Abstract
Background
Robot-assisted radical prostatectomy (RARP) is increasingly used worldwide, but comparisons of perioperative, functional, and oncologic outcomes among RARP, laparoscopic radical prostatectomy (LRP), and open radical prostatectomy (ORP) remain inconsistent.
Material/Methods
Systematic literature searches were conducted using EMBASE, PubMed, the Cochrane Library, CNKI, and Science Direct/Elsevier up to April 2017. A meta-analysis was conducted using Review Manager and Stata software.
Results
We included 33 studies. Meta-analysis revealed that blood loss, transfusion rate, and positive surgical margin (PSM) rate were significantly lower following RARP compared with LRP (SMD (95% confidence interval [CI]) 0.31 [0.01, 0.61]; combined ORs (95% CI) 5.32 [1.29, 21.98]; 1.27 [1.10, 1.46]) and ORP (SMD (95% CI) 0.75 [0.30, 1.21]; and combined ORs (95% CI) 3.44 [1.21, 9.79]); positive surgical margin (PSM) rates were significantly lower following RARP compared with LRP (combined ORs (95% CI) 1.27 [1.10, 1.46]), but not ORP. Operation time was also shorter for RARP than for LRP. The rates of nerve-sparing, recovery of complete urinary continence, and recovery of erectile function were significantly higher following RARP compared with LRP (combined ORs (95% CI) 0.55 [0.31, 0.95]; 0.66 [0.55, 0.78]; 0.46 [0.30, 0.71]) and ORP (combined ORs (95% CI) 0.36 [0.21, 0.63]; 0.33 [0.15, 0.74]; 0.65 [0.37, 1.14]).
Conclusions
This meta-analysis demonstrates that RARP results in better overall outcomes than LRP and ORP in terms of blood loss, transfusion rate, nerve sparing, urinary continence and erectile dysfunction recovery, and suggests that RARP offers better results than LRP and ORP in treatment of prostate cancer. However, studies with larger sample sizes and long-term results are needed.
MeSH Keywords: Erectile Dysfunction, Hand-Assisted Laparoscopy, Prostatic Neoplasms
Background
The incidence rates of prostate cancer are currently increasing in most countries, especially in some developed countries [1,2]. Open radical prostatectomy (ORP) has been the criterion standard for the treatment of prostate cancer for some time; however, this procedure is associated with considerable blood loss and postoperative pain, and a prolonged hospital stay. Laparoscopic radical prostatectomy (LRP) was first reported in the early 1990s [3], and demonstrated advantages in terms of reduced blood loss and postoperative pain, and shorter hospital stay, as well as lower rates of urinary incontinence and erectile dysfunction, compared with open procedures [4–6]. LRP has thus since become the standard procedure in many institutions. However, there have been numerous refinements in terms of both prostatectomy techniques and equipment. Although ORP and LRP have thus formed the mainstay of treatment for prostate cancer, technical procedures for radical prostatectomy have recently been improved and updated to ensure oncological control and satisfactory postoperative functional outcomes, and the use of Robotic-assisted radical prostatectomy (RARP) has subsequently increased dramatically. Robot-assisted surgery offers several advantages compared with standard laparoscopy, including the use of a high-resolution camera with three-dimensional visualization, while the robotic arms allow surgeons to perform more precise dissection of the anatomic structures, potentially leading to better preservation of functional structures, reduced PSM, and better perioperative outcomes [7–9].
Although several studies have compared the perioperative, functional, and oncologic outcomes among RARP, LRP, and ORP, the results have been inconsistent. Some studies reported significantly lower blood loss, transfusion rate, and positive surgical margin (PSM) rate with RARP compared with LRP and ORP, and higher nerve-sparing, recovery of complete urinary continence, and recovery of erectile function rates, while others have failed to find these relationships [7–39]. We therefore conducted a systematic review of the existing literature and conducted a meta-analysis to assess the perioperative, functional, and oncologic outcomes after RARP, LRP, and ORP, to help provide valuable insights into the appropriate choice of surgical procedures for patients with prostate cancer.
Material and Methods
Literature search
This study was limited to published studies that compared the perioperative, functional, and oncologic outcomes after RARP, LRP, and ORP. The literature was searched in the Cochrane Library, Medline, EMBASE, CNKI, Elsevier, and PubMed by 2 independent reviewers, from their inception to April 2017. The search terms comprised MeSH terms and text words. For example, perioperative, functional, and oncologic outcomes were: ‘perioperative outcomes’, ‘functional outcomes’, ‘oncologic outcomes’, ‘operation time’, ‘blood loss’, ‘transfusion rate’, ‘erectile function’, ‘urinary continence’, ‘nerve sparing’, ‘positive surgical margin’, and ‘PSM’, while those for surgical method were: ‘open radical prostatectomy’, ‘laparoscopic radical prostatectomy’, ‘robot-assisted radical prostatectomy’, ‘RARP’, ‘LRP’, and ‘ORP’. All related articles and abstracts were retrieved.
Eligibility criteria
Studies in which patients were diagnosed with prostate cancer and underwent primary treatment with RARP, LRP, or ORP were included. Included studies also reported on the perioperative, oncological, and functional outcomes after RARP, LRP, and ORP. Perioperative outcomes included operation time, blood loss, and transfusion rate; oncological outcomes included PSM; and functional outcomes included nerve-sparing, urinary continence, and erectile dysfunction. Data on operation time and blood loss are presented as continuous data with means and standard deviations (SDs). Transfusion rate, PSM, nerve-sparing, urinary continence, and erectile dysfunction are presented as dichotomous variables.
We excluded case reports, review articles, meeting reports, and abstracts, as well as studies reporting on duplicate patient populations where some or all of the same patients were included in more than 1 study reporting on the same parameters, as well as studies in which the patients had urinary incontinence or erectile dysfunction before surgery.
Study selection and validity assessment
The titles and abstracts of the relevant literature were screened by 2 independent reviewers, and relevant reports were retrieved. If the title and abstract were ambiguous, the full text was analyzed. The final decision on eligible studies was made after reviewing the selected articles. If 2 independent reviewers disagreed on the same document, then the inclusion of the document required consensus or consultation with a third reviewer.
Data extraction and statistical analysis
Data, including demographic data and outcome data (operation time, blood loss, transfusion rate, PSM, nerve sparing, urinary continence, and erectile dysfunction), were recovered from the selected literature. The differences were settled by consensus. Quantitative meta-analysis was performed using Review Manager (RevMan) software and Stata software by 2 reviewers. Available data, including mean, SD, and available number, were analyzed in the meta-analysis to calculate standard mean differences (SMD), combined odds ratios (ORs), and 95% confidence intervals (CIs). Heterogeneity assessment used the p-value and the I-squared statistic (I2) in pooled analyses, representing the percentage of total variation across studies. If p<0.1 or I2 >50%, the summary estimate was analyzed in a random-effects model; otherwise, a fixed-effects model was applied. The results are expressed as SMDs for continuous outcomes and as ORs for dichotomous variables. Publication bias was assessed by assessing visual symmetry of funnel plots, in which asymmetry may indicate publication bias, and by Begg’s and Egger’s tests in the meta-analysis. Publication bias was indicated by p<0.05.
Results
Characteristics of included studies
Figure 1 shows the review process in detail. A total of 3091 nonduplicate studies were extracted, 33 of which were ultimately selected according to the eligibility criteria: 19 compared the perioperative, functional, and oncologic outcomes between ORP and RARP; 11 compared the 3 outcomes between LRP and RARP; and 5 compared the 3 outcomes between LRP and ORP. After group discussion, all reviewers agreed to include all 33 papers.
Figure 1.
