Short abstract
Background
Limited data exist on the prevalence and distribution of sedentary behavior (SB) in multiple sclerosis (MS).
Objective
The objective of this paper is to describe sitting time as a metric of SB in a large national sample of people with MS.
Methods
A total of 8004 individuals from the North American Research Committee on MS (NARCOMS) Registry completed the sitting time question from the International Physical Activity Questionnaire in spring 2015. We present descriptive data on sitting time for the total sample and across sociodemographic, clinical, and behavioral characteristics.
Results
The final sample included 6483 individuals. Of these, 36.7% were classified with mild disability, 24.7% with moderate disability, and 38.6% with severe disability. Median sitting time for the total sample was 480 min/day (P25 = 310 min/day, P75 = 720 min/day). Sitting time was highest for individuals with MS who were male (540 min/day), not married (540 min/day), had a disease duration >30 years (540 min/day), were underweight (540.5 min/day), had an annual income of < $15,000 (585 min/day), presented with a progressive form of MS (600 min/day), were classified as insufficiently active (600 min/day), or presented with severe disability (661 min/day).
Conclusion
Sitting time is twice as high in individuals with MS compared to the general population (240 min/day).
Keywords: Sedentary behavior, prevalence, epidemiology, adult, multiple sclerosis
Introduction
Sedentary behavior (SB) has been defined as any waking activities performed while sitting or lying that do not increase energy expenditure above 1.5 metabolic equivalents of task (METs; one MET being the resting metabolic rate).1 Sitting, in particular, has become an increasingly prevalent form of SB in modern society. Epidemiologic data from different countries indicate that adults typically spend five hours per day or more sitting.2 Excessive time spent in SB is concerning because it has been associated with increased risk of chronic diseases including diabetes,3 cardiovascular disease,4,5 obesity,6 and cancer7 in the general adult population.
To date, there are minimal data regarding sitting time among individuals with disabling conditions that limit mobility8 such as multiple sclerosis (MS).9 The focus on MS is important, as its manifestations such as walking and balance dysfunctions, muscle weakness, fatigue, pain, and depression may increase the likelihood of spending more time sitting.9 The common recommendation that people with MS should rest periodically for energy conservation and avoiding fatigue10 may result in an elevated amount of sitting time. We recognize that larger amounts of sitting time in MS might have considerable benefit for fatigue management, but this could actually aggravate the disease in the long term, if excessive sitting increases the likelihood of comorbidities as it has in the general population.3–7 In MS, we are aware of one study linking sitting time with blood pressure.11 Comorbidities could accelerate disease progression9 and result in a vicious cycle among manifestations of MS, SB, comorbidity, and disease progression. Whereas studies examining those associations are necessary to establish if SB has deleterious effects in patients with MS, a current priority is to determine the prevalence of this behavior in MS. This will be the first step to map out the possible SB issue in MS.
Population-based estimates of sitting time in adults with MS are limited. We are aware of one study that examined sitting time in individuals with MS versus controls.12 The study reported no differences between groups, although both reported substantial sitting time.12 However, the estimates were not derived from a nationally representative sample and this precludes assumptions about the prevalence of SB in individuals with MS. The provisions of estimates from a large national sample of MS patients are important for allowing comparisons with the general population, describing the distribution across segments of the population with MS, as well as informing and guiding future directed efforts toward reducing SB in MS at large.
The importance of obtaining large-scale data on SB in MS has become evident,9 but the operationalization for doing so has been complex. Epidemiologic data on sitting time in people with MS in the United States of America (USA) and abroad are currently scarce, yet such data are available for the general population of adults in the USA and worldwide.2,13 To address this gap in knowledge, we included a standard question on sitting time from the abbreviated International Physical Activity Questionnaire (IPAQ)14 in the semi-annual survey of the North American Research Committee on MS (NARCOMS) Registry. In this study, we report the descriptive statistics of sitting time obtained from that survey in overall terms and based on sociodemographic, clinical, and behavioral variables, for characterization and understanding of SB in individuals with MS.
