Abstract
Background
Although non-invasive telemonitoring in patients with heart failure (HF) does not reduce mortality or hospitalizations, less is known about its effect on health status. This study reports the results of a randomized clinical trial of telemonitoring on health status in patients with HF.
Methods and Results
Among 1,521 patients with recent HF hospitalization randomized in the Tele-HF trial (NCT 00303212), 756 received telephonic monitoring and 765 usual care. Disease-specific health status was measured with the Kansas City Cardiomyopathy Questionnaire (KCCQ) within 2 weeks of discharge and at 3 and 6 months. Repeated measures linear regression models were used to assess differences in KCCQ scores between patients assigned to telemonitoring and usual care over 6 months. The baseline characteristics of the two treatment arms were similar (mean age 61 years, 43% female and 39% black). Over the 6-month follow-up period, there was a statistically significant, but clinically small, difference between the two groups in their KCCQ overall summary and subscale scores. The average KCCQ overall summary score for those receiving telemonitoring was 2.5 points (95% Confidence Interval [CI]= 0.38,4.67 p=0.02) higher than usual care, driven primarily by improvements in symptoms (3.5 points [95% CI=1.18, 5.82], p=0.003) and social function (3.1 points [95% CI=0.30, 6.00], p=0.03).
Conclusions
Telemonitoring results in statistically significant, but clinically small, improvements in health status as compared with usual care. Given that the KCCQ was a secondary outcome, the benefits should be confirmed in future studies.
Keywords: Heart failure, health status, disease management
Journal Subject Terms: Heart Failure, Quality and Outcomes, Information Technology
Although progress has been made in the management of heart failure (HF), a highly prevalent and costly condition, the risks of death and readmission after hospital discharge remain high.1–3 While prior studies have suggested that disease management programs may improve HF readmission outcomes4–6, the results of two large, randomized, multicenter trials have shown that supplementing care with telemonitoring does not reduce death and hospitalizations.7,8 An equally important goal in managing HF, however, is to improve patients’ health status (e.g. their symptoms, function and quality of life).9–11 Telemonitoring allows for more frequent assessment of clinical status with the opportunity to modify medical management (e.g., increase diuretics). Thus, telemonitoring could potentially improve patients’ health status, even without concurrent improvement in survival or readmission rates. While prior studies have reported on telemonitoring’s effects on health status, these studies were smaller, of variable methodologic quality, and described mixed results, creating uncertainty about the impact of telemonitoring on health status.9
The Telemonitoring to Improve Heart Failure Outcomes (Tele-HF) study is the largest randomized trial, to date, to study outcomes in a large group of HF patients enrolled in a telemonitoring program. While the trial found no benefit in terms of survival or hospital readmission7, the impact of telemonitoring on health status was a secondary endpoint and used the well-validated Kansas City Cardiomyopathy Questionnaire (KCCQ) to quantify the impact of telemonitoring on patients’ health status. We report the health status outcomes from this randomized trial to describe the health status benefits of telemonitoring as compared with usual care.
Methods
Study Design
A full description of the study design has been previously published.12 Briefly, Tele-HF was a randomized controlled trial comparing the effectiveness of telemonitoring with usual care in reducing re-hospitalizations and mortality among patients recently hospitalized for HF. Participants from 33 US cardiology practices who were hospitalized for HF were enrolled from 2006–2009. Subjects were excluded if they were younger than 18 years old, non-English or non-Spanish speakers, residents of a long-term care or correctional facility, severely cognitively impaired, or unable to stand for daily weights. Additionally, patients not expected to survive beyond 6 months (for reasons other than HF), patients scheduled for a surgical/medical procedure, or other individuals unable to comply with the study protocol were excluded. Study coordinators at each individual site were responsible for identification and enrollment of subjects. Once enrolled, subjects were randomly assigned to the telemonitoring or usual care arm of the study using a random number-generated sequence, stratified by study site. The study protocol was approved by the Institutional Review Board (IRB) at Yale University as well as the IRBs of each participating site. All study participants provided their informed consent prior to enrolling in the study. The lead author had full access to all the data in the study and hereby takes responsibility for its integrity and data analysis. The data, analytic methods, and study materials are available to others for purposes of reproducing the results or replicating the procedure, and they can be obtained through the National Institute of Health BioLINCC information coordinating center.
