Abstract
Genetic engineering now enables the design of live viral vaccines that are potentially transmissible. Some designs merely modify a single viral genome to improve on the age-old method of attenuation whereas other designs create chimeras of viral genomes. Transmission has the benefit of increasing herd immunity above that achieved by direct vaccination alone but also increases the opportunity for vaccine evolution, which typically undermines vaccine utility. Different designs have different epidemiological consequences but also experience different evolution. Approaches that integrate vaccine engineering with an understanding of evolution and epidemiology will reap the greatest benefit from vaccine transmission.
Keywords: epidemiology, genome engineering, vaccine evolution, population dynamics, herd immunity
Trends
Two types of live viral vaccine are amenable to transmission: attenuated and recombinant vector vaccines.
The epidemiological consequences of vaccine transmission vary with vaccine design and are often case-specific.
Recombinant vector vaccines offer the greatest and least appreciated potential for transmission.
Vaccine evolution is a major issue that stems from transmission and can undermine vaccine utility.
Attenuated vaccines can now be designed that largely suppress evolution; recombinant vectors are prone to evolution.
Vaccine Transmission Is Easier than We Think. Do We Know How to Manage It?
Many viral vaccines in use, and even more being planned, use live viruses 1, 2, 3, 4. When introduced into a patient, they establish a subdued infection that spreads among cells of the host, the infection being sufficient to elicit immunity but not cause disease. Being live, these vaccines are, in principle, capable of transmission to new hosts, although perhaps at a far reduced level compared to viruses capable of causing disease.
The qualitative consequences of vaccine transmission are easy to anticipate: increased herd immunity for a given level of direct vaccination, unintended recipients, and possible vaccine evolution. The quantitative consequences are less obvious, but they are ripe for study. Little attention has been given to vaccine transmission, possibly because transmission is rarely measured and largely unknown in humans except for the oral polio vaccine 3, 5, 6. Whether transmission is indeed rare for other live vaccines, or has merely gone unnoticed, is not clear – polio vaccine transmission is accompanied by evolution to high virulence, creating problems that draw attention to transmission.
Regardless of the transmission capacity of contemporary vaccines, genome engineering has expanded the capacity to create new vaccines far more prone to transmission 1, 3, 7, 8, 9. In some wildlife applications, transmission is even a goal 10, 11, 12, 13, 14, 15. Understanding the ramifications of transmission is now a matter of importance. In this treatise, we bring together results from genome engineering, evolutionary biology, and mathematical epidemiology to discuss the problems and unknowns facing the design, implementation, and outcomes of transmissible vaccines. Our understanding is yet rudimentary, so this document is both a review and a recommendation for new studies. The technology of genome engineering has advanced by leaps, enabling many new transmissible vaccine designs. By contrast, our understanding of the epidemiological and evolutionary ramifications of transmission is in its infancy. Transmissible vaccines are but one set of strategies of transmissible interventions (Box 1), and the general topic offers many exciting opportunities for research and possible implementation.
Box 1. Other Forms of Transmissible Defense.
Advances in genome engineering have created opportunities for other forms of transmissible defenses. Here, we briefly discuss two prominent alternatives.
Viral Defective Interfering Particles
Defective interfering particles (DIPs) are subgenomic derivatives of a fully competent virus and act as parasites of the competent virus. Cells coinfected with the DIP and standard virus vastly overproduce the DIP, and the asymmetry in output leads to an overall reduction in standard viral load 44, 45. Because DIPs suppress viral load, they have long been entertained as therapies for viral diseases 46, 47. A more recent proposal is to engineer DIPs as therapeutic interfering particles (TIPs); any TIP transmission among hosts is a strong potential benefit 48, 49. Thus, TIPs that protect against HIV would not only suppress the disease but would also spread and automatically target superspreaders [7]. Despite the promise of this approach, challenges await. For instance, because DIPs and TIPs require a high density of the competent virus for effective replication, an interfering virus that profoundly suppresses the pathogenic virus – otherwise a good property – will ultimately suppress its own replication, with poor transmission to other hosts.
Gene Drives
Gene drive systems are elements of a genome and thus not ‘infectious’. They nonetheless spread through populations by biasing transmission during sexual reproduction – the classic ‘selfish gene’. Because gene drive systems transmit only vertically from parent to offspring, they spread through a population more slowly than infectious agents. Even so, for short-lived organisms, gene drives provide a powerful mechanism for spreading a particular gene through a population, such as a gene for resistance to malaria in Anopheles mosquitoes 50, 51, 52. Conceptually similar approaches use vertically transmitted bacterial symbionts (genus Wolbachia) that reduce or block transmission of virus from mosquitoes carrying the symbiont 53, 54.
Gene drive (and symbiont based) approaches offer powerful and exciting opportunities for controlling infectious diseases that rely on short-lived vector organisms, or for eliminating infectious disease from animal reservoir populations with short generation times (e.g., hantavirus in deer mice). Compared to transmissible vaccines, gene drive systems have restricted utility: they require sexual reproduction and short generation time and cannot be used in humans.
Alt-text: Box 1
Attenuated Vaccines
Live, attenuated viruses have provided one of the two pillars of vaccine design, the other being inactivated (killed) viruses 3, 4. Recombinant vector vaccines, another form of live vaccines, appear to be a rapidly ascending third pillar (addressed below). Live, attenuated vaccines are genetically ‘weakened’ versions of the wild type. They have a medicinal advantage over killed vaccines in generating an appropriate immune response because they infect cells, and hence can elicit both humoral and cell-mediated defenses. They also infect the same tissues as does the pathogenic wild type.
