Abstract
Objective
To review and critically evaluate the extant research literature pertaining to adherence in youth and adults with headache and to provide recommendations for future research.
Background
This article provides the first systematic review of pediatric headache adherence and updates a previous review of treatment adherence in adults with headache.
Design
Systematic review of empirical literature.
Methods
A literature search with no date restriction was conducted using PubMed and PsycINFO electronic databases and bibliographies of relevant articles.
Results
Adherence rates in adults with headache range considerably from 25% to 94% across treatment, assessment method, and definition of adherence utilized. Methods to assess adherence included retrospective prescription claims data, paper or electronic diaries, follow-up appointment attendance, written and verbal self-report of general adherence, verbal self-report of adherence over a specific amount of time via in person interview or telephone, validated adherence measures, adherence questionnaires without validation, and counselor ratings of homework. Each methodology and assessment tool demonstrated strengths and weaknesses. No studies have systematically examined medication adherence in children with headache, and the few available studies examining adherence to behavioral treatment have documented adherence rates ranging from 52% to 86%.
Conclusions
Adherence research in adults with headache is growing, but studies demonstrate a number of methodological shortcomings. Adherence research in children with headache, and adherence intervention research in both adults and children, is scant. Future research should use objective measures of adherence, consider over-the-counter medications and medication overuse, examine demographic, psychological, and behavioral correlates of adherence, assess adherence to botulinum toxin type A, and examine the efficacy of adherence interventions in individuals with headache.
Keywords: headache, migraine, pediatric, adherence, patient compliance, self-management
Nonadherence to prescribed treatment regimens is an important and widespread behavioral health issue in the management of chronic conditions. Rates of nonadherence range from 50% to 60% across adult chronic illness populations and from 50% to 88% across pediatric populations.1–4 Poor adherence to prescribed treatment regimens can lead to increased disease severity, risk of relapse, greater health care utilization, and sub-optimal symptom management.4,5 Clinical decision-making regarding prescribed treatment is typically made by patient reported improvements in symptoms and/or functioning, resulting in increases or alterations in medication regimens without accurate knowledge of the patient’s adherence.
Treatment adherence, “the extent to which a person’s behavior coincides with medical or health advice,”6 is particularly relevant to headache management given that regimens can be complicated. Treatment regimens for headache often require development of acute strategies, preventative treatments including medications and behavioral lifestyle changes, self-monitoring of symptoms and treatment, and attending medical appointments related to the diagnosis and treatment of headache.7,8 Adherence to acute treatment strategies requires an understanding of how and when to use acute medication as well as the behavioral skills to organize and to plan for differing medication regimens. Individuals must learn how to identify the onset of a headache, to determine the proper dose of nonsteroidal anti-inflammatory drugs (NSAIDs), and to track the frequency of medication administration.9 Some treatments involve a multimechanism approach in which one must decide at the onset whether to take NSAIDs or combine with a triptan based on perceived headache severity. In addition to acute strategies, prevention of headaches also often requires a combination of daily medications and biobehavioral techniques.5 Adherence to daily medication and behavioral lifestyles changes further complicate the treatment regimen and are well-known barriers to successful response.5
Rains et al presented an excellent review of the literature on adult headache treatment adherence and noted that existing studies reported adherence rates similar to those observed in other medical conditions.10 Specifically, 25–50% of adult patients with headache were nonadherent to preventative headache medication,11–13 up to 70% of patients failed to use acute medication in an optimal fashion,14,15 11% of patients opted to not fill a previous prescription for headache medication, and 71% of patients delayed or avoided taking a prescription due to adverse side effect or safety concerns.16 This review also reported that approximately 40% of patients did not return for follow-up appointments after their initial consultation.17 Although less frequently studied, rates of adherence to behavioral lifestyle changes (eg, diet, exercise, sleep, relaxation for stress management) range from 22% to 85%.18 Importantly, 35 studies have examined treatment adherence in patients with headache since the review conducted by Rains and colleagues, and an updated review of the literature is necessary and timely.
Adherence rates in adults with headache do not directly translate into an understanding of pediatric headache management given the unique factors that impact adherence in children and adolescents (eg, developmental considerations, shared responsibility for treatment with a caregiver, cognitive/emotional maturity, etc). Therefore, an examination of adherence in pediatric populations is needed to better understand the specific challenges to headache self-management in this subpopulation. The purpose of this article is to provide a systematic review of the extant literature assessing adherence to treatment regimen in adult and pediatric headache. Although treatment adherence is assessed in a variety of ways, this review will examine all current studies which report adherence findings related to acute medication, preventative medication, behavioral lifestyle changes, self-monitoring through headache diary, and appointment attendance for children and adults with headache. These studies are organized by treatment modality and then by the type of adherence assessment utilized within each treatment type. In addition, a critique of adherence assessment methodology, specific recommendations for future research, and clinical implications are provided.
METHODS
Data Search
A systematic search of the biomedical and behavioral science literature was conducted in October 2013 using PubMed and PsycINFO electronic databases and in accordance with the guidelines presented in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement.19 The search strategy included a combination of a Boolean search using Medical Subject Heading terms (eg, headache disorders, child, adolescent, adult, selfcare, patient compliance, and botulinum toxin type A) and key words (eg, adherence, compliance, self-management, concordance). No date restriction was utilized. Returned articles were included in this review if the study was empirical, participant sample included only individuals with primary headache (studies including patients with headache along with patients with other pain conditions were excluded), adherence was assessed as a part of clinical care or for research purposes, and the original article was in English. Reference sections of included articles were reviewed, and relevant articles that met inclusion criteria were included.
Study Selection and Screening
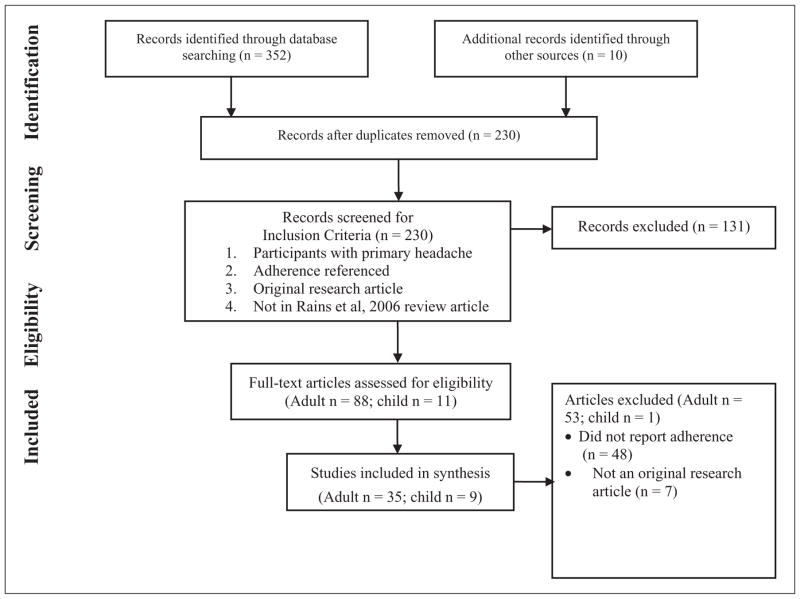
See the Figure for details regarding the selection of articles that were included in the current review.19 The initial search strategy resulted in 352 records identified through the database searches and 11 articles identified through other sources. A total of 231 abstracts were screened after duplicates were removed. Of these, 100 full-text articles were reviewed (89 adult, 11 pediatric). Studies were excluded if they did not assess adherence (46 adult, 2 pediatric) or were not original research articles (ie, review or commentary; 7 adult).
Figure.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram demonstrating the literature search and review process.
Data Extraction
Two reviewers (R.R. and J.R.) completed data extraction from the 36 adult and 9 pediatric articles included in this review. A third reviewer (K.H.) assessed the included articles for accuracy. Collectively, the three reviewers resolved questions regarding the inclusion of articles and adherence data to be reported. Study design, sample characteristics, method utilized to assess adherence, and results of each study can be found in the Table.
Table.
