Abstract
Background
It is unclear whether traditional application of Kinesio taping, which produces wrinkles in the skin, is effective for improving blood circulation. This study investigated local skin temperature changes after the application of an elastic therapeutic tape using convolution and non-convolution taping methods (CTM/NCTM).
Material/Methods
Twenty-eight pain-free men underwent CTM and NCTM randomly applied to the right and left sides of the lower back. Using infrared thermography, skin temperature was measured before, immediately after application, 5 min later, 15 min later, and after the removal of the tape.
Results
Both CTM and NCTM showed a slight, but significant, decrease in skin temperature for up to 5 min. The skin temperature at 15 min and after the removal of the tape was not significantly different from the initial temperature for CTM and NCTM. There were also no significant differences in the skin temperatures between CTM and NCTM.
Conclusions
Our findings do not support a therapeutic effect of wrinkling the skin with elastic tape application as a technique to increase local blood flow.
MeSH Keywords: Blood Circulation, Pain, Thermography
Background
Kinesio taping (KT) is a type of taping treatment method involving the application of elastic therapeutic tapes to the skin, and was developed by Kase Kenzo, a chiropractor in the 1970s [1]. Previous studies have reported that KT is effective in increasing the flow of blood and lymph in local and peripheral areas [2], enhancing proprioceptive sensation [3,4], increasing muscular strength [5,6], controlling pain [7–9], and promoting an improved range of motion [7,10,11].
The traditional KT application method involves applying an elastic therapeutic tape to the skin while the participant is in a stretched position. In particular, the elastic therapeutic tape should be stretched 10~15% from the middle of the tape, not from the beginning and end of the tape. Thus, when the participant returns to an unstretched position, the elastic therapeutic tape creates wrinkles in the skin where it has been applied [1]. Kase Kenzo proposed that the wrinkles produced after KT application raise the skin, which reduces the pressure of pain receptors under the tissues, increases the space under the skin, enhances blood and lymphatic circulation, and eventually, reduces pain [1].
However, recent studies have suggested that KT does not affect blood circulation. For example, Stedge et al. [12] reported that KT of the gastrocnemius muscle in healthy adults did not affect local blood circulation. Kirsty et al. [13] also claimed that KT of the forearms in healthy football players had no effect on local skin blood flow. Our aim in this study was to clarify this issue by evaluating change in skin temperature, using infrared thermography (IRT), for 2 modes of application of elastic tape to the skin over the lower back: the convolution taping method (CTM), which causes wrinkling of the skin under the tape that is proposed to be the mechanism for increasing local circulation, and the non-convolution taping method (NCTM).
Material and Methods
A total of 32 male adults were recruited. Recruited subjects were screened based on the following exclusion criteria: 1) an orthopaedic or neurosurgical injury occurred during the last 3 months, 2) medication for a musculoskeletal disorder was taken during the last 3 months, or 3) the area to be treated (lower back) showed a between-side temperature difference>0.5°C prior to the application of the tape. A total of 4 subjects were excluded: one with pain in the lower back, one with a history of taking medications, and 2 with skin temperature differences>0.5°C. Thus, the final sample consisted of 28 subjects (age: 22.00±2.57 years, height: 174.75±6.47 cm, weight: 71.41±9.26 kg, mean±SD). All participants provided written informed consent, and the study was approved by the Institutional Review Board of Dong-Eui University. The study flowchart is shown in Figure 1 and the general characteristics of the subjects are shown in Table 1.
Figure 1.

Study flow diagram.
Table 1.