Historically, a serious drawback of attenuated vaccines has been that haphazard methods were used to create them 4, 16. The virus was grown in unnatural conditions, perhaps novel temperatures, novel hosts, or novel host cells. Adaptation to the new conditions compromised viral growth ability in the natural host – resulting in a viral growth rate reduction that subdued the infection enough to avoid disease. The endpoint of the adaptation was chosen by trial and error, with little insight to the vaccine properties until tested in an actual host. It was thus not feasible to knowingly generate a variety of vaccine candidates differing in the degree of attenuation. Consequently, the range of attenuation compatible with avirulence and immunogenicity was never worked out. But the fact that adequate immunity and avirulence were often achieved by such an imprecise method suggests that the acceptable range of attenuation levels is broad. (Of course, the inoculum dose could always be adjusted to compensate for different levels of attenuation.)
Genetic engineering now affords ‘tunable’ attenuation, enabling the construction of an almost limitless range of intermediates across the spectrum from wild-type growth to zero growth, although the challenge remains to find the right balance between attenuation and immunogenicity [8]. Three promising methods (that do not yield chimeric genomes of different viruses) include synonymous codon replacement, genome rearrangement, and introduction of nonlethal deletions; these methods are considered below.
Synonymous Codon Replacement
Perhaps the most exciting new design is to engineer many synonymous codon changes into viral protein coding sequences; in some cases, the existing codons for each amino acid are merely exchanged with each other, creating new codon pairs but not changing the numbers of each codon 17, 18, 19, 20. The protein sequences are unaltered from the wild type, but protein expression and intracellular growth are reduced (by mechanisms not fully understood but likely involving reduced translation). Greater attenuation is achieved with larger numbers of synonymous codon changes, allowing a very precise tunability. This method can be applied to parts or the whole of any viral genome. This type of attenuation is very slow to recover high fitness.
Genome Rearrangement
A seemingly simple approach is to reorder the genes in a genome; the main effect is likely in gene regulation 21, 22, 23. Tunability is afforded by different rearrangements, but not with the flexibility of codon replacement. Experiments with virus grown in culture suggest that the rearrangements are stable and that seemingly permanent attenuation can be achieved despite ongoing viral growth. This method may be difficult to implement in small genomes and in those expressed as polyproteins.
Deletions
Nonessential genes, or portions of genes, may be removed from the genome to reduce viral growth rate 9, 24, 25. Tunability is afforded by different deletions. Experiments with virus grown in culture suggest that fitness effects of the deletions can be at least partly recovered by evolution, and RNA viruses with deletions have sometimes evolved to restore the lost sequences.
Transmission of attenuated vaccines has not typically been considered in their development – immunogenicity and avirulence were the important concerns and were difficult enough to balance without considering a third variable. The only existing attenuated human vaccine known to be frequently transmitted is the oral polio vaccine, although there are isolated reports of transmission by other attenuated vaccines 6, 26, 27, 28, 29; transmission of vaccines intended for wildlife is well documented in a few cases [15]. The tunability now enabled by genetic engineering may finally allow the deliberate creation of attenuated vaccines that are avirulent and also transmit. Furthermore, if the viral genome carries nonessential genes that effect virulence, deletions may achieve avirulence while allowing transmission. And radically new approaches to attenuation may become feasible that greatly increase transmission above standard methods (Box 2).
Box 2. Virus Attenuation by Changing Tissue Tropism.
Engineering viruses to infect tissues required for transmission, but avoiding tissues involved in virulence, offers a possible viral attenuation design that may enable levels of transmission near wild-type levels. Traditional methods of attenuation have aimed at reducing the within-host viral growth rate, invariably reducing transmission as a by-product. Direct measures of oral polio virus transmission are available [55], but the apparent absence of transmission by many other live vaccines suggests that standard methods of attenuation suppress transmission. Yet, if virulence is due to infection of a secondary tissue – one not essential for transmission – engineering might eliminate virulence (attenuate) by blocking that tropism without harming transmission and thus yield an avirulent but highly transmissible vaccine.
One apparently general method of tissue-specific attenuation is to engineer microRNA response elements (MREs) into the vaccine strain; MREs are sites targeted by host-cell microRNAs that downregulate expression of the targeted gene. If the MREs are targeted only in tissues contributing to virulence, but not other tissues of viral replication, disease phenotypes can be attenuated while vaccine replication is maintained in other tissues 56, 57, 58. The engineered MREs may be prone to evolutionary loss within the host, but some designs can reduce this loss [59], and if the tissues contributing to virulence are not important to transmission (as with the neurotropism of poliovirus [64]), the MREs may even be maintained as the vaccine spreads across hosts.
A conceptually similar approach to MRE engineering is to change other regulatory elements in the viral genome. For example, replacement of the poliovirus internal ribosomal entry site (IRES) by an IRES from rhinoviruses can eliminate CNS tropism [60]. It is likely that the higher frequency of CNS infections by type 1, compared to type 2 and 3, strains is related to different degrees of attenuation at the IRES locus [5].