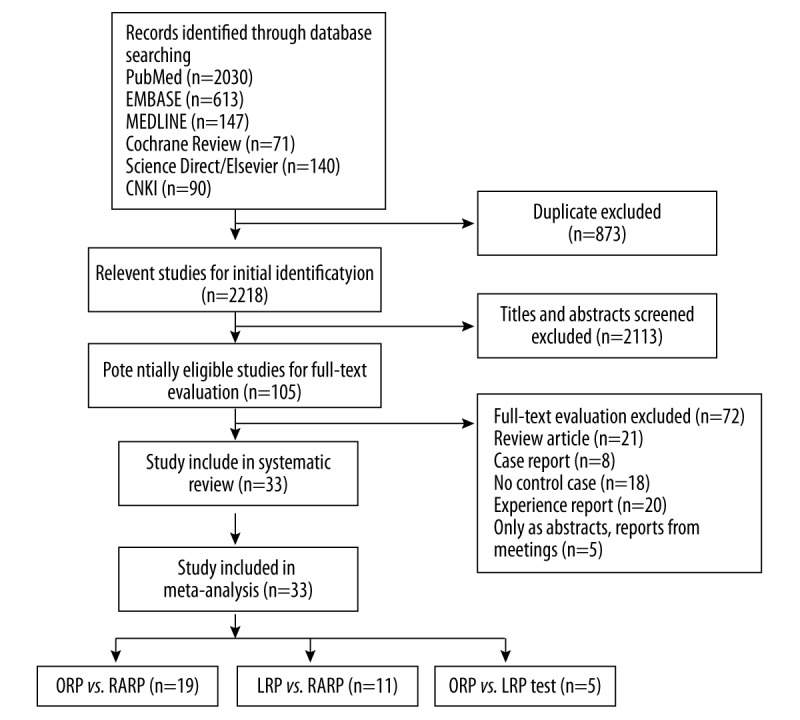
Flow diagram of selection of eligible studies.
Table 1 summarizes the general data from the 33 studies. The mean age ranges of the patients who underwent ORP, RARP, and LRP were 49.3±2.4–70.03±6.10 years, 32.6±2.9–69.05±4.78 years, and 57.2±7.4–62.5±6.0 years, respectively. All of the included studies reported exclusion/inclusion criteria [7–39]. The 19 studies [8,10,14,16–20,22,23,27,29,30–33,36–38] that compared the outcomes between ORP and RARP groups included 16 830 prostate cancer patients. Eleven of these studies [7,9–13,15,21,34,35] compared the outcomes between LRP and RARP, and 5 studies [10,24–26,39] compared the outcomes between ORP and LRP.
Table 1.
Characteristics of included studies.
| Study | Country | Mean age (case/control) | Study design | Case (n) | Outcomes |
|---|---|---|---|---|---|
| Papachristos A et al. 2014 | Australia | 62.5/60.5 | LRP vs. RARP, retrospective | LRP: 100, RARP: 100 | OT, BL, PSM, NS, UC, EF |
| Koo KC et al. 2014 | Korea | 65.9/65.6 | ORP vs. RARP, retrospective | ORP: 580, RARP: 592 | PSM |
| Tozawa K et al. 2014 | Japan | 67.4/67.0 | LRP vs. RARP, retrospective | LRP: 551, RARP: 551 | PSM |
| Sugihara T et al. 2014 | Japan | 68/68/67 | ORP, LRP vs. RARP, retrospective | ORP: 7202, LRP: 2483, RARP: 2126 | OT, TF |
| Rozet F et al. 2007 | France | 62.5/62.0 | LRP vs. RARP, retrospective | LRP: 133, RARP: 133 | OT, BL, TR, NS |
| Hakimi AA et al. 2009 | America | 59.6/59.8 | LRP vs. RARP, prospective | LRP: 75, RARP: 75 | OT, BL, PSM, NS, UC, EF |
| Ploussard G et al. 2014 | France | 62.7/62.7 | LRP vs. RARP, prospective | LRP: 1377, RARP: 1009 | OT, BL, PSM, NS, UC, EF |
| Froehner M et al. 2012 | Germany | 65.2/62.8 | ORP vs. RARP, prospective | LRP: 1925, RARP: 252 | TR |
| Park JW et al. 2011 | Korea | 65.7/62.7 | LRP vs. RARP, prospective | LRP: 62, RARP: 44 | OT, BL, PSM, NS, UC, EF |
| Martinschek A et al. 2012 | Germany | 67.6±5.3/69.1±4.8 | ORP vs. RALP, prospective | ORP: 19, RARP: 19 | PSM |
| Barry MJ et al. 2012 | America | 49.3±2.4/32.6±2.9 | ORP vs. RARP, prospective | ORP: 220, RARP: 406 | EF |
| Choo MS et al. 2013 | Korea | 67±6.3/66±7.8 | ORP vs. RARP, prospective | ORP: 176, RARP: 77 | BL, PSM, NS, UC, EF |
| Schroeck FR et al. 2008 | America | 60.3/59.2 | ORP vs. RARP, prospective | ORP: 219, RARP: 181 | EF |
| Voss BL et al. 2013 | Grenada | 61.9±4.1/61.1±5.8 | ORP vs. RARP, prospective | ORP: 10, RARP: 10 | OT, BL |
| Henry C et al. 2011 | America | 65.1±5.9/61.9±7.2 | LRP vs. RARP, prospective | LRP: 97, RARP: 312 | OT, PSM, NS |
| Philippou P et al. 2012 | United Kingdom | 62.5±6.4/62.4±5.6 | ORP vs. RARP, prospective | ORP: 50, RARP: 50 | OT, BL, TR, PSM, NS |
| Barocas DA et al. 2010 | America | 62±7.3/61±7.3 | ORP vs. RARP, prospective | ORP: 491, RARP: 1413 | PSM |
| Springe C et al. 2013 | Germany | 56.8±6.7/57.2±7.4 | ORP vs. LRP, prospective | LRP: 125, RARP: 128 | OT, BL, TR, PSM, UC, EF |
| Rassweiler J et al. 2003 | Germany | 65/64 | ORP vs. LRP, prospective | ORP: 219, LRP: 219 | OT, BL, TR, NS, UC, EF |
| Roumeguere T et al. 2003 | Belgium | 63.9±5.5/62.5±6.0 | ORP vs. LRP, prospective | ORP: 77, LRP: 85 | OT, BL, PSM, NS, UC, EF |
| Wallerstedt A 2015 | Sweden | 63/63 | ORP vs. RARP, prospective | ORP: 778, RARP: 1847 | OT, BL |
| Akand M et al. 2015 | Turkey | 62.7/60.3 | LRP vs. RARP, retrospective | LRP: 308, RARP: 79 | TR, PSM |
| Lee D et al. 2015 | Korea | 66.0/66.5 | ORP vs. RARP, retrospective | ORP: 106, RARP: 250 | PSM |
| Di Pierro GB et al. 2011 | Switzerland | 64.3/62.8 | ORP vs. RARP, prospective | ORP: 75, RARP: 75 | OT, PSM, UC |
| Ou YC et al. 2009 | America | 70.0±6.1/67.3±6.2 | ORP vs. RARP, prospective | ORP: 30, RARP: 30 | OT, BL, PSM, NS, UC |
| Rocco B et al. 2007 | Italy | 63/63 | ORP vs. RARP, prospective | ORP: 240, RARP: 120 | OT, BL, EF |
| Krambeck AE et al. 2002 | America | 61.0/61.0 | ORP vs. RARP, prospective | ORP: 588, RARP: 294 | NS, EF |
| Trabulsi EJ et al. 2010 | America | 58.1/59.9 | LRP vs. RARP, prospective | LRP: 45, RARP: 205 | OT, TR, BL, PSM, NS, UC |
| Kwon EO et al. 2010 | America | 59.4±67.4/58.8± 6.6 | LRP vs. RARP, prospective | LRP: 165, RARP: 121 | PSM |
| Chung JS et al. 2011 | Korea | 65.8±6.6/66.3±7.6 | ORP vs. RARP, retrospective | LRP: 155, RARP: 105 | OT, BL, EF |
| Ficarra V et al. 2009 | Italy | 65/61 | ORP vs. RARP, prospective | ORP: 105, RARP: 103 | |
| Yaxley JW et al. 2016 | Australia | 59.64/60.38 | ORP vs. RARP prospective | RARP: 157 ORP: 151 | OT, TR, BL, PSM, NS, UC |
OT – operate time; BL – blood loss; TR – transfusion; NS – nerve sparing; PSM – positive surgical margin; UC – urinary continence; EF – erectile function.
