining the validity of ‘MELD purgatory’, we seek to evaluate the current data pertaining to chronic HCV treatment in the context of liver transplantation.
NATURAL HISTORY OF HCV PRIOR TO LIVER TRANSPLANTATION
HCV can cause both acute and chronic infections although the latter is more common. Within two weeks after exposure to HCV, up to 20% of patients develop acute hepatitis, which is often asymptomatic although a few may experience nausea, anorexia, malaise, and jaundice. Due to inability to spontaneously clear the virus, a clear majority of patients (approximately 55%-85%) develop chronic HCV infection. As a result of chronicity and slow progression, HCV leads to cirrhosis in 10%-40% of patients over a period of 20-30 years[10]. However, in certain populations such as those with HIV co-infection, elderly patients, and liver transplant recipients, a rapid progression to advanced stages of liver disease can occur[11]. Since most patients with chronic HCV infection are asymptomatic, the diagnosis of HCV is often delayed until after the development of cirrhosis or onset of an index complication. After the onset of cirrhosis, the rates of hepatic decompensation in these patients are 3%-6% and annual risk of HCC is 1%-5%[12]. The rates of decompensation and HCC are influenced by interplay of a variety of host and viral factors. HCV accounts for 55% of all HCC in cirrhosis patients currently, making it the leading cause of HCC in the US[13]. There is 15%-20% risk of mortality within one year after the development of hepatic decompensation, and LT usually serves as the only life-saving therapeutic option[14].
NATURAL HISTORY OF HCV IN LIVER TRANSPLANT RECIPIENTS
HCV-infected patients with end-stage liver disease with or without HCC have a clear survival advantage with LT, which serves as a curative therapy. However, in patients with pre-transplant viremia who do not receive HCV treatment prior to LT, post-transplant HCV recurrence is usually immediate and universal. HCV reinfection results in graft dysfunction with progression to cirrhosis in about one-third of patients within 5 years after LT compared to less than 5% in non-transplant patients[15]. Spontaneous viral clearance following LT is reported in a few published cases although the underlying mechanism is not clearly understood[16]. Nevertheless, HCV infection of allograft has protracted course with rapid progression and higher mortality risk compared to non-transplant chronic HCV infection.
The recurrent HCV infection is defined as presence of HCV RNA in serum and/or liver, however histological confirmation is required for establishing the recurrent disease[17]. Histopathological changes related to recurrent disease in the allograft are similar to those of an immunocompetent patient, usually develop within 3 months after the LT surgery, with 70%-90% of transplant recipients demonstrating the changes of chronic hepatitis at 1 year, and 90%-95% at 5 years[18]. Similarly, the rates of decompensation after onset of graft cirrhosis are > 40% and > 60% at 1 and 3 years respectively[19,20], whereas in pre-transplant chronic HCV patients the rates are < 5% and < 20% at 1 and 5 years respectively[21,22].
In pre-DAA era, due to poorly tolerated, ineffective interferon-based therapy and accelerated fibrosis, LT recipients with HCV had inferior graft and patient survival compared to those who underwent LT for non-HCV indications. In a large study using United Network for Organ Sharing (UNOS) data comparing 4439 HCV-positive and 6597 HCV-negative recipients, the 5-year graft and patient survival rates were found to be 57% and 70% in HCV-positive recipients compared with 68% and 77% respectively in HCV-negative counterparts[23]. However, with the availability of highly effective and safer DAA-based agents, HCV-positive LT recipients are expected to have outcomes similar to those undergoing LT for other indications[24,25].
TREATMENT OF HCV PRIOR TO LIVER TRANSPLANTATION
In pre-DAA era, pegylated interferon and ribavirin were cornerstone of HCV treatment. Prior studies have shown that achieving SVR by viral eradication with interferon-based treatment regimen has shown to significantly reduce the rates of cirrhosis, decompensation, HCC, and both liver-related and all-cause mortality[7,26]. However, interferon-based regimen was poorly tolerated due to high rates of adverse events, had poor clinical efficacy with low SVR rates and could not be used in patients with decompensated cirrhosis[27]. DAA-based therapy, on the other hand, is highly efficacious with high rates of SVR, well tolerated leading to better patient adherence, and can be used safely in patients with advanced liver disease[28]. Although these attributes can be compelling for clinicians to treat all chronic HCV patients, it is however important to understand the optimal timing of HCV therapy.