Observations of natural evolution also support the possibility of attenuation through changes in tissue tropism while maintaining transmission. In pigs, the corona viruses TGEV (transmissible gastroenteritis virus) and PRCV (porcine respiratory corona virus) infect different tissues (the gut and respiratory tract, respectively) despite few genetic differences. This tissue tropism is caused by just two amino acid substitutions in the S spike gene that encodes a glycoprotein essential for attachment to host cells [61]. Although TGEV is more fatal than PRCV, infection by the genetically similar PRCV can provide some protection from TGEV 62, 63. In this case, there seems to be little possibility of the ‘vaccine’ strain (PRCV) evolving back to high virulence. Studying the genetic basis of naturally occurring tissue tropism should inform blueprints for the genetic engineering of vaccines that maintain transmissibility despite low virulence.
Alt-text: Box 2
Recombinant Vector Vaccines
A somewhat new vaccine design is the live recombinant vector vaccine (RVV), a chimera of two viral genomes. There are many flavors of these, and our focus is live, self-replicating vaccines in which the vector is a harmless virus whose genome is left largely intact except for inserts of foreign genes 12, 10, 30, 31, 32, 33, 34, 35, 36, 37, 38. Its genome is engineered to carry one or a few antigenic genes from a pathogen. The goal is to elicit immunity against the pathogen’s antigens, and the vector merely provides the means to amplify those antigens within the host. In contrast to an attenuated vaccine, a ‘recombinant vector’ of this type is intrinsically safe because it carries only a small part of the pathogen’s genome. However, even supposedly benign vectors may be pathogenic in individuals with compromised immune systems, so an RVV may be safe only in some individuals. RVVs have long been used in wildlife applications (e.g., some rabies vaccines), some have entered human trials, and a great many others are being considered. A comprehensive listing of RVVs has been compiled.i
The RVV design is versatile. For any set of pathogen genes, the vector can be chosen from many candidates to be avirulent; methods to engineer reduced virulence while maintaining transmission are unnecessary. Yet because only one or a few genes from the pathogen are engineered into the vector, and the tissues of vaccine infection may differ from those of the pathogen, RVVs risk eliciting only weak immunity. The fact that the pathogen’s genes are not only nonessential to the vector but potentially detrimental to it may allow their rapid evolutionary loss.
Transmissibility may be a common property of live RVVs, whether desired or not. If the vector is capable of autonomous spread, the vaccine is likely to be transmissible as well. The possibility of vector virulence in some classes of individuals becomes a problem because transmission cannot be limited to appropriate recipients the way that direct vaccination can. However, vectors that require an intermediate host for transmission (such as arboviruses) will not transmit if the intermediate host is absent.
Properties of Transmissible Vaccines, and Challenges
The two flavors of transmissible vaccines, RVVs and attenuated vaccines, have different epidemiological and evolutionary properties and consequences. In the four sections below, we explain those properties and the challenges we face in correcting the problems stemming from the consequences.
Viral Genome Engineering Can Influence Transmission
Attenuated vaccines and RVVs present somewhat opposing challenges for the goal of transmission. Attenuated vaccines will be prone to transmit poorly – the reduced growth rate will limit viral titers within the host and thereby limit the dissemination of virions to new hosts (Figure 1, Key Figure). If transmission is desired, it may be necessary to test a range of attenuations to find one that is safe but also transmits, or to use designs that suppress pathogenesis but enable transmission (e.g., Box 2). By contrast, live RVVs may unavoidably transmit because they have the (largely) complete genome of the vector. Engineering may be used to partly disable the vector, thereby limiting transmission, and the use of heterospecific vectors may also effectively block transmission (e.g., a nonhuman vector virus for a human vaccine).
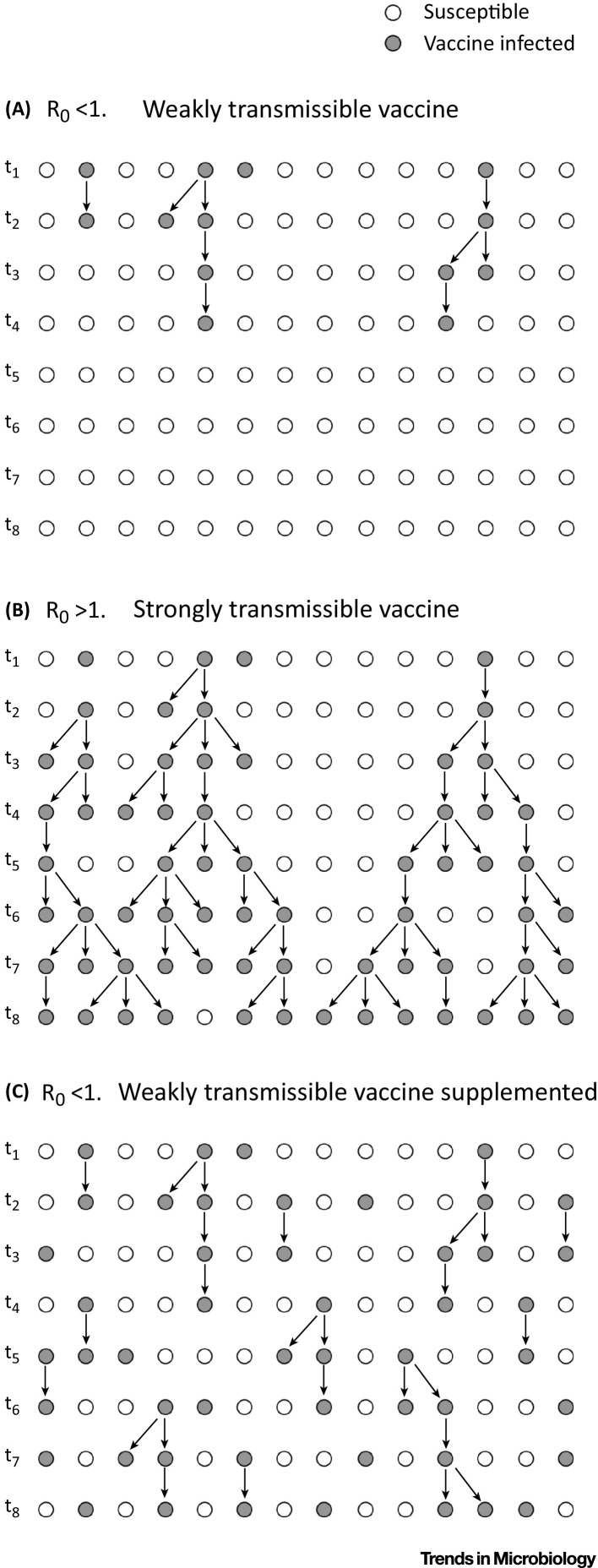
Figure 1.