Meta-analysis
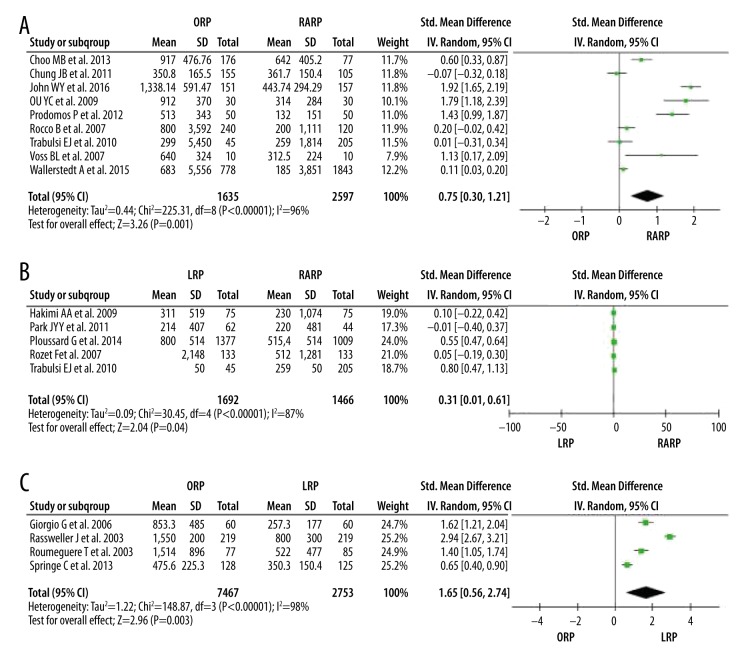
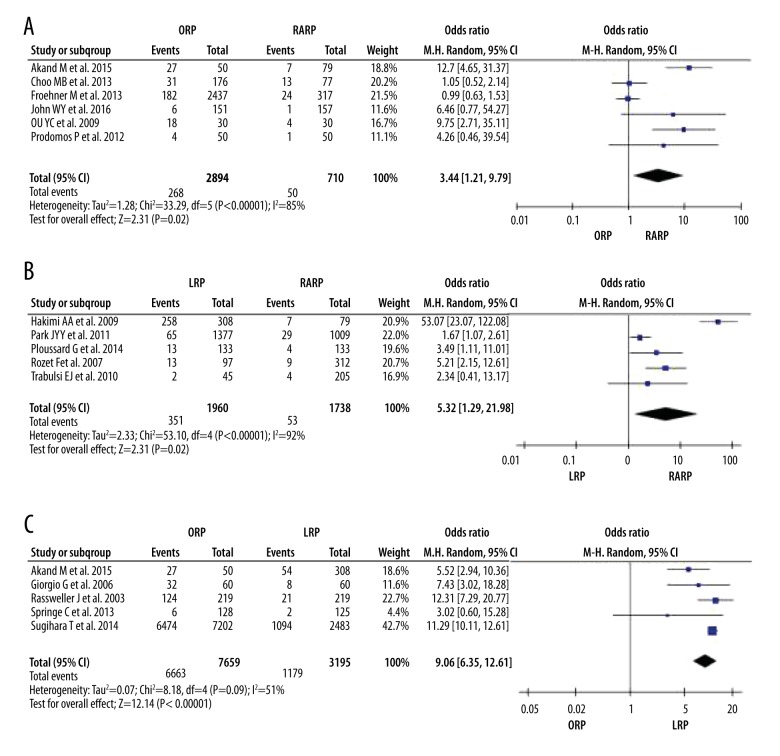
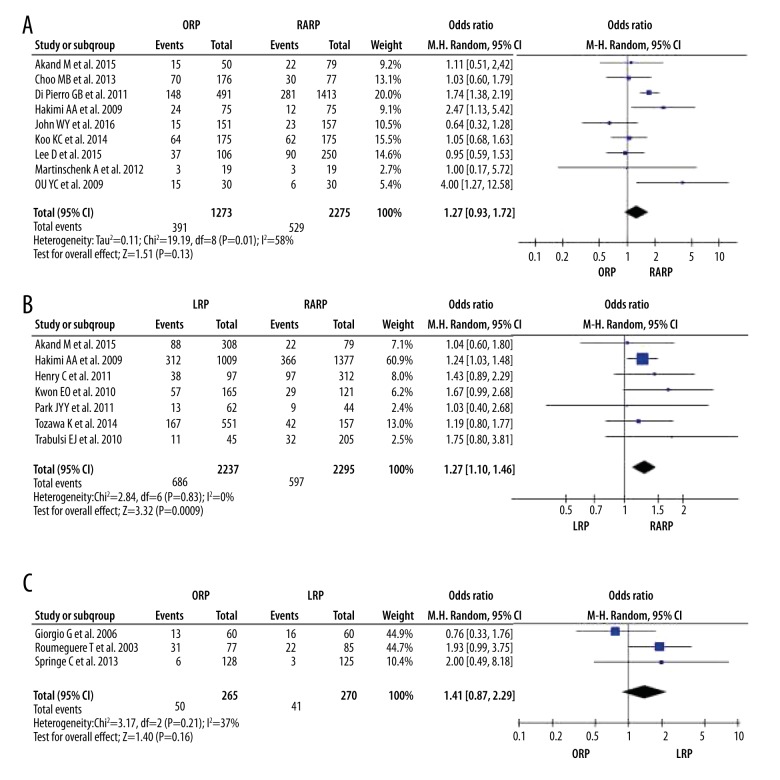
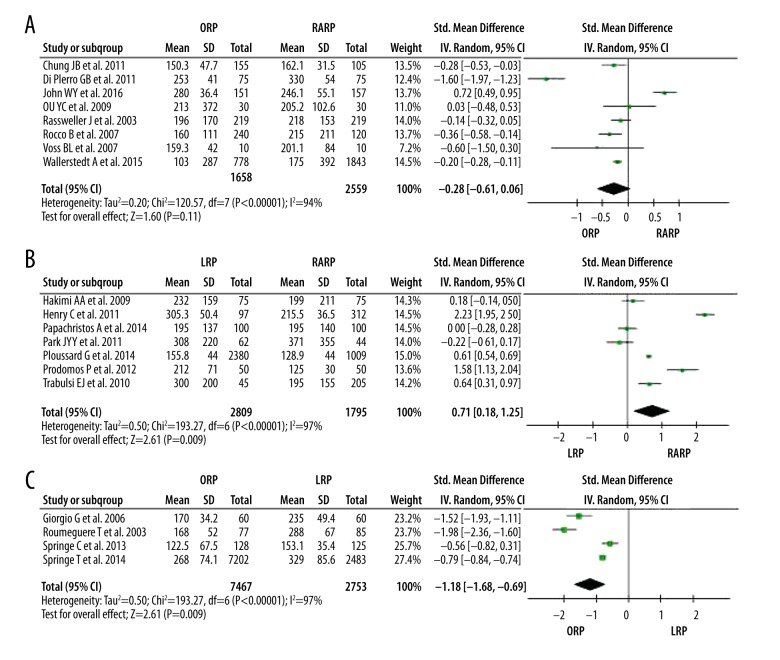
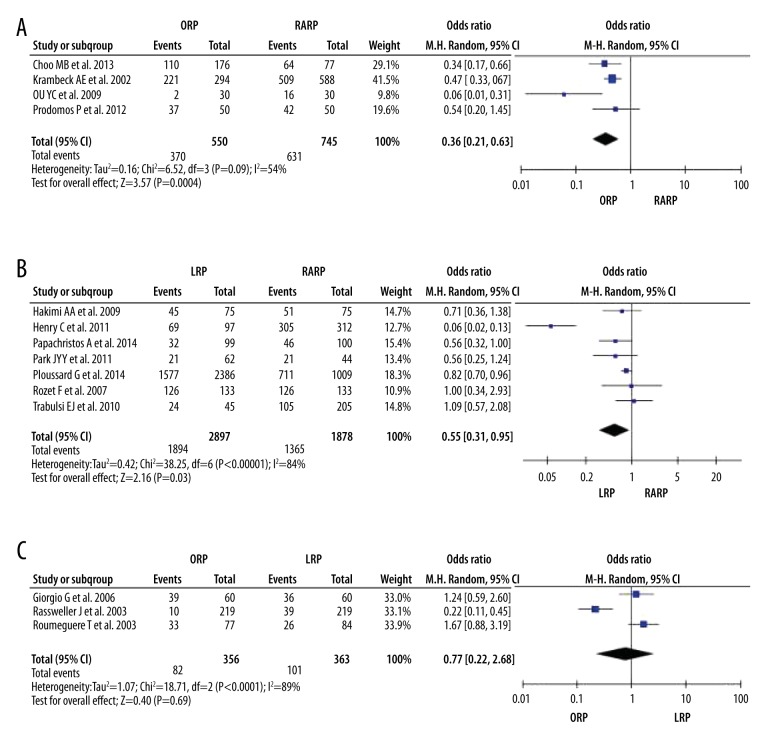
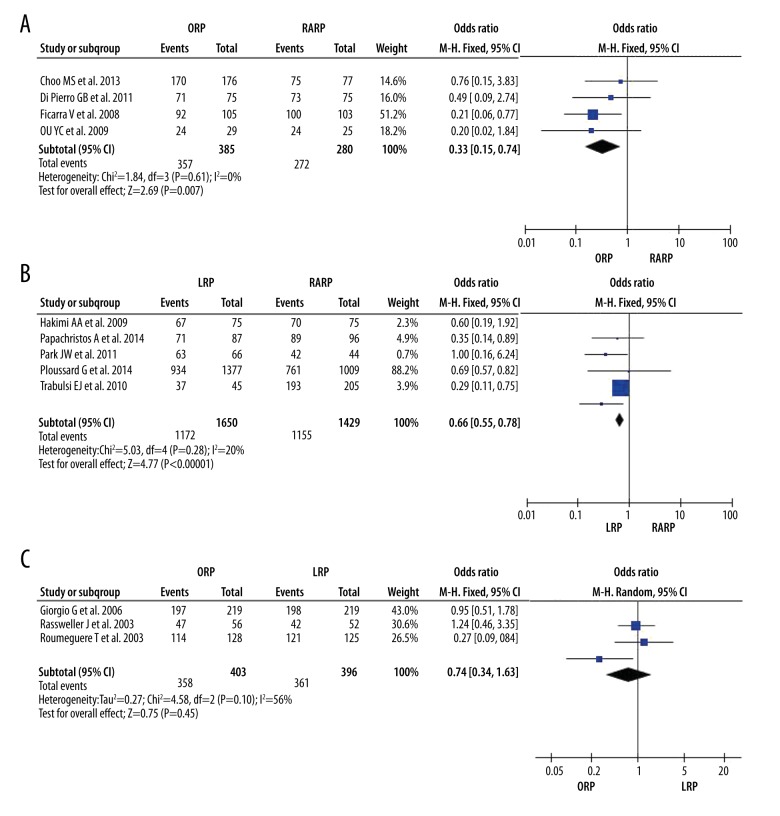
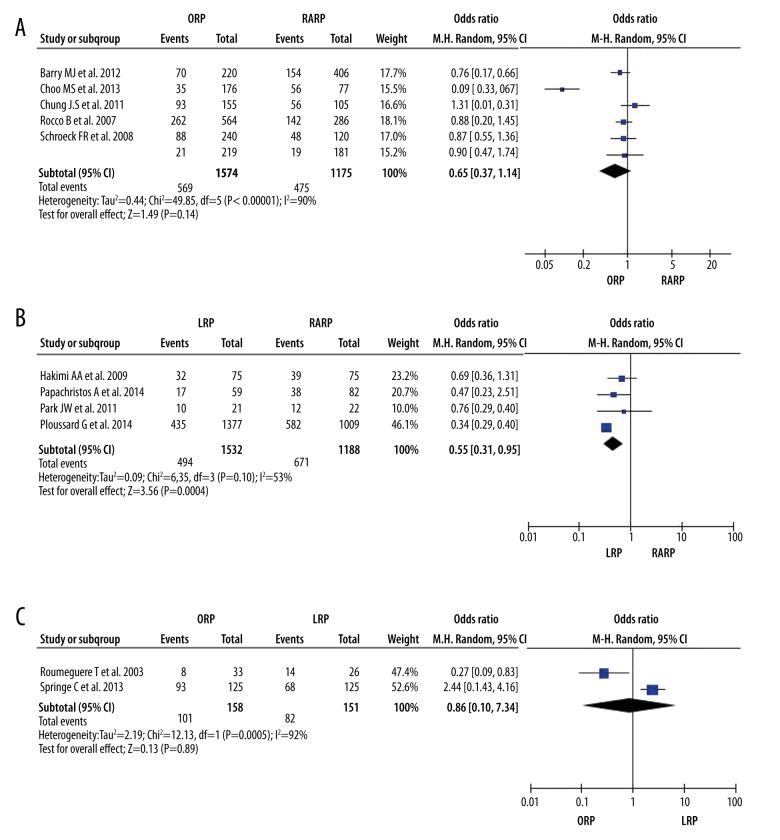
This meta-analysis revealed that blood loss, transfusion rate, and positive surgical margin (PSM) rate were significantly lower following RARP compared with LRP (SMD (95% confidence interval [CI]) 0.31 [0.01, 0.61]; combined ORs (95% CI) 5.32 [1.29, 21.98]; 1.27 [1.10, 1.46]) and ORP (SMD (95% CI) 0.75 [0.30, 1.21]; and combined ORs (95% CI) 3.44 [1.21, 9.79]); positive surgical margin (PSM) rate were significantly lower following RARP compared with LRP (combined ORs (95% CI) 1.27 [1.10, 1.46]), but not ORP (combined ORs (95% CI) 1.27[0.93, 1.72]). These results are presented in Figures 2–4. Operation time was also shorter for RARP than for LRP (SMD (95% CI) 0.71 [0.18, 1.25]), but not significantly shorter than in the ORP group (SMD (95% CI) −0.28 [−0.61, 0.06]). These results are presented in Figure 5. The nerve-sparing, recovery of complete urinary continence, and recovery of erectile function rates were also significantly higher in the RARP compared with the LRP (combined ORs (95% CI) 0.55 [0.31, 0.95]; 0.66 [0.55, 0.78]; 0.46 [0.30, 0.71]) and ORP groups (combined ORs (95% CI) 0.36 [0.21, 0.63]; 0.33 [0.15, 0.74]; 0.65 [0.37, 1.14]). These results are presented in Figures 6–8.