Study Characteristics of Included Studies
| Study | Study Design, Recruitment and Sample | Research Question | Adherence Measure | Adherence Findings | Comments |
|---|---|---|---|---|---|
| Adult | |||||
| Allena et al (2012)51 | Prospective observational study Participants recruited during detoxification 85 adults MOH† (mean 39.7 years) 80% female |
Acceptability of and adherence to an electronic HA diary | Electronic HA diary; paper HA diary | 98% adherence rate to electronic diary; no differences in adherence based on age, education, or baseline HA disability | Adherence classification defined as e-diary completely filled in; single-site study; inpatient sample with only MOH; self-report diary is subject to reporting bias; patients tracked HA in both diary forms but no adherence data on paper diary |
| Attar and Chandramani (2012)42 | Prospective observational study Participants referred by physicians from variety of medical clinics 53 adults Migraine‡ (mean 37.0 years; 20–55 years) 100% female |
Role of physician empathy in migraine outcomes and adherence to treatment regimen | Self-reported adherence to diet/meal timings, exercise, de-stressing/sleep modification, and consumption of medications/vitamins via telephone questionnaire | Diet/meal timing (32% “always” adherent, 26% “often,” 13% “sometimes,” 11% “rarely,” 13% “no”); Exercise (32% “always,” 19% “often,” 24% “sometimes,” 17% “rarely,” 7% “no”); De-stress/sleep (41% “always,” 14% “often,” 15% “sometimes,” 6% “rarely,” 8% “no”); Medications/vitamins (45% “always,” 26% “often,” 17% “sometimes”; 9% “rarely,” 2% “no”); adherence to all domains positively associated with physician empathy and decreased migraine disability, migraine days, pain intensity | Adherence classification criteria not defined; small sample; measure of adherence used in study not validated as an adherence measure; self-report diary is subject to reporting bias; study excluded males |
| Cady et al (2009)22 | Combined retrospective prescription claims analysis with prospective study data Participants self-recruited by questionnaire cards at PCP office 785 adults Migraine§ (mean for females 48.9 years, males 42.6 years) 86.6% female |
Factors that predict adherence to triptans | HMO pharmacy records; self-report “Migraine Survey” regarding migraine and medication use | 74.6% adherence rate (triptans); adherent group indicated higher confidence in triptan response, importance of triptan to treatment, satisfaction of triptan, and decreased amount of time following triptan to migraine stop/no pain, and number of triptan doses required for relief | Adherence classification described in terms of persistence (≥1 triptan refill within the past year) per pharmacy records or self-report; large sample with migraine for ≥1 year and prescribed triptan; subset of sample based on subjective, biased self-report of medication use; self-reported HA diagnosis and classification; no reliability or validity for questionnaire |
| Cady et al (2004)50 | Prospective observational study Participants recruited by pharmacist 728 adults Migraine‡ 693 with demographic data (mean 39.9 years; 18–55 years) 93% female |
Effectiveness of rizatriptan and non-triptan medications | Self-reported treatment diary | 95% of consented sample were adherent | Adherence classification defined as diary completion within 24 hours following next migraine and after using newly prescribed medication; self-report diary is subject to reporting bias; nonrandomized study design; all study endpoints were patient self-report and not validated measures |
| Donnet et al (2009)27 | Prospective observational study of pharmacists Participants recruited from random sample of pharmacists 2,462 pharmacists HA/Migraine¶ (mean 38.2 years) 90.1% female |
Migraine management by pharmacy personnel who consider themselves to have migraines | Questionnaire | 27.6% used only recommended medication, 14.1% used non-recommended medications, 58.3% used both; 21.1% met ICHD-II criteria for medication overuse | Adherence classification defined as using only recommended medications; sample only includes pharmacists; subjective, 31% with unconfirmed diagnosis and 69% with confirmed diagnosis, symptoms, and medication use; no reliability/validity data for questionnaire |
| Dozza and Krymchantowski (2013)35 | Retrospective chart review of consecutive records at tertiary care center 500 children and adults Migraine† (mean 38.7 years; 4–88 years) 71.8% female |
Adherence between monotherapy and polytherapy in prophylactic migraine treatment | HA diary and face-to-face interview | 79.6% of the sample were adherent to prescribed medications; no difference in adherence to monotherapy or polytherapy | Adherence classification defined as ≥80% of days complying with prescribed medication; self-report diary is subject to reporting bias; no mention of training/reliability of interviewer; large age range |
| Etemad et al (2005)25 | Retrospective prescription claims analysis 8,488 adults Migraine†† (mean 42.9 years; 18–65 years) 83.6% female |
Utilization patterns of new users of triptan therapy; Direct costs of migraine-related health care services | Pharmacy refill records | 17% of new users did not receive a triptan medication during the 12-months follow up; 39% received only 1 triptan claim | Adherence classification described in terms of persistence; claims data could not account for migraine frequency or severity during 12-months follow-up |
| Ezra et al (2012)43 | Retrospective chart review of consecutive records at HA Clinic 92 adults HA† (mean 42.2 years) 68.5% female 74 with adherence data |
Patient choice of HA treatment, long-term adherence, and clinical outcomes | Self-reported continuation with chosen treatment via phone interview after 12 months | Adherence significantly higher in the hypnosis group than the amitriptyline group | Adherence classification criteria not defined; potential for skewed adherence rates when patients were instructed they could switch therapies; self-reported continuation is subject to reporting bias; adherence to relaxation assessed via self-report but not documented; possible self-selection bias related to long-term adherence; no mention of training/reliability of interviewer |
| Ferrari et al (1997)26 | Prospective observational study Participants referred by PCP to HA Center 280 adults HA‡‡ (mean 39.2 years; 18–65 years) 83.2% female |
Ideas and behaviors of patients to use of analgesic medicines; Differences between opinion and behavior | Self-reported questionnaire (made specifically for this study) about medication beliefs and behaviors | 43% of patients prescribed at least 1 analgesic drug used it; 49% nonadherent to sumatriptan | Adherence classification criteria not defined; no information on measure of beliefs used in the study; self-report measure is subject to reporting bias; no information on instructions given to patients prescribed sumatriptan |
| Gaul et al (2011)39 | Prospective observational study Participants recruited from active participants of a multidisciplinary treatment program at a HA Center 295 adolescents and adults HA/migraine† (mean 41.0 years; 16–76 years) 89% female |
Adherence to treatment recommendations in a multidisciplinary tertiary HA center | Self-reported adherence to preventative medication, progressive muscle relaxation, aerobic exercise, and lifestyle changes via telephone interview | 9% did not fill preventive medication, 39% filled prescriptions for a limited time (mean 5 months); 20% never performed progressive muscle relaxation during follow-up, 19% for a limited time (mean 3 months), 61% on a regular basis; 15% discontinued aerobic exercise after treatment program, 13% continued for 6 months, 72% strictly followed; 56% implemented at least 6 lifestyle recommendations; adherence to >5 associated with reduction in HA frequency and ≥50% reduction of HA days/months | Adherence classification criteria not defined; self-report is subject to reporting bias; no mention of training/reliability of interviewer long-term follow up (12 and 18 months); selection bias in tertiary HA center/day treatment program |
| Golden et al (2009)66 | Prospective observational study No recruitment information provided 2,001 adults Migraine‡ (mean 42.7 years) 74.2% female 1,752 with adherence data |
Factors associated with early treatment of migraine | “Regular adherence to physician’s instructions” dichotomized into “rarely/sometimes” and “most of the time/always” adherent based on self-report | 77% self-reported “regular adherence to physician’s instructions”; Adherence to physician’s instructions was related to early treatment of migraines | Adherence classification defined as “most of the time/always” adherent to physician’s instructions; self-report is subject to reporting bias; not all participants were instructed to treat early by a physician |
| Heckman and Ellis (2011)37 | Naturalistic longitudinal cohort study Participants self-recruited by brochures at outpatient HA Centers 109 adults HA/Migraine† (mean 36.5 years Caucasian, 40.8 years African American; 18–66 years) |
Race-related differences in adherence to preventative medication; Factors predictive of medication adherence | Self-reported daily diary (30 days) | 69% preventative medication adherence in African American patients, 82% in Caucasians (not a significant difference); adherence rate of ≤80% associated with major depressive disorder and lower levels of HA management self-efficacy; no demographic variable predicted adherence | Adherence to diary dichotomized as “inconsistent” or “consistent” based on 80% of days cut point; participants had to agree to delaying the initiation of a new preventive HA agent for 1 month; self-report bias with diary; African Americans recruited more aggressively; no data on incompleters |
| Heckman et al (2008)45 | Naturalistic longitudinal cohort study Participants self-recruited by procedures at outpatient HA Centers 186 adults HA‡‡ (mean 37.6 years; 18–66 years) 89% female; 118 Caucasian, 68 African American |
Race differences in adherence to HA treatment appointments; Variables associated with missed treatment appointments | Follow-up appointment attendance | 41% terminated treatment prematurely; 47% terminated after the pretreatment visit; patients who terminated prematurely were younger, more likely African American, and reported lower SES; premature termination not associated with health insurance status, gender, depression diagnosis, treatment self-efficacy or locus of control, social support, HA severity, frequency or disability | Adherence classification defined as attending all four treatment appointments; convenience sample; SES only significant predictor for Whites; all data based on self-report; no information provided on reasons for missed appointments/attempts to reschedule; limited generalizability to other racial groups |
| Hedenrud et al (2008)34 | Prospective observational study Participants recruited consecutively in tertiary care clinic 174 adults Migraine† (7% 18–24 years, 17% 25–34 years, 20% 35–44 years, 34% 45–54 years, 22% ≥ 55 years) 84% female |
Assess beliefs about medication and medication related factors and relationship with adherence to prophylactic drug therapy | Medication Adherence Report Scale (MARS) | 64% adherent to prophylactic medicine; Users of β-blockers were more adherent compared with patients using other drugs (tricyclic antidepressants or antiepileptics); beliefs about medication and medication-related factors did not predict nonadherence | Adherence classification defined as ≥23 on the MARS (considered adherent if participant responded “sometimes” for 1 or “rarely” for 2 of the MARS statements); participant self-report is subject to reporting bias |
| Holroyd et al (2010)30 | Randomized placebo controlled trial Participants referred by physicians at outpatient clinics and through advertisements 232 adults Migraine† (mean 38.2 years; 18–65 years) 79% female |
Effect of preventative (β blocker) treatment, behavioral migraine management, or combination approach in acute migraine treatment | Daily electronic diary for medication adherence; Counselor rating of homework quality for behavior migraine management | 90% adherent to electronic diary; 94% adherent to β blocker at 5 months, 95% at 10 months, 92% at 16 months; 70% adherent to behavior management homework assignments; 71% adherent to homework at session 2, 76% at session 3, 77% at session 4 | Adherence to β blocker defined as 25 +/30 days; adherence to behavior management defined as at least 60% completion with good or excellent ratings for quality; self-report diary is subject to reporting bias; no information on how adherence issues were measured or addressed during telephone contacts |
| Ifergane et al (2006)23 | Retrospective prescription claims analysis 1,498 adults Migraine§ (mean 44.0 years) 77.1% female |
Triptan use patterns in an Israeli Health Maintenance Organization district | Prescription refill data | 56.1% purchased triptans 1 time during follow-up (6–18 months), 21.3% filled 2–3 prescriptions, 17.8% filled 4–12 prescriptions, 4.7% filled 13 or more; single-time users were more likely male and younger than 30 or older than 70 years; single-time users more commonly prescribed 50 mg tablets compared with 100 mg tablets | Adherence classification described in terms of persistence; diagnosis of migraine was not validated in the sample; prescription filling data could not account for migraine frequency or severity during follow-up; no information on instructions given to patients prescribed triptans |