Key Figure: Basic Epidemiological Properties of Transmissible Vaccines
Each row represents a population at a point in time. Time flows down. Gray circles are individuals with the vaccine, open circles are susceptible. Arrows represent transmission of the vaccine from one individual to another. Directly vaccinated individuals are those with no arrow leading into them. (A) A weakly transmissible vaccine. Direct vaccination occurs in the first time interval shown, and the vaccine quickly dies out. (B) A highly transmissible vaccine; the vaccine spreads. (C) A weakly transmissible vaccine in which direct vaccination continues throughout the time shown. Although chains of transmission are short, they increase the number of vaccinated individuals within the population.
Transmissible Attenuated Vaccines Do Not Persist Indefinitely
Transmission means that a vaccine will sometimes spread to contacts of the vaccinated individuals. Transmission does not ensure vaccine persistence in the population, however. Most transmissible vaccines will simply die out unless continually introduced (Figure 1). A key factor predicting vaccine fate is its basic reproductive number, R0 [39]. If the vaccine R0 is less than 1 – such that the average vaccine-infected person transmits the vaccine to less than one new individual in a naive population – the vaccine is guaranteed to become extinct whenever supplementation stops.
At first glance, this epidemiological result seems to imply that a transmissible vaccine must have R0 > 1 to be an effective tool. This conclusion is misleading for two reasons. First, the transmission from weakly transmissible vaccines (those with R0 < 1) reduces the direct vaccination effort required to eradicate a disease [40], so even weak transmission has a measurable benefit. Second, R0 > 1 is not an assurance of utility: the vaccine may still die out without supplementation. These outcomes can be understood from standard epidemiological models of infectious agents [40].
To address the first point, if the wild-type pathogen’s R0 is denoted R 0,W and the transmissible vaccine’s R0 is denoted R 0,V, the rate at which individuals must be directly vaccinated to eradicate the disease is reduced to a fraction
| [1] |
of vaccinations needed in the absence of transmission – up to R 0,V = R 0,W [40]. For example, if R 0,V = 0.5 R 0,W, then half as many vaccinations are required for a transmissible vaccine as for a nontransmissible vaccine. Any vaccine transmission helps – the ratio is fully indifferent to whether R 0,V is greater or less than 1. The impact of vaccine transmission is merely measured relative to that of the pathogen, and the same R 0,V will have a larger impact for a poorly transmitted pathogen than for a highly transmitted pathogen. The amount of direct vaccination required goes to 0 as the R0 of the vaccine approaches that of the pathogen. As is well known from classical theory, the agent with largest R0 will prevail in the long term [41], so were the vaccine R0 to exceed that of the disease agent, the disease agent would disappear without any intervention beyond the initial introduction of the vaccine (the expression in Equation 1 becomes negative). And this realization also leads to the second point above: whenever the vaccine R0 is less than that of the pathogen’s R0 – even if the vaccine is capable of maintaining itself in a naïve population – the vaccine will die out in the absence of continual supplementation until the pathogen is eradicated.
The pros and cons of transmission go beyond these simple considerations. Aside from the relative biological ease of engineering the combination of avirulence and weak transmission (R0 < 1), weakly transmissible vaccines have the advantage that they do not transmit far beyond the directly vaccinated individuals, so they are less likely to evolve ([42], and see under the heading ‘Vaccine Evolution’, below). On the downside, weakly transmissible vaccines may have such short chains of transmission that they fail to reach isolated or sequestered host individuals and subpopulations any better than a traditional vaccine. Models evaluating the efficacy of such weakly transmissible vaccines in structured host populations will help to determine their useful scope.
RVVs Have a Transmission Advantage over Attenuated Vaccines, but Their Epidemiology Is Complicated
RVVs have one intrinsic advantage over attenuated vaccines – in transmission. Whereas, the transmission (or R0) of an attenuated vaccine will almost assuredly be lower than that of the pathogen, the intrinsic transmission of an RVV may exceed that of the pathogen. An attenuated vaccine and pathogen are essentially the same virus, so the attenuation is likely to suppress transmission. The vector of the RVV and pathogen are different, so there is no constraint on vector transmission. In principle, a vector can even be chosen based on its having a suitably high R0.
