Abstract
Malignant B cells in chronic lymphocytic leukemia serve an essential role in the whole immune response, so their interactions with other immune cells are more complex than observed in solid tumors. The latest study results indicate that the immune dysregulation in chronic lymphocytic leukemia (CLL) also affects a small population of invariant natural killer T cells (iNKT). Using peripheral blood iNKT cells obtained from patients with CLL, the objective of the present study was to assess the intracellular expression of typical cytokines involved in the Th1 (IFN-γ) and Th2 (IL-4) response pathways following stimulation with the iNKT-specific ligand α-galactosylceramide. iNKT cells from patients with CLL exhibited upregulated IL-4 and IFN-γ expression in comparison to those from HVs. No significant association between the ability of iNKT cells to produce IL-4 or IFN-γ and the expression of CD1d on leukemic B lymphocytes or monocytes was identified. However, the function of iNKT cells was compromised in patients with CLL by a strong Th2 bias (high IL-4 and low IFN-γ expression). The ratio of iNKT+IFN-γ+:iNKT+IL-4+ was significantly decreased in the CLL group when compared with HVs, and this decreased further as the disease progressed. This change may result in the promotion of leukemic B lymphocyte survival. Therefore, in the pathogenesis of CLL, Th2 bias may delay the antitumor response that relies on stimulation of the Th1 immune response.
Keywords: chronic lymphocytic leukemia, invariant natural killer T cells, interleukin-4, interferon-γ, CD1d
Introduction
In chronic lymphocytic leukemia (CLL), malignant B lymphocytes, similar to other tumor cells, are in constant cooperation with the tumor microenvironment, which is formed by cancer cells through the recruitment and alteration of non-malignant cells of the immune system (1). In their proximate surroundings, neoplastic B cells interact with neighboring cells that include mesenchymal stromal cells, monocytes, monocyte-derived nurse-like cells, and T cells (2). These interactions provide B cell clones with supporting factors that inhibit or delay programmed apoptosis and thereby sustain disease progression (3). The dialogue between CLL B cells and interacting T lymphocytes may involve cytokines (4). The present study focused on a population of T lymphocytes, known as invariant natural killer T cells (iNKT) (5). The role of iNKT in tumor immunity is only partially understood and is poorly described in CLL. This unique cell subset combines features of T lymphocytes and NK cells (6). Unlike conventional T lymphocytes, they express markedly less variable T cell receptors (TCRαβ), and are formed by an invariant α chain (Vα24Jα18) combined with a limited set of β chains, mainly containing Vβ11 (7–9). Using such TCR receptors, iNKT cells recognize lipids and glycolipids, presented by a non-classical MHC molecule known as CD1d (10). The agent most efficient in binding to CD1d is a synthetic compound that originated from marine sponges, known as α-galactosylceramide (α-GalCer). The discovery of this potent agonist facilitated further understanding of the biology of iNKT (11–13). Activated iNKT cells simultaneously secrete interferon (IFN)-γ and interleukin (IL)-4 (14). In addition, they can release other pro-inflammatory Th1 cytokines [such as tumor necrosis factor (TNF)-α and IL-6] and anti-inflammatory Th2 cytokines [such as IL-10, IL-13 and transforming growth factor (TGF)-β] (14–16). This enables iNKT cells to influence other cells of the immune system, including NK cells, cytotoxic T lymphocytes, helper T cells, B cells and antigen presenting cells (APC) (17–19). Certain pathological conditions may cause a change in the Th0-like pattern of cytokines secreted by iNKT cells and polarize their response in the Th1 or Th2 direction (10,20). Such iNKT cells can modify the microenvironment and influence tumor control (21). The role of these cells in the pathogenesis and clinical course of CLL is not well known. Understanding the function of iNKT cells in this specific type of leukemia requires critical analysis of the cytokine release profile. In the current study, the intracellular expression of IFN-γ and IL-4 was analyzed by stimulating the iNKT cells.
Materials and methods
Patients and samples
Peripheral blood (PB) samples were obtained from 60 patients with CLL (29 females and 31 males; median age, 67 years; range, 46–87 years) who met the diagnostic criteria of the International Workshop on Chronic Lymphocytic Leukemia (IWCLL) 2008 (22). All samples were collected at the time of diagnosis and prior to any anticancer therapy from September 2014 to June 2016 in the Department of Hemato-Oncology and Bone Marrow Transplantation of the Medical University of Lublin (Lublin, Poland). According to the Rai classification (23), 24 patients were Stage 0, 17 patients were Stage I, 7 patients were Stage II, 8 patients were Stage III and 4 patients were Stage IV. Participants' characteristics at the time of diagnosis are summarized in Table I. Control PB samples were obtained from 28 healthy volunteers (HVs; 12 females and 16 males, aged from 36–83 years, median, 57 years).
Table I.
Clinical characteristics of patients with CLL.
| A, Total number of patients. | |
|---|---|
| Variables | Patient no. (%) |
| Sex | |
| Female (%) | 29 (48.30) |
| Male (%) | 31 (51.70) |
| Rai stage | |
| 0 (%) | 24 (40.00) |
| I (%) | 17 (28.30) |
| II (%) | 7 (11.70) |
| III (%) | 8 (13.30) |
| IV (%) | 4 (6.70) |
| ZAP-70 (cut-off 20%)a | |
| Positive (%) | 28 (46.70) |
| Negative (%) | 32 (53.30) |
| CD38 (cut-off 20%)b | |
| Positive (%) | 26 (46.30) |
| Negative (%) | 34 (56.70) |
| Cytogenetic abnormalities | |
| del(17p13.1) (%) | 4 (6.70) |
| del(11q22.3) (%) | 6 (10.00) |
| Without del(17p13.1) and | 50 (83.30) |
| del(11q22.3) (%) | |
| Patients requiring therapy | 12 (20.00) |
| Untreated patients | 48 (80.00) |
| B, Median range of patient data. | |
| Variables | Median (range) |
| Age at diagnosis (years) | 67 (46–87) |
| WBC count (G/l) | 26.41 (11.96–280.46) |
| Lymphocyte count (G/l) | 19.91 (5.62–269.13) |
| β2M (mg/dl) | 2.26 (1.36–8.10) |
| LDH (IU/l) | 387.00 (287.00–839.00) |
| Hemoglobin (g/dl) | 14.20 (8.20–17.20) |
| Platelets (G/l) | 183.00 (70.00–339.00) |
| % CD19+/CD5+/ZAP-70+ cellsa | 17.02 (2.41–58.43) |
| % CD19+/CD5+/CD38+ cellsb | 10.13 (0.72–87.72) |
| % iNKT cells (Vα24-Jα18+/CD3+)c | 0.21 (0.01–1.51) |
CLL, chronic lymphocytic leukemia; WBC, white blood cell; LDH, Lactate dehydrogenase; β2M, β2-microglobulin.
Patients with ZAP-70 expression lower or higher than 20% were classified as ZAP-70 negative or positive, respectively.
Patients with CD38 expression lower or higher than 30% were classified as CD38 negative or positive, respectively.
% among CD3+ lymphocytes.
Ethics statement
The current study was approved by the Ethics Committee of the Medical University of Lublin (Lublin, Poland). Written informed consent was obtained from all patients with respect to the use of their blood for scientific purposes.
Activation of iNKT cells with α-GalCer and analysis of intracellular IL-4 and IFN-γ expression
PB samples were collected into heparinized tubes. PB samples were kept at room temperature and used within 1–2 h. Whole blood samples were cultured in round-bottom FACS tubes. For intracellular cytokine expression, iNKT cells in the PB were activated using 100 ng/ml α-GalCer (KRN700; Enzo Life Sciences, Inc., Farmingdale, NY, USA) for 24 h at 37°C in a 5% CO2 atmosphere, followed by the addition of the protein transport inhibitor BD GolgiPlug™ (BD Biosciences, Franklin Lakes, NJ, USA) for the last 6 h of activation. Furthermore, this procedure was performed on non-activated lymphocytes using only BD GolgiPlug™ to assess the level of residual IL-4 and IFN-γ synthesis from in vivo activation. Cultured cells were then stained with monoclonal antibodies (MoAbs) against cell-surface markers: anti-iNKT cells FITC (TCR Vα24-Jα18, clone 6B11; cat. no. 558371, 20 µl/test) and anti-CD3 PE-Cy5 (clone HIT3a; cat. no. 555341, 20 µl/test) supplied by BD Biosciences; incubation was performed for 20 min at room temperature. Following membrane staining, cells were fixed and permeabilized with Cytofix/Cytoperm™ solution and Perm/Wash buffer (BD Biosciences), according to the manufacturer's protocol. Cells were then intracellularly stained with anti-IL-4 PE (clone 3010.211; BD Biosciences; cat. no. 340451, 20 µl/test, 1.25 µg/ml) or anti-IFN-γ PE (clone 25723.11, BD Biosciences; cat. no. 340452, 20 µl/test, 7.5 µg/ml) MoAbs (30 min at 4°C in the dark) and washed twice in PBS. Finally, the cells were analyzed by flow cytometry using FACSCalibur™ (BD Biosciences).
