Summary
Background
Influenza continues to have a significant socioeconomic and health impact despite a long established vaccine program and approved antivirals. Preclinical data suggest combination antivirals might be more effective than oseltamivir alone in the treatment of influenza.
Methods
We conducted a randomized, double-blinded, multicenter phase 2 trial of combination antivirals versus monotherapy for the treatment of influenza. Participants ≥18 years with influenza at increased risk of complications from influenza were randomized by an online computer-generated randomization system to receive either oseltamivir, amantadine, and ribavirin or oseltamivir alone for 5 days, and followed for 28 days. The primary endpoint was the percentage of participants with virus detectable by polymerase chain reaction in nasopharyngeal swab at Day 3. Among the secondary outcomes, there were safety and time to alleviation of influenza clinical symptoms. ClinicalTrials.gov Identifier: NCT01227967.
Findings
Between March 2011 and April 2016 we randomized 633 participants. Seven participants were excluded from analysis: 3 were given treatment without randomization, 3 withdrew before taking any medication, and 1 was lost to follow-up. The primary analysis included 394 participants, excluding 47 in the pilot phase, 172 without confirmed influenza, and 13 without an endpoint sample. 80 of 200 (40.0%) participants in the combination arm had virus detectable at Day 3 compared to 97 of 194 (50.0%) (95%C.I. 0.2–19.8%, p=0.046) in the control arm. There was no benefit, however, in multiple clinical secondary endpoints, such as median duration of symptoms (4.5 days in the combination arm vs 4.0 days in the oseltamivir arm; p = 0.21).
Interpretation
Although oseltamivir, amantadine, and ribavirin showed a statistically significant decrease in viral shedding at Day 3 relative to oseltamivir, this difference was not associated with improved clinical benefit. More work is needed to understand the lack of clinical benefit when a difference in virologic outcome was identified.
Funding
National Institute of Allergy and Infectious Diseases, National Institutes of Health, United States.
Introduction
Influenza continues to have a significant socioeconomic and health impact despite a long-established vaccine program and approved antivirals. The CDC has defined the populations most at risk for adverse outcomes from influenza as adults 65 years of age or older, those with certain underlying medical conditions, children younger than 2 years old, and pregnant women.1 Additionally, for the 2009 H1N1 pandemic, morbid obesity was also suggested as an independent risk factor.2
The paradigm of combination antivirals to more effectively control viral replication was explored in influenza even before it became an established tenant in the treatment of HIV.3 In-vitro studies of dual antivirals have evaluated amantadine/oseltamivir4–6, amantadine/ribavirin5,7; rimantadine/neuraminidase inhibitors (NAI, i.e. zanamivir, oseltamivir, or peramivir)8 ribavirin/adamantanes (amantadine or rimantadine)5–7, ribavirin/NAI (oseltamivir or peramivir)5,6,9, dual NAI6 and combinations involving novel agents such as favipiravir/oseltamivir.10 Dual antiviral combinations have also been evaluated in animal studies including amantadine/oseltamivir5,11, amantadine/ribavirin5 rimantadine/oseltamivir12,13 and ribavirin/NAI (oseltamivir and peramivir)4,5,14,15. Dual antiviral therapy has had mixed efficacy results in-vitro and in-vivo although the combination of amantadine and oseltamivir may reduce the emergence of both oseltamivir and amantadine-resistant viruses in-vivo.16
The combination of amantadine, oseltamivir, and ribavirin has been shown to increase the antiviral activity in vitro (reduction in the EC50) of each drug compared to its activity in double combinations or as single agents.17 Circulating strains of influenza A have high levels of resistance to amantadine18, though preclinical data would suggest activity of amantadine when used in combination against amantadine resistant viruses.19 The combination of amantadine, oseltamivir, and ribavirin was more effective at preventing death as compared to dual and single drug regimens in mice infected with either influenza A/H5N1 or influenza A/H1N119. Furthermore, this combination provided survival benefit when treatment was delayed until 72 hours post-infection, whereas oseltamivir monotherapy was not protective after 24 hours postinfection19. Given the encouraging preclinical data, and the need for better therapeutics in high-risk populations, we conducted a blinded randomized, controlled trial (RCT) to test the hypothesis that the combination of amantadine, oseltamivir, and ribavirin is superior to oseltamivir alone in participants at risk for complications from influenza.
Methods
Study Design
The study was a randomized, double-blind, phase 2 study conducted in the United States, Thailand, Mexico, Argentina, and Australia. The study protocol was approved by an institutional review board/ethics committee for each study site as well as by all local and/or country governing bodies as applicable. All study participants provided written informed consent.
Participants
Males and non-pregnant females ≥18 years of age who had the presence of an underlying medical condition(s) that may increase risk of complications from influenza, who had influenza A(H1N1), A(H3N2) or B virus infections diagnosed locally by rapid antigen or polymerase chain reaction (PCR), and who had the onset of respiratory symptoms no more than 96 hours before screening were eligible for the study. The risk factors included: age 65 years or older, presence of one or more chronic medical conditions (detailed in the supplemental appendix), or BMI ≥ 40 kg/m2. Participants were excluded if they had anemia, leukopenia, neutropenia, thrombocytopenia, genetic hemoglobinopathy, creatinine clearance less than indicated for clinical dosing with these antivirals, history of autoimmune hepatitis, uncompensated or severe liver disease, or had received more than two doses of any antiviral influenza medications since the onset of influenza symptoms.
Randomization and masking
Participants were randomized by an online computer-generated randomization system in a 1:1 ratio to receive either combination treatment with amantadine, oseltamivir, and ribavirin, or oseltamivir monotherapy. Randomization was not stratified. A computer generated central randomization scheme was used. The study treatment kits had open label oseltamivir 75 mg, three capsules of over-encapsulated ribavirin 200 mg or matching placebo, and one capsule of over-encapsulated amantadine 100 mg or matching placebo. The study treatments were identical in appearance. The treatment of 5 capsules was given twice daily for 5 days.
Procedures
Participants were assessed on Study Day 0 (pre-dose), and on Study Days 3, 7, and 28. The study was originally designed with visits on Days 1, 2, 3, 5, 7, 10, 14, and 28, and was amended in 2012 after completion of the pilot study (below) in order to simplify study visits and improve enrollment. Nasopharyngeal (NP) swab to test for influenza virus were collected from the participants by the study team on Days 0, 3, 7, and blood samples collected on Days 0, 3, 7, and 28. The study teams were trained by in person training, training videos, and pre-study quality assurance test swabs (assaying for presence of housekeeping genes from nasal epithelium). Participants received diary cards that were to be completed twice daily from Day 0 to Day 7, once daily for Days 8–14, and again on Day 28.
