Abstract
Introduction
Blacks, Hispanics, and women of lower socioeconomic status tend to have a higher risk of obesity. Numerous studies over the past decade examined the role of the neighborhood food environment in body weight. However, few were longitudinal.
Purpose
This study examined whether multiple measures of neighborhood food availability were associated with body mass index (BMI) over time in a predominately black and Hispanic adult sample living in low to moderate income urban neighborhoods.
Methods
This longitudinal study utilized two waves of data (2002 (2008), including interviewer-measured height and weight, from a community survey of adults (n=219). In both 2002 and 2008, multiple measures characterized neighborhood food availability: GIS-derived availability of retail food outlets (large grocery store, small grocery store, convenience store, liquor stores), observed fruit and vegetable availability (count of stores selling 10 or more fresh fruit or vegetable varieties), and perceived fruit and vegetable access. Random intercept models estimated multivariable associations, controlling for individual-level demographics and neighborhood median household income.
Results
Small grocery store availability was associated with 1.22-unit increase in BMI (p=0.047), while each unit increase in perceived fruit and vegetable access was associated with a 0.69-unit decrease in BMI (p=0.055). BMI over time was not associated with large grocery store, convenience store, or liquor store availability, or with observed fruit and vegetable availability.
Conclusions
Findings suggest that improving the neighborhood food environment, particularly at small grocery stores, may help urban residents living in low to moderate income neighborhoods achieve healthier body weights over time.
Keywords: Fruit and vegetable, Food environment, Fast food, Supermarket, Grocery store, Convenience store
Introduction
Obesity is a public health threat that disproportionately affects many socially and economically disadvantaged groups (Berghofer et al., 2008; Flegal, Carroll, Kit, & Ogden, 2012; Hossain, Kawar, & El Nahas, 2007; Kelly, Yang, Chen, Reynolds, & He, 2008; Thorburn, 2005). The overall age-adjusted prevalence of obesity in the U.S. is 34.9% and is even higher among non-Hispanic black women (56.6%) and Hispanic women (44.4%) compared to non-Hispanic white women (32.8) (Ogden, Carroll, Kit, & Flegal, 2014). Non-Hispanic black men (37.1%) and Hispanic men (40.1%) also have somewhat higher age-adjusted prevalence of obesity than non-Hispanic white men (32.1%) (Ogden et al., 2014). Obesity is also inversely associated with socioeconomic status (SES) among women, although association strength can vary by race/ethnicity (Freedman & Centers for Disease Control and Prevention (CDC), 2011; Grabner, 2012; Ljungvall & Zimmerman, 2012). Obesity increases risk of a variety of adverse health conditions including cancer, type 2 diabetes, cardiovascular disease, osteoarthritis, and depression (Calle, Rodriguez, Walker-Thurmond, & Thun, 2003; Flegal, Graubard, Williamson, & Gail, 2007; Luppino et al., 2010; McTigue et al., 2012; Sowers & Karvonen-Gutierrez, 2010). Excess energy intake relative to energy expenditure contributes to weight gain and ultimately obesity (Kumanyika et al. 2008). Fruit and vegetable intake is among the dietary behaviors that may help adults prevent weight gain, although it is still unclear whether the effects are independent of reductions in energy intake (Ledoux, Hingle, & Baranowski, 2011; Mytton, Nnoaham, Eyles, Scarborough, & Mhurchu, 2014). The scope of the obesity problem calls for upstream approaches to promote healthier body weights. Social ecological models propose environmental factors, such as the food environment, as one upstream level of influence on or “risk regulator” of dietary behaviors and body weight (Glass & McAtee, 2006; Story, Kaphingst, Robinson-O’Brien, & Glanz, 2008).
Considerable research over the past decade examined the role of the neighborhood food environment in adult obesity; however, less than half measured height and weight objectively (Zenk, Thatcher, Reina, & Odoms-Young, 2014) and few studies were longitudinal (Auchincloss et al., 2013; Block, Christakis, O’Malley, & Subramanian, 2011; Boone-Heinonen et al., 2013; Gibson, 2011; Han, Powell, & Isgor, 2012; Li et al., 2009; Powell & Han, 2011). Some cross-sectional studies found that living in neighborhoods with more healthy food options or fewer retailers that predominately sell energy-dense, nutrient-poor foods was associated with lower body weight, while other studies found no association (Feng, Glass, Curriero, Stewart, & Schwartz, 2010; Fleischhacker, Evenson, Rodriguez, & Ammerman, 2011; Larson & Story, 2009; Lovasi, Hutson, Guerra, & Neckerman, 2009; Zenk, Thatcher, et al., 2014). Longitudinal studies based on objectively measured outcomes are needed to strengthen the evidence base. Like cross-sectional studies, extant longitudinal research produced mixed results and most commonly measured healthy and unhealthy food availability solely as the number, density, or proximity of retail food outlets based on secondary data (Block et al., 2011; Boone-Heinonen et al., 2013; Gibson, 2011; Han et al., 2012; Li et al., 2009; Powell & Han, 2011).
Retail food outlet type is a reasonable proxy for healthy food availability. Absolute and relative availability of healthier foods tend to be highest in supermarkets and large grocery stores and lowest in convenience stores and liquor stores (Farley et al., 2009; Glanz, Sallis, Saelens, & Frank, 2007; Liese, Weis, Pluto, Smith, & Lawson, 2007; Sharkey, Dean, & Nalty, 2012; Zenk, Powell, et al., 2014). Direct observation, nonetheless, arguably provides the most accurate estimate of healthy food availability, while perceived measures may capture other dimensions of food access such as food quality difficult to capture through other measures (Farley et al., 2009; Moore, Diez Roux, Nettleton, & Jacobs, 2008; Williams, Thornton, Ball, & Crawford, 2012; Zenk et al., 2009). However, neither type of measure is typically available in longitudinal studies. One longitudinal study measured neighborhood healthy food availability based on an aggregate of local informants’ perceptions and found a one standard deviation increase in the average score was associated with a 10% decrease in incident obesity during the 5-year follow-up period (Auchincloss et al., 2013). To our knowledge, no longitudinal study to date on the neighborhood food environment and body weight used directly observed neighborhood food availability.
The question of whether neighborhood food availability is associated with change in body weight (body mass index or BMI) over time remains a pressing one in the field. We addressed this question in a predominately black and Hispanic sample of urban adults living in low to moderate income neighborhoods who had their height and weight measured at two time points, 6 years apart. Our study captured the impact on BMI not only of change in neighborhood food availability between the two time points, but also of living in a neighborhood with stable food availability over time, such as a consistently “good” or “bad” food environment. Multiple measures were used to characterize neighborhood food availability. We hypothesized that availability of a large grocery store and better observed and perceived fruit and vegetable availability in the neighborhood are negatively associated with BMI over time, while neighborhood availability of a small grocery store, convenience store, and more liquor stores are positively associated with BMI over time.