Figure 2.
Forest plot showing the meta-analysis outcomes of the comparisons of blood loss after ORP, LRP and RARP, (A) ORP vs. RARP; (B) LRP vs. RARP; (C) ORP vs. LRP.
Figure 3.
Forest plot showing the meta-analysis outcomes of the comparisons of transfusion rate after ORP, LRP, and RARP, (A) ORP vs. RARP; (B) LRP vs. RARP; (C) ORP vs. LRP.
Figure 4.
Forest plot showing the meta-analysis outcomes of the comparisons of PSM after ORP, LRP and RARP, (A) ORP vs. RARP; (B) LRP vs. RARP; (C) ORP vs. LRP.
Figure 5.
Forest plot showing the meta-analysis outcomes of the comparisons of operate time after ORP, LRP and RARP, (A) ORP vs. RARP; (B) LRP vs. RARP; (C) ORP vs. LRP.
Figure 6.
Forest plot showing the meta-analysis outcomes of the comparisons of nerve sparing rate after ORP, LRP and RARP, (A) ORP vs. RARP; (B) LRP vs. RARP; (C) ORP vs. LRP.
Figure 7.
Forest plot showing the meta-analysis outcomes of the comparisons of urinary continence after ORP, LRP and RARP, (A) ORP vs. RARP; (B) LRP vs. RARP; (C) ORP vs. LRP.
Figure 8.
Forest plot showing the meta-analysis outcomes of the comparisons of erectile function after ORP, LRP and RARP, (A) ORP vs. RARP; (B) LRP vs. RARP; (C) ORP vs. LRP.
