Abstract
Background:
Sagittal translation (ST) is an accidental event that surgeons commonly encounter during a spinal osteotomy in the correction of kyphosis in ankylosing spondylitis (AS). However, there is a paucity of effective techniques to prevent ST. The purpose of this study was to propose a pedicle subtraction osteotomy (PSO) with a cage as a method to prevent ST and to explore the efficacy and feasibility of this method in the treatment of kyphosis in AS.
Methods:
We retrospectively reviewed 89 consecutive patients with AS kyphosis who underwent a PSO (Group B, 46 patients) or a PSO with a cage (Group A, 43 patients) from February 2009 to December 2013. Pre- and post-operative radiographic results were reviewed. ST and complications were analyzed in both groups. Clinical assessment was performed using the Scoliosis Research Society-22 (SRS-22) outcomes metric. The patients were followed up for at least 2 years.
Results:
Group A achieved the same re-alignment of the kyphotic spine as Group B. Two (4.7%) of the 43 patients in Group A and 14 (30.4%) of the 46 patients in Group B had intraoperative ST (χ2 = 10.020, P = 0.002). Significant differences were identified between the two groups in the height change of the osteotomized column. SRS-22 scores improved significantly in both groups. Seven patients experienced neurologic complications (1 in Group A and 6 in Group B). Eight patients had cerebrospinal fluid leakage (2 in Group A and 6 in Group B).
Conclusion:
PSO with a cage significantly avoided ST during the osteotomy procedure and might represent a new, safe, and feasible choice for treating patients with AS kyphosis.
Keywords: Ankylosing Spondylitis, Kyphosis, Pedicle Subtraction Osteotomy, Pedicle Subtraction Osteotomy with a Cage, Sagittal Translation
INTRODUCTION
Ankylosing spondylitis (AS) is a chronic inflammatory seronegative arthropathy that progressively affects the axial skeleton, leading to a characteristic spinal kyphotic deformity in its later stages.[1] Severe deformities cause muscle fatigue, an inability to look straight ahead, and functional disabilities.[2,3,4,5] Surgical correction is necessary in many patients with AS kyphosis to restore sagittal balance and improve the quality of life.[6,7,8,9]
Pedicle subtraction osteotomy (PSO), a V-shaped wedge resection of the vertebral body, is the most popular technique in the surgical treatment of kyphosis in AS patients.[10,11] In the PSO procedure, correction is obtained through a closing wedge osteotomy that hinges on the anterior column of the vertebral body. However, this procedure releases all the three columns of the spine, leading to unrestricted movement of the anterior column hinge. If the hinge moves during surgery, displacement of the vertebral column, or sagittal translation (ST), may occur at the osteotomy site [Figure 1a]. ST is an accidental event commonly encountered during spinal osteotomies to correct kyphosis in AS, and it dramatically increases the potential risk of neurovascular complications.[12,13,14,15,16,17,18]
Figure 1.
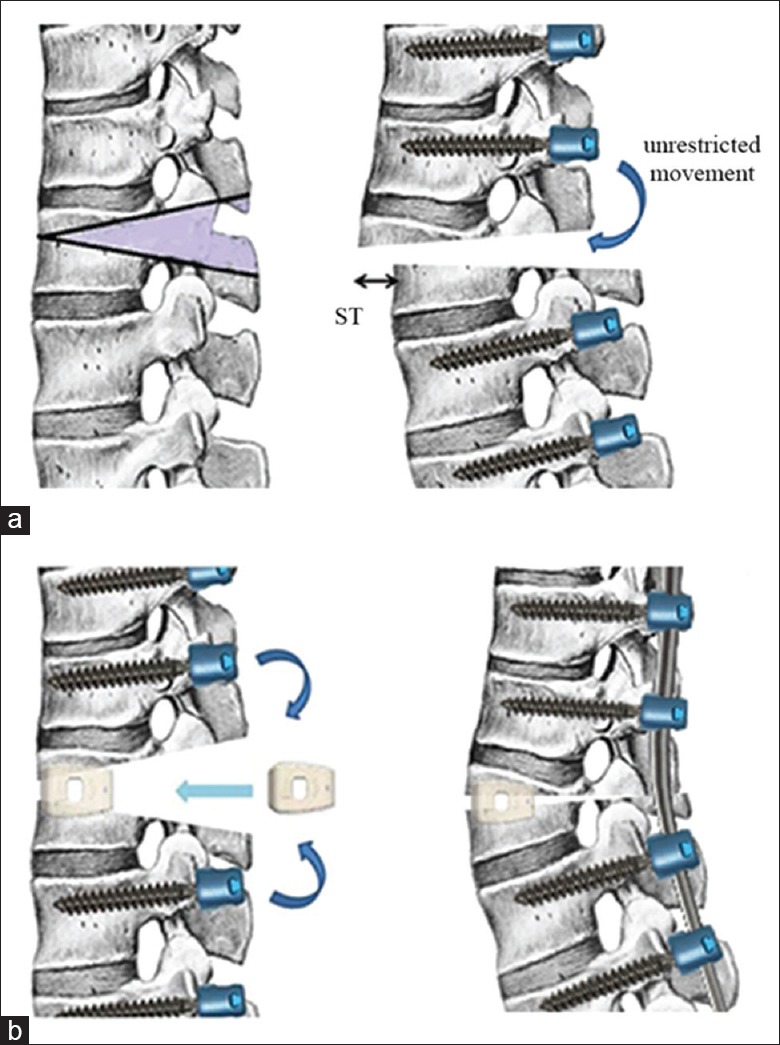
Mechanism of ST in PSO. (a) A V-shaped wedge is resected and the osteotomy gap is unrestricted and ST happens after sagittal movement of the osteotomy site during closure. (b) Illustration of the cage method. It involves inserting a cage large enough into the anterior of the osteotomy gap to restrict the sagittal movement of the osteotomy site. ST: Sagittal translation; PSO: Pedicle subtraction osteotomy.