Methods
Design and Sample
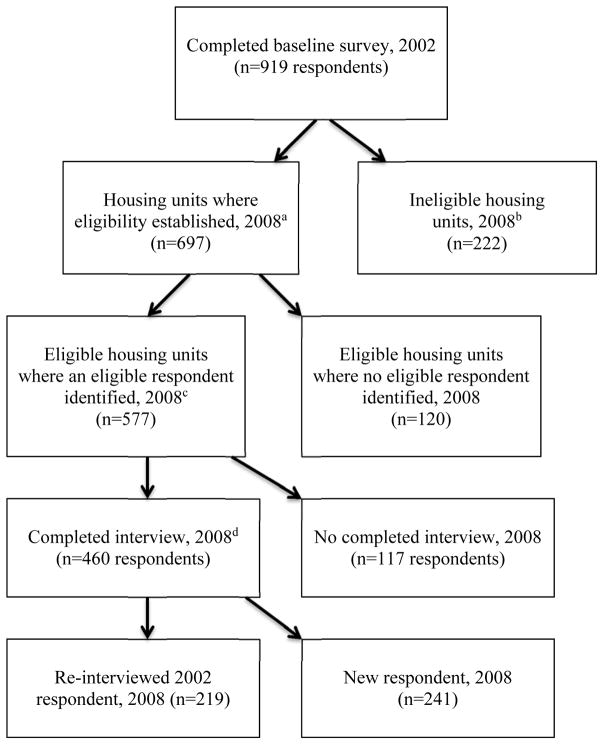
This was a longitudinal cohort study using two waves of data (2002 (2008) from a community survey of adults ages >25 years conducted by the Healthy Environments Partnership, a community-based participatory research partnership working together to understand and address cardiovascular disease risk in Detroit, Michigan (Schulz et al., 2005). The 2002 baseline survey involved a stratified two-stage equal probability sample of occupied housing units in three areas of Detroit: eastside, southwest, and northwest. It was designed to achieve similar distributions of socioeconomic status (SES) across the predominant racial/ethnic groups: blacks, Hispanics, and whites. Interviews were completed with 75% of households in which an eligible respondent was identified, with 919 completing the survey at baseline (Schulz et al., 2005). In 2008, interviews were conducted with current residents of those households. Interviews were completed at 80% of eligible households, 219 of which were re-interviews with respondents who had completed the 2002 survey and remained at the same address. Based on a multivariable regression approach to detecting selection bias (Cuddeback, Wilson, Orme, & Combs-Orme, 2004), we found no association between 2008 survey participation and age, education, or income. However, men were significantly less likely than women and non-Hispanic whites were significantly less likely than Hispanics to have been re-interviewed in 2008. The final sample for this analysis was 219 respondents for which data were available in 2002 and 2008. Respondent were nested in 102 census blocks, and those census blocks were, in turn, nested in 61 census block groups. (See the Figure for more information on the sample across survey waves.)
Figure.
Healthy Environments Partnership’s community survey sampling outcomes across two waves
aHousing unit eligibility criteria: Located in one of three areas of Detroit: east side, southwest, or northwest.
bHousing unit was ineligible if vacant or demolished.
cEligible respondent: Adult age 25 or older
dIf the original 2002 survey respondent was still living in the housing unit, re-interview was attempted. If original 2002 survey respondent was no longer living in housing unit and new eligible respondents were identified in the housing unit, a new respondent was randomly selected.
Measures
Body mass index
The dependent variable was BMI. A trained interviewer measured height to the nearest centimeter using a stadiometer and body weight using a calibrated digital scale. BMI was calculated using the standard formula of weight in kilograms divided by height in meters squared (kg/m2). For descriptive purposes, we categorized BMI as underweight (BMI <18.5), normal weight (BMI 18.5–24.9), overweight (BMI 25–29.9), obese, class I (BMI 30–34.9), obese, class II (BMI 34–39.9), and obese, class III (BMI >39.9).
Neighborhood food availability
In 2002 and 2008, we measured three aspects of neighborhood food availability: availability of four types of food stores, observed fruit and vegetable availability, and perceived fruit and vegetable access. The first two measures were derived based on direct observation of respondents’ neighborhoods (Izumi et al., 2012; Zenk, Schulz et al., 2012; Zenk et al., 2006). In each survey year, a list of food stores was obtained from the Michigan Department of Agriculture, ground-truthed using field observations, and audited for food availability by trained field staff. Respondents’ “neighborhoods” were defined as a 0.5-mile radial buffer around their census block centroid, a common metric in prior neighborhood food environment research (Charreire et al., 2010). Census block centroids are good representations for respondents’ homes in this sample due to the small size of census blocks (median=0.009 square miles) (Zenk et al., 2011).
Food stores were classified as liquor stores (categorized “liquor” store in the telephone directory; had “liquor” or “party” in name; or had “liquor,” “beer,” or “wine” as largest sign on storefront), specialty stores (e.g., meat market, produce market), convenience stores (food stores with limited capacity for customer check-out (i.e., food stores where cashiers encased in plexiglass with only turnstile for ringing up groceries but not a liquor or specialty store; not including gas stations), small grocery stores (food stores with less than three cash registers and not a liquor, specialty, or convenience store), and large grocery stores (food stores with at least three cash registers but not a liquor, specialty, or convenience store). For large grocery stores, small grocery stores, and convenience stores, availability was included in the analysis as a dichotomous indicator for presence of at least one store of that type in the neighborhood. Liquor store availability was included as a count due to the large number of these stores. Specialty stores were not included in the analysis as a separate store type because there were too few.
Observed fruit and vegetable availability was measured in 2002 and 2008 based on store audits as a count of the number of food stores in the neighborhood (0.5 mile radius from centroid of the census block) that carried at least 10 fresh fruits or vegetable varieties (Izumi et al., 2012; Zenk et al., 2012; Zenk et al., 2006), which we considered a “good” selection.
Perceived fruit and vegetable access was measured in 2002 and 2008 as an individual-level variable using a 3-item scale. Respondents rated their satisfaction from 1 (very satisfied) to 4 (not at all satisfied) with the variety, quality, and price or affordability of fresh fruits and vegetables in their neighborhood, defined as a 10–15 minute walk or 5-minute drive (roughly corresponding to 0.5 mile). Scores were reverse coded, and mean scores calculated, with higher scores corresponding with greater satisfaction (α=0.86 in 2002 and 0.82 in 2008).