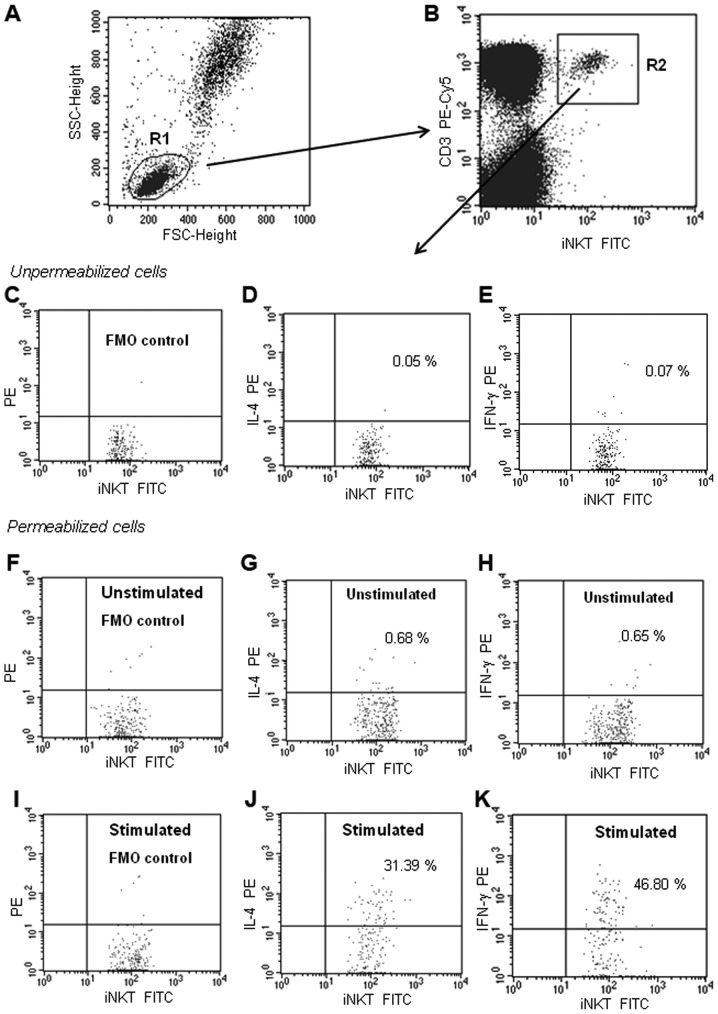
Flow cytometry analysis
Samples were analyzed by flow cytometry directly following preparation. A FACSCalibur™ instrument (BD Biosciences) and BD CellQuest Pro software version 6.0 (BD Biosciences) were used. For each analysis, 200,000 events were acquired and analyzed. In the experiment, the percentage of iNKT cells with IL-4 or IFN-γ expression was determined. iNKT were defined as Vα24-Jα18+/CD3+ cells. Dot plots illustrating the analysis method for the identification of iNKT cells expressing IL-4 and IFN-γ are presented in Fig. 1A-K. An acquisition gate was put on lymphocytes according to the forward scatter (FSC) and side scatter (SSC) properties (Fig. 1A). iNKT cells were defined and gated on a dot plot of iNKT FITC (TCR Vα24-Jα18) vs. CD3 PE-Cy5 (Fig. 1B). Within those cells, the cytokine expressing cells were identified. To establish the gating strategy, a fluorescence minus one (FMO) control was used. The FMO control tube included all antibodies that were used for iNKT cell staining (anti-TCR Vα24-Jα18 FITC and anti-CD3 PE-Cy5), except for the antibody (IL-4 PE or IFN-γ PE) that was measured. The FMO control allowed the consideration of any spread of fluorochromes into the unlabeled channel, and the placing of gates in the correct place. The results are expressed as the percentage of iNKT cells with intracellular IL-4 or IFN-γ expression. Specificity of anti-IL-4 PE and anti-IFN-γ PE MoAbs was evaluated through the estimation of unpermeabilized cells (Fig. 1C-E). Staining of unstimulated (24-h culture only with BD GolgiPlug™; Fig. 1F-H) as well as stimulated iNKT cells was performed (Fig. 1I-K).
Figure 1.
Representative dot plots illustrating the analysis method for the identification of iNKT+ cells with IL-4 or IFN-γ expression. (A) An acquisition gate was established based on FSC and SSC that included mononuclear cells. The R1 region was drawn around the lymphocytes. (B) The R1 gated events were analyzed for TCR Vα24-Jα18 FITC (anti-iNKT) and CD3 PE-Cy5 staining, and the positive cells were gated (region R2). The dot plots C-K were established by the combined gating of events using R1 and R2 regions. Three dot plots (C-E) indicate no-permeabilization control (checking whether the antibody binds to the antigen only after permeabilization). Six dot plots (F-K) indicate the identification of iNKT cells with intracellular IL-4 or IFN-γ (after permeabilization). (C, F and I) Dot plots indicating the FMO control, which contains all the fluorochromes in a panel, except for the one (IL-4 PE or IFN-γ PE) that was measured. The final dot plots indicate iNKT cells (TCR Vα24-Jα18 FITC+CD3PE-Cy5+) cells positive for (D, G and J) IL-4 or (E, H and K) IFN-γ. (D and E) The number in the upper right quadrant represents the percentage of iNKT cells that bound the anti-IL-4 or anti-IFN-γ MoAbs without permeabilization (non-specific binding). (G and H) The two dot-plots represent IL-4 and IFN-γ expression in the unstimulated iNKT cells (non-activated cells from 24-h culture only with BD GolgiPlug™). (J and K) The number in the upper right quadrant represents the percentage of iNKT cells with intracellular IL-4 or IFN-γ expression (after α-GalCer stimulation). FSC, forward scatter; SCC side scatter; FMO, Fluorescence Minus One Control; CLL, chronic lymphocytic leukemia; iNKT, invariant natural killer T cells; IL, interleukin; IFN, interferon; α-GalCer, α-galactosylceramide; MoAb, monoclonal antibody.
Sorting of iNKT cells for reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
In 10 CLL cases and 5 HV cases (from 24-h culture with and without α-GalCer stimulation), the iNKT cells were purified. A BD FACSAria™ flow cytometer (BD Biosciences) was used for iNKT cell sorting. In this case, the iNKT cells were labeled with antibodies against TCR, Vα24-Jα18 PE and CD3 FITC (BD Biosciences), following which the double-positive population was selected. A standard whole-blood assay with erythrocyte cell lysis was used for preparing the PB specimens. After sorting, the iNKT cell purity was >97%.
RNA preparation and RT-qPCR) for IL-4 and IFN-γ in iNKT cells
Purified iNKT cells were used for RNA isolation. Total RNA was isolated using the QIAamp® RNA Blood Mini kit (Qiagen, Inc., Valencia, CA, USA; cat. no. 52304). RNA was transcribed into cDNA using the QuantiTect® Reverse Transcription kit (Qiagen, Inc.; cat. no. 205311), according to the manufacturer's protocol. RT-qPCR was performed using TaqMan reagents specific for human IL-4 and IFN-γ (Applied Biosystems; Thermo Fisher Scientific, Inc., Waltham, MA, USA; cat. no. 4331182), and β-actin was used as the internal control (Applied Biosystems; Thermo Fisher Scientific, Inc.; cat. no. 4326315E). RT-qPCR reactions were run for 40 cycles using universal cycling conditions (95°C for 10 min followed by 40 cycles at 95°C for 15 sec and 60°C for 1 min) on an Applied Biosystems 7300 Real-Time PCR System. Data were normalized to β-actin expression (endogenous control), analyzed using the threshold cycle (Cq) and presented as 2ΔCq. ΔCq is the difference between the Cq of the target gene (Cqt) and the reference gene (Cqr; DCq = Cqt-Cqr) (24).