Methods
The NARCOMS Registry is a voluntary, self-report registry developed by the Consortium of MS Centers (CMSC) wherein participants with MS complete an enrollment questionnaire and semi-annual surveys. Participants typically provide information regarding sociodemographic, clinical, and behavioral characteristics. The current study reports on data obtained from the semi-annual survey of spring 2015 and analyzed in April–May 2017. A total of 8004 individuals with MS completed the survey that included the IPAQ question on sitting time. Permission for using the dataset was granted by NARCOMS and the study was approved by the Institutional Review Board of the University of Alabama at Birmingham. We included sociodemographic, clinical, and behavioral variables that have been previously examined as potential correlates of sitting time in the general population and/or patients with MS.12,15–17 Since the investigation of SB in MS is relatively new, we have taken an exploratory approach in selecting the variables for this study, wherein even those variables that have not been significantly correlated with sitting time in previous studies were included in the analyses.
Sociodemographic variables
Sociodemographic variables included sex, body mass index (BMI) calculated from self-reported height and weight, age, race, marital status, education, employment, and annual household income. BMI was used to classify individuals as normal weight (18.5–24.9 kg/m2), overweight/obese (>25 kg/m2), or underweight (<18.5 kg/m2). The original response options for race included 15 options; however, in the dataset we had access to from NARCOMS, race classifications were: (a) White, (b) Black, (c) Multi-race, and (d) other. For this study, answers were re-categorized into: (a) Caucasian (White) and (b) other (Black, Multi-race, and other). Marital status was originally reported as: (a) never married, (b) married, (c) divorced, (d) widowed, (e) separated, or (f) cohabitating/domestic partner. These categories were combined into: (a) never married, (b) married/cohabitating/domestic partner, and (c) divorced/widowed/separated. For education, possible answers were: (a) high school, (b) associate degree, (c) bachelor, (d) post-graduate, and (e) technical degree. These categories remained the same with the exception of the combination of associate and technical degree. Employment status was reported as one of the following: (a) yes, full time, (b) yes, part time, or (c) no. Answers were re-categorized into either (a) yes, or (b) no. As for annual household income, possible responses were: (a) less than $15,000, (b) $15,001–$30,000, (c) $30,001–$50,000, (d) $50,001–$100,000, (e) over $100,000, and (f) “I do not wish to answer.” The latter was eliminated and the categories “$50,001–$100,000” and “over $100,000” were combined into a category of >$50,000. The other categories remained the same.
Clinical variables
The clinical variables included in this study were MS course, disease duration, and disability status. MS course was categorized as: (a) clinically isolated syndrome, (b) relapsing–remitting, (c) secondary progressive, (d) primary progressive, and (e) don’t know/unsure. Disease duration was categorized into four groups: (a) 0–10 years, (b) 11–20 years, (c) 21–30 years, and d) >30 years. Disability status was assessed using the Patient-Determined Disease Steps (PDDS), a patient-reported measure of disability level on an ordinal scale that ranges from 0 (normal) to 8 (bedridden). We used the nine ordinal levels and clustered the scores into those with mild (PDDS = 0 to 2), moderate (PDDS = 3 and 4), and severe (PDDS ≥5) disability.18 The PDDS has been previously validated in individuals with MS.19
Behavioral variables
Smoking status was assessed with following question “Do you smoke now?” Response options were (a) “No, not at all,” (b) “Yes, some days,” and (c) “Yes, every day.” These answers were further reduced to a binary category (no or yes). Regarding physical activity (PA), we included the questions on weekly frequency of moderate and vigorous PA from the abbreviated IPAQ. We computed a Health Contribution Score using the criteria typically applied to the Godin Leisure-Time Exercise Questionnaire, wherein the frequency of moderate PA was multiplied by five METs and frequency of vigorous PA was multiplied by nine METs.20 We then summed the two values into a single value. This value was used to classify participants as sufficiently active if score was ≥24 units, moderately active for a score of 14–23 units, and insufficiently active if score was <14 units.21
Sitting time
We included the question on sitting time from the abbreviated IPAQ.22 The sitting item from IPAQ has been validated in participants from the general population using accelerometry as the criterion method.22 The correlation coefficient between IPAQ-derived sitting time and accelerometer-derived SB was r = 0.34.22 The question itself assesses the number of hours and minutes (min) spent sitting on a usual weekday (i.e., “During the last 7 days, how much time did you usually spend sitting on a weekday?”). The question preface includes prompts and examples for reminding participants to consider multiple domains (e.g., work, home) and activities (e.g., sitting at a desk, lying down to watch television) when recalling total sitting time.