Covariates
Time-varying covariates derived from the respondent surveys in 2002 and 2008 were age, annual per capita income (annual household income divided by the number of household members), employment status (in the workforce or not), auto ownership, home ownership, length of neighborhood residence, and a physical limitations scale that was the mean of responses to four items assessing the degree of difficulty with doing heavy work around the house (e.g., washing walls, shoveling snow), climbing flights of stairs, walking several blocks, or bathing (1=no difficulty at all, 5=can’t do it at all) (House et al., 1994). Neighborhood median household income was measured at the census block group level using data from the 2000 decennial census (for 2002) and the 2005–2009 American Community Survey (for 2008). Time-invariant covariates were self-reported race/ethnicity (non-Hispanic black or African American, Hispanic or Latino, non-Hispanic white, and non-Hispanic other), gender, and education [less than a high school diploma or general equivalency diploma (GED), high school diploma or GED, and more than a high school education].
Data Analysis
Multiple imputation using Imputation and Variance Estimation software (IVEware, Ann Arbor MI, 2002) was performed to account for missing data. Weighted four-level hierarchical linear models using PROC MIXED procedure (SAS 9.2, SAS Institute, Cary NC, 2008) were employed to estimate multivariable associations between neighborhood food availability and BMI over time. Specifically, we used random intercept models to regress BMI change on each category of time-varying neighborhood food availability variables (store type, observed fruit and vegetable availability, perceived fruit and vegetable access), year, and interaction terms between these food availability variables and year in a series of models rather than a single model, controlling for covariates. In these models, level 1 was time (observations within respondents); level 2 was respondents (including measures of individual gender and race/ethnicity); level 3 was neighborhoods or 0.5 mile buffers around census block centroid (including measures of observed food store availability and observed fruit and vegetable availability); and level 4 was census block groups (including median household income). Weights were applied to account for loss to follow up, adjust for probabilities of selection within race and SES strata, and match the sample to Census 2000 population distributions of the study communities.
We tested the sensitivity of the results to inclusion of additional neighborhood-level covariates that may confound associations between neighborhood food availability and BMI: fast food restaurant density (2008 only), street connectivity (i.e., mean number of streets connecting with each street; 2002 only), land use mix (i.e., mix of residential, industrial, and commercial land uses; 2002 only), and population density (i.e., population per square mile). With the exception of population density which was measured at the census block group level (level 4), the other variables were measured for respondents’ neighborhoods, or 0.5 mile buffers from census block centroids (level 3). We also conducted sensitivity analyses for a different version of the observed fruit and vegetable availability measure: number of stores with any (1 or more) fresh fruit or vegetable variety.
Results
Table 1 shows descriptive statistics of sample, neighborhood, and census block group characteristics at baseline. The mean BMI at baseline was 32.1 kg/m2 (SE=0.5), with 16.7% underweight or normal weight, 27.2% overweight and 56.2% obese (class I-III). This includes 16.3% with class III obesity.
Table 1.
Weighted baseline sample and neighborhood characteristics
| Variable | n | % | Mean (SE) | Minimum | Maximum |
|---|---|---|---|---|---|
|
| |||||
| Person Level (N=219) | |||||
| Body mass index (BMI), kg/m2 | 219 | 32.1 (0.5) | 17.4 | 63.1 | |
| Underweight: <18.5 | 3 | 1.3 | |||
| Normal weight: 18.5–24.9 | 34 | 15.4 | |||
| Overweight: 25.0–29.9 | 59 | 27.2 | |||
| Obese, Class I: 30.0–34.9 | 55 | 25.2 | |||
| Obese, Class II: 35.0–39.9 | 32 | 14.6 | |||
| Obese, Class III: ≥40.0 | 36 | 16.3 | |||
| Age in years | 219 | 49.5 (1.1) | 26.0 | 88.0 | |
| Gender, % Female | 110 | 50.3 | |||
| Race/Ethnicity, % | |||||
| White | 47 | 21.5 | |||
| Hispanic | 66 | 29.9 | |||
| Black | 100 | 45.7 | |||
| Other | 6 | 2.9 | |||
| Marital Status, % Married | 73 | 33.4 | |||
| Car Ownership, % Owner | 161 | 73.4 | |||
| Home Ownership, % Owner | 150 | 68.5 | |||
| Employment Status, % In Labor Force | 142 | 64.7 | |||
| Education, % | |||||
| Less than High School | 91 | 41.5 | |||
| High School | 52 | 23.8 | |||
| More than High School | 76 | 34.7 | |||
| Annual Household Income, Per Capita | 219 | 13,257.5a (1,140.9) | 1,000.0 | 162,499.0 | |
| Length of Neighborhood Residence, Years | 219 | 22.1 (17.2) | 0.2 | 65.0 | |
| Physical Health Limitations | 219 | 1.8 (0.1) | 1.0 | 5.0 | |
| Perceived Fruit and Vegetable Access | 219 | 2.8 (0.8) | 1.0 | 4.0 | |
|
| |||||
| % | Mean (SD) | Minimum | Maximum | ||
|
| |||||
| Neighborhood Level (N=102)b | |||||
| Large Grocery Store Availability, % Yes | 43 | 42.2 | 0.9 (1.7) | 0.0 | 8.0 |
| Small Grocery Store Availability, % Yes | 41 | 40.2 | 0.6 (1.3) | 0.0 | 5.0 |
| Convenience Store Availability, % Yes | 33 | 32.4 | 0.8 (1.6) | 0.0 | 8.0 |
| Liquor Store Availability, Numberc | 102 | 6.4 (3.2) | 0.0 | 14.0 | |
| Stores with 10+ Fresh Fruit or Vegetable Varieties,d Number | 63 | 61.8 | 1.1 (1.1) | 0.0 | 4.0 |
| Census Block Group Level (N=61) | |||||
| Median Household Income | 61 | 28,124.7e (11207.5) | 10583.0 | 83115.0 | |
Median for annual household income, per capita $7,499.5
Dichotomous variables were used in regression analysis for large grocery store, small grocery store, and convenience store availability. Continuous variables were used in regression analysis for liquor store availability and observed fruit and vegetable availability.
All but two neighborhoods had at least one liquor store; therefore, the prevalence of having at least one liquor store is not reported.
This is the measure of observed fruit and vegetable availability.
Median for census block group median household income $25,139
Table 2 presents multivariable regression results for associations between neighborhood food availability and BMI over time. Small grocery store availability was associated with a 1.22-unit (SE=0.59) increase in BMI over time (p=0.047), controlling for individual-level covariates, neighborhood median household income, and other store types (Model 1). There was no statistically significant association between observed fruit and vegetable availability and BMI over time, controlling for individual-level covariates and neighborhood median household income (Model 2). Each unit increase in perceived fruit and vegetable access was marginally significantly associated with a 0.69-unit reduction (SE=0.34) in BMI over time (p=0.055), controlling for individual-level covariates and neighborhood median household income (Model 3).
Table 2.