Although some epidemiological conclusions described in the previous section apply here, the epidemiology is more complicated for an RVV than for an attenuated vaccine. The challenge for an RVV lies in the presence of two wild-type viruses that will interfere with RVV spread: the pathogen and the vector. The dynamics of a transmissible attenuated vaccine are simple because the vaccine and its pathogen are in direct competition for susceptible hosts: a host previously infected by either the pathogen or vaccine is immune to both. But the competition is limited to the two viruses. With an RVV, there is a three-way interaction because the RVV faces competition from the pathogen and vector. If immunity to the vector is widespread, vaccine transmission may be limited even when the intrinsic vaccine transmission rate is high. RVVs whose vectors have low levels of cross-immunity in the host population will thus benefit the most from transmission.
Choice of the vector will influence several of these critical properties, and indeed may have a profound effect on vaccine success, on vaccine evolution, and on side-effects. In the extreme case of a vector that is not found in the host population (e.g., is from a different species) pre-existing immunity will be absent – a benefit. Transmission may even be avoided by use of a vector from a different species. But use of a vector that already exists in the population has the advantage of a priori known transmission (known R0) and known avirulence. Of course, vector choice will also likely be important to whether the vaccine retains its engineered properties amid within-host evolution and important to the very immunogenicity of the vaccine.
Vaccine Evolution
Release of a transmissible vaccine capable of long-term persistence virtually guarantees that evolution will occur, although that evolution may or may not have important consequences. The poster child for vaccine evolution is the Sabin oral polio vaccine: much of the present-day, disease-causing virus has evolved directly from the vaccine 2, 6. Predicting evolution in detail is problematic, but some evolutionary patterns are expected. First, the virulence of a vaccine is unlikely to evolve above that of its wild-type counterpart. Second, a transmissible vaccine that dies out quickly (e.g., whose R0 < 1) is less likely to evolve than is one that persists long term [42]. This conclusion applies both to viral persistence in populations and in individuals: immune compromised hosts may allow a long-standing infection that leads to evolution within one host [6].
Although the undesirable consequences of evolution differ for attenuated and recombinant vector vaccines (Figure 2), we expect evolution to drive the vaccine back closer to its wild-type phenotype in both cases. Evolution of an attenuated vaccine is thus likely to be toward the higher transmission and virulence of the ancestral, wild-type state. It is thus significant that some engineering methods may greatly thwart or even block evolutionary reversal [9]. Modest levels of vaccine reversion are not a serious setback to eradication when the wild type remains abundant because revertants will be a minor contribution to all infections. By contrast, even infrequent reversion of an attenuated vaccine will preclude its use against a not-yet-present infectious disease where it would have the undesirable consequence of introducing the disease it was designed to block. And reversion thwarts the final steps of eradication [43].
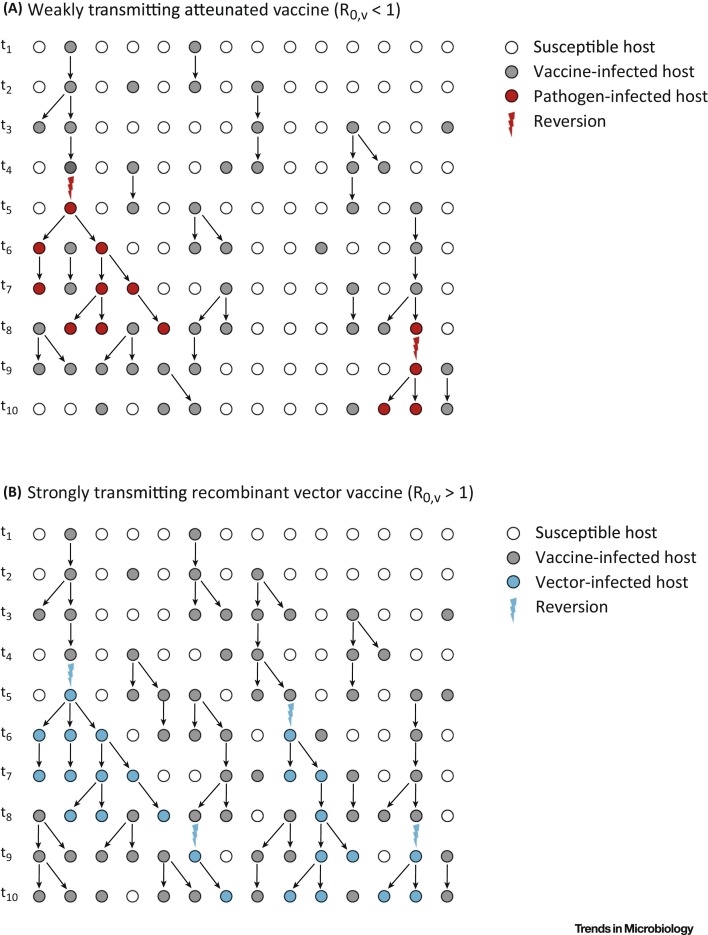
Figure 2.
