SUMMARY
Internal contamination with radioactive material can expose patients to radiation leading to short- and long-term clinical consequences. After the patient’s emergency conditions are addressed and the skin is decontaminated, the treating physicians assess the amount of radioactive material that has been internalized. This evaluation allows the estimation of the radiation dose that is delivered the specific radionuclide inside the body and supports the need for additional therapies and monitoring. These complex assessments warrant the reliance on a multidisciplinary approach that incorporates local, regional, and national experts in radiation medicine and emergencies.
Keywords: Radioactive terrorism, Contamination, Radioactive elements, Radiation dosage, Chelation therapy
INTRODUCTION
Definition
Emergency physicians care for a wide range of illnesses and injuries, including those that are sustained during a radiologic or nuclear emergency. There are several possible scenarios that cause people to become exposed to ionizing radiation; the most common incidents reported to the Radiation Emergency Assistance and Training Site involve inadvertent exposure to radiation from a radioactive source used in a medical or industrial setting. The Radiation Emergency Assistance and Training Site offers 24–7 assistance to health care professionals or the public with questions about ionizing radiation. Occasionally, a transportation accident involving radioactive material can occur. Less frequently, a nuclear power plant malfunction leads to the release of radioactive material in the environment. This has occurred only a few times in history, yet they have had a large impact on the environment (Fukushima 2011) and public health (Chernobyl 1986). Additionally, the US Government recommends that states prepare for 15 National Planning Scenarios, two of which involve radiation. These are the detonation of an improvised nuclear device and a radiologic dispersal device.1
These radiologic or nuclear incidents occur infrequently and some occur rarely; however, they can be potentially devastating. When they do occur, they cause a disproportionate amount of fear and concern in the public and emergency responders, including emergency physicians.2–4 This fact is combined with a suboptimal amount of health care provider knowledge about the evaluation and care of victims as supported by several previous studies.5,6
Radioactive material exists in a solid, liquid, or gaseous physical form. They can occur naturally in the environment (eg, uranium, thorium, and potassium)7 or are manufactured in a reactor (eg, polonium and plutonium). Although some of these materials are stored in secured locations, like nuclear power plants or military facilities, the majority are available for use in broad range of industries and for a number of applications, including radiography, sterilization of products, materials testing, and medicine. In fact, the International Atomic Energy Agency and US Nuclear Regulatory Commission report the loss of a significant number of sources, some of which are never recovered.8
Patients can become contaminated with radioactive material when the substance in question deposits on their body surface or enters their body through the gastrointestinal tract, the respiratory tract, open wounds, or, less commonly, through intact skin. These routes of exposure need to be differentiated from scenarios in which the patient is exposed to an external source of ionizing radiation, that is, from a source that is external to the body and not contaminating skin or clothing.9
This article discusses the emergency department evaluation and management of a patient who is externally and or internally contaminated with radioactive material.
HISTORICAL BACKGROUND: GOIANIA BRAZIL AND MR LITVINENKO
To better illustrate the concept of contamination with radioactive material, a description of 2 important historical incidents follows.
The radiologic incident in Goiania, Brazil (1987)
On September 28, 1987, a woman visited the clinic at the local Goiania health department in Brazil.10 She claimed that her family members and herself had fallen ill because of handling an unknown solid substance. This material was eventually identified as cesium-137 that originated from the theft of an abandoned teletherapy source on September 13, 1987. The material consisted of about 100 g of cesium-137 in the form of the chloride salt. During the 16 days that followed the theft of the source, several people came into contact with the material and fell ill. They were initially misdiagnosed with food poisoning or allergic reactions by local physicians. In total, 249 people were found to be contaminated with cesium-137 and 4 people died, including a 6-year-old girl who handled the material while eating food. The incident caused severe economic and social impacts. More than 125,000 people presented for monitoring for contamination with the radioactive material. To this day, the psychological consequences of this incident are still apparent in the exposed population.11
The poisoning of Mr Alexander Litvinenko with Polonium-210 (2006)
On November 1, 2006, Mr Alexander Litvinenko developed a gastrointestinal illness after a business meeting at a London restaurant.12 On November 23, 2006, he died from acute radiation syndrome (ARS). On the preceding day, he was discovered to be internally contaminated with a minute yet lethal amount of polonium-210. The particular radioactive properties of this radionuclide facilitated its evasion of early detection tests that were performed and highlighted the hazardous nature of this radioactive element when internalized into the body. In the aftermath of his death, English public health authorities conducted screening of potentially contaminated areas and people. This process included identifying foreign nationals who could have been contaminated during travel and who had to be screened for polonium-210 in their home country.13
AGENTS OF TOXICITY
Mechanism of Injury
Basic definitions (intake, uptake and deposition–initial deposition, excretion)
Radioactive material can enter the body through inhalation, ingestion, or injection. The skin is usually an effective barrier, except when it is damaged (eg, burn) or open (eg, wound). Infrequently, certain radioactive elements may have chemical properties or can be formulated in a manner that makes them absorbable through intact skin. Tritium, which is present in nuclear power plants, is an example of an element that can be absorbed through intact skin. Other than tritium, most radioactive materials are metals or have metallike properties and are not easily absorbed through intact skin.14
An intake is defined as the result of a radioactive element entering the physical confines of the human body (eg, the nares or the mouth). This occurs before uptake (or absorption) of the element into the circulation (eg, into blood or lymph). Once the element enters the circulation, it is distributed in the body and is deposited in various organs or tissues on the basis of its chemical rather than its radioactive properties. For example, iodine-131 deposits primarily in the thyroid gland and cesium-137 behaves like potassium and distributes uniformly in muscle tissue.15
After deposition into various organs and tissues, the element undergoes elimination. The elimination biological half-life varies for different elements and in different patients. For example, the biological half-life for iodine is approximately 57 days and depends on individual factors like thyroid gland activity and iodine content.16 Elimination occurs via different routes including urine, feces, sweat, lungs, and saliva. For example, cesium-137 is naturally primarily eliminated in urine rather than feces. However, when oral Prussian blue chelation therapy is administered, fecal elimination becomes the dominant route.17 Additionally, some elements deposit in bone after being absorbed into the circulation and are less amenable to excretion. For example, strontium has a long biological half-life of approximately 50 years.18
Radiation physics basics (ionizing radiation, radiobiology)
Some atoms are radioactive because they contain too much energy and they emit radiation from the nucleus to reach a more favorable, stable energy state (this process is called radioactive decay). The greater the number of decays per unit time the greater the activity of the material and the more radioactive it is. The unit of activity is the becquerel, where 1 becquerel is equivalent of 1 disintegration or decay per second. As time elapses, the activity of the material decreases because of physical (radioactive) decay. The rate of decay of a specific element is governed by the corresponding physical half-life. For example, the physical half-life of iodine-131 is about 8 days whereas the physical half-life of cesium-137 is about 30 years.19,20 Therefore, radioactive elements that are internalized are subject to both the biological elimination and physical decay processes.21
The effective half-life reflects both processes and is shorter than either one. The effective half-life can be calculated as 1/effective half-life = (1/biological half-life + 1/physical half-life.) For example, iodine-131 has an approximate biological half-life of 57 days and a physical half-life of 8 days. The effective half-life is approximately 7 days (1/effective half-life = 1/8 + 1/57 = 0.1425).