Longitudinal, multivariable associations between neighborhood food availability and BMI change over timea
| Independent Variables | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Est. (S.E.) | 95% C.I. | p-value | Est. (S.E.) | 95% C.I. | p-value | Est. (S.E.) | 95% C.I. | p-value | |
| Large Grocery Store Availability | 0.54 (0.62) | −0.68, 1.31 | 0.391 | ||||||
| Small Grocery Store Availability | 1.22 (0.59) | 0.06, 1.31 | 0.047 | ||||||
| Convenience Store Availability | −0.43 (0.55) | −1.51, 0.45 | 0.450 | ||||||
| Liquor Store Availability, Number | −0.07 (0.10) | −0.27, 0.91 | 0.502 | ||||||
| Stores with 10+ Fresh Fruit or Vegetable Varieties, Numberb | 0.35 (0.21) | −0.09, 0.79 | 0.113 | ||||||
| Perceived Fruit and Vegetable Access | −0.69 (0.34) | −1.36, −0.02 | 0.055 | ||||||
Est. = Regression estimate S.E. = Standard error C.I. = Confidence interval
All models include the following covariates: age, annual per capita income, employment status, auto ownership, home ownership, length of neighborhood residence, physical health limitations, race/ethnicity, gender, education, and neighborhood median household income.
This is the measure of observed fruit and vegetable availability.
Sensitivity analyses including other potential neighborhood-level confounders (fast food restaurant density, population density, street connectivity, land use mix) did not change the results appreciably (not shown). Therefore, we presented results from the more parsimonious models in order to maximize statistical power with our limited sample size. Sensitivity analyses for Model 2 that substituted a measure of the number of stores with any fresh fruit or vegetable variety were also consistent with those presented here (not shown).
Discussion
To our knowledge, this longitudinal cohort study was one of the first to examine multiple measures of neighborhood food availability in relation to BMI over time. Results suggest that improving some aspects of the neighborhood food environment may lead to healthier body weights among urban residents living in low to moderate income neighborhoods. Consistent with our expectations, small grocery store availability was positively associated with BMI over time, while perceptions of better neighborhood fruit and vegetable access was negatively associated with BMI over time. However, we found no associations of BMI over time with availability of large grocery stores, convenience stores, liquor stores, or number of stores with fresh fruits or vegetables.
Our finding that small grocery store availability was associated with higher BMI over time adds to inconsistent findings from longitudinal as well as cross-sectional research on grocery store availability and body weight (Block et al., 2011; Gibson, 2011; Powell & Han, 2011; Zenk, Thatcher, et al., 2014). The Framingham Heart Study Offspring Cohort Study found proximity to a grocery store (any size non-chain grocery store) was negatively associated with BMI over time, although the effect was small (Block et al., 2011). Data from the Panel Study of Income Dynamics showed mixed results for grocery stores (any size) in different subgroups, with a small negative association between grocery store density and BMI observed for poor men and small positive associations among some women (e.g., non-poor and those with no child) (Powell & Han, 2011). Only Gibson looked at small grocery stores specifically (Gibson, 2011). Using data from the NLSY79, she found a negative association between a 2-year change in neighborhood small grocery store density and BMI for respondents who moved from a rural to an urban area, although there was a positive cross-sectional association between small grocery store density and BMI among urban residents (Gibson, 2011).
Because they offer fewer healthier foods and beverages, small grocery or “corner” store availability may contribute to poorer diets, specifically higher energy intake, and thus higher body weights among local residents who shop there (Gibson, 2011). Research shows that small grocery or food stores generally have lower absolute and relative availability of healthy products than large grocery stores or supermarkets (Farley et al., 2009; Glanz, Sallis, Saelens, & Frank, 2007; Liese et al., 2007; Zenk, Powell, et al., 2014). For example, a study in Louisiana and Los Angeles found that the ratio of shelf space for healthier to less healthy products was 0.18 and 0.30, respectively, in small food stores compared to 0.55 and 0.72, respectively, in supermarkets (Farley et al., 2009). Because grocery stores are more heterogeneous in the healthfulness of food offerings than supermarkets, convenience stores, or other food stores (which may contribute to discrepancies in findings to date) (Zenk, Powell, et al., 2014), it is important that future studies distinguish between different sizes of grocery stores in order to better understand their role in body weight.
Despite that they also have a lower ratio of healthier alternatives to less healthy food products (Farley et al., 2009; Zenk, Powell, et al., 2014) and contrary to our hypothesis, we found no associations of BMI change over time with convenience or liquor store availability. One potential explanation is that people do not use these store types to obtain much of their groceries; therefore, their presence does not affect body weight (Gibson, 2011).
We unexpectedly found no evidence that BMI change over time was associated with large grocery store availability. Overall, longitudinal research on the association between large grocery store availability and BMI is mixed (Block et al., 2011; Boone-Heinonen et al., 2013; Gibson, 2011; Han et al., 2012). Some research suggests that the evidence for salubrious effects of large grocery stores is strongest for very large “supermarkets,” particularly chain supermarkets (Powell, Auld, Chaloupka, O’Malley, & Johnston, 2007). Detroit had very few chain full-service supermarkets in 2002 and 2008 and only one located in the study neighborhoods (Zenk et al., 2005). Thus, it is possible that the large grocery stores located in the study neighborhoods did not offer as large of a selection of healthy foods at low enough prices to help local residents achieve healthier weights over time.
Our finding that perceptions of better fruit and vegetable access in the neighborhood was negatively associated with BMI over time (p=0.055), while marginal, is consistent with the only other longitudinal study that we identified of perceived food availability and body weight (Auchincloss et al., 2013). Observed fruit and vegetable availability was not associated with BMI change. It is possible that perceptions more accurately reflect fruit and vegetable access than the observational data, for example, capturing quality and price, in addition to fruit and vegetable availability. The perceived fruit and vegetable access measure may also correlate better with the availability of other foods that are supportive of healthy weights such as whole grains and low-fat dairy. Still, we cannot rule out that perceived food availability reflects unmeasured personal factors (e.g., importance placed on nutrition or maintaining a healthy weight) that were correlated with weight change over time.
Implications for Future Research
With relatively little longitudinal research on the food environment and BMI, more research is needed in adults as well as children and in urban as well as rural areas. Research with children and rural populations need to consider the uniqueness of these populations including, for example, their independent interactions with the food environment as well as the influence of parents’ food environments and the relevant exposure area (e.g., 0.5-mile buffer may not be relevant or realistic in rural areas), respectively. Longitudinal research is important to identify the most promising arenas in which to focus policy and other environmental interventions. This includes longitudinal studies that: (1) move beyond retail food outlet type as a proxy to include observed measures of the food environment; (2) are based on larger and more socioeconomically diverse samples with more variability in the neighborhood food environment; (3) account for change over time in environmental features that may influence energy expenditure or otherwise confound food environment-BMI relationships over time; (4) incorporate food shopping and purchasing behaviors—such as those included in the USDA’s National Household Food Acquisition and Purchase Survey—as a mediator in food environment-BMI associations; and (5) assess other objectively measured health outcomes such as blood pressure (Zenk, Thatcher, et al., 2014). Quasi-experimental studies that evaluate naturally occurring changes in the neighborhood food environment, such as those supported by the Pennsylvania Fresh Food Financial Initiative and the federal Healthy Food Financing Initiative, are also a valuable direction for additional research (Cummins, Flint, & Matthews, 2014; Cummins, Petticrew, Higgins, Findlay, & Sparks, 2005; Elbel et al., 2015; Mayne, Auchincloss, & Michael, 2015; Wrigley, Warm, & Margetts, 2003).