Intervention Protocols
Patients in both the telemonitoring and the usual care group were provided with HF educational materials and, if needed, a scale to measure body weight. Clinicians caring for patients in the usual care group were instructed to care for patients according to established national guidelines.13 The Tel-Assurance (Pharos Innovations; Chicago, IL) monitoring system was used for patients enrolled in the telemonitoring arm of the study. Patients randomized into this group were instructed to call a toll-free number daily for six months, respond to a series of automated questions regarding their symptoms, and enter their daily weight. Responses were downloaded to a secure webpage where they were reviewed by a clinician at each site on all weekdays, excluding holidays. Responses meeting pre-specified criteria triggered a “variance” within the system. Variances were flagged for immediate attention by clinicians at the individual site. After reviewing the variances, clinicians were instructed to contact the patient and verify accuracy of the responses. Clinicians were then instructed to provide and document medical recommendations as they would for a routine office visit; medical management protocols were not provided to the participating institutions. Patients who did not call into the system on two consecutive days received an automated reminder call; continued non-participation was followed by a personal phone call to encourage system use.
Health Status and Clinical Assessment
Following study enrollment, site coordinators conducted a brief interview and physical assessment on patients in both the usual care and telemonitoring arms of the study. Additionally, ‘baseline’ (within 2 weeks of enrollment), 3-month, and 6-month telephone interviews were conducted by personnel at the central coordinating site to minimize the burden of data collection at enrolling sites and to ensure consistent interviews across all centers (Figure 1). Information collected during these phone interviews consisted of general health information, health status information, and information related to satisfaction with care. The outcome for this analysis was disease-specific health status, as assessed by the KCCQ. The KCCQ is a validated tool specifically designed to evaluate health status in individuals with HF.14 This 23-item questionnaire assesses several domains of health status including physical limitations, symptoms, symptom stability, self-efficacy, social limitation, and quality of life. The physical limitations, symptoms, quality of life, and social limitations subscales can be combined to produce an overall summary score that was the primary outcome of interest for this analysis. The symptom stability score assesses recent changes in symptoms over the preceding 2 weeks and was not relevant for this longitudinal study. Each domain of the KCCQ is scored from 0–100, with higher scores indicating better health status (fewer symptoms, less social or physical limitations and better quality of life).14 A 5-point difference in the KCCQ overall summary score represents a clinically important difference between groups and within individual patients.15
Figure 1.
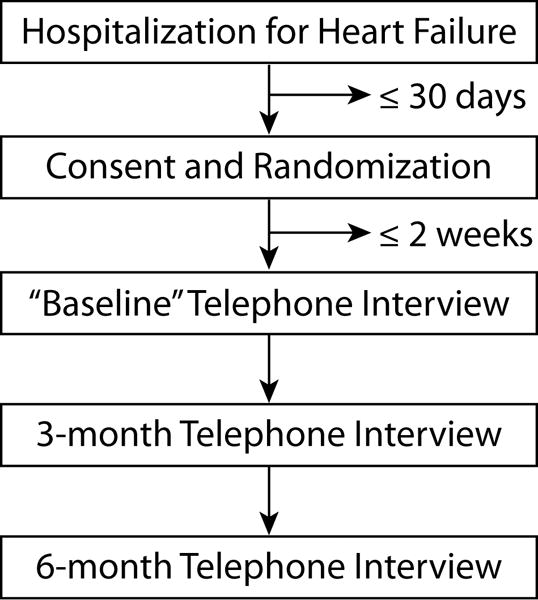
Process of Participants through the trial.
Statistical Analysis
Baseline demographic and clinical characteristics of the two groups were compared using Student’s t-test for continuous variables and chi-square or Fisher’s exact test for categorical variables. Unadjusted KCCQ scores for the telemonitoring group were compared to the usual care group using Student’s t-test. For the main outcome of interest, comparing KCCQ overall summary score between telemonitoring and usual care, and for the secondary comparisons of KCCQ subscale scores, hierarchical linear models were used. The models included fixed effects for treatment, time and treatment by time interaction, within-patient repeated measures over time using an unstructured covariance matrix, and a random effect for site. These hierarchical models adjust for the clustering of patients’ outcomes within site. The baseline KCCQ score assessment, which was collected within 2 weeks of randomization, was considered a follow-up outcome for the purposes of the repeated measures model. A treatment group-by-time interaction was tested to assess whether KCCQ scores differed based upon the study time point (baseline, 3-months, 6-months). This interaction was not significant for any domain of the KCCQ, therefore only the main effect is reported. Patients with no KCCQ data for any of the three time points were excluded from analysis (n=132, 8.0%). To reduce a possible bias related to missing data, the repeated measures models were weighted by the inverse of the probability of participating in follow-up so that patients who were most like those who did not participate in follow-up were given more weight than those who were more completely assessed during follow-up.16 Variables used for inverse probability weighting included race, gender, age, insurance status, body mass index, presence of coronary artery disease (CAD), left ventricular ejection fraction (LVEF) <40%, study group, and mortality during the study period. Given that the a priori-defined main outcome of interest in this study was a comparison of KCCQ overall summary score between telemonitoring and usual care, a correction for multiple comparisons was not performed. To better describe the 6-month health status outcomes across randomized treatment strategies, a cumulative frequency plot was constructed by using the 6-month KCCQ overall summary score for each patient in whom this was available and calculating the percentage of patients in each study arm achieving a KCCQ score greater than or equal to varying thresholds of clinical significance. Dividing 100 by the difference in the proportion of patients at any threshold of KCCQ score provides the number-needed-to-treat for 1 patient assigned to telemonitoring to have a better health status than if they were treated with usual care. Statistical significance was assumed when a 2-sided p-value was <0.05. All study analyses were performed with SAS 9.2 (SAS Institute, Cary, NC).
