Abstract
Accurate epidemiological surveillance of the burden of stroke is direly needed to facilitate the development and evaluation of effective interventions in Africa. The authors therefore conducted a systematic review of the methodology of stroke epidemiological studies conducted in Africa from 1970 to 2017 using gold standard criteria obtained from landmark epidemiological publications. Of 1330 articles extracted, only 50 articles were eligible for review grouped under incidence, prevalence, case‐fatality, health‐related quality of life, and disability‐adjusted life‐years studies. Because of various challenges, no study fulfilled the criteria for an excellent stroke incidence study. The relatively few stroke epidemiology studies in Africa have significant methodological flaws. Innovative approaches leveraging available information and communication technology infrastructure are recommended to facilitate rigorous epidemiological studies for accurate stroke surveillance in Africa.
Keywords: African, epidemiology, incidence, prevalence, stroke, surveillance
1. INTRODUCTION
Africa bears the greatest burden of hypertension,1 which is the strongest and most common modifiable risk factor for stroke.2, 3, 4 Consequently, strokes are an increasingly important health determinant especially in Africa, where these events were historically reported to be rare likely as a result of lack of resources to conduct proper community‐based studies to assess its burden.5 Despite the proposition that increased stroke occurrence is linked to gains in longevity on the continent, people of African descent clearly experience strokes at a younger age and have worse outcomes.6, 7 Furthermore, Africa appears to have the highest incidence, prevalence, and case fatality rates of stroke.8, 9, 10, 11, 12
However, making unambiguous statements about the trend of the burden of stroke and the impact of any interventions on this trend on the African continent is limited by the quality of epidemiological information from this population.
Stroke surveillance is useful in determining the present and projected burden of the disease and monitoring the impact of interventions.13 Rigorous stroke epidemiology is prerequisite for the efficient planning and delivery of stroke services, the effective application of current stroke prevention strategies, the development of new strategies, and our understanding of the mechanisms of stroke.14 The accuracy of a stroke epidemiological study is, however, contingent on multiple prerequisites, which include: obtaining an accurate diagnosis of stroke events based on standard definitions and methods in a clearly defined (enumerated) population or sample (also known as the reference population or the denominator).15 This will also allow comparison of estimates across regions and nations without methodological bias.16
Although there are no consensus guidelines, there have been numerous efforts to standardize epidemiological methods for various study designs.5, 16, 17 Conforming with these standard methods is required for rigorous and up‐to‐date epidemiological studies of stroke in Africa. Such studies will provide data and risk estimates that are critical resources for research programs such as Human Heredity and Health in Africa (H3Africa)17 and the Stroke Investigative Research and Education Network (SIREN) component.5
This systematic review was therefore conducted to assess the methodological rigor of existing stroke epidemiological studies conducted in Africa with respect to the recommended standards. We also provide a succinct description of a proposed stroke surveillance study, the ARISES (African Rigorous Innovative Stroke Epidemiological Surveillance) trial, which has been designed to address the identified methodological limitations in this field by incorporating innovative solutions based on emerging technologies.
2. METHODS
2.1. Search strategy and selection criteria
Using the Preferred Reporting Items for Systematic Review and Meta‐Analyses guidelines,18 data for this review were identified by searches of PubMed, Google Scholar, African Journals Online, and from the references of relevant articles from the years 1970 to 2017. The search terms were: “methodology,” “population‐based,” “community‐based,” “community,” “health facility–based,” “epidemiology,” “epidemiological,” “incidence,” “prevalence,” “Africa,” “survey,” “surveillance,” “fatality,” “case‐fatality,” “stroke,” “ischemic stroke,” “intracerebral,” “intraparenchymal,” “subarachnoid,” “hemorrhage,” “health‐related quality of life,” and “disability‐adjusted life‐years.” The data were collected and synthesized by the first two authors independently. Only publications in the English language were reviewed. These were later harmonized and emphasis was on articles with full publication for critical review of their methodologies. The criteria for selection included: (1) primarily an epidemiological study in Africa, and (2) full text available.
2.2. Data extraction, synthesis, and critical appraisal
A total of 1328 articles were retrieved from the aforementioned online databases. An additional two studies were identified through other sources by manual search. These articles were independently reviewed by two authors. After the removal of duplicates and articles that were not truly epidemiological studies, 112 articles were left. Of these, the 61 that were not full‐text articles and mostly from non–African countries were excluded. The only article not written in English was also excluded. Fifty articles were therefore retained for review (Figure 1). This review emphasized the methods of these studies and each article was critically appraised under the following headings: study period, recruitment process, case definition and ascertainment, confirmation by computed tomography (CT) or magnetic resonance imaging (MRI), classification as first‐ever or recurrent stroke, classification of ischemic stroke subtypes, and denominator population.16, 19 This approach methodically and practically answers all the questions needed for the critical appraisal of epidemiological studies.20
Figure 1.
