Abstract
Objective
This pilot study conducted an open trial of a manualized adaptation to Family-Based Treatment for Transition Age Youth (FBT-TAY) for Anorexia Nervosa (AN). The aims were: (1) determine the acceptability of FBT for TAY; and, (2) establish preliminary effect sizes for the impact of FBT-TAY on eating disorder behaviour and weight restoration.
Method
Twenty-six participants across two paediatric and one adult hospital site were recruited to participate. Participants completed the Eating Disorder Examination Questionnaire (EDE-Q) at the start of treatment, the end-of-treatment, and three-month follow-up.
Results
FBT-TAY is an acceptable and feasible treatment to all study therapists as evidenced by their fidelity to the model. FBT-TAY is a feasible and acceptable intervention to transition age youth, given only 27.27% chose treatment as usual over FBT-TAY. Participants presented significant improvement at end-of-treatment and three-months post-treatment (p < .001; ES = 0.34) from baseline on the EDE-Q Global Score. Participants also achieved and maintained weight restoration at the end-of-treatment and three-months post-treatment when compared to baseline (p < .0001, ES = 0.54).
Conclusions
FBT-TAY, the first manualized AN treatment for TAY, demonstrated feasibility and acceptability with therapists and participants as well as improvement for participants in EDE-Q global score and weight. Given the current dearth of effective treatments for TAY with AN, FBT-TAY is a promising adaptation of FBT. A larger clinical trial with a 12-month follow-up is recommended.
Keywords: anorexia, family-based treatment, transition age youth, eating disorders, family therapy
Résumé
Objectif
Cette étude pilote a mené un essai ouvert de l’adaptation dans un manuel du traitement familial pour jeunes en âge de transition (TF-JAT) pour l’anorexie mentale (AM). Les objectifs étaient: (1) déterminer l’acceptabilité du TF pour les JAT; et (2) établir des tailles de l’effet (TE) préliminaires pour l’effet du TF-JAT sur le comportement du trouble alimentaire et la reprise de poids.
Méthode
Vingt-six participants dans deux centres pédiatriques et un hôpital pour adultes ont été recrutés pour participer. Les participants ont répondu au questionnaire d’examen sur les troubles alimentaires (EDE-Q) au début du traitement, à la fin du traitement, et au suivi de 3 mois.
Résultats
Le TF-JAT est un traitement acceptable et faisable pour tous les thérapeutes de l’étude comme en atteste leur fidélité au modèle. Le TF-JAT est une intervention faisable et acceptable pour les jeunes en âge de transition, étant donné que seulement 27,27% ont choisi le traitement habituel plutôt que le TF-JAT. Les participants ont présenté une amélioration significative au score global du EDE-Q à la fin du traitement et au suivi de trois mois (p < 0,001; TE = 0,34) comparé au début. Les participants ont également réussi à reprendre du poids et à le maintenir à la fin du traitement et au suivi de 3 mois comparé au début (p < 0,0001, TE = 0,54).
Conclusions
Le TF-JAT, le premier traitement de l’AM dans un manuel pour les JAT, a démontré faisabilité et acceptabilité chez les thérapeutes et les participants ainsi qu’une amélioration pour les participants au score global de l’EDE-Q et de leur poids. Étant donné la rareté actuelle de traitements efficaces pour les JAT souffrant d’AM, le TF-JAT est une adaptation prometteuse du TF. Un essai clinique plus vaste avec suivi de 12 mois est recommandé.
Mots clés: anorexie, traitement familial, jeunes en âge de transition, troubles alimentaires, thérapie familiale
Anorexia nervosa (AN) is a serious mental disorder with significant psychological and medical morbidity, increased mortality and diminished quality of life (Zipfel, Giel, Bulik, Hay & Schmidt, 2015). Research shows that one in five deaths in AN is due to suicide (Smink, van Hoeken & Hoek, 2012), and malnutrition and starvation contribute to severe medical complications such as cardiac failures, seizures and osteoporosis (Vo, Lau & Rubinstein, 2016; Westmoreland, Krantz & Mehler, 2016). To date, family-based treatment (FBT) has been the leading evidence based psychosocial treatment of AN for children and adolescents (Agras et al., 2014; Le Grange et al., 2016; Lock et al., 2010). Approximately one third of participants achieve remission (defined as Expected Body Weight + within one Standard Deviation of the Global Eating Disorder Examination), and a similar percent of participants remain remitted four years post-treatment (Le Grange, Accurso, Lock, Agras, & Bryson, 2014). A multi-site randomized controlled trial (RCT), comparing FBT to systemic family therapy, demonstrated that FBT led to more rapid weight restoration and fewer hospitalizations than systemic family therapy (Agras et al., 2014). FBT is designed to create a sense of urgency in parents by emphasizing the need for parental involvement to address emaciation, loss of menses and starvation (Lock & Le Grange, 2015). A primary goal of FBT for AN is the achievement of weight restoration to ameliorate medical instability and to minimize long-term health consequences that often accompany starvation and malnutrition.
FBT for AN consists of three phases. In phase one, the focus is on the enhancement of parental self-efficacy over AN, through which parents take chief responsibility for weight restoring their child by closely preparing and monitoring their meals. In phase two, parents hand control over eating back to the adolescent who incrementally eats their meals with greater independence. In phase three, the family discusses adolescent developmental issues and terminates treatment. There are five therapeutic principles that form the foundation of FBT: an agnostic view of the illness, a non-authoritative stance of the clinician, parental empowerment, externalization of the illness, and encouragement of sibling support (Lock & Le Grange, 2015.
Adolescents who respond well to early interventions, such as FBT, have better health outcomes (Darcy et al., 2013; Doyle, Le Grange, Loeb, Doyle & Crosby, 2010; Le Grange et al., 2014; Lock, Couturier, Bryson & Agras, 2006; Treasure & Russell, 2011) than those who develop a protracted course into adulthood (Arcelus, Mitchell, Wales & Nielsen, 2011; Fairburn & Harrison, 2003; Touyz et al., 2013). There are limited treatments available for adults with AN who are often characterized by poor treatment outcomes and high rates of relapse (Hay, Touyz & Sud, 2012; Touyz et al., 2013; Zipfel et al., 2014). Previous research shows that FBT might be less effective for older adolescents than for younger adolescents with AN (Eisler et al., 1997; Le Grange et al., 2012). In a recent feasibility and acceptability study for young adults and their family members, Chen et al. (2016) found that FBT is suitable for this patient population. In this study, four adaptations were made to FBT: 1) the young adult had the discretion to choose whom to involve in their treatment; 2) a collaborative therapeutic stance with the young adult; 3) increased focus on developmental issues; and, 4) incorporation of individual sessions in phase three. However, this study did not manualize the adaptations, the number of individual sessions received by participants in phase 3 was not tracked, on average, participants received relatively few sessions (12 rather than the 18–20 originally proposed), and nine out of 22 participants dropped out of treatment (Chen et al., 2016).