Results
Of the 1,653 patients enrolled in the Tele-HF study, there were 132 patients (8.0%) with no KCCQ data for any of the three time points who were excluded from analysis, 70 (53.0%) of whom were in the telemonitoring group and 62 (47.0%) in the usual care group (p = 0.46). A comparison of demographic and clinical characteristics for those with and without data for the KCCQ is provided in the Supplementary Appendix.
Among the 1,521 patients with available KCCQ data, 756 were randomized to receive telemonitoring and 765 randomized to receive usual care. There were no significant differences in the baseline demographic or clinical characteristics between the two groups (Table 1). The median age of the study population was 61 years old, 39% were black and 43% were female. Patients were similar with respect to their HF severity, with over half of patients categorized as New York Heart Association (NYHA) class III or IV at the time of randomization. Over two-thirds of patients in each group had depressed ventricular function with an LVEF of <40% and approximately half had co-existing CAD. Mortality was similar in both groups, with roughly one in eleven patients being deceased at 180 days.
Table 1.
Baseline Characteristics of the Study Population, According to Treatment Group
| Telemonitoring | Usual Care | Total | ||
|---|---|---|---|---|
| (n =756) | (n=765) | (N=1521) | P value | |
| Age–mean±s.d. | 61.2±15.2 | 60.8±14.7 | 61.0±14.9 | 0.62 |
| Female–no. (%) | 331 (43.8) | 315 (41.2) | 646 (42.5) | 0.30 |
| Race–no. (%) | 0.53 | |||
| White | 386 (51.1) | 380 (49.7) | 766 (50.4) | |
| Black | 282 (37.3) | 305 (39.9) | 587 (38.6) | |
| Other | 88 (11.6) | 80 (10.5) | 168 (11.0) | |
| Hispanic or Latino ethnic group–no. (%)* | 20 (2.7) | 20 (2.6) | 40 (2.7) | 0.95 |
| Insurance Status–no. (%)† | 0.09 | |||
| None/Self-pay | 100 (13.5) | 79 (10.7) | 179 (12.1) | |
| Commercial Insurance | 232 (31.4) | 214 (29.0) | 446 (30.2) | |
| Public Insurance | 407 (55.1) | 445 (60.3) | 852 (57.7) | |
| Body Mass Index–mean±s.d.‡ | 26.9 ± 11.5 | 26.4 ± 11.3 | 26.6 ± 11.4 | 0.37 |
| Seated SBP (mmHg)–mean±s.d. | 121.5 ± 22.9 | 120.1 ± 21.6 | 120.8 ± 22.2 | 0.22 |
| Serum Potassium (mmol/L)–mean±s.d.§ | 4.1 ± 0.6 | 4.1 ± 0.6 | 4.1 ± 0.6 | 0.77 |
| GFR (ml/minute)ǁ | 58.3 ± 27.3 | 58.7 ± 26.0 | 58.5 ± 26.7 | 0.79 |
| LVEF less than 40%–no. (%) | 515 (68.1) | 520 (68.0) | 1035 (68.0) | 0.95 |
| NYHA Class–no. (%) | ||||
| I | 41(5.4) | 47 (6.1) | 88(5.8) | 0.24 |
| II | 285(37.7) | 280(36.6) | 565(37.2) | |
| III | 373(49.3) | 398(52.0) | 771(50.7) | |
| IV | 57(7.5) | 40(5.2) | 97(6.4) | |
| Coronary Artery Disease–no. (%) | 404 (53.4) | 375 (49.0) | 779 (51.2) | 0.09 |
| Death within 180 days–no. (%) | 70 (9.3) | 72 (9.4) | 142 (9.3) | 0.92 |
19 Patients with missing information for Hispanic/Latino ethnicity group (12 TM, 7 UC)
44 Patients with missing information for Insurance status (17 TM, 27 UC)
2 Patients with missing information for body mass index (1 TM, 1 UC)
Abbreviations: GFR, glomerular filtration rate; LVEF, left ventricular ejection fraction; ml, milliliters; mmHg, millimeters Mercury; mmol/L, millimoles per liter; NYHA, New York Heart Association; no., number; s.d, standard deviation; SBP, systolic blood pressure.