General subject characteristics (n=28).
| Variable | Mean±SD |
|---|---|
| Male (n=28) | |
| Age (years) | 22.00±2.57 |
| Height (cm) | 174.75±6.47 |
| Weight (kg) | 71.41±9.26 |
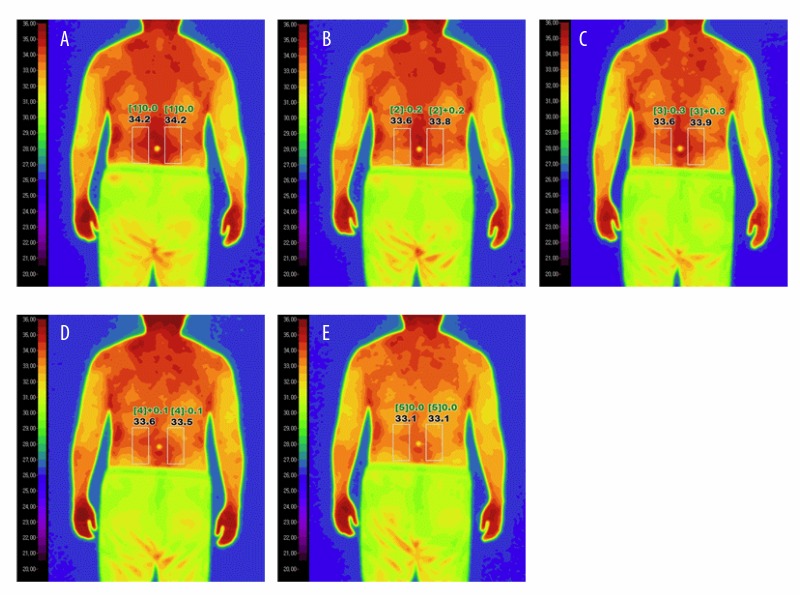
A single-blind, randomized controlled study was conducted. While the subjects were in a standing position, skin temperatures of the right and left lower back were measured using IRT. The CTM and NCTM were applied to the right and left sides of the lower back, with the 2 methods randomly assigned to a side via a table of arbitrary numbers generated by a computer. Another evaluator, blind to the taping method condition, repeatedly measured the skin temperature using IRT at the following time points: before application (Figure 2A), immediately after application (Figure 2B), 5 min later (Figure 2C), 15 min later (Figure 2D), and after the removal of the tape (Figure 2E).
Figure 2.
Infrared thermography (IRT) images for CTM and NCTM at the following time points: before (A), immediately after application (B), 5 min later (C), 15 min later (D), and after removal of the tape (E).
IRT was used to measure the local skin temperature of the lower back before and after the application of CTM and NCTM. IRT is a non-invasive instrument and measures the infrared rays emitting from various objects [14,15]. Each pixel of an IRT image represents the measured surface temperature of the object [14]. Color scales are displayed as blue and black in cold areas, and as white and red in warm areas [14]. IRT has been used as a diagnostic tool for the detection of symmetric or asymmetrical changes in surface temperature [16]. IRT was performed in a sealed room, with sunlight and air flow blocked. The room temperature was maintained at 25~27°C with 62~66% humidity.
The CTM was applied to a randomly selected side on the lower back using an elastic therapeutic tape (BB TAPE, WETAPE Inc., Paju, Korea) stretched approximately 10~15% (from the middle of the tape, not from the beginning and end of the tape). The tape was applied to the lumbar erector spinae muscles from Lumber 1 to Lumbar 5 while the subjects maintained a flexion position, stretching their lower back. Therefore, once the subjects returned to a standing position, wrinkles in the elastic therapeutic tape were shown (Figure 3A). The NCTM was applied to the other side on the lower back; the elastic therapeutic tape was applied to the lumbar erector spinae muscles from Lumbar 1 to Lumbar 5 while the subjects were in a standing position, without stretching their lower back (Figure 3B).
Figure 3.

The convolution taping method (A) and non-convolution taping method (B).
Statistical analyses were performed using SPSS 18.0 (IBM Corp., Armonk, NY). The result of the normality of variables, as analyzed using the Shapiro-Wilk test, was p>0.05 Therefore, the repeated one-way ANOVA was used for statistical analysis instead of the Kruskal Wallis. Repeated one-way ANOVAs were performed to investigate skin temperature changes over time (before, immediately after application, 5 min later, 15 min later, and after the removal of the tape). Post hoc analyses were performed using Bonferroni correction. In addition, skin temperature differences between CTM and NCTM were evaluated at each time point using independent-samples t-tests. A p-value<0.05 was considered statistically significant.