Outcomes
The first 50 participants randomized were part of a pilot study to help determine the virologic endpoint to be used in the primary efficacy analysis based on virologic and practical considerations (actual N=47). These participants had NP and oropharyngeal (OP) swabs performed and all samples were tested by both PCR and tissue culture infectious dose (TCID50) measurements. Additionally, these participants had duplicate virologic samples obtained on Day 0 to determine reproducibility of the virologic assays. After analysis of this pilot study without unblinding to treatment, the primary endpoint was selected to be the percentage of participants with virus detectable by PCR in NP swab at Day 3.
Secondary clinical endpoints included time to alleviation of influenza clinical symptoms (grade 1 or below), time to absence of fever, time to alleviation of influenza clinical symptoms and fever, time to resumption of pre-influenza level of activity, proportion of participants who developed bronchitis, pneumonia, or other complications of influenza, proportion of participants that required hospitalization after randomization, proportion of participants who required new or increased use of supplemental oxygen, safety and tolerability (AEs and SAEs) and 28-day mortality.
At the time of study commencement, there was no standardized, validated patient-reported outcome tool for influenza.20 The diary cards asked participants to record maximum temperature and to rate 11 symptoms (derived from prior efficacy studies of oseltamivir): cough, fatigue, subjective fever (feverishness), diarrhea, myalgia, vomiting, headache, nausea, sore throat, nasal obstruction, and nasal discharge to be graded from absent to severe (0–3).
Two global assessment questions were asked: “Are you feeling as good as you did before you had the flu?” and “Are you functioning as well as you were before you had the flu?”. The diary card contained the 10-question physical domain of the SF-36 (completed daily per SF-36 instructions), and each functional characteristic was graded by participants as being limited a lot, a little, or not at all (1–3 points respectively) that was then transformed into a 100-point scale and averaged across the 10 questions.21 At baseline and at each visit investigators asked participants about any signs/symptoms suggestive of otitis media, bronchitis / bronchiolitis, or pneumonia. The presence of these complications was determined by the site investigator based on clinical data available at the time, as there was no protocol-defined evaluation for these complications. The investigators were also asked to assess the use of antibiotics for reasons besides the complications noted above. A Data Safety Monitoring Board (DSMB) reviewed the safety data from the study.
Virologic Analysis
Influenza type and subtype was determined using the CDC protocol of real-time RT-PCR for influenza A and B, and performed at the Naval Health Research Center (NHRC) in San Diego, CA. Influenza viral load in swab samples was determined by qPCR using the TaqMan method. See appendix for full virology methods.
Statistical Analysis
The sample size was chosen to be 560 randomized participants (including 50 in the pilot study) and was determined to give approximately 90% power to detect an absolute difference of 15% in the proportion of participants with undetectable virus shedding at Day 3 in NP swabs (e.g. a reduction of 15% from 57·5% in the combination arm to 42·5% in the oseltamivir arm) using a two-sided type I error rate of 0·05. This power calculation was based on the fact that approximately 50% of participants in the pilot study had undetectable virus in NP swabs at Day 3 (pooled over randomized arms) and included allowance for 10% of participants to have unavailable viral shedding results at Day 3. Due to the larger than expected number of Day 0 samples without detectable virus, the protocol permitted randomization through the end of the influenza season in 2016 up to a maximum of 720 participants. Additional statistical analysis methods are noted in the supplemental appendix.
Role of the Funding Source
Employees of the sponsor of the study were involved with study design, analysis, and the writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
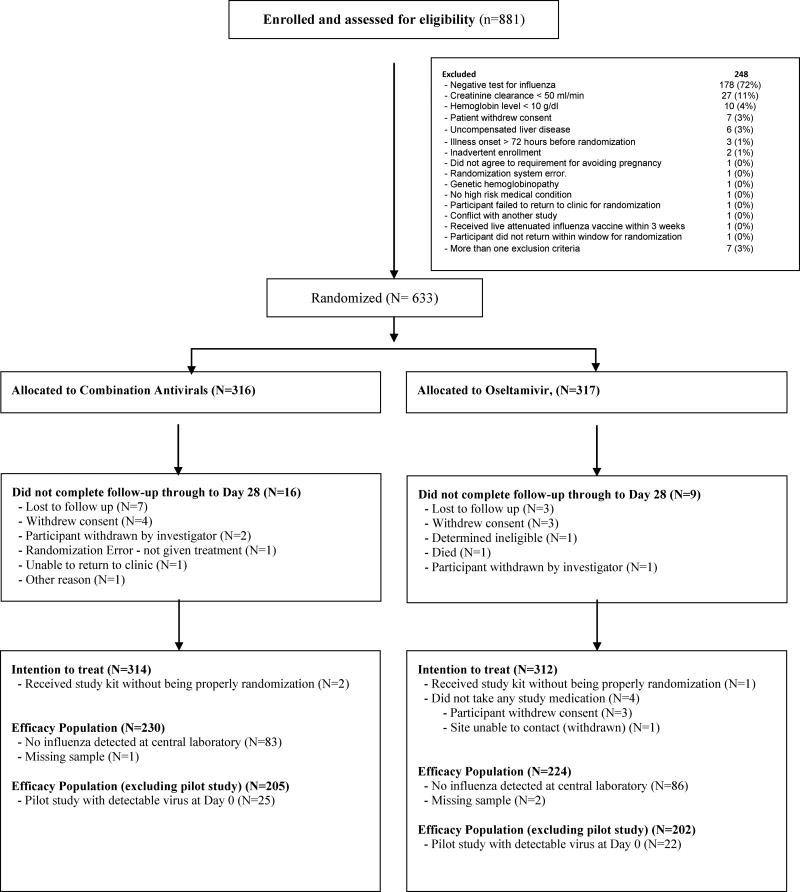
Between March 2011 and April 2016, 881 participants signed consent at 65 sites (Figure 1). Two hundred forty-eight were excluded during screening: 178 did not have a positive test for influenza, 28 had a creatinine clearance < 50 ml/min, 10 had a hemoglobin < 10 g/dL, 7 withdrew consent, 6 had uncompensated liver disease, 3 had onset of illness > 72 hours prior to randomization and the remainder were excluded for other study reasons or multiple of the reasons listed above. 633 participants were randomized at 50 sites: 439 participants (69%) at 37 sites in US, 131 participants (21%) at 4 sites in Thailand, 38 (6%) at 3 sites in Mexico, 23 participants (4%) at 4 sites in Argentina, and 2 participants (<0·5%) at 2 sites in Australia. 22 participants had minor enrollment deviations. Three participants at one site were given a study medication kit without proper randomization, 3 participants were randomized but withdrew or lost to follow-up prior to receiving study treatment. These 7 participants were excluded from all analyses (per protocol defined ITT population). The study was stopped after reaching planned enrollment.
Figure 1.