Radioactive elements are potentially hazardous to people because of the radiation that they emit during decay. This radiation carries enough energy to ionize another atom and is appropriately called ionizing radiation. When this radiation energy deposits in a cell, it can damage genetic material or induce the production of free radicals from water molecules in a process called hydrolysis. These highly reactive species in turn damage genetic material or cellular constituents, which could cause cell damage and death. Gamma rays, alpha particles, beta particles, positrons, and neutrons are examples of ionizing radiation and originate from the nucleus of an atom. X-rays are also ionizing; however, they are not released from the nucleus of an atom. They can be generated by a machine or occur naturally when an electron drops from an orbital with higher energy down to a lower energy orbital shell. Typically, x-rays are lower in energy than gamma rays.22,23 In comparison, ultraviolet, visible light, and radio waves do not have enough energy and are unable to ionize atoms. They belong to the category of nonionizing radiation. Every radioactive atom decays to a more stable state by emitting 1 or more types of ionizing radiation. For example, every 137-cesium atom decays by emitting a single gamma ray and a single beta particle and becomes stable barium-137 after going through a barium-137 m (metastable) state.20 On the other hand, every polonium-210 atom decays by emitting an alpha particle and becomes the stable atom lead-206.24
The specific decay information for every radioactive element is available through a variety of sources and can be used to better characterize the health hazards from external or internal contamination with the corresponding element or material (eg, The Health Physics Society Webpage http://hps.org/publicinformation/radardecaydata.cfm). The amount of ionizing radiation energy that deposits in the body or in a specific organ is called absorbed dose and is expressed using the unit gray (Gy) that reflects the energy in joules deposited per kilogram of tissue. The gray is defined as 1 J/kg.25 The biological health effect equivalent of an absorbed dose in gray is expressed using the unit sievert (Sv) and is called equivalent dose. It is calculated by multiplying the dose in gray by a dimensionless radiation weighting factor (previously termed quality factor- “Q”).26 Table 1 below shows the radiation weighting factor for several radiation types.
Table 1.
Radiation weighting factors in ICRP Publication 60
| Type and Energy Range | Radiation Weighting Factor |
|---|---|
| Photons, all energies | 1 |
| Electrons and muons, all energies | 1 |
| Neutrons, energy | |
| <10 keV | 5 |
| >10 keV–100 keV | 10 |
| >100 keV–2 MeV | 20 |
| >2 MeV–20 MeV | 10 |
| >20 MeV | 5 |
| Protons, energy >2 MeV | 5 |
| Alpha particles, fission fragments, heavy nuclei | 20 |
Data from ICRP. 1990 Recommendations of the International Commission on Radiological Protection. ICRP Publication 60; 1991. Ann. ICRP 21 (1–3).
Committed equivalent dose and committed effective dose
The committed equivalent dose is the dose that will be received by an organ after intake of radioactive material into the body over 50 years for adults and 70 years for children. To account for differences in sensitivity between tissues, the equivalent dose to each organ is multiplied by a tissue weighting factor, which is the factor by which the equivalent dose in a tissue or organ is weighted to represent the relative contributions of that tissue or organ to the total detriment resulting from uniform irradiation of the body. The committed effective dose is the sum of the products of the committed organ equivalent doses and the appropriate organ weighting factors. Committed doses are evaluated over 50 years for adults, and from intake to age 70 years for children. The recommended values of the tissue weighting factors are given in Table 2.27
Table 2.
Tissue weighting factors in ICRP Publication 60
| Organ or Tissue | Tissue Weighting Factor |
|---|---|
| Gonads | 0.20 |
| Bone marrow (red) | 0.12 |
| Colon | 0.12 |
| Lung | 0.12 |
| Stomach | 0.12 |
| Bladder | 0.05 |
| Breast | 0.05 |
| Liver | 0.05 |
| Esophagus | 0.05 |
| Thyroid | 0.05 |
| Skin | 0.01 |
| Bone surface | 0.01 |
| Remainder | 0.05 |
The values have been developed from a reference population of equal numbers of both sexes and a wide range of ages. In the definition of effective dose they apply to workers, to the whole population, and to either sex.
Data from ICRP. 1990 Recommendations of the International Commission on Radiological Protection. ICRP Publication 60; 1991. Ann. ICRP 21 (1–3).
The United States has historically used a different set of units than those listed. This can lead to errors when interpreting measurements or other types of data during emergencies. The United States Health Physics Society has recommended using the international system of units (SI) for future activities.28 The conversion between SI units and the ones traditionally used traditional in the United States is listed in Table 3.
Table 3.