Data analyses
Data analyses were carried out using the IBM SPSS Statistics (IBM Corporation), version 24.0, Mac OS X. Data normality was examined using the Kolmogorov–Smirnov test, which indicated non-normal distribution across variables. Sitting time therefore was reported as median, 25th percentile (P25), and 75th percentile (P75) for the total sample and based on the sociodemographic (sex, BMI, age, race, marital status, education, employment, and annual household income), clinical (MS course, disease duration, and disability status), and behavioral categories (smoking status and PA classification). We examined differences in the distribution of sitting time between or among variable categories using the nonparametric median test. Statistically significant differences were considered present at the level of p < 0.05. For variables with three or more categories (n = 9), we further applied post hoc pairwise comparisons to determine the location of the differences. Bonferroni corrections for multiple tests were applied variable-wise for determining statistical significance (α/number of comparisons). Further testing was conducted to examine differences in sitting time according to PDDS scores by also using the nonparametric median test and post hoc follow-up tests with Bonferroni corrections for statistical significance.
Results
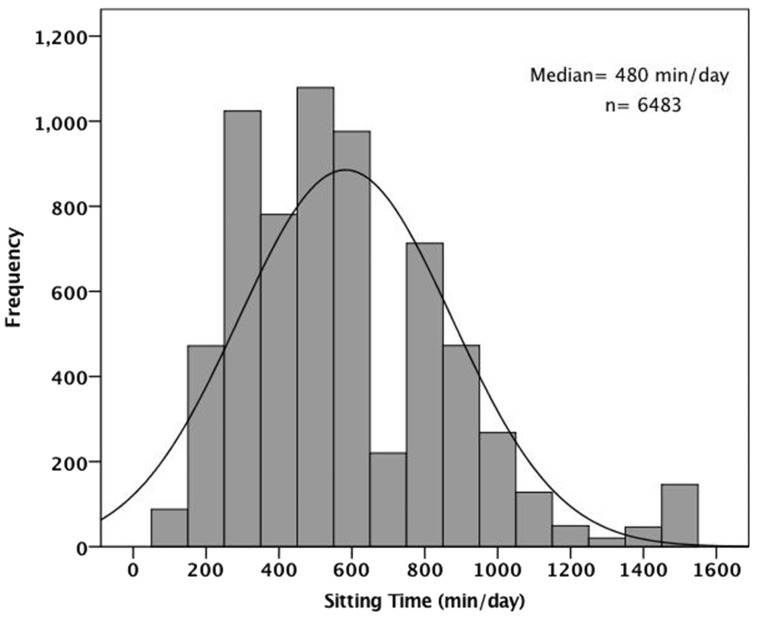
Of the 8004 participants, 1521 were excluded based on missing data for sitting time or impossible/unlikely values for sitting time (i.e., zero min/day) and/or body weight (i.e., <30 kg). Frequency distributions for all variables, except for PA classification, were significantly different between included and excluded participants (data not presented). However, the percentages of individuals for each category were very close between the groups. Data from the 6483 participants included in the study yielded a median sitting time estimate of 480 min/day (P25 = 310 min/day, P75 = 720 min/day) (Figure 1 and Table 1). The frequency distribution for sitting time revealed that most participants reported values between 300 and 600 min/day (Figure 1). There was a bimodal trend in the distribution curve of the sitting time estimates (Figure 1).