To the best of our knowledge, there are few methods to prevent ST effectively during osteotomy surgery for AS kyphosis at present. We have developed a method of performing a PSO with a cage, a fusion device in the anterior column at the level of the osteotomy, to restrict the sagittal movement of the osteotomy site and to prevent ST during surgery. The goal of this study was to introduce the cage method to prevent ST and to explore the efficacy and feasibility of this method in the treatment of kyphosis in AS.
METHODS
Ethical approval
Consent from all patients was received for this study. This study was approved by the institutional review board of our hospital.
Study subject
Between February 2009 and December 2013, 263 consecutive AS patients who underwent a spinal osteotomy for sagittal imbalance at our institution were retrospectively reviewed. All the patients were diagnosed with AS with spinal kyphosis by radiographic examinations and laboratory tests according to New York standards.[19] Inclusion criteria were patients who underwent a one-level PSO or PSO with a cage to correct sagittal deformity, with a follow-up period of at least 2 years. Exclusion criteria were patients with cervical kyphosis, revision surgery, coronal deformity, and dislocation of the sacroiliac and hip joints. A total of 89 patients were included in this study.
Eighty-nine patients were divided into two groups based on the surgical methods applied as follows: Group A (PSO with a cage) and Group B (PSO). Group A consisted of 43 patients (36 men and 7 women), with a mean age of 43.1 years (range, 26–58 years). Group B was composed of 46 patients (41 men and 5 women), with a mean age of 46.5 years (range, 28–54 years). The mean follow-up time was 34 months (range, 24–54 months).
Radiologic assessment
Pre- and post-operative full-length spinal radiographs with the patients standing unsupported were available for all patients. Radiographic parameters included sagittal Cobb angle (from T1 to S1), sagittal vertical axis (SVA), lumbar lordosis (LL), and pelvic tilt (PT), which were documented as key parameters for surgical evaluation.[11,20,21,22] The local radiographic parameters at the osteotomy site, including the height of the anterior and posterior columns of the vertebral osteotomy segment (AC and PC), were documented pre- and postoperatively.[23] Postoperative radiographs were performed before hospital discharge, at the 6- and 12-month postoperative period, and at the final follow-up.
ST was measured as the distance between the posterior superior edge of the caudal vertebral body to the posterior inferior edge of the cranial body at the osteotomy level in postoperative standing lateral radiographs.[12] The ST was considered positive if the displacement distance was >2 mm. Otherwise, it was negative.
Surgical technique
All patients were continuously monitored intraoperatively by somatosensory-evoked potentials and motor-evoked potentials. Following the induction of general anesthesia, each patient was placed in the prone position. The thoracolumbar spine was exposed through a posterior midline incision, and the posterior elements were exposed through a subperiosteal approach. Pedicle screw fixation was performed by a freehand technique.
The osteotomy was initiated by probing the pedicles of the osteotomized vertebrae on both sides using a pedicle probe. Then, the pedicles were dilated by incrementally increasing the probe or bone tap size. A high-speed drill was used to enlarge the pedicle holes as necessary. After this, the vertebral bone was adequately removed. The decancellation procedure carefully created a triangular wedge. Before the closing procedure, a temporary rod was used to avoid intraoperative ST in one side in all of the patients when the other side of the osteotomy was completed. After the osteotomy, the cage method was performed with a polyetheretherketone cage [Figure 2] (Weigao Orthopedic, Shandong, China) and bone autograft packed into the osteotomy space at the anterior column of the vertebral body. Thus, the cage sank into the cancellous bone of the vertebral body to stabilize it, and the correction hinge was located at the anterior column without an unpredictable ST. The size ranged from 12 cm × 10 cm × 22 cm to 14 cm × 10 cm × 22 cm, based on the width of the osteotomy gap after removing the vertebral bone. A cantilever maneuver with contoured rods was used to close the osteotomy [Figure 1b]. The patient's position and the operating table were simultaneously adjusted. After closure, evoked potentials were performed to assess spinal cord and nerve root function. Then, the screw nuts were tightened, a posterior fusion bed was prepared, and local bone was grafted to create a fusion. C-arm fluoroscopy was used to examine the magnitude of the correction [Figure 3]. Postoperatively, the patients were allowed to mobilize using a custom-made plastic thoracolumbosacral orthosis during the first 3 months.
Figure 2.