Some clinicians have questioned the appropriateness of using FBT, in its current format, with older adolescents and young adults who may be experiencing a multitude of transitions in their lives (Dimitropoulos et al., 2015a), including a transfer of care from paediatric to adult mental health services where, typically, adults are solely responsible for directing their treatment rather than their parents (Davidson & Cappelli, 2011). Transition age youth (TAY) (16 to 25 years) have been identified as distinct from both adolescents and older adults since many continue to reside with their family of origin and/or receive substantial financial and emotional support from their family members. In the context of eating disorders, young adults with this illness have been shown to simultaneously strive for independence, but also desire parental involvement and support especially while in treatment (Dimitropoulos & Freeman, 2016).
In a recent study, clinicians were asked to discuss how they were using FBT, whether similarly or differently, with children, adolescents, and young adults (Dimitropoulos et al., 2015a; Dimitropoulos, Lock, Le Grange & Anderson, 2015b). Like Chen et al. (2016), clinicians reported that they developed a more collaborative stance with TAY and their families in contrast to FBT for children and younger adolescents. For instance, in the second and third phases of FBT, clinicians also reported working with parents and TAY to practice eating with greater independence in a variety of contexts, e.g., on campus, at work and with their peers. These adaptations to the FBT model were seen as necessary in the face of increased autonomy and independence, as well as the pending transfer of care from paediatric to adult services where treatment is less likely to integrate the family.
Findings from the aforementioned qualitative studies led to the development of a manualized treatment of family-based treatment for transition age youth (FBT-TAY) (Dimitropoulos et al., 2015a; 2015b). FBT-TAY builds on the foundational model of FBT for adolescents with AN and Bulimia Nervosa (BN) (Le Grange & Lock, 2009; Lock & Le Grange, 2015, but has incorporated fundamental changes that are responsive to the unique developmental needs of older teenagers and young adults. The primary aim of the present study was to assess the feasibility and acceptability of a manualized model of FBT adapted for TAY in paediatric and adult specialized eating disorder programs. The second aim of this pilot study was to estimate the clinical impact of FBT-TAY on the primary outcome (eating behaviours) and secondary outcome (weight restoration). This study hypothesized that FBT-TAY would bring about improvements in eating behaviours, as measured by the EDEQ, and weight restoration at end of treatment (EOT) and at three-month follow-up.
Methods
Data Collection
From August 2014 to September 2016, we conducted a pilot study using an open trial of FBT-TAY methodology to assess the (1) acceptability and feasibility, as well as (2) the impact of FBT-TAY on eating disorder psychopathology and weight. This open trial was conducted at three different hospital sites in Ontario, Canada: one specialized adult eating disorder treatment and two paediatric eating disorder treatment programs.
The study obtained ethics approval from all participating hospital sites. Treatment as usual (TAU) in all three sites requires participants to achieve weight restoration, and to reduce or abstain from eating disorder behaviours, such as restriction, exercising, and binge eating, before discharge. Toronto General Hospital provides intensive day hospital (4–6 weeks) and inpatient (4–6 months) treatment for individuals with eating disorders at or over the age of 17. Therapy within the program uses Cognitive Behavioural Therapy and Dialectical Behavioural Therapy principles. Family-work is incorporated within the inpatient and day treatment programs at the request of the patient, but is not required for participation in treatment. North York General Hospital offers an intensive outpatient program for adolescents with eating disorders between the ages of 12 to 19. The program is founded on FBT principles and offers outpatient FBT or day hospital treatment. Family work is intrinsic to the program. The Hospital for Sick Children provides intensive treatment for eating disorders up to age 18 through their inpatient program for medical stabilization, their outpatient program which offers FBT, and their day hospital program which consists of skills and arts based group therapy including cognitive behavioural therapy.
At each hospital site, recruitment occurred at the time of assessment in their respective eating disorders programs; potential participants were presented with information regarding the study treatment alongside TAU, and referred to the study coordinator if they were eligible to participate in the FBT-TAY study. Recruitment also occurred through referrals from the community, other treatment facilities, and student health and counselling services at local universities. A screening process was administered to ensure eligibility for the study. Following the screening process, all participants received a comprehensive assessment by a psychologist or psychiatrist to confirm diagnosis and study eligibility. Participants were eligible for the study if they met diagnostic criteria for AN, were age 16.5 to 25, were medically stable to receive outpatient treatment and were willing to involve supportive others in family based treatment. Exclusion criteria consisted of previous history of FBT, acute suicidality, medical instability, current substance abuse, psychosis, and current family violence. Using DSM-5 criteria, the assessment ensured participants had a diagnosis of AN (restrictive or binge-purge subtype), and were not currently meeting any study exclusion criteria. At the point of assessment, participants were asked to identify whom they would be including in their treatment. After assessment, the study participants met with the study coordinator to undergo the informed consent process and schedule their first appointment for FBT-TAY.
Family-Based Treatment for Transition Age Youth with Anorexia Nervosa
FBT-TAY consists of 25 sessions. Sessions were once weekly throughout phase one and part of phase two. In collaboration with the study therapists and the family, sessions were spread to bi-monthly partway through phase two and for the duration of phase three. Family was defined broadly and could be a parent, sibling, extended family member, partner, friend, or supportive other. Family members were chosen by the participant with AN following the informed consent process and prior to starting the first session of FBT TAY.