Conversion between SI Units and units traditionally used in the United States
| SI Units | Units Used in the United States | Conversion |
|---|---|---|
| Gray (Gy) | Rad | 1 Gy = 100 Rad |
| Sievert (Sv) | Rem | 1 Sv = 100 Rem |
| Becquerel (Bq) | Curie (Ci) | 1 Bq = 1/3.7 × 1010 Ci |
CLINICAL MANIFESTATIONS
Stochastic and Deterministic
The primary goal of the evaluation and management of patients who are contaminated with a radioactive material is to prevent the occurrence of adverse deterministic and stochastic health effects. Deterministic clinical effects occur when the radiation dose to the body or organ is great enough to damage critical cells and lead to organ malfunction like bone marrow failure and neutropenia. The severity and rate of manifestation of these effects are dose dependent. An example of a deterministic effect is the sunburn; the longer one is in the sun, the greater the redness. By the same token, clinically relevant deterministic effects do not occur if the dose received by the organ or body is below a certain threshold (eg, 1 Gy of absorbed dose in general is considered to be the threshold for the development of ARS). Additional factors that determine the type and severity of clinical effects include dose rate, type of ionizing radiation, type and volume of tissue affected, individual patient susceptibilities, co-morbid conditions, and concomitant injuries.23 On the other hand, stochastic effects occur in a random, probabilistic manner and do not require the dose received to be greater than a threshold. Stochastic effects include cancer and birth defects. The greater the dose of radiation deposited in an organ or in the body, the greater the chance of developing the effect, although there is no dose–response relationship between the radiation dose and these effects.23 Last, although genetic hereditary effects have been observed in animals exposed to radiation, they have not been seen in human population studies.29
Chemical toxicity from uranium
The chemical toxicity of the element occasionally is more significant than the clinical effects caused by exposure to the emitted radiation. This is especially true for internal contamination with soluble compounds of natural uranium. This element is radioactive, but causes chemical nephrotoxicity at a lesser concentration in the body than what is required to deliver a radiation dose that is great enough to cause any stochastic clinical effects.30 Therefore, when dealing with internal contamination with one of the isotopes of natural uranium, the main concern is for renal damage from the toxic uranyl ion.
MANAGEMENT
Staff Protection and Safety (Personal Protective Equipment and Concern About Hazards from Body Fluid like Urine, Blood Samples, Management of Waste)
Radiation protection principles
Every effort should be made to keep the dose received by the public and responders including health care providers as low as possible.31 This is known as the ALARA principle where ALARA is an abbreviation for “As Low As Reasonably Achievable.”32 Exposure to radiation during a specific activity can be decreased by limiting its duration and by maximizing the distance between the person and the source of radiation. In fact, the radiation dose is inversely proportional to the square of the distance from the source. At times, shielding from the radiation is possible, using plastics, concrete or lead (for all types of radiation except neutrons).33
Emergency department staff members who initially evaluate patients contaminated with radioactive material (first receivers) should work closely with the hospital radiation safety officer or nuclear medicine technologists, who are an integral part of the team receiving patients in a dedicated area of the emergency department. The radiation safety officer or nuclear medicine technologist advises staff on the following items:
Set up of the work area (also called a radiation emergency area)
Necessary level of personal protective equipment, including the need for a higher level of respiratory precautions
Use of personal dosimeters to monitor the occupational dose received
Level of contamination detected on patients
Extent and efficacy of decontamination procedures
Shielding, storage, and disposal of waste, including patient contaminated belongings or waste water
Personal protective equipment protects staff from becoming externally and or internally contaminated with radioactive material during the care of patients. Unfortunately, it does not protect staff from exposure to gamma radiation emitted from the patients’ body, skin surface, or clothing. Maximizing the distance from the patient and minimizing the time of exposure to the radiation source can significantly decrease the radiation dose received by the first responders or receivers.34
Providers use appropriate garments that cover their skin, mouth, and eyes. Respiratory protection should be in the form of a full-face piece air purifying respirator with a P-100 or high-efficiency particulate air (HEPA) filter. Based on initial assessment of the level and extent of external contamination, the radiation safety officer can advise on whether a lower level of respiratory protection using an N-95 or surgical mask are appropriate.34 Although health care providers may be concerned about secondary hazards of caring for patients who are contaminated with radioactive material, the risk posed to them is minimal and should not delay the performance of life-saving medical evaluation and interventions.
Mr Alexander Litvinenko came into contact with 43 health care providers during his 3-week illness who were not aware of the cause of his illness. These providers used standard precautions during their contact with the victim and were tested for internal contamination after his death. Using a 24-h urine collection bioassay, none were found to have been internally contaminated with any significant amount of polonium that would expose them to a radiation dose above the acceptable dose limit to the public.12
Patients who were contaminated with cesium-137 during the Goiania incident, were treated by health care providers who were using standard precautions for several weeks. During this incident, providers used standard precautions and respiratory precautions were not deemed necessary.35
Radiation dose limits
Dose limits to the public and workers including emergency responders and health care providers are determined using a conservative assessment of the risk of clinical effects after exposure to a specific radiation dose. The goal of these limits is to serve as a guideline for assessing the risk from a dose and should include consideration of the duration and nature of the activity during which the dose would be received. For example, the recommended dose limit to the public is 1 mSv. The occupational total effective dose equivalent annual limit to a worker is 50 mSv.36,37
In an emergency, the National Council on Radiation Protection and Measurements (NCRP) does not set a dose limit dose when performing life-saving activities. Instead, it lists a cumulative dose of 0.5 Gy as a decision point at which the team leader or incident commander needs to consider various aspects of this specific response and decide accordingly how to proceed.31
Decontamination
After the patient’s emergent, life-threatening conditions are stabilized, the patient is surveyed for contamination with radioactive material. Contaminated clothes are removed carefully and stored away in a double (usually plastic) bag for possible later analysis and forensics if necessary. Removal of clothing eliminates any contamination deposited on the garments.
The radiation survey is then repeated to locate any facial orifice, skin, or wound contamination. If radiation is detected, decontamination of the nose/mouth, skin, and/or wound follows using soap and water. The goal of decontaminating the skin is to decrease the risk of additional intake of radioactive material into the body and to decrease the radiation exposure to the skin (eg, when the radioactive material emits beta particles or gamma rays) and internal organs (eg, when the radioactive material emits gamma rays). Decontamination also decreases the risk to health care providers of being exposed to radiation or becoming secondarily contaminated with radioactive material.
After decontaminating the skin, the radiation survey is repeated. Additional decontamination can be performed if persistent contamination is detected. However, this process can be discontinued when the level of contamination ceases to decrease or when the decontamination procedure starts to cause any e trauma to the skin (eg, erythema, abrasions). The survey detection and decontamination procedures are covered in other publications and are demonstrated in accompanying online videos.38,39
Health care providers should also decontaminate wounds that are contaminated with radioactive material by irrigation with saline, with care taken to ensure no additional tissue trauma. Gross foreign bodies should be removed using a forceps. Because foreign bodies can be radioactive, they should be placed in a specimen bag or, preferably, a leaded container and saved in an isolated location for later analysis and proper disposal. If a repeat radiation survey of the wound fails to show additional decrease in the amount of radiation detected, decontamination should cease and the wound should be repaired as medically indicated without significant regard for the contamination.