Enrollment, Randomization and Treatment
Characteristics of participants are described in Table 1. The median age of the randomized participants was 49·5 years, with a range of 18–98 years; 128 (20%) were ≥ 65 years of age. The most common medical conditions that put the participants at risk for severe influenza were asthma and endocrine disorders such as diabetes, and were comparable across arms. Participants presented with a median of 42 hours of illness, were randomized a median of 1 hour after screening, with study medication started a median of 1 hour after randomization. By local site testing, 440 (70%) had influenza A and 155 (25%) had influenza B, 15 (2%) not specified, and 16 (3%) reported more than one subtype. By central laboratory qualitative PCR testing, 244 (39%) participants had influenza A/H3N2, 104 (17%) influenza A/H1N1, 106 (17%) influenza B, and 169 (27%) were influenza-negative (the remaining 3 had no baseline sample available for testing). The primary efficacy analyses included these 454 participants with confirmed influenza infection by central laboratory testing.
Table 1.
Demographics, and Baseline Characteristics (ITT Population)
| Total (N=626) | Combination Antivirals (N=314) |
Oseltamivir (N=312) |
|
|---|---|---|---|
| Age | |||
| Median (quartiles) | 49·5 (36·0, 61·0) | 49·5 (37·0, 61·0) | 49·5 (35·5, 61·0) |
| Min, Max | 18, 98 | 18, 89 | 18, 98 |
| Sex | |||
| Female | 385 (62%) | 187 (60%) | 198 (63%) |
| Race | |||
| White | 392 (63%) | 203 (65%) | 189 (61%) |
| Asian | 143 (23%) | 70 (22%) | 73 (23%) |
| Black or African American | 43 (7%) | 18 (6%) | 25 (8%) |
| American Indian | 3 (0%) | 1 (0%) | 2 (1%) |
| Race not available to clinic | 45 (7%) | 22 (7%) | 23(7%) |
| Ethnicity | |||
| Hispanic or Latino | 113 (18%) | 55 (18%) | 58 (19%) |
| Country | |||
| USA | 436 (70%) | 220 (70%) | 216 (69%) |
| Thailand | 131 (21%) | 65 (21%) | 66 (21%) |
| Mexico | 35 (6%) | 17 (5%) | 18 (6%) |
| Argentina | 22 (4%) | 12 (4%) | 10 (3%) |
| Australia | 2 (0%) | 0 (0%) | 2 (1%) |
| Influenza type (by central lab) | |||
| Influenza A/H3N2 | 244 (39%) | 126 (40%) | 118 (38%) |
| Influenza A/H1N1 | 104 (17%) | 55 (18%) | 49 (16%) |
| Influenza B | 106 (17%) | 49 (16%) | 57 (18%) |
| Negative | 169 (27%) | 83 (27%) | 86 (28%) |
| # missing | 3 | 1 | 2 |
| Medical condition* | |||
| Age 65 years or greater | 128 (20%) | 63 (20%) | 65 (21%) |
| Asthma | 199 (32%) | 100 (32%) | 99 (32%) |
| Endocrine | 175 (28%) | 87 (28%) | 88 (28%) |
| Weakened immune system | 90 (14%) | 44 (14%) | 46 (15%) |
| Heart disease | 69 (11%) | 30 (10%) | 39 (13%) |
| Chronic Lung disease | 38 (6%) | 17 (5%) | 21 (7%) |
| Neurological condition | 36 (6%) | 17 (5%) | 19 (6%) |
| Metabolic | 20 (3%) | 12 (4%) | 8 (3%) |
| Kidney | 14 (2%) | 8 (3%) | 6 (2%) |
| Blood disorder | 13 (2%) | 8 (3%) | 5 (2%) |
| Liver disorder | 10 (2%) | 3 (1%) | 7 (2%) |
| BMI ≥ 40 kg/m2 | 125 (20%) | 74 (24%) | 51 (16%) |
| Fever (≥ 38·0 C) | 187 (30%) | 94 (30%) | 93 (30%) |
| Hours from onset of influenza-like illness to screening | |||
| Median (quartiles) | 42 (27, 54) | 43 (28, 55) | 41 (25, 52) |
| Min, Max | 0, 97 | 1, 97 | 0, 95 |
| Hours from screening to randomization | |||
| Median (quartiles) | 1 (0, 2) | 1 (0, 2) | 1 (0, 2) |
| Min, Max | 0, 24 | 0, 23 | 0, 24 |
| Hours from randomization to treatment initiation | |||
| Median (quartiles) | 1 (0, 2) | 1 (0, 2) | 1 (0, 2) |
| Min, Max | 0, 18 | 0, 18 | 0, 18 |
| Smoking (ever)? | |||
| Yes | 177 (28%) | 88 (28%) | 89 (29%) |
| Influenza vaccination in the season of enrollment? | |||
| Yes | 193 (31%) | 90 (29%) | 103 (33%) |
some participants had multiple conditions, so the sum of the percentages may exceed 100%.
At baseline, participants were moderately symptomatic (median 15 points on the 11-item symptom score graded 0–3 (absent – severe) (Supplemental Table 1). Participants had moderate physical limitations as assessed on the SF-36 physical domain (median 35), and were almost universally not feeling as good or functioning as well as before they developed the influenza illness (603 (97%) and 576 (93%) respectively).
Of the 454 participants with confirmed influenza infection in central laboratory testing, 20 (4%) did not have virus detected on the quantitative PCR assay, and 13 (3%) had virus detected below the assay LLOQ, though the presence of housekeeping genes GAPDH and B2M in the majority of these samples suggested that this was not due to poor sample collection technique. The median (quartiles) viral load at baseline was 6·5 (5·4, 7·4) log10 copies/mL. These were similar in the two treatment arms: median 6·4 (5·6, 7·2) vs 6·7 (5·1, 7·7) for the combination arm and the oseltamivir arm, respectively.
Ninety-three percent of participants (583 of 626) reported taking all study drug on all 5 days and were similar in both arms (289 (92%) vs 294 (94%)), 6% (36) had partially completed the treatment course (1–4 days), and 1% (6 participants) were lost to follow up before treatment compliance was assessed.
In the 454 participants in the Efficacy Population, 437 (96%) had a Day 3 virologic endpoint sample available for testing (9 missing in the combination arm and 8 in the oseltamivir arm). In the Efficacy Population when excluding the participants from the pilot study, 80 (40·0%) of 200 participants had virus detectable (i.e. above the PCR limit of detection, LOD) in the combination arm compared to in the oseltamivir arm, a difference of a difference of 10·0% (95% CI 0·2–19·8, p=0·046). Similar results were observed when including the participants from the pilot study,87 of 221 (39·4%) vs 112 of 216 (51·9%) in the oseltamivir arm, a difference of 12·5% (95% CI 3·2–21·8, p=0·009). (Table 2) This difference between the two arms did not appear to vary by sex (interaction p=0·74, logistic regression), influenza type (interaction p=0·23), or country and race (interaction p=0·062). At Day 3, the median (quartiles) viral shedding in the Efficacy Population was 3·4 (3·2, 4·2) log10 copies/mL in the combination arm compared to 3·9 (<3·2, 4·95) log10 copies/mL in the oseltamivir arm (p = 0·004) (Table 2). By Day 7, 54 (13%) participants had detectable virus (23 (11%) vs 31 (14%), p = 0·24)).