Recently, several studies have demonstrated very favorable results with DAAs in patients with advanced liver disease before and after LT. In SOLAR-1 trial in 2015, a combination of sofosbuvir, ledipasvir and ribavirin for 12-24 wk achieved high rates of SVR at 12 wk (SVR12) in patients with advanced liver disease, including those with decompensated cirrhosis both before and after LT[25]. In this landmark trial, SVR12 in non-transplant cohort with moderate to severe hepatic impairment [Child-Turcotte-Pugh (CTP) class B and C] was 86%-89%, whereas the rates in transplant recipients were 96%-98% in mild hepatic impairment group (CTP A), 85%-88% in moderate hepatic impairment group (CTP B), and 60%-75% severe hepatic impairment group (CTP C). More importantly, among seven patients who required re-transplantation, including four patients who underwent LT prior to completion of HCV therapy, six patients achieved SVR 12 suggesting the high efficacy of DAAs in preventing the recurrence of HCV infection after LT.
DAAs have shown to be equally effective in different ethnic groups and certain high-risk HCV populations including elderly, and treatment experienced patients who failed prior therapies. In a multicenter, international ASTRAL-1 trial, a combination sofosbuvir and velpatasvir noted high efficacy rates in African-Americans and previously failed, treatment experienced HCV patients[29]. Similarly, ASTRAL-2 and ASTRAL-3 trials showed that HCV patients with genotype 2 and 3 infection achieved SVR rates of 99% and 95% respectively, which were superior to standard therapy with sofosbuvir and ribavirin which had SVR rate of 80%[30]. DAA agents are highly effective in elderly patients as well and are generally safe. In a retrospective study evaluating the safety and efficacy of ledipasvir/sofosbuvir with or without ribavirin, elderly HCV patients (age > 65 years) with genotype 1 infection achieved similar SVR rates (98%) compared to the younger subjects (97%), however treatment related adverse events that lead to discontinuation of therapy in elderly subjects was largely related to ribavirin rather than ledipasvir/sofosbuvir[31]. DAA-based therapy, through an expanded access program, in patients with decompensated cirrhosis (CTP B and C) who are at risk of irreversible disease achieved overall SVR of 81.6% (genotype 1, 90.5% and genotype 3, 68.8%)[32]. Importantly, within 6 months following viral clearance, 60% patients noted improvement in hepatic function while 17% had no change and 23% had worsening MELD score.
These major trials have repeatedly demonstrated that DAA-based therapy is not only efficacious but well tolerated across the wide spectrum of patients with HCV-related liver disease including those with advanced and decompensated cirrhosis. Data from integrated safety analysis of SOLAR 1 and 2 trials showed that a combination of sofosbuvir and ledipasvir with ribavirin in decompensated liver cirrhosis patients was generally safe and well-tolerated and major adverse events noted in 28%-30% patients and death in 5%[33]. Although all the major studies had enrolled HCV-patients with decompensated cirrhosis, it is important to note that the proportion of patients with higher MELD scores (> 20) and CTP-C was very low. Therefore, these results should be applied with caution in patients with severe hepatic impairment (higher MELD scores).
While all HCV patients can and should be treated, it may not be beneficial in patients for whom LT is the only curative option, for example, those with advanced liver disease or those with HCC. Additionally, after achieving viral clearance before LT, HCV patients are no longer able to accept the organs from HCV-positive donors, further shrinking the already limited donor pool. This is particularly relevant in midst of opioid epidemic, where the young and otherwise healthy HCV-positive donors are becoming increasingly available due to deaths related to overdose. In regions with high HCV prevalence, HCV treatment prior to LT may potentially extend the transplant wait period and thus increasing the risk of waitlist dropout due to inability to accept the offer from HCV-positive donors. Therefore, the decision of HCV treatment before or after LT largely depends on proportion of HCV-positive donors in the local and regional areas[34]. If the proportion of HCV-positive donor is sufficiently high, it may be beneficial to wait and treat HCV infection after transplantation. However, in future, policies may change necessitating the uniform acceptance of HCV-positive donors by all patients with or without HCV.
COST-EFFECTIVENESS OF HCV TREATMENT
HCV patients who are already treated and cured prior to LT can still accept HCV-positive donors, however, these patients require re-treatment for recurrent HCV infection after transplantation incurring additional health-care costs associated with generally expensive DAA agents. But, the cost of HCV treatment should be examined in the context of overall costs associated with LT surgery, which is several fold higher than HCV therapy. In addition to mortality benefit, substantial cost-savings can be obtained as a result of reduction in the hospitalizations related to complications and need for transplantation[35]. Younossi et al[36], showed that number needed to treat with DAAs to prevent one LT in patients with compensated cirrhosis is 15, which is quite remarkable. However, this study does not include the patients with advanced liver disease or decompensated cirrhosis. Results from another European study involving LT candidates demonstrated that following the DAA therapy, one out of five patients on transplant waitlist were successfully delisted due to significant clinical improvement[37]. Nevertheless, in patients with severe hepatic dysfunction and HCC in whom the LT cannot be avoided, HCV treatment prior to LT may not be beneficial or cost-effective[35]. Advantages and disadvantages of this treatment strategy are summarized (Table 1).