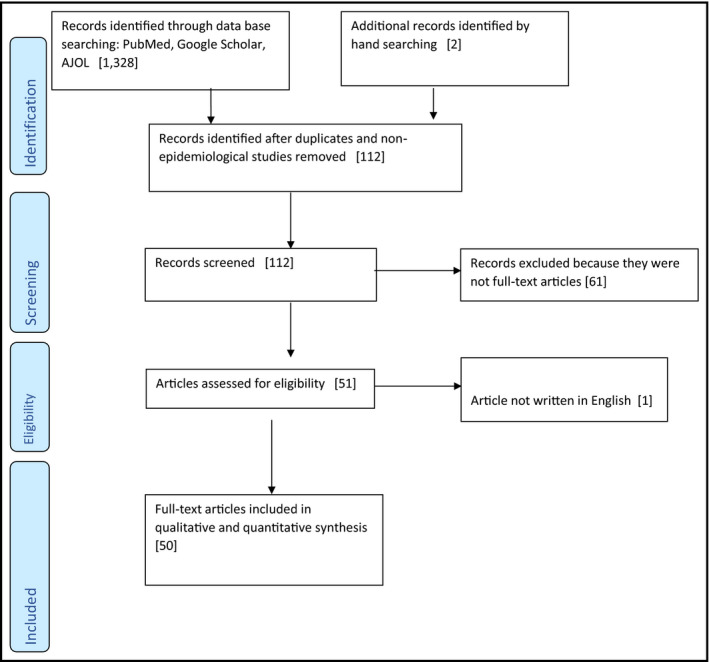
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses flow chart showing the search and selection process for the eligible publications on epidemiological studies of stroke in Africa. AJOL indicates African Journals Online.
2.3. Gold standard methods for assessing stroke epidemiology studies
The standards for stroke incidence studies are summarized in Table 1. In addition, there should be complete population‐based case ascertainment, based on multiple overlapping sources of information from hospitals, outpatient clinics, and death certificates.16, 21 Follow‐up of patients’ vital status for at least 1 month with a reliable method for estimating denominator (census data not more than 5 years old) are essential requirements.16, 21
Table 1.
Stroke incidence studies in Africa
| Country, Location, Setting | Author, y | Study period | Recruitment | Case definition | Confirmation by CT or MRI | Classification: first or recurrent | Classification of ischemic stroke | Denominator population |
|---|---|---|---|---|---|---|---|---|
| Gold standard/recommendations | Feigin,16 2004, Sudlow,21 1996, and Vandenbroucke,68 2013 | At least 3 y | Population or community based, prospective, hot pursuit | WHO definition/criteria | >80% | Yes | Yes | Large, well‐defined, and stable population |
| Eastern Africa | ||||||||
| Tanzania, rural | Walker,12 2011 | June 15, 2003, until June 15, 2006 | Community and health institution based | WHO definition | <80% | Yes | No | Yes |
| Tanzania, rural and urban | Walker,8 2010 | June 15, 2003, until June 15, 2006 | Community and health institution based | WHO definition | <80% | Yes | No | Yes |
| Northern Africa | ||||||||
| Egypt, Qena, mixed | Khedr,10 2014 | September 1, 2011, to August 31, 2013 | Door‐to‐door, community based | Not stated | >80% | Yes | No | Yes |
| Egypt, Al‐Kharga, mixed | Farghaly,39 2013 | June 1, 2005, to May 31, 2008 | Door‐to‐door survey, in three phases | WHO criteria | <80% | No | Yes | Yes |
| Egypt, Al Quseir, urban | El‐Tallawy,42 2013 | July 1, 2009, to January 31, 2012 | Door‐to‐door survey | WHO criteria | >80% | No | No | Yes |
| Libya, Benghazi, urban | Ashok,27 1986 | November 1, 1983, and October 31, 1984 | Health institution based | US National Survey of Stroke | >80% | No | Yes | Yes |
| Southern Africa | ||||||||
| South Africa, Atteridgeville, and Mamelodi suburban areas of Pretoria, urban | Rosman29 1986 | May 1, 1984, through April 30, 1985 | Health institution based | Harvard Cooperative Stroke Registry | <80% | No | Yes | Yes |
| South Africa, Agincourt subdistrict, rural | Maredza,71 2000 | 2007–2011 | Population based | Not stated | No | No | No | Yes |
| Mozambique | Damasceno,44 2011 | August 1, 2005, to July 31, 2006 | Health institution based | WHO definition | >80% | Yes | No | Yes (Maputo City population aged 25 years according to the 2007 Census) |
| Western Africa | ||||||||
| Nigeria, Ibadan, urban | Osuntokun,38 1979 | April 1, 1973, to March 30, 1975 | Health institution based | Not stated | No | Yes | Yes | Yes (projection of the 1963 Census) |
| Nigeria, Lagos, urban | Danesi,43 2013 | Between January 1 and December 31, 2007 | Health institution based | WHO definition | <80% | Yes | No | Yes |
| Nigeria, Akure, urban | Okon,72 2015 | Between November 1, 2010, and October 31, 2011 | Both healthcare and population based | Not stated | >80% | Yes | Yes | Yes |
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; WHO, World Health Organization.