Implications for Interventions
Although more longitudinal and quasi-experimental research is needed, our findings suggest that improving neighborhood food availability, as one upstream level of influence on weight outcomes according to social ecological models, may help urban residents living in low to moderate income neighborhoods achieve healthier body weights. While evidence outside the U.S. is more equivocal (Ball, Timperio, & Crawford, 2009; Beaulac, Kristjansson, & Cummins, 2009; Cummins & Macintyre, 2006; Winkler, Turrell, & Patterson, 2006), a number of U.S. studies have shown that black and low-income neighborhoods have fewer supermarkets and potentially more small grocery stores (or “corner stores” or “bodegas”) (Morland, Wing, Diez Roux, & Poole, 2002; Powell, Slater, Mirtcheva, Bao, & Chaloupka, 2006; Zenk et al., 2005). They may also have fewer healthy options, after accounting for store type (Baker, Schootman, Barnidge, & Kelly, 2006; Franco, Diez Roux, Glass, Caballero, & Brancati, 2008; Zenk, Powell, et al., 2014). Our results suggest the importance of working with small grocery stores to increase healthier food options and reduce less healthy offerings. This could be accomplished by providing small grocers with financial and other incentives to renovate their space and offer more healthy alternatives, an option available through the Healthy Food Financing Initiative and similar state initiatives (Centers for Disease Control and Prevention, n.d.; Fleischhacker, Flournoy, & Moore, 2013; Karpyn, Young, & Weiss, 2012). It may also be achieved through buying cooperatives that help small grocery stores obtain fresh fruits and vegetables and other healthy foods at lower prices. Revisions to the USDA Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) that strengthened minimum stocking requirements for healthy foods have also proved successful in increasing healthy food availability in small stores (Andreyeva, Luedicke, Middleton, Long, & Schwartz, 2012; Hillier et al., 2012; Schultz, Shanks, & Houghtaling, 2015; Zenk, Odoms-Young et al., 2012). Strengthening USDA Supplemental Nutrition Assistant Program (SNAP) minimum stocking requirements for healthy foods is another opportunity to improve healthy food availability in small stores (Kennelly, Neff, & Rutkow, 2013) because an even larger proportion of retail food outlets are SNAP retailers. In 2008 in our study’s communities, for example, 22% of stores were authorized WIC retailers while 77% were authorized SNAP retailers. The success of strategies to improve the neighborhood food environment is likely to be enhanced by policymakers, local residents, advocates, and when possible, the business community working in partnership (Karpyn et al., 2012; Ulmer, Rathert, & Rose, 2012). Evaluation data examining changes in diet and body weight among community members where these initiatives are unfolding will provide critical information to help assess their implications for health and well being of community residents (Chiasson et al., 2013; Schultz et al. 2015; Whaley, Ritchie, Spector, & Gomez, 2012).
Strengths and Limitations
In contrast to most longitudinal studies to date that relied solely on secondary data of retail food outlet locations (Zenk, Thatcher, et al., 2014), a notable strength of this study is the use of multiple time-varying measures of neighborhood food availability. This includes GIS-derived measures of retail food outlet availability and fruit and vegetable availability at stores derived from direct observation of respondents’ neighborhoods, as well as perceived fruit and vegetable access. Other study strengths include the racially/ethnically diverse sample and BMI assessed via interviewer-measured height and weight. Furthermore, although sometimes only with measures from one time point, we were also able to test whether the results were sensitive to controls for other aspects of the neighborhood environment that may confound the associations of interest.
Nonetheless, the study has limitations, including related to the sample. The sample was small, and a relatively small proportion of the original probability sample from 2002 was retained in 2008 for several reasons. First, because of our understanding factors that affect health in the study neighborhoods, we surveyed the originally sampled housing units in 2008, rather than following individuals who moved outside the focal neighborhoods. Second, the study period (2002–2008) occurred during a period of substantial population outmigration in the city of Detroit, with 25% of the city’s population leaving the city between the 2000 and 2010 decennial census (Wisely & Spangler, 2011). Our survey was conducted in low to moderate income neighborhoods, and there is evidence that low-income households move more frequently than higher income households (Coulton, Theodos, & Turner, 2012). Third, the study period overlapped with the beginning of the mortgage crisis, which disproportionately affected Detroit homeowners: 5% of Detroit households entered some stage of foreclosure in 2007 alone (Rooney, 2008). Still, those who participated in the 2008 survey differed from non-participants only on gender and race/ethnicity, but not age, education, or income. Related to the sample size, some of the estimates, including for small grocery store and perceived fruit and vegetable access, are rather imprecise, as evidenced by the wide confidence interval. Thus, the results should be interpreted carefully in the context of similar studies. The sample tended to have a higher BMI and had a higher prevalence of overweight and obesity than the U.S. population. Thus, while it represents an important population, it is possible that the results do not apply to the general population.
While this is the first longitudinal study to our knowledge to include both directly observed and perceived measures of healthy food availability, there are limitations associated with these measures, as well as the diet measure. Even though a number of studies show that healthy food availability tends to differ significantly by retail food outlet type, healthy food availability can differ across neighborhoods among outlets of the same type (Franco, Diez Roux, Glass, Caballero, & Brancati, 2008). Moreover, other aspects of the retail food environment may differ by retail food outlet type such as food quality, prices, and marketing. Thus, interpretation of the findings regarding small grocery stores is subject to alternative explanations beyond healthy food availability. Another limitation is the observed healthy food availability measure is restricted to fresh fruit and vegetables and does not capture availability of other types of healthy foods important for maintaining a healthier body weight. Finally, we were unable to directly test whether diet mediated associations between neighborhood food availability over time, due to non-comparable measures of diet in 2002 and 2008.
Conclusions
Despite these limitations, this study contributes to a still small number of longitudinal research examining associations between the neighborhood food environment and body weight. Prior research shows that low-income individuals, blacks, and to some extent Hispanics are disproportionately exposed to neighborhoods with poor availability of healthier foods like fruits and vegetables and more small food stores that predominately sell energy-dense, nutrient poor foods and few healthier alternatives. Our study suggests this may have adverse consequences for their body weight over time, and is consistent with recommendations that promoting better access to healthy foods may help residents of low to moderate income urban communities maintain a healthier weight.