The polyetheretherketone cage used in our study.
Figure 3.
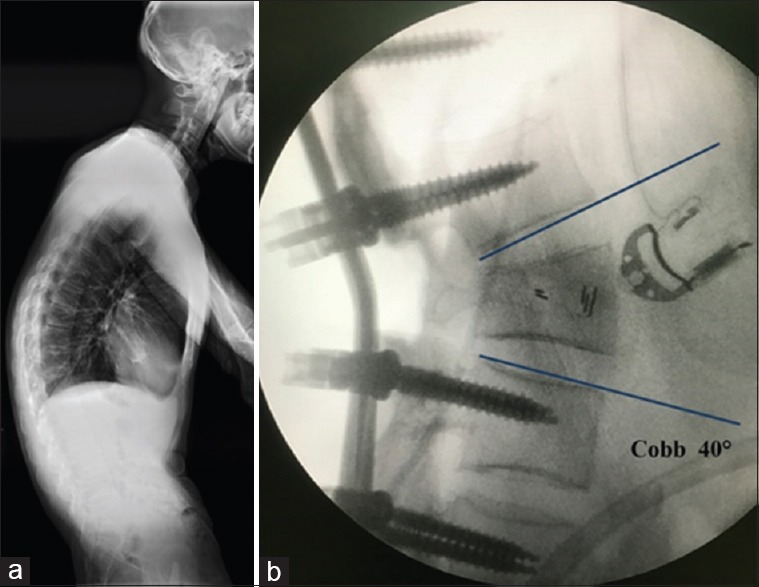
(a) Lateral preoperative radiograph of a 30-year-old male patient who underwent PSO with cage. (b) Intraoperative imaging showing that a correction of 40° at the osteotomy segment was obtained, without sagittal translation. PSO: Pedicle subtraction osteotomy.
Outcomes
Operating time, blood loss, and fused levels were recorded in detail. Clinical outcomes were evaluated using the Scoliosis Research Society-22 (SRS-22) outcome questionnaire[24] preoperatively and at the final follow-up. Complications and other data were also recorded and reviewed.
Statistical analysis
A paired t-test was performed to compare the pre- and postoperative radiographic parameters and the SRS-22 domain scores of each group. An independent sample t-test was used to compare results between groups.
Pearson's Chi-squared test was used to evaluate the ST of different osteotomy methods. An odds ratio (OR) with a 95% confidence interval (CI) was calculated to allow more meaningful interpretation. The OR is a way of comparing whether the probability of a certain event (ST) is the same for two groups. An OR of 1 implies that the event is equally likely in both groups. An OR >1 implies that the event is more likely in that group. An OR <1 implies that the event is less likely in that group.
All data were analyzed using SPSS (version 17.0, SPSS Inc., Chicago, IL, USA). P < 0.05 was considered statistically significant.
RESULTS
Surgical results
A one-level osteotomy was performed on all patients. In Group A, the most frequent osteotomy level was L2 (17 patients), followed by L3 (14 patients), L1 (9 patients), and T12 (3 patients). In Group B, osteotomies over L1, L2, L3, and T12 were performed in 6, 15, 21, and 4 patients, respectively. The mean number of fused levels was 6.8 (range, 5–10) in Group A and 6.5 (range, 5–10) in Group B. The mean operative time was 305 min (range, 240–360 min) in Group A and 310 min (range, 250–380 min) in Group B. The average estimated blood loss was 700 ml (range, 400–1350 ml) in Group A and 780 ml (range, 550–1400 ml) in Group B.
Sagittal translation
Two (4.7%) out of 43 patients in Group A and 14 (30.4%) out of 46 patients in Group B had intra- and postoperative ST. The patients who underwent a PSO were associated with a significantly higher risk of ST than those who underwent the cage method (χ2 = 10.020, P = 0.002) [Figure 4]. The ORs with 95% CIs are shown in Table 1.
Figure 4.
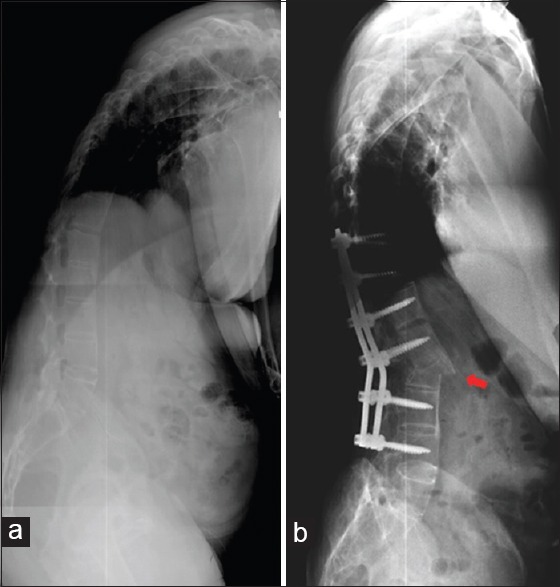
(a) Preoperative radiograph of a 43-year-old male patient of Group B who underwent PSO. (b) The red arrow shows significant ST after closure of the osteotomized vertebra. PSO: Pedicle subtraction osteotomy; ST: Sagittal translation.