A Transmissible Vaccine That Occasionally Reverts to Its Wild-Type State. (A) A weakly transmissible attenuated vaccine that reverts. The revertants (red) have high transmissibility, but are suppressed by ongoing vaccination. (B) A highly transmissible recombinant vector vaccine that reverts – loses its antigenic insert (blue). Revertants are also blocked by ongoing vaccination, provided the complete vaccine elicits immunity against both the pathogen and vector.
Evolution of recombinant vector vaccines will also likely favor reversion toward the wild-type phenotype. Rather than increasing virulence, this evolution is likely to introduce ineffective but harmless strains that have ejected or downregulated the antigenic insert (revertants will experience less within-host and herd immunity than the vaccine). When revertant, ‘empty’ vectors circulate within the population they will compete with the vaccine and inhibit its spread through the host population.
Concluding Remarks
Viral genome engineering has opened the door to a new property of live vaccines: transmission among hosts. The vaccine may be for humans or wildlife, and transmission may be intentional or accidental. In addition to possible social objections to human vaccine transmission, there are several biological issues that may lead to unintended consequences or vaccine inefficacy. This Opinion paper has identified many basic questions in understanding how to manipulate and control vaccine transmission, but other exciting questions will quickly present themselves (see Outstanding Questions). Exploiting the possible benefits of transmissible vaccines will require a collaboration between epidemiologists, evolutionary biologists, and genome engineers.
Outstanding Questions.
Current evidence suggests that attenuation is minimally compatible with transmission. Can new engineering methods ensure avirulence (attenuation) but enable more than sporadic transmission?
Transmission of attenuated vaccines may establish subclinical infections and thus weaker immunity and shorter durations of immunity than direct vaccination. How will these different levels of immunity affect the spread of the wild-type pathogen?
Will it be possible to engineer vaccines that can transmit only once (or a finite number of times) but cannot transmit indefinitely?
Does the benefit of transmission depend on whether the vaccine confers immunity versus merely blocking transmission and reducing symptoms of the wild-type virus?
Is it possible to engineer evolutionarily stable recombinant vector vaccines?
Cross-immunity between recombinant vector vaccines and a circulating vector has a large effect on dissemination of the vaccine, and even small levels can be inhibitory. Can we measure small levels of cross immunity?
Acknowledgments
We thank A. Lauring, A. Basinksi, C. Remien, T. Varrelman, R. May, and two reviewers for feedback. We thank Raw Shorts, Inc. and Adobe Systems, Inc. for access to images and animations used in the video abstract (see Supplemental Information online). Supported by NIH GM122079 to SLN.
Footnotes
Supplemental information associated with this article can be found, in the online version, at https://doi.org/10.1016/j.tim.2017.09.007.
Contributor Information
James J. Bull, Email: bull@utexas.edu.
Scott L. Nuismer, Email: snuismer@uidaho.edu.
Resources
Supplemental Information
The following is Supplemental information to this article:
References
- 1.Mackett M. Recombinant live virus vaccines. Immunol. Lett. 1987;16:243–248. doi: 10.1016/0165-2478(87)90153-2. [DOI] [PubMed] [Google Scholar]
- 2.Kew O.M. Vaccine-derived polioviruses and the endgame strategy for global polio eradication. Annu. Rev. Microbiol. 2005;59:587–635. doi: 10.1146/annurev.micro.58.030603.123625. [DOI] [PubMed] [Google Scholar]
- 3.Lauring A.S. Rationalizing the development of live attenuated virus vaccines. Nat. Biotechnol. 2010;28:573–579. doi: 10.1038/nbt.1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hanley K.A. The double-edged sword: How evolution can make or break a live-attenuated virus vaccine. Evolution. 2011;4:635–643. doi: 10.1007/s12052-011-0365-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guest S. Molecular mechanisms of attenuation of the Sabin strain of poliovirus type 3. J. Virol. 2004;78:11097–11107. doi: 10.1128/JVI.78.20.11097-11107.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burns C.C. Vaccine-derived polioviruses. J. Infect. Dis. 2014;210(Suppl 1):S283–S293. doi: 10.1093/infdis/jiu295. [DOI] [PubMed] [Google Scholar]
- 7.Metzger V.T. Autonomous targeting of infectious superspreaders using engineered transmissible therapies. PLoS Comput. Biol. 2011;7:e1002015. doi: 10.1371/journal.pcbi.1002015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galen J.E., Curtiss R. The delicate balance in genetically engineering live vaccines. Vaccine. 2014;32:4376–4385. doi: 10.1016/j.vaccine.2013.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bull J.J. Evolutionary reversion of live viral vaccines: Can genetic engineering subdue it? Virus Evol. 2015;1 doi: 10.1093/ve/vev005. vev005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hardy C.M. Current status of virally vectored immunocontraception for biological control of mice. Soc. Reprod. Fertil. Suppl. 2007;63:495–506. [PubMed] [Google Scholar]