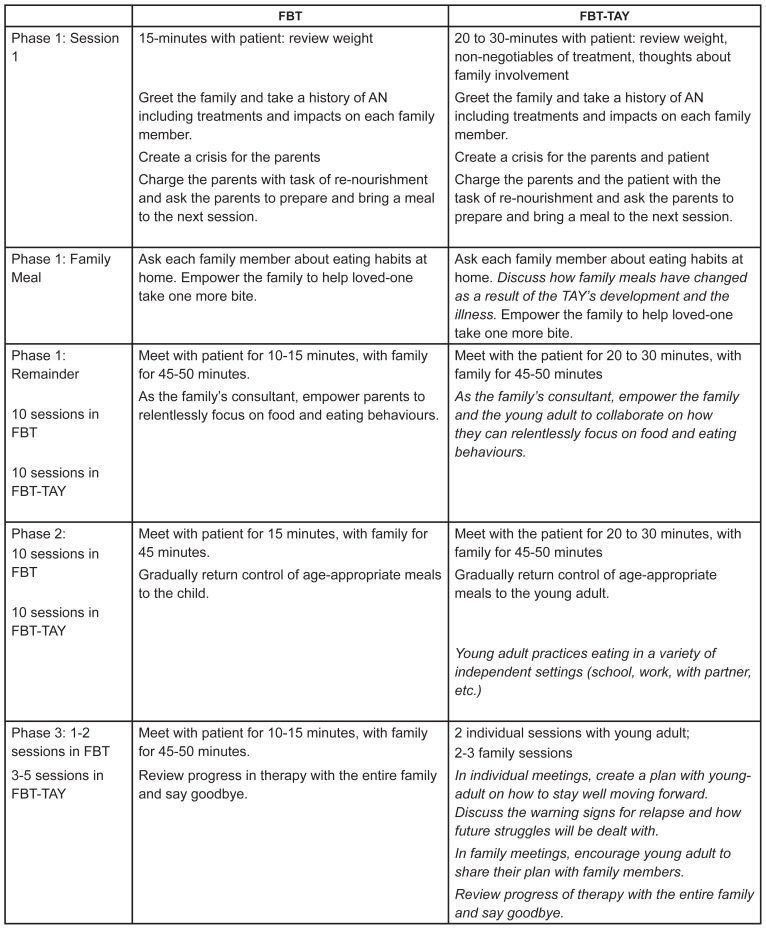
FBT was adapted for TAY throughout all three phases of the model (Figure 1). One change that spanned across all phases was the integration of increased individual time with the TAY. Before each family session (duration 50 minutes), the participant met with their study therapist for a one-on-one 20 to 30-minute session. In these sessions, the study therapist weighed the participant. Participants were asked to reflect on their progress with both the quality and quantity of eating and to identify what supportive practices they would like to solicit from their supportive other(s) to facilitate their progress. Participants were made aware in the first session of FBT-TAY that sharing weight and any information pertaining to the eating disorder or other mental health issues could not be kept confidential. Details about relationships, and other more personal struggles (e.g., sexuality) were kept confidential.
Figure 1.
Summary of Family-Based Treatment Versus Family-Based Treatment for Transition Age Youth
In phase one (approximately sessions 1–10), the participant and family members were encouraged to work collaboratively against the eating disorder with the study therapist working as their consultant. The family members were asked to support their loved one during mealtimes and provide symptom monitoring. The participant was asked to describe what kind of support they needed from their family members during meal times. In this way, the participant had a say in how their treatment was delivered. In the second phase of treatment (approximately session 11 onward), control over meals was returned to the participant and there was a larger emphasis on what they needed to eat in developmentally appropriate situations (e.g. eating on campus, preparing meals independently, etc.). Finally, in the third phase of FBT-TAY (approximately four sessions), the participant attended two to three individual sessions to develop a plan to maintain recovery and focused on age-appropriate transition issues (e.g., transition to school, work, or living with a partner or friends). In one to two family sessions, the participant shared this plan with their family. Common topics throughout phase three were warning signs of relapse, planning for re-integration into life and identifying next steps to achieve long-term life goals, such as post-secondary education, and repairing friend and family relationships.
Study Therapists
Study therapists at each site received the standard training (1.5 day workshop) in the foundational model of FBT for AN with one of the founders of this treatment modality (Author DLG). Following this training, all the study therapists were trained in FBT-TAY during a 1.5-day intensive workshop with the principal investigator GD (PI: GD) and DLG. After receiving training in the foundational and adapted FBT version for TAY, all study therapists had a pilot participant to ensure fidelity to the model. All of the sessions were recorded and carefully reviewed by the PI who offered weekly supervision with the study therapists at each site to maintain adherence to the model. The study therapists also completed a fidelity measure to assess their adherence to the model and described when drift occurred in each session. All therapists were employed at participating hospital sites and held at least a Master’s degree (MSW = 3; MD Psychiatry = 2; Psychologist = 1). The average years of experience in eating disorders treatment was 12.5 years (SD = 8.34) with a range of five to 22 years.
Measures
Feasibility and Acceptability
Feasibility and acceptability of FBT-TAY were evaluated in the following ways: 1) acceptability of FBT-TAY by the study therapists by maintaining fidelity to the model and regular attendance in weekly supervision; 2) acceptance of FBT-TAY over treatment as usual (TAU); and, 3) participant completion of treatment (retention). To assess acceptability of FBT-TAY, two paediatric and an adult eating disorder program were selected with clinicians who had variable training in FBT and clinicians who had no exposure to any family therapy training. The paediatric systems both delivered standard FBT for adolescents while family involvement in the adult program was optional. The study therapists completed a fidelity measure and documented if and when drift to the model occurred. The principal investigator (GD) reviewed the fidelity measures and discussed adherence to the model with study therapist in weekly supervision. To determine acceptability of FBT-TAY to the participants, we tracked acceptance of this intervention by TAY compared with treatment as usual, and the willingness of TAY to involve their family members in treatment. Finally, we assessed feasibility by retention rates in the treatment.
Eating Disorder Behaviour
Participants were assessed at baseline (time 1), at the EOT (time 2), and three-months follow-up (time 3). The primary outcome was the Eating Disorder Examination Questionnaire (EDE-Q) global score. The EDE-Q (Fairburn & Beglin, 1994) is a 33-item self-report measure with four subscales (Restraint, Weight Concern, Shape Concern and Eating Concern). The reliability of each subscale is high, with a minimum Cronbach’s alpha of .78 and maximum of .93 during the test-retest period. The scale also produces excellent internal consistency with Pearson’s r ranging from .81 to .94 across the four subscales (Luce & Crowther, 1999). The EDE-Q global score is calculated based on the mean of all subscale scores.