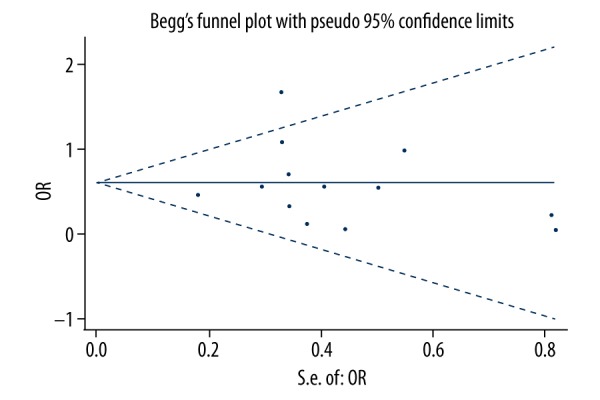
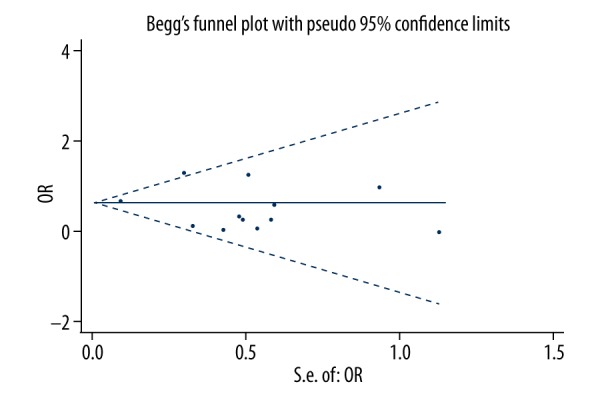
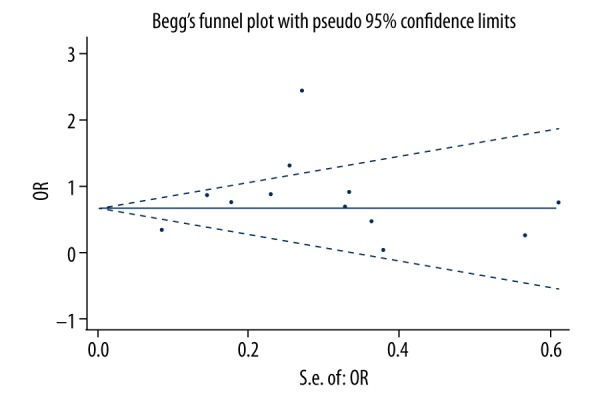
Operation time was lower in the ORP group compared with the LRP group (SMD (95% CI) −1.18 [−1.68, −0.69] (Figure 5), while blood loss and transfusion rate were significantly higher (SMD (95% CI) 1.65 [0.56, 2.74] combined ORs (95% CI) 9.06 [6.35, 12.94]) (Figures 2, 3). However, there was no significant difference in PSM, nerve-sparing, complete urinary continence rate, or erectile dysfunction between the ORP and LRP groups (Figures 7, 8). Begg’s funnel plot showed no substantial asymmetry, except for transfusion rate (Figures 9–15). Begg’s and Egger’s regression tests indicated no significant publication bias (p>0.05) (Tables 2, 3).
Figure 9.
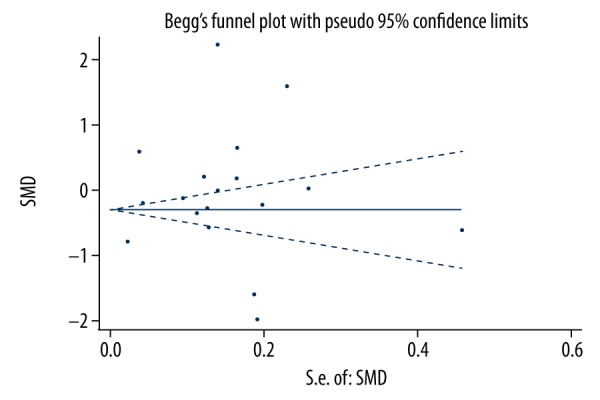
Begg’s publication bias plot of operate time.
Figure 10.
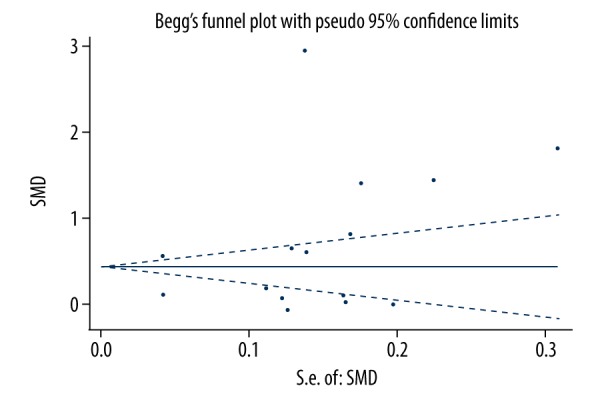
Begg’s publication bias plot of blood loss.
Figure 11.
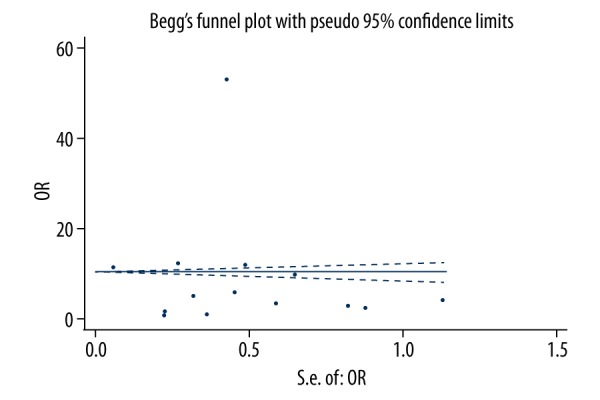
Begg’s publication bias plot of transfusion rate.
Figure 12.
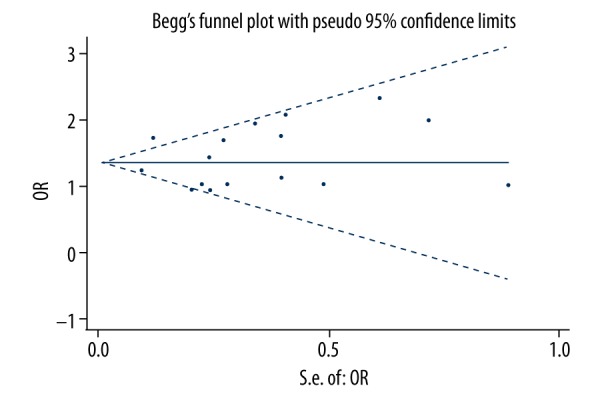
Begg’s publication bias plot of PSM.
Figure 13.
Begg’s publication bias plot of nerve sparing.
Figure 14.
Begg’s publication bias plot of urinary continence.
Figure 15.
Begg’s publication bias plot of erectile function.
Table 2.
The Begg’s test of publication bias.
| Operate time | Blood loss | Transfusion rate | Nerve sparing | PSM | Urinary continence | Erectile function | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Z | P | Z | P | Z | P | Z | P | Z | P | Z | P | Z | P | |
| ORP vs. RARP | −1.33 | 0.171 | 0.96 | 0.319 | 0.97 | 0.321 | −1.36 | 0.174 | 0.71 | 0.455 | −0.68 | 0.497 | −0.56 | 0.573 |
| LRP vs. RARP | 0.25 | 0.805 | 0.49 | 0.624 | −0.49 | 0.624 | −0.75 | 0.453 | 0.45 | 0.652 | 0.00 | 1.000 | 0.68 | 0.497 |
| ORP vs. LRP | −1.54 | 0.113 | −1.39 | 0.177 | 0.69 | 0.492 | −1.00 | 0.315 | 1.00 | 0.314 | −1.57 | 0.117 | −1.00 | 0.317 |
Table 3.
The Egger’s test of publication bias.
| Operate time | Blood loss | Transfusion rate | Nerve sparing | PSM | Urinary continence | Erectile function | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bias | P | Bias | P | Bias | P | Bias | P | Bias | P | Bias | P | Bias | P | |
| ORP vs. RARP | −2.17 | 0.312 | 14.51 | 0.258 | 8.47 | 0.279 | −0.36 | 0.391 | −0.72 | 0.549 | −0.17 | 0.334 | −0.91 | 0.633 |
| LRP vs. RARP | 0.34 | 0.924 | 28.88 | 0.683 | 6.53 | 0.602 | −0.78 | 0.559 | 0.43 | 0.647 | −0.36 | 0.372 | 0.88 | 0.093 |
| ORP vs. LRP | −2.89 | 0.650 | −9.85 | 0.322 | 8.55 | 0.267 | 33.71 | – | 0.16 | – | −2.46 | 0.447 | −7.38 | – |
Discussion
This meta-analysis reviewed and analyzed 33 published studies to investigate and compare the perioperative, functional, and oncologic outcomes of RARP, LRP, and ORP in patients with prostate cancer. The results revealed that RARP was preferable to the other 2 techniques with regard to blood loss, transfusion, nerve-sparing, recovery of urinary continence, and recovery of erectile function rates.
The outcomes were relatively inconsistent because of differences in surgical experiences, equipment, and patient conditions. Among these, surgical experience has been shown to play an important role in improving perioperative outcomes and complications [40–44]. RARP involves high abdominal pressure during surgery by pneumoperitoneum, which could explain the lower bleeding and transfusion rates in the robot-assisted group. Positioning of the patient in the Trendelenburg position, which reduces venous blood pressure, may also contribute to the positive effect of RARP on perioperative bleeding. The longer operating time compared with the open technique, as reported in this study, may explain the more precise operative procedure in RARP, as confirmed in other reports [45,46].