Acknowledgments
The Detroit Healthy Environments Partnership (HEP) (www.hepdetroit.org) is a community-based participatory research project affiliated with the Detroit Community-Academic Urban Research Center (www.detroiturc.org). We thank the members of the HEP Steering Committee for their contributions to the work presented here, including representatives from Brightmoor Community Center, Detroit Department of Health and Wellness Promotion, Detroit Hispanic Development Corporation, Friends of Parkside, Henry Ford Health System, Warren Conner Development Coalition/Detroit Neighborhood Partnership East, and University of Michigan School of Public Health. We also thank Margarita Reina and Kelly Jones for research assistance. We gratefully acknowledge support from the National Institute of Environmental Health Sciences (R01ES10936, R01ES014234) and the Aetna Foundation, a national Foundation based in Hartford, Connecticut that supports projects to promote wellness, health and access to high quality health care for everyone. Support for the first author’s time for manuscript preparation was provided by the Robert Wood Johnson Foundation Nurse Faculty Scholars Program (68033). The results presented here are solely the responsibility of the authors and do not necessarily represent the views of the study funders.
Contributor Information
Shannon N. Zenk, University of Illinois at Chicago College of Nursing.
Graciela Mentz, University of Michigan Department of Health Behavior and Health Education.
Amy J. Schulz, University of Michigan Department of Health Behavior and Health Education.
Vicki Johnson-Lawrence, University of Michigan-Flint Department of Public Health and Health Sciences.
Causandra R. Gaines, Healthy Environments Partnership.
References
- Andreyeva T, Luedicke J, Middleton AE, Long MW, Schwartz MB. Positive influence of the revised special supplemental nutrition program for women, infants, and children food packages on access to healthy foods. Journal of the Academy of Nutrition and Dietetics. 2012;112(6):850–858. doi: 10.1016/j.jand.2012.02.019. [DOI] [PubMed] [Google Scholar]
- Auchincloss AH, Mujahid MS, Shen M, Michos ED, Whitt-Glover MC, Diez Roux AV. Neighborhood health-promoting resources and obesity risk (the multi-ethnic study of atherosclerosis) Obesity. 2013;21(3):621–628. doi: 10.1038/oby.2012.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker EA, Schootman M, Barnidge E, Kelly C. The role of race and poverty in access to foods that enable individuals to adhere to dietary guidelines. Preventing Chronic Disease. 2006;3(3):A76. [PMC free article] [PubMed] [Google Scholar]
- Ball K, Timperio A, Crawford D. Neighbourhood socioeconomic inequalities in food access and affordability. Health Place. 2009;15(2):578–585. doi: 10.1016/j.healthplace.2008.09.010. [DOI] [PubMed] [Google Scholar]
- Beaulac J, Kristjansson E, Cummins S. A systematic review of food deserts, 1966–2007. Preventing Chronic Disease. 2009;6(3):1–10. [PMC free article] [PubMed] [Google Scholar]
- Berghofer A, Pischon T, Reinhold T, Apovian CM, Sharma AM, Willich SN. Obesity prevalence from a European perspective: A systematic review. BMC Public Health. 2008;8 doi: 10.1186/1471-2458-8-200. 200-2458-8-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block JP, Christakis NA, O’Malley AJ, Subramanian SV. Proximity to food establishments and body mass index in the Framingham heart study offspring cohort over 30 years. American Journal of Epidemiology. 2011;174(10):1108–1114. doi: 10.1093/aje/kwr244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boone-Heinonen J, Diez-Roux AV, Goff DC, Loria CM, Kiefe CI, Popkin BM, Gordon-Larsen P. The neighborhood energy balance equation: Does neighborhood food retail environment + physical activity environment= obesity? The CARDIA study. PloS One. 2013;8(12):e85141. doi: 10.1371/journal.pone.0085141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. New England Journal of Medicine. 2003;348(17):1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. State initiatives supporting healthier food retail: An overview of the national landscape. n.d Retrieved December 19, 2015, from http://www.cdc.gov/obesity/downloads/healthier_food_retail.pdf.
- Charreire H, Casey R, Salze P, Simon C, Chaix B, Banos A, … Oppert JM. Measuring the food environment using geographical information systems: A methodological review. Public Health Nutrition. 2010;13(11):1773–1785. doi: 10.1017/S1368980010000753. [DOI] [PubMed] [Google Scholar]
- Chiasson MA, Findley S, Sekhobo J, Scheinmann R, Edmunds L, Faly A, McLeod N. Changing WIC changes what children eat. Obesity. 2013;21(7):1423–1429. doi: 10.1002/oby.20295. [DOI] [PubMed] [Google Scholar]
- Cuddeback G, Wilson E, Orme JG, Combs-Orme T. Detecting and statistically correcting sample selection bias. Journal of Social Service Research. 2004;30(3):19–33. [Google Scholar]
- Cummins S, Flint E, Matthews SA. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Affairs. 2014;33(2):283–291. doi: 10.1377/hlthaff.2013.0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummins S, Macintyre S. Food environments and obesity--neighbourhood or nation? International Journal of Epidemiology. 2006;35(1):100–104. doi: 10.1093/ije/dyi276. [DOI] [PubMed] [Google Scholar]
- Cummins S, Petticrew M, Higgins C, Findlay A, Sparks L. Large scale food retailing as an intervention for diet and health: Quasi-experimental evaluation of a natural experiment. Journal of Epidemiology and Community Health. 2005;59(12):1035–1040. doi: 10.1136/jech.2004.029843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbel B, Moran A, Dixon LB, Kiszko K, Cantor J, Abrams C, Mijanovich T. Assessment of a government-subsidized supermarket in a high-need area on household food availability and children’s dietary intakes. Public Health Nutrition. 2015;18(5):2881–2890. doi: 10.1017/S1368980015000282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farley TA, Rice J, Bodor JN, Cohen DA, Bluthenthal RN, Rose D. Measuring the food environment: Shelf space of fruits, vegetables, and snack foods in stores. Journal of Urban Health. 2009;86(5):672–682. doi: 10.1007/s11524-009-9390-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng J, Glass TA, Curriero FC, Stewart WF, Schwartz BS. The built environment and obesity: A systematic review of the epidemiologic evidence. Health & Place. 2010;16(2):175–190. doi: 10.1016/j.healthplace.2009.09.008. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. Journal of the American Medical Association. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. Journal of the American Medical Association. 2007;298(17):2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- Fleischhacker S, Evenson K, Rodriguez D, Ammerman A. A systematic review of fast food access studies. Obesity Reviews. 2011;12(5):e460–471. doi: 10.1111/j.1467-789X.2010.00715.x. [DOI] [PubMed] [Google Scholar]