| Katíc et al (2011)21 | Prospective prescription claims analysis 40,892 adults Migraine†† (mean 37.8 years) 78.9% female |
Prescription refill patterns among patients newly prescribed triptans | Prescription claims data | 53.8% received no consecutive refill of the index triptan; 12.8% persistent with one additional refill; 10% remained persistent at time of 7th refill; patients more likely to remain persistent after 2nd refill | Adherence classification described in terms of persistence; no minimum criterion for persistency (could fill 2 prescriptions and considered persistent); no information on migraine frequency or severity during 2-year study period |
| Kleiboer et al (2009)54 | Prospective observational study Participants recruited from behavioral training RCT participants 44 adults Migraine‡‡ (mean 43.0 years; 25–63 years) 82% female |
Utility of online digital assistance (real time monitoring + personalized coaching) in behavioral training | HA diary via Palm™ device | 85% adherent to “time” diaries (range 61–100%) | Adherence classification defined as ≥80% completed diary; small sample; self-report diary is subject to reporting bias; no information on adherence to diaries when not prompted by a “beep” |
| Krymchantowski and Tavares (2004)36 | Open-label nonrandomized prospective trial Participants recruited consecutively at private HA Center 175 adults Migraine‡‡,§§ (mean age for women 39.6 years; mean age for men 41.7 years) 88.5% female |
Evaluate adherence, weight loss, tolerability, and response to topiramate in a real-world setting | Patient verbal report of adherence and return follow-up appointment | 76.6% were adherent to topiramate and returned for follow-up | Adherence classification defined as patient returning for 3 months follow-up; medication not prescribed at random (investigator decision) |
| Krymchantowski and Jevoux (2011)46 | Open-label nonrandomized prospective trial Participants recruited from 2 outpatient HA Centers 120 adults Migraine† (mean 41.2 years; 18–68 years) 86.7% female |
Compare topiramate and divalproex sodium for the prevention of migraine in a real-world setting | HA Diary and patient return to follow-up appointment | 85.5% treated with topiramate returned for follow-up, 84.3% treated with divalproex sodium returned | Adherence classification defined as patient returning for 3 months follow-up; medication not prescribed at random (investigator decision); no data reported on adherence to HA diary during treatment period |
| Lafata et al (2010)40 | Retrospective case control study Participants recruited via mail or telephone 2,517 adults Migraine¶ (mean 40.3 years; 18–55 years) 77.4% female; 941 control participants |
Use of migraine preventative medications among patients with and without migraines | Prescription claims data | 88% adherent between first and last dispensing; 56% adherent during 12-months observation period; 88% (antidepressants) – 100% (antihypertensives) adherent between dispensings, 47% (anticonvulsants) – 58% (antihypertensives) adherent for fixed 12-months; adherence between dispensings related to less migraine-related disability and higher drug costs (not total medical care costs) | Adherence classification described in terms of persistence (access to medications ≥80%); only 13.4% of migraine cases used preventative medications; survey may have misclassified participants as controls |
| Lemstra et al (2002)48 | Prospective randomized clinical trial Participants referred by PCP for research 80 adults Migraine‡‡ (mean 34.4 years) 66.3% female; 41 with adherence data; 36 control participants |
Multidisciplinary intervention for migraine treatment in a group, low cost, nonclinical setting | Attendance to multidisciplinary appointments | 87.6% of intervention completers were adherent | Adherence classification defined as attending all multidisciplinary appointments; small intervention sample; participants not blinded to intervention status |
| Linde et al (2008)29 | Prospective observational study Participants recruited prior to outpatient HA clinic visit 174 adults Migraine† (mean 45.0 years; 19–79 years) 84% women |
Association between physician-reported clinical features and migraine adherence | Self-report on Medication Adherence Report Scale (MARS) | 35% were nonadherent (mean 22.5); no demographic characteristics or disease specific variables were significantly associated with adherence | Adherence classification defined using MARS, but cut-off point not provided; subjective measure of adherence with little information regarding MARS scoring; no reliability/validity data provided for MARS; only includes those with preventative prescription |
| Moloney et al (2009)53 | Prospective observational study Participants recruited through advertisements to public and physicians 77 women Migraine¶ (mean 37.5 years) 100% women |
Feasibility and acceptability of internet-based HA diary | Internet based HA Diary | 68% completed at least 50% of diary pages within 24 hours; 75% of all pages were completed within 2 days | Adherence classification criteria not described but all participants included in analyses “completed 4 months of diary entries”; 83% reported keeping notes when they lacked internet access |
| Packard and O’Connell (1986)12 | Prospective observational study Participants recruited consecutively from new patient population at outpatient HA Clinic 100 children and adults HA§ (Non-adherent group mean 34 years; 16–61 years; Adherent group mean 35 years; 9–71 years) 81% female |
Adherence among HA patients being treated with prescription medication | Self-reported adherence to prescribed medication via interview | 52% of the initial sample determined to be nonadherent; At the 3-months follow-up, 46% (24/52) continued to be nonadherent and 46% (24/52) were determined to be adherent; 30/48 of the initially adherent patients were still adherent at 3 months, 10 were nonadherent at 3 months (5 were determined nonadherent during initial interview) | Adherence classification described as not taking prescribed medication as instructed (forgetting, missing doses, taking extra, or using other medicine); self-report via interview is subject to reporting bias; no information on training/reliability of the interview; large age range |
| Panconesi et al (2010)24 | Retrospective prescription claims analysis 1,453 adolescents and adults Migraine§ (14–>65 years) |
Patterns of triptan utilization | Prescription claims data | 52.1% (2005) – 57.7% (2006) received only one prescription in a year | Adherence classification described in terms of persistence; no information on migraine frequency or severity over the 2 years; limited participant demographic information |
| Rahimtoola et al (2003)31 | Retrospective prescription claims analysis 729 adults Migraine§ (mean 40.0 years; 12–93 years) 80.8% female |
Use of migraine preventative medications in ergotamine and triptan patients | Prescription claims data | 74.7% of patients stopped preventative treatment after 12 months | Adherence classification defined as “stop use” (presentation of the last preventative prescription 6 months or more prior to the end of the observation period); patients had unconfirmed migraine diagnosis; no information on migraine frequency or severity over the follow-up year |
| Rahimtoola et al (2001)32 | Retrospective prescription claims analysis 6,383 adultsb Migraine§ |
Patterns of ergotamine and sumatriptan use | Prescription claims data | 53% of patients prescribed ergotamine were single-time users (34% of patients prescribed sumatriptan were single-time users) | Adherence classification defined as “incidental use” (presenting only one prescription and not switching during the follow-up year), “continuous use”(more than one prescription during follow-up year), and “switch use”; patients had unconfirmed migraine diagnosis; no information on migraine frequency or severity over the follow-up year |
| Ramsden et al (2011)44 | Prospective randomized clinical trial Participants recruited through HA clinics, neurology clinics, and advertisements 40 adults HA† 18 years and older |
Preliminary adherence to targeted analgesic dietary interventions | HA diary; erythrocyte fatty acids | 83.3% adherent to HA diary; “demonstrated changes in diet adherence via changes in erythrocyte fatty acids” | Diary adherence defined as ≥80% completion of daily entries; dietary adherence not defined; ongoing study at time of publication; no data on dietary adherence; self-report diary is subject to reporting bias |
| Rossi et al (2006)47 | Open-label prospective trial Participants recruited consecutively from HA Clinic 118 adults MOH/migraine† (mean 44.0 years; 16–65 years) 83.8% female |
Effectiveness of advice vs structured detoxification programs for MOH | Attendance to follow-up visit 2 months after withdrawal therapy | 89% of the sample completed the follow-up visit (92.5% from simple advice group, 87.2% from outpatient detoxification, 87.2% from inpatient detoxification); no significant group differences in adherence | Adherence classification defined as attending 2-months follow-up visit; limited generalizability due to inclusion and exclusion criteria |
| Rothrock et al (2006)38 | Prospective randomized controlled trial Participants recruited consecutively from HA Clinic 100 adults Migraine‡‡,§§ (mean 42.5 years; 17–62 years) 92% female |
Addition of patient education to routine medical management on migraine outcomes and health care utilization | HA diary of self-reported use of acute or preventative medications | 58.5% of the “no school” group were adherent to their preventative medication (96% of the “school” group); 36% of the “no school” group reported analgesic overuse (zero in the “school” group) | Nonadherence (overuse) to analgesics defined as self-administration of any given prescription or nonprescription >3 days/wk for >4 consecutive wks with ≥2 doses/day; self-report diary is subject to reporting bias; healthcare utilization based on self-report diary |
| Seok et al (2006)33 | Prospective observational study Participants recruited consecutively from HA Clinic 145 adults Transformed migraine† 136 with demographic and adherence data (Conversion to episodic migraine mean 46.99 years; Persistent chronic daily HA mean 45.07 years) 89.7% female |
Factors associated with the reversion of transformed migraine into episodic migraine | Self-reported discontinuation of overused medication, use of preventative medication and lifestyle modification via clinic or telephone interview | 78.4% (69/88) of patients adherent to prescribed preventive medications; 89.4% (84/94) of patients who met medication overuse criteria discontinued overused drugs; Adherence to regular exercise associated with reversion of CDH to episodic attacks; Poor adherence to preventive medication and failure to discontinue overused medication associated with poor HA outcome | Adherence classification defined as “regular use of preventive medications” and exercising >3 times/wk for >30 minutes at a time; self-report is subject to reporting bias; no mention of training/reliability of interviewer; possible that improvement in HA preceded regular exercise |
| Sorbi et al (2007)55 | Prospective observational study Participants recruited from completers of behavioral training program 5 adults Migraine‡‡ (24–52 years) 100% female |
Feasibility and acceptability of online digital assistance in behavioral treatment | HA diary | 78.6% adherence with 4–5 prompts per day (run 1); 86.8% adherence with 2–3 prompts (run 2); 50–70% perceived they were adherent to first “beep”; “good” adherence in both runs to morning and evening diaries | Adherence classification defined as ≥80% diary completion; pilot study; self-report diary is subject to reporting bias; participants prompted three times before recorded as missed entry; no data on average number of “beeps” before completion |
| Tassorelli et al (2008)52 | Prospective observational study Participants recruited via mailings to a random sample of patients prior to initial consult at HA Center 76 adolescents and adults HA/migraine¶ (mean 39.1 years; 11–85 years) 72.4% female |
Usefulness and applicability of a simplified HA diary prior to initial consultation | HA diary | 71% returned the “completed” diary; 28% “almost” complete diary; 1% “fair” completion | Adherence classification defined as “complete” when data for all 14 items entered, “almost” complete for 12 items, “fair” completion for <12 items; no rationale for adherence cutoffs; self-report diary is subject to reporting bias; large age range; pilot study |
| Yaldo et al (2008)41 | Retrospective cohort study 12,783 adults Migraine§ (Amitriptyline mean 43.9 years, Propranolol/Rimolol mean 42.0 years, Divalproex mean 43.1 years, Topiramate mean 43.9 years) Female (83%, 83%, 76%, 88%) |
Persistence with preventative treatment and acute migraine medication utilization in patients prescribed migraine preventative treatment | Pharmacy/medical claims data | Topiramate group more likely to remain persistent with prophylactics compared with other prophylactic medication groups; risk for discontinuing treatment was higher with amitriptyline (23%), propranolol (6%), and divalproex sodium (11%); men 13% more likely to discontinue medications | Adherence classification described in terms of persistence (refilling medications within 1.5 times the days of supply of the previous fill); large multi-region study |
| Child | |||||
| Allen and McKeen (1991)61 | Multiple baseline across subjects Participants referred by pediatric neurologists 21 children HA/Migraine‡‡ (7–12 years) |