With regard to oncologic outcomes, some studies found that surgical technique was not an independent predictor of PSM [47,48], while some reported that the risk of PSM was dependent on TNM stage and the patient’s preoperative prostate-specific antigen level. Coelho et al. reported that clinical stage was the only preoperative variable independently associated with PSM after RARP [49]. However, the present meta-analysis showed that the PSM rate of RARP was significantly lower than those of LRP. Our results thus differed from the previous studies. The prostatic apex was reported to be the most common location of PSM, and improved visualization of the prostatic apex during RARP may reduce the risk of PSM [8,50–53].
The main objective of radical prostatectomy is cancer control, but maintaining quality of life is an important secondary goal [54]. Many studies have shown that the most common factors influencing quality of life following radical prostatectomy are decreased erectile ability and urinary incontinence [55,56]. Although conventional nerve-sparing radical prostatectomy generally preserves some erectile function, most patients suffer some loss of erectile ability. Some researchers have suggested that bilateral nerve-sparing may aid the recovery of urinary continence and erectile function, but Ludovice et al. reported that bilateral nerve-sparing RARP was associated with faster recovery of continence, but not of erectile function, compared with open prostatectomy [57]. Novara et al. suggested that patient selection was a key factor determining the success of the nerve-sparing technique in the era of robotic surgery [58]. In patients younger than 65 years, the absence of associated co-morbidities and good preoperative erectile function were the most important preoperative factors in selecting patients for bilateral nerve-sparing RARP [58]. In our study, nerve sparing was significantly higher in the RARP group compared with the LRP and ORP groups, but the correlation between nerve sparing and erectile function requires further study.
Urinary continence and erectile function after radical prostatectomy are difficult to compare among studies because their etiology and pathophysiology are poorly understood, and their definitions vary among different investigators. Furthermore, different studies may involve multiple surgeons with different levels of training and laparoscopic surgical experience. These factors thus limit the direct comparison of continence and erectile outcomes between RARP, LRP, and ORP [59].
The advantages of RARP include visualization of locations within the pelvic cavity from various angles, providing excellent views for the surgeon. High-resolution cameras generating three-dimensional images and robotic arms allow surgeons to perform more precise dissection of the anatomic structures, potentially leading to better functional preservation. We suggest that these advantages of RARP would help to overcome the potential impact of prostatic apical shape on the postoperative recovery of urinary continence.
However, the etiologies of incontinence and erectile dysfunction after radical prostatectomy remain unclear. Several studies reported that various factors, including patient characteristics [60–64], surgical techniques, and surgeon experience [65–67], were also associated with postoperative incontinence and erectile dysfunction after radical prostatectomy. A detailed description of pelvic anatomy in relation to radical prostatectomy suggests a positive association between the location of the prostatic apex and membranous urethra in terms of postoperative incontinence [68]. It was suggested that overlap of the urethra by the prostatic apex may be associated with prolonged postoperative incontinence, and overlap may exist anteriorly, posteriorly, or on both sides. Maximal preservation of the sphincter mechanism is widely regarded to be essential for preventing postoperative incontinence. The distal sphincter only extends from the penile bulb to the prostate apex, whereas the proximal sphincter extends to the verumontanum. In our meta-analysis, urinary continence rate and erectile function were significantly better in the RARP group compared with the ORP and LRP groups. However, urinary incontinence and erectile dysfunction are complex multifactorial conditions that require further studies.
There were some limitations to this meta-analysis that need to be considered when interpreting the results. First, the samples were relatively small in all 33 studies. Second, several related studies were excluded because of a lack of control data, or means and SDs. Third, because the studies were conducted in different hospitals, the uneven surgical technique of surgeons may have influenced the results. Fourth, there was strong evidence of heterogeneity among the included studies. Some differences among the studies should be considered: the included studies were based on different populations; PSM was influence by the subjectivity of pathologists and surgeons; and we did not compare the cost of consumables and capital between RARP and LRP or ORP, but a study suggested that RARP con reduce the cost of consumables [69]. These factors limit the ability to form definitive conclusions about the relative clinical value of different prostatectomy procedures. However, this meta-analysis demonstrates that RARP provides more advantages in prostate cancer patients, especially regarding decreased adverse events.
Conclusions
This meta-analysis demonstrates that RARP is superior to LRP and ORP in terms of blood loss, transfusion rate, nerve sparing, urinary continence, and erectile dysfunction recovery, and suggests that RARP offers better results than LRP and ORP in treatment of prostate cancer. However, studies with larger sample sizes and long-term results are needed.
Footnotes
Conflict of interests
None.
Source of support: Our study was supported by the National Science Foundation of China (grant No. 81072107 and 81372736)
References
- 1.Shen H, Zhang L, Zhou J. Epidermal growth factor-containing fibulin-like extracellular matrix protein 1 (EFEMP1) acts as a potential diagnostic biomarker for prostate cancer. Med Sci Monit. 2018;24:216–22. doi: 10.12659/MSM.898809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deng QK, Lei YG, Lin YL. Prognostic value of Protocadherin10 (PCDH10) methylation in serum of prostate cancer patients. Med Sci Monit. 2016;22:516–21. doi: 10.12659/MSM.897179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Raboy A, Ferzli G, Albert P. Initial experience with extraperitoneal endoscopic radical retropubic prostatectomy. Urology. 1997;50:849–53. doi: 10.1016/S0090-4295(97)00485-8. [DOI] [PubMed] [Google Scholar]
- 4.Rassweiler J, Seemann O, Schulze M, et al. Laparoscopic versus open radical prostatectomy: A comparative study at a single institution. J Urol. 2003;169:1689–93. doi: 10.1097/01.ju.0000062614.56629.41. [DOI] [PubMed] [Google Scholar]
- 5.Anastasiadis AG, Salomon L, Katz R, et al. Radical retropubic versus laparoscopic prostatectomy: A prospective comparison of functional outcome. Urology. 2003;62:292–97. doi: 10.1016/s0090-4295(03)00352-2. [DOI] [PubMed] [Google Scholar]
- 6.Ghavamian R, Knoll A, Boczko J, Melman A. Comparison of operative and functional outcomes of laparoscopic radical prostatectomy and radical retropubic prostatectomy: Single surgeon experience. Urology. 2006;67:1241–46. doi: 10.1016/j.urology.2005.12.017. [DOI] [PubMed] [Google Scholar]
- 7.Papachristos A, Basto M, Te Marvelde L, Moon D. Laparoscopic versus robotic-assisted radical prostatectomy: An Australian single-surgeon series. ANZ J Surg. 2015;85:154–58. doi: 10.1111/ans.12602. [DOI] [PubMed] [Google Scholar]
- 8.Koo KC, Tuliao P, Yoon YE, et al. Robot-assisted radical prostatectomy in the Korean population: A 5-year propensity-score matched comparative analysis versus open radical prostatectomy. Int J Urol. 2014;21:781–85. doi: 10.1111/iju.12447. [DOI] [PubMed] [Google Scholar]