Table 1.
The effects of surgical approach on the risk of developing ST in the PSO with a cage group (Group A) and the PSO group (Group B)
| Groups | n | With ST | Without ST | OR (95% CI) | χ2 | P |
|---|---|---|---|---|---|---|
| Group A | 43 | 2 | 41 | 0.11 (0.02–0.53) | 10.020 | 0.002 |
| Group B | 46 | 14 | 32 | 8.97 (1.90–42.34) | ||
| Total | 89 | 16 | 73 | |||
ST: Sagittal translation; PSO: Pedicle subtraction osteotomy; CI: Confidence interval; OR: Odds ratio.
Radiographical and clinical results
The pre- and postoperative radiographic parameters of all patients were recorded. Postoperative correction was achieved in all patients. The sagittal parameters significantly improved in both groups [Table 2]. There was no significant difference between the two groups in the correction of Cobb angle, SVA, LL, and PT [Table 3]. No obvious correction loss was observed at the final follow-up in either group [Figure 5].
Table 2.
Comparison of the pre- and postoperative radiographic parameters in the PSO with a cage group (Group A) and in the PSO group (Group B) (mean ± SD)
| Radiographic parameters | Preoperative | Postoperative | t | P |
|---|---|---|---|---|
| Group A | ||||
| Cobb angle (°) | 43.5 ± 14.8 | 7.8 ± 6.7 | 17.076 | <0.01 |
| SVA (cm) | 25.1 ± 15.2 | 6.8 ± 7.6 | 6.454 | <0.01 |
| LL (°) | 11.2 ± 10.3 | −30.8 ± 15.3 | 15.134 | <0.01 |
| PT (°) | 42.3 ± 15.7 | 25.3 ± 11.1 | 8.237 | <0.01 |
| Group B | ||||
| Cobb angle (°) | 46.2 ± 16.7 | 8.8 ± 7.3 | 14.849 | <0.01 |
| SVA (cm) | 26.4 ± 14.5 | 7.5 ± 8.2 | 8.822 | <0.01 |
| LL (°) | 10.5 ± 12.3 | −28.6 ± 18.5 | 11.123 | <0.01 |
| PT (°) | 40.6 ± 18.2 | 26.5 ± 13.1 | 4.770 | <0.01 |
SD: Standard deviation; PSO: Pedicle subtraction osteotomy; Cobb angle: Cobb angle from T1 to S1; SVA: Sagittal vertical axis; LL: Lumbar lordosis; PT: Pelvic tilt.
Table 3.
Radiographic parameter correction comparison between the two groups (mean ± SD)
| Radiographic parameters | Group A (PSO with a cage) | Group B (PSO) | t | P |
|---|---|---|---|---|
| Correction of Cobb angle (°) | 35.7 ± 12.6 | 37.4 ± 14.3 | 0.157 | 0.876 |
| Correction of SVA (cm) | 18.3 ± 13.2 | 18.9 ± 14.8 | 1.371 | 0.174 |
| Correction of LL (°) | 42.0 ± 11.6 | 39.1 ± 10.5 | −0.629 | 0.531 |
| Correction of PT (°) | 17.0 ± 13.8 | 14.1 ± 17.8 | −1.184 | 0.240 |
| Change in AC (mm) | 3.2 ± 2.7 | 0.6 ± 1.6 | 5.598 | <0.01 |
| Change in PC (mm) | 13.6 ± 3.1 | 18.0 ± 3.8 | 5.899 | <0.01 |
SD: Standard deviation; PSO: Pedicle subtraction osteotomy; Cobb angle: Cobb angle from T1 to S1; SVA: Sagittal vertical axis; LL: Lumbar lordosis; PT: Pelvic tilt; AC: Height of the anterior column of osteotomy vertebrae; PC: Height of the posterior column of osteotomy vertebrae.
Figure 5.