Table 2.
Influenza Virus Over Time (Efficacy Population)
| Total (N=454) | Combination Antivirals (N=230) |
Oseltamivir (N=224) |
p-value | |
|---|---|---|---|---|
| Day 0 | 454 | 230 | 224 | |
| Median (quartiles) log10 copies/mL | 6·50 (5·40, 7·40) | 6·40 (5·60, 7·20) | 6·70 (5·10, 7·70) | |
| Min, Max log10 copies/mL | <3·20, 9·40 | <3·20, 9·00 | <3·20, 9·40 | |
| ≥ LLOQ | 421 (93%) | 221 (96%) | 200 (89%) | |
| ≥ LOD, < LLOQ | 13 (3%) | 4 (2%) | 9 (4%) | |
| < LOD | 20 (4%) | 5 (2%) | 15 (7%) | |
| Day 3 | 437 | 221 | 216 | |
| Median (quartiles) log10 copies/mL | 3·40 (3·20, 4·60) | 3·40 (3·20, 4·20) | 3·90 (3·20, 4·95) | 0·004 |
| Min, Max log10 copies/mL | <3·20, 7·80 | <3·20, 7·60 | <3·20, 7·80 | |
| # missing | 17 | 9 | 8 | |
| ≥ LLOQ | 152 (35%) | 65 (29%) | 87 (40%) | 0·009 |
| ≥ LOD, <LLOQ | 47 (11%) | 22 (10%) | 25 (12%) | |
| < LOD | 238 (54%) | 134 (61%) | 104 (48%) | |
| Day 7 | 431 | 216 | 215 | |
| Median (quartiles) log10 copies/mL | <3·20 (<3·20, 3·40) | <3·20 (<3·20, 3·40) | <3·20 (<3·20, 3·40) | 0·38 |
| Min, Max log10 copies/mL | <3·20, 7·60 | <3·20, 6·90 | <3·20, 7·60 | |
| # missing | 23 | 14 | 9 | |
| ≥ LLOQ | 43 (10%) | 19 (9%) | 24 (11%) | 0·24 |
| ≥ LOD, < LLOQ | 11 (3%) | 4 (2%) | 7 (3%) | |
| < LOD | 377 (87%) | 193 (89%) | 184 (86%) |
LLOQ: lower limit of quantification of PCR assay; LOD: limit of detection of PCR assay. Primary endpoint percentage of participants with virus detectable by PCR (i.e. ≥ LLOQ + ≥ LOD, < LLOQ)
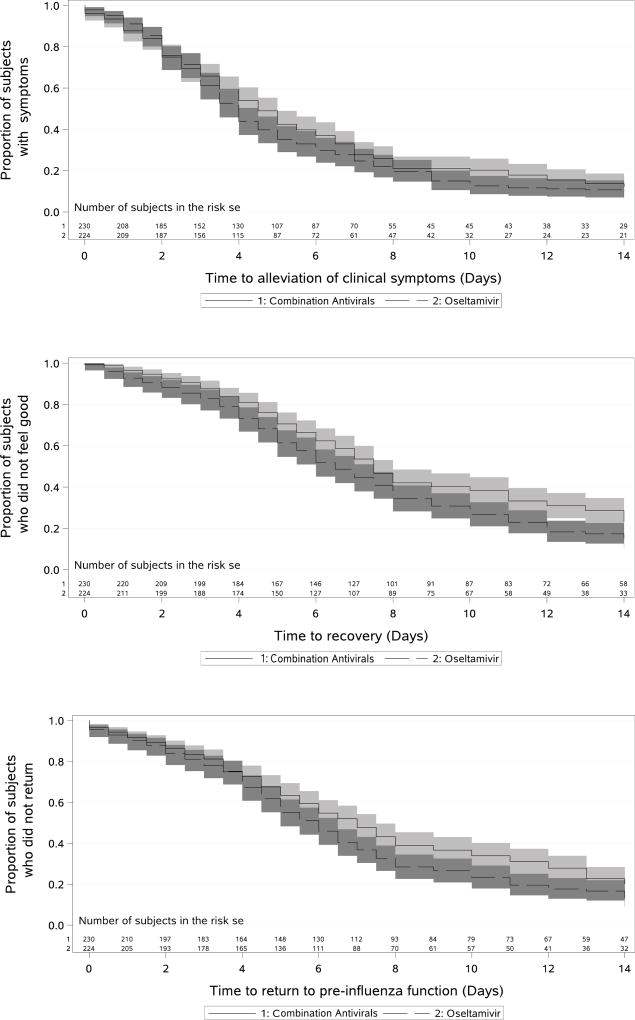
Among the 454 participants in the Efficacy Population, the median duration of symptoms was 4·5 days in the combination arm vs 4·0 days in the oseltamivir arm (p = 0·21). (Figure 2A, Table 3). When all 626 participants in the ITT population are evaluated, the results are similar (4·5 vs 4·0 days, p = 0·44) (Table 3) When restricting the ITT population to those participants with more severe symptoms (at least one grade 2 or 3 symptom at randomization), the medians were unchanged (4·5 (95% CI 4·0–5·0) vs 4·0 (95% CI 4·0–4·5), p = 0·18). In subgroup analyses for the ITT population, there was no significant difference in duration of symptoms by sex (interaction p = 0·87), flu type (p=0·53), or country and race (p=0·55).
Figure 2.
Proportion of participants with clinical symptoms (A, p=0·21), not feeling as good as before illness (B, p=0·009), and not functioning as well as before illness (C, p=0·019) (Efficacy Population, Shaded areas denote 95% confidence intervals)
Table 3.