- 9.Tozawa K, Yasui T, Umemoto Y, et al. Pitfalls of robot-assisted radical prostatectomy: A comparison of positive surgical margins between robotic and laparoscopic surgery. Int J Urol. 2014;21:976–79. doi: 10.1111/iju.12492. [DOI] [PubMed] [Google Scholar]
- 10.Sugihara T, Yasunaga H, Horiguchi H. Robot-assisted versus other types of radical prostatectomy: Population-based safety and cost comparison in Japan, 2012–2013. Cancer Sci. 2014;105:1421–26. doi: 10.1111/cas.12523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rozet F, Jaffe J, Braud G, et al. A direct comparison of robotic assisted versus pure laparoscopic radical prostatectomy: A single institution experience. J Urol. 2007;178(2):478–82. doi: 10.1016/j.juro.2007.03.111. [DOI] [PubMed] [Google Scholar]
- 12.Hakimi AA, Blitstein J, Feder M, et al. Direct comparison of surgical and functional outcomes of robotic-assisted versus pure laparoscopic radical prostatectomy: Single-surgeon experience. Urology. 2009;73:119–23. doi: 10.1016/j.urology.2008.08.491. [DOI] [PubMed] [Google Scholar]
- 13.Ploussard G, Moulin M, Vordos D. Comparisons of the perioperative, functional, and oncologic outcomes after robot-assisted versus pure extraperitoneal laparoscopic radical prostatectomy. Eur Urol. 2014;65:610–19. doi: 10.1016/j.eururo.2012.11.049. [DOI] [PubMed] [Google Scholar]
- 14.Froehner M, Koch R, Leike S, et al. Urinary tract-related quality of life after radical prostatectomy: Open retropubic versus robot-assisted laparoscopic approach. Urol Int. 2013;90:36–40. doi: 10.1159/000345320. [DOI] [PubMed] [Google Scholar]
- 15.Park JW, Won Lee H, Kim W. Comparative assessment of a single surgeon’s series of laparoscopic radical prostatectomy: Conventional versus robot-assisted. J Endourol. 2011;25:597–602. doi: 10.1089/end.2010.0229. [DOI] [PubMed] [Google Scholar]
- 16.Park JW, Won Lee H, et al. Radical prostatectomy after previous transurethral resection of the prostate: Robot-assisted laparoscopic versus open radical prostatectomy in a matched-pair analysis. J Endourol. 2012;26:1136–41. doi: 10.1089/end.2012.0074. [DOI] [PubMed] [Google Scholar]
- 17.Barry MJ, Gallagher PM, Skinner JS, Fowler FJ., Jr Adverse effects of robotic-assisted laparoscopic versus open retropubic radical prostatectomy among a nationwide random sample of medicare-age men. J Clin Oncol. 2012;30:513–18. doi: 10.1200/JCO.2011.36.8621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Choo MS, Choi WS, Cho SY, et al. Impact of prostate volume on oncological and functional outcomes after radical prostatectomy: Robot-assisted laparoscopic versus open retropubic. Korean J Urol. 2013;54:15–21. doi: 10.4111/kju.2013.54.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schroeck FR, Krupski TL, Sun L, et al. Satisfaction and regret after open retropubic or robot-assisted laparoscopic radical prostatectomy. Eur Urol. 2008;54:785–93. doi: 10.1016/j.eururo.2008.06.063. [DOI] [PubMed] [Google Scholar]
- 20.Voss BL, Santiano K, Milano M, et al. Integrity and amplification of nucleic acids from snap-frozen prostate tissues from robotic-assisted laparoscopic and open prostatectomies. Arch Pathol Lab Med. 2013;137:525–30. doi: 10.5858/arpa.2011-0550-OA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Henry C, Sauvain J, Dubernard P. Mid-term biochemical recurrence-free outcomes following robotic versus laparoscopic radical prostatectomy. J Robotic Surg. 2011;5:251–57. doi: 10.1007/s11701-011-0266-7. [DOI] [PubMed] [Google Scholar]
- 22.Philippou P, Waine E, Rowe E. Robot-assisted laparoscopic prostatectomy versus open: Comparison of the learning curve of a single surgeon. J Endourol. 2012;26:1002–8. doi: 10.1089/end.2011.0569. [DOI] [PubMed] [Google Scholar]
- 23.Barocas DA, Salem S, Kordan Y. Robotic assisted laparoscopic prostatectomy versus radical retropubic prostatectomy for clinically localized prostate cancer: Comparison of short-term biochemical recurrence-free survival. J Urol. 2010;183:990–96. doi: 10.1016/j.juro.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 24.Springer C, Inferrera A, Pini G, et al. Laparoscopic versus open bilateral intrafascial nerve-sparing radical prostatectomy after TUR-P for incidental prostate cancer: Surgical outcomes and effect on postoperative urinary continence and sexual potency. World J Urol. 2013;31:1505–10. doi: 10.1007/s00345-013-1036-0. [DOI] [PubMed] [Google Scholar]
- 25.Rassweiler J, Seemann O, Schulze M, et al. Laparoscopic versus open radical prostatectomy: A comparative study at a single institution. J Urol. 2003;169:1689–93. doi: 10.1097/01.ju.0000062614.56629.41. [DOI] [PubMed] [Google Scholar]
- 26.Roumeguere T, Bollens R, Vanden Bossche M, et al. Radical prostatectomy: A prospective comparison of oncological and functional results between open and laparoscopic approaches. World J Urol. 2003;20:360–66. doi: 10.1007/s00345-002-0306-z. [DOI] [PubMed] [Google Scholar]
- 27.Wallerstedt A, Tyritzis SI, Thorsteinsdottir T, et al. Short-term results after robot-assisted laparoscopic radical prostatectomy compared to open radical prostatectomy. Eur Urol. 2015;67:660–70. doi: 10.1016/j.eururo.2014.09.036. [DOI] [PubMed] [Google Scholar]
- 28.Akand M, Celik O, Avci E, et al. Open, laparoscopic and robot-assisted laparoscopic radical prostatectomy: Comparative analysis of operative and pathologic outcomes for three techniques with a single surgeon’s experience. Eur Rev Med Pharmacol Sci. 2015;19:525–31. [PubMed] [Google Scholar]
- 29.Lee D, Choi SK, Park J, et al. Comparative analysis of oncologic outcomes for open vs. robot-assisted radical prostatectomy in high-risk prostate cancer. Korean J Urol. 2015;56:572–79. doi: 10.4111/kju.2015.56.8.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Di Pierro GB, Baumeister P, Stucki P, et al. A prospective trial comparing consecutive series of open retropubic and robot-assisted laparoscopic radical prostatectomy in a centre with a limited caseload. Eur Urol. 2011;59:1–6. doi: 10.1016/j.eururo.2010.10.026. [DOI] [PubMed] [Google Scholar]
- 31.Ou YC, Yang CR, Wang J. Comparison of robotic-assisted versus retropubic radical prostatectomy performed by a single surgeon. Anticancer Res. 2009;29:1637–42. [PubMed] [Google Scholar]
- 32.Rocco B, Matei DV, Melegari S, et al. Robotic vs. open prostatectomy in a laparoscopically native centre: A matched-pair analysis. BJU Int. 2009;104:991–95. doi: 10.1111/j.1464-410X.2009.08532.x. [DOI] [PubMed] [Google Scholar]
- 33.Krambeck AE, DiMarco DS, Rangel LJ. Radical prostatectomy for prostatic adenocarcinoma: A matched comparison of open retropubic and robot-assisted techniques. BJU Int. 2009;103:448–53. doi: 10.1111/j.1464-410X.2008.08012.x. [DOI] [PubMed] [Google Scholar]
- 34.Trabulsi EJ, Zola JC, Gomella LG, Lallas CD. Transition from pure laparoscopic to robotic-assisted radical prostatectomy: A single surgeon institutional evolution. Urol Oncol. 2010;28:81–85. doi: 10.1016/j.urolonc.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 35.Kwon EO, Bautista TC, Jung H. Impact of robotic training on surgical and pathologic outcomes during robot-assisted laparoscopic radical prostatectomy. Urology. 2010;76:363–68. doi: 10.1016/j.urology.2009.09.085. [DOI] [PubMed] [Google Scholar]
- 36.Chung JS, Kim WT, Ham WS, et al. Comparison of oncological results, functional outcomes, and complications for transperitoneal versus extraperitoneal robot-assisted radical prostatectomy: A single surgeon’s experience. J Endourol. 2011;25:787–92. doi: 10.1089/end.2010.0222. [DOI] [PubMed] [Google Scholar]
- 37.Ficarra V, Novara G, Fracalanza S, et al. A prospective, non-randomized trial comparing robot-assisted laparoscopic and retropubic radical prostatectomy in one European institution. BJU Int. 2009;104:534–59. doi: 10.1111/j.1464-410X.2009.08419.x. [DOI] [PubMed] [Google Scholar]
- 38.Yaxley JW, Coughlin GD, Chambers SK, et al. Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: Early outcomes from a randomised controlled phase 3 study. Lancet. 2016;388:1057–66. doi: 10.1016/S0140-6736(16)30592-X. [DOI] [PubMed] [Google Scholar]