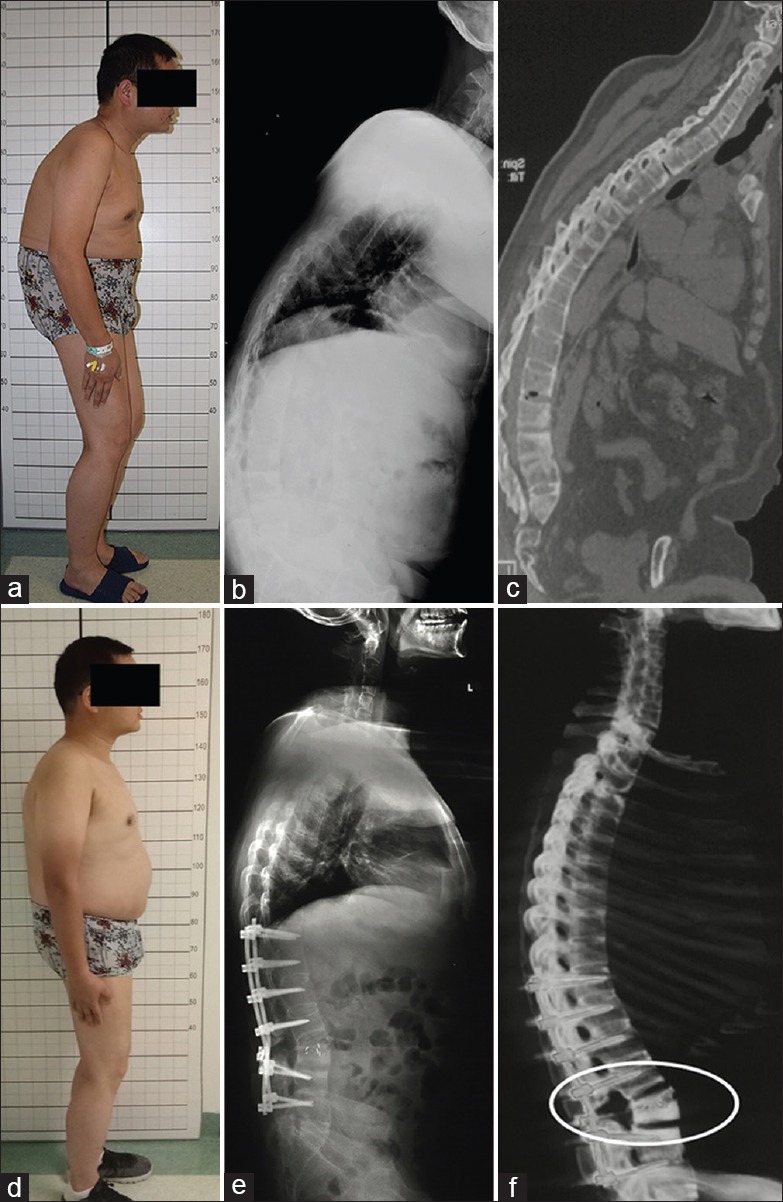
(a) Preoperative clinical photograph of a 34-year-old male patient with AS kyphotic deformity of Group A. (b) Preoperative full-length radiograph showing a remarkable kyphosis in thoracolumbar spine with a global kyphosis of 74°. (c) Preoperative computed tomography sagittal reconstruction image of the patient. (d) Postoperative lateral photograph after single-level PSO with a cage at the L3. (e) Two years of follow-up revealed a correction of about 43° and solid fusion at the osteotomy site without ST. (f) Postoperative three-dimensional reconstruction demonstrated that moderate opening of the anterior cortex of the osteotomized vertebrae was obtained after the cage method, as the circle shows. AS: Ankylosing spondylitis; ST: Sagittal translation; PSO: Pedicle subtraction osteotomy.
In Group A, the AC was prolonged from 29.4 ± 2.8 mm preoperatively to 32.6 ± 2.5 mm postoperatively, and the PC was shortened from 31.2 ± 2.4 mm preoperatively to 17.6 ± 3.5 mm postoperatively. In Group B, the PC was shortened from 30.7 ± 2.5 mm preoperatively to 12.7 ± 3.1 mm postoperatively. Significant differences were identified in postoperative PC (t = 5.899, P < 0.01) and AC (t = 5.598, P < 0.01) between the two groups [Table 3].
At the final follow-up, the SRS-22 scores improved from preoperative 1.9 ± 0.6 to 4.5 ± 0.5 in Group A and from 2.0 ± 0.7 to 4.6 ± 0.4 in Group B. The SRS-22 scores at the final follow-up did not demonstrate a significant difference between the two groups [Table 4].
Table 4.
Comparison of the SRS-22 outcomes between the PSO with a cage group (Group A) and the PSO group (Group B) (mean ± SD)
| SRS-22 | Group A | Group B | t | P |
|---|---|---|---|---|
| Preoperative | 1.9 ± 0.6 | 2.0 ± 0.7 | 0.788 | 0.433 |
| Postoperative | 4.5 ± 0.5 | 4.6 ± 0.4 | 0.691 | 0.492 |
| Final follow-up | 4.4 ± 0.6 | 4.5 ± 0.4 | 0.923 | 0.359 |
SD: Standard deviation; PSO: Pedicle subtraction osteotomy; SRS-22: Scoliosis Research Society-22.
Complications
The complications for each group are shown in Table 5. No fatal complications or aortic injuries occurred in either group. Two patients in Group A experienced cerebrospinal fluid (CSF) leakage secondary to dural tears during the removal of the posterior longitudinal ligament. CSF leakages occurred in six patients in Group B due to dural tears. Three of them experienced it during the resection, and the other three developed it during osteotomy closure. All dural tears were managed uneventfully using muscle and fat graft coverage intraoperatively, and the patients were discharged within 2 weeks of surgery. Superficial infections occurred in both groups and were managed with local wound care and antibiotics (2 in Group A and 3 in Group B). Postoperative pneumonia occurred (2 in Group A and 1 in Group B) and was treated without adverse effects. Seven patients experienced neurologic complications (1 in Group A and 6 in Group B), which were characterized by postoperative unilateral leg numbness and weakness. Four of these recovered spontaneously within 3 months.
Table 5.