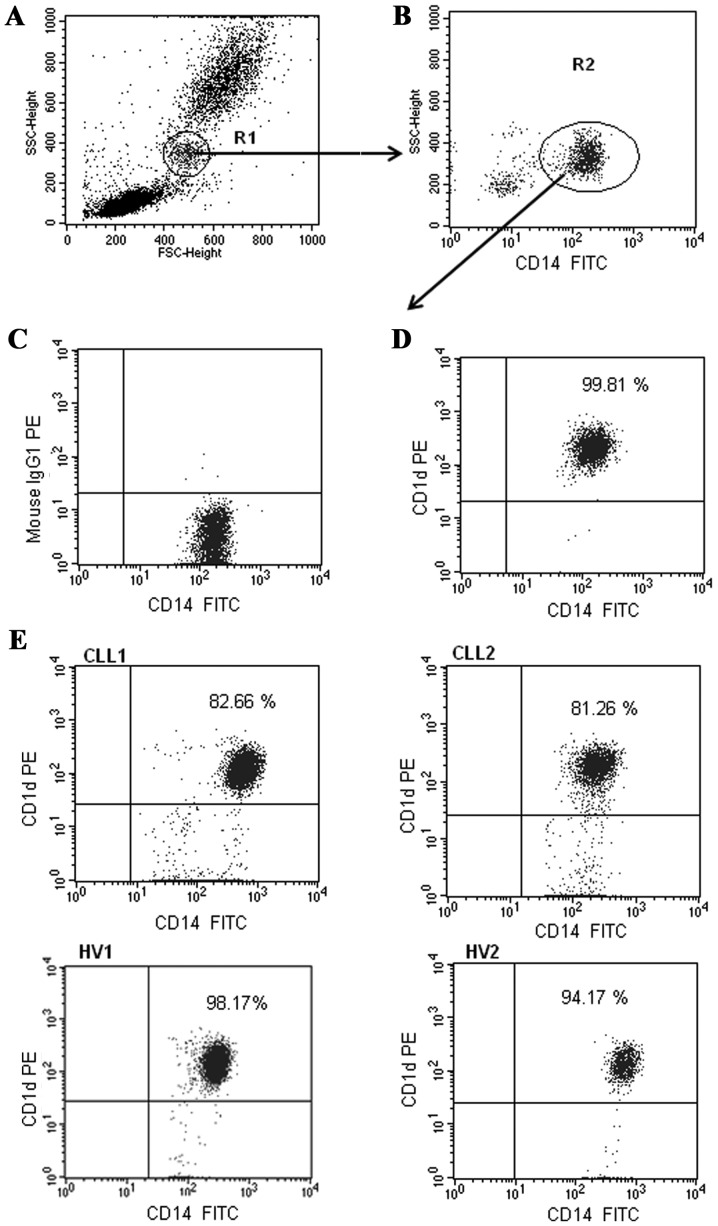
Analysis of CD1d expression on monocytes and B cells
Flow cytometry analysis of CD19+ B cells and CD14+ monocytes expressing CD1d was performed on fresh PB samples stained with anti-CD1d PE (clone CD1d42; cat. no. 550255, 20 µl/test), anti-CD19 FITC (clone SJ25C1; cat. no. 34040, 20 µl/test, 6 µg/ml) and anti-CD14 FITC (clone MφP9; cat. no. 347493; 20 µl/test, 25 µg/ml) MoAbs from BD Biosciences. Cells were incubated for 20 min at room temperature. A standard whole-blood assay with erythrocyte cell lysis was used for preparing all PB specimens. Samples were analyzed by flow cytometry directly following preparation. In the experiment, the percentage of CD1d+/CD19+ and CD1d+/CD14+ cells, and the level of CD1d expression on monocytes and B cells, indicated by the mean fluorescence intensity (MFI), were analyzed. Dot plots illustrating the analysis method for the identification of monocytes with membrane expression of CD1d are presented in Fig. 2. The identification method of CD1d-positive CD19+ B lymphocytes was exhibited in our previous study (25).
Figure 2.
Representative dot plots illustrating the method of analysis for the identification of monocytes with CD1d expression. (A) First, monocytes were gated (R1 region) based on FSC and SSC. (B) Dot plot of monocytes: CD14 FITC vs. SSC. CD14 positive cells were selected (region R2). Final dot plots (C) CD14 FITC vs. mouse IgG1 PE and (D and E) CD14 FITC vs. CD1d PE were established via the combined gating of events using R1 and R2 regions. The numbers in the upper right quadrant on the dot plots represent the percentage of monocytes with CD1d membrane expression (CD14+CD1d+). (E) The dot plots indicate two representative types of CD1d expression on the monocytes from patients with CLL (CLL1-CLL2) and two representative types of CD1d expression on the monocytes from HVs (HV1-HV2). FSC, forward scatter; SCC side scatter; HV, healthy volunteer.
Cells isolation for the determination of apoptosis
Mononuclear cells were separated from PB samples by density gradient centrifugation with Biocoll Separating Solution (Biochrom, Ltd., Cambridge, UK) for 25 min at 400 × g and room temperature. Interphase cells were removed, washed twice and resuspended in PBS.
Determination of apoptosis by MitoTracker® Red CMXRos
In 20 patients with CLL an apoptosis analysis within the CD19+ cell population was performed. A previously described method was used for flow cytometric examination of the percentage of early apoptotic cells (ΔΨmlow) (26–28). The level of apoptosis was measured by chloromethyl-X-rosamine staining (MitoTracker® Red CMXRos; Molecular Probes; Thermo Fisher Scientific, Inc.; cat. no. M7512). CMXRos is a cationic lipophilic fluorochrome that can be used to detect disruptions in the mitochondrial membrane potential (∆Ψm). CMXRos was used in combination with an anti-CD19 FITC MoAb (BD Biosciences). Mononuclear cells were incubated with CMXRos for 30 min at 37°C and, after 15 min of incubation, the anti-CD19 MoAb was added. The CD19+ cells that were determined to be apoptotic exhibited a decrease in the mitochondrial membrane potential following CMXRos staining (∆Ψmlow). The percentage of apoptotic cells (∆Ψmlow/CD19+) was measured at the time of diagnosis (ex vivo), and in vitro after 24 h incubation at 37°C in RPMI-1640 supplemented with 2 mmol/l L-glutamine (Biochrom, Ltd., Cambridge, UK; cat. no. FG1215), 10% fetal calf serum (Biochrom, Ltd.; cat. no. S0113), 100 U/ml penicillin and 100 µg/ml streptomycin (Biochrom, Ltd.; cat. no. A2212), and with and without 100 ng/ml α-GalCer stimulation.
Analysis of CD69 expression on iNKT cells
For the assessment of CD69 expression on iNKT cells, PB mononuclear cells were incubated with the following MoAbs: TCR Vα24-Jα18 FITC (clone 6B11; BD Biosciences; cat. no. 558371; 20 m/test), CD3 PE-Cy5 (clone HIT3a; BD Biosciences; cat. no. 555341; 20 µl/test) and CD69 PE (clone FN50; BD Biosciences; cat. no. 555531, 20 µl/test). Samples were analyzed using flow cytometry immediately following preparation.
Statistical analysis
Data are presented as the median and range. The Mann-Whitney U test was applied for statistical comparisons between the CLL and HV groups, as well as between the patient subgroups. The Spearman's rank correlation coefficient was used for correlation analysis. Statistica version 9.0 PL software (StatSoft, Cracow, Poland) and GraphPad Prism software version 5.0 (GraphPad Software, Inc., La Jolla, CA, USA) were used for statistical procedures. P<0.05 was considered to indicate a statistically significant difference.
Results
Intracellular IL-4 and IFN-γ expression in iNKT cells
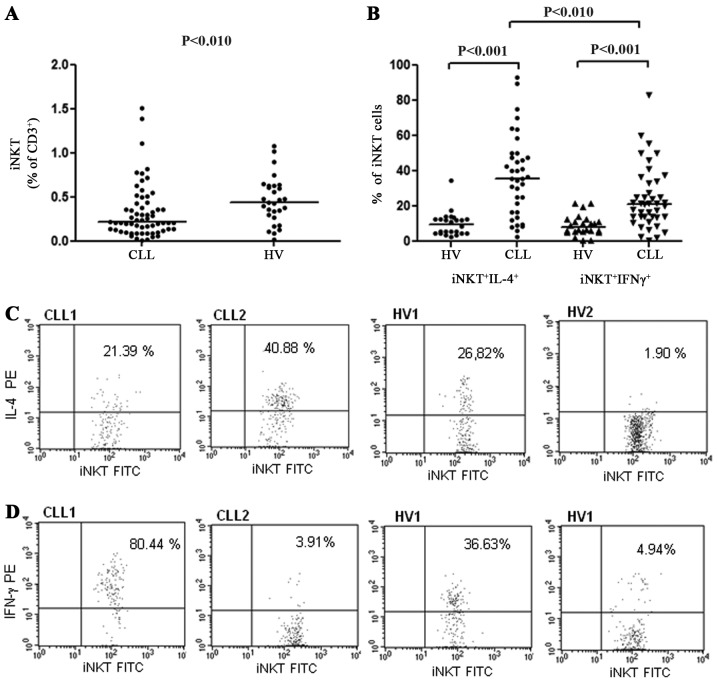
The percentage of iNKT cells within CD3+ T lymphocytes was significantly decreased in patients with CLL in comparison to the HVs (median, 0.21 vs. 0.42%, P<0.01; Fig. 3A). The frequency of iNKT cells also decreased with the disease stage. The median percentage of iNKT cells in stage 0 was 0.25, 0.21% in stages I/II and 0.13% in stages III/IV, according to the Rai classification. However, the difference was not significant. In the group of patients with CLL no significant association was identified between the frequency of iNKT cells in the PB and the expression of ZAP-70 or CD38 (data not presented).
Figure 3.
(A) Percentage of CLL iNKT cells (among CD3+ T lymphocytes) in patients with CLL and in HVs. (B) Percentage of CLL iNKT cells with IL-4 or IFN-γ expression in patients with CLL and in HVs. (C) Dot plots depict iNKT cells with high and low expression of IL-4 for two patients with CLL (CLL1, CLL2) and two HVs (HV1, HV2). (D) Dot plots depict iNKT cells with high and low expression of IFN-γ for two patients with CLL (CLL1, CLL2) and two HVs (HV1, HV2). CLL, chronic lymphocytic leukemia; iNKT, invariant natural killer T cells; IL, interleukin; IFN, interferon; HV, healthy volunteer.