Weight Restoration
The secondary outcome was weight restoration, defined as percent of the Median Body Mass Index (MBMI) (Centres for Disease Control and Prevention, 2009). In adolescents, MBMI is defined as the 50th percentile for age and sex (Flegal & Cole, 2013), which is a “moving target” that increases rapidly during adolescent growth acceleration. In adults, MBMI plateaus as it approaches 22 Kg/m2 in young women age 20. Therefore, as with previous studies of AN (Garber, Michihata, Hetnal, Shafer, & Moscicki, 2012; Garber et al., 2013), we used the MBMI for each adolescent participant according to their individual age at each time point, and we used BMI 22 Kg/m2 as the median for all adult participants (≥ 18 years). The weight restoration outcome reported at baseline, EOT and follow-up was calculated by dividing the participants’ BMI by the MBMI and multiplying by 100. Height and weight was measured at baseline by a nurse using a medical grade stadiometer at each hospital site. As the mean age of the study sample was 18.5 years, which is past the linear growth spurt for boys and girls, it was not expected for height to change significantly within the 25 study sessions and therefore height was not reassessed. Furthermore, patients were asked to self-report height at the EOT of follow-up questionnaires and no differences were noted in pediatric patients. Weight was measured at each session of FBT-TAY by the study therapist using a medical grade scale on a hard (non-carpeted) surface. Weight at the three-month follow-up period was self-reported on the EDE-Q since participants were not actively being seen in the treatment centre.
Analyses
The aims of the study were as (1) to determine the feasibility and acceptability of FBT for TAY, and (2) to assess the impact of FBT-TAY on eating disorder behaviour and weight restoration. Analyses were performed in IBM SPSS Statistics Version 24. An analysis of variance (ANOVA) was conducted on the EDE-Q global score and %MBMI at baseline, EOT, and three-months follow-up. A repeated measures analysis of variance (ANOVA) was conducted on the EDE-Q global score and weight gained from baseline to EOT, and three-months follow-up in order to determine whether the changes in these outcome variables between time points were statistically significant. For each ANOVA, we report the effect size as partial eta-squared.
Missing outcome data was addressed using intent-to-treat (last observation carried forward). Every participant who consented to the study was analyzed at all three time points, regardless of their study completion or withdrawal (c.f. Chen et al. 2016; Couturier, Kimber, & Szatmari, 2012; Stein, Wing, Lewis, & Raghunathan, 2011). This analysis was conducted in order to mimic real-world applicability of the data, retain a higher sample size for analysis, and remove potential bias from an analysis that excludes those who withdrew from treatment prematurely. There were no significant differences between participants who completed FBT-TAY and those who dropped out before four weeks with regard to duration of illness, age of onset, baseline EDE-Q global score, and weight restoration.
Results
Twenty-six participants diagnosed with AN between the ages of 16 and 22 were recruited for this pilot study open trial. The mean age of the sample was 18.15 years (SD = 2.11; range of 16 – 22). The mean age for adolescent patients was 16.6 (SD = 0.51) years, and the mean age for adult patients was 19.82 (SD = 1.66) years. The sample consisted of 25 females and 1 male. Three participants reported that they were in committed relationships. The rest of the participants identified as single. The sample consisted of mainly Caucasian individuals (61.5%) and the rest of the sample identified as bi-racial (7.7%), Indian (3.8%), Hispanic (11.5%), Asian (11.5%), and Persian (3.8%). The majority lived with their families (24 out of 26). All of the participants elected to live with their families (even if they were not previously living with them) in the first phase of treatment. The mean duration of illness was 27.50 months (SD = 26.61), or 2.29 years (SD = 2.22). All left school for the first phase of treatment, but resumed school in phase two. On average, participants attended 14.54 sessions (SD = 6.65, range of 22). For participant and family demographics, please see Table 1. Of the 26 participants in this study, 15 were diagnosed with one to two comorbid disorders by a psychiatrist at the baseline assessment. Comorbid disorders included Obsessive Compulsive Disorder, Major Depressive Disorder, Generalized Anxiety Disorder, and Social Anxiety Disorder.
Table 1.
Baseline sample characteristics
| Patients (n = 27) | Caregivers (n = 50) | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| n | Percent or Mean | SD | n | Percent or Mean | SD | |
| Age | 18.10 | 2.10 | 46.00 | 12.60 | ||
| Gender | ||||||
| Female | 26 | 96.30 | 30 | 60.00 | ||
| Male | 1 | 3.70 | 20 | 40.00 | ||
| Race | ||||||
| Caucasian | 17 | 63.00 | 36 | 72.00 | ||
| Non-Caucasian | 10 | 37.00 | 14 | 28.00 | ||
| Marital Status | ||||||
| Single | 24 | 89.00 | 25 | 50.00 | ||
| Partnered/Married | 3 | 11.00 | 25 | 50.00 | ||
| Living Situation | ||||||
| With family, relatives, friends or partner | 25 | 93.00 | 13 | 86.00 | ||
| Student residence | 2 | 7.00 | 7 | 14.00 | ||
| Education | ||||||
| Some high school | 12 | 44.00 | 3 | 6.00 | ||
| High school diploma | 6 | 22.00 | 4 | 8.00 | ||
| Some undergraduate university | 6 | 22.00 | 3 | 6.00 | ||
| Undergraduate university degree | 2 | 7.00 | 26 | 52.00 | ||
| Some graduate education | 0 | 0.00 | 1 | 2.00 | ||
| Graduate degree or higher | 1 | 4.00 | 13 | 26.00 | ||
| Employment | ||||||
| Part-time | 7 | 25.90 | 5 | 10.00 | ||
| Summer employment | 1 | 3.70 | 0 | 0.00 | ||
| Unemployed | 15 | 55.50 | 7 | 14.00 | ||
| Student full-time | 1 | 3.70 | 2 | 4.00 | ||
| Employed full-time | 3 | 11.10 | 33 | 66.00 | ||
| Homemaker | 0 | 0.00 | 2 | 4.00 | ||
| Disabled | 0 | 0.00 | 1 | 2.00 | ||
| Religion | ||||||
| Christian | 13 | 48.10 | 26 | 52.00 | ||
| None | 10 | 37.00 | 13 | 26.00 | ||
| Judaism | 1 | 3.70 | 6 | 12.00 | ||
| Atheist | 1 | 3.70 | 1 | 2.00 | ||
| Hindu | 1 | 3.70 | 3 | 6.00 | ||
| Muslim | 1 | 3.70 | 1 | 2.00 | ||
| Duration of Illness (months) | 26.90 | 26.30 | N/A | N/A | ||
| Age of onset | 15.70 | 2.30 | N/A | N/A | ||
| Purging status - average number of days vomited over the past 28 days | 2.70 | 7.50 | N/A | N/A | ||
| Purging status - average number of days taken laxatives over the past 28 days | 1.20 | 5.7 | N/A | N/A | ||
Treatment Feasibility and Acceptability
The study was designed to test the feasibility and acceptability of FBT-TAY in both paediatric and adult hospital settings as the target age group bridges across both systems. Feasibility and acceptability of the FBT-TAY protocol at each hospital site was assessed using a fidelity measure and during weekly supervision between the PI (GD) and study therapists. The goal of supervision was to address any issues in implementing FBT-TAY within the hospital systems as well as any therapist deviations from FBT-TAY. FBT-TAY was conducted without issue at both paediatric and adult hospital sites and therapists did not cite major deviations from the model. Study therapists with different levels of training in family therapy in both the paediatric and adult programs found the FBT-TAY to be an acceptable treatment and closely followed the manualized protocol.