Results
For both the CTM and NCTM, skin temperatures in the lower back treatment area significantly changed over time (p<0.05) (Tables 2, 3). For both the CTM and NCTM, post-hoc analyses demonstrated that skin temperatures very slightly and significantly decreased immediately after application and at 5 min after application, compared to the initial temperature (all p<0.05). However, the skin temperature at 15 min after application and after removal of the tape was not significantly different from the initial temperature for both the CTM and NCTM (p>0.05) (Figures 4, 5). In addition, there were no statistically significant differences in skin temperature between the CTM and NCTM at any time point (p>0.05) (Table 4).
Table 2.
Skin temperature changes using the CTM.
| Before CTM | Start of CTM | 5 min of CTM | 15 min of CTM | Removal of CTM | p |
|---|---|---|---|---|---|
| Mean±SD (°C) | |||||
| 34.79±0.70 | 34.14±0.60 | 34.19±0.65 | 34.37±0.74 | 34.40±0.91 | 0.01* |
p<0.05;
CTM – convolution taping method.
Table 3.
Skin temperature changes using the NCTM.
| Before NCTM | Start of NCTM | 5 min of NCTM | 15 min of NCTM | Removal of NCTM | p |
|---|---|---|---|---|---|
| Mean±SD (°C) | |||||
| 34.75±0.71 | 34.15±0.58 | 34.22±0.61 | 34.40±0.74 | 34.38±0.93 | 0.01* |
p<0.05;
NCTM – non-convolution taping method.
Figure 4.

Skin temperature changes using the convolution taping method (CTM).
Figure 5.

Skin temperature changes using the non-convolution taping method (NCTM).
Table 4.
Differences in skin temperature changes between CTM and NCTM.
| Time | CTM | NCTM | p |
|---|---|---|---|
| Mean±SD (°C) | |||
| Before | 34.79±0.70 | 34.75±0.71 | 0.85 |
| At start | 34.14±0.60 | 34.15±0.58 | 0.92 |
| 5 min | 34.19±0.65 | 34.22±0.61 | 0.88 |
| 15 min | 34.37±0.74 | 34.40±0.74 | 0.90 |
| Removal | 34.40±0.91 | 34.38±0.93 | 0.93 |
p<0.05;
CTM – convolution taping method; NCTM – non-convolution taping method.
Discussion
Based on the IRT measurements of local skin temperature, we did not identify an effect of CTM or NCTM on increased local blood flow. Compared to the initial skin temperature, both the CTM and NCTM showed a slight, but significant, decrease in skin temperatures up to 5 min after the application, which is not clinically significant. Furthermore, there were no significant differences between CTM and NCTM at any time point. Our findings agree with previous studies which failed to identify a specific effect of KT on local circulation when applied to the forearm of healthy adult football players [13] or over the gastrocnemius muscle of healthy adults [12]. Luz Júnior et al. [17] reported that CTM, compared to a placebo taping using Micropore™, was not effective in relieving chronic, non-specific low back pain. Parreira et al. [18] applied the same CTM and NCTM as in the present study to the lumbar erector spinae muscles of patients with chronic non-specific low back pain, but could not validate an effect on pain relief. Thus, Parreira et al. [18] suggested that it is necessary to perform further research regarding mechanisms of pain relief through KT other than the securing of space underlying the tissues. Previous reports have explained the pain relieving mechanism of CTM as follows: CTM reduces the pressure of the mechanoreceptors of the underlying tissues through its lifting effects, increasing the space underlying the tissue and increasing blood circulation. Based on the outcomes of the present study, it can be inferred that the pain relieving effects of KT may not be attributable to the mechanism of securing space via the creation of wrinkles.
The application of elastic therapeutic tape has also been postulated to enhance proprioception by stimulating cutaneous mechanoreceptors [19,20] which, in turn, activates large diameter fibers, including the A-beta fibers involved in gaiting the nociceptive inputs from activation of small diameter fibers, such as the C- and A-delta fibers [21]. The effectiveness of mechanical stimulation of the A-beta fibers of low threshold mechanoreceptors, located in muscles, joints, tendons, and skin in painful areas, has been well-described [22], with activation of A-beta fibers activating inhibitory interneurons to block the pain signals conducted A-delta and C-fibers [23,24].