35 Patients with missing information for serum potassium (18 TM, 17 UC)
121 Patients with missing information for GFR (61 TM, 60 UC)
KCCQ scores of those in the telemonitoring arm of the study were compared with those patients receiving usual care (Table 2). The baseline KCCQ scores (obtained within 2 weeks of randomization) were similar for all domains of the KCCQ aside from the total symptom score which was slightly higher in the telemonitoring arm (64.2 ± 26.7 vs. 60.6 ± 28.4, p=0.02). At six-months, KCCQ overall summary scores were higher for those in the telemonitoring arm as compared with usual care (72.3±24.4 vs. 68.5± 26.4, p=0.01). Similarly, those in the telemonitoring arm had improved quality of life at 6-months (68.7±27.1 vs. 65.2±29.4, p=0.04), and better symptom control (74.0±26.0 vs. 69.6±28.9, p=0.007). In the unadjusted analysis, there were no significant differences between the two groups with regards to their physical limitations, social limitations, or self-efficacy at any of the follow-up time points.
Table 2.
Comparison of KCCQ Score Between Treatment Groups
| Telemonitoring | Usual Care | Total | ||
|---|---|---|---|---|
| (n =756) | (n=765) | (N=1521) | P value | |
| KCCQ Overall Summary Score– mean±s.d. | ||||
| Baseline | 60.7 ± 24.1 | 58.6 ± 24.9 | 59.6 ± 24.5 | 0.11 |
| 3-months | 69.9 ± 24.5 | 67. 9 ± 25.8 | 68.9 ± 25.2 | 0.15 |
| 6-months | 72.3 ± 24.4 | 68.5 ± 26.4 | 70.4 ± 25.5 | 0.01 |
| KCCQ Physical Limitations– mean±s.d. | ||||
| Baseline | 69.6 ± 27.8 | 68.7 ± 28.5 | 69.1 ± 28.2 | 0.55 |
| 3-months | 75.8 ± 27.3 | 75.1 ± 27.2 | 75.5 ± 27.2 | 0.70 |
| 6-months | 77.1 ± 26.1 | 74.9 ± 27.9 | 76.0 ± 27.0 | 0.18 |
| KCCQ Total Symptom Score– mean±s.d. | ||||
| Baseline | 64.2 ± 26.7 | 60.6 ± 28.4 | 62.4 ± 27.6 | 0.02 |
| 3-months | 72.2 ± 26.3 | 69.4 ± 27.6 | 70.9 ± 27.0 | 0.07 |
| 6-months | 74.0 ± 26.0 | 69.6 ± 28.9 | 71.8 ± 27.5 | 0.007 |
| KCCQ Self-Efficacy– mean±s.d. | ||||
| Baseline | 83.1 ± 20.9 | 82.9 ± 20.3 | 83.0 ± 20.6 | 0.88 |
| 3-months | 86.2 ± 18.8 | 87.1 ± 17.5 | 86.6 ± 18.2 | 0.39 |
| 6-months | 88.5 ± 18.1 | 87.1 ± 17.8 | 87.8 ± 18.0 | 0.23 |
| KCCQ Quality of Life– mean±s.d. | ||||
| Baseline | 54.4 ± 26.9 | 53.8 ± 27.3 | 54.1 ± 27.1 | 0.65 |
| 3-months | 66.2 ± 28.0 | 64.5 ± 28.8 | 65.4 ± 28.4 | 0.32 |
| 6-months | 68.7 ± 27.1 | 65.2 ± 29.4 | 67.0 ± 28.3 | 0.04 |
| KCCQ Social Limitations – mean±s.d. | ||||
| Baseline | 56.6 ± 33.2 | 53.0 ± 33.0 | 54.8 ± 33.1 | 0.06 |
| 3-months | 66.4 ± 31.2 | 65.4 ± 32.8 | 65.9 ± 32.0 | 0.61 |
| 6-months | 69.7 ± 31.3 | 66.6 ± 32.1 | 68.1 ± 31.7 | 0.12 |
Abbreviations: KCCQ, Kansas City Cardiomyopathy Questionnaire; s.d., standard deviation
Repeated measures analysis with inverse probability weighting16 was used to compare KCCQ scores over the six-month study period (Table 3). Telemonitoring was associated with a statistically significant improvement in patients’ health status, as assessed by the KCCQ overall summary score. Those enrolled in the telemonitoring program had an average overall summary score that was 2.5 (95% CI= 0.38,4.67) points higher than those receiving usual care (p=0.02). Findings were similar for the total symptoms and social limitation subscales, with average scores being 3.5 (p=0.003) and 3.1 (p=0.03) points higher in the telemonitoring group. No significant differences were detected between the groups on the physical limitations, self-efficacy, or quality of life subscales.