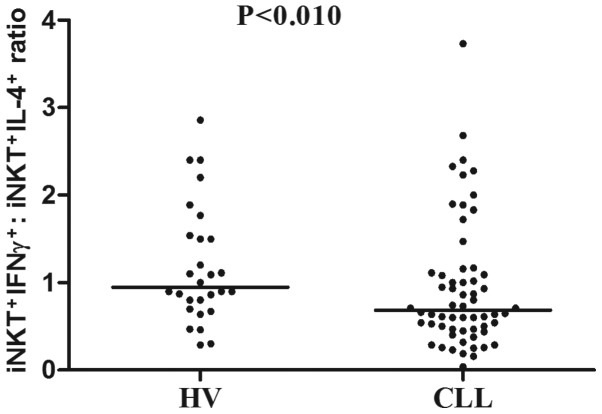
The function of iNKT lymphocytes was investigated through the analysis of intracellular cytokine expression following stimulation with the iNKT-specific ligand α-GalCer. At the end of a 24-h stimulation period, the synthesis of IL-4 and IFN-γ in iNKT cells was assessed by intracellular staining. In patients with CLL as well as in HVs, the percentage of iNKT cells with intracellular IL-4 or IFN-γ expression in non-activation assays was frequently <1%, comparable with the level of auto-fluorescence (Fig. 1G-H). In vitro stimulation of iNKT cells with α-GalCer resulted in CD69 upregulation, indicating the activation of iNKT cells (median of iNKT+CD69+ cells, 15.79% before and 29.32% after α-GalCer). Higher percentages of iNKT with IL-4 expression were noted in patients with CLL (median, 35.20%), as compared with in the HV control group (median, 12.64%; P<0.001, Fig. 3B). There was also a statistically significant difference between patients with CLL and HVs in terms of the percentage of iNKT cells with IFN-γ expression (median, 10.96% vs. 24.50%; P<0.001; Fig. 3B). Representative plots of data from two patients with CLL and two HVs with distinct IL-4 and IFN-γ expression profiles are presented in Fig. 3C-D. In patients with CLL, the percentage of iNKT+IL-4+ cells was significantly higher when compared with the percentage of iNKT+IFN-γ+ cells (P<0.01; Fig. 3B). Further analysis revealed that the ratio of iNKT+IFN-γ+ to iNKT+IL-4+ was significantly decreased in the CLL group compared with the HV group (median, 0.68 vs. 0.95; P<0.01; Fig. 4).
Figure 4.
iNKT+IFN-γ+: iNKT+IL-4+ ratio in HVs and in patients with CLL. CLL, chronic lymphocytic leukemia; iNKT, invariant natural killer T cells; IL, interleukin; IFN, interferon; HV, healthy volunteer.
The CLL group was further divided into three risk groups: Low risk (stage 0), intermediate-risk (stage I or II), and high-risk (stage III or IV). Each of these groups exhibited a significantly higher percentage of iNKT+IL-4+ cells in comparison with the HVs. However, there was no significant difference between the three risk groups (Fig. 5A). Furthermore, each risk group exhibited a significantly higher percentage of iNKT+IFN-γ+ cells in comparison with the control group (Fig. 5B). However, when the risk groups were compared, the only significant finding was that patients with CLL at Rai stage III–IV had a lower percentage of iNKT+IFN-γ+ (median, 19.65%) compared with those at Rai stage 0 (median, 33.0%; P<0.05; Fig. 5B). Additional analysis indicated that the ratio of iNKT+IFN-γ+ to iNKT+IL-4+ decreased during disease progression. The ratio was lower in patients at stages III–IV (median, 0.39) than at stages I–II (median, 0.66) or 0 (median, 0.86; Fig. 5C). Nevertheless, the difference was statistically significant only between the low and high-risk groups (P<0.05). Only the iNKT+IFN-γ+: iNKT+IL-4+ ratio of the intermediate-risk and high-risk groups was significantly lower in comparison with the HVs (Fig. 5C).
Figure 5.
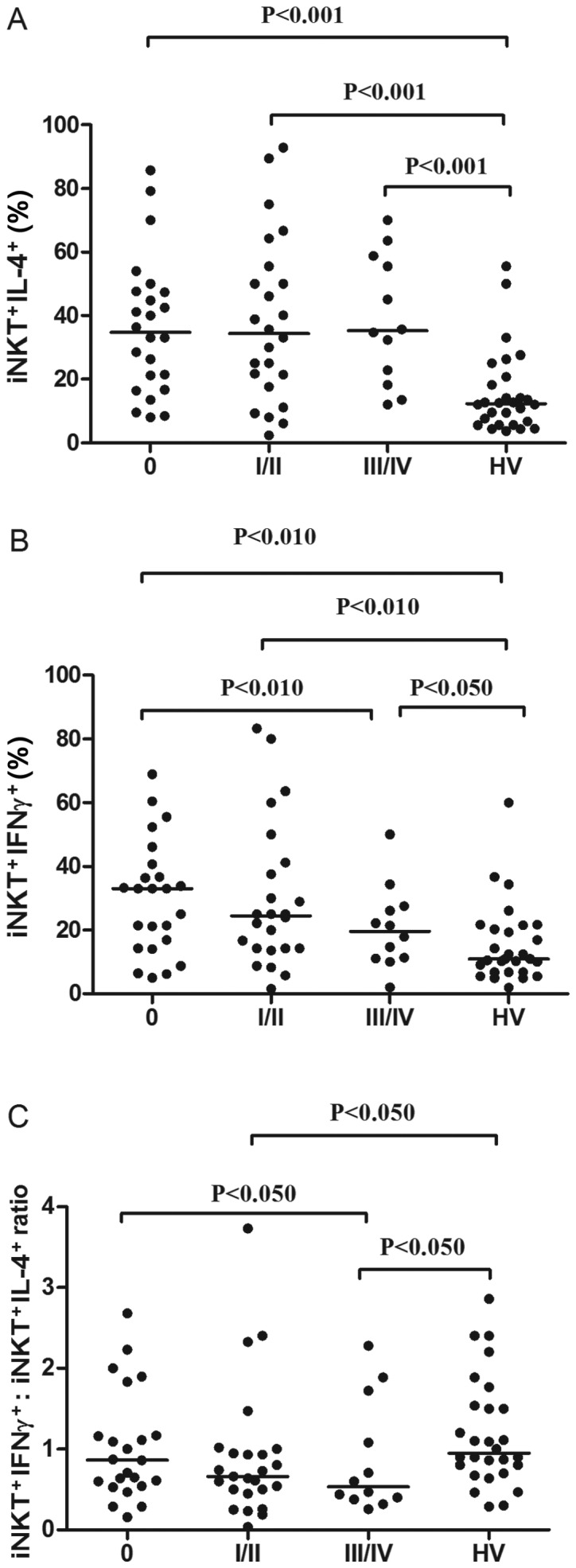
Percentage of CLL iNKT cells with (A) IL-4 or (B) IFN-γ expression in patients with CLL at various disease stages (three risk groups), as compared with in HVs. (C) Inter-group comparisons of the iNKT+IFN-γ+: iNKT+IL-4+ ratio among different risk groups of patients with CLL, and HVs. CLL, chronic lymphocytic leukemia; iNKT, invariant natural killer T cells; IL, interleukin; IFN, interferon; HV, healthy volunteer.
The proportions of CLL group iNKT differed slightly in the intracellular expression of cytokines, depending on the ZAP-70 factor expression. The percentage of iNKT cells expressing IL-4 was increased in ZAP-70-positive patients, as compared with in ZAP-70-negative patients (Table II). Additionally, a tendency towards an increased percentage of iNKT cells expressing IL-4 in CD38-positive in comparison with CD38-negative patients was noted, but this difference was not statistically significant (Table II). There was no significant difference in the iNKT+IFN-γ+ percentage between the ZAP-70-positive and ZAP-70-negative or the CD38-positive and CD38-negative patients. However, there was a statistically significant difference in the iNKT+IFN-γ+: iNKT+IL-4+ ratio between ZAP-70-positive and ZAP-70-negative patients (Table II).
Table II.
Percentage of iNKT cells with expression of IL-4 or IFN-γ divided according to adverse prognostic factors.
| Variable | ZAP-70-positive patients | ZAP-70-negative patients | P-value |
|---|---|---|---|
| iNKT+IL-4+ (%) | 37.86 (8.00–92.86) | 30.19 (2.36–89.47) | 0.049a |
| iNKT+IFN-γ+ (%) | 22.23 (2.00–68.97) | 25.00 (0.60–83.33) | 0.495 |
| iNKT+IFN-γ+/iNKT+IL-4+ ratio | 0.60 (0.04–2.28) | 0.89 (0.16–3.73) | 0.046a |
| CD38-positive patients | CD38-negative patients | ||
| iNKT+IL-4+ (%) | 36.71 (8.00–92.86) | 33.85 (2.36–89.47) | 0.462 |
| iNKT+IFN-γ+ (%) | 21.43 (5.81–68.97) | 25.55 (0.60–83.33) | 0.382 |
| iNKT+IFN-γ+/iNKT+IL-4+ ratio | 0.57 (0.16–2.68) | 0.77 (0.04–3.73) | 0.176 |
| del(17p13.1) and/or del(11q22.3) | Without del(17p13.1), del(11q22.3) | ||
| iNKT+IL-4+ (%) | 32.13 (12.07–55.56) | 37.71 (2.36–92.86) | 0.548 |
| iNKT+IFN-γ+ (%) | 16.08 (10.53–60.62) | 24.00 (0.60–83.33) | 0.064 |
| iNKT+IFN-γ+/iNKT+IL-4+ ratio | 0.53 (0.32–2.29) | 0.71 (0.04–3.73) | 0.365 |
The P-value was calculated using the Mann-Whitney U test.