- 39.Guazzoni G, Cestari A, Naspro R, et al. Intra- and peri-operative outcomes comparing radical retropubic and laparoscopic radicalprostatectomy: Results from a prospective, randomised, single-surgeon study. Eur Urol. 2006;50:98–104. doi: 10.1016/j.eururo.2006.02.051. [DOI] [PubMed] [Google Scholar]
- 40.Menon M, Hemal AK. Vattikuti Institute prostatectomy: A technique of robotic radical prostatectomy: Experience in more than 1000 cases (discussion 619) J Endourol. 2004;18:611–19. doi: 10.1089/end.2004.18.611. [DOI] [PubMed] [Google Scholar]
- 41.Ahlering TE, Skarecky D, Lee D, Clayman RV. Successful transfer of open surgical skills to a laparoscopic environment using a robotic interface: Initial experience with laparoscopic radical prostatectomy. J Urol. 2003;170:1738–41. doi: 10.1097/01.ju.0000092881.24608.5e. [DOI] [PubMed] [Google Scholar]
- 42.Patel VR, Tully AS, Holmes R, Lindsay J. Robotic radical prostatectomy in the community setting: The learning curve and beyond: Initial 200 cases. J Urol. 2005;174:269–72. doi: 10.1097/01.ju.0000162082.12962.40. [DOI] [PubMed] [Google Scholar]
- 43.Smith JA, Herrell SD. Robotic-assisted laparoscopic prostatectomy: Do minimally invasive approaches offer significant advantages? J Clin Oncol. 2005;23:8170–75. doi: 10.1200/JCO.2005.03.1963. [DOI] [PubMed] [Google Scholar]
- 44.Hoznek A, Salomon L, Olsson LE, et al. Laparoscopic radical prostatectomy. The Creteil experience. Eur Urol. 2001;40:38–45. doi: 10.1159/000049747. [DOI] [PubMed] [Google Scholar]
- 45.Krambeck AE, DiMarco DS, Rangel LJ. Radical prostatectomy for prostatic adenocarcinoma: A matched comparison of open retropubic and robot-assisted techniques. BJU Int. 2009;103:448–53. doi: 10.1111/j.1464-410X.2008.08012.x. [DOI] [PubMed] [Google Scholar]
- 46.Tewari A, Srivasatava A, Menon M. A prospective comparison of radical retropubic and robot-assisted prostatectomy: Experience in one institution. BJU Int. 2003;92:205–10. doi: 10.1046/j.1464-410x.2003.04311.x. [DOI] [PubMed] [Google Scholar]
- 47.Silberstein JL, Su D, Glickman L, et al. A case-mix-adjusted comparison of early oncological outcomes of open and robotic prostatectomy performed by experienced high-volume surgeons. BJU Int. 2013;111:206–12. doi: 10.1111/j.1464-410X.2012.11638.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Laurila TA, Huang W, Jarrard DF. Robotic-assisted laparoscopic and radical retropubic prostatectomy generate similar positive margin rates in low and intermediate risk patients. Urol Oncol. 2009;27:529–33. doi: 10.1016/j.urolonc.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 49.Coelho RF, Chauhan S, Orvieto MA, et al. Predictive factors for positive surgical margins and their locations after robot-assisted laparoscopic radical prostatectomy. Eur Urol. 2010;57:1022–29. doi: 10.1016/j.eururo.2010.01.040. [DOI] [PubMed] [Google Scholar]
- 50.White MA, De Haan AP, Stephens DD. Comparative analysis of surgical margins between radical retropubic prostatectomy and RARP: Are patients sacrificed during initiation of robotics program? Urology. 2009;73:567–71. doi: 10.1016/j.urology.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 51.Williams SB, Chen MH, D’Amico AV. Radical retropubic prostatectomy and robot-assisted laparoscopic prostatectomy: Likelihood of positive surgical margin(s) Urology. 2010;76:1097–101. doi: 10.1016/j.urology.2009.11.079. [DOI] [PubMed] [Google Scholar]
- 52.Kasraeian A, Barret E, Chan J, et al. Comparison of the rate, location and size of positive surgical margins after laparoscopic and robot-assisted laparoscopic radical prostatectomy. BJU Int. 2011;108:1174–78. doi: 10.1111/j.1464-410X.2010.10077.x. [DOI] [PubMed] [Google Scholar]
- 53.Srigley JR. Key issues in handling and reporting radical prostatectomy specimens. Arch Pathol Lab Med. 2006;130:303–17. doi: 10.5858/2006-130-303-KIIHAR. [DOI] [PubMed] [Google Scholar]
- 54.Magheli A, Gonzalgo ML, Su LM. Impact of surgical technique (open vs. laparoscopic vs. robotic-assisted) on pathological and biochemical outcomes following radical prostatectomy: An analysis using propensity score matching. BJU Int. 2011;107:1956–62. doi: 10.1111/j.1464-410X.2010.09795.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Walsh PC. Patient-reported impotence and incontinence after nerve-sparing radical prostatectomy. J Urol. 1998;159:308–9. [PubMed] [Google Scholar]
- 56.Stanford JL, Feng Z, Hamilton AS, et al. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: The Prostate Cancer Outcomes Study. JAMA. 2000;283:354–60. doi: 10.1001/jama.283.3.354. [DOI] [PubMed] [Google Scholar]
- 57.Ludovico GM, Dachille G, Pagliarulo G. Bilateral nerve sparing robotic-assisted radical prostatectomy is associated with faster continence recovery but not with erectile function recovery compared with retropubic open prostatectomy: The need for accurate selection of patients. Oncol Rep. 2013;29:2445–50. doi: 10.3892/or.2013.2365. [DOI] [PubMed] [Google Scholar]
- 58.Novara G, Ficarra V, D’Elia C. Evaluating urinary continence and preoperative predictors of urinary continence after robot assisted laparoscopic radical prostatectomy. J Urol. 2010;184:1028–33. doi: 10.1016/j.juro.2010.04.069. [DOI] [PubMed] [Google Scholar]
- 59.Shikanov S, Desai V, Razmaria A, et al. Robotic radical prostatectomy for elderly patients: probability of achieving continence and potency 1 year after surgery. J Urol. 2010;183:1803–7. doi: 10.1016/j.juro.2010.01.016. [DOI] [PubMed] [Google Scholar]
- 60.Link BA, Nelson R, Josephson DY. The impact of prostate gland weight in robot assisted laparoscopic radical prostatectomy. J Urol. 2008;180:928–32. doi: 10.1016/j.juro.2008.05.029. [DOI] [PubMed] [Google Scholar]
- 61.Skolarus TA, Hedgepeth RC, Zhang Y, et al. Does robotic technology mitigate the challenges of large prostate size? Urology. 2010;76:1117–21. doi: 10.1016/j.urology.2010.03.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zorn KC, Wille MA, Thong AE. Continued improvement of perioperative, pathological and continence outcomes during 700 robot-assisted radical prostatectomies. Can J Urol. 2009;16:4742–49. [PubMed] [Google Scholar]
- 63.Bentas W, Wolfram M, Jones J, et al. Robotic technology and the translation of open radical prostatectomy to laparoscopy: The early Frankfurt experience with robotic radical prostatectomy and one year follow-up. Eur Urol. 2003;44:175–81. doi: 10.1016/s0302-2838(03)00256-2. [DOI] [PubMed] [Google Scholar]
- 64.Menon M, Kaul S, Bhandari A, et al. Potency following robotic radical prostatectomy: A questionnaire based analysis of outcomes after conventional nerve sparing and prostatic fascia sparing techniques. J Urol. 2005;174:2291–96. doi: 10.1097/01.ju.0000181825.54480.eb. [DOI] [PubMed] [Google Scholar]
- 65.Talcott JA, Rieker P, Propert KJ. Patient-reported impotence andincontinence after nerve-sparing radical prostatectomy. J Natl Cancer Inst. 1997;89:1117–23. doi: 10.1093/jnci/89.15.1117. [DOI] [PubMed] [Google Scholar]
- 66.Hu JC, Gu X, Lipsitz SR, et al. Comparative effectiveness of minimally invasive vs. open radical prostatectomy. JAMA. 2009;302:1557–64. doi: 10.1001/jama.2009.1451. [DOI] [PubMed] [Google Scholar]
- 67.Cooperberg MR, Odisho AY, Carroll PR. Outcomes for radical prostatectomy: Is it the singer, the song, or both? J Clin Oncol. 2012;30:476–78. doi: 10.1200/JCO.2011.38.9593. [DOI] [PubMed] [Google Scholar]
- 68.Masterson TA, Cheng L, Boris RS, Koch MO. Open vs. robotic-assisted radical prostatectomy: A single surgeon and pathologist comparison of pathologic and oncologic outcomes. Urol Oncol. 2013;31:1043–48. doi: 10.1016/j.urolonc.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 69.Basto M, Sathianathen N, Te Marvelde L, et al. Patterns-of-care and health economic analysis of robot-assisted radical prostatectomy in the Australian public health system. BJU Int. 2016;117:930–39. doi: 10.1111/bju.13317. [DOI] [PubMed] [Google Scholar]