Figure 1.
Histogram depicting the frequency distribution for sitting time.
Table 1.
Median (P50), 25th percentile (P25) and 75th percentile (P75) of sitting time according to different demographic, clinical, and behavioral characteristics.
|
Sitting time |
|||||
|---|---|---|---|---|---|
| Characteristic | n | Median (P50) | P25 | P75 | p value |
| Total | 6483 | 480 | 310 | 720 | – |
| Sex | |||||
| Female | 5043 | 480 | 300 | 720 | <0.001 |
| Male | 1439 | 540 | 360 | 750 | |
| Race | |||||
| Other | 427 | 480 | 300 | 630 | 0.164 |
| Caucasian | 5947 | 480 | 315 | 720 | |
| Age | |||||
| <40 years | 235 | 480 | 360 | 601 | 0.883 |
| 40–49 years | 773 | 480 | 300 | 660 | |
| 50–59 years | 1917 | 480 | 330 | 720 | |
| 60–69 years | 2531 | 480 | 301 | 720 | |
| ≥70 years | 1023 | 480 | 300 | 720 | |
| BMI classification | |||||
| Normal weight | 2565 | 480 | 300 | 720 | <0.001 |
| Overweight/Obese | 3559 | 481a | 360 | 720 | |
| Underweight | 206 | 540.5a | 360 | 780 | |
| Marital status | |||||
| Never married | 578 | 540b | 360 | 720 | <0.001 |
| Married/Cohabitating/Domestic partner | 4488 | 480 | 300 | 720 | |
| Divorced/Widowed/Separated | 1368 | 540b | 360 | 720 | |
| Employment status | |||||
| Employed | 2136 | 480 | 330 | 602.5 | 0.024 |
| Unemployed | 4268 | 480 | 301 | 720 | |
| Education | |||||
| High school | 632 | 480 | 360 | 720 | 0.011 |
| Associate or technical | 2353 | 480c | 330 | 720 | |
| Bachelor | 1407 | 480 | 300 | 720 | |
| Post-Graduate | 1721 | 480 | 330 | 720 | |
| Annual household income | |||||
| <$15,000 | 422 | 585d | 348.75 | 780 | 0.002 |
| $15,001–$30,000 | 868 | 480 | 330 | 720 | |
| $30,001–$50,000 | 1003 | 480 | 330 | 720 | |
| >$50,000 | 2821 | 480 | 315 | 720 | |
| MS course | |||||
| Clinically isolated syndrome/Other | 159 | 420e | 300 | 600 | <0.001 |
| Relapsing–remitting | 3617 | 470e | 300 | 600 | |
| Secondary progressive | 1407 | 600e,f,g | 420 | 840 | |
| Primary progressive | 701 | 600e,f,g | 420 | 840 | |
| Do not know/Unsure | 547 | 482f | 300 | 720 | |
| Disease duration | |||||
| 0–10 years | 811 | 480 | 305 | 600 | <0.001 |
| 11–20 years | 2501 | 480h | 300 | 720 | |
| 21–30 years | 1883 | 509h,i | 335 | 720 | |
| >30 years | 937 | 540i | 360 | 780 | |
| Disability status | |||||
| Mild | 2372 | 390 | 270 | 600 | <0.001 |
| Moderate | 1593 | 480j | 300 | 600 | |
| Severe | 2491 | 661j | 480 | 900 | |
| Smoker | |||||
| No | 5836 | 480 | 310 | 720 | 0.863 |
| Yes | 595 | 480 | 330 | 720 | |
| Physical activity classification | |||||
| Sufficiently active | 1789 | 360 | 240 | 550 | <0.001 |
| Moderately active | 889 | 480k | 300 | 600 | |
| Insufficiently active | 3712 | 600k | 360 | 780 | |
aSignificantly different from Normal weight group.
bSignificantly different from Married/Cohabitating/Domestic partner group.
cSignificantly different from Bachelor group.
dSignificantly different from >$50,000 group.
eSignificantly different from Do not know/Unsure group.
fSignificantly different from Clinically isolated syndrome/Other group.
gSignificantly different from Relapsing–Remitting group.
hSignificantly different from 0–10 years group.
iSignificantly different from 11–20 years group.
jSignificantly different from Mild group.
kSignificantly different from Sufficiently active group.