P<0.05 was considered to indicate a statistically significant difference.
A higher percentage of iNKT+IL-4+ cells and a lower percentage of iNKT+IFN-γ+ cells were observed in patients carrying unfavorable cytogenetic abnormalities (11q22.3 and/or 17p13.1 deletion), compared with in patients without these genetic changes (Table II). Similarly, patients with del (11q22.3) and/or del (17p13.1) exhibited a lower ratio of iNKT+IFN-γ+ to iNKT+IL-4+. However, these differences were not statistically significant (Table II).
The percentage of iNKT+IL-4+ cells correlated positively with the WBC count (R=0.387; P<0.05), PB lymphocyte count (R=0.358; P<0.05) and β2-microglobulin levels (R=0.474; P<0.01). There was also an inverse correlation between the iNKT+IFN-γ+: iNKT+IL-4+ ratio and the WBC count (R=−0.302; P<0.05) and β2-microglobulin levels (R=0.507; P<0.01). However, no significant association between the percentage of iNKT+IFN-γ+ cells and other disease parameters was identified.
In the present study, PB samples were obtained from untreated patients with CLL diagnosed between September 2014 and June 2016 (21 months of observations). During the follow-up period, the treatment was initiated in 12 patients (20%). For these patients, the median time to treatment (TTT) was 7 months (range, 0–12 months). TTT was defined as the interval from the date of diagnosis to the date of first treatment. There was no significant association between the percentage of iNKT+IL-4+ or iNKT+IFN-γ+ cells and the time to treatment. No statistically significant differences were identified in the percentage of iNKT+IL-4+ and iNKT+IFN-γ+ or the iNKT+IFN-γ+: iNKT+IL-4+ ratio between patients requiring therapy, as compared with patients without treatment, during the observation period (Table III).
Table III.
Percentage of iNKT cells with intracellular expression of IL-4 or IFN-γ in untreated and requiring therapy patients with CLL.
| NKT/IL-4% | NKT/IFN % | IFN:IL-4 | ||||
|---|---|---|---|---|---|---|
| Untreated patients | Requiring therapy | Untreated patients | Requiring therapy | Untreated patients | Requiring therapy | |
| Median | 34.36 | 35.20 | 24.50 | 23.61 | 0.71 | 0.53 |
| Minimum | 2.36 | 12.07 | 0.60 | 11.11 | 0.04 | 0.32 |
| Maximum | 92.86 | 58.82 | 83.33 | 60.00 | 3.73 | 2.40 |
Expression of IL-4 and IFN-γ mRNAs in iNKT cells
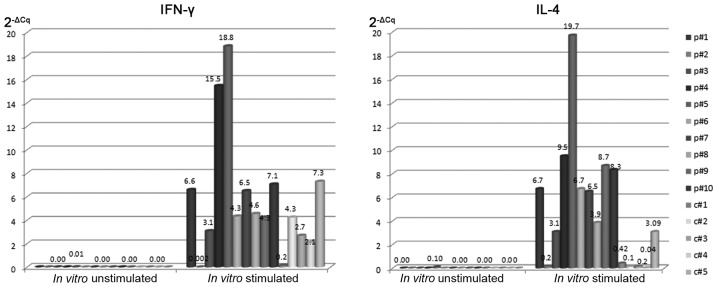
Purified iNKT cells were analyzed for IL-4 and IFN-γ mRNA expression using RT-qPCR. For the analysis of IL-4 and IFN-γ mRNA expression, each sample was normalized to β-actin. Generally, after 24 h of culture without stimulation, no IL-4 or IFN-γ mRNA was identified in the iNKT cells from patients with CLL or from the HVs. Only in one patient (p#5) was the presence of IL-4 and IFN-γ mRNA in an unstimulated culture observed (Fig. 6). iNKT cells from patients with CLL and HVs were identified to express IL-4 (median 2−ΔCq: 6.70 vs. 0.20) and IFN-γ (median 2−ΔCq: 5.50 vs. 2.70) mRNAs after α-GalCer stimulation (Fig. 6). After 24-h α-GalCer stimulation the presence of IL-4 and IFN-γ mRNAs was determined in iNKT cells isolated from patients with CLL as well as HVs. However, IL-4 or IFN-γ mRNAs were identified at higher levels in iNKT cells from patients with CLL compared with iNKT cells of HVs (P<0.05). In the present study, IL-4 mRNA levels directly correlated with the percentage of IL-4-positive iNKT cells (R=0.481; P<0.01). Similarly, IFN-γ mRNA levels directly correlated with the percentage of iNKT cells with intracellular IFN-γ expression (R=0.473; P<0.01).
Figure 6.
Quantitative expression of IL-4 and IFN-γ mRNA. RT-qPCR was performed on RNA samples isolated from iNKT cells obtained from patients with CLL (p#1 to p#10) or from iNKT cells obtained from HVs (c#1 to c#5). IL-4 and IFN-γ mRNA expression was analyzed in iNKT cells following a 24-h culture with or without α-GalCer stimulation. CLL, chronic lymphocytic leukemia; iNKT, invariant natural killer T cells; IL, interleukin; IFN, interferon; HV, healthy volunteer; α-GalCer, α-galactosylceramide; RT-qPCR, reverse transcription-quantitative polymerase chain reaction.
Membrane CD1d expression on B cells and monocytes from patients with CLL and HVs
Our previous data (25) indicated that the median percentage of CD1d-positive B cells in patients with CLL was significantly lower than in HVs. Similarly, when the level of membrane CD1d expression determined by MFI on B cells was compared between patients with CLL and HVs, we identified a significant difference between the groups. In the present study, our previous results (25) that the percentage of B cells CD1d+ in CLL patients was significantly lower than in HVs were confirmed. Furthermore, in the current study, CD1d expression was detected on monocytes. Fig. 2 presents two representative types of monocytes with CD1d expression for patients with CLL (CLL1-CLL2), and two representative types of CD1d-positive monocytes for HVs (HV1-HV2). The percentage of monocytes with CD1d expression was significantly lower in patients with CLL in comparison with the HVs (median, 85.73%; range, 65.78–99.15% vs. median, 92.86%; range, 88.55–99.89%; P<0.05). Similarly, the level of membrane CD1d expression determined by MFI on monocytes was reduced in patients with CLL (median 182.60 MFI in HVs; 161.40 MFI in the CLL group). However, this difference was not statistically significant. Furthermore, no significant association between the expression levels of IL-4 or IFN-γ in iNKT cells and CD1d expression on leukemic B lymphocytes or monocytes from patients with CLL was identified.
Apoptosis
The ex vivo percentage of apoptotic B lymphocytes (∆Ψmlow/CD19+) was significantly lower than the percentage of ∆Ψmlow/CD19+ lymphocytes in 24 h in vitro culture (P<0.05). However, there was no significant difference in the percentage of apoptotic CD19+ lymphocytes between the cultures with and without α-GalCer (Table IV). No correlation between the percentage of iNKT+IL-4+ or iNKT+IFN-γ+ cells and the percentage of ∆Ψmlow/CD19+ lymphocytes was noted. iNKT cells with various cytokine profiles did not affect B cell apoptosis. Additionally, no correlation was identified between the percentage of iNKT cells in PB from patients with CLL and the percentage of ∆Ψmlow/CD19+ lymphocytes determined directly ex vivo.
Table IV.
Ex vivo and in vitro (with and without α-GalCer stimulation) percentage of apoptotic CD19+ cells (∆Ψmlow/CD19+) evaluated by CMXRos.
| Conditions | ∆Ψmlow/CD19+ (%) Median (range) |
|---|---|
| ex vivo | 3.60 (0.40–26.70) |
| 24-h in vitro culture without stimulation | 19.20 (5.30–30.60) |
| 24-h in vitro culture with α-GalCer | 22.50 (7.60–28.70) |
Discussion
Deficiencies in cytokine production by the T-lymphocytes of patients with CLL have previously been noted in certain studies (29,30), but few concentrated on the small but essential T cell subpopulation of iNKT (31). iNKT cells recognize lipid antigens, such as αGalCer, when presented in a complex with CD1d (32). To evaluate the functionality of iNKT lymphocytes, they were cultured in vitro and stimulated with the iNKT-specific ligand α-GalCer. It is challenging to select suitable stimulation methods for the analysis of cytokine production, especially for rare cell populations (e.g., iNKT cells). In the present study, whole blood samples were stimulated in vitro. Analysis of cytokine synthesis in whole blood has been utilized in previous studies (33–35). Such a method may imitate the natural in vivo environment (34). It was identified that α-GalCer stimulation induced a stronger intracellular cytokine response in patients with CLL, when compared with HVs. Following culture with α-GalCer, iNKT cells exhibited upregulated expression of CD69, an early activation marker, indicating that the examined cells retained the ability to respond to stimulation. In patients with CLL, the percentage of iNKT+IFN-γ+ cells, and of iNKT+IL-4+, was increased with the noticeable dominance of a iNKT subset with intracellular expression of IL-4, while in HVs, the percentage of iNKT cells with IL-4 and IFN-γ expression was similar.