Clinical Efficacy by treatment arm (median estimate, 95% CI)
| Combination Antivirals (N=230) | Oseltamivir (N=224) | p value | ||
| Efficacy Population | Duration of clinical symptoms (days) | 4·5 (4·0–5·0) | 4·0 (3·5–4·5) | 0·21 |
| Duration of fever # (days) | 1·0 (1·0,1·5) | 1·0 (0·5,1·5) | 0·59 | |
| Duration of clinical symptoms and /or fever (days) | 5·0 (4·5–6·0) | 4·0 (3·5–5·0) | 0·10 | |
| Duration of time to feel as good as before the onset of the influenza illness (days) | 7·5 (7·0–8·0) | 6·5 (6·0–7·5) | 0·009 | |
| Duration of time to return to pre-influenza function (days) | 7·0 (6·0–7·5) | 6·0 (5·0–6·5) | 0·019 | |
| Combination Antivirals (N=314) | Oseltamivir (N=312) | p value | ||
| ITT Population | Duration of clinical symptoms (days) | 4·5 (4·0–5·0) | 4·0 (3·5–4·5) | 0·44 |
| Duration of fever # (days) | 1·0 (*) | 1·0 (0·5,1·0) | 0·69 | |
| Duration of clinical symptoms and fever (days) | 4·5 (4·0–5·0) | 4·5 (4·0–5·0) | 0·30 | |
| Duration of time to feel as good as before the onset of the influenza illness (days) | 7·5 (7·0–7·5) | 6·5 (6·0–7·0) | 0·003 | |
| Duration of time to return to pre-influenza function(days) | 7·0 (6·0–7·5) | 6·0 (5·0–6·5) | 0·009 |
restricted to those with fever at randomization
confidence interval not estimable
Those treated with combination antivirals in the Efficacy Population took longer until they felt as good as before the onset of the influenza illness (median 7·5 vs 6·5 days, p=0·009, Figure 2B) or until the participant functioned as well as before the onset of influenza illness (7·0 vs 6·0 days, p=0·019) (Figure 2C, Table 3). There was no difference in the physical function score on the SF- 36 between arms (Supplemental Figure 1). There were 74 complications noted among the 626 participants through Day 28: 28 participants had sinusitis (14 vs 14 in the combination arm versus the oseltamivir arm, respectively), 4 had otitis media (1 vs 3), 29 had bronchitis (18 vs 11) and 13 had pneumonia (7 vs 6). Additionally, antibiotics were given for reasons other than the complications noted above in 56 participants (27 vs 29). Complication or antibiotic use occurred in a total of 100 participants (52 vs 48, as some participants had more than one complication and/or antibiotic use), and was not different among treatment arms (p = 0·69).
One death occurred in the study in an elderly participant randomized to oseltamivir monotherapy who died of cardiovascular failure 13 days after randomization, and judged by the site investigator as not related to study intervention. 28-day mortality was a specified secondary endpoint, but given there was only 1 death during the study, no analysis was performed.
Fifty-four participants that had detectable virus on Day 7, and per protocol Day 0 and 7 samples from these participants were sequenced for the presence of resistance. All successfully sequenced influenza samples contained the S31N substitution in the M2 gene at baseline, known to be associated with resistance to amantadine. Five participants had virus with oseltamivir resistance in the NA gene at baseline: three H1N1 I117T, one H1N1 I117M, and one H3N2 K150S (2 in the combination arm, and 3 in the oseltamivir arm). There were no participants with influenza B virus resistance at baseline. No Day 7 samples showed a change in sequence at loci (compared to Day 0) associated with oseltamivir resistance.
Three hundred seventeen of the 626 participants randomized reported a total of 1141 adverse events, between randomization and Day 28. The most common adverse events (by events, not by participants) were gastrointestinal-related disorders, primarily nausea (65 (12%) vs 63 (11%) in the combination arm versus the oseltamivir arm), vomiting (56 (10%) vs 64 (11%)), and diarrhea (39 (7%) vs 23 (4%)). The number of participants with adverse events are noted in Supplemental Table 2. All adverse events occurred in similar proportions in both arms. In review of laboratory abnormalities, the median total bilirubin increased in the combination arm from a median (quartiles) of 0·4 (0·3,0·6) mg/dL on Day 0, to 0·5 (0·3,0·7) mg/dL on Day 3, and to 0·6 (0·3,0·8) mg/dL on Day 7, and returned to 0·4 (0·3,0·6) mg/dL on Day 28, compared to median 0·4 mg/dL (0·3,0·5–0·6) on all study days in the oseltamivir arm. The hemoglobin was not different between arms with a median (quartiles) on Day 0, 3, 7 of 13·8 (12·8,14·9), 13·8 (12·9,14·8) 13·5 (12·5,14·5) in the combination arm vs 13·7 (12·6,14·8), 13·6 (12·6,14·6) and 13·4 (12·5,14·6) in the oseltamivir arm.
Twenty-two serious adverse events (SAEs) occurred in 20 participants: 16 events in 14 participants in the combination arm and 6 events in 6 participants in the oseltamivir arm (Table 4). Only asthma exacerbation, diarrhea, and pneumonia occurred in more than one participant. There were four gastrointestinal SAEs in the combination arm (3 diarrhea, 1 nausea) and none in the oseltamivir arm. Only two of the SAEs (delirium and personality change) were judged to be related to study medication, and both of these occurred in the oseltamivir arm. One participant in the oseltamivir arm died from cardiovascular failure during the study observation period was judged by the site investigators to be “not related” to study intervention. Thirteen participants in the combination arm and 3 participants in the oseltamivir arm were hospitalized (p=0·011, logrank test).
Table 4.