Efficacy of thermal biofeedback and parent-implemented pain behavior management guidelines; Relation of treatment adherence and HA activity | Self-report diary on length of practice and temperature changes achieved | 14% of children nonadherent to biofeedback; nonadherence related to lower baseline HA activity, no reduction of HA activity; 14% of parents nonadherent to pain behavior management; parental nonadherence related to increased HA activity over time; amount of biofeedback practice related to HA activity | Adherence classification defined as engaging in biofeedback on average ≥1/day; small sample; excluded migraine with aura; self-report diary is subject to reporting bias; baseline HA information obtained prior to treatment; no statistical test conducted for adherent vs nonadherent patients |
| Andrasik et al (2007)60 | Nonrandomized assessment of treatments Participants recruited at outpatient HA Center 35 children HA‡‡ (7–17 years) |
Efficacy of relaxation training and amitriptyline | No formal assessment | All patients in behavioral group came regularly for sessions, practiced routinely, and appeared adherent; “low” adherence to medication | Adherence classification criteria not defined; small sample; no information regarding adherence assessment |
| Engel (1993)62 | Multiple baseline across subjects Participants referred by neurologists and pediatricians 10 children HA‡ (mean 11.5 years) 80% female |
Relation of HA activity with both the use of progressive muscle relaxation and adherence to relaxation recommendation | HA diary and relaxation log (including recording of the password randomly played during relaxation exercise) | Average patient adherence was 84% (range 36–100%); relationship between adherence and number of HA free days; nonadherence occurred on 74% of days when children were HA free; nonadherence more frequent Friday-Sunday | Adherence classification calculated using the following formula: (self-reported # of days practiced + # of correct recorded “relaxation password of the day”)/total number of days; small sample; “relaxation password of the day” may have promoted adherence |
| Grazzi et al (2004)57 | Nonrandomized assessment of treatments 26 children and adolescents HA‡‡ |
Relaxation training vs amitriptyline in the treatment of tension-type HA | No formal assessment | Patients in the behavioral treatment group appeared to be adherent; 41% of patients in the medication group dropped out due to side effects and/or nonadherence | Adherence classification criteria not defined; small sample; no information regarding how adherence was assessed |
| Guibert et al (1990)64 | Prospective observational study Participants referred by pediatricians, PCP, and neurologists 160 children Migraine¶¶ (9–17 years) 64.4% female |
Adherence factors in the behavioral treatment of HA | Therapist rated youth as “never,” “sometimes,” or “always” adherent to completion of intensity ratings, diary, and homework at 4 time points (baseline, treatment, 1-month post, 3-months post) | 52% of children classified as adherent; adherent children had lower HA index at baseline; age, child perception of the treatment rationale, and initial severity of HA related to adherence | Adherence classification defined as completion of intensity ratings, diary, and homework ≥80% at all time points; large sample; children who dropped out were considered adherent if they were adherent up until drop out |
| Hershey et al (2000)56 | Unblind medication trial Participants recruited from HA Clinic 192 children HA/Migraine‡‡ (mean 12.0 years) |
Efficacy of a standardized dose of amitriptyline in childhood HA | Self or parent verbal report | 2/192 stopped taking amitriptyline due to HAs being better/worse and were described as nonadherent | Adherence classification defined as continued use of amitriptyline; large sample; self and parent report is subject to reporting bias; no information provided about adherence assessment; no mention of training/reliability of interviewer |
| Usai et al (2011)59 | Open-label prospective trial Participants recruited from HA Center 30 children Migraine‡‡ (8–18 years) |
Effectiveness of ginkgolide B | Not documented | Adherence was good | Adherence classification criteria not defined; small sample; no information regarding adherence assessment |
| Usai et al (2010)58 | Open-label prospective trial Participants recruited from HA Center 24 children Migraine‡‡ (8–18 years) |
Effectiveness of ginkgolide B at one year follow-up | Not documented | Adherence was good | Adherence classification criteria not defined; small sample; no information regarding adherence assessment |
| Wisniewski et al (1988)63 | Prospective observational study Participants referred by physician, health professional or school nurse 10 adolescents HA/Migraine‡ (mean 13.5 years) 70% female |
Effectiveness of relaxation; Relation between treatment adherence and outcome | Self and parent report of amount of time practiced (subjective); cassette recorder with a hidden watch that was activated with recorder use (objective) | 42% adherence per the objective measure; children over reported (mean 132%) practice time on 66% of study wks; when underreporting (eg, child let someone use player) is controlled children over reported by 70% and practiced on 53% of the time requested | Adherence classification defined as amount of time practiced; small sample; sequential assignment to treatment condition; objective and subjective measures of adherence; objective results not included when families underreported |
ICHD2 classification criteria utilized by physician to diagnose.
Participants referred by physician with a specific diagnosis, but no information regarding specific diagnostic classification criteria provided.
No information regarding diagnostic classification criteria provided.
Self-report questionnaire data utilized to make diagnosis based on ICHD2 or IHS criteria.
Diagnosis supported by ICD9 diagnosis.
IHS classification criteria utilized by physician to diagnose.
Silberstein classification system utilized.
Ad hoc committee on classification of headache criteria.
Studies that assess adherence for the same dataset.
Demographic information provided by year across a 7-year period.
HA = headache; MOH = medication overuse headache; PCP = primary care physician; RCT = randomized clinical trial.
RESULTS
Acute Medication Adherence
Seven studies have examined adherence to acute medications in adults with headache. Many studies examining adherence to acute medications have utilized prescription claims data to measure persistence or the “time from initiation to discontinuation of therapy.”20,21 In general, prescription claims data analysis has found poor persistence in patients prescribed triptans for migraine treatment, with 25.6–56.1% of patients receiving, at most, one triptan claim during a follow-up period (range 1–2 years).21–25 Adherence assessment of acute medication is complicated by the preventative treatment effect in that as headache frequency improves, the number of times an acute medication is needed is reduced. Additionally, the headache’s response to over-the-counter (OTC) medication may improve, further reducing the need to fill a prescription medication.
A retrospective review of prescription filling data in an Israeli Health Maintenance Organization district found that single-time triptan users were more likely to be male and younger than 30 or older than 70 years.23 In this study, nonpersistence was more common in patients prescribed 50 mg tablets of sumatriptan compared with those using 100 mg tablets. In a recent U.S. pharmacy claims data analysis, 22,013/40,892 (53.8%) new triptan users did not persistently refill their index triptan over the 2-year period and 12.8% were persistent for only one additional refill.21 Of those patients who did not persistently refill their index triptan, 25.5% discontinued migraine prescriptions, 34% switched to opioids, 23% received an NSAID, 7.4% tried another triptan, and the remainder received other nonspecific migraine medications. Once patients filled 2 or more triptan prescriptions (refills ranged from 1 to 70), they were more likely to remain persistent over the course of the observation period.
Given the evidence supporting the inconsistency in triptan persistence, Cady and colleagues conducted a survey with lapsed and sustained triptan users to identify factors predictive of triptan adherence.22 Compared with patients who had lapsed from use of their prescribed triptan, predictors of sustained use included satisfaction with, and confidence that the triptan would resolve the headache, the reliability of the triptan to be effective on a regular basis, and fewer doses required to control the headache.22 Headache-related factors including patient-reported severity and impact were not predictive of triptan adherence; however, disability scores did indicate that sustained users may experience less time lost from daily activities.22
Findings related to OTC medicines are similar. In a prospective examination of beliefs and behaviors with regard to the acute use of medicine, the majority of the sample reported it was better to treat headaches with medication, yet 57% of patients did not actually take their prescription medication.26 In a study examining medication use by pharmacy personnel with self-reported migraine, 27.6% used only recommended medication (nonspecific agents: NSAIDs, aspirin, or both; migraine-specific agents: triptans, ergotamine, and dihydroergotamine), 14.1% used nonrecommended medication (opiate analgesics and paracetamol), and 58.3% reported using both recommended and nonrecommended medication to treat migraine attacks.27 Furthermore, self-report survey indicated that 21.1% of pharmacy personnel (88.2% with true migraines) met criteria for medication overuse according to International Classification of Headache Disorders-II criteria.27,28
Preventative Medication Adherence
Fourteen studies have examined preventative medication adherence in adults with headache through a variety of methods such as adherence questionnaires, self-reported headache medication diaries, and face-to-face interviews. Documented preventative medication adherence rates range from 48% to 94%.12,29–32
An early prospective observational study assessing self-reported adherence to prescribed medication through interviews with adults with headache reported that only 48% of patients were adherent to preventative medication.12 Adherence rates declined at 3 months, with 75% of the initially adherent group continuing to take their preventative medication as recommended.12 A longitudinal examination including adults with chronic migraine found that 78.4% of patients reported being adherent to prescribed medications in a face-to-face or telephone interview, and 89.4% of patients who initially met medication overuse criteria reported abrupt discontinuation at 12 months.33 In addition, this study documented that poor adherence to preventative medication and failure to discontinue overused medication was associated with persistent chronic daily headaches.33
A more recent study reported that 65% of adults with migraine were adherent based on a self-report questionnaire, the Medication Adherence Report Scale (MARS).29 A study analyzing the association of self-reported adherence based on the MARS and beliefs about medicines and medication-related factors demonstrated a 64% adherence rate to preventative medications and also found that beliefs about medicine and medication-related factors are not predictive of nonadherence.34 Additional analyses, however, revealed that among patients using preventative medication, patients using β-blockers were more adherent than patients not taking β-blockers and that patients using tricyclic antidepressants are less adherent than patients not taking tricyclic antidepressants.34
A study assessing adherence in individuals with migraine through self-reported medication diary found 79.6% of the sample to be adherent to preventative medication on at least 80% of days and that adherence rates did not differ between patients with monotherapy and polytherapy treatment.35 Similarly, Krymchantowski and Tavares utilized headache diaries as a measure of adherence and reported that 76.6% of the patients were adherent to preventative regimen with 4% being nonadherent prior to the 3-month evaluation and 19.4% not returning for the 3-month follow up.36 A longitudinal study also examining adherence to β-blockers through headache medication diaries found that 94% (85/90) of patients had taken the prescribed β-blocker on at least 25 of 30 days over a 5-month period.30 Information regarding adherence rates for participants remaining in the study over time were also gathered and indicated that 95% (72/76) and 92% (54/59) of the remaining participants remained adherent at the 10-month and 16-month follow ups, respectively.30 Heckman and Ellis examined adherence to preventative medication in adults with migraine across racial groups based on self-reported headache diary data and documented that 69% of African American patients and 82% of Caucasian patients were adherent to preventative medication.37 The observed difference in adherence rates, however, was not statistically significant. Interestingly for the combined sample (Caucasian and African Americans), adherence rates lower than 80% were associated with major depressive disorder and lower levels of headache management self-efficacy; however, no demographic variables significantly predicted adherence.37 Finally, Rothrock and colleagues utilized headache diary report to examine the adherence rates of migraineurs to preventative and acute headache medications following “headache school” to the adherence rates of migraineurs who did not receive “headache school.” Ninety-six percent of participants receiving additional education on migraine symptoms, diagnosis, treatment, and prevention were classified as adherent, while 58% of participants not receiving patient education were classified as adherent to their preventative medication.38