Table 3.
Effect of Telemonitoring on KCCQ Score Over 6-Month Study Period
| TM vs. UC Effect Size (95% Confidence Interval) |
P value | |
|---|---|---|
| Overall Summary Score | 2.5 (0.38, 4.67) | 0.02 |
| Physical Limitation | 1.1 (−1.37, 3.47) | 0.39 |
| Total Symptom Score | 3.5 (1.18, 5.82) | 0.003 |
| Self-Efficacy | 0.1 (−1.36, 1.56) | 0.89 |
| Quality of Life | 1.6 (−0.73, 3.96) | 0.18 |
| Social Limitation | 3.14 (0.30, 6.00) | 0.03 |
Abbreviations: TM, telemonitoring; UC, usual care
Figure 2 provides a cumulative response curve of 6-month KCCQ Overall Summary scores. For example, 78.5% of patients in the telemonitoring arm achieved a KCCQ score of ≥50 versus 71.6% in the usual care group (absolute difference = 6.9%), indicating that for every 15 patients treated with telemonitoring, one more would be expected to have fair-to-excellent health status at 6 months as compared with usual care. Likewise, 54.5% of patients in the telemonitoring arm of the study achieved a 6-month KCCQ overall summary score of ≥75 versus 50.8% in the usual care group, indicating that for every 27 patients treated with telemonitoring, one more would be expected to have good-to-excellent health status at 6 months as compared with usual care.
Figure 2.
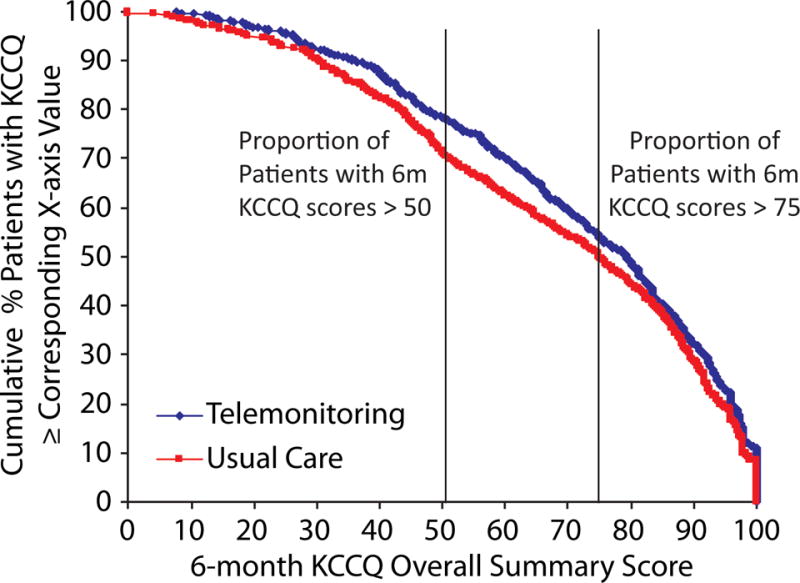
Cumulative Frequency Plot showing percentage of patients (Telemonitoring vs. Usual Care) achieving varying 6-month KCCQ overall summary scores.
Discussion
In this multicenter, randomized, controlled trial, we found that patients randomized to receive telemonitoring had a statistically significant, but small, improvement in their disease-specific health status as compared with those who received usual care. KCCQ overall summary scores for patients enrolled in the telemonitoring arm of the study were, on average, 2.5 points higher over the first 6 months, as compared with usual care, and the number needed to treat (NNT) for achieving clinically important thresholds of better health status ranged from 15 to 27 for patients experiencing better health status at 6 months, depending on the threshold selected. In contrast to the absence of a survival or re-hospitalization benefit, these analyses demonstrate a small improvement in patients’ health status, particularly their symptom control and social functioning. These results support the need for more definitive testing of the effect of non-invasive telemonitoring on health status as part of future studies.
This analysis, conducted within the largest randomized trial to date of telemonitoring in HF, adds important insight to a literature historically clouded with mixed findings in patient-related outcomes.5–7 In the TIM-HF randomized controlled trial of ambulatory patients with HF, participants were randomized to remote telemonitoring that included daily blood pressure and body weight recordings versus usual care. This intervention was associated with an improvement in general health status over a 2-year follow-up period, as assessed with the SF-36.8 Similarly, a smaller randomized trial of ambulatory HF patients managed with a comprehensive, telephone-based disease management program showed improved disease-specific health status as measured by the KCCQ (mean change of 16.3 points in intervention group and 1.2 points in control group).17 Health status improvements were also present in a recent meta-analysis of all prior structured telephone support (STS) and non-invasive telemonitoring programs for patients with HF, as well as reduction in heart failure hospitalizations.18 It is notable that the efficacy of both interventions in improving disease-specific health status was limited by mixed-quality evidence. Of 43 studies included in this systematic review, 11 non-invasive telemonitoring studies reported on quality of life. Although using different health status measures, 9 (82%) of the structured telephone support studies and 5 (45%) of the non-invasive telemonitoring studies showed an improvement, while the others showed no difference. Only two telemonitoring studies used the KCCQ to measure health status outcomes.19,20 Of these, one small study found statistically significant results in favor of the intervention group19, while the other did not provide a complete report of KCCQ changes during the study period.20 In our large randomized study, our findings were congruent, but more precise, than these prior reports.