Complications in the PSO with a cage group (Group A) and the PSO group (Group B)
| Complications | Group A (n = 43) | Group B (n = 46) |
|---|---|---|
| CSF leakage | 2 | 6 |
| Superficial infection | 2 | 3 |
| Pneumonia | 2 | 1 |
| Neurologic complications | 1 | 6 |
CSF: Cerebrospinal fluid.
DISCUSSION
Late-stage AS patients suffer from thoracolumbar kyphosis, characterized by a round spinal curvature, which requires surgical correction. The PSO has recently become increasingly popular among various osteotomy techniques to correct kyphosis in AS patients. This osteotomy permits the restoration of LL and reduces SVA through a closing wedge osteotomy, thereby leading to good functional results.[25] Unfortunately, neurologic complications following PSOs are common. Bridwell et al. reported a 15.2% incidence of neurologic complications in a case series of patients treated by PSO.[17] Ahn et al. found a neurologic complication rate of 12.0%.[26] Buchowski et al. noted neurologic deficits in 11.1% of patients and 3 patients had permanent deficits.[27] In our study, the neurologic complication rate was 13.0% in the PSO group. All authors identified residual dorsal bony impingement combined with dural buckling and intraoperative ST as the main cause of neurologic complications. Preventative measures have been established for these risk factors. Nevertheless, intraoperative ST during osteotomy closure has been deemed a matter of concern. Currently, there are few effective measures that have been proposed to prevent ST during osteotomy for AS with kyphosis patients.
In 2011, a method that used temporary malleable rods was reported to prevent ST during osteotomy surgery by Arun et al.[6] We used this method in most of our patients. We found that this method plays a limited role in preventing ST before the reduction maneuver finished. Based on our experience, most STs occur because of unrestricted movement at the osteotomy site after anterior cortex fractures during the closing procedure. However, the temporary rods should be removed before the osteotomy gap is closed. Using temporary rods in the correction of AS with kyphosis was not able to avert the occurrence of ST, and the neurovascular complications caused by ST could be critical for individual patients.
If the osteotomy site was stable enough during closure, the management of osteotomy surgery could become safer. The PSO with a cage method includes inserting a cage with bone autograft into the osteotomy space in the anterior column of the osteotomized vertebra. The cage immediately sinks into the cancellous bone of the cranial and caudal sides of the osteotomized site. It provides a stable hinge to close the osteotomy gap, restricts the movement of the cranial or caudal aspects of the osteotomy site, and reduces the possibility of ST after anterior cortex fractures. In this cage method, the cage must be large enough and we recommend its height up to 14 mm. It is only in this way that the cage can make the closure process more stable, as the forces on the osteotomy during closure are mainly focused on the cage in the anterior column. This procedure helps to avoid sagittal displacement and ensures procedure safety. Since 2009, the cage method has been used to stabilize the osteotomy site for AS in 43 patients. This method truly improved the safety of the osteotomy surgery. In this retrospective study, the incidence of ST in AS patients treated with the cage method was significantly reduced compared with those managed with the traditional PSO method. The management of PSOs appeared to carry more risk of developing ST, with an observed OR of 8.97 compared with an OR of 0.11 for the new method.
In our retrospective study, significant differences were identified between the two groups with respect to changes in the height of the anterior (AC) and posterior (PC) vertebral columns. A mean shortening of 0.6 mm of AC and 18 mm of PC was identified in Group B, while a mean elongation of 3.2 mm of AC and a mean shortening of 13.6 mm of PC were identified in Group A. Even though the cage may sink into the cancellous bone of the vertebra in most cases, a moderate opening of the anterior cortex of the osteotomized vertebrae could be obtained with the cage method in the patients of Group A. It decreased the need for posterior column shortening and avoided vertebral compression, thereby preventing dural or spinal cord buckling, which are important causes of neurologic complications.[28,29] Theoretically, the risk of CSF leakage during osteotomy closure can be reduced because of less reduction of the spinal column and sufficient stability of the osteotomized vertebra. However, CSF leakage after dural tears during resection cannot be avoided, and it requires a more careful technique by the surgeon. It is worth noting that the cage method cannot improve the degree of operative correction, as most cages sank into the cancellous bone without providing adequate support. In our study, the correction of radiographic parameters was not significantly different between the two groups.
There are a number of limitations to this study. Limitations are mainly tied to the small sample size (single center). There are also many unpredictable surgical factors that may be associated with ST, even though we have excluded these effects as much as possible in our study. Furthermore, to obtain a satisfactory correction, a two-level osteotomy may be required for some patients with severe rigid kyphotic deformities.