- 11.Hardy C.M. Biological control of vertebrate pests using virally vectored immunocontraception. J. Reprod. Immunol. 2006;71:102–111. doi: 10.1016/j.jri.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 12.Bárcena J. Horizontal transmissible protection against myxomatosis and rabbit hemorrhagic disease by using a recombinant myxoma virus. J. Virol. 2000;74:1114–1123. doi: 10.1128/jvi.74.3.1114-1123.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Torres J.M. First field trial of a transmissible recombinant vaccine against myxomatosis and rabbit hemorrhagic disease. Vaccine. 2001;19:4536–4543. doi: 10.1016/s0264-410x(01)00184-0. [DOI] [PubMed] [Google Scholar]
- 14.Hood G.M. Biological control using sterilizing viruses: host suppression and competition between viruses in non-spatial models. J. Appl. Entomol. 2000;37:914–925. [Google Scholar]
- 15.Murphy A.A. Self-disseminating vaccines for emerging infectious diseases. Expert Rev. Vaccines. 2016;15:31–39. doi: 10.1586/14760584.2016.1106942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fenner, F. and Cairns, J. (1959) Variation in virulence in relation to adaptaton to new hosts. In The Viruses, vol. 3. Animal viruses 3 (Burnet, F.M. and Stanley, W.M., eds), pp. 225–249, Academic Press
- 17.Burns C.C. Modulation of poliovirus replicative fitness in HeLa cells by deoptimization of synonymous codon usage in the capsid region. J. Virol. 2006;80:3259–3272. doi: 10.1128/JVI.80.7.3259-3272.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mueller S. Reduction of the rate of poliovirus protein synthesis through large-scale codon deoptimization causes attenuation of viral virulence by lowering specific infectivity. J. Virol. 2006;80:9687–9696. doi: 10.1128/JVI.00738-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coleman J.R. Virus attenuation by genome-scale changes in codon pair bias. Science. 2008;320:1784–1787. doi: 10.1126/science.1155761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bull J.J. Slow fitness recovery in a codon-modified viral genome. Mol. Biol. Evol. 2012;29:2997–3004. doi: 10.1093/molbev/mss119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wertz G.W. Gene rearrangement attenuates expression and lethality of a nonsegmented negative strand RNA virus. Proc. Natl. Acad. Sci. U. S. A. 1998;95:3501–3506. doi: 10.1073/pnas.95.7.3501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flanagan E.B. Rearrangement of the genes of vesicular stomatitis virus eliminates clinical disease in the natural host: new strategy for vaccine development. J. Virol. 2001;75:6107–6114. doi: 10.1128/JVI.75.13.6107-6114.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cecchini N. Evolutionarily stable attenuation by genome rearrangement in a virus. G3 Bethesda Md. 2013;3:1389–1397. doi: 10.1534/g3.113.006403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berkhout B. Genetic instability of live, attenuated human immunodeficiency virus type 1 vaccine strains. J. Virol. 1999;73:1138–1145. doi: 10.1128/jvi.73.2.1138-1145.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Licis N. Forced retroevolution of an RNA bacteriophage. Virology. 2000;271:298–306. doi: 10.1006/viro.2000.0327. [DOI] [PubMed] [Google Scholar]
- 26.Kew O. Reaching the last one per cent: progress and challenges in global polio eradication. Curr. Opin. Virol. 2012;2:188–198. doi: 10.1016/j.coviro.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 27.Mallory R.M. Shedding of Ann Arbor strain live attenuated influenza vaccine virus in children 6–59 months of age. Vaccine. 2011;29:4322–4327. doi: 10.1016/j.vaccine.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 28.Anderson E.J. Rotavirus vaccines: viral shedding and risk of transmission. Lancet Infect. Dis. 2008;8:642–649. doi: 10.1016/S1473-3099(08)70231-7. [DOI] [PubMed] [Google Scholar]
- 29.Otrashevskaia E.V. [Mumps vaccine virus transmission] Vopr. Virusol. 2013;58:42–45. [PubMed] [Google Scholar]
- 30.Wu X., Rupprecht C.E. Glycoprotein gene relocation in rabies virus. Virus Res. 2008;131:95–99. doi: 10.1016/j.virusres.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 31.Hansen S.G. Profound early control of highly pathogenic SIV by an effector memory T-cell vaccine. Nature. 2011;473:523–527. doi: 10.1038/nature10003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Naim H.Y. Applications and challenges of multivalent recombinant vaccines. Hum. Vaccines Immunother. 2013;9:457–461. doi: 10.4161/hv.23220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Navarro A. Generation of genetically stable recombinant rotaviruses containing novel genome rearrangements and heterologous sequences by reverse genetics. J. Virol. 2013;87:6211–6220. doi: 10.1128/JVI.00413-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ranasinghe S., Walker B.D. Programming CMV for vaccine vector design. Nat. Biotechnol. 2013;31:811–812. doi: 10.1038/nbt.2688. [DOI] [PubMed] [Google Scholar]
- 35.Dong B. An overview of live attenuated recombinant pseudorabies viruses for use as novel vaccines. J. Immunol. Res. 2014;2014 doi: 10.1155/2014/824630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ljungberg K., Liljeström P. Self-replicating alphavirus RNA vaccines. Expert Rev. Vaccines. 2015;14:177–194. doi: 10.1586/14760584.2015.965690. [DOI] [PubMed] [Google Scholar]
- 37.Wu X.-X. Ebolavirus vaccines: progress in the fight against Ebola virus disease. Cell. Physiol. Biochem. 2015;37:1641–1658. doi: 10.1159/000438531. [DOI] [PubMed] [Google Scholar]
- 38.Quinn M. Cytomegalovirus and immunotherapy: opportunistic pathogen, novel target for cancer and a promising vaccine vector. Immunotherapy. 2016;8:211–221. doi: 10.2217/imt.15.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Anderson R.M., May R.M., editors. Infectious Diseases of Humans: Dynamics and Control. Oxford University Press; 1992. [Google Scholar]