Table 1.
Advantages and disadvantages of hepatitis C virus treatment in liver transplant candidates before liver transplantation
| Advantages | Disadvantages |
| 1. Liver function and MELD score may improve | 1. MELD score may improve but with ongoing poor health (MELD purgatory) |
| 2. Liver transplantation may no longer be necessary | 2. Possibly eliminates the option of a curative treatment for liver disease |
| 3. Societal benefits given the scarcity of organs and limited donor pool | 3. May limit access to HCV-positive donors, thereby prolonging the transplant waitlist time and risk of dropout or death |
| 4. Prevent post-transplant recurrence of HCV | 4. If treatment fails, risk of resistance to NS5A inhibitors and compromised SVR rates when re-treating after liver transplantation |
| 5. Cost savings if liver transplantation can be obviated |
HCV: Hepatitis C virus; SVR: Sustained virological response; MELD: Model for end-stage liver disease.
TREATMENT OF HCV FOLLOWING LIVER TRANSPLANTATION
HCV patients who are viremic at the time of transplantation almost always develop recurrent HCV infection after LT. Treatment of recurrent HCV infection in LT recipients followed by viral eradication results in significant improvement in post-transplant mortality and morbidity[38]. Prior to the approval DAAs, standard of care for recurrent HCV infection was based on pegylated interferon and ribavirin, which were poorly tolerated and had sub-optimal success. A systematic review by Berenguer et al[39], involving 19 studies and total 611 LT recipients with recurrent HCV infection that were treated with interferon-based therapy, reported low rate of SVR (30.2%) due to significant adverse effects that lead to reduction in dose in 73% patients and discontinuation of therapy in 27.6%[39]. In contrast, DAA-based therapy is well tolerated and efficacious with high rates of SVR in LT recipients. Sofosbuvir plus ribavirin for 24 wk was first all-oral DAA regimen that was used in LT recipients which achieved SVR12 rate of 70%[40]. The combination of Sofosbuvir and simeprevir in several clinical trials demonstrated better tolerability and improved efficacy. This combination achieved SVR12 in 88% of LT recipients, however the rate was lower (64%) in LT recipients with advanced fibrosis[41,42]. Recently, in ALLY-1 study that included 55% LT recipients with advanced fibrosis, a combination of sofosbuvir, declatasavir, and ribavirin for 12 wk was well-tolerated and achieved high SVR rate (91%-95%) across different genotypes[43]. Although all DAAs are generally safe and approved in post-transplant setting, attention must be paid to drug-drug interaction especially with immunosuppressive agents. For example, simeprevir is contraindicated in LT recipients who are on cyclosporine and ritonavir can increase the tacrolimus level 57 to 68-fold and cyclosporine level 4.3 to 5.8-fold[44]. Therefore, careful selection of DAA agents is warranted based on the patient’s immunosuppressive therapy.
Fibrosing cholestatic hepatitis (FCH) is a severe form of HCV recurrence that results in progressive hepatic dysfunction and graft failure which was associated with high mortality in interferon era. However, in DAA era, the outcomes associated with FCH patients have been encouraging. In a compassionate use program, treatment of FCH patients with sofosbuvir and simeprevir achieved SVR12 of 80%[45]. Despite the absence of large prospective studies, the available evidence favors early treatment of recurrent HCV in post-transplant setting before the onset of fibrosis to achieve improved patient and graft survival.
CONCEPT OF ‘MELD PURGATORY’
Current LT allocation algorithm employs MELD score based prioritization, where sicker patients with higher MELD score are transplanted first. DAA-based therapy with viral eradication in candidates on LT waitlist may improve MELD score and hepatic dysfunction sufficiently enough that they may no longer require LT. This is an ideal scenario. However, some patients may experience decrease in MELD score without significant improvement in quality of life or hepatic dysfunction that puts them at risk of waitlist dropout or death- ‘MELD purgatory’. These patients perhaps are best served by deferring the HCV treatment until after LT. A European study demonstrated that after achieving SVR following HCV treatment, 1 out of 5 candidates were removed from LT waitlist due to significant reversal of hepatic dysfunction[37]. More recently, another study from Spain showed that about a quarter of patients with decompensated cirrhosis were successfully removed from LT waitlist due to clinical improvement[46]. However, both studies demonstrated that the patients with MELD > 20 were less likely to be removed from waitlist due to inadequate clinical or biochemical improvement. Thus, algorithms for HCV treatment have been proposed to avoid ‘MELD purgatory’-authors recommended HCV treatment in patients with hepatic decompensation and MELD < 20 and scheduled for living donor LT[47]. However, patients with MELD 20-27 can be treated depending on the regional trends. In patients with MELD > 27 and/or severe kidney dysfunction (GFR < 30) should be treated after LT[47]. The safety and efficacy of DAAs in chronic kidney disease patients (GFR < 30) and those on hemodialysis is unknown. A few recent single center studies involving HCV patients with advanced chronic kidney disease (GFR < 30) or those on hemodialysis have shown favorable results with DAA agents in terms of safety and SVR rates compared to general population[48,49]. Although, these are small and single center studies, the preliminary results are encouraging, and evidence regarding DAA therapy in renal failure patients continues to emerge.