In conclusion, the PSO with a cage method represents a new, safe, and feasible choice for treating patients with AS kyphosis. This method achieves appropriate re-alignment of the kyphotic spine, significantly prevents ST during osteotomy, and moderately reduces spinal column shortening.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Li-Shao Guo
REFERENCES
- 1.Braun J, Sieper J. Ankylosing spondylitis. Lancet. 2007;369:1379–90. doi: 10.1016/S0140-6736(07)60635-7. doi: 10.1016/S0140-6736(07)60635-7. [DOI] [PubMed] [Google Scholar]
- 2.Fu J, Zhang G, Zhang Y, Liu C, Zheng G, Song K, et al. Pulmonary function improvement in patients with ankylosing spondylitis kyphosis after pedicle subtraction osteotomy. Spine (Phila Pa 1976) 2014;39:E1116–22. doi: 10.1097/BRS.0000000000000441. doi: 10.1097/BRS.0000000000000441. [DOI] [PubMed] [Google Scholar]
- 3.Liu C, Song K, Zhang Y, Fu J, Zheng G, Tang X, et al. Changes of the abdomen in patients with ankylosing spondylitis kyphosis. Spine (Phila Pa 1976) 2015;40:E43–8. doi: 10.1097/BRS.0000000000000662. doi: 10.1097/BRS.0000000000000662. [DOI] [PubMed] [Google Scholar]
- 4.Zhang G, Fu J, Zhang Y, Zhang W, Zhang X, Wang Z, et al. Lung volume change after pedicle subtraction osteotomy in patients with ankylosing spondylitis with thoracolumbar kyphosis. Spine (Phila Pa 1976) 2015;40:233–7. doi: 10.1097/BRS.0000000000000717. doi: 10.1097/BRS.0000000000000717. [DOI] [PubMed] [Google Scholar]
- 5.Debarge R, Demey G, Roussouly P. Radiological analysis of ankylosing spondylitis patients with severe kyphosis before and after pedicle subtraction osteotomy. Eur Spine J. 2010;19:65–70. doi: 10.1007/s00586-009-1158-7. doi: 10.1007/s00586-009-1158-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arun R, Dabke HV, Mehdian H. Comparison of three types of lumbar osteotomy for ankylosing spondylitis: A case series and evolution of a safe technique for instrumented reduction. Eur Spine J. 2011;20:2252–60. doi: 10.1007/s00586-011-1894-3. doi: 10.1007/s00586-011-1894-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kiaer T, Gehrchen M. Transpedicular closed wedge osteotomy in ankylosing spondylitis: Results of surgical treatment and prospective outcome analysis. Eur Spine J. 2010;19:57–64. doi: 10.1007/s00586-009-1104-8. doi: 10.1007/s00586-009-1104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hu WH, Wang Y. Osteotomy techniques for spinal deformity. Chin Med J. 2016;129:2639–41. doi: 10.4103/0366-6999.192774. doi: 10.4103/0366-6999.192774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tan R, Ma HS, Zou DW, Wu JG, Chen ZM, Zhou XF, et al. Surgical treatment of severe scoliosis and kyphoscoliosis by stages. Chin Med J. 2012;125:81–6. doi: 10.3760/cma.j.issn.0366-6999.2012.01.015. [PubMed] [Google Scholar]
- 10.Liu H, Yang C, Zheng Z, Ding W, Wang J, Wang H, et al. Comparison of Smith-Petersen osteotomy and pedicle subtraction osteotomy for the correction of thoracolumbar kyphotic deformity in ankylosing spondylitis: A systematic review and meta-analysis. Spine (Phila Pa 1976) 2015;40:570–9. doi: 10.1097/BRS.0000000000000815. doi: 10.1097/BRS.0000000000000815. [DOI] [PubMed] [Google Scholar]
- 11.Qian BP, Jiang J, Qiu Y, Wang B, Yu Y, Zhu ZZ, et al. Radiographical predictors for postoperative sagittal imbalance in patients with thoracolumbar kyphosis secondary to ankylosing spondylitis after lumbar pedicle subtraction osteotomy. Spine (Phila Pa 1976) 2013;38:E1669–75. doi: 10.1097/BRS.0000000000000021. doi: 10.1097/BRS.0000000000000021. [DOI] [PubMed] [Google Scholar]
- 12.Chang KW, Chen HC, Chen YY, Lin CC, Hsu HL, Cai YH, et al. Sagittal translation in opening wedge osteotomy for the correction of thoracolumbar kyphotic deformity in ankylosing spondylitis. Spine (Phila Pa 1976) 2006;31:1137–42. doi: 10.1097/01.brs.0000216479.09250.96. doi: 10.1097/01.brs.0000216479.09250.96. [DOI] [PubMed] [Google Scholar]
- 13.Chang KW, Cheng CW, Chen HC, Chang KI, Chen TC. Closing-opening wedge osteotomy for the treatment of sagittal imbalance. Spine (Phila Pa 1976) 2008;33:1470–7. doi: 10.1097/BRS.0b013e3181753bcd. doi: 10.1097/BRS.0b013e3181753bcd. [DOI] [PubMed] [Google Scholar]