BMI: body mass index; MS: multiple sclerosis.
Median sitting time across all variables ranged from 360 min/day to 661 min/day (Table 1). The frequency distributions of sitting time were not statistically significantly different across categories of race, age, and smoking status. There were significant differences in the distribution of sitting time across categories for sex, BMI classification, marital status, employment status, education, annual household income, MS course, disease duration, disability status, and PA classification (Table 1). For those variables with three or more categories, the locations of the differences are presented in Table 1. Of note, for disease duration, distributions for the 11–20 years and 21–30 years categories were significantly different from that of the 0–10 years category. Significant differences were also observed for the 21–30 years and >30 years categories compared to the 0–10 years category. For disability status, the categories of moderate and severe disability significantly differed from the mild disability category. Regarding PA classification, distributions of sitting time from the moderately active and insufficiently active categories were significantly different from the sufficiently active category.
Overall, sitting time was highest for individuals with MS who were male (540 min/day), not married (540 min/day), had a disease duration >30 years (540 min/day), were underweight (540.5 min/day), had an annual income of < $15,000 (585 min/day), presented with a progressive form of MS (600 min/day), were classified as insufficiently active (600 min/day), or presented with severe disability (661 min/day).
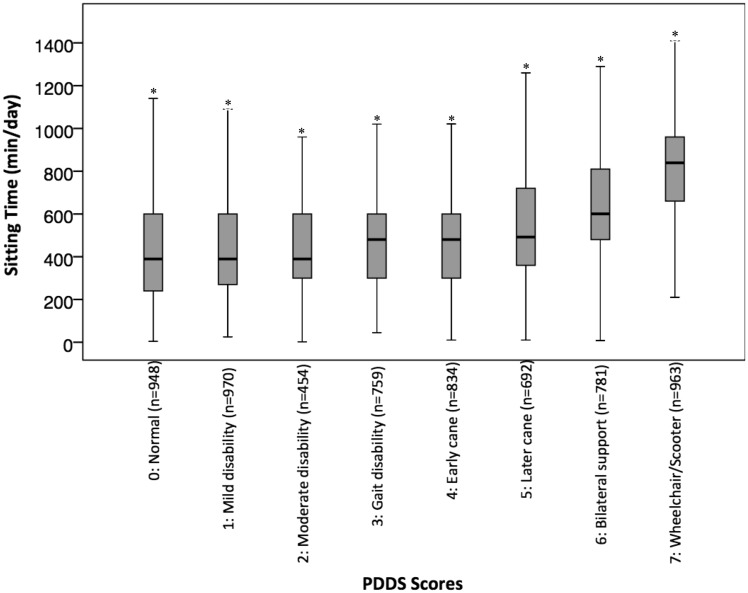
We further examined sitting time across PDDS scores, with the exception of the PDDS score of 8, as there were too few participants in this category (n = 55). Data indicated increasing median sitting times with higher PDDS scores (Figure 2). Those individuals with normal gait (PDDS = 0) reported sitting for 390 min/day, and those relying on a wheelchair/scooter (PDDS = 7) reported sitting for 840 min/day (Figure 2). There were statistically significantly differences in the distributions of sitting time among all categories of disability.
Figure 2.
Median, interquartile range, and minimum and maximum sitting time values according to Patient-Determined Disease Steps score.
*Distribution is significantly different from the other categories.