- 40.Nuismer S.L. Eradicating infectious disease using weakly transmissible vaccines. Proc. Biol. Sci. 2016;283 doi: 10.1098/rspb.2016.1903. 20161903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lenski R.E. Dynamics of interactions between bacteria and virulent bacteriophage. Adv. Microb. Ecol. 1988;10:1–44. [Google Scholar]
- 42.Antia R. The role of evolution in the emergence of infectious diseases. Nature. 2003;426:658–661. doi: 10.1038/nature02104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kew O.M. Reaching the last one per cent: progress and challenges in global polio eradication. Curr. Opin. Virol. 2012;2:188–198. doi: 10.1016/j.coviro.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 44.Von Magnus P. Incomplete forms of influenza virus. Adv. Virus Res. 1954;2:59–79. doi: 10.1016/s0065-3527(08)60529-1. [DOI] [PubMed] [Google Scholar]
- 45.Huang A.S. Defective interfering viruses. Annu. Rev. Microbiol. 1973;27:101–117. doi: 10.1146/annurev.mi.27.100173.000533. [DOI] [PubMed] [Google Scholar]
- 46.Doyle M., Holland J.J. Prophylaxis and immunization in mice by use of virus-free defective T particles to protect against intracerebral infection by vesicular stomatitis virus. Proc. Natl. Acad. Sci. U. S. A. 1973;70:2105–2108. doi: 10.1073/pnas.70.7.2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dimmock N.J., Easton A.J. Defective interfering influenza virus RNAs: time to reevaluate their clinical potential as broad-spectrum antivirals? J. Virol. 2014;88:5217–5227. doi: 10.1128/JVI.03193-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Notton T. The case for transmissible antivirals to control population-wide infectious disease. Trends Biotechnol. 2014;32:400–405. doi: 10.1016/j.tibtech.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 49.Tanner E.J. Exploiting genetic interference for antiviral therapy. PLoS Genet. 2016;12:e1005986. doi: 10.1371/journal.pgen.1005986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ito J. Transgenic anopheline mosquitoes impaired in transmission of a malaria parasite. Nature. 2002;417:452–455. doi: 10.1038/417452a. [DOI] [PubMed] [Google Scholar]
- 51.Windbichler N. A synthetic homing endonuclease-based gene drive system in the human malaria mosquito. Nature. 2011;473:212–215. doi: 10.1038/nature09937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gantz V.M., Bier E. Genome editing. The mutagenic chain reaction: a method for converting heterozygous to homozygous mutations. Science. 2015;348:442–444. doi: 10.1126/science.aaa5945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Osborne S.E. Antiviral protection and the importance of Wolbachia density and tissue tropism in Drosophila simulans. Appl. Environ. Microbiol. 2012;78:6922–6929. doi: 10.1128/AEM.01727-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Turley A.P. Wolbachia infection reduces blood-feeding success in the dengue fever mosquito, Aedes aegypti. PLoS Negl. Trop. Dis. 2009;3:e516. doi: 10.1371/journal.pntd.0000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Duintjer Tebbens R.J. Expert review on poliovirus immunity and transmission. Risk Anal. 2013;33:544–605. doi: 10.1111/j.1539-6924.2012.01864.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Barnes D. Harnessing endogenous miRNAs to control virus tissue tropism as a strategy for developing attenuated virus vaccines. Cell Host Microbe. 2008;4:239–248. doi: 10.1016/j.chom.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kelly E.J. Attenuation of vesicular stomatitis virus encephalitis through microRNA targeting. J. Virol. 2010;84:1550–1562. doi: 10.1128/JVI.01788-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ylösmäki E. Attenuation of Semliki Forest virus neurovirulence by microRNA-mediated detargeting. J. Virol. 2013;87:335–344. doi: 10.1128/JVI.01940-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Teterina N.L. Silencing of neurotropic flavivirus replication in the central nervous system by combining multiple microRNA target insertions in two distinct viral genome regions. Virology. 2014;456–457:247–258. doi: 10.1016/j.virol.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gromeier M. Internal ribosomal entry site substitution eliminates neurovirulence in intergeneric poliovirus recombinants. Proc. Natl. Acad. Sci. U. S. A. 1996;93:2370–2375. doi: 10.1073/pnas.93.6.2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ballesteros M.L. Two amino acid changes at the N-terminus of transmissible gastroenteritis coronavirus spike protein result in the loss of enteric tropism. Virology. 1997;227:378–388. doi: 10.1006/viro.1996.8344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cox E. Intestinal protection against challenge with transmissible gastroenteritis virus of pigs immune after infection with the porcine respiratory coronavirus. Vaccine. 1993;11:267–272. doi: 10.1016/0264-410X(93)90028-V. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Saif L.J. Immunity to transmissible gastroenteritis virus and porcine respiratory coronavirus infections in swine. Vet. Immunol. Immunopathol. 1994;43:89–97. doi: 10.1016/0165-2427(94)90124-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bodian D., Horstmann D.M. Viral and Rickettsial Infections of Man. 4th edn. J. P. Lippincott; 1965. Polioviruses; pp. 430–473. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.