Three studies have described adherence to preventative medications for headache by retrospectively examining medication persistency. One of the preventative persistency studies, conducted with a sample of individuals attending a multidisciplinary headache center and day treatment program, found 9% of patients did not fill preventative medication even once while 39% filled prescriptions for only a limited time (on average 5 months).39 Another study utilizing pharmacy claims data and an adherence cut point of access to medication (obtained refills) at least 80% of the time documented an average preventative medication adherence rate of 88% between the time of their first and last dispensing and a 56% average adherence rate during the 12-month observation period.40 Adherence rates based on type of preventative medication utilized ranged from 88% for antidepressants to 100% for antihypertensives between dispensings and 47% for anticonvulsants to 58% for antihypertensives for the fixed 12-month period.4 Moreover, adherence rates between dispensings were related to decreased migraine-related disability and higher drug costs, but not total medical care costs.40 Of note, telephone interview rather than a visit with a health care provider was utilized to assess migraine symptoms and diagnosis, and only 13.4% of individuals fitting diagnostic criteria utilized preventive medications suggesting the potential for diagnostic misclassification of participants. Finally, Yaldo, Wertz, Rupnow, and Quimbo utilized prescription claims data to classify patients as “discontinued” or nonadherent if they did not refill preventative medications within 1.5 times the days of supply of the previous refill.41 Specifically, the risk for discontinuing preventative medication use was 23% higher with amitriptyline, 6% higher with propranolol, and 11% higher with divalproex sodium than with topiramate. In addition, men were 13% more likely to discontinue medications than women.41
Behavioral Lifestyle Recommendations
Similar to medication adherence, there is large variability in adherence rates to behavioral lifestyle recommendations (eg, relaxation, sleep, diet, exercise) and adherence is not optimal. A prospective observational study by Gaul and colleagues assessed long-term adherence to treatment recommendations following completion of a multidisciplinary program through telephone interviews.39 During the 12–18-month follow up, 61% of patients were adherent and still practicing progressive muscle relaxation an average of 3 days a week, whereas 19% stopped after the first 3 months, and 20% never performed relaxation during the follow-up period. There was greater long-term adherence to aerobic exercise, with 72% following recommendations during the entire follow-up period, 13% adherent for the first 6 months, and 15% who discontinued once the program was completed. During the multidisciplinary program, patients were instructed to implement 8 general lifestyle modifications (eg, not exceeding 10 different medication intake days/month, accepting a headache and not rebelling against it, and establishing regular sleep times), and the majority of patients (56%) implemented 6 or more recommendations. On average, patients who were more adherent to progressive muscle relaxation, aerobic exercise, and implemented more than 5 lifestyle modifications reported significant reductions in headache frequency and met the primary outcome criterion (ie, at least 50% reduction of headache days/month) at the 12–18-month follow-up.39
Another study examining the relationship between physician empathy and migraine disability and treatment adherence examined how often patients adhered to physician instructions across 4 areas: diet/meal timings, exercise, stress management/sleep modification, and medications/vitamins.42 Non-adherence rates were high across the sample, such that “always” or even “often” following instructions was seldom reported (45% and 26% for medications/vitamins, 41% and 14% for stress management/sleep modification, 32% and 19% for exercise, and 32% and 26% for diet/meal timing, respectively). However, adherence to all 4 domains was associated with improved clinical outcomes (migraine disability, migraine days, and pain) and physician empathy.42
In addition, a randomized placebo-controlled trial reported that 70% of participants were adherent to behavioral migraine management and adherence rates increased over the course of the treatment.30 Patients were asked during 3 sessions to complete relevant homework assignments that coincided with didactic instruction and practice (eg, deep breathing, relaxation by recall, integration of skills). High adherence was defined as completing at least 60% of the homework with “good” or “excellent” ratings for quality given by the counselor. Another study demonstrated that even when patients have the ability to choose a preferred treatment modality, long-term adherence rates are less than optimal. In an examination of hypnotic relaxation vs amitriptyline for tension-type headache, patients were asked to choose between the two modalities and allowed to switch once they started either treatment.43 Retrospective chart review found adherence with hypnotic relaxation was better than adherence to amitriptyline, such that 26/47 (55.32%) and 10/27 (37.04%) patients continued with their treatment.43
Unlike the aforementioned studies, Ramsden and colleagues employed an objective measure of adherence in their preliminary results of a randomized clinical trial on a targeted analgesic dietary intervention for chronic daily headache.44 For 12 weeks, randomized participants were instructed to follow 1 of 2 diets: low omega-6 polyunsaturated fatty acids or low omega-6 polyunsaturated fatty acids plus high omega-3 polyunsaturated fatty acids. Blood was drawn at 4 time points and used as a biomarker to assess adherence and changes. At the time of publication, analysis of the first 20 participants who had completed the 12-week intervention indicated dietary adherence via reductions in erythrocyte fatty acids.44
Appointment Attendance
Headache treatment frequently involves continual adjustment to the medication regimen and close monitoring of progress. Patients are often asked to attend follow-up appointments after an initial consultation or periodically throughout treatment to assess changes in headache frequency/severity and make changes to the regimen when needed. In other words, adherence to headache treatment often includes attending medical appointments in order to receive treatment recommendations. Utilizing the same dataset as Heckman and Ellis,37 Heckman and colleagues found that 41% of patients presenting to a headache specialty treatment clinic were nonadherent to scheduled follow-up appointments and ultimately terminated treatment prematurely.45 While the majority of patients attended their initial pretreatment visit, 47% did not return for the 1-month follow-up visit in which patients were to begin their new preventative headache medication. Premature treatment termination was associated with younger age, being African American, and reported lower socioeconomic status (ie, years of education and annual income).45 African American patients were more likely to terminate prematurely independent of socioeconomic status, whereas socioeconomic status scores above the median served as a protective factor for Caucasians. Factors unrelated to premature termination for the sample included health insurance status, gender, a diagnosis of depression, treatment self-efficacy and internal locus of control, perceived social support, and headache severity, frequency, and disability.45
Krymchantowski and Jevoux reported that after starting a neuromodulator for the prevention of migraine symptoms, 15% of patients failed to attend the 3-month follow-up appointment to evaluate medication tolerability.46 There were no significant differences in adherence between the 2 treatment groups (topiramate – 14.41% nonadherent; divalproex sodium – 15.69% nonadherent).46 Similarly, Rossi and colleagues examined the effectiveness of physician advice to withdraw overused medications (group A) compared with structured pharmacological detoxification programs (group B – outpatient and group C – inpatient) in a sample of patients with probable medication overuse headache plus migraine, and found that 12.5% of patients did not complete follow-up visits 1 and 2 months after the start of the detoxification program.47 Adherence was comparable across the 3 groups. Lastly, in a randomized clinical trial testing the effectiveness of a multidisciplinary migraine management intervention in a group, low cost, and nonclinical setting, there was 87.58% (±11.98%) attendance adherence for patients who completed the intervention.48 Adherence to the 6-week multidisciplinary intervention included a neurologist visit, an intake with a physical therapist, 18 exercise therapy sessions, 2 group lectures given by a psychologist, 1 group lecture with a dietitian, 2 massage therapy sessions, and discharge meetings with the neurologist and physical therapist.
Headache Diary
Patients suffering from headache are often asked to use charts to monitor a variety of headache and treatment factors such as headache frequency, severity, length, utilization of pharmacological and non-pharmacological treatments, and triggers.49 Similar to appointment attendance, adherence to self-monitoring through a headache diary is an initial step in treatment which allows for optimal diagnosis and headache management. The extant literature includes nine studies examining patient adherence to a variety of headache diaries, such as paper and pencil diaries, electronic diaries, and online digital assistant (ODA) self-monitoring. Documented adherence rates to paper headache diaries for patients with headache and migraine are 83.3% and 95%,44,50 while adherence rates to electronic headache diaries are 90% in patients with migraine30 and 98% in patients receiving inpatient treatment for medication overuse headache.51 Allena and colleagues also investigated the relationship between demographic and disease variables with electronic headache diary adherence and found differences in diary adherence based on age, education, or baseline headache disability.51 Tassorelli and colleagues provided data for varying levels of diary completion which demonstrated that 71% of patients with headache and migraine returned a “completed” diary, 28% returned an “almost” completed diary, and 1% returned a “fairly” completed diary.52 Meanwhile, Moloney and colleagues documented that 68% of patients completed at least 50% of the diary pages within 24 hours and that 75% of all pages were completed within 2 days.53
Two studies specifically examined adherence to ODA which provided real-time monitoring of headache activity and treatment as well as personalized coaching of health behaviors to avoid a migraine through a portable personal digital assistant. Adherence ranged from 61% to 100% with the average individual being 85% adherent to the ODA.54 Meanwhile, Sorbi and colleagues examined adherence to ODA based on the number of prompts for completion provided per day.55 Mean adherence was 78.6% with 4–5 prompts per day and 86.8% with 2–3 prompts. Interestingly, 50–70% of participants perceived they were adherent to the first“beep.”Both studies of ODA adherence reported “good” adherence overall given that average rates of adherence were above 80%.54,55
Adherence in Pediatric Headache and Migraine
Treatment adherence has also been examined in children and adolescents with headache and migraine; however, only 5 pediatric studies have reported medication adherence related findings. In an unblinded medication trial assessing the efficacy of a standardized dose of amitriptyline for children with headache and migraine, 2 of 192 patients were described as nonadherent/nonpersistent because they stopped taking amitriptyline.56 Similarly, in a treatment comparison study of amitriptyline and relaxation training, Grazzi and colleagues indicated that 41% of patients in the medication group “dropped out due to side effects and/or noncompliance.”57 Two open-label prospective trials investigating the effectiveness of ginkgolide B after 3 months of treatment and at 1-year follow up also reported “compliance was good” without providing any information regarding the basis of this conclusion.58,59 Finally, Andrasik and colleagues reported that medication adherence was “low” in an efficacy comparison of relaxation training and amitriptyline, but also stated that they did not conduct a formal assessment of adherence.60
Five studies have examined adherence to behavioral treatment recommendations (ie, relaxation and biofeedback) in children with headache and migraine. Two studies comparing the efficacy of amitriptyline with relaxation training treatment noted that the patients in the relaxation training groups “appeared compliant” to the behavioral treatment without providing formal assessment or information for the basis of the comments,57,60 while 4 other studies provided a formal assessment of adherence to behavioral treatment for headache.