Finally, if transplantation is imminent and in the setting of severe hepatic impairment, it is prudent to wait and treat HCV infection after transplantation. Nonetheless, DAA-based therapy is beneficial and recommended in patients with mild hepatic impairment and select patients with moderate to severe hepatic impairment.
To avoid ‘MELD purgatory’, we suggest a modified algorithm (Figure 1) summarizing the approach to optimal timing of HCV therapy in LT candidates. At present, evidence favors DAA-based HCV therapy in patients with lower MELD scores and mild hepatic impairment in pre-transplant period. Additionally, with exception to those needing imminent LT, carefully selected patients with moderate hepatic decompensation may also benefit from HCV therapy prior to transplantation.
Figure 1.
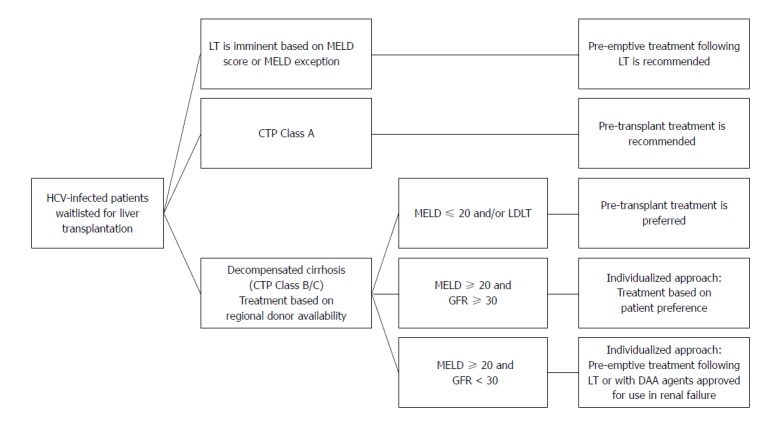
A pragmatic treatment approach in hepatitis C virus-infected liver transplant candidates. HCV: Hepatitis C virus; MELD: Model for End-Stage Liver Disease; LT: Liver transplantation; CTP: Child-Turcotte-Pugh; GFR: Glomerular filtration rate; LDLT: Living donor liver transplantation.
CONCLUSION
The advent of DAA agents has revolutionized the HCV treatment landscape. Due to their safety profile, effectiveness in viral eradication and tolerability, DAA agents can be used in all HCV patients including those with advanced hepatic impairment. The optimal timing of HCV therapy in LT candidates is long debated. DAA agents have shown to improve the hepatic function to the degree where transplantation may no longer be required in some LT candidates whereas in others, the reduction in MELD score may not necessarily improve poor quality of life. Therefore, it is crucial to identify such candidates to maintain the access to LT and treat HCV in post-transplant setting. The viral eradication and improvement in hepatic function with subsequent delisting from LT waitlist is not only cost-effective but has a substantial societal benefit in the setting of limited donor pool. The available data suggests that LT candidates with mild to moderate impairment benefit from pre-transplant HCV treatment, whereas post-transplant DAA therapy may be employed for those in whom LT cannot be avoided. However, the decision to treat LT candidates should also reflect patient preferences, local/regional waitlist parameters and specific needs of a transplant center. Nevertheless, future studies are needed to identify the accurate predictors of improvement in quality of life and hepatic function in LT candidates following DAA therapy to better guide the providers caring for these patients.
Footnotes
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
Conflict-of-interest statement: The authors have no conflict of interest related to this publication.
Peer-review started: November 7, 2017
First decision: November 30, 2017
Article in press: December 12, 2017
P- Reviewer: Kakaei F, Marzaban R S- Editor: Gong ZM L- Editor: A E- Editor: Li RF
Contributor Information
Chiranjeevi Gadiparthi, Division of Gastroenterology and Hepatology, University of Tennessee Health Sciences Center, Memphis, TN 38104, United States.
George Cholankeril, Division of Gastroenterology and Hepatology, Stanford University School of Medicine, Stanford, CA 94304, United States.
Brandon J Perumpail, Drexel University College of Medicine, Philadelphia, PA 19129, United States.