Number of Participants with Hospitalization and/or Serious Adverse Events -Total, and by Treatment Arm (ITT Population) including all events reported after randomization through to Day 28
| Randomized Treatment | |||
|---|---|---|---|
| Event | Total (N=626) |
Combination Antivirals (N=314) |
Oseltamivir (N=312) |
| Any Hospitalization | 16 (3%) | 13 (4%) | 3 (1%) |
|
| |||
| Serious Adverse Events | |||
| Any Serious Adverse Events | 20 (3%) | 14 (4%) | 6 (2%) |
| Respiratory, thoracic and mediastinal disorders | 5 (1%) | 4 (1%) | 1 (<0·5%) |
| Asthma | 2 (<0·5%) | 2 (1%) | 0 (0%) |
| Pulmonary oedema | 1 (<0·5%) | 1 (<0·5%) | 0 (0%) |
| Respiratory distress | 1 (<0·5%) | 1 (<0·5%) | 0 (0%) |
| Bronchospasm | 1 (<0·5%) | 0 (0%) | 1 (<0·5%) |
| Gastrointestinal disorders | 4 (1%) | 4 (1%) | 0 (0%) |
| Diarrhoea | 2 (<0·5%) | 2 (1%) | 0 (0%) |
| Nausea | 1 (<0·5%) | 1 (<0·5%) | 0 (0%) |
| Diarrhoea haemorrhagic | 1 (<0·5%) | 1 (<0·5%) | 0 (0%) |
| Infections and infestations | 4 (1%) | 3 (1%) | 1 (<0·5%) |
| Pneumonia | 2 (<0·5%) | 1 (<0·5%) | 1 (<0·5%) |
| Gastroenteritis | 1 (<0·5%) | 1 (<0·5%) | 0 (0%) |
| Cellulitis | 1 (<0·5%) | 1 (<0·5%) | 0 (0%) |
| Cardiac disorders | 3 (<0·5%) | 2 (1%) | 1 (<0·5%) |
| Atrial fibrillation | 1 (<0·5%) | 1 (<0·5%) | 0 (0%) |
| Cardiac failure | 1 (<0·5%) | 0 (0%) | 1 (<0·5%) |
| Atrial tachycardia | 1 (<0·5%) | 1 (<0·5%) | 0 (0%) |
| Psychiatric disorders | 2 (<0·5%) | 0 (0%) | 2 (1%) |
| Delirium | 1 (<0·5%) | 0 (0%) | 1 (<0·5%) |
| Personality change | 1 (<0·5%) | 0 (0%) | 1 (<0·5%) |
| Skin and subcutaneous tissue disorders | 1 (<0·5%) | 1 (<0·5%) | 0 (0%) |
| Diabetic foot | 1 (<0·5%) | 1 (<0·5%) | 0 (0%) |
| Metabolism and nutrition disorders | 1 (<0·5%) | 1 (<0·5%) | 0 (0%) |
| Dehydration | 1 (<0·5%) | 1 (<0·5%) | 0 (0%) |
| Injury, poisoning and procedural complications | 1 (<0·5%) | 1 (<0·5%) | 0 (0%) |
| Spinal compression fracture | 1 (<0·5%) | 1 (<0·5%) | 0 (0%) |
| Injury, poisoning and procedural complications | 1 (<0·5%) | 0 (0%) | 1 (<0·5%) |
| Febrile neutropenia | 1 (<0·5%) | 0 (0%) | 1 (<0·5%) |
Discussion
To our knowledge, this is the first large randomized controlled comparison of oseltamivir, amantadine, and ribavirin vs oseltamivir alone for the treatment of influenza. The study, conducted in an ambulatory population with risk factors for complications from influenza, demonstrated a modest but statistically significant 10% absolute reduction from 50% to 40% in the proportion of participants shedding virus on Day 3. Together with the quantitative reduction in viral load at Day 3, the combination of oseltamivir, amantadine and ribavirin does indeed appear to decrease viral shedding relative to conventional monotherapy. By Day 7, however, a similarly high proportion of participants in both arms (89% and 86%) had stopped shedding influenza virus, and the difference between treatments was no longer significant.
This reduction in viral shedding by combination antivirals, however, did not translate into clinical benefit when evaluated across multiple different parameters. When assessed by symptoms, fever, and by the physical domain of SF-36, and occurrence of complications it also did not appear that participants “felt” better any more quickly after treatment with combination antivirals than with oseltamivir alone. Indeed, by some metrics such as the global assessments, participants receiving the combination antivirals may have recovered somewhat slower.
This is the largest and most comprehensive study evaluating combination antivirals for the treatment of influenza. A prior pilot study evaluated the use of combination antivirals (amantadine 75 mg, oseltamivir 50 mg, and ribavirin 200 mg three times a day) in 7 immunocompromised patients with influenza H1N1 or H3N2 (3 with randomized allocation (one to oseltamivir monotherapy and two combination), and 4 were given combination antivirals without randomization).22 The authors report the general safety of combination antivirals in this population, but no inference of efficacy could be made. A non-randomized retrospective review of patients with influenza H1N1 on mechanical ventilation compared the outcomes of 24 patients receiving combination antiviral therapy to 103 patients receiving oseltamivir monotherapy.23 The dose and duration of all these medications including oseltamivir was not standardized in this population. A 14- day mortality of 17% vs 35% and 90-day mortality of 46% vs 59% was reported in the combination group and oseltamivir monotherapy group respectively, though neither reached statistical significance and interpretation is difficult given differences in the populations and drug interventions. Another retrospective review of 14 patients with complicated H1N1 influenza compared the viral shedding seen in high-dose oseltamivir (150 mg twice a day) in 8 patients to 6 patients treated with combination antiviral drugs (150 mg oseltamivir twice a day, 100 mg amantadine twice a day, and 300 mg ribavirin three times a day).24 The authors concluded that combination antivirals could be useful to achieve virologic clearance, though viral shedding after 5 days was seen in 1 of 6 participants treated with oseltamivir monotherapy, and 2 of 6 of those treated with combination antivirals.
In this study, although there were more SAEs in the combination antiviral arm, nonetheless the combination of oseltamivir, amantadine, and ribavirin appeared generally safe and well tolerated. There were significantly more hospital admissions in the combination arm. There were a greater number of respiratory SAEs, but these seemed unlikely to be due to the antiviral medications themselves given the known side effects with these medications. There were more gastrointestinal SAEs in the combination arm, which could be due to either the medications or to the underlying influenza illness, but the rate of gastrointestinal AEs was not notably different between the two treatment arms. Neurologic AEs, a particular concern of regimens using amantadine, were also not notably different between the treatment arms.
The lack of demonstrable clinical benefit despite enhanced viral clearance is both intriguing and disappointing. In preclinical studies, viral titers measured by PCR and TCID50 correlated with severity of disease across multiple animal models, and antiviral effects correlated with reduced morbidity.25 In influenza challenge models, viral titers (TCID50), nasal cytokines and chemokines, and upper and lower respiratory symptoms were all strongly correlated.26 In observational studies, early oseltamivir treatment was associated with a decrease in viral RNA concentration, and viral RNA clearance on Day 5 was associated with a shorter time to discharge from the hospital (6·0 vs 8·0 days; p =0·038).27 For these reasons, it has been argued that virologic primary endpoints should be used in antiviral studies in those at high risk of severe disease.28 However, to date the FDA has not accepted this argument, noting “there is no established predictive relationship between magnitude and timing of viral reductions and extent of clinical benefit of how a patient ‘feels, functions, or survives’”.29
In this large double-blind prospective multicenter RCT conducted in multiple countries, virologic treatment benefit was observed without improved clinical outcomes. This calls into question whether changes in viral shedding from an antiviral can be used to predict changes in clinical outcomes. It is possible that assessing viral shedding by PCR at a fixed time point after influenza diagnosis is not sufficiently sensitive as an overall measure of antiviral efficacy, and other, more comprehensive or alternative measures might be required. Until the relationship between change in viral shedding and change in symptoms is better understood, the results of this study argue that using primary virologic for clinical endpoints in future trials of promising antiviral agents should be met with appropriate caution. There may be other benefits of reducing viral shedding, such as lower infectivity and decreased emergence of antiviral resistance, although this study was not designed to assess these important public health outcomes. In our population of patients with seasonal influenza, close to one-half of participants stopped shedding virus within 3 days with oseltamivir alone. It is known that patients who are hospitalized with severe influenza and/or other influenza strains such as H5N1 and H7N9 shed higher amounts of virus for longer periods of time. Therefore, it is difficult to know if the lack of clinical benefit in our population would apply to those who are hospitalized with severe influenza or infected with other strains of influenza.