Allen and McKeen found 14% of patients to be nonadherent to biofeedback practice and 14% of parents of patients to be nonadherent to pain behavior management guidelines.61 Child nonadherence to biofeedback was related to lower baseline headache activity and a lack of reduction in headache activity while parental nonadherence to pain behavior management guidelines was related to increased headache activity over time. In addition, higher amounts of biofeedback practice were related to reduction in headache frequency.61
Similarly, Engel documented that the average patient adherence to progressive muscle relaxation was 84% (range 36–100%) utilizing a formula to combine both subjective self-reported number of days practiced and objective reports of adherence.62 An objective report of adherence was obtained based on the number of correct “relaxation passwords of the day” identified during a relaxation practice tape and recorded on the child’s relaxation log. Additional adherence-related findings included a significant relationship between adherence and number of headache free days, nonadherence occurred on 74% of days when children were headache free, and nonadherence was more frequent during the weekend days (Friday-Sunday). Wisniewski and colleagues, on the other hand, reported lower adherence (44%) using an objective measure to record time spent practicing relaxation exercises.63 Although these studies are the only pediatric headache studies to capture adherence through an objective measure, both authors noted the possibility that the “relaxation password of the day” and “hidden recorder” provide more accurate measurements of adherence.62,63
Conversely, Guibert and colleagues classified 52% of children as adherent based on the completion of intensity ratings, headache diary, and behavioral treatment homework at least 80% of the time at all time points across the study.64 Children who were adherent had lower headache index at baseline than nonadherent children, and child age, perception of the treatment rationale, and initial severity of headache were found to be related to adherence.64 Unlike many of the other studies of adherence with children, children who dropped out of this study were considered adherent if they had been adherent up until the point of termination.64,65
DISCUSSION
The purpose of this review was to provide the first systematic review of pediatric headache treatment adherence as well as an update to the review of adult headache adherence by Rains and colleagues.10 Research examining adherence in individuals with headache has been conducted using primarily prospective cross-sectional design; however, retrospective chart reviews and prescription claims analysis have also been utilized. Nine studies examined adherence to medication treatment recommendations in children and adolescents and reported mixed findings based on primarily on retrospective verbal report while 5 studies reported that adherence rates to behavioral treatment varied from 52% to 86%. Thirty-six studies examined adherence to a variety of treatment regimens in adults with headache including preventative medication, acute medication, behavioral lifestyle changes (eg, exercise, relaxation strategies for stress management, diet), health care appointment keeping, and headache diaries while only 9 studies have examined medication and behavioral lifestyle treatment adherence in children and adolescents with headache. Adult adherence rates vary greatly depending on the treatment regimen examined, assessment method, and definition of adherence utilized; adherence rates to preventative medication ranged from 48% to 94%, adherence to behavioral lifestyle changes ranged from 32% to 72%, and adherence to follow-up appointments ranged from 59% to 88% (see the Table for study specifications). Acute medication adherence rates are more difficult to delineate based on the current literature given that 6 studies included in this review used prescription claims data; however, it was documented that 25–56% of adults with headache filled their prescription only once or not at all. Results of this review indicate that rates of adherence are similar to those observed in the previous review in adult headache adherence.10 Moreover, the observed adherence rates are similar to the 50–60% nonadherence rates documented in the general chronic condition literature.1–4
The variability in adherence rates is likely the combined result of true variation in adherence among individuals with headache and the disparate adherence measurement methodology and adherence classification systems utilized within the extant literature. This lack of standard measurement and conceptualization of adherence is perhaps the most significant limitation in the current state of the literature. Study methodologies have documented adherence with retrospective prescription claims data, paper or electronic diaries, follow-up appointment attendance, written and verbal self-report of general adherence, verbal self-report of adherence over a specific amount of time via in person interview or telephone, adherence questionnaires that have not been validated, a one-item rating of general adherence, validated measures of adherence (MARS), and counselor ratings of homework (for behavioral interventions). Although there are limitations to each assessment method, data collected through several of these methodologies are merely proxy measures of adherence, and not necessarily a true representation of adherence.
Retrospective prescription claims analysis, for example, is related to adherence given that an individual must obtain a prescription in order to be adherent; however, it cannot be determine from these data whether medications were accessed from the bottle, taken, or taken appropriately. Persistency data pertaining to acute medication is a particularly complicated marker of adherence because key information is missing. For instance, it may be that participants stopped obtaining refills due to physician-recommended changes in medication type/class or because the individual’s headaches were less frequent/severe and acute medication wasn’t needed as often, if at all. Although prescription claims analysis is a useful noninvasive measure, it has the potential to result in inaccurate adherence data.
Similarly, self-report is a common approach to measuring adherence because questionnaires and interviews are practical, relatively inexpensive, and allow for the potential to monitor in real time. However, headache diaries and other self-report measures are subject to recall and social desirability biases and often result in inflated adherence rates when they are the only measure of adherence employed.66 Finally, studies assessing only appointment attendance provide important information regarding adherence to follow-up appointments, but do not provide information regarding treatment adherence between appointments. In addition, patients enrolled in studies using appointment attendance as the adherence measure may be more motivated to return for a follow-up appointment. Interestingly, none of the reviewed studies utilized electronic monitoring as an objective measure of medication adherence, and only one study, assessing adherence to dietary changes, used bioassays to measure erythrocyte fatty acids.
The classification systems used to determine whether participants were “adherent” or “non-adherent” also varied greatly by study. Within prospective observational studies, several classified individuals as “adherent” to medication if they took at least 80% of their prescribed medication while other studies considered patients to be “adherent” if they took their medication on at least 25 of 30 days during the study period. One study allowed patients with headache to switch between medication therapy and behavior therapy but classified patients as non-adherent if they did not continue using the original therapy. Other studies had vague adherence criteria (eg, “taking prescribed medications,” “regular medication use,” “good adherence”), and as previously noted, a subset of studies utilized prescription claims analysis with a wide variety of cut points for adherence (eg, access to greater than 80% of medications, lack of overuse, fewer than 1 refill in 1 calendar year). Finally, a majority of the studies did not provide a specific description or definition of the adherence classification criteria utilized in the study. Adherence classification for diaries and behavioral lifestyle changes were similarly incongruent as several studies noted specific yet arbitrary percentages (eg, 60%, 80%, 100%) of diary completion in order for participant data to be included in analyses, and other studies described either non-specific requirements to be considered “adherent” (eg, 4 months completed) or no requirements at all. In sum, adherence cut points were often not described or arbitrarily set. It should be noted that the majority of studies reported adherence rates as a secondary outcome rather than adherence as a primary end-point of the study.
Additional methodological shortcomings that are pervasive in current headache treatment adherence literature include a lack of information on how patients are instructed to take medication, the potential discrepancies between a prescribed regimen and the patients’ beliefs about the treatment, and whether adherence data accounts for OTC medication use. Furthermore, several studies with large sample sizes recruited participants from the general population and a diagnosis of headache and/or migraine was based on self-reported symptom questionnaires rather than a medical evaluation. These shortcomings limit the generalizability and direct clinical utility of the current state of the literature. These aforementioned methodological shortcomings are not unique to the headache adherence literature, but the further delineation of these questions would allow for a better understanding of treatment adherence in adult and pediatric patients with headache.
This review has identified several gaps in the current literature which should be the focus of future headache adherence research. First, few studies specifically examined adherence by defining the target behavior, identifying a systematic way to measure the target behavior, and describing a classification system to categorize participants as “adherent” or “nonadherent.” This is not surprising given that the primary research question in many of the studies did not pertain to adherence. Indeed, adherence measurement and analyses appeared to have been deprioritized in most of the studies examining medication use. Self-report questionnaires, prescription claims data, interviews, headache diaries, and behavioral self-monitoring have provided estimates of adherence rates within the current literature, but also have the potential to overestimate adherence and provide no verification of treatment completion (eg, ingestion of medication, practice of relaxation).
Future investigations on medication adherence in headache treatment should be designed to not only systematically assess specific adherence behaviors and classify patients, but should also utilize improved objective measures of adherence where possible. For example, objective measures of adherence such as electronic medication adherence monitoring devices would allow for a better understanding of the number of preventative and acute medications taken and the frequency and duration of nonadherence. In addition, electronic monitoring systems allow for long-term measurement of adherence in real time and have been associated with pharmacy claims data and serum assays in other chronic conditions.67,68 While there is no “gold standard” measure of medication adherence and adherence rates based on electronic monitors cannot guarantee that the patient consumed the medication, electronic monitors are quickly becoming the standard to which other adherence measures are compared.67,69 Because adherence has not been a primary aim of most adult or pediatric headache research, future research would benefit from using a multimethod (eg, electronic monitors, headache diaries, and pharmacy claims data) approach to examine the convergence between measures and identify which methods have the best clinical utility for the individuals with headache.
Another significant gap in the extant research is the relationship between adherence and sociodemographic and psychological/behavioral variables. For example, future studies investigating the relationship of adherence with variables such as age, sex, years with headache, socioeconomic status, health literacy/beliefs, and psychological symptoms would extend the current state of the literature. The only pediatric study in the existing literature examining correlates of adherence demonstrated that adherence is significantly related to child age, perception of the treatment rationale, and initial severity of headaches. Within the adult literature, one study reported that adherence was significantly related to a diagnosis of major depressive disorder and lower levels of headache management self-efficacy while 3 other studies reported no relationship between demographic variables and adherence. Examining risk and protective factors in adherence research will allow health care providers to identify patients in a clinical setting who are at risk for nonadherence and poorer health outcomes. Moreover, delineating correlates of nonadherence would allow for early problem identification and targeting of interventions to improve adherence in a targeted, efficient manner.
The third major gap in the headache adherence literature is the lack of research on interventions to improve treatment adherence. The only study examining interventions to enhance adherence in adults with headache found that adherence to preventative medication improved after receiving patient education. No pediatric studies have examined interventions to improve adherence to headache treatment. Recent meta-analyses examining psychological interventions to promote adherence to treatment in pediatric and adult chronic health conditions demonstrate that adherence interventions are effective and that behavioral and/or multicomponent interventions are particularly potent in improving adherence among chronically ill youth.70,71 Given the rates of nonadherence for individuals28 with headache, the prevalence and chronicity of these diseases, and the complexity of headache treatment, future research should focus on examining the efficacy of behavioral treatments for nonadherence, particularly via randomized controlled trials.