Diagnosis and Assessment of Internal Contamination
After the patient’s external surface is decontaminated, the clinician needs to assess whether the patient is internally contaminated with radioactive material. The clinician also needs to consider whether the patient is at risk of developing ARS. The ARS component of the assessment is covered in previous publications and will not be discussed in this paper.23,40
The goal of assessing for internal contamination is to determine whether the patient has taken up enough of the material to deliver a significant dose of radiation to the body or to specific organs like the thyroid gland in the case of radioactive iodine. The clinical concern is for deterministic diseases like ARS or stochastic consequences like cancer. These result from the cumulative radiation dose absorbed by the body or a specific organ over the duration of residency of the element inside the body. The duration of radiation exposure is influenced in part by the physical and biological half-lives, as discussed. Consequently, the clinician considers therapies that facilitate the removal of the radioactive material and therefore mitigate the radiation dose absorbed by the patient.
External contamination is associated with a greater risk of concomitant internal contamination. Detecting radioactive material on 2 swabs of both nasal cavities can point toward internal contamination by inhalation. Unfortunately, this method is not practical for a large number of patients after a mass casualty incident. Additionally, the natural variation is nasal cavity size, the delay before evaluation and the natural nasal mucosa clearance rates make this method less favorable than in the occupational setting where it is used traditionally.
Once the patient is no longer externally contaminated, the presence, identity, and amount of radioactive material inside the body can be measured directly by using an external radiation detector when the element emits gamma rays. There are currently several radiation detectors that can be used for this purpose by a radiation safety specialist. Examples of these detectors are whole body counters, and some hand-held instruments. Additionally, hospital nuclear medicine departments potentially have equipment that can be adapted and used for the diagnosis of internal contamination and internal dose assessment in an emergency. Examples of such equipment include thyroid scanner and gamma cameras used in positron emission tomography scanning technology and cardiology departments performing stress tests. Additional guidance on the use of hospital equipment to detect internal contamination is available at the US Centers for Disease Control and Prevention website.41 It is important to note that radioactive chemicals that decay by emitting only beta particles or alpha particles cannot be detected in this manner.
Alternatively, the amount of internalized material can be measured indirectly by using a urinary or fecal bioassay. Ideally, a 24-hour urine or feces collection can be used to produce a measurement of the activity of the specific radioactive element per liter of urine or feces. The Centers for Disease Control and Prevention has developed relatively rapid assays that can use a spot urine sample and measure the activity of several radionuclides. The activity measured in the urine can be then compared to guidance values (eg, clinical decision guide [CDG]) that translates into a radiation dose. The Centers for Disease Control and Prevention has developed a downloadable android and iOS application that can be used by clinicians for this purpose.42 Using this assessment, the clinician can better determine the risk from the contamination and potential management options if available.43
Use of the clinical decision guide
The CDG has been defined by the NCRP (2008) as the maximum once-in-a-lifetime intake (in Bq) of a radionuclide that represents a stochastic risk and avoidance of deterministic effects. The CDG is a tool intended to guide physicians during their assessment of the clinical significance of a specific radionuclide intake by a patient. The NCRP states that the objective of using a CDG is “to reduce the risk of stochastic effects, cancer, to a level consistent with current regulatory guidance for responding to emergency situations and to prevent the risks of deterministic effects.”44 When a patient intake of a specific radionuclide is greater than the corresponding CDG value, decorporation therapy can be used, if one exists for the radionuclide in question. Additionally, the patient will be monitored long term for the development of any clinical consequences like cancer. The CDG values for children and pregnant females are set at a more protective level (one fifth of the CDG adult values). The duration of exposure for a child is assumed to be 70 years as opposed to 50 years for adults.
Use of the annual limit on intake
Before the introduction of the CDG by the NCRP in its report number 161, the annual limit on intake (ALI) values were relied on to assess the significance of a potential contamination with a radioactive chemical. This value is still used by radiation experts to assess the severity of an intake although it is primarily an annual regulatory limit used for workers. The Health Physics Society defines the ALI as follows: “The derived limit for the permissible amount of radioactive material taken into the body of an adult radiation worker by inhalation or ingestion in a year. The ALI is the smaller value of intake of a given radionuclide in a year by the reference man that would result in either a committed effective dose of 50 mSv or a committed equivalent dose of 500 mSv to any individual organ or tissue.”45
Note that the CDG relates to a total body committed effective dose of 250 mSv compared with a committed effective dose of 50 mSv for the ALI. The CDG also relates to a single intake over a lifetime, whether the ALI relates to the limit on an annual intake of a specific radionuclide. The CDG value was created to assist clinicians in determining whether a certain amount of radioactive chemical inside the body is significant clinically during an emergency. The ALI is more useful when evaluating workers who may have become contaminated with a radioactive chemical.
Management Strategies for Internal Contamination
The management of internal contamination includes, in addition to supportive care, measures to decrease the radiation dose that is delivered to body organs and tissues. This measurement can be achieved by decreasing the absorption of the radioactive element from the gastrointestinal tract, the lungs, or an open wound, enhancing excretion in urine or feces, or blocking incorporation into specific organs.
The use of gastric lavage, charcoal, and cathartics are not well-studied. They are possibly efficacious when the route is via ingestion and when the patient presents for care shortly after the incident. Additionally, bronchoalveolar lavage is recommended in specific situations in which a patient has inhaled a large amount of insoluble forms of a radioactive element like plutonium oxide that is absorbed poorly through the pulmonary epithelium and can cause local damage instead. Because of the complexity of this procedure, it is unlikely to be used except in rare circumstances.44
Specific Therapies
Certain radioactive elements can be amenable to specific additional therapies. Currently, the US Food and Drug Administration (FDA) has approved the use of the following drugs for the treatment of internal contamination with a specific set of radioactive elements (Table 4):
- Prussian blue (Fig. 1)
-
◦Prussian blue-insoluble is currently approved by the FDA for the treatment of internal contamination with radioactive cesium and thallium (radioactive and nonradioactive). More commonly, it is used for nonradioactive thallium poisoning. The drug is administered orally and binds cesium or thallium in the intestinal tract during enterohepatic circulation. The resulting complex shifts excretion from the urine to the feces reducing the effective time of residence of the radioactive element inside the body and secondary radiation dose delivered to the body. The dose in adults is 3 g every 8 hours for at least 30 days. The duration of therapy is guided by the amount of radioactive cesium or thallium that is being removed.46
-
◦
- Pentetate calcium trisodium (calcium DTPA) and pentetate zinc trisodium (Zinc DTPA; Fig. 2)47,48
-
◦Calcium and zinc DTPA are currently approved by the FDA for the treatment of internal contamination with americium, plutonium, and curium. These drugs enhance the renal elimination of these elements when internalized. The dose is 1 g IV every 24 hours. The duration of therapy is guided by the amount of radioactive material that is being removed from the body. Calcium DTPA may also be given by nebulizer. Calcium DTPA is preferred over zinc DTPA during the initial 24 hours after contamination. Zinc DTPA is preferred over calcium DTPA in pregnant women and children owing to the concern for associated depletion of essential elements like manganese and zinc.