See supporting information for references 42, 43, 44, 68, 71, and 72.
Suggested criteria for stroke prevalence studies are included in Table 2.19 Studies on health‐related quality of life also need accurate case ascertainment,22 including the use of World Health Organization (WHO) definitions for stroke. Additionally, stroke and stroke type should be confirmed by neuroimaging, while health‐related quality of life should be measured using a stroke‐specific health‐related quality of life questionnaire.23, 24 There may not be any specific standards for the study of stroke disability‐adjusted life‐years–its accurate determination is dependent on the quality of the prevalence and incidence studies from which it is calculated.25
Table 2.
Prevalence studies
| Country, Location, Setting | First author, y | Recruitment | Case definition | Clarification by CT or MRI | Denominator population |
|---|---|---|---|---|---|
| Gold standard/recommendation | Feigin,19 2003 and Vandenbroucke,68 2013 | Community door‐to‐door based | WHO definition/criteria | Yes (>80%) | Well‐defined and stable population |
| Eastern Africa | |||||
| Tanzania, rural | Walker,73 2000 | Community and health institution based | WHO definition | No | Yes |
| Northern Africa | |||||
| Egypt, Qena, mixed | Khedr,10 2014 | Door‐to‐door, community based | Not stated | >80% | Yes |
| Egypt, Al‐Kharga, mixed | Farghaly,39 2013 | Door‐to‐door survey, in three phases | WHO criteria | <80% | Yes |
| Egypt, Al Quseir, urban | El‐Tallawy,42 2013 | Door‐to‐door survey | WHO criteria | >80% | Yes |
| Egypt, Assiut, urban | Khedr,60 2013 | Three‐phase door‐to‐door community‐based study | WHO criteria | <80% | Yes |
| Morocco, Casablanca and Rabat, mixed | Engels,74 2014 | Two‐phase door‐to‐door community‐based survey | WHO criteria | Yes but percentage not stated | Yes |
| Western Africa | |||||
| Nigeria, Lagos, urban | Danesi,36 2007 | Community based | WHO definition | No | Yes |
| Nigeria, middle belt region semiurban | Sanya,37 2015 | Community based | WHO criteria | No | Yes |
| Nigeria, multicenter study in urban centers | Madu,75 2014 | Health institution based | Not stated | No | Yes |
| Nigeria, Zaria, urban | Danjuma,76 2005 | Health institution based | Not stated | No | No |
| Nigeria, Niger‐Delta/Ebubu and Usokun, rural | Ezejimofor,9 2017 | Door‐to‐door, community based | WHO criteria | No | Yes |
| Nigeria, Niger Delta/Kegbara‐Dere, rural | Onwuchekwa,77 2014 | Door‐to‐door, community based | WHO criteria | No | Yes |
| Benin, Cotonou, urban | Cossi,78 2012 | Door‐to‐door community‐based survey in three phases | WHO criteria | <80% | Yes |
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; WHO, World Health Organization.
See supporting information for references 68, 42, 60, 73–78.
3. RESULTS
The studies (n = 50) were regionally grouped into Eastern, Northern, Southern, and Western Africa. Nigeria, from Western Africa had 22 epidemiological studies followed by Egypt from Northern Africa with seven studies. There were 12 studies on incidence, 13 studies on prevalence, 13 studies on case fatality, and 10 studies on health‐related quality of life. The only two studies on disability‐adjusted life‐years were from South Africa (Tables 1, 2, 3 and S1, S2).
Table 3.