Eric R Yoo, Department of Medicine, Santa Clara Valley Medical Center, San Jose, CA 95128, United States.
Sanjaya K Satapathy, Division of Gastroenterology and Hepatology, University of Tennessee Health Sciences Center, Memphis, TN 38104, United States.
Satheesh Nair, Division of Gastroenterology and Hepatology, University of Tennessee Health Sciences Center, Memphis, TN 38104, United States.
Aijaz Ahmed, Division of Gastroenterology and Hepatology, Stanford University School of Medicine, Stanford, CA 94304, United States. aijazahmed@stanford.edu.
References
- 1.Denniston MM, Jiles RB, Drobeniuc J, Klevens RM, Ward JW, McQuillan GM, Holmberg SD. Chronic hepatitis C virus infection in the United States, National Health and Nutrition Examination Survey 2003 to 2010. Ann Intern Med. 2014;160:293–300. doi: 10.7326/M13-1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edlin BR, Eckhardt BJ, Shu MA, Holmberg SD, Swan T. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology. 2015;62:1353–1363. doi: 10.1002/hep.27978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ryerson AB, Eheman CR, Altekruse SF, Ward JW, Jemal A, Sherman RL, Henley SJ, Holtzman D, Lake A, Noone AM, et al. Annual Report to the Nation on the Status of Cancer, 1975-2012, featuring the increasing incidence of liver cancer. Cancer. 2016;122:1312–1337. doi: 10.1002/cncr.29936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crespo G, Mariño Z, Navasa M, Forns X. Viral hepatitis in liver transplantation. Gastroenterology. 2012;142:1373–1383.e1. doi: 10.1053/j.gastro.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Moyer VA; U. S. Preventive Services Task Force. Screening for hepatitis C virus infection in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159:349–357. doi: 10.7326/0003-4819-159-5-201309030-00672. [DOI] [PubMed] [Google Scholar]
- 6.Chhatwal J, Wang X, Ayer T, Kabiri M, Chung RT, Hur C, Donohue JM, Roberts MS, Kanwal F. Hepatitis C Disease Burden in the United States in the era of oral direct-acting antivirals. Hepatology. 2016;64:1442–1450. doi: 10.1002/hep.28571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van der Meer AJ, Veldt BJ, Feld JJ, Wedemeyer H, Dufour JF, Lammert F, Duarte-Rojo A, Heathcote EJ, Manns MP, Kuske L, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012;308:2584–2593. doi: 10.1001/jama.2012.144878. [DOI] [PubMed] [Google Scholar]
- 8.Bunchorntavakul C, Reddy KR. Treat chronic hepatitis C virus infection in decompensated cirrhosis - pre- or post-liver transplantation? the ironic conundrum in the era of effective and well-tolerated therapy. J Viral Hepat. 2016;23:408–418. doi: 10.1111/jvh.12534. [DOI] [PubMed] [Google Scholar]
- 9.Carrion AF, Khaderi SA, Sussman NL. Model for end-stage liver disease limbo, model for end-stage liver disease purgatory, and the dilemma of treating hepatitis C in patients awaiting liver transplantation. Liver Transpl. 2016;22:279–280. doi: 10.1002/lt.24383. [DOI] [PubMed] [Google Scholar]
- 10.Lingala S, Ghany MG. Natural History of Hepatitis C. Gastroenterol Clin North Am. 2015;44:717–734. doi: 10.1016/j.gtc.2015.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davis GL, Alter MJ, El-Serag H, Poynard T, Jennings LW. Aging of hepatitis C virus (HCV)-infected persons in the United States: a multiple cohort model of HCV prevalence and disease progression. Gastroenterology. 2010;138:513–521, 521.e1-521.e6. doi: 10.1053/j.gastro.2009.09.067. [DOI] [PubMed] [Google Scholar]
- 12.Wray CM, Davis AM. Screening for hepatitis C. JAMA. 2015;313:1855–1856. doi: 10.1001/jama.2015.2833. [DOI] [PubMed] [Google Scholar]
- 13.Snowberger N, Chinnakotla S, Lepe RM, Peattie J, Goldstein R, Klintmalm GB, Davis GL. Alpha fetoprotein, ultrasound, computerized tomography and magnetic resonance imaging for detection of hepatocellular carcinoma in patients with advanced cirrhosis. Aliment Pharmacol Ther. 2007;26:1187–1194. doi: 10.1111/j.1365-2036.2007.03498.x. [DOI] [PubMed] [Google Scholar]