Discussion
This is the first study to present sitting time estimates for adults with MS from a large national sample. We presented median sitting times in MS based on an array of sociodemographic, clinical, and behavioral characteristics. The results indicated that North American adults with MS report spending twice as much time sitting (480 min/day) compared with normative data from the general population of North Americans (i.e., 240 min/day).2 This ratio remains similar when comparing sitting times across the different age groups from this study (480 min/day for all age groups) with adults from the general population aged 18–39 and 40–65 years (in both cases 240 min/day).2 When examined by sex, sitting time estimates from this study indicate that women with MS sit for approximately 480 min/day, whereas men with MS sit for approximately 540 min/day. Normative values for the general population indicate that men and women sit for approximately 240 min/day.2
Of note, self-reported sitting time for patients with severe disability (PDDS ≥ 5) was almost three times higher than that of an average North American individual (661 vs 240 min/day).2 This suggests that the substantially higher sitting time in people with MS may be partly due to gait impairment, which is common in this condition.8,9 Our results indicate that those classified with mild disability reported sitting for approximately 390 min/day, whereas those with moderate and severe disability spent approximately 480 and 661 min/day sitting, respectively. Further examination of sitting time based on PDDS scores indicated that the PDDS score of 3 (gait disability) emerged as the point at which estimates of sitting time become markedly higher compared with normal gait (PDDS = 0). This suggests that reducing sitting time before or at the stage of gait disability may be fundamental for interrupting and/or decelerating the possible vicious cycle of SB and functional limitations in MS.
Our line of reasoning somewhat conflicts with current energy management strategies for fatigue in MS—reducing energy expenditure by lowering engagement in physically demanding activities, taking regular rest breaks, and using assistive technologies for ambulation.10 A high level of SB may increase the risk of developing comorbid conditions in MS, which may in turn accelerate disease progression over time. Indeed, significant associations of SB with different comorbidities, including diabetes, cancer, and cardiovascular disease, have been documented in the general population.3–5,7 These associations are concerning in MS, as comorbidities may accelerate disease progression.9 However, symptoms such as fatigue may require periodic rest, especially in those individuals presenting with gait impairment as fall risk may increase with fatigue, which consequently increases engagement in SB. This suggests that education regarding the benefits of PA and risks of SB must occur early in the MS disease course, and that effective strategies to address these issues need to be in place before MS symptoms become limiting factors. Moreover, the recommendations for acceptable sitting time and PA may vary over the course of the disease, and strategies to address them may need to be modified.
In this study, we identified a tendency for a bimodal curve in the distribution of sitting time (Figure 1) that is possibly related to the existence of clusters of associated factors that characterize two groups with distinct sitting behavior. Whereas the distribution of sitting time according to the sociodemographic, clinical, and behavioral characteristics provide some indications, further studies are needed to specifically examine the predictors of excessive sitting in this sample of adults with MS. This is important because, according to our results, disability status appears to be the leading factor associated with sitting time in individuals with MS. Future studies examining predictors of sitting time in MS will need to control for disability status or stratify association measures between sitting time and its predictors by disability categories. Another logical step will be to conduct associational studies in MS to better understand the potential deleterious associations of SB with health outcomes in this population. This will potentially inform and guide future interventions aiming at reducing SB in individuals with MS.
Finally, an important result of the current study pertains to the prevalence of sitting time in participants with different PA levels. The current literature suggests that SB and PA are independent behaviors;1 however, it is particularly interesting that highest sitting time was observed for the insufficiently active group. Such a finding suggests that, in MS, insufficiently active individuals may be the most concerning group in terms of SB. This group is exposed to both the detrimental effects of physical inactivity and SB on health. Therefore, interventions for insufficiently active individuals may need to target both interruptions in SB and replacement with PA. Studies have demonstrated that breaks in sedentary time are related to better metabolic and cardiovascular health.5,23,24 Epidemiological data further indicate that, in the general population, one hour per day of moderate to vigorous PA attenuates or even eliminates the increased risk of death resulting from excessive daily sitting.25 Collectively, these findings suggest that reducing SB and increasing PA may maximize health benefits particularly in those with more severe disability, as this group was identified as the one reporting the highest time spent sitting among all the other categories.