Case‐fatality studies
| Country, Location, Setting | First author, y | Study period | Recruitment | Case definition | Clarification by CT or MRI | Classification: first or recurrent | Classification of ischemic stroke |
|---|---|---|---|---|---|---|---|
| Gold standard/recommendation | Vandenbroucke,68 2013 and Lavados,79 2005 | At least 1 mo | Community based | WHO definition/criteria | >80% | Yes | Yes |
| Eastern Africa | |||||||
| Tanzania/rural | Walker,12 2011 | June 15, 2003, until June 15, 2006 | Community and health institution based | WHO definition | <80% | Yes | No |
| Southern Africa | |||||||
| South Africa, Atteridgeville, and Mamelodi suburban areas of Pretoria, urban | Rosman,29 1986 | May 1, 1984, through April 30, 1985 | Health institution based | Harvard Cooperative Stroke Registry | <80% | No | Yes |
| South Africa, Johannesburg, urban | Mudzi,80 2012 | Between 2006 and 2010 and followed up for 12 mo | Health institution based | Not stated | >80% | No | Yes |
| South Africa, Cape Town, urban | de Villiers,81 2011 | Between August 24, 2004, and January 12, 2006 | Health institution based | WHO definition | <80% | No | No |
| West Africa | |||||||
| Nigeria, Lagos, urban | Danesi,43 2013 | Between January 1 and December 31, 2007 | Health institution based | WHO definition | <80% | Yes | No |
| Gambia, Banjul, urban | Garbusinski,82 2005 | February 2000 to February 2001 | Health institution based | WHO criteria | No | No | No |
| Gambia, Banjul, rural/urban | Walker,83 2003 | 1 y beginning April 1, 1990 | Hospital based | WHO definition | No | No | No |
| Cameroon, Douala, urban | Mapoure,84 2014 | January 1, 2010, to December 31, 2012 | Hospital based | No | >80% | No | No |
| Nigeria, Jos, urban | Ekeh,85 2015 | January and December 2006 | Hospital based | WHO definition | <80% | No | No |
| Nigeria, Lagos, urban | Wahab,86 2008 | February 2003 to May 2004 | Hospital based | WHO definition | <80% | Yes | No |
| Nigeria, Abuja, urban | Alkali,87 2013 | January 2010 and June 30, 2012 | Hospital based | WHO definition | <80% | Yes | Yes |
| Nigeria, Akure, urban | Okon,72 2015 | Between November 1, 2010, and October 31, 2011 | Both community and health institution based | Not stated | >80% | Yes | Yes |
| Nigeria, Kano, urban | Femi,88 2013 | From June 2007 to June 2010 | Hospital based | WHO definition | Yes but percentage not stated | No | No |
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; WHO, World Health Organization.
See supporting information for references 43, 68, 72, 79, 80, 81, 82, 83, 84, 85, 86, 87, and 88.
Three incidence studies were determined at the health institution level, while only one was determined both at the health institution and community levels. Two of the prevalence studies from Nigeria were health institution based and the case definition for these studies was not stated. All but two studies conducted in the Niger Delta region of Nigeria were only in the urban settings. Thirty studies (60%) based their case definitions on the recommended WHO definition of stroke (Tables 1, 2, 3 and S1).
Only 16 studies (32%) classified stroke as first‐ever or recurrent. These were predominantly incidence studies (Tables 1, 3, and S1). Thirty‐four studies (68%) ascertained the diagnosis of stroke with CT or MRI, 11 (32.3%) of which had more than 80% of their patients diagnosed with CT or MRI. Only nine studies (18%) further classified ischemic stroke using neuroimaging (Tables 1, 2, 3 and S1). Three incidence studies were conducted in less than 3 years (Table 2). Three studies did not state the denominator population for calculating the indices. Two of them only gave the population census from which the denominators were derived.
Only six of the studies on health‐related quality of life in patients with stroke used a stroke‐specific quality‐of‐life instrument (Table S1). None of the studies were community based and only four used the WHO definition criteria to select their patients. No study classified ischemic stroke.
In summary, the only study that fulfilled the gold standard criteria for stroke epidemiological study was the prevalence study performed in urban Egypt (Al Qusei) by El‐Tallawy and colleagues.42 Other epidemiological studies on stroke incidence, case fatality, and health‐related quality of life were deficient in at least one criterion.