-
◦
- Potassium iodide
-
◦Potassium iodide (KI) is used to saturate the thyroid gland with stable iodine and prevent additional subsequent uptake of radioactive iodine. To be efficacious, KI should be taken shortly before or shortly after the internalization of radioactive iodine. It can also be given before a potential exposure or internal contamination. The dose of KI depends on the age of the patient. Children younger than 18 years of age and pregnant women (because of the fetus they are carrying) are more vulnerable to the effects of radioactive iodine and should be prioritized to receiving this therapy when indicated.49,50
-
◦The recent nuclear power plant accident in Fukushima highlighted the common misconception that KI is an antiradiation pill. Many people took KI without any proper indication. These actions can cause harm to patients and need to be mitigated by proactive public health messaging.51
-
◦
Table 4.
Therapies approved by the US Food and Drug Administration
| Drug | Indication | Dose | End Point | Pediatric | Pregnancy Category | Precautions and Adverse Effects | Available Forms |
|---|---|---|---|---|---|---|---|
| Prussian Blue | Internal contamination with radioactive Cesium | 3 g PO, every 8 h | 30 d of therapy, guided by urinary and fecal excretion of cesium | 1 g PO every 8 h | C | Constipation Hypokalemia Bluish discoloration of sweat and feces Bluish discoloration of teeth when capsule is ruptured in the mouth |
Radiogardase Available through the United States Strategic National Stockpile |
| Calcium DTPA Pentetate Calcium Trisodium | Internal contamination with plutonium, americium, and curium | 1 g IV or by nebulizer every 24 h | Duration of therapy guided by urinary excretion of the radionuclide | 14 mg/kg IV per day not to exceed 1 g per day | C; zinc DTPA is preferred | Depletion of essential minerals like zinc Bronchoconstriction in asthmatic receiving the dose by nebulizer |
Available through the United States Strategic National Stockpile |
| Zinc DTPA Pentetate Zinc Trisodium | Internal contamination with plutonium, americium, and curium | 1 g IV every 24 h | Duration of therapy guided by urinary excretion of the radionuclide | 14 mg/kg per day, not to exceed 1 g per day | C | Adverse effects not common Headache, lightheadedness, and pelvic reported by one patient who received Zn DTPA |
Available through the United States Strategic National Stockpile |
| Potassium Iodide | Prevent uptake of radioactive iodine by the thyroid | Dose varies by age See FDA | Until risk of exposure to radioactive iodine has gone away | Dose varies by age See FDA | C | Hypothyroidism GI Upset Rash | Over the Counter Thyroshield Thyrosafe Iosat |
Fig. 1.
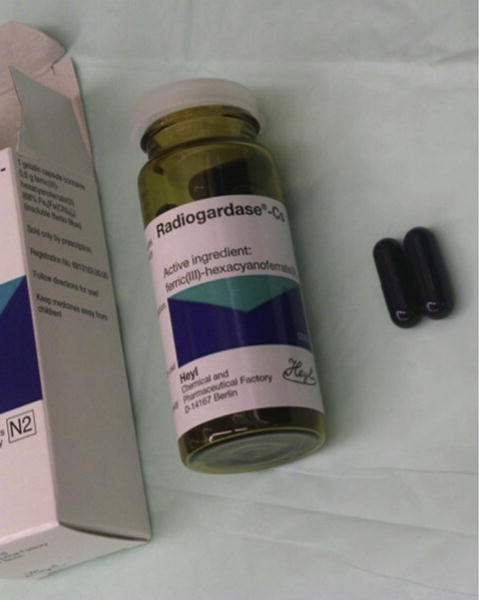
Prussian blue.
Fig. 2.
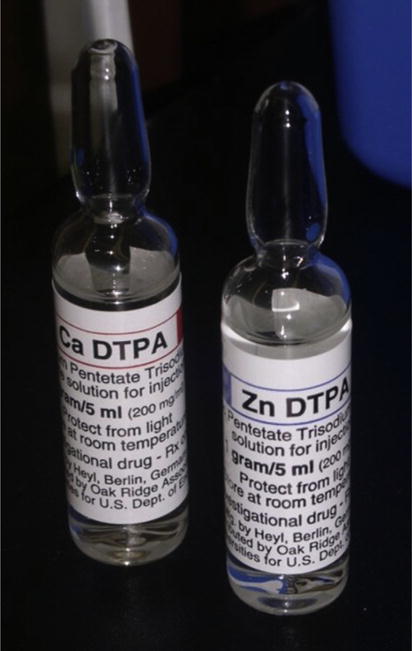
Calcium and zinc diethylenetriamine pentaacetic acid (DTPA).
There are other drugs available that are FDA approved for other indications that are not related to internal contamination. The use of these drugs would be off-label in these situations (Table 5). Last, increasing urinary output increases the elimination of internalized tritium, which behaves inside the body primarily like water does.52 On the other hand, alkalinizing the urine can be used to prevent the renal toxicity from internalized uranium. As mentioned, toxicity from internal contamination with isotopes of uranium is generally chemical and not related to emitted radiation.53,54
Table 5.
Some of the therapies recommended by the National Council for Radiation Protection and Measurements report number 161 and the Radiation Emergency Assistance Center and Training Site
| Drug | Indication |
|---|---|
| Alginates | Internal contamination with radioactive strontium |
| British anti-Lewisite (BAL) | Internal contamination with polonium |
| N-Acetylcysteine | Internal contamination with radioactive cobalt |
These therapies are not approved by the US Food and Drug Administration.