The major limitation to the study is the large percentage of participants (27%) without detectable virus at baseline by qualitative PCR testing at the central laboratory despite having had virus detectable in site testing. This was an unexpected finding as, based on the pilot study, only approximately 5% would have been expected to be negative. With a median of 1 hour between screening and randomization, we do not believe this can be attributed to spontaneous resolution of viral shedding. Between the conclusion of the pilot study and the end of the full study, the study sites were given the option of using newer, more sensitive influenza diagnostic assays. In examining potential causes of the large number of Day 0 negative endpoint specimens, samples of local site influenza diagnostic assays (often processed in 200 mcl or less) were tested and compared to the endpoint specimens (collected in 3 ml viral transport media). In a limited number of site diagnostic assay samples tested by RT-PCR in the central laboratory, many of the site assay samples were indeed positive for influenza though this could not be detected in the baseline central lab sample obtained (data not shown). The unintended consequence of providing more sensitive influenza diagnostic testing to the sites is that, as a result of such factors as viral dilution in transport medium or possible attenuation during shipping, the ability to detect small amounts of virus in the larger endpoint sample may have suffered.
Another limitation is the choice of medications used in the combination arm. At the time of protocol development, there were limited newer antivirals. Amantadine and ribavirin were chosen as they are generic, and if efficacy was demonstrated the combination could have been available at a low cost. However, both amantadine and ribavirin can cause adverse symptoms and intolerances, some of which may have contributed to persistent clinical symptoms. It is possible that newer more effective antivirals with less side effects used in combination could lead to a different clinical outcome.
We demonstrated that the combination of oseltamivir, amantadine, and ribavirin had improved antiviral efficacy over oseltamivir alone in a population at risk for severe disease. However, no clinical symptomatic benefit could be demonstrated with the use of combination antivirals (and by some measures the oseltamivir monotherapy arm was superior). More work is needed to explore and hopefully better understand this lack of a difference between treatments in clinical outcome when a difference in virologic outcome was identified.
Supplementary Material
Panel: Research in context.
Evidence before this study
We searched PubMed in April 2017 for studies using the search terms “combination”, “antivirals” and “influenza”, restricting to the article type of “clinical trials”, and excluded studies that did not study the combination of more than one antiviral, studies that did not evaluate clinical or virologic efficacy (i.e. drug-drug interaction studies), and studies that used combinations targeting the same viral enzyme. Three prior studies were identified. A prior pilot study evaluated combination in 7 immunocompromised patients with influenza A (3 with randomized allocation and 4 given combination antivirals without randomization).22 The authors report the general safety of combination antivirals in this population, but inference of efficacy could not be made. A second study was a retrospective review of 24 patients with influenza H1N1 treated with combination antiviral therapy, and compared to 103 patients receiving oseltamivir monotherapy.23 A lower 14- and 90-day mortality was reported in the combination group than in an oseltamivir monotherapy group (17% vs 35% and 46% vs 59% respectively), though the study was not randomized, did not have standard dosing of the combination antivirals, and did not have uniform inclusion criteria. A third study retrospective review of 6 patients with severe H1N1 treated with combination antivirals, and compared to 8 patients treated with high-dose oseltamivir.24 The clinical outcomes and viral shedding was not significantly different in the treatment arm.
Added value of this study
To our knowledge, this is the largest and most comprehensive study evaluating combination antivirals for the treatment of influenza. Our findings showed that participants with influenza treated with combination antivirals had less viral shedding on Day 3, though there was no benefit in terms of resolution of symptoms or fever, or time to recovery after illness as measured by global assessment questions.
Implications of all the available evidence
The evidence from this study shows that the combination of oseltamivir, amantadine, and ribavirin had improved antiviral efficacy over oseltamivir alone, but there was no evidence of improved clinical outcomes in this population.
Acknowledgments
The study was funded and sponsored by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health, Bethesda, MD. This project has been funded in part with federal funds from the National Cancer Institute, National Institutes of Health, under Contracts HHSN261200800001E and HHSN261201500003I. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
This work was prepared as part of official duties. The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of the Army, Department of the Air Force, Department of Veterans Affairs, Department of Defense, or the U.S. Government.
Adamas Pharmaceuticals provided ribavirin and amantadine (and matching placebo) for the study medication kits.
JH reports stock ownership in Adamas Pharmaceuticals. NM reports employment and stock ownership in in Adamas Pharmaceuticals. Drs Perez-Patrigeon, Losso, Hoopes, and Hughes report receiving funding by subcontracts to National Institute of Allergy and Infectious Diseases for work performed in the conduct of this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors:
JHB, YB, NM, JH, HCL, MDH and RTD were responsible for initial study design, though all authors were involved with subsequent study amendments. JHB, JB, SP-P, GS, MHL, DRB, HPH, JH, and RTD were responsible for study implementation and ongoing management. WM, AS, SMD, JP and RLB enrolled the majority of the participants (all participating sites are noted in the Supplementary Appendix). JB was responsible for monitoring oversight, and SPH was responsible for safety oversight of the study. JH and CM were responsible for the virology testing. JHB, YB, MDH and RTD analyzed and interpreted the data and wrote the first draft of the report though all authors had opportunity to review the data and provided editing of the final report.
Declaration of interests
All authors declare no competing interests.