Changes in T cell cytokine secretion profile, associated with a Th2 shift, were described for advanced CLL cases (30). Hill et al (36) reported a reduction in IFN-γ and IL-4 expression by CD4+ T cells from patients with CLL. However, little data concerning cytokine production by iNKT cells have previously been presented. Weinkove et al (31) analyzed the cytokine profile and the proliferative capacity of circulating iNKT cells from patients with CLL. These authors observed an increased tendency towards an iNKT CD4+ subset (characterized by a production of Th2 cytokines) and a reduced tendency towards an iNKT CD8+ subset, although the results were not statistically significant. A comparison of patients with CLL and HVs revealed a lack of functional differences in, and no difference in the numbers of, iNKT cells; the cytokine production and in vitro proliferation of iNKT were similar. In the study, the authors evaluated a population of iNKT cells obtained from patients primarily in the early stages of the disease (31). It was suggested that the analysis of iNKT cells from patients with advanced-stage CLL could provide more diverse results. In the present study, no significant differences were observed in the percentage of iNKT+IL-4+ cells between the CLL risk groups. However, patients with CLL at Rai stage III–IV had a lower percentage of iNKT+IFN-γ+ cells than those at Rai stage 0. Concordant with our results, Tahir et al (21) identified a strong Th2 bias; α-GalCer-stimulated iNKT cells from patients with prostate cancer predominantly produced IL-4, while the production of IFN-γ was decreased. It must be emphasized that, in the present study, the iNKT+IFN-γ+: iNKT+IL-4+ ratio was decreased in the CLL group as compared with in the HVs. An inverse correlation was identified between the iNKT+IFN-γ+: iNKT+IL-4+ ratio and the WBC count, as well as the β2-microglobulin levels. Furthermore, the ratio was lower in advanced-stages compared with the early stages of the disease, and was lower in ZAP-70-positive patients. Similarly, a tendency towards the reduction in the ratio of iNKT+IFN-γ+ to iNKT+IL-4+ was observed in patients with CLL who also had del (11q22.3) and/or del (17p13.1). In a study of Dhodapkar et al (37), the loss of IFN-γ production by freshly isolated iNKT cells in the course of progressive myeloma was observed. An increase in IL-4 production, in comparison to IFN-γ expression, by iNKT cells was identified in mice following immunization with α-GalCer (38,39). Tahir et al (21) reported decreased IFN-γ:IL-4 ratio in prostate cancer patients. IL-4 inhibits the programmed death of CLL B cells and prolongs the cell lifespan (40). This effect was not detected for the B cells obtained from healthy subjects (4). Smyth et al (41) suggested that IL-4 is not required for mediating α-GalCer activity against cancer. The results suggest that the frequency of iNKT cells and the profile of cytokines expressed by iNKT cells does not affect B cell apoptosis in patients with CLL. The results obtained by Palmer et al (42) indicate that iNKT cells are dispensable in the development or accumulation of CD5+ B cells in mice prone to benign or leukemic CLL-like B cell expansion.
According to the literature, numerous studies have noted not only qualitative, but also quantitative changes concerning iNKT cells in the course of neoplastic diseases (21,43–47). The number of analyzed iNKT cells decreased in patients with solid tumors (21,43,47) and hematological malignancies, in comparison with healthy subjects (45,46,48). Fais et al (49) observed a significantly lower number of iNKT cells in patients with CLL compared with HVs. The results of the present study, and of our previous study (46), indicated a significantly lower percentage of iNKT cells in the PB of patients with CLL when compared with that of HVs. Certain prior studies have associated a reduced number of iNKT cells not with a tumor, but with a risk of tumor growth (43,50). Conversely, Weinkove et al (31) suggested that the absolute number of circulating iNKT cells in patients with untreated CLL is normal, and the reduction occurred in a group of patients undergoing chemotherapy. The data obtained in the current study are concordant with those recently reported by Weinkove et al (31), who determined there was no significant association between the iNKT cell frequency and the clinical disease stage or expression of adverse prognostic markers (i.e., ZAP-70).
In the present study, flow cytometry and RT-qPCR were used to detect the levels of IL-4 and IFN-γ mRNA in iNKT cells. The level of transcription for IL-4 and IFN-γ was higher in leukemic B cells compared with HVs. Similarly, the percentage of iNKT cells expressing these molecules was higher in patients with CLL. However, the methods used in the present study were not able to indicate whether iNKT cells with IL-4 and IFN-γ expression could also secrete IL-4 and IFN-γ. Nevertheless, the pattern of IL-4 and IFN-γ expression in the cytoplasm of iNKT cells together with the expression of IL-4 and IFN-γ mRNA may suggest that iNKT cells are able to produce these cytokines. Further study is required in order to determine whether a change in the pattern of released cytokines may have an important role in the pathogenesis of CLL. It must be noted that no significant association was identified between the percentage of iNKT cells with intracellular IL-4 or IFN-γ expression and the TTT. Furthermore, no statistically significant difference was observed in the iNKT+IFN-γ+: iNKT+IL-4+ ratio between the patients requiring therapy and the patients without treatment.
CD1d expression is crucial for the presentation of glycolipids to iNKT cells (31). It was previously demonstrated that there is lower CD1d molecule expression in the B cells of patients with CLL, as compared with HVs (25). Similarly, Weinkove et al (31) identified that leukemic B cells express CD1d at lower levels. The results of the current study are consistent with those of Weinkove et al (31), who reported reduced CD1d expression on the monocytes of patients with CLL. Nevertheless, the role of CD1d in antitumor immunity is not well understood. It has been reported that iNKT cells fail to develop in CD1d−/− mice (51). Wang et al (52) identified that resting iNKT cells that had not been exposed to APC with CD1d expression did not contain detectable levels of IFN-γ mRNA. Fais et al (49) reported that CD1d on leukemic B cells was able to present α-GalCer to NKT cells, as revealed by cytokine production, cytotoxicity and proliferation assays. In the present study, no association between the expression levels of IL-4 or IFN-γ in iNKT cells and CD1d molecule expression on leukemic B lymphocytes or monocytes of patients with CLL was identified.
Numerous issues concerning the development and progression of CLL are still unclear. Over the years, numerous abnormalities concerning leukemic B lymphocytes and non-leukemic cells of the immune system that occur during the course of CLL have been characterized (53). The functional dysfunction of NKT-like cells in terms of cytokine production have previously been demonstrated (54). However, there are currently few publications concerning the cytokine expression profiles of iNKT cells obtained from patients with CLL (31,49). By producing a variety of cytokines, the iNKT lymphocytes modify the microenvironment and, therefore, may influence tumor growth (21,55,56). As an important regulator of the Th1/Th2 balance (21,56), iNKT cells may have a significant role in the pathogenesis of CLL. An attempt was made to evaluate the ratio of iNKT+IFN-γ+: iNKT+IL4+ in patients with CLL. It was expected that its decrease may result in the promotion of leukemic B lymphocyte survival. However, in the present study iNKT cells with multiple cytokines profiles did not affect B cell apoptosis. Although iNKT cells are considered to enhance the antitumor response (57,58) in certain tumors, such as CLL, the cells may gain specific immunosuppressive properties (25,54). However, further studies are required. In the present study, CD4+CD25+Foxp3+ regulatory T cells (Tregs) were not analyzed. Nevertheless, an inverse correlation was identified between the percentages of iNKT cells and CD4+CD25high T cells (data not presented). Tregs can suppress the proliferation, cytokine secretion and cytotoxic activity of NKT cells (59). Monitoring the number and function of iNKT cells may be important for assessing immunological dysfunction in patients with CLL. However, currently it cannot unequivocally be said that monitoring the percentage of iNKT cells or their function can provide useful information concerning the activity or progression of the disease. In the present study, only two cytokines were analyzed. They were chosen since they represent cytokines typical for Th1- and Th2-type lymphocytes with a well-known antagonizing action. Further analysis of other cytokines produced by iNKT cells, including IL-17 and TGF-β, may be important for understanding the pathogenesis of CLL.
Acknowledgements
The present study was supported in part by a research grant (grant no. N N402 439139) from the State Funds for Scientific Research National Science Centre (NCN) and by a grant from the Medical University of Lublin (grant no. DS 458).