CONCLUSION
The body of literature examining adherence with headache treatment is growing, but remains small. Although additional studies examining adult adherence to headache treatment have been published since the previous review,10 few studies specifically defined and systematically measured adherence and rates of adherence to headache treatment remain varied, but generally consistent with the larger chronic illness literature. The literature pertaining to adherence to headache treatment in children and adolescents is scant and shares many of the same methodological shortcomings as the adult literature. In fact, only 5 pediatric studies assessed medication adherence and none of these studies involved a formal assessment of adherence. Although there is much research to be conducted within the field of headache adherence, the available literature provides evidence to support that nonadherence to treatment is a salient issue to consider for adults and children with headaches. Examining adherence in headache-specific populations is particularly desirable given that unique barriers to adherence might exist with the complexity of treatment regimens prescribed. Given that adults and children with headaches are at risk for poor health-related quality of life,72,73 it is likely that improved self-management and adherence to headache treatment recommendations may not only decrease headache frequency and severity, but also improve health-related quality of life and headache-related disability.
Footnotes
Conflict of Interest: None.
STATEMENT OF AUTHORSHIP
-
Conception and DesignRachelle R. Ramsey; Kevin A. Hommel; Scott W. Powers; Andrew D. Hershey
-
Acquisition of DataRachelle R. Ramsey; Jamie L. Ryan; Kevin A. Hommel
-
Analysis and Interpretation of DataRachelle R. Ramsey; Jamie L. Ryan; Kevin A. Hommel; Scott W. Powers; Andrew D. Hershey; Brandon S. Aylward
-
Drafting the ManuscriptRachelle R. Ramsey; Jamie L. Ryan; Kevin A. Hommel; Scott W. Powers; Andrew D. Hershey; Brandon S. Aylward
-
Revising It for Intellectual ContentRachelle R. Ramsey; Jamie L. Ryan; Kevin A. Hommel; Scott W. Powers; Andrew D. Hershey; Brandon S. Aylward
-
Final Approval of the Completed ManuscriptRachelle R. Ramsey; Jamie L. Ryan; Kevin A. Hommel; Scott W. Powers; Andrew D. Hershey; Brandon S. Aylward
References
- 1.Drotar D. Promoting Adherence to Medical Treatment in Chronic Childhood Illness: Concepts, Methods, and Interventions. Mahwah: Lawrence Eribaum Associates; 2000. [Google Scholar]
- 2.Dunbar-Jacob J, Mortimer-Stephens MK. Treatment adherence in chronic disease. J Clin Epidemiol. 2001;54(Suppl 1):S57–S60. doi: 10.1016/s0895-4356(01)00457-7. [DOI] [PubMed] [Google Scholar]
- 3.Hommel KA, Davis CM, Baldassano RN. Objective vs subjective assessment of oral medication adherence in pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:589–593. doi: 10.1002/ibd.20798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rapoff MA. Adherence to Pediatric Medical Regimens. 2. New York: Springer; 2010. [Google Scholar]
- 5.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 6.Haynes RB. Introduction. In: Haynes RB, Taylor DW, Sackett DL, editors. Compliance in Health Care. Baltimore: Johns Hopkins University Press; 1979. pp. 1–7. [Google Scholar]
- 7.Powers SW, Gilman DK, Hershey AD. Suggestions for a biopsychosocial approach to treating children and adolescents who present with headache. Headache. 2006;46(Suppl 3):S149–S150. doi: 10.1111/j.1526-4610.2006.00568.x. [DOI] [PubMed] [Google Scholar]
- 8.Powers SW, Andrasik F. Biobehavioral treatment, disability, and psychological effects of pediatric headache. Pediatr Ann. 2005;34:461–465. doi: 10.3928/0090-4481-20050601-11. [DOI] [PubMed] [Google Scholar]
- 9.Kabbouche MA, Gilman DK. Management of migraine in adolescents. Neuropsychiatr Dis Treat. 2008;4:535–548. doi: 10.2147/ndt.s495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rains JC, Lipchik GL, Penzien DB. Behavioral facilitation of medical treatment for headache – part I: Review of headache treatment compliance. Headache. 2006;46:1387–1394. doi: 10.1111/j.1526-4610.2006.00581.x. [DOI] [PubMed] [Google Scholar]
- 11.Mulleners WM, Whitmarsh TE, Steiner TJ. Non-compliance may render migraine prophylaxis useless, but once-daily regimens are better. Cephalalgia. 1998;18:52–56. doi: 10.1046/j.1468-2982.1998.1801052.x. [DOI] [PubMed] [Google Scholar]
- 12.Packard RC, O’Connell P. Medication compliance among headache patients. Headache. 1986;26:416–419. doi: 10.1111/j.1526-4610.1986.hed2608416.x. [DOI] [PubMed] [Google Scholar]
- 13.Fitzpatrick RM, Hopkins AP. Effects of referral to a specialist for headache. J R Soc Med. 1983;76:112–115. doi: 10.1177/014107688307600205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foley KA, Cady R, Martin V, et al. Treating early vs treating mild:Timing of migraine prescription medications among patients with diagnosed migraine. Headache. 2005;45:538–545. doi: 10.1111/j.1526-4610.2005.05107.x. [DOI] [PubMed] [Google Scholar]
- 15.Holroyd KA, Powers SW, Andrasik F. Methodological issues in clinical trials of drug and behavior therapies. Headache. 2005;45:487–492. doi: 10.1111/j.1526-4610.2005.05100.x. [DOI] [PubMed] [Google Scholar]
- 16.Gallagher RM, Kunkel R. Migraine medication attributes important for patient compliance: Concerns about side effects may delay treatment. Headache. 2003;43:36–43. doi: 10.1046/j.1526-4610.2003.03006.x. [DOI] [PubMed] [Google Scholar]
- 17.Spierings ELH, Miree LF. Non-compliance with follow-up and improvement after treatment at a headache center. Headache. 1993;33:205–209. doi: 10.1111/j.1526-4610.1993.hed33040205.x. [DOI] [PubMed] [Google Scholar]
- 18.Hoodin F, Brines BJ, Lake AE, III, Wilson J, Saper JR. Behavioral self-management in an inpatient headache treatment unit: Increasing adherence and relationship to changes in affective distress. Headache. 2000;40:377–383. doi: 10.1046/j.1526-4610.2000.00057.x. [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 20.Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: Terminology and definitions. Value Health. 2008;11:44–47. doi: 10.1111/j.1524-4733.2007.00213.x. [DOI] [PubMed] [Google Scholar]
- 21.Katíc BJ, Rajagopalan S, Ho TW, Chen YT, Hu XH. Triptan persistency among newly initiated users in a pharmacy claims database. Cephalalgia. 2011;31:488–500. doi: 10.1177/0333102410383058. [DOI] [PubMed] [Google Scholar]
- 22.Cady RK, Maizels M, Reeves DL, Levinson DM, Evans JK. Predictors of adherence to triptans: Factors of sustained vs lapsed users. Headache. 2009;49:386–394. doi: 10.1111/j.1526-4610.2009.01343.x. [DOI] [PubMed] [Google Scholar]
- 23.Ifergane G, Wirguin I, Shvartzman P. Triptans – why once? Headache. 2006;46:1261–1263. doi: 10.1111/j.1526-4610.2006.00435.x. [DOI] [PubMed] [Google Scholar]
- 24.Panconesi A, Pavone E, Franchini M, et al. Triptans: Low utilization and high turnover in the general population. Cephalalgia. 2010;30:576–581. doi: 10.1111/j.1468-2982.2009.02001.x. [DOI] [PubMed] [Google Scholar]
- 25.Etemad LR, Yang W, Globe D, Barlev A, Johnson KA. Costs and utilization of triptan users who receive drug prophylaxis for migraine vs triptan users who do not receive drug prophylaxis. J Manag Care Pharm. 2005;11:137–144. doi: 10.18553/jmcp.2005.11.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ferrari A, Stefani M, Sternieri S, Bertolotti M, Sternieri E. Analgesic drug taking: Beliefs and behavior among headache patients. Headache. 1997;37:88–94. doi: 10.1046/j.1526-4610.1997.3702088.x. [DOI] [PubMed] [Google Scholar]
- 27.Donnet A, Lanteri-Minet M, Aucoin F, Allaf B. Use and overuse of antimigraine drugs by pharmacy personnel in France: COTA survey. Headache. 2009;49:1014–1021. doi: 10.1111/j.1526-4610.2009.01395.x. [DOI] [PubMed] [Google Scholar]
- 28.The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 29.Linde M, Jonsson P, Hedenrud T. Influence of disease features on adherence to prophylactic migraine medication. Acta Neurol Scand. 2008;118:367–372. doi: 10.1111/j.1600-0404.2008.01042.x. [DOI] [PubMed] [Google Scholar]
- 30.Holroyd KA, Cottrell CK, O’Donnell FJ, et al. Effect of preventive (beta blocker) treatment, behavioural migraine management, or their combination on outcomes of optimised acute treatment in frequent migraine: Randomised controlled trial. BMJ. 2010;341:c4871. doi: 10.1136/bmj.c4871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rahimtoola H, Buurma H, Tijssen CC, Leufkens HG, Egberts AC. Migraine prophylactic medication usage patterns in The Netherlands. Cephalalgia: an international journal of headache. 2003 May;23(4):293–301. doi: 10.1046/j.1468-2982.2003.00494.x. [DOI] [PubMed] [Google Scholar]
- 32.Rahimtoola H, Egberts AC, Buurma H, Tijssen CC, Leufkens HG. Patterns of ergotamine and sumatriptan use in the Netherlands from 1991 to 1997. Cephalalgia: an international journal of headache. 2001 Jun;21(5):596–603. doi: 10.1046/j.1468-2982.2001.00212.x. [DOI] [PubMed] [Google Scholar]
- 33.Seok JI, Cho HI, Chung CS. From transformed migraine to episodic migraine: Reversion factors. Headache. 2006;46:1186–1190. doi: 10.1111/j.1526-4610.2006.00509.x. [DOI] [PubMed] [Google Scholar]
- 34.Hedenrud T, Jonsson P, Linde M. Beliefs about medicines and adherence among Swedish migraineurs. Ann Pharmacother. 2008;42:39–45. doi: 10.1345/aph.1K354. [DOI] [PubMed] [Google Scholar]
- 35.Dozza AL, Krymchantowski AV. Adherence to migraine treatment does not depend on the number of prescribed medications. Arq Neuropsiquiatr. 2013;71:171–173. doi: 10.1590/s0004-282x2013000300008. [DOI] [PubMed] [Google Scholar]