- 14.Bunchorntavakul C, Reddy KR. Management of Hepatitis C Before and After Liver Transplantation in the Era of Rapidly Evolving Therapeutic Advances. J Clin Transl Hepatol. 2014;2:124–133. doi: 10.14218/JCTH.2014.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferrarese A, Zanetto A, Gambato M, Bortoluzzi I, Nadal E, Germani G, Senzolo M, Burra P, Russo FP. Liver transplantation for viral hepatitis in 2015. World J Gastroenterol. 2016;22:1570–1581. doi: 10.3748/wjg.v22.i4.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kogiso T, Hashimoto E, Ikarashi Y, Kodama K, Taniai M, Torii N, Egawa H, Yamamoto M, Tokushige K. Spontaneous clearance of HCV accompanying hepatitis after liver transplantation. Clin J Gastroenterol. 2015;8:323–329. doi: 10.1007/s12328-015-0602-y. [DOI] [PubMed] [Google Scholar]
- 17.Berenguer M, López-Labrador FX, Wright TL. Hepatitis C and liver transplantation. J Hepatol. 2001;35:666–678. doi: 10.1016/s0168-8278(01)00179-9. [DOI] [PubMed] [Google Scholar]
- 18.Berenguer M, Rayón JM, Prieto M, Aguilera V, Nicolás D, Ortiz V, Carrasco D, López-Andujar R, Mir J, Berenguer J. Are posttransplantation protocol liver biopsies useful in the long term? Liver Transpl. 2001;7:790–796. doi: 10.1053/jlts.2001.23794. [DOI] [PubMed] [Google Scholar]
- 19.Berenguer M, Prieto M, Rayón JM, Mora J, Pastor M, Ortiz V, Carrasco D, San Juan F, Burgueño MD, Mir J, et al. Natural history of clinically compensated hepatitis C virus-related graft cirrhosis after liver transplantation. Hepatology. 2000;32:852–858. doi: 10.1053/jhep.2000.17924. [DOI] [PubMed] [Google Scholar]
- 20.Pruthi J, Medkiff KA, Esrason KT, Donovan JA, Yoshida EM, Erb SR, Steinbrecher UP, Fong TL. Analysis of causes of death in liver transplant recipients who survived more than 3 years. Liver Transpl. 2001;7:811–815. doi: 10.1053/jlts.2001.27084. [DOI] [PubMed] [Google Scholar]
- 21.Fattovich G, Giustina G, Degos F, Tremolada F, Diodati G, Almasio P, Nevens F, Solinas A, Mura D, Brouwer JT, et al. Morbidity and mortality in compensated cirrhosis type C: a retrospective follow-up study of 384 patients. Gastroenterology. 1997;112:463–472. doi: 10.1053/gast.1997.v112.pm9024300. [DOI] [PubMed] [Google Scholar]
- 22.Niederau C, Lange S, Heintges T, Erhardt A, Buschkamp M, Hürter D, Nawrocki M, Kruska L, Hensel F, Petry W, et al. Prognosis of chronic hepatitis C: results of a large, prospective cohort study. Hepatology. 1998;28:1687–1695. doi: 10.1002/hep.510280632. [DOI] [PubMed] [Google Scholar]
- 23.Forman LM, Lewis JD, Berlin JA, Feldman HI, Lucey MR. The association between hepatitis C infection and survival after orthotopic liver transplantation. Gastroenterology. 2002;122:889–896. doi: 10.1053/gast.2002.32418. [DOI] [PubMed] [Google Scholar]
- 24.Curry MP, Forns X, Chung RT, Terrault NA, Brown R Jr, Fenkel JM, Gordon F, O’Leary J, Kuo A, Schiano T, Everson G, Schiff E, Befeler A, Gane E, Saab S, McHutchison JG, Subramanian GM, Symonds WT, Denning J, McNair L, Arterburn S, Svarovskaia E, Moonka D, Afdhal N. Sofosbuvir and ribavirin prevent recurrence of HCV infection after liver transplantation: an open-label study. Gastroenterology. 2015;148:100–107.e1. doi: 10.1053/j.gastro.2014.09.023. [DOI] [PubMed] [Google Scholar]
- 25.Charlton M, Everson GT, Flamm SL, Kumar P, Landis C, Brown RS Jr, Fried MW, Terrault NA, O’Leary JG, Vargas HE, Kuo A, Schiff E, Sulkowski MS, Gilroy R, Watt KD, Brown K, Kwo P, Pungpapong S, Korenblat KM, Muir AJ, Teperman L, Fontana RJ, Denning J, Arterburn S, Dvory-Sobol H, Brandt-Sarif T, Pang PS, McHutchison JG, Reddy KR, Afdhal N; SOLAR-1 Investigators. Ledipasvir and Sofosbuvir Plus Ribavirin for Treatment of HCV Infection in Patients With Advanced Liver Disease. Gastroenterology. 2015;149:649–659. doi: 10.1053/j.gastro.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 26.Tada T, Kumada T, Toyoda H, Kiriyama S, Tanikawa M, Hisanaga Y, Kanamori A, Kitabatake S, Yama T, Tanaka J. Viral eradication reduces all-cause mortality, including non-liver-related disease, in patients with progressive hepatitis C virus-related fibrosis. J Gastroenterol Hepatol. 2017;32:687–694. doi: 10.1111/jgh.13589. [DOI] [PubMed] [Google Scholar]