Our findings require a balanced interpretation. Whereas previous work has suggested that a mean difference in the KCCQ overall summary score of five points is clinically important15, the mean difference in this study was smaller. While other clinical trials with even smaller group differences concluded a health status benefit from interventions (e.g. the mean benefit from exercise in ACTION-HF was 1.93)21, we acknowledge that some may interpret the small differences observed in this study as not being sufficiently clinically important to justify the use of telemonitoring. Moreover, this is a secondary outcome of a randomized trial and so the effect should be replicated to provide more confidence in the findings.
To help facilitate the interpretation of our results, we compared the proportion of patients with KCCQ overall summary scores greater than 50 (fair-to-excellent health status) and greater than 75 (good-to-excellent health status) at six months. From these comparisons, we calculated an NNT of 15 and 27, respectively. This suggests that for every 15 patients offered telemonitoring, one would have fair-to-excellent health-status as compared with not offering any of these patients telemonitoring therapy and that for every 27 patients offered telemonitoring, one would have good-to-excellent health status. While some would perceive this as a good return for their investment, others might not.
The findings of this study should be interpreted in consideration of the following potential limitations. First, patients were not blinded to the intervention and this may have biased their reports of their health status. Second, the KCCQ assesses health status over the preceding 2 weeks and health status information in our study was first collected within 2 weeks of study enrollment and randomization and a true change from the time of randomization was not obtained. Given the similar initial KCCQ scores between groups, however, we do not believe that this timing altered the comparison of the treatment arms at 6 months and the improved health status took longer than 2 weeks to be achieved. Third, health status information was not available for all patients at all time points. However, the rates of missing KCCQ were similar for both treatment arms and the use of inverse probability weighting for the likelihood of participating in follow-up assessments should minimize the generalizability of our findings across the entire population. Fourth, the small mean differences between groups may mask substantial benefits to a sub-group of patients and further work to identify patient characteristics associated with greater benefits from tele-monitoring are warranted. Fifth, as an NIH-funded clinical trial with support for implementation and monitoring the intervention, the results in usual care may be different than that observed in this study. Finally, one out of seven patients in the intervention arm never activated the system and overall adherence to telemonitoring declined - from 90.2% to 55.1% over the follow-up period. While these proportions are greater than those described previously22–25, our ability to make conclusive comparisons was limited by the absence of a uniform definition for telemonitoring “adherence.” Given that the patients participating in the trial formally agreed to participate, the true activation and attrition rates in routine clinical care may be even larger and the differences in health status smaller than observed in this study.
Conclusions
In a secondary analysis of a large, randomized-controlled trial comparing telemonitoring with usual care for HF patients, telemonitoring using KCCQ was associated with statistically significant but small improvements in disease-specific health status over the first 6 months of treatment. In the absence of any benefits from telemonitoring on mortality or hospitalization rates, these data suggest that it may serve a role in improving patients’ symptoms and function after a recent HF hospitalization and be worthy of further testing of the reproducibility of this finding.
Supplementary Material
What is Known
Telemonitoring in heart failure allows for more frequent assessment of clinical status with the opportunity to modify medical management (e.g., increase diuretics), thereby potentially improving patients’ health status
Prior studies have reported on telemonitoring’s impact on health status, but these were smaller, of variable methodologic quality, and described mixed results
What the Study Adds
In this largest, randomized trial to date of telemonitoring in heart failure, we found that patients assigned to receive telemonitoring experienced a statistically significant, but small, improvement in their disease-specific health status as compared to patients in the usual care arm
At 6 months, for every 15 patients offered telemonitoring compared to usual care, one had fair-to-excellent health-status (KCCQ > 50); for every 27 patients offered telemonitoring compared to usual care, one had good-to-excellent health-status (KCCQ > 75)
Acknowledgments
All authors have reviewed and approved the final manuscript.