SPECIAL CONSIDERATIONS REGARDING CHILDREN, PREGNANT WOMEN, AND BREASTFEEDING WOMEN
Children and Pregnant Women
A child and the fetus carried by pregnant woman are more sensitive to the stochastic effects of radiation. For example, internal contamination with iodine-131 is more likely to cause thyroid cancer in children compared with adults.55 Therefore, children and pregnant women should be prioritized during the implementation of protective action measures like evacuation and KI administration. Additionally, when assessing the level of internal contamination, the CDG used is 20% of the value used in an adult. Last, dose adjustments need to be followed for available drug therapies.
Breastfeeding Women
Breastfeeding is extremely beneficial to nursing infants and mothers and is encouraged by several professional organizations and societies.56,57 After a radiologic incident that involves the dispersal of radioactive material in the environment, breastfeeding women can become internally contaminated with 1 or more radioactive elements. Some of these elements, depending on their biokinetic properties, can be transferred to the child in the breast milk. This can lead to the internal contamination of the child. Additionally, the child can be secondarily exposed to radiation emitted from the mother’s body during breastfeeding if she is internally contaminated with a radioactive element that emits gamma rays. These conditions may lead to the recommendation that breastfeeding be temporarily discontinued if alternative noncontaminated foods are available.58
However, the child is usually at a similar risk of becoming internally contaminated like the mother through other routes. For this reason, breastfeeding may be acceptable especially if no other source of food is available including noncontaminated water to prepare formula. Ideally, the level of internal contamination in the mother should be assessed to determine the expected amount in breast milk. Unfortunately, this information will not be available in the initial period of an emergency. Breastfeeding recommendations and guidance will need to be made by public health officials using the best evidence available to them.
Long-Term Monitoring
Victims involved in a radiologic emergency need to be monitored for a number of health effects, some of which may be tracked for several decades. For example, the Radiation Effects Research Foundation is tracking the health of the Hiroshima and Nagasaki atomic bomb survivors.59 Additionally, victims who were exposed to radiation during the recent nuclear power plant accident in Fukushima, Japan, will be monitored for health effects for several years to come. This process is complex and requires a national plan that includes participation from a large number of stakeholders.
Risk Communication
Patients involved in a radiologic emergency have been subjected to a variety of stressors and likely display signs and symptoms that are at times out of proportion to the degree and severity of their injuries. Many of these patients are at risk for mental illness, as seen after previous incidents such as the nuclear power plant in Chernobyl in 1986.60 Additionally, a disproportionate number of concerned uninjured survivors will present to emergency departments for evaluation and reassurance. For example, after the criticality accident in Tokai Mura, Japan (1999), that led to 2 fatalities (out of 3 workers who were involved in the accident), approximately 75,000 people were monitored for contamination with radioactive material and 1844 were provided with a medical evaluation.61
The emergency physician who is caring for these patients will need to be skilled at risk communication. The article by McCormick discusses psychological aspects of radiologic disasters. Additionally, the physician can seek assistance from experts in the area of radiation exposure that are available in his hospital or state. The Radiation Emergency Assistance and Training Site is also available to offer medical advice and should be contacted when necessary.
KEY POINTS.
Patients can become contaminated with radioactive material after the detonation of an improvised nuclear device, a nuclear power plant accident, or a radioactive dispersal device incident.
Depending on the scenario, radioactive material can enter the body through ingestion, inhalation or injection.
Life-saving care of a patient contaminated with radioactive material should not be delayed to perform a radiation survey or decontamination.
Once stabilized, a patient should be undressed, surveyed for contamination, and washed with soap and water.
In addition to supportive care, chelators can remove certain radioactive materials, such as cesium-137, plutonium, americium, and curium.
Acknowledgments
The authors acknowledge the following individuals for their contributions to this paper: Dr Adam Pomerleau and Mr Paul Charp, from the Centers for Disease Control and Prevention.
Footnotes
Disclosure Statement: No financial support was provided to any author in relationship to this article. No author declares a conflict of financial interest in relationship to this article.
CDC disclosure statement: “The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention/the Agency for Toxic Substances and Disease Registry.”
References
- 1.National Planning Guidelines. The United States Federal Emergency Management Agency Accessed. Accessed July 28, 2014. Available at: http://www.fema.gov/pdf/emergency/nrf/National_Preparedness_Guidelines.pdf. Published in 2007.
- 2.Balicer RD, Catlett CL, Barnett DJ, et al. Characterizing hospital workers’ willingness to respond to a radiological event. PLoS One. 2011;6(10):e25327. doi: 10.1371/journal.pone.0025327. http://dx.doi.org/10.1371/journal.pone.0025327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Watson CM, Barnett DJ, Thompson CB, et al. Characterizing public health emergency perceptions and influential modifiers of willingness to respond among pediatric healthcare staff. Am J Disaster Med. 2011;6(5):299–308. doi: 10.5055/ajdm.2011.0069. [DOI] [PubMed] [Google Scholar]
- 4.Errett NA, Barnett DJ, Thompson CB, et al. Assessment of medical reserve corps volunteers’ emergency response willingness using a threat- and efficacy-based model. Biosecur Bioterror. 2013;11(1):29–40. doi: 10.1089/bsp.2012.0047. http://dx.doi.org/10.1089/bsp.2012.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheikh S, McCormick LC, Pevear J, et al. Radiological preparedness-awareness and attitudes: a cross-sectional survey of emergency medicine residents and physicians at three academic institutions in the United States. Clin Toxicol (Phila) 2012;50(1):34–8. doi: 10.3109/15563650.2011.637047. http://dx.doi.org/10.3109/15563650.2011.637047. [DOI] [PubMed] [Google Scholar]
- 6.Sadigh G, Khan R, Kassin MT, et al. Radiation safety knowledge and perceptions among residents: a potential improvement opportunity for graduate medical education in the United States. Acad Radiol. 2014;21(7):869–78. doi: 10.1016/j.acra.2014.01.016. http://dx.doi.org/10.1016/j.acra.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 7.Natural Sources of Radiation. The United States Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/nceh/radiation/natural.htm. Accessed July 28, 2014. Page last updated: March 10, 2014.