References
- 1.Joyce JA. Therapeutic targeting of the tumor microenvironment. Cancer Cell. 2005;7:513–520. doi: 10.1016/j.ccr.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 2.Burger JA, Gribben JG. The microenvironment in chronic lymphocytic leukemia (CLL) and other B cell malignancies: Insight into disease biology and new targeted therapies. Semin Cancer Biol. 2014;24:71–81. doi: 10.1016/j.semcancer.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 3.Tinhofer I, Rubenzer G, Holler C, Hofstaetter E, Stoecher M, Egle A, Steurer M, Greil R. Expression levels of CD38 in T cells predict course of disease in male patients with B-chronic lymphocytic leukemia. Blood. 2006;108:2950–2956. doi: 10.1182/blood-2006-03-010553. [DOI] [PubMed] [Google Scholar]
- 4.Mainou-Fowler T, Prentice AG. Modulation of apoptosis with cytokines in B-cell chronic lymphocytic leukaemia. Leuk Lymphoma. 1996;21:369–377. doi: 10.3109/10428199609093434. [DOI] [PubMed] [Google Scholar]
- 5.Terabe M, Swann J, Ambrosino E, Sinha P, Takaku S, Hayakawa Y, Godfrey DI, Ostrand-Rosenberg S, Smyth MJ, Berzofsky JA. A nonclassical non-Valpha14Jalpha18 CD1d-restricted (type II) NKT cell is sufficient for down-regulation of tumor immunosurveillance. J Exp Med. 2005;202:1627–1633. doi: 10.1084/jem.20051381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gapin L. Development of invariant natural killer T cells. Curr Opin Immunol. 2016;39:68–74. doi: 10.1016/j.coi.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dellabona P, Abrignani S, Casorati G. iNKT-cell help to B cells: A cooperative job between innate and adaptive immune responses. Eur J Immunol. 2014;44:2230–2237. doi: 10.1002/eji.201344399. [DOI] [PubMed] [Google Scholar]
- 8.Exley M, Porcelli S, Furman M, Garcia J, Balk S. CD161 (NKR-P1A) costimulation of CD1d-dependent activation of human T cells expressing invariant V alpha 24 J alpha Q T cell receptor alpha chains. J Exp Med. 1998;188:867–876. doi: 10.1084/jem.188.5.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seino K, Taniguchi M. Functionally distinct NKT cell subsets and subtypes. J Exp Med. 2005;202:1623–1626. doi: 10.1084/jem.20051600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Godfrey DI, MacDonald HR, Kronenberg M, Smyth MJ, Van Kaer L. NKT cells: What's in a name? Nat Rev Immunol. 2004;4:231–237. doi: 10.1038/nri1309. [DOI] [PubMed] [Google Scholar]
- 11.Kawano T, Cui J, Koezuka Y, Toura I, Kaneko Y, Motoki K, Ueno H, Nakagawa R, Sato H, Kondo E, et al. CD1d-restricted and TCR-mediated activation of valpha14 NKT cells by glycosylceramides. Science. 1997;278:1626–1629. doi: 10.1126/science.278.5343.1626. [DOI] [PubMed] [Google Scholar]
- 12.Spada FM, Koezuka Y, Porcelli SA. CD1d-restricted recognition of synthetic glycolipid antigens by human natural killer T cells. J Exp Med. 1998;188:1529–1534. doi: 10.1084/jem.188.8.1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hayakawa Y, Godfrey DI, Smyth MJ. Alpha-galactosylceramide: Potential immunomodulatory activity and future application. Curr Med Chem. 2004;11:241–252. doi: 10.2174/0929867043456115. [DOI] [PubMed] [Google Scholar]
- 14.Matsuda JL, Naidenko OV, Gapin L, Nakayama T, Taniguchi M, Wang CR, Koezuka Y, Kronenberg M. Tracking the response of natural killer T cells to a glycolipid antigen using CD1d tetramers. J Exp Med. 2000;192:741–754. doi: 10.1084/jem.192.5.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matsuda JL, Mallevaey T, Scott-Browne J, Gapin L. CD1d-restricted iNKT cells, the ‘Swiss-Army knife’ of the immune system. Curr Opin Immunol. 2008;20:358–368. doi: 10.1016/j.coi.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gumperz JE, Miyake S, Yamamura T, Brenner MB. Functionally distinct subsets of CD1d-restricted natural killer T cells revealed by CD1d tetramer staining. J Exp Med. 2002;195:625–636. doi: 10.1084/jem.20011786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brennan PJ, Brigl M, Brenner MB. Invariant natural killer T cells: An innate activation scheme linked to diverse effector functions. Nat Rev Immunol. 2013;13:101–117. doi: 10.1038/nri3369. [DOI] [PubMed] [Google Scholar]
- 18.Godfrey DI, Kronenberg M. Going both ways: Immune regulation via CD1d-dependent NKT cells. J Clin Inves. 2004;114:1379–1388. doi: 10.1172/JCI200423594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fujii S, Shimizu K, Smith C, Bonifaz L, Steinman RM. Activation of natural killer T cells by alpha-galactosylceramide rapidly induces the full maturation of dendritic cells in vivo and thereby acts as an adjuvant for combined CD4 and CD8 T cell immunity to a coadministered protein. J Exp Med. 2003;198:267–279. doi: 10.1084/jem.20030324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smyth MJ, Godfrey DI. NKT cells and tumor immunity-a double-edged sword. Nat Immunol. 2000;1:459–460. doi: 10.1038/82698. [DOI] [PubMed] [Google Scholar]
- 21.Tahir SM, Cheng O, Shaulov A, Koezuka Y, Bubley GJ, Wilson SB, Balk SP, Exley MA. Loss of IFN-gamma production by invariant NK T cells in advanced cancer. J Immunol. 2001;167:4046–4050. doi: 10.4049/jimmunol.167.7.4046. [DOI] [PubMed] [Google Scholar]
- 22.Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Döhner H, Hillmen P, Keating MJ, Montserrat E, Rai KR, et al. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: A report from the international workshop on chronic lymphocytic leukemia updating the national cancer institute-working group 1996 guidelines. Blood. 2008;111:5446–5456. doi: 10.1182/blood-2007-06-093906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rai KR, Sawitsky A, Cronkite EP, Chanana AD, Levy RN, Pasternack BS. Clinical staging of chronic lymphocytic leukemia. Blood. 1975;46:219–234. doi: 10.1182/blood-2016-08-737650. [DOI] [PubMed] [Google Scholar]
- 24.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 25.Bojarska-Junak A, Hus I, Chocholska S, Tomczak W, Woś J, Czubak P, Putowski L, Roliński J. CD1d expression is higher in chronic lymphocytic leukemia patients with unfavorable prognosis. Leuk Res. 2014;38:435–442. doi: 10.1016/j.leukres.2013.12.015. [DOI] [PubMed] [Google Scholar]
- 26.Bojarska-Junak A, Hus I, Chocholska S, Wasik-Szczepanek E, Sieklucka M, Dmoszyńska A, Roliński J. BAFF and APRIL expression in B-cell chronic lymphocytic leukemia: Correlation with biological and clinical features. Leuk Res. 2009;33:1319–1327. doi: 10.1016/j.leukres.2009.03.030. [DOI] [PubMed] [Google Scholar]
- 27.Sieklucka M, Pozarowski P, Bojarska-Junak A, Hus I, Dmoszynska A, Rolinski J. Apoptosis in B-CLL: The relationship between higher ex vivo spontaneous apoptosis before treatment in III–IV Rai stage patients and poor outcome. Oncol Rep. 2008;19:1611–1620. [PubMed] [Google Scholar]
- 28.Bojarska-Junak A, Hus I, Olszewska-Bożek K, Chocholska S, Wąsik-Szczepanek E, Tomczak W, Miłczak J, Dmoszyńska A, Roliński J. Analysis of ex vivo apoptosis of B and T cells from peripheral blood and bone marrow of patients with chronic lymphocytic leukemia. Acta Haematol Pol. 2012;43:336–341. doi: 10.1016/S0001-5814(12)70005-1. [DOI] [Google Scholar]
- 29.Christopoulos P, Pfeifer D, Bartholomé K, Follo M, Timmer J, Fisch P, Veelken H. Definition and characterization of the systemic T-cell dysregulation in untreated indolent B-cell lymphoma and very early CLL. Blood. 2011;117:3836–3846. doi: 10.1182/blood-2010-07-299321. [DOI] [PubMed] [Google Scholar]
- 30.Rossmann ED, Lewin N, Jeddi-Tehrani M, Osterborg A, Mellstedt H. Intracellular T cell cytokines in patients with B cell chronic lymphocytic leukaemia (B-CLL) Eur J Haematol. 2002;68:299–306. doi: 10.1034/j.1600-0609.2002.01612.x. [DOI] [PubMed] [Google Scholar]