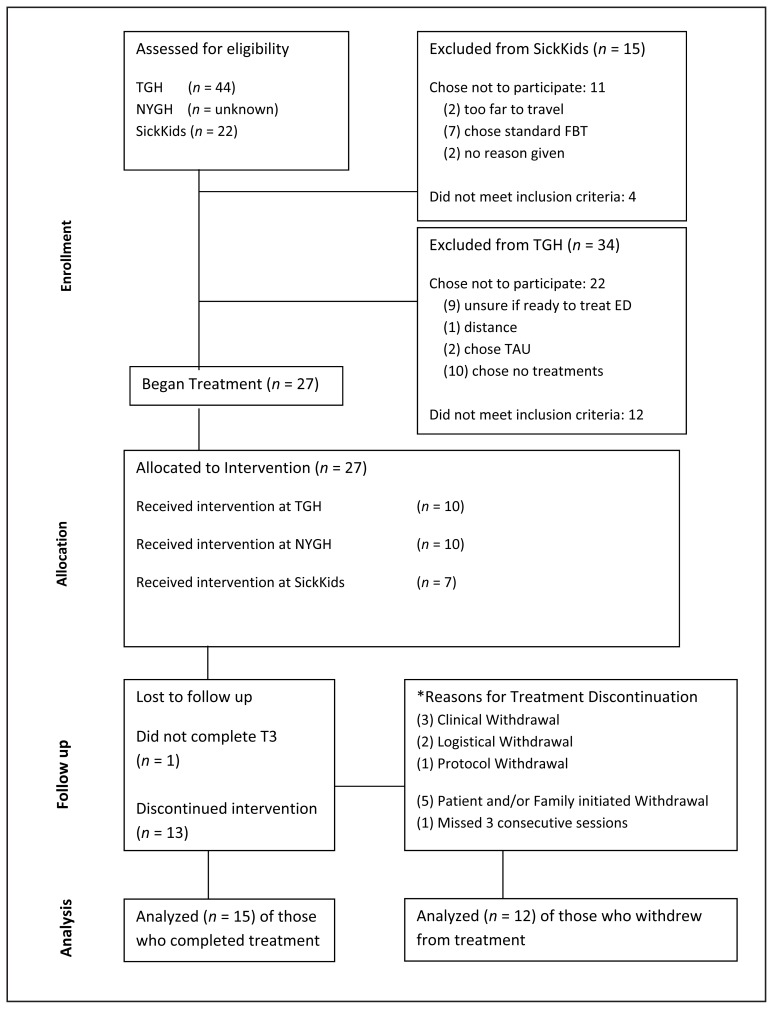
Acceptability and feasibility of the study treatment was evaluated based on the number of participants accepting study treatment over TAU and the retention of individuals in the study. Based on these criteria, the FBT-TAY treatment appears to be both feasible and acceptable to TAY and their families. All of the TAY elected to have their family members participate in their treatment and only three (11.54%) involved friends or a partner. Of those approached for treatment who met inclusion criteria (N = 60), 45.0% (n = 27) accepted FBT-TAY. Further, of the 55.0% (n = 33) who did not express an interest in FBT-TAY, only 27.27% (n = 9) accepted TAU at that time. The remainder of the potential participants declined all treatments for their eating disorder. Common reasons for declining care included ambivalence about engaging in treatment to address the illness and low readiness for change. Of those that chose to participate in treatment one was removed from analysis by the study team for having a high BMI at the start of treatment.
Treatment acceptability was also determined by participant retention. Of the 26 study participants, 12 withdrew (46.15%) and only 5/26 (19.23%) withdrew within four weeks of treatment. Categories for withdrawal were based on criteria for dropout described by DeJong, Broadbent, and Schmidt (2012). With respect to clinical withdrawals (n = 3), one participant left the study because they were acutely suicidal and two required intensive inpatient treatment due to medical instability. Participants also withdrew for logistical reasons (n = 2); one family commuted seven hours to the treatment setting and another family lacked the financial means to attend treatment regularly. One participant was withdrawn (n = 1) due to a protocol deviation (sought concurrent treatment for a co-morbid diagnosis concurrently with FBT-TAY). Participants and family members initiated a withdrawal (n = 5) from the program: One participant withdrew because they were highly invested in their athletic career and maintaining a low body weight and four families initiated withdrawal from the study due to an inability to tolerate witnessing their child’s distress while undergoing treatment. Finally, a participant (n=1) was withdrawn as they missed three consecutive sessions.
Eating Disorder Behaviour and Weight Restoration
Table 2 presents descriptive statistics of all primary and secondary outcome variables by treatment time-point. At the p < 05 level, the total mean score of global EDE-Q significantly improved over time from baseline (M = 3.14; SD = 1.91) to EOT (M = 1.97, SD = 1.78) (p = .001) and three-months follow-up (M = 2.01, SD = 1.72) (p = .001). The corresponding partial eta squared, a measure of effect size was 0.34. The %MBMI at baseline (M = 82.80, SD = 6.41) was significantly lower compared to the MBMI achieved at EOT (M = 91.11, SD = 7.74) (p = .0001), and three-months follow-up (M = 90.05, SD = 7.95) (p = .0001). The corresponding partial eta squared was 0.54. For descriptive purposes only, mean BMI and MBMI are presented in Table 3 by age group (adolescents and young adults).