- 8.Press Release. The International Atomic Energy Agency; Available at: http://www.iaea.org/newscenter/pressreleases/2002/prn0209.shtml. Accessed February 5, 2014. Published September 2002. [Google Scholar]
- 9.Video: Radiological Contamination and Exposure. The United States Centers for Disease Control and Prevention; Available at: http://www.bt.cdc.gov/radiation/resourcelibrary/all.asp. Accessed June 17, 2014. [Google Scholar]
- 10.The Radiological Incident in Goiania, Brazil. The International Atomic Energy Agency. 1987 Available at: http://www-pub.iaea.org/MTCD/publications/PDF/Pub815_web.pdf. Accessed April 21, 2014. Published in 1988.
- 11.Fuini SC, Souto R, Amaral GF, et al. Quality of life in individuals exposed to cesium-137 in Goiânia, Goiás State, Brazil. Cad Saude Publica. 2013;29(7):1301–10. doi: 10.1590/s0102-311x2013000700005. [DOI] [PubMed] [Google Scholar]
- 12.Fraser G, Giraudon I, Cohuet S, et al. Epidemiology of internal contamination with polonium-210 in the London incident, 2006. J Epidemiol Community Health. 2012;66(2):114–20. doi: 10.1136/jech.2009.102087. [DOI] [PubMed] [Google Scholar]
- 13.Miller CW, Whitcomb RC, Ansari A, et al. Murder by radiation poisoning: implications for public health. J Environ Health. 2012;74(10):8–13. [PubMed] [Google Scholar]
- 14.Trivedi A. Percutaneous absorption of tritium-gas-contaminated pump oil. Health Phys. 1995;69(2):202–9. doi: 10.1097/00004032-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 15.The National Council on Radiation Protection and Measurements Report Number 161. I:29. [Google Scholar]
- 16.Biological Half life of Iodine in Normal and Athyroidic persons. The Los Alamos National Laboratory; Available at: http://www.lanl.gov/BAER-Conference/BAERCon-46p027.htm. Accessed May 16, 2014. [Google Scholar]
- 17.Farina R, Brandão-Mello CE, Oliveira AR. Medical aspects of 137Cs decorporation: the Goiânia radiological accident. Health Phys. 1991;60(1):63–6. doi: 10.1097/00004032-199101000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Toxicological Profile for Strontium. The Agency for Toxic Substances and Disease Registry; Available at: http://www.atsdr.cdc.gov/ToxProfiles/tp159.pdf. Appendix D page 4. Accessed June 16, 2014. [PubMed] [Google Scholar]
- 19.Iodine. The United States Environmental Protection Agency; Available at: http://www.epa.gov/radiation/radionuclides/iodine.html. Accessed June 17, 2014. Last updated on 3/6/2012. [Google Scholar]
- 20.Cesium. The United States Environmental Protection Agency; Available at: http://www.epa.gov/rpdweb00/radionuclides/cesium.html. Accessed June 17, 2014. Last updated on 3/6/2012. [Google Scholar]
- 21.Effective Half Life. The Health Physics Society; Available at: http://hps.org/publicinformation/radterms/radfact64.html. Accessed June 17, 2014. Last updated 27 August 2011. [Google Scholar]
- 22.Hall EJ, Giaccia AJ. Radiobiology for the radiologist. 7th. Philadelphia: Lippincott Williams & Wilkins; 2012. [Google Scholar]
- 23.Christensen DM, Iddins CJ, Sugarman SL. Ionizing radiation injuries and illnesses. Emerg Med Clin North Am. 2014;32(1):245–65. doi: 10.1016/j.emc.2013.10.002. http://dx.doi.org/10.1016/j.emc.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 24.The International Atomic Energy Agency. Available at: http://www.iaea.org/Publications/Factsheets/English/polonium210.html. Accessed June 17, 2014.
- 25.Radiation Terms and Definitions. The Health Physics Society; Available at: http://www.hps.org/publicinformation/radterms. Accessed May 16, 2014. Last updated 27 August 2011. [Google Scholar]
- 26.Quality Factor. The Health Physics Society; Available at: http://hps.org/publicinformation/radterms/radfact116.html. Accessed May 16, 2014. Last updated 27 August 2011. [Google Scholar]
- 27.International Commission on Radiological Protection (ICRP) recommendations of the international commission on radiological Protection. 1–3. Vol. 21. Pergamon Press; 1990. (ICRP Publication 60). 1991. Ann. ICRP. [PubMed] [Google Scholar]
- 28.Exclusive Use of the SI Units to Express Radiological Quantities. Position Statement of the Health Physics Society. The United States Health Physics Society; Available at: http://hps.org/documents/SIunits_ps025-0.pdf. Accessed June 17, 2014. Adapted February 2012. [Google Scholar]
- 29.The National Council on Radiation Protection and Measurements Report Number 161. 2011;I:14. [Google Scholar]
- 30.Pavlakis N, Pollock CA, McLean G, et al. Deliberate overdose of uranium: toxicity and treatment. Nephron. 1996;72(2):313–7. doi: 10.1159/000188862. [DOI] [PubMed] [Google Scholar]
- 31.The National Council on Radiation Protection and Measurements Report Number 165. :20–21. Section 3.2.2. [Google Scholar]
- 32.As Low As Reasonably Achievable (ALARA) The Health Physics Society; Available at: http://www.hps.org/publicinformation/radterms/radfact1.html. Last updated August 27, 2011. Accessed June 20, 2014. [Google Scholar]
- 33.The Medical Aspects of Radiation Incidents. The Radiation Emergency Assistance Center/Training Site; Available at: http://orise.orau.gov/files/reacts/medical-aspects-of-radiation-incidents.pdf. Accessed June 20, 2014. Revised 9/25/2013. [Google Scholar]
- 34.Personal Protective Equipment (PPE) in a Radiation Emergency. Radiation Emergency Medical Management; Available at: http://www.remm.nlm.gov/radiation_ppe.htm#firstresponder. Accessed May 27, 2014. Last updated May 4, 2014. [Google Scholar]
- 35.Oliveira AR, Hunt JG, Valverde NJ, et al. Medical and related aspects of the Goiânia accident: an overview. Health Phys. 1991;60(1):17–24. doi: 10.1097/00004032-199101000-00002. [DOI] [PubMed] [Google Scholar]