References
- 1.http://www.cdc.gov/H1N1flu/recommendations.htm - e
- 2.Bautista E, Chotpitayasunondh T, Gao Z, et al. Clinical aspects of pandemic 2009 influenza A (H1N1) virus infection. N Engl J Med. 2010;362(18):1708–19. doi: 10.1056/NEJMra1000449. [DOI] [PubMed] [Google Scholar]
- 3.Galegov GA, Pushkarskaya NL, Obrosova-Serova NP, Zhdanov VM. Combined action of ribovirin and rimantadine in experimental myxovirus infection. Experientia. 1977;33(7):905–6. doi: 10.1007/BF01951273. [DOI] [PubMed] [Google Scholar]
- 4.Ilyushina NA, Hay A, Yilmaz N, Boon ACM, Webster RG, Govorkova EA. Oseltamivir-ribavirin combination therapy for highly pathogenic H5N1 influenza virus infection in mice. Antimicrobial agents and chemotherapy. 2008;52(11):3889–97. doi: 10.1128/AAC.01579-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smee DF, Hurst BL, Wong M-H, Bailey KW, Morrey JD. Effects of double combinations of amantadine, oseltamivir, and ribavirin on influenza A (H5N1) virus infections in cell culture and in mice. Antimicrobial agents and chemotherapy. 2009;53(5):2120–8. doi: 10.1128/AAC.01012-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nguyen JT, Hoopes JD, Le MH, et al. Triple Combination of Amantadine, Ribavirin, and Oseltamivir Is Highly Active and Synergistic against Drug Resistant Influenza Virus Strains In Vitro. PLoS ONE. 2010;5(2):e9332. doi: 10.1371/journal.pone.0009332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hayden FG, Douglas RG, Simons R. Enhancement of activity against influenza viruses by combinations of antiviral agents. Antimicrobial agents and chemotherapy. 1980;18(4):536–41. doi: 10.1128/aac.18.4.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Govorkova EA, Fang H-B, Tan M, Webster RG. Neuraminidase inhibitor-rimantadine combinations exert additive and synergistic anti-influenza virus effects in MDCK cells. Antimicrobial agents and chemotherapy. 2004;48(12):4855–63. doi: 10.1128/AAC.48.12.4855-4863.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smee DF, Bailey KW, Morrison AC, Sidwell RW. Combination treatment of influenza A virus infections in cell culture and in mice with the cyclopentane neuraminidase inhibitor RWJ-270201 and ribavirin. Chemotherapy. 2002;48(2):88–93. doi: 10.1159/000057668. [DOI] [PubMed] [Google Scholar]
- 10.Smee D, Hurst B, Wong M, et al. Effects of Combinations of Favipiravir (T-705) and Oseltamivir on Influenza A (H1N1, H3N2, and H5N1) Virus Infections in Mice. Antimicrobial agents and chemotherapy. 2009 doi: 10.1128/AAC.00933-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ilyushina NA, Hoffmann E, Salomon R, Webster RG, Govorkova EA. Amantadine-oseltamivir combination therapy for H5N1 influenza virus infection in mice. Antivir Ther (Lond) 2007;12(3):363–70. [PubMed] [Google Scholar]
- 12.Galabov AS, Simeonova L, Gegova G. Rimantadine and oseltamivir demonstrate synergistic combination effect in an experimental infection with type A (H3N2) influenza virus in mice. Antivir Chem Chemother. 2006;17(5):251–8. doi: 10.1177/095632020601700502. [DOI] [PubMed] [Google Scholar]
- 13.Leneva IA, Roberts N, Govorkova EA, Goloubeva OG, Webster RG. The neuraminidase inhibitor GS4104 (oseltamivir phosphate) is efficacious against A/Hong Kong/156/97 (H5N1) and A/Hong Kong/1074/99 (H9N2) influenza viruses. Antiviral Research. 2000;48(2):101–15. doi: 10.1016/s0166-3542(00)00123-6. [DOI] [PubMed] [Google Scholar]
- 14.Smee DF, Huffman JH, Morrison AC, Barnard DL, Sidwell RW. Cyclopentane neuraminidase inhibitors with potent in vitro anti-influenza virus activities. Antimicrobial agents and chemotherapy. 2001;45(3):743–8. doi: 10.1128/AAC.45.3.743-748.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smee DF, Wong M-H, Bailey KW, Sidwell RW. Activities of oseltamivir and ribavirin used alone and in combination against infections in mice with recent isolates of influenza A (H1N1) and B viruses. Antivir Chem Chemother. 2006;17(4):185–92. doi: 10.1177/095632020601700403. [DOI] [PubMed] [Google Scholar]
- 16.Ilyushina NA, Bovin NV, Webster RG, Govorkova EA. Combination chemotherapy, a potential strategy for reducing the emergence of drug-resistant influenza A variants. Antiviral Res. 2006;70(3):121–31. doi: 10.1016/j.antiviral.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 17.Nguyen JT, Hoopes JD, Smee DF, et al. Triple combination of oseltamivir, amantadine, and ribavirin displays synergistic activity against multiple influenza virus strains in vitro. Antimicrobial agents and chemotherapy. 2009;53(10):4115–26. doi: 10.1128/AAC.00476-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith S, Blanton L, Kniss K, et al. Update: Influenza Activity - United States. MMWR Morb Mortal Wkly Rep. 2015;64(48):1342–8. doi: 10.15585/mmwr.mm6448a4. [DOI] [PubMed] [Google Scholar]
- 19.Nguyen JT, Smee DF, Barnard DL, et al. Efficacy of combined therapy with amantadine, oseltamivir, and ribavirin in vivo against susceptible and amantadine-resistant influenza A viruses. PLoS One. 2012;7(1):e31006. doi: 10.1371/journal.pone.0031006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Powers JH, Guerrero ML, Leidy NK, et al. Development of the Flu-PRO: a patient-reported outcome (PRO) instrument to evaluate symptoms of influenza. BMC Infect Dis. 2016;16:1. doi: 10.1186/s12879-015-1330-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 2016;4 doi: 10.1177/2050312116671725. 2050312116671725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seo S, Englund JA, Nguyen JT, et al. Combination therapy with amantadine, oseltamivir and ribavirin for influenza A infection: safety and pharmacokinetics. Antivir Ther. 2013;18(3):377–86. doi: 10.3851/IMP2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim WY, Young Suh G, Huh JW, et al. Triple-combination antiviral drug for pandemic H1N1 influenza virus infection in critically ill patients on mechanical ventilation. Antimicrob Agents Chemother. 2011;55(12):5703–9. doi: 10.1128/AAC.05529-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kang SJ, Park KH, Kee SJ, et al. Virological clearance rate of high-dose oseltamivir or triple-combination antiviral therapy in complicated 2009 pandemic influenza A (H1N1) infection. Jpn J Infect Dis. 2013;66(5):425–7. doi: 10.7883/yoken.66.425. [DOI] [PubMed] [Google Scholar]
- 25.Barnard DL. Animal models for the study of influenza pathogenesis and therapy. Antiviral Res. 2009;82(2):A110–22. doi: 10.1016/j.antiviral.2008.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fritz RS, Hayden FG, Calfee DP, et al. Nasal cytokine and chemokine responses in experimental influenza A virus infection: results of a placebo-controlled trial of intravenous zanamivir treatment. J Infect Dis. 1999;180(3):586–93. doi: 10.1086/314938. [DOI] [PubMed] [Google Scholar]
- 27.Lee N, Chan PK, Hui DS, et al. Viral loads and duration of viral shedding in adult patients hospitalized with influenza. J Infect Dis. 2009;200(4):492–500. doi: 10.1086/600383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ison MG, de Jong MD, Gilligan KJ, et al. End points for testing influenza antiviral treatments for patients at high risk of severe and life-threatening disease. J Infect Dis. 2010;201(11):1654–62. doi: 10.1086/652498. [DOI] [PubMed] [Google Scholar]
- 29.U.S. Food and Drug Administration. Guidance for Industry - Influenza: Developing Drugs for Treatment and/or Prophylaxis. U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) 2011 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.