Table 2.
Primary and Secondary Outcomes (n = 27)
| Baseline | End of treatment | 3 month follow-up | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| Primary Outcome | ||||||
| EDE-Q Global Score | 27 | 3.20 (1.90) | 27 | 2.07 (1.81) | 27 | 2.11 (1.76) |
| Significance | 0.006 | 0.006 | 0.006 | |||
| Partial eta-squared | 0.34 | |||||
| Secondary Outcome | ||||||
| Weight Restoration | 27 | 89.00 (6.04) | 27 | 95.76 (6.07) | 27 | 94.89 (6.44) |
| Significance | 0.001 | 0.001 | 0.001 | |||
| Partial eta-squared | 0.61 | |||||
Note. EDE Global = Eating Disorder Examination Global score.
Table 3.
BMI across treatment timepoints broken down by age grouping
| Baseline | End of treatment | 3 month follow-up | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| BMI Percentile (Patients 16 – 20 Years of Age) | 22 | 14.48 (15.73) | 22 | 31.74 (21.85) | 22 | 34.45 (23.12) |
| BMI (Patients 20.1 – 22 Years of Age) | 5 | 17.67 (0.95) | 5 | 19.72 (2.23) | 5 | 20.07 (2.61) |
Discussion
This is the first open trial of a manualized FBT-TAY treatment for TAY in paediatric and adult specialized eating disorder programs. Historically, FBT has been studied for adolescents between the ages of 12 and 18 (Couturier et al., 2013), and typically has shown diminished outcomes for older adolescents or those with a more chronic illness (Eisler et al., 1997). Based on the findings of the present study, FBT-TAY is feasible in specialized paediatric and adult programs and acceptable to study therapists and to TAY and their families. The study also showed that FBT-TAY resulted in statistically significant reductions in Global EDE-Q scores at the end-of-treatment and three-months follow-up, as well as statistically significant increases in weight from baseline to end-of-treatment and three-months follow-up. Furthermore, of those participants who completed treatment, all achieved weight restoration by end-of-treatment, however, weight started to decline at three-months follow-up for a few participants. These findings are congruent with prior studies regarding the improvements in weight in FBT for adolescents with AN (e.g. Le Grange et al., 2016; Lock et al., 2006). Our findings are promising as weight gain in adolescents with AN has been found to significantly improve psychological recovery (eating disorder psychopathology, depression and self-esteem) at end-of-treatment as well as up to one-year follow-up (Accurso, Ciao, Fitzsimmons-Craft, Le Grange et al., 2014; Lock & Le Grange, 2015 Lock et al., 2013). Given that some of our participants experienced a decline in weight at time three, our findings suggest that continual familial support of TAY during follow-up is essential for sustaining recovery overtime. In contrast to younger adolescents who continue to reside with their families, many of our participants transitioned to post-secondary school and lived independently decreasing the ability of family members to identify and promptly intervene when eating behavious begin to present themselves again.
Our findings underscore those of a recent proof-of concept investigation (Chen et al., 2016), which showed the application of FBT for young adults to have positive results in terms of weight gain and EDE-Q scores for young adults with AN and atypical AN. In this sample, 15/22 achieved their weight gain goals, 13/22 maintained weight gain at 12-months follow-up and 10/22 reduced their EDE-Q global functioning score to below clinical cut-offs. Overall, evidence is building that an adaptation of FBT for young adults is a feasible avenue of treatment.
Interestingly, the majority of participants (>95%) chose to participate in FBT-TAY with their family of origin even though they had the option to invite their peers, or partners (if present). Only three participants (11.54%) included a partner or friend to expand their support system. This finding is consistent with Chen et al. (2016) who found young adults typically invited their parents, even though they have the option of including others. It is important to note that more than 90% of our sample chose to live with parents especially in the first phase of treatment when the focus is on eating and weight gain. Our finding provides preliminary evidence that the inclusion of parents in treatment of AN beyond the paediatric system may be helpful for young adults, especially those who are still cohabitating with their parents. Given that our sample included older adolescents and young adults 16–22, the feasibility of using the manualized FBT model for a broader age of TAY (up to the age of 25) is needed. Only a small number of young adults were treated in the adult system therefore additional research is needed to test the feasibility and acceptability of employing FBT-TAY in adult eating disorder programs. For systems that continue to offer FBT for older adolescents (up to age 18), we would strongly recommend that the foundational model of FBT for adolescents with AN be used. There is significant evidence to support the effectiveness of FBT for adolescents up to the age of 18 whereas there is only preliminary results for FBT TAY for this age group. Finally, the high dropout rate in our study and Chen and her colleagues work raises questions about the unique challenges of engaging TAY whose emerging independence creates increasing opportunities for them to withdraw from family based treatments (and treatments in general). In Western societies, independence from one’s family is expected if not celebrated making it more challenging for parents to insist that their young adult stay in treatment. Future adaptations are required in FBT-TAY with a focus on developing clinical interventions that addresses the ego-syntonic nature of the illness, and parental empowerment to assist young adults even if the support does not seem developmentally appropriate.
Clinical Implications and Future Directions
Current treatments for adults with AN are largely ineffective and the FBT-TAY model attends to young adults with this disorder who are in need of effective treatments. The FBT-TAY model empowers families to continue support across the artificial divide of paediatric to adult treatment systems. Our findings should encourage clinicians to continue including families in the treatment of AN for individuals over the age of 18 with careful attention to issues of autonomy, independence and collaboration with the young adult. Clinicians should take note of the older teenager or young adult’s developmental stage (living at home, at school, financial dependence, etc.), and use this information to inform the integration of families in therapy. In future research, a sufficiently powered RCT of FBT-TAY, with a 12-month follow-up, should be conducted to better understand the efficacy of the model. An RCT comparing FBT-TAY to CBT is recommended especially given preliminary findings on CBT with adolescents in inpatient settings (Dalle Grave, Calugi, Doll, & Fairburn, 2013).