- 14.O'shaughnessy BA, Kuklo TR, Hsieh PC, Yang BP, Koski TR, Ondra SL, et al. Thoracic pedicle subtraction osteotomy for fixed sagittal spinal deformity. Spine (Phila Pa 1976) 2009;34:2893–9. doi: 10.1097/BRS.0b013e3181c40bf2. doi: 10.1097/BRS.0b013e3181c40bf2. [DOI] [PubMed] [Google Scholar]
- 15.Gavaskar AS, Naveen Chowdary T. Pedicle subtraction osteotomy for rigid kyphosis of the dorsolumbar spine. Arch Orthop Trauma Surg. 2011;131:803–8. doi: 10.1007/s00402-010-1224-y. doi: 10.1007/s00402-010-1224-y. [DOI] [PubMed] [Google Scholar]
- 16.Hyun SJ, Kim YJ, Rhim SC. Spinal pedicle subtraction osteotomy for fixed sagittal imbalance patients. World J Clin Cases. 2013;1:242–8. doi: 10.12998/wjcc.v1.i8.242. doi: 10.12998/wjcc.v1.i8.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bridwell KH, Lewis SJ, Edwards C, Lenke LG, Iffrig TM, Berra A, et al. Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine (Phila Pa 1976) 2003;28:2093–101. doi: 10.1097/01.BRS.0000090891.60232.70. doi: 10.1097/01.BRS.0000090891.60232.70. [DOI] [PubMed] [Google Scholar]
- 18.Hao CK, Li WS, Chen ZQ. The height of the osteotomy and the correction of the kyphotic angle in thoracolumbar kyphosis. Chin Med J. 2008;121:1906–10. doi: 10.3760/j.issn: 0366-6999.2008.19.010. [PubMed] [Google Scholar]
- 19.Moll JM. New criteria for the diagnosis of ankylosing spondylitis. Scand J Rheumatol Suppl. 1987;65:12–24. doi: 10.3109/03009748709102173. doi: 10.3109/03009748709102173. [DOI] [PubMed] [Google Scholar]
- 20.Song K, Zheng G, Zhang Y, Cui G, Zhang X, Mao K, et al. Hilus pulmonis as the center of gravity for AS thoracolumbar kyphosis. Eur Spine J. 2014;23:2743–50. doi: 10.1007/s00586-013-3134-5. doi: 10.1007/s00586-013-3134-5. [DOI] [PubMed] [Google Scholar]
- 21.Debarge R, Demey G, Roussouly P. Sagittal balance analysis after pedicle subtraction osteotomy in ankylosing spondylitis. Eur Spine J. 2011;20(Suppl 5):619–25. doi: 10.1007/s00586-011-1929-9. doi: 10.1007/s00586-011-1929-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang XS, Zhang YG, Wang Z, Chen C, Wang Y. Correction of severe post-traumatic kyphosis by posterior vertebra column resection. Chin Med J. 2010;123:680–5. doi: 10.3760/cma.j.issn.0366-6999.2010.06.008. [PubMed] [Google Scholar]
- 23.Zhang X, Zhang Z, Wang J, Lu M, Hu W, Wang Y, et al. Vertebral column decancellation: A new spinal osteotomy technique for correcting rigid thoracolumbar kyphosis in patients with ankylosing spondylitis. Bone Joint J. 2016;98-B:672–8. doi: 10.1302/0301-620X.98B5.35726. doi: 10.1302/0301-620X.98B5.35726. [DOI] [PubMed] [Google Scholar]
- 24.Asher M, Min Lai S, Burton D, Manna B. Scoliosis Research Society-22 patient questionnaire: Responsiveness to change associated with surgical treatment. Spine (Phila Pa 1976) 2003;28:70–3. doi: 10.1097/00007632-200301010-00016. doi: 10.1097/01.BRS.0000047635.95839.2E. [DOI] [PubMed] [Google Scholar]
- 25.Berjano P, Aebi M. Pedicle subtraction osteotomies (PSO) in the lumbar spine for sagittal deformities. Eur Spine J. 2015;24(Suppl 1):S49–57. doi: 10.1007/s00586-014-3670-7. doi: 10.1007/s00586-014-3670-7. [DOI] [PubMed] [Google Scholar]
- 26.Ahn UM, Ahn NU, Buchowski JM, Kebaish KM, Lee JH, Song ES, et al. Functional outcome and radiographic correction after spinal osteotomy. Spine (Phila Pa 1976) 2002(27):1303–11. doi: 10.1097/00007632-200206150-00011. doi: 10.1097/00007632-200206150-00011. [DOI] [PubMed] [Google Scholar]
- 27.Buchowski JM, Bridwell KH, Lenke LG, Kuhns CA, Lehman RA, Jr, Kim YJ, et al. Neurologic complications of lumbar pedicle subtraction osteotomy: A 10-year assessment. Spine (Phila Pa 1976) 2007;32:2245–52. doi: 10.1097/BRS.0b013e31814b2d52. doi: 10.1097/BRS.0b013e31814b2d52. [DOI] [PubMed] [Google Scholar]
- 28.Murrey DB, Brigham CD, Kiebzak GM, Finger F, Chewning SJ. Transpedicular decompression and pedicle subtraction osteotomy (eggshell procedure): A retrospective review of 59 patients. Spine (Phila Pa 1976) 2002;27:2338–45. doi: 10.1097/00007632-200211010-00006. doi: 10.1097/01.BRS.0000030853.62990.BC. [DOI] [PubMed] [Google Scholar]
- 29.Thomason K, Emran IM, Chan D. Shortening osteotomy for the treatment of spinal neuroarthropathy following spinal cord injury. A case report and literature review. Eur Spine J. 2007;16(Suppl 3):318–21. doi: 10.1007/s00586-007-0343-9. doi: 10.1007/s00586-007-0343-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