Both the CTM and NCTM showed a temporary and slight, but significant, decrease in the skin temperature of the lower back. Among sensory receptors, the distribution of thermal sensors varies greatly, depending on location, and more cold receptors are located in the abdominal side and lower back of the human body [25]. Moreover, Ouzzahra et al. [26] and Nakamura et al. [27] confirmed that cold receptors are more widely spread in the lower back areas. Therefore, it has been speculated that because skin stimulation during CTM and NCTM triggers the nerves of the cold receptors, which are widely distributed in the lower back, the activity of cutaneous vasoconstrictor neurons can decrease the blood flow, resulting in a temporary decrease in the local skin temperature at the area of the taping.
Several limitations exist in the present study. 1) The present study included only male adults with no back pain; thus, the findings cannot be generalized to all individuals. 2) The present study did not measure changes in skin temperatures past 15 min from the application of the CTM and NCTM. 3) This study failed to test how much the elastic therapeutic tape interferes with the measurement of skin temperature using IRT. However, even if the therapeutic elastic tape caused a difference in skin temperature, the results of present study do not support the concept that CTM has a greater effect on blood circulation than does NCTM, as there were no significant differences in skin temperature between CTM and NCTM at any time point. Therefore, additional research is necessary to overcome these limitations, including research using patients with back pain.
Conclusions
The CTM, a traditional KT application, does not increase local blood circulation. Therefore, the practice of producing wrinkles in the skin during the application of an elastic therapeutic tape in an attempt to increase local blood circulation is not recommended.
Footnotes
Conflicts of interest
None.
Source of support: Departmental sources
References
- 1.Kase K, Wallis J, Kase J. Clinical therapeutic applications of the kinesio taping method. 2nd ed. Tokyo: Kinesio Taping Association; 2003. [Google Scholar]
- 2.Lipinska A, Sliwinski Z, Kiebzak W, et al. The influence of kinesiotaping applications on lymphoedema of an upper limb in women after mastectomy. Fizjo Pol. 2007;7:258–69. [Google Scholar]
- 3.Lin JJ, Hung CJ, Yang PL. The effects of scapular taping on electromyographic muscle activity and proprioception feedback in healthy shoulders. J Orthop Res. 2011;29:53–57. doi: 10.1002/jor.21146. [DOI] [PubMed] [Google Scholar]
- 4.Murray H, Husk L. Effect of kinesio taping on proprioception in the ankle. J Orthop Sports Phys Ther. 2001;31:A-37. [Google Scholar]
- 5.Murray H. Effects of kinesio taping on muscle strength after ACL-repair. J Orthop Sports Phys Ther. 2000;30:14. [Google Scholar]
- 6.Vithoulka I, Beneka A, Malliou P, et al. The effects of Kinesio-Taping® on quadriceps strength during isokinetic exercise in healthy non athlete women. Isokinet Exerc Sci. 2010;18:1–6. [Google Scholar]
- 7.Cho HY, Kim EH, Kim J, et al. Kinesio taping improves pain, range of motion, and proprioception in older patients with knee osteoarthritis: A randomized controlled trial. Am J Phys Med Rehabil. 2015;94:192–200. doi: 10.1097/PHM.0000000000000148. [DOI] [PubMed] [Google Scholar]
- 8.Hashemirad F, Karimi N, Keshavarz R. The effect of Kinesio taping technique on trigger points of the piriformis muscle. J Bodyw Mov Ther. 2016;20:807–14. doi: 10.1016/j.jbmt.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Kelle B, Güzel R, Sakallı H. The effect of Kinesio taping application for acute non-specific low back pain: A randomized controlled clinical trial. Clin Rehabil. 2016;30:997–1003. doi: 10.1177/0269215515603218. [DOI] [PubMed] [Google Scholar]