- 27.Everson GT, Terrault NA, Lok AS, Rodrigo del R, Brown RS Jr, Saab S, Shiffman ML, Al-Osaimi AM, Kulik LM, Gillespie BW, Everhart JE; Adult-to-Adult Living Donor Liver Transplantation Cohort Study. A randomized controlled trial of pretransplant antiviral therapy to prevent recurrence of hepatitis C after liver transplantation. Hepatology. 2013;57:1752–1762. doi: 10.1002/hep.25976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Osinusi A, Meissner EG, Lee YJ, Bon D, Heytens L, Nelson A, Sneller M, Kohli A, Barrett L, Proschan M, et al. Sofosbuvir and ribavirin for hepatitis C genotype 1 in patients with unfavorable treatment characteristics: a randomized clinical trial. JAMA. 2013;310:804–811. doi: 10.1001/jama.2013.109309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Feld JJ, Jacobson IM, Hézode C, Asselah T, Ruane PJ, Gruener N, Abergel A, Mangia A, Lai CL, Chan HL, et al. Sofosbuvir and Velpatasvir for HCV Genotype 1, 2, 4, 5, and 6 Infection. N Engl J Med. 2015;373:2599–2607. doi: 10.1056/NEJMoa1512610. [DOI] [PubMed] [Google Scholar]
- 30.Foster GR, Afdhal N, Roberts SK, Bräu N, Gane EJ, Pianko S, Lawitz E, Thompson A, Shiffman ML, Cooper C, et al. Sofosbuvir and Velpatasvir for HCV Genotype 2 and 3 Infection. N Engl J Med. 2015;373:2608–2617. doi: 10.1056/NEJMoa1512612. [DOI] [PubMed] [Google Scholar]
- 31.Saab S, Park SH, Mizokami M, Omata M, Mangia A, Eggleton E, Zhu Y, Knox SJ, Pang P, Subramanian M, et al. Safety and efficacy of ledipasvir/sofosbuvir for the treatment of genotype 1 hepatitis C in subjects aged 65 years or older. Hepatology. 2016;63:1112–1119. doi: 10.1002/hep.28425. [DOI] [PubMed] [Google Scholar]
- 32.Foster GR, Irving WL, Cheung MC, Walker AJ, Hudson BE, Verma S, McLauchlan J, Mutimer DJ, Brown A, Gelson WT, et al. Impact of direct acting antiviral therapy in patients with chronic hepatitis C and decompensated cirrhosis. J Hepatol. 2016;64:1224–1231. doi: 10.1016/j.jhep.2016.01.029. [DOI] [PubMed] [Google Scholar]
- 33.Samuel D, Manns M, Forns X, Flamm SL, Reddy KR, Denning J, Arterburn S, Brandt-Sarif T, Pang PS, McHutchison JG, et al. P0774: Ledipasvir/sofosbuvir with ribavirin is safe in >600 decompensated and post liver transplantation patients with HCV infection: An integrated safety analysis of the solar 1 and solar 2 trials. J Hepatol. 2015;62:S620–S621. [Google Scholar]
- 34.Goldberg DS, Blumberg E, McCauley M, Abt P, Levine M. Improving Organ Utilization to Help Overcome the Tragedies of the Opioid Epidemic. Am J Transplant. 2016;16:2836–2841. doi: 10.1111/ajt.13971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tapper EB, Afdhal NH, Curry MP. Before or After Transplantation? A Review of the Cost Effectiveness of Treating Waitlisted Patients With Hepatitis C. Transplantation. 2017;101:933–937. doi: 10.1097/TP.0000000000001611. [DOI] [PubMed] [Google Scholar]
- 36.Younossi ZM, Park H, Saab S, Ahmed A, Dieterich D, Gordon SC. Cost-effectiveness of all-oral ledipasvir/sofosbuvir regimens in patients with chronic hepatitis C virus genotype 1 infection. Aliment Pharmacol Ther. 2015;41:544–563. doi: 10.1111/apt.13081. [DOI] [PubMed] [Google Scholar]