4. DISCUSSION
4.1. Case definition
The WHO definition of stroke26 with confirmation by CT/MRI scan is one of the suggested criteria for use in stroke epidemiological studies.19 In their study on the incidence study in Benghazi, Libya, Ashok and colleagues27 based their diagnosis and categorization of stroke type on an algorithm from the US National Survey of Stroke.28 However, stroke was confirmed by neuroimaging in over 80% of the clinically diagnosed cases. In addition, Rosman and colleagues29 adopted the criteria used in the Harvard Cooperative Stroke Registry30 in their study on the epidemiology of stroke in an urban black population in South Africa. This involved the combination of clinical and laboratory parameters for large artery thrombosis, lacunar infarct, intracerebral hemorrhage, and subarachnoid hemorrhage. Khedr and colleagues10 did not state the case definition in their study on the prevalence of ischemic and hemorrhagic strokes in Qena Governorate, Egypt.
4.2. Epidemiological study design and location
In the Libyan and South African studies, incidence rate was determined only at the level of health institutions. In epidemiological studies, this would result in underreporting, as many patients with stroke do not present to health institutions.31 Conversely, in Tanzania, the incidence rate was determined prospectively at both the community level and health facilities with “hot pursuit.”16 This has been found to be more accurate and reliable compared with retrospective studies.21
Typically, prevalence studies should be performed with a door‐to‐door survey in both the rural and urban communities.13 However, sometimes prevalence is estimated from cohort studies or by indirect calculation from incidence studies where cases have been followed up at regular intervals over time to determine fatality.32, 33 Most of the studies peformed in Nigeria were in the urban settings, which might not provide the full picture.
The only identified study on stroke mortality, conducted in Yaoundé, Cameroon,34 was not population based. The studies conducted on health‐related quality of life and disability‐adjusted life‐years were all hospital based and may not give an accurate indication of burden of stroke at the population level.
4.3. Confirmation by CT or MRI and further classification of ischemic stroke
A recommendation for an “ideal” high‐quality population‐based stroke epidemiological study is that at least 80% of the recruited cases should have brain CT/MRI peformed.16 This is for case ascertainment, pathologic classification, and phenotyping of ischemic and hemorrhagic strokes.35 The stroke incidence studies in rural Tanzania,12 Lagos, Nigeria,36 the middle belt region of Nigeria,37 and one incidence study from Ibadan, Nigeria,38 did not confirm cases of stroke by CT or MRI. During the time of conduct of the Ibadan stroke registry, CT technology was not available. This might be the reason these cases were not ascertained and not further classified. Even in Northern Africa, where neuroimaging was performed, only the incidence studies from Egypt, Al‐Kharga,39 and Libya, Benghazi,27 had further classification of ischemic stroke. Unlike the study by Owolabi,23 Akinpelu40 and Vincent‐Onabajo41 and colleagues did not confirm stroke with neuroimaging in their studies on health‐related quality of life.
4.4. Classification as first‐ever or recurrent stroke
For incidence studies, only the cases of first stroke should be reported and separated from recurrent strokes.16 Stroke incidence rate would be overestimated if patients with recurrent strokes within the period of surveillance are recruited. It was not clear why this essential criterion was not applied during the course of the four incidence studies.27, 29, 39 ,42 A potential explanation is the possibility of recall bias. Therefore, studies that would indirectly calculate disability‐adjusted life‐years from incidence rates without excluding recurrent stroke would give a wrong estimate of the disease burden.
4.5. Study period and denominator population
The conduct of a prevalence study should be in a population that is large, well‐defined, and stable.19 For incidence studies, data collection should be over a period of several years (continuously or periodically for at least 3 whole calendar years each period) in one and the same catchment area.16 However, three incidence studies, by Danesi,43 Damasceno,44 and Rosman29 and colleagues were conducted in less than 3 years. This would not be representative of the population being studied. The population census of the area of study is usually used because it has a complete enumeration of the population. The study must also be conducted within 5 years of the census.19 In this review, an incidence study in Ibadan, Nigeria,38 was conducted after 5 years of the last census, which rendered the population denominator invalid.
4.6. Challenges and solutions for rigorous stroke epidemiology in Africa
Common challenges in stroke epidemiological studies include finding stroke events across the myriad of settings where these events occur and where patients seek care, investigating events to determine that strokes meet defined criteria, valid investigations to rule out other causes of symptoms and establish stroke phenotype, accurate determination of poststroke morbidity and mortality, and accurate counts of the population to establish accurate census and epidemiological indices.
The problem of event reporting is especially important in Africa where knowledge of stroke is limited, significant portions of the populations have limited orthodox health access, and health data reporting is challenging.45,46 These challenges can be mitigated by establishing a mobile