- 10.Jaraczewska E, Long C. Kinesio® taping in stroke: Improving functional use of the upper extremity in hemiplegia. Top Stroke Rehabil. 2006;13:31–42. doi: 10.1310/33KA-XYE3-QWJB-WGT6. [DOI] [PubMed] [Google Scholar]
- 11.González-Iglesias J, Fernández-de-Las-Peñas C, Cleland J, et al. Short-term effects of cervical kinesio taping on pain and cervical range of motion in patients with acute whiplash injury: A randomized clinical trial. J Orthop Sports Phys Ther. 2009;39:515–21. doi: 10.2519/jospt.2009.3072. [DOI] [PubMed] [Google Scholar]
- 12.Stedge HL, Kroskie RM, Docherty CL. Kinesio taping and the circulation and endurance ratio of the gastrocnemius muscle. J Athl Train. 2012;47:635–42. doi: 10.4085/1062-6050-47.5.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Woodward KA, Unnithan V, Hopkins ND. Forearm skin blood flow after kinesiology taping in healthy soccer players: An exploratory investigation. J Athl Train. 2015;50:1069–75. doi: 10.4085/1062-6050-50.9.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eddy AL, Van Hoogmoed LM, Snyder JR. The role of thermography in the management of equine lameness. Vet J. 2001;162:172–81. doi: 10.1053/tvjl.2001.0618. [DOI] [PubMed] [Google Scholar]
- 15.Turner TA. Thermography as an aid to the clinical lameness evaluation. Vet Clin N Am Equine Pract. 1991;7:311–38. doi: 10.1016/s0749-0739(17)30502-3. [DOI] [PubMed] [Google Scholar]
- 16.Jones M, Denson A, Williams E, et al. Assessing pregnancy status using digital infrared thermal imaging in Holstein heifers. J Anim Sci. 2005;88:40–41. [Google Scholar]
- 17.Luz MA, Júnior, Sousa MV, Neves LA, et al. Kinesio Taping® is not better than placebo in reducing pain and disability in patients with chronic non-specific low back pain: A randomized controlled trial. Braz J Phys Ther. 2015;19:482–90. doi: 10.1590/bjpt-rbf.2014.0128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parreira PD, Costa LD, Takahashi R, et al. Kinesio Taping to generate skin convolutions is not better than sham taping for people with chronic non-specific low back pain: A randomised trial. J Physiother. 2014;60:90–96. doi: 10.1016/j.jphys.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 19.Konishi Y. Tactile stimulation with Kinesiology tape alleviates muscle weakness attributable to attenuation of Ia afferents. J Sci Med Sport. 2013;16:45–48. doi: 10.1016/j.jsams.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 20.Bravi R, Quarta E, Cohen EJ, et al. A little elastic for a better performance: Kinesiotaping of the motor effector modulates neural mechanisms for rhythmic movements. Front Syst Neurosci. 2014;8:181. doi: 10.3389/fnsys.2014.00181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Illes JD. Kinesiotaping Workbooks, Kinesiotaping Level 1–3. Kinesio Taping Association International; USA: 2009. [Google Scholar]
- 22.Lee JH, Choi SW. Balance taping: Clinical application of elastic therapeutic tape for musculoskeletal disorders. Paju, Korea: WETAPE; 2016. [Google Scholar]
- 23.Martini FH. Fundamentals of anatomy and physiology. San Francisco: Benjamin-Cummings; 2004. [Google Scholar]
- 24.Melzack R. The story of pain. Psychologist. 2011;24:470–71. [Google Scholar]
- 25.Filingeri D, Havenith G. Human skin wetness perception: Psychophysical and neurophysiological bases. Temperature. 2015;2:86–104. doi: 10.1080/23328940.2015.1008878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ouzzahra Y, Havenith G, Redortier B. Regional distribution of thermal sensitivity to cold at rest and during mild exercise in males. J Therm Biol. 2012;37:517–23. [Google Scholar]
- 27.Nakamura M, Yoda T, Crawshaw LI, et al. Regional differences in temperature sensation and thermal comfort in humans. J Appl Physiol. 2008;105:1897–906. doi: 10.1152/japplphysiol.90466.2008. [DOI] [PubMed] [Google Scholar]