- 36.Regulatory Dose Limits. The Health Physics Society; Available at: http://www.hps.org/publicinformation/ate/faqs/regdoselimits.html. Accessed June 20, 2014. Last updated December 7, 2013. [Google Scholar]
- 37.NRC Regulations 10 Code of Federal Regulations. The Nuclear Regulatory Commission; Available at: http://www.nrc.gov/reading-rm/doc-collections/cfr/part020/part020-1201.htm. Accessed June 20, 2014. Last updated July 21, 2014. [Google Scholar]
- 38.Procedure Demonstrations. The Radiation Emergency Assistance/Training Site; Available at: http://orise.orau.gov/reacts/guide/procedures.htm. Accessed June 20, 2014. [Google Scholar]
- 39.Radiation Basics Made Simple. The Centers for Disease Control and Prevention; Available at: http://orau.gov/rsb/radbasics. Accessed June 20, 2014. [Google Scholar]
- 40.Donnelly EH, Nemhauser JB, Smith JM, et al. Acute radiation syndrome: assessment and management. Southampt Med J. 2010;103(6):541–6. doi: 10.1097/SMJ.0b013e3181ddd571. http://dx.doi.org/10.1097/SMJ.0b013e3181ddd571. [DOI] [PubMed] [Google Scholar]
- 41.Use of Radiation Detection, Measuring, and Imaging Instruments to Assess Internal Contamination from Intakes of Radionuclides. The Centers for Disease Control and Prevention; Available at: http://emergency.cdc.gov/radiation/clinicians/evaluation. Accessed June 20, 2014. [Google Scholar]
- 42.Internal Contamination Clinical Reference Application. The Centers for Disease Control and Prevention; Available at: http://emergency.cdc.gov/radiation/iccr.asp. Accessed June 20, 2014. [Google Scholar]
- 43.Pillai SK, Chang A, Murphy MW, et al. 2011 investigation of internal contamination with radioactive strontium following rubidium Rb 82 cardiac PET scan. Biosecur Bioterror. 2014;12(1):42–8. doi: 10.1089/bsp.2013.0072. http://dx.doi.org/10.1089/bsp.2013.0072. [DOI] [PubMed] [Google Scholar]
- 44.Management of Persons Contaminated with Radionuclides: Handbook. The National Council on Radiation Protection and Measurements Report Number 161. 2008;I:6–179. [Google Scholar]
- 45.Annual Limit on Intake. The Health Physics Society; Available at: http://hps.org/publicinformation/radterms/radfact30.html. Accessed May 27, 2014. Last updated August 27, 2011. [Google Scholar]
- 46.Prussian Blue. The United States Centers for Disease Control and Prevention; Available at: http://www.bt.cdc.gov/radiation/prussianblue.asp. Accessed June 26, 2014. Last update February 2014. [Google Scholar]
- 47.DTPA (Diethylenetriamine pentaacetate) The United States Centers for Disease Control and Prevention; Available at: http://www.bt.cdc.gov/radiation/dtpa.asp. Accessed June 26, 2014. Last updated August 22, 2013. [Google Scholar]
- 48.Kazzi ZN, Heyl A, Ruprecht J. Calcium and zinc DTPA administration for internal contamination with plutonium-238 and americium-241. Curr Pharm Biotechnol. 2012;13(10):1957–63. doi: 10.2174/138920112802273308. [DOI] [PubMed] [Google Scholar]
- 49.Potassium Iodide. The United States Centers for Disease Control and Prevention; Available at: http://emergency.cdc.gov/radiation/ki.asp. Accessed June 26, 2014. Last updated February 4, 2014. [Google Scholar]
- 50.Guidance Potassium Iodide as a Thyroid Blocking Agent in Radiation Emergencies. The United State Food and Drug Administration; Available at: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM080542.pdf. Accessed July 28, 2014. [Google Scholar]
- 51.Law RK, Schier JG, Martin CA, et al. National surveillance for radiological exposures and intentional potassium iodide and iodine product ingestions in the United States associated with the 2011 Japan radiological incident. Clin Toxicol (Phila) 2013;51(1):41–6. doi: 10.3109/15563650.2012.732701. http://dx.doi.org/10.3109/15563650.2012.732701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tritium. The Health Physics Society; Available at: http://hps.org/documents/tritium_fact_sheet.pdf. Accessed June 26, 2014. Published March 2011. [Google Scholar]
- 53.Fatome M. Management of accidental internal exposure. J Radiol. 1994;75(11):571–5. [PubMed] [Google Scholar]
- 54.Agency for Toxic Substances Disease Registry (ATSDR) Case studies in Environmental medicine (CSEM) Uranium toxicity. Atlanta (GA): US Department of Health and Human Services, Public Health Service; 2009. Available at: http://www.atsdr.cdc.gov/csem/uranium/docs/uranium.pdf. [Google Scholar]
- 55.The Chernobyl Accident. The United Nations Scientific Committee on the Effects of Atomic Radiation; Available at: http://www.unscear.org/unscear/en/chernobyl.html. Accessed June 11, 2014. [Google Scholar]
- 56.Breastfeeding. The American Congress of Obstetricians and Gynecologists; Available at: http://www.acog.org/About_ACOG/ACOG_Departments/Breastfeeding. Accessed June 26, 2014. [Google Scholar]
- 57.Breastfeeding. The American Academy of Pediatrics; Available at: http://www2.aap.org/breastfeeding. Accessed June 26, 2014. [Google Scholar]
- 58.Gartner LM, Morton J, Lawrence RA, et al. American Academy of Pediatrics Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2005;115(2):496–506. doi: 10.1542/peds.2004-2491. [DOI] [PubMed] [Google Scholar]
- 59.The Radiation Effects Research Foundation. Available at: http://www.rerf.jp/index_e.html. Accessed June 13, 2014.
- 60.Bromet EJ. Mental health consequences of the Chernobyl disaster. J Radiol Prot. 2012;32(1):N71–5. doi: 10.1088/0952-4746/32/1/N71. http://dx.doi.org/10.1088/0952-4746/32/1/N71. [DOI] [PubMed] [Google Scholar]
- 61.Lessons Learned from the JCO Nuclear Criticality Accident in Japan in 1999. The International Atomic Energy Agency; Available at: http://www-ns.iaea.org/downloads/iec/tokaimura-report.pdf. Accessed June 16, 2014. [Google Scholar]