- 36.Krymchantowski A, Tavares C. Weight variations in patients receiving topiramate migraine prophylaxis in a tertiary care setting. [accessed March 14, 2014];Medgenmed. 2004 6:48. Available at: www.medscape.com/viewarticle/482361. [PMC free article] [PubMed] [Google Scholar]
- 37.Heckman BD, Ellis G. Preventive medication adherence in African American and Caucasian headache patients. Headache. 2011;51:520–532. doi: 10.1111/j.1526-4610.2011.01866.x. [DOI] [PubMed] [Google Scholar]
- 38.Rothrock JF, Parada VA, Sims C, Key K, Walters NS, Zweifler RM. The impact of intensive patient education on clinical outcome in a clinic-based migraine population. Headache. 2006;46:726–731. doi: 10.1111/j.1526-4610.2006.00428.x. [DOI] [PubMed] [Google Scholar]
- 39.Gaul C, van Doorn C, Webering N, et al. Clinical outcome of a headache-specific multidisciplinary treatment program and adherence to treatment recommendations in a tertiary headache center: An observational study. J Headache Pain. 2011;12:475–483. doi: 10.1007/s10194-011-0348-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lafata JE, Tunceli O, Cerghet M, Sharma KP, Lipton RB. The use of migraine preventive medications among patients with and without migraine headaches. Cephalalgia. 2010;30:97–104. doi: 10.1111/j.1468-2982.2009.01909.x. [DOI] [PubMed] [Google Scholar]
- 41.Yaldo AZ, Wertz DA, Rupnow MF, Quimbo RM. Persistence with migraine prophylactic treatment and acute migraine medication utilization in the managed care setting. Clin Ther. 2008;30:2452–2460. doi: 10.1016/j.clinthera.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 42.Attar HS, Chandramani S. Impact of physician empathy on migraine disability and migraineur compliance. Ann Indian Acad Neurol. 2012;15(Suppl 1):S89–S94. doi: 10.4103/0972-2327.100025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ezra Y, Gotkine M, Goldman S, Adahan HM, Ben-Hur T. Hypnotic relaxation vs amitriptyline for tension-type headache: Let the patient choose. Headache. 2012;52:785–791. doi: 10.1111/j.1526-4610.2011.02055.x. [DOI] [PubMed] [Google Scholar]
- 44.Ramsden CE, Mann JD, Faurot KR, et al. Low omega-6 vs low omega-6 plus high omega-3 dietary intervention for chronic daily headache: Protocol for a randomized clinical trial. Trials. 2011;12:97. doi: 10.1186/1745-6215-12-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Heckman BD, Holroyd KA, O’Donnell FJ, et al. Race differences in adherence to headache treatment appointments in persons with headache disorders. J Natl Med Assoc. 2008;100:247–255. doi: 10.1016/s0027-9684(15)31213-x. [DOI] [PubMed] [Google Scholar]
- 46.Krymchantowski AV, Jevoux CC. Topiramate vs divalproex sodium in the preventive treatment of migraine: A prospective “real-world” study. Headache. 2011;51:554–558. doi: 10.1111/j.1526-4610.2011.01868.x. [DOI] [PubMed] [Google Scholar]
- 47.Rossi P, Di Lorenzo C, Faroni J, Cesarino F, Nappi G. Advice alone vs structured detoxification programmes for medication overuse headache: A prospective, randomized, open-label trial in transformed migraine patients with low medical needs. Cephalalgia. 2006;26:1097–1105. doi: 10.1111/j.1468-2982.2006.01175.x. [DOI] [PubMed] [Google Scholar]
- 48.Lemstra M, Stewart B, Olszynski WP. Effectiveness of multidisciplinary intervention in the treatment of migraine: A randomized clinical trial. Headache. 2002;42:845–854. doi: 10.1046/j.1526-4610.2002.02202.x. [DOI] [PubMed] [Google Scholar]
- 49.Nappi G, Jensen R, Nappi RE, Sances G, Torelli P, Olesen J. Diaries and calendars for migraine. A review. Cephalalgia. 2006;26:905–916. doi: 10.1111/j.1468-2982.2006.01155.x. [DOI] [PubMed] [Google Scholar]
- 50.Cady R, Martin V, Adelman J, Diamond M, Sajjan S, Hu XH. Migraine treatment with rizatriptan and non-triptan usual care medications: A pharmacy-based study. Headache. 2004;44:900–907. doi: 10.1111/j.1526-4610.2004.04172.x. [DOI] [PubMed] [Google Scholar]
- 51.Allena M, Cuzzoni MG, Tassorelli C, Nappi G, Antonaci F. An electronic diary on a palm device for headache monitoring: A preliminary experience. J Headache Pain. 2012;13:537–541. doi: 10.1007/s10194-012-0473-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tassorelli C, Sances G, Allena M, et al. The usefulness and applicability of a basic headache diary before first consultation: Results of a pilot study conducted in two centres. Cephalalgia. 2008;28:1023–1030. doi: 10.1111/j.1468-2982.2008.01639.x. [DOI] [PubMed] [Google Scholar]
- 53.Moloney MF, Aycock DM, Cotsonis GA, Myerburg S, Farino C, Lentz M. An internet-based migraine headache diary: Issues in internet-based research. Headache. 2009;49:673–686. doi: 10.1111/j.1526-4610.2009.01399.x. [DOI] [PubMed] [Google Scholar]
- 54.Kleiboer A, Sorbi M, Merelle S, Passchier J, van Doornen L. Utility and preliminary effects of online digital assistance (ODA) for behavioral attack prevention in migraine. Telemed J E Health. 2009;15:682–690. doi: 10.1089/tmj.2009.0014. [DOI] [PubMed] [Google Scholar]
- 55.Sorbi MJ, Mak SB, Houtveen JH, Kleiboer AM, van Doornen LJ. Mobile web-based monitoring and coaching: Feasibility in chronic migraine. J Med Internet Res. 2007;9:e38. doi: 10.2196/jmir.9.5.e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hershey AD, Powers SW, Bentti AL, Degrauw TJ. Effectiveness of amitriptyline in the prophylactic management of childhood headaches. Headache. 2000;40:539–549. doi: 10.1046/j.1526-4610.2000.00085.x. [DOI] [PubMed] [Google Scholar]
- 57.Grazzi L, Andrasik F, Usai S, D’Amico D, Bussone G. Pharmacological behavioural treatment for children and adolescents with tension-type headache: Preliminary data. Neurol Sci. 2004;25(Suppl 3):S270–S271. doi: 10.1007/s10072-004-0305-5. [DOI] [PubMed] [Google Scholar]
- 58.Usai S, Grazzi L, Andrasik F, Bussone G. An innovative approach for migraine prevention in young age: A preliminary study. Neurol Sci. 2010;31(Suppl 1):S181–S183. doi: 10.1007/s10072-010-0321-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Usai S, Grazzi L, Bussone G. Gingkolide B as migraine preventive treatment in young age: Results at 1-year follow-up. Neurol Sci. 2011;32(Suppl 1):S197–S199. doi: 10.1007/s10072-011-0522-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Andrasik F, Grazzi L, Usai S, Bussone G. Pharmacological treatment compared to behavioural treatment for juvenile tension-type headache: Results at two-year follow-up. Neurol Sci. 2007;28(Suppl 2):S235–S238. doi: 10.1007/s10072-007-0786-0. [DOI] [PubMed] [Google Scholar]
- 61.Allen KD, McKeen LR. Home-based multicomponent treatment of pediatric migraine. Headache. 1991;31:467–472. doi: 10.1111/j.1526-4610.1991.hed3107467.x. [DOI] [PubMed] [Google Scholar]
- 62.Engel JM. Children’s compliance with progressive relaxation procedures for improving headache control. OTJR (Thorofare N J) 1993;13:219–230. [Google Scholar]
- 63.Wisniewski JJ, Genshaft JL, Mulick JA, Coury DL, Hammer D. Relaxation therapy and compliance in the treatment of adolescent headache. Headache. 1988;28:612–617. doi: 10.1111/j.1526-4610.1988.hed2809612.x. [DOI] [PubMed] [Google Scholar]
- 64.Guibert MB, Firestone P, McGrath P, Goodman JT, Cunningham JS. Compliance factors in the behavioural treatment of headache in children and adolescents. Can J Behav Sci. 1990;22:37–44. [Google Scholar]
- 65.Kabbouche MA, Powers SW, Vockell AL, et al. Outcome of a multidisciplinary approach to pediatric migraine at 1, 2, and 5 years. Headache. 2005;45:1298–1303. doi: 10.1111/j.1526-4610.2005.00261.x. [DOI] [PubMed] [Google Scholar]
- 66.Golden W, Evans JK, Hu H. Migraine strikes study: Factors in patients’ decision to treat early. J Headache Pain. 2009;10:93–99. doi: 10.1007/s10194-008-0091-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Farley J, Hines S, Musk A, Ferrus S, Tepper V. Assessment of adherence to antiviral therapy in HIV-infected children using the Medication Event Monitoring System, pharmacy refill, provider assessment, caregiver self-report, and appointment keeping. J Acquir Immune Defic Syndr. 2003;33:211–218. doi: 10.1097/00126334-200306010-00016. [DOI] [PubMed] [Google Scholar]
- 68.Gerson AC, Furth SL, Neu AM, Fivush BA. Assessing associations between medication adherence and potentially modifiable psychosocial variables in pediatric kidney transplant recipients and their families. Pediatr Transplant. 2004;8:543–550. doi: 10.1111/j.1399-3046.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- 69.Burgess SW, Sly PD, Morawska A, Devadason SG. Assessing adherence and factors associated with adherence in young children with asthma. Respirology. 2008;13:559–563. doi: 10.1111/j.1440-1843.2008.01292.x. [DOI] [PubMed] [Google Scholar]
- 70.Kahana S, Drotar D, Frazier T. Meta-analysis of psychological interventions to promote adherence to treatment in pediatric chronic health conditions. J Pediatr Psychol. 2008;33:590–611. doi: 10.1093/jpepsy/jsm128. [DOI] [PubMed] [Google Scholar]
- 71.Peterson AM, Takiya L, Finley R. Meta-analysis of trials of interventions to improve medication adherence. Am J Health Syst Pharm. 2003;60:657–665. doi: 10.1093/ajhp/60.7.657. [DOI] [PubMed] [Google Scholar]
- 72.Powers SW, Patton SR, Hommel KA, Hershey AD. Quality of life in childhood migraines: Clinical impact and comparison to other chronic illnesses. Pediatrics. 2003;112:1–5. doi: 10.1542/peds.112.1.e1. [DOI] [PubMed] [Google Scholar]
- 73.Terwindt GM, Ferrari MD, Tijhuis M, Groenen SMA, Picavet HSJ, Launer LJ. The impact of migraine on quality of life in the general population: The GEM study. Neurology. 2000 Sep 12;55:624–629. doi: 10.1212/wnl.55.5.624. [DOI] [PubMed] [Google Scholar]