Strengths and Limitations
This study outlines an important advancement in the use of FBT-TAY, and provides preliminary evidence that FBT-TAY is a potentially helpful treatment for individuals with AN between the ages of 16 and 25. The study was conducted across multiple hospital sites, both paediatric and adult, increasing the real-world applicability of the findings as study participants experienced the treatment within a variety of settings. The study treatment was manualized and all study therapists were rigorously trained in the model, and given thorough supervision to ensure fidelity to the model. Furthermore, intention-to-treat analysis strengthened the study findings by ensuring all participants were included in the analyses at all three time points; reducing the chance of a false positive result as both participants who completed and withdrew are accounted for in outcome findings.
There are several limitations that should be taken into account when interpreting the results of this study. Given the high rate of relapse associated with AN, a three-month follow up is clearly not sufficient as a true estimate of maintenance of treatment response. However, it is important to note that this was a pilot study to assess the feasibility and preliminary impact of FBT-TAY on the primary and secondary outcome. A second limitation is that weight at follow-up was established via self-report. Given that participants with AN often over-estimate their weight, it is possible that this time point did not provide an accurate reflection of weight. A third limitation is that our sample size is modest with a 46.15% drop-out rate, although both of these are comparable to that of a recent study on FBT for young adults with AN and atypical AN (Chen et al., 2016), and other studies on adults with AN (Halmi et al., 2005, Watson & Bulik, 2013). Finally, although study therapists were supervised to monitor their adherence to the model, in future standardized fidelity forms should be used to assess drift from the model from the perspective of the therapist, family members and affected individuals.
Conclusion
We have described the feasibility and preliminary effectiveness of a manualized FBT for TAY with AN. FBT-TAY seems feasible for this population, and produced statistically significant improvements in global EDE-Q scores at the end-of-treatment and three-month follow-up, and weight restoration for participants who completed the treatment, with statistically significant weight gain through follow-up. FBT-TAY should be considered for further study and implementation with TAY who are otherwise lacking effective treatment options for AN.
Figure 2.
Consort Diagram
Acknowledgements/Conflicts of Interest
We would like to thank the study therapists, participating hospital sites, and young adults and their families for involvement in the study. We would also like to thank the Ontario Mental Health Foundation for funding this study.
References
- Accurso EC, Ciao AC, Fitzsimmons-Craft EE, Lock JD, Le Grange D. Is weight gain really a catalyst for broader recovery? The impact of weight gain on psychological symptoms in the treatment of adolescent anorexia nervosa. Behaviour Research and Therapy. 2014;56:1–6. doi: 10.1016/j.brat.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agras WS, Lock J, Brandt H, Bryson SW, Dodge E, Halmi KA, Woodside B. Comparison of 2 family therapies for adolescent anorexia nervosa: A randomized parallel trial. JAMA Psychiatry. 2014;71(11):1279–1286. doi: 10.1001/jamapsychiatry.2014.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: A meta-analysis of 36 studies. Archives of General Psychiatry. 2011;68(7):724–731. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Clinical Growth Charts. 2009. Retrieved from http://www.cdc.gov/growthcharts/clinical_charts.htm.
- Chen EY, Weissman JA, Zeffiro TA, Yiu A, Eneva KT, Arlt JM, Swantek MJ. Family-based therapy for young adults with anorexia nervosa restores weight. International Journal of Eating Disorders. 2016;49(7):701–707. doi: 10.1002/eat.22513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couturier J, Kimber M, Szatmari P. Efficacy of family-based treatment for adolescents with eating disorders: A systematic review and meta-analysis. International Journal of Eating Disorders. 2012;46(1):3–11. doi: 10.1002/eat.22042. [DOI] [PubMed] [Google Scholar]
- Dalle Grave R, Calugi S, Doll HA, Fairburn CG. Enhanced cognitive behaviour therapy for adolescents with anorexia nervosa: An alternative to family therapy? Behaviour Research and Therapy. 2013;51(1):R9–R12. doi: 10.1016/j.brat.2012.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darcy AM, Bryson SW, Agras WS, Fitzpatrick KK, Le Grange D, Lock J. Do in-vivo behaviors predict early response in family-based treatment for anorexia nervosa? Behaviour Research and Therapy. 2013;51(11):762–766. doi: 10.1016/j.brat.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson SI, Cappelli M. We’ve got growing up to do: Transitioning youth from child and adolescent mental health services to adult mental health services. Ontario Centre of Excellence for Child and Youth Mental Health; 2011. [Google Scholar]
- DeJong H, Broadbent H, Schmidt U. A systematic review of dropout from treatment in outpatients with anorexia nervosa. International Journal of Eating Disorders. 2012;45(5):635–647. doi: 10.1002/eat.20956. [DOI] [PubMed] [Google Scholar]
- Dimitropoulos G, Freeman VE. The perceptions of individuals with anorexia nervosa regarding their family’s understanding of their illness, treatment, and recovery. Journal of Eating Disorders. 2016;24(4):1–8. doi: 10.1080/10640266.2015.1090870. [DOI] [PubMed] [Google Scholar]
- Dimitropoulos G, Freeman VE, Allemang B, Couturier J, McVey G, Lock J, Le Grange D. Family-based treatment with transition age youth with anorexia nervosa: A qualitative summary of application in clinical practice. Journal of Eating Disorders. 2015a;3(1):1–13. doi: 10.1186/s40337-015-0037-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimitropoulos G, Lock J, Le Grange D, Anderson K. Family therapy for adolescent eating and weight disorders: New applications. Routledge, NY: 2015b. Family therapy for transition youth; pp. 230–255. [Google Scholar]