This study has limitations. We used a self-report instrument to assess SB. Self-report instruments are subject to recall bias and this is especially concerning in patients with MS, since they are more prone to cognitive limitations.26 The use of objective monitoring could result in more accurate measures of SB in this population; yet, a vast literature in the general population has evolved around the use of self-report estimates.2,13,25,27–29 Another limitation of our study was the inability to obtain daily patterns of SB; we simply provide an estimate of total volume. Future studies using accelerometry might be able to tackle this limitation and generate knowledge on the length of SB bouts, number of breaks in daily sedentary time, as well as time of day with greater prevalence of SB in individuals with MS. Nonetheless, our results will remain important, given that self-report instruments will continue to be used in epidemiological studies. The present study included a large sample of people with MS, but our results may not be generalizable to groups of the population that are underrepresented in the NARCOMS Registry (e.g., minorities, low-income, adults <40 years old). This should be addressed in future investigations. A final limitation of our study was the substantial data loss (i.e., 1521 participants) from the initial sample. However, since the percentage of individuals within each category between included and excluded participants was close, it is unlikely that the exclusions affected the generalizability of our results.
Conclusion
We provide an estimate of sitting time for a large national sample of individuals with MS, and our results indicate that patients with MS spend twice as much time sitting compared with normative estimates of the general population. The distribution of sitting time further differed based on demographic, clinical, and behavioral characteristics. Our results characterize SB in MS and will serve as normative values for comparison with the general population as well as individuals with other chronic conditions.
Conflicts of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a grant from the National Multiple Sclerosis Society (PP 1412). Jeffer E Sasaki was supported by a mentor-based fellowship from National Multiple Sclerosis Society (MB0011). NARCOMS is supported in part by the Consortium of Multiple Sclerosis Centers (CMSC) and the Foundation of the CMSC.
References
- 1.Owen N, Healy GN, Matthews CE, et al. Too much sitting: The population health science of sedentary behavior. Exerc Sport Sci Rev 2010; 38: 105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bauman A, Ainsworth BE, Sallis JF, et al. The descriptive epidemiology of sitting. A 20-country comparison using the International Physical Activity Questionnaire (IPAQ). Am J Prev Med 2011; 41: 228–235. [DOI] [PubMed] [Google Scholar]
- 3.Hu FB, Li TY, Colditz GA, et al. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. J Am Med Assoc 2003; 289: 1785–1791. [DOI] [PubMed] [Google Scholar]
- 4.Katzmarzyk PT, Church TS, Craig CL, et al. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc 2009; 41: 998–1005. [DOI] [PubMed] [Google Scholar]
- 5.Healy GN, Matthews CE, Dunstan DW, et al. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J 2011; 32: 590–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sugiyama T, Healy GN, Dunstan DW, et al. Joint associations of multiple leisure-time sedentary behaviours and physical activity with obesity in Australian adults. Int J Behav Nutr Phys Act 2008; 5: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lynch BM. Sedentary behavior and cancer: A systematic review of the literature and proposed biological mechanisms. Cancer Epidemiol Biomarkers Prev 2010; 19: 2691–2709. [DOI] [PubMed] [Google Scholar]
- 8.Manns PJ, Dunstan DW, Owen N, et al. Addressing the nonexercise part of the activity continuum: A more realistic and achievable approach to activity programming for adults with mobility disability? Phys Ther 2012; 92: 614–625. [DOI] [PubMed] [Google Scholar]