- 31.Weinkove R, Brooks CR, Carter JM, Hermans IF, Ronchese F. Functional invariant natural killer T-cell and CD1d axis in chronic lymphocytic leukemia: Implications for immunotherapy. Haematologica. 2013;98:376–384. doi: 10.3324/haematol.2012.072835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Borg NA, Wun KS, Kjer-Nielsen L, Wilce MC, Pellicci DG, Koh R, Besra GS, Bharadwaj M, Godfrey DI, McCluskey J, Rossjohn J. CD1d-lipid-antigen recognition by the semi-invariant NKT T-cell receptor. Nature. 2007;448:44–49. doi: 10.1038/nature05907. [DOI] [PubMed] [Google Scholar]
- 33.Fernandez CS, Cameron G, Godfrey DI, Kent SJ. Ex-vivo α-galactosylceramide activation of NKT cells in humans and macaques. J Immunol Methods. 2012;382:150–159. doi: 10.1016/j.jim.2012.05.019. [DOI] [PubMed] [Google Scholar]
- 34.Ai W, Li H, Song N, Li L, Chen H. Optimal method to stimulate cytokine production and its use in immunotoxicity assessment. Int J Environ Res Public Health. 2013;10:3834–3842. doi: 10.3390/ijerph10093834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu Z, Yuan X, Luo Y, He Y, Jiang Y, Chen ZK, Sun E. Evaluating the effects of immunosuppressants on human immunity using cytokine profiles of whole blood. Cytokine. 2009;45:141–147. doi: 10.1016/j.cyto.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 36.Hill SJ, Peters SH, Ayliffe MJ, Merceica J, Bansal AS. Reduced IL-4 and interferon-gamma (IFN-gamma) expression by CD4 T cells in patients with chronic lymphocytic leukaemia. Clin Exp Immunol. 1999;117:8–117. doi: 10.1046/j.1365-2249.1999.00944.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dhodapkar MV, Geller MD, Chang DH, Shimizu K, Fujii S, Dhodapkar KM, Krasovsky J. A reversible defect in natural killer T cell function characterizes the progression of premalignant to malignantmultiple myeloma. J Exp Med. 2003;197:1667–1676. doi: 10.1084/jem.20021650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Singh N, Hong S, Scherer DC, Serizawa I, Burdin N, Kronenberg M, Koezuka Y, Van Kaer L. Cutting edge: Activation of NK T cells by CD1d and alpha-galactosylceramide directs conventional T cells to the acquisition of a Th2 phenotype. J Immunol. 1999;163:2373–2377. [PubMed] [Google Scholar]
- 39.Burdin N, Brossay L, Kronenberg M. Immunization with alpha-galactosylceramide polarizes CD1-reactive NK T cells towards Th2 cytokine synthesis. Eur J Immunol. 1999;29:2014–2025. doi: 10.1002/(SICI)1521-4141(199906)29:06<2014::AID-IMMU2014>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 40.Dancescu M, Rubio-Trujillo M, Biron G, Bron D, Delespesse G, Sarfati M. Interleukin 4 protects chronic lymphocytic leukemic B cells from death by apoptosis and upregulates Bcl-2 expression. J Exp Med. 1992;176:1319–1326. doi: 10.1084/jem.176.5.1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smyth MJ, Crowe NY, Pellicci DG, Kyparissoudis K, Kelly JM, Takeda K, Yagita H, Godfrey DI. Sequential production of interferon-gamma by NK1.1(+) T cells and natural killer cells is essential for the antimetastatic effect of alpha-galactosylceramide. Blood. 2002;99:1259–1266. doi: 10.1182/blood.V99.4.1259. [DOI] [PubMed] [Google Scholar]
- 42.Palmer VL, Nganga VK, Rothermund ME, Perry GA, Swanson PC. Cd1d regulates B cell development but not B cell accumulation and IL10 production in mice with pathologic CD5(+) B cell expansion. BMC Immunol. 2015;16:66. doi: 10.1186/s12865-015-0130-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Molling JW, Kölgen W, van der Vliet HJ, Boomsma MF, Kruizenga H, Smorenburg CH, Molenkamp BG, Langendijk JA, Leemans CR, von Blomberg BM, et al. Peripheral blood IFN-gamma-secreting Valpha24+Vbeta11+ NKT cell numbers are decreased in cancer patients independent of tumor type or tumor load. Int J Cancer. 2005;116:87–93. doi: 10.1002/ijc.20998. [DOI] [PubMed] [Google Scholar]
- 44.Giaccone G, Punt CJ, Ando Y, Ruijter R, Nishi N, Peters M, von Blomberg BM, Scheper RJ, van der Vliet HJ, van den Eertwegh AJ, et al. A phase I study of the natural killer T-cell ligand alpha-galactosylceramide (KRN7000) in patients with solid tumors. Clin Cancer Res. 2002;8:3702–3709. [PubMed] [Google Scholar]
- 45.Yoneda K, Morii T, Nieda M, Tsukaguchi N, Amano I, Tanaka H, Yagi H, Narita N, Kimura H. The peripheral blood Valpha24+ NKT cell numbers decrease in patients with haematopoietic malignancy. Leuk Res. 2005;29:147–152. doi: 10.1016/j.leukres.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 46.Hus I, Bojarska-Junak A, Gonet-Sebastianka J, Glazer M, Drab E, Woś J, Roliński J. iNKT cell percentage is decreased in patients with chronic lymphocytic leukemia and correlates inversely with the clinical stage and negative prognostic factors. Centr Eur J Immunol. 2011;36:79–84. [Google Scholar]
- 47.Singh AK, Shukla NK, Das SN. Altered invariant natural killer T cell subsets and its functions in patients with oral squamous cell carcinoma. Scand J Immunol. 2013;78:468–477. doi: 10.1111/sji.12104. [DOI] [PubMed] [Google Scholar]
- 48.Fujii S, Shimizu K, Klimek V, Geller MD, Nimer SD, Dhodapkar MV. Severe and selective deficiency of interferon-gamma-producing invariant natural killer T cells in patients with myelodysplastic syndromes. Br J Haematol. 2003;122:617–622. doi: 10.1046/j.1365-2141.2003.04465.x. [DOI] [PubMed] [Google Scholar]
- 49.Fais F, Morabito F, Stelitano C, Callea V, Zanardi S, Scudeletti M, Varese P, Ciccone E, Grossi CE. CD1d is expressed on B-chronic lymphocytic leukemia cells and mediates alpha-galactosylceramide presentation to natural killer T lymphocytes. Int J Cancer. 2004;109:402–411. doi: 10.1002/ijc.11723. [DOI] [PubMed] [Google Scholar]
- 50.Fujii S, Shimizu K, Okamoto Y, Kunii N, Nakayama T, Motohashi S, Taniguchi M. NKT cells as an ideal anti-tumor immunotherapeutic. Front Immunol. 2013;4:409. doi: 10.3389/fimmu.2013.00409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mendiratta SK, Martin WD, Hong S, Boesteanu A, Joyce S, Van Kaer L. CD1d1 mutant mice are deficient in natural T cells that promptly produce IL-4. Immunity. 1997;6:469–477. doi: 10.1016/S1074-7613(00)80290-3. [DOI] [PubMed] [Google Scholar]
- 52.Wang X, Bishop KA, Hegde S, Rodenkirch LA, Pike JW, Gumperz JE. Human invariant natural killer T cells acquire transient innate responsiveness via histone H4 acetylation induced by weak TCR stimulation. J Exp Med. 2012;209:987–1000. doi: 10.1084/jem.20111024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lanasa MC. Novel insights into the biology of CLL. Hematology Am Soc Hematol Educ Program. 2010;2010:70–76. doi: 10.1182/asheducation-2010.1.70. [DOI] [PubMed] [Google Scholar]
- 54.Bojarska-Junak A, Hus I, Sieklucka M, Wasik-Szczepanek E, Mazurkiewicz T, Polak P, Dmoszynska A, Rolinski J. Natural killer-like T CD3+/CD16+CD56+ cells in chronic lymphocytic leukemia: Intracellular cytokine expression and relationship with clinical outcome. Oncol Rep. 2010;24:803–810. doi: 10.3892/or_00000924. [DOI] [PubMed] [Google Scholar]
- 55.Robertson FC, Berzofsky JA, Terabe M. NKT cell networks in the regulation of tumor immunity. Front Immunol. 2014;5:543. doi: 10.3389/fimmu.2014.00543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang Y, Hu X, Guo C, Zhang Q, Peng J, Zhang J, Li L, Zhang T, Xu C. Polarization of natural killer T cells towards an NKT2 subpopulation occurs after stimulation with alpha-galactosylceramide and rhG-CSF in aplastic anemia. Acta Haematol. 2008;119:178–186. doi: 10.1159/000137501. [DOI] [PubMed] [Google Scholar]
- 57.Mattarollo SR, Smyth MJ. NKT cell adjuvants in therapeutic vaccines against hematological cancers. Oncoimmunology. 2013;2:e22615. doi: 10.4161/onci.22615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McEwen-Smith RM, Salio M, Cerundolo V. The regulatory role of invariant NKT cells in tumor immunity. Cancer Immunol Res. 2015;3:425–435. doi: 10.1158/2326-6066.CIR-15-0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.La Cava A, Van Kaer L, Fu-Dong-Shi CD4+CD25+ Tregs and NKT cells: Regulators regulating regulators. Trends Immunol. 2006;27:322–327. doi: 10.1016/j.it.2006.05.003. [DOI] [PubMed] [Google Scholar]