- 37.Belli LS, Berenguer M, Cortesi PA, Strazzabosco M, Rockenschaub SR, Martini S, Morelli C, Donato F, Volpes R, Pageaux GP, Coilly A, Fagiuoli S, Amaddeo G, Perricone G, Vinaixa C, Berlakovich G, Facchetti R, Polak W, Muiesan P, Duvoux C; European Liver and Intestine Association (ELITA) Delisting of liver transplant candidates with chronic hepatitis C after viral eradication: A European study. J Hepatol. 2016;65:524–531. doi: 10.1016/j.jhep.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 38.Picciotto FP, Tritto G, Lanza AG, Addario L, De Luca M, Di Costanzo GG, Lampasi F, Tartaglione MT, Marsilia GM, Calise F, et al. Sustained virological response to antiviral therapy reduces mortality in HCV reinfection after liver transplantation. J Hepatol. 2007;46:459–465. doi: 10.1016/j.jhep.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 39.Berenguer M. Systematic review of the treatment of established recurrent hepatitis C with pegylated interferon in combination with ribavirin. J Hepatol. 2008;49:274–287. doi: 10.1016/j.jhep.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 40.Charlton M, Gane E, Manns MP, Brown RS Jr, Curry MP, Kwo PY, Fontana RJ, Gilroy R, Teperman L, Muir AJ, McHutchison JG, Symonds WT, Brainard D, Kirby B, Dvory-Sobol H, Denning J, Arterburn S, Samuel D, Forns X, Terrault NA. Sofosbuvir and ribavirin for treatment of compensated recurrent hepatitis C virus infection after liver transplantation. Gastroenterology. 2015;148:108–117. doi: 10.1053/j.gastro.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 41.Crittenden NE, Buchanan LA, Pinkston CM, Cave B, Barve A, Marsano L, McClain CJ, Jones CM, Marvin MR, Davis EG, et al. Simeprevir and sofosbuvir with or without ribavirin to treat recurrent genotype 1 hepatitis C virus infection after orthotopic liver transplantation. Liver Transpl. 2016;22:635–643. doi: 10.1002/lt.24422. [DOI] [PubMed] [Google Scholar]
- 42.Jackson WE, Hanouneh M, Apfel T, Alkhouri N, John BV, Zervos X, Zein NN, Hanouneh IA. Sofosbuvir and simeprevir without ribavirin effectively treat hepatitis C virus genotype 1 infection after liver transplantation in a two-center experience. Clin Transplant. 2016;30:709–713. doi: 10.1111/ctr.12738. [DOI] [PubMed] [Google Scholar]
- 43.Poordad F, Schiff ER, Vierling JM, Landis C, Fontana RJ, Yang R, McPhee F, Hughes EA, Noviello S, Swenson ES. Daclatasvir with sofosbuvir and ribavirin for hepatitis C virus infection with advanced cirrhosis or post-liver transplantation recurrence. Hepatology. 2016;63:1493–1505. doi: 10.1002/hep.28446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.AASLD/IDSA HCV Guidance Panel. Hepatitis C guidance: AASLD-IDSA recommendations for testing, managing, and treating adults infected with hepatitis C virus. Hepatology. 2015;62:932–954. doi: 10.1002/hep.27950. [DOI] [PubMed] [Google Scholar]
- 45.Forns X, Charlton M, Denning J, McHutchison JG, Symonds WT, Brainard D, Brandt-Sarif T, Chang P, Kivett V, Castells L, et al. Sofosbuvir compassionate use program for patients with severe recurrent hepatitis C after liver transplantation. Hepatology. 2015;61:1485–1494. doi: 10.1002/hep.27681. [DOI] [PubMed] [Google Scholar]
- 46.Pascasio JM, Vinaixa C, Ferrer MT, Colmenero J, Rubin A, Castells L, Manzano ML, Lorente S, Testillano M, Xiol X, et al. Clinical outcomes of patients undergoing antiviral therapy while awaiting liver transplantation. J Hepatol. 2017;67:1168–1176. doi: 10.1016/j.jhep.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 47.Verna EC. The dynamic landscape of liver transplant in the era of effective hepatitis C virus therapy. Hepatology. 2017;65:763–766. doi: 10.1002/hep.29054. [DOI] [PubMed] [Google Scholar]
- 48.Aggarwal A, Yoo ER, Perumpail RB, Cholankeril G, Kumari R, Daugherty TJ, Lapasaran AS, Ahmed A. Sofosbuvir Use in the Setting of End-stage Renal Disease: A Single Center Experience. J Clin Transl Hepatol. 2017;5:23–26. doi: 10.14218/JCTH.2016.00060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nazario HE, Ndungu M, Modi AA. Sofosbuvir and simeprevir in hepatitis C genotype 1-patients with end-stage renal disease on haemodialysis or GFR <30 ml/min. Liver Int. 2016;36:798–801. doi: 10.1111/liv.13025. [DOI] [PubMed] [Google Scholar]