- 9.Veldhuijzen van Zanten JJ, Pilutti LA, Duda JL, et al. Sedentary behaviour in people with multiple sclerosis: Is it time to stand up against MS? Mult Scler 2016; 22: 1250–1256. [DOI] [PubMed] [Google Scholar]
- 10.Blikman LJ, Huisstede BM, Kooijmans H, et al. Effectiveness of energy conservation treatment in reducing fatigue in multiple sclerosis: A systematic review and meta-analysis. Arch Phys Med Rehabil 2013; 94: 1360–1376. [DOI] [PubMed] [Google Scholar]
- 11.Hubbard EA Motl RW andFernhall B. Sedentary behavior and blood pressure in multiple sclerosis patients. Int J MS Care Epub ahead of print 7 March 2017. DOI: 10.7224/1537-2073.2016-021. [DOI] [PMC free article] [PubMed]
- 12.Hubbard EA Motl RW andManns PJ.. The descriptive epidemiology of daily sitting time as a sedentary behavior in multiple sclerosis. Disabil Health J 2015; 8: 594–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol 2008; 167: 875–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Craig CL, Marshall AL Sjöström M, et al. International Physical Activity Questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003; 35: 1381–1395. [DOI] [PubMed] [Google Scholar]
- 15.Wallmann-Sperlich B, Bucksch J, Hansen S, et al. Sitting time in Germany: An analysis of socio-demographic and environmental correlates. BMC Public Health 2013; 13: 196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meneguci J, Sasaki J, da Silva Santos Á, et al. Socio-demographic, clinical and health behavior correlates of sitting time in older adults. BMC Public Health 2015; 15: 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mabry RM, Winkler EA, Reeves MM, et al. Correlates of Omani adults’ physical inactivity and sitting time. Public Health Nutr 2013; 16: 65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marrie RA, Cutter GR, Tyry T, et al. Upper limb impairment is associated with use of assistive devices and unemployment in multiple sclerosis. Mult Scler Relat Disord 2017; 13: 87–92. [DOI] [PubMed] [Google Scholar]
- 19.Learmonth YC, Motl RW, Sandroff BM, et al. Validation of Patient Determined Disease Steps (PDDS) scale scores in persons with multiple sclerosis. BMC Neurol 2013; 13: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Godin G andShephard RJ.. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci 1985; 10: 141–146. [PubMed] [Google Scholar]
- 21.Motl RW, McAuley E, Sandroff BM, et al. Descriptive epidemiology of physical activity rates in multiple sclerosis. Acta Neurol Scand 2015; 131: 422–425. [DOI] [PubMed] [Google Scholar]
- 22.Rosenberg DE, Bull FC, Marshall AL, et al. Assessment of sedentary behavior with the International Physical Activity Questionnaire. J Phys Act Health 2008; 5(Suppl 1): S30–S44. [DOI] [PubMed] [Google Scholar]
- 23.Healy GN, Dunstan DW, Salmon J, et al. Breaks in sedentary time: Beneficial associations with metabolic risk. Diabetes Care 2008; 31: 661–666. [DOI] [PubMed] [Google Scholar]
- 24.Brocklebank LA, Falconer CL, Page AS, et al. Accelerometer-measured sedentary time and cardiometabolic biomarkers: A systematic review. Prev Med 2015; 76: 92–102. [DOI] [PubMed] [Google Scholar]
- 25.Ekelund U, Steene-Johannessen J, Brown WJ, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016; 388: 1302–1310. [DOI] [PubMed] [Google Scholar]
- 26.Rahn K, Slusher B and, Kaplin A. Cognitive impairment in multiple sclerosis: A forgotten disability remembered. Cerebrum 2012; 2012: 14. [PMC free article] [PubMed] [Google Scholar]
- 27.Young DR, Hivert MF.Alhassan S, et al. Sedentary behavior and cardiovascular morbidity and mortality: A science advisory from the American Heart Association. Circulation 2016; 134: e262–e279. [DOI] [PubMed] [Google Scholar]
- 28.de Rezende LF, Rodrigues Lopes M, Rey-López JP, et al. Sedentary behavior and health outcomes: An overview of systematic reviews. PLoS One 2014; 9: e105620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Rezende LF, Rey-López JP, Matsudo VK, et al. Sedentary behavior and health outcomes among older adults: A systematic review. BMC Public Health 2014; 14: 333. [DOI] [PMC free article] [PubMed] [Google Scholar]