Sources of Funding: This work was supported by grants U01 HL105270 (Center for Cardiovascular Outcomes Research at Yale University) and R01 HL080228 (Telemonitoring to Improve Heart Failure Outcomes [Tele-HF]), both from the National Heart, Lung, and Blood Institute. The NIH had no role in the analysis, interpretation, and decision to publish the results. Dr. Jayaram and Dr. Khariton were supported by a T32 training grant from the National Heart, Lung, and Blood Institute. Dr. Chaudhry is the recipient of a Paul Beeson/K23 Career Development Award (K23AG030986) from the National Institute on Aging. Miss Hodshon is a Yale University employee. Her salary is funded in part by grants from the National Heart Lung and Blood Institute, the US Food and Drug Administration, Medtronic, and Johnson & Johnson.
Disclosures: Dr. Spertus discloses grant funding from NIH, PCORI, Lilly, Abbott Vascular and Genentech. He serves on Scientific Advisory Boards for United Healthcare, Novartis, Amgen and Bayer. He has intellectual property rights for the Seattle Angina Questionnaire, Kansas City Cardiomyopathy Questionnaire, Peripheral Artery Questionnaire and an equity interest in Health Outcomes Sciences. Dr. Krumholz discloses that he is the recipient of research grants from Medtronic and from Johnson & Johnson, through Yale University, to develop methods of clinical trial data sharing and is chair of a cardiac scientific advisory board for United Health. All other listed authors have no affiliation with industry.
Footnotes
Clinical Trial Registration: clinicaltrials.gov; URL: NCT00303212
References
- 1.Liao L, Allen LA, Whellan DJ. Economic burden of heart failure in the elderly. Pharmacoeconomics. 2008;26:447–462. doi: 10.2165/00019053-200826060-00001. [DOI] [PubMed] [Google Scholar]
- 2.Kosiborod M, Lichtman JH, Heidenreich PA, Normand SL, Wang Y, Brass LM, Krumholz HM. National trends in outcomes among elderly patients with heart failure. Am J Med. 2006;119:616 e611–617. doi: 10.1016/j.amjmed.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 3.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 4.Gonseth J, Guallar-Castillon P, Banegas JR, Rodriguez-Artalejo F. The effectiveness of disease management programmes in reducing hospital re-admission in older patients with heart failure: a systematic review and meta-analysis of published reports. Eur Heart J. 2004;25:1570–1595. doi: 10.1016/j.ehj.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 5.Dendale P, De Keulenaer G, Troisfontaines P, Weytjens C, Mullens W, Elegeert I, Ector B, Houbrechts M, Willekens K, Hansen D. Effect of a telemonitoring-facilitated collaboration between general practitioner and heart failure clinic on mortality and rehospitalization rates in severe heart failure: the TEMA-HF 1 (TElemonitoring in the MAnagement of Heart Failure) study. Eur J Heart Fail. 2012;14:333–340. doi: 10.1093/eurjhf/hfr144. [DOI] [PubMed] [Google Scholar]
- 6.Koehler F, Winkler S, Schieber M, Sechtem U, Stangl K, Bohm M, de Brouwer S, Perrin E, Baumann G, Gelbrich G, Boll H, Honold M, Koehler K, Kirwan BA, Anker SD. Telemedicine in heart failure: pre-specified and exploratory subgroup analyses from the TIM-HF trial. International journal of cardiology. 2012;161:143–150. doi: 10.1016/j.ijcard.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Chaudhry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, Lin Z, Phillips CO, Hodshon BV, Cooper LS, Krumholz HM. Telemonitoring in patients with heart failure. N Engl J Med. 2010;363:2301–2309. doi: 10.1056/NEJMoa1010029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koehler F, Winkler S, Schieber M, Sechtum U, Stangl K, Bohm M, Boll H, Baumann G, Honold M, Koehler K, Gelbrich G, Kirwan BA, Anker SD, Telemedical Interventional Monitoring in Heart Failure Investigators Impact of remote telemedical management on mortality and hospitalizations in ambulatory patients with chronic heart failure: the telemedical interventional monitoring in heart failure study. Circulation. 2011;123:1873–1880. doi: 10.1161/CIRCULATIONAHA.111.018473. [DOI] [PubMed] [Google Scholar]
- 9.Dracup K, Walden JA, Stevenson LW, Brecht ML. Quality of life in patients with advanced heart failure. J Heart Lung Transplant. 1992;11:273–279. [PubMed] [Google Scholar]
- 10.Spertus JA. Evolving applications for patient-centered health status measures. Circulation. 2008;118:2103–2110. doi: 10.1161/CIRCULATIONAHA.107.747568. [DOI] [PubMed] [Google Scholar]