- Doyle PM, Le Grange D, Loeb K, Doyle AC, Crosby RD. Early response to family-based treatment for adolescent anorexia nervosa. International Journal of Eating Disorders. 2010;43(7):659–662. doi: 10.1002/eat.20764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisler I, Dare C, Russell GF, Szmukler G, le Grange D, Dodge E. Family and individual therapy in anorexia nervosa: A 5-year follow-up. Archives of General Psychiatry. 1997;54(11):1025–1030. doi: 10.1001/archpsyc.1997.01830230063008. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire? International Journal of Eating Disorders. 1994;16(4):363–370. [PubMed] [Google Scholar]
- Fairburn CG, Harrison PJ. Eating disorders. The Lancet. 2003;361(9355):407–416. doi: 10.1016/S0140-6736(03)12378-1. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Cole TJ. Construction of LMS parameters for the Centers for Disease Control and Prevention 2000 growth charts. National Health Statistics Report. 2013;63:1–4. [PubMed] [Google Scholar]
- Garber AK, Mauldin K, Michihata N, Buckelew SM, Shafer MA, Moscicki AB. Higher calorie diets increase rate of weight gain and shorten hospital stay in hospitalized adolescents with anorexia nervosa. Journal of Adolescent Health. 2013;53(5):579–584. doi: 10.1016/j.jadohealth.2013.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber AK, Michihata N, Hetnal K, Shafer MA, Moscicki AB. A prospective examination of weight gain in hospitalized adolescents with anorexia nervosa on a recommended refeeding protocol. Journal of Adolescent Health. 2012;50(1):24–29. doi: 10.1016/j.jadohealth.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halmi KA, Agras WS, Crow S, Mitchell J, Wilson GT, Bryson SW, Kraemer HC. Predictors of treatment acceptance and completion in anorexia nervosa: implications for future study designs. Archives of general psychiatry. 2005;62(7):776–781. doi: 10.1001/archpsyc.62.7.776. [DOI] [PubMed] [Google Scholar]
- Hay PJ, Touyz S, Sud R. Treatment for severe and enduring anorexia nervosa: A review. Australian and New Zealand Journal of Psychiatry. 2012;46(12):1136–1144. doi: 10.1177/0004867412450469. [DOI] [PubMed] [Google Scholar]
- Le Grange D, Accurso EC, Lock J, Agras S, Bryson SW. Early weight gain predicts outcome in two treatments for adolescent anorexia nervosa. International Journal of Eating Disorders. 2014;47(2):124–129. doi: 10.1002/eat.22221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Grange D, Hughes E, Court A, Yeo M, Crosby R, Sawyer S. Randomized clinical trial of parent-focused treatment and family-based treatment for adolescent anorexia nervosa. Journal of the American Academy for Child and Adolescent Psychiatry. 2016;55(8):683–692. doi: 10.1016/j.jaac.2016.05.007. [DOI] [PubMed] [Google Scholar]
- Le Grange D, Lock J. Treating bulimia in adolescents: A family-based approach. Guilford Press; 2009. [Google Scholar]
- Le Grange D, Lock J, Agras WS, Moye A, Bryson SW, Jo B, Kraemer HC. Moderators and mediators of remission in family-based treatment and adolescent focused therapy for anorexia nervosa. Behaviour Research and Therapy. 2012;50(2):85–92. doi: 10.1016/j.brat.2011.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lock J, Agras WS, Fitzpatrick KK, Bryson SW, Jo B, Tchanturia K. Is outpatient cognitive remediation therapy feasible to use in randomized clinical trials for anorexia nervosa? International Journal of Eating Disorders. 2013;46(6):567–575. doi: 10.1002/eat.22134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lock J, Couturier J, Bryson S, Agras S. Predictors of dropout and remission in family therapy for adolescent anorexia nervosa in a randomized clinical trial. International Journal of Eating Disorders. 2006;39(8):639–647. doi: 10.1002/eat.20328. [DOI] [PubMed] [Google Scholar]
- Lock J, Le Grange D. Treatment manual for anorexia nervosa: A family-based approach. Second Edition. New York, NY: Guilford Publications; 2015. [Google Scholar]
- Lock J, Le Grange D, Agras WS, Moye A, Bryson SW, Jo B. Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa. Archives of General Psychiatry. 2010;67(10):1025–1032. doi: 10.1001/archgenpsychiatry.2010.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luce KH, Crowther JH. The reliability of the eating disorder examination – Self-report questionnaire version (EDE-Q) International Journal of Eating Disorders. 1999;25(3):349–351. doi: 10.1002/(sici)1098-108x(199904)25:3<349::aid-eat15>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Smink FR, Van Hoeken D, Hoek HW. Epidemiology of eating disorders: Incidence, prevalence and mortality rates. Current Psychiatry Reports. 2012;14(4):406–414. doi: 10.1007/s11920-012-0282-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein KF, Wing J, Lewis A, Raghunathan T. An eating disorder randomized clinical trial and attrition: Profiles and determinants of dropout. International Journal of Eating Disorders. 2011;44(4):356–368. doi: 10.1002/eat.20800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Touyz S, Le Grange D, Lacey H, Hay P, Smith R, Maguire S, … Crosby RD. Treating severe and enduring anorexia nervosa: A randomized controlled trial. Psychological Medicine. 2013;43(12):2501–2511. doi: 10.1017/S0033291713000949. [DOI] [PubMed] [Google Scholar]
- Treasure J, Russell G. The case for early intervention in anorexia nervosa: Theoretical exploration of maintaining factors. The British Journal of Psychiatry. 2011;199(1):5–7. doi: 10.1192/bjp.bp.110.087585. [DOI] [PubMed] [Google Scholar]
- Vo M, Lau J, Rubinstein M. Eating disorders in adolescent and young adult males: presenting characteristics. Journal of Adolescent Health. 2016;10(1):1–7. doi: 10.1016/j.jadohealth.2016.04.005. [DOI] [PubMed] [Google Scholar]
- Watson HJ, Bulik CM. Update on the treatment of anorexia nervosa: review of clinical trials, practice guidelines and emerging interventions. Psychological medicine. 2013;43(12):2477–2500. doi: 10.1017/S0033291712002620. [DOI] [PubMed] [Google Scholar]
- Westmoreland P, Krantz MJ, Mehler PS. Medical complications of anorexia nervosa and bulimia. The American Journal of Medicine. 2016;129(1):30–37. doi: 10.1016/j.amjmed.2015.06.031. [DOI] [PubMed] [Google Scholar]
- Zipfel S, Giel KE, Bulik CM, Hay P, Schmidt U. Anorexia nervosa: Aetiology, assessment, and treatment. The Lancet Psychiatry. 2015;2(12):1099–1111. doi: 10.1016/S2215-0366(15)00356-9. [DOI] [PubMed] [Google Scholar]
- Zipfel S, Wild B, Groß G, Friederich HC, Teufel M, Schellberg D, Burgmer M. Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in outpatients with anorexia nervosa (ANTOP study): Randomized controlled trial. The Lancet. 2014;383(9912):127–137. doi: 10.1016/S0140-6736(13)61746-8. [DOI] [PubMed] [Google Scholar]