- Fleischhacker SE, Flournoy R, Moore LV. Meaningful, measurable, and manageable approaches to evaluating healthy food financing initiatives: An overview of resources and approaches. Journal of Public Health Management and Practice. 2013;19(6):541–549. doi: 10.1097/PHH.0b013e318271c6eb. [DOI] [PubMed] [Google Scholar]
- Franco M, Diez Roux AV, Glass TA, Caballero B, Brancati FL. Neighborhood characteristics and availability of healthy foods in Baltimore. American Journal of Preventive Medicine. 2008;35(6):561–567. doi: 10.1016/j.amepre.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franco M, Diez Roux AV, Glass TA, Caballero B, Brancati FL. Neighborhood characteristics and availability of healthy foods in Baltimore. American Journal of Preventive Medicine. 2008;35(6):561–567. doi: 10.1016/j.amepre.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman DS Centers for Disease Control and Prevention (CDC) Obesity—United states, 1988–2008. MMWR Surveill Summ. 2011;60(01):73–77. [PubMed] [Google Scholar]
- Gibson DM. The neighborhood food environment and adult weight status: Estimates from longitudinal data. American Journal of Public Health. 2011;101(1):71–78. doi: 10.2105/AJPH.2009.187567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Sallis JF, Saelens BE, Frank LD. Nutrition environment measures survey in stores (NEMS-S): Development and evaluation. American Journal of Preventive Medicine. 2007;32(4):282–289. doi: 10.1016/j.amepre.2006.12.019. [DOI] [PubMed] [Google Scholar]
- Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: Extending horizons, envisioning the future. Social Science & Medicine. 2006;62(7):1650–1671. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- Grabner M. BMI trends, socioeconomic status, and the choice of dataset. Obesity Facts. 2012;5(1):112–126. doi: 10.1159/000337018. [DOI] [PubMed] [Google Scholar]
- Han E, Powell LM, Isgor Z. Supplemental nutrition assistance program and body weight outcomes: The role of economic contextual factors. Social Science & Medicine. 2012;74(12):1874–1881. doi: 10.1016/j.socscimed.2012.02.032. [DOI] [PubMed] [Google Scholar]
- Hillier A, McLaughlin J, Cannuscio CC, Chilton M, Krasny S, Karpyn A. The impact of WIC food package changes on access to healthful food in 2 low-income urban neighborhoods. Journal of Nutrition Education and Behavior. 2012;44(3):210–216. doi: 10.1016/j.jneb.2011.08.004. [DOI] [PubMed] [Google Scholar]
- Hossain P, Kawar B, El Nahas M. Obesity and diabetes in the developing world—a growing challenge. New England Journal of Medicine. 2007;356(3):213–215. doi: 10.1056/NEJMp068177. [DOI] [PubMed] [Google Scholar]
- House JS, Lepkowski JM, Kinney AM, Mero RP, Kessler RC, Herzog AR. The social stratification of aging and health. Journal of Health and Social Behavior. 1994;35(3):213–234. [PubMed] [Google Scholar]
- Izumi BT, Zenk SN, Schulz AJ, Mentz GB, Sand SL, de Majo RF, … Odoms-Young A. Inter-rater reliability of the food environment audit for diverse neighborhoods (FEAD-N) Journal of Urban Health. 2012;89(3):1–14. doi: 10.1007/s11524-011-9657-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karpyn A, Young C, Weiss S. Reestablishing healthy food retail: Changing the landscape of food deserts. Childhood Obesity. 2012;8(1):28–30. doi: 10.1089/chi.2011.0113. [DOI] [PubMed] [Google Scholar]
- Kelly T, Yang W, Chen C, Reynolds K, He J. Global burden of obesity in 2005 and projections to 2030. International Journal of Obesity. 2008;32(9):1431–1437. doi: 10.1038/ijo.2008.102. [DOI] [PubMed] [Google Scholar]
- Kennelly ME, Neff R, Rutkow L. Strengthening vendor standards in the supplemental nutrition assistance program: Are healthier foods within reach. Journal of Health Care Law and Policy. 2013;16(1):141–191. [Google Scholar]
- Kumanyika SK, Obarzanek E, Stettler N, Bell R, Field AE, Fortmann SP, … Hong Y. Population-based prevention of obesity the need for comprehensive promotion of healthful eating, physical activity, and energy balance: A scientific statement from american heart association council on epidemiology and prevention, interdisciplinary committee for prevention (formerly the expert panel on population and prevention science) Circulation. 2008;118(4):428–464. doi: 10.1161/CIRCULATIONAHA.108.189702. [DOI] [PubMed] [Google Scholar]
- Larson N, Story M. A review of environmental influences on food choices. Annals of Behavioral Medicine. 2009;38:56–73. doi: 10.1007/s12160-009-9120-9. [DOI] [PubMed] [Google Scholar]
- Ledoux T, Hingle M, Baranowski T. Relationship of fruit and vegetable intake with adiposity: A systematic review. Obesity Reviews. 2011;12(5):e143–e150. doi: 10.1111/j.1467-789X.2010.00786.x. [DOI] [PubMed] [Google Scholar]
- Li F, Harmer P, Cardinal BJ, Bosworth M, Johnson-Shelton D, Moore JM, … Vongjaturapat N. Built environment and 1-year change in weight and waist circumference in middle-aged and older adults: Portland neighborhood environment and health study. American Journal of Epidemiology. 2009;169(4):401–408. doi: 10.1093/aje/kwn398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liese AD, Weis KE, Pluto D, Smith E, Lawson A. Food store types, availability, and cost of foods in a rural environment. Journal of the American Dietetic Association. 2007;107(11):1916–1923. doi: 10.1016/j.jada.2007.08.012. [DOI] [PubMed] [Google Scholar]
- Ljungvall Å, Zimmerman FJ. Bigger bodies: Long-term trends and disparities in obesity and body-mass index among US adults, 1960–2008. Social Science & Medicine. 2012;75(1):109–119. doi: 10.1016/j.socscimed.2012.03.003. [DOI] [PubMed] [Google Scholar]
- Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiologic Reviews. 2009;31(1):7–20. doi: 10.1093/epirev/mxp005. [DOI] [PubMed] [Google Scholar]
- Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Archives of General Psychiatry. 2010;67(3):220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- Mayne SL, Auchincloss AH, Michael YL. Impact of policy and built environment changes on obesity-related outcomes: a systematic review of naturally occurring experiments. Obesity Reviews. 2015;16(5):362–375. doi: 10.1111/obr.12269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McTigue KM, Chang Y, Eaton C, Garcia L, Johnson KC, Lewis CE, … Rosal MC. Severe obesity, heart disease and death among white, African-American and Hispanic postmenopausal women. Obesity. 2014;22(3):801–810. doi: 10.1002/oby.20224. [DOI] [PubMed] [Google Scholar]