- 11.Krumholz HM, Currie PM, Riegel B, Phillips CO, Peterson ED, Smith R, Yancy CW, Faxon DP, American Heart Association Disease Management Taxonomy Writing Group A taxonomy for disease management: a scientific statement from the American Heart Association Disease Management Taxonomy Writing Group. Circulation. 2006;114:1432–1445. doi: 10.1161/CIRCULATIONAHA.106.177322. [DOI] [PubMed] [Google Scholar]
- 12.Chaudhry SI, Barton B, Mattera J, Spertus J, Krumholz HM. Randomized trial of Telemonitoring to Improve Heart Failure Outcomes (Tele-HF): study design. J Card Fail. 2007;13:709–714. doi: 10.1016/j.cardfail.2007.06.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EW, Smith SC, Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Helperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005;112:e154–235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 14.Green CP, Porter CB, Bresnahan DR, Spertus JA. Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J Am Coll Cardiol. 2000;35:1245–1255. doi: 10.1016/s0735-1097(00)00531-3. [DOI] [PubMed] [Google Scholar]
- 15.Spertus J, Peterson E, Conard MW, Heidenreich PA, Krumholz HM, Jones P, McCollough PA, Pina I, Tooley J, Weintraub WS, Rumsfeld JS, Cardiovascular Outcomes Research Consortium Monitoring clinical changes in patients with heart failure: a comparison of methods. Am Heart J. 2005;150:707–715. doi: 10.1016/j.ahj.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 16.Seaman SR, White IR. Review of inverse probability weighting for dealing with missing data. Stat Methods Med Res. 2013;22:278–295. doi: 10.1177/0962280210395740. [DOI] [PubMed] [Google Scholar]
- 17.Ramachandran K, Husain N, Maikhuri R, Seth S, Vij A, Kumar M, Srivastava N, Prabhakaran D, Airan B, Reddy KS. Impact of a comprehensive telephone-based disease management programme on quality-of-life in patients with heart failure. Natl Med J India. 2007;20:67–73. [PubMed] [Google Scholar]
- 18.Inglis SC, Clark RA, McAlister FA, Ball J, Lewinter C, Cullington D, Stewart S, Cleland JG. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev. 2010;(8):CD007228. doi: 10.1002/14651858.CD007228.pub2. [DOI] [PubMed] [Google Scholar]
- 19.Soran OZ, Pina IL, Lamas GA, Kelsey SF, Selzer F, Pilotte J, Lave JR, Feldman AM. A randomized clinical trial of the clinical effects of enhanced heart failure monitoring using a computer-based telephonic monitoring system in older minorities and women. J Card Fail. 2008;14:711–717. doi: 10.1016/j.cardfail.2008.06.448. [DOI] [PubMed] [Google Scholar]
- 20.Kent DM, Rothwell PM, Ioannidis JP, Altman DG, Hayward RA. Assessing and reporting heterogeneity in treatment effects in clinical trials: a proposal. Trials. 2010;11:85. doi: 10.1186/1745-6215-11-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Flynn KE, Pina IL, Whellan DJ, Lin L, Blumenthal JA, Ellis SJ, Fine LJ, Howlett JG, Keteyian SJ, Kitzman DW, Kraus WE, Miller NH, Schulman KA, Spertus JA, O’Conner CM, Weinfurt KP, HF-ACTION Investigators Effects of exercise training on health status in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301:1451–1459. doi: 10.1001/jama.2009.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldberg LR, Piette JD, Walsh MN, Frank TA, Jaski BE, Smith AL, Rodriguez R, Mancini DM, Hopton LA, Orav EJ, Loh E, WHARF Investigators W Randomized trial of a daily electronic home monitoring system in patients with advanced heart failure: the Weight Monitoring in Heart Failure (WHARF) trial. Am Heart J. 2003;146:705–12. doi: 10.1016/S0002-8703(03)00393-4. [DOI] [PubMed] [Google Scholar]
- 23.Wakefield BJ, Ward MM, Holman JE, Ray A, Scherubel M, Burns TL, Kienzle MG, Rosenthal GE. Evaluation of home telehealth following hospitalization for heart failure: a randomized trial. Telemed J E Health. 2008;14:753–61. doi: 10.1089/tmj.2007.0131. [DOI] [PubMed] [Google Scholar]
- 24.Baker DW, Dewalt DA, Schillinger D, Hawk V, Ruo B, Bibbins-Domingo K, Weinberger M, Macabasco-O’Connell A, Grady KL, Holmes GM, Erman B, Broucksou KA, Pignone M. The effect of progressive, reinforcing telephone education and counseling versus brief educational intervention on knowledge, self-care behaviors and heart failure symptoms. J Card Fail. 2011;17:789–96. doi: 10.1016/j.cardfail.2011.06.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Biannic C, Coutance G, Calus J, Belin A, Loiselet P, Michel L, Pradere G, Delmas P, Grollier G, Sabatier R. Educational Home Follow-up by Telemedicine in Cases of Cardiac Insufficiency. Randomised, Multicentric Study from the Basse-Normandie Region: Preliminary Results. European Research in Telemedicine. 2012;1:40–48. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