- Moore LV, Diez Roux AV, Nettleton JA, Jacobs DR., Jr Associations of the local food environment with diet quality--a comparison of assessments based on surveys and geographic information systems: The multi-ethnic study of atherosclerosis. American Journal of Epidemiology. 2008;167(8):917–924. doi: 10.1093/aje/kwm394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland K, Wing S, Diez Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. American Journal of Preventive Medicine. 2002;22(1):23–29. doi: 10.1016/s0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- Mytton OT, Nnoaham K, Eyles H, Scarborough P, Mhurchu CN. Systematic review and meta-analysis of the effect of increased vegetable and fruit consumption on body weight and energy intake. BMC Public Health. 2014;14(1):886. doi: 10.1186/1471-2458-14-886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the united states, 2011–2012. Journal of the American Medical Association. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell LM, Auld MC, Chaloupka FJ, O’Malley PM, Johnston LD. Associations between access to food stores and adolescent body mass index. American Journal of Preventive Medicine. 2007;33(4 Suppl):S301–S307. doi: 10.1016/j.amepre.2007.07.007. [DOI] [PubMed] [Google Scholar]
- Powell LM, Han E. Adult obesity and the price and availability of food in the United States. American Journal of Agricultural Economics. 2011;93(2):378–384. [Google Scholar]
- Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Preventive Medicine. 2006;44(3):189–195. doi: 10.1016/j.ypmed.2006.08.008. [DOI] [PubMed] [Google Scholar]
- Rooney B. Rust and sunbelt cities lead ‘07 foreclosures. CNN Money. 2008 Feb 13; Retrieved December 22, 2015, from http://money.cnn.com/2008/02/12/real_estate/realtytrac/
- Schultz DJ, Shanks CB, Houghtaling B. The impact of the 2009 Special Supplemental Nutrition Program for Women, Infants, and Children Food Package Revisions on participants: A systematic review. Journal of the Academy of Nutrition and Dietetics. 2015;115(11):1832–1846. doi: 10.1016/j.jand.2015.06.381. [DOI] [PubMed] [Google Scholar]
- Schulz AJ, Kannan S, Dvonch JT, Israel BA, Allen A, III, James SA, … Lepkowski J. Social and physical environments and disparities in risk for cardiovascular disease: The healthy environments partnership conceptual model. Environmental Health Perspectives. 2005;113(12):1817–1825. doi: 10.1289/ehp.7913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharkey JR, Dean WR, Nalty C. Convenience stores and the marketing of foods and beverages through product assortment. American Journal of Preventive Medicine. 2012;43(3):S109–S115. doi: 10.1016/j.amepre.2012.05.012. [DOI] [PubMed] [Google Scholar]
- Sowers MR, Karvonen-Gutierrez CA. The evolving role of obesity in knee osteoarthritis. Current Opinion in Rheumatology. 2010;22(5):533–537. doi: 10.1097/BOR.0b013e32833b4682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K. Creating healthy food and eating environments: Policy and environmental approaches. Annual Review of Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- Thorburn A. Prevalence of obesity in Australia. Obesity Reviews. 2005;6(3):187–189. doi: 10.1111/j.1467-789X.2005.00187.x. [DOI] [PubMed] [Google Scholar]
- Ulmer VM, Rathert AR, Rose D. Understanding policy enactment: The new orleans fresh food retailer initiative. American Journal of Preventive Medicine. 2012;43(3):S116–S122. doi: 10.1016/j.amepre.2012.05.011. [DOI] [PubMed] [Google Scholar]
- Whaley SE, Ritchie LD, Spector P, Gomez J. Revised WIC food package improves diets of WIC families. Journal of Nutrition Education and Behavior. 2012;44(3):204–209. doi: 10.1016/j.jneb.2011.09.011. [DOI] [PubMed] [Google Scholar]
- Williams LK, Thornton L, Ball K, Crawford D. Is the objective food environment associated with perceptions of the food environment? Public Health Nutrition. 2012;15(2):291–298. doi: 10.1017/S1368980011001947. [DOI] [PubMed] [Google Scholar]
- Winkler E, Turrell G, Patterson C. Does living in a disadvantaged area entail limited opportunities to purchase fresh fruit and vegetables in terms of price, availability, and variety? findings from the Brisbane food study. Health & Place. 2006;12(4):741–748. doi: 10.1016/j.healthplace.2005.09.006. [DOI] [PubMed] [Google Scholar]
- Wisely J, Spangler T. Motor city population declines 25% USA Today. 2011 Mar 24; Retrieved December 22, 2015, from http://usatoday30.usatoday.com/news/nation/census/2011-03-22-michigan-census_N.htm.
- Wrigley N, Warm D, Margetts B. Deprivation, diet and food retail access: Findings from the Leeds ‘food deserts’ study. Environment and Planning A. 2003;35(1):151–188. [Google Scholar]
- Zenk SN, Thatcher E, Reina M, Odoms-Young A. A systematic review of local food environments, body weight, and other diet-related health outcomes. In: Morland K, editor. Local food environments: Food access in America. Baton Rouge, FL: CRC Press; 2014. pp. 167–204. [Google Scholar]
- Zenk SN, Odoms-Young A, Powell LM, Campbell RT, Block D, Chavez N, … Armbruster J. Fruit and vegetable availability and selection: Federal food package revisions, 2009. American Journal of Preventive Medicine. 2012;43(4):423–428. doi: 10.1016/j.amepre.2012.06.017. [DOI] [PubMed] [Google Scholar]
- Zenk SN, Schulz AJ, Izumi B, Sand S, Lockett M, Odoms-Young A. Development, evolution, and implementation of the food environment audit for diverse neighborhoods. In: Israel BA, Eng E, Schulz AJ, Parker E, editors. Methods for conducting community-based participatory research for health. 2. San Francisco, CA: Jossey Bass; 2012. pp. 277–304. [Google Scholar]
- Zenk SN, Schulz AJ, Matthews SA, Odoms-Young A, Wilbur J, Rapp L, … Stokes C. Activity space environment and eating and physical activity behaviors: A pilot study. Health & Place. 2011;17(5):1150–1161. doi: 10.1016/j.healthplace.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenk SN, Powell LM, Rimkus L, Isgor Z, Barker DC, Ohri-Vachaspati P, Chaloupka F. Relative and absolute availability of healthier food and beverage alternatives across communities in the United States. American Journal of Public Health. 2014;104(11):2170–2178. doi: 10.2105/AJPH.2014.302113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Neighborhood racial composition, neighborhood poverty, and the spatial accessibility of supermarkets in metropolitan Detroit. American Journal of Public Health. 2005;95(4):660–667. doi: 10.2105/AJPH.2004.042150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Fruit and vegetable access differs by community racial composition and socioeconomic position in Detroit, Michigan. Ethnicity & Disease. 2006;16(1):275–280. [PubMed] [Google Scholar]
- Zenk SN, Schulz AJ, Lachance LL, Mentz G, Kannan S, Ridella W, Galea S. Multilevel correlates of satisfaction with neighborhood availability of fresh fruits and vegetables. Annals of Behavioral Medicine. 2009;38(1):48–59. doi: 10.1007/s12160-009-9106-7. [DOI] [PMC free article] [PubMed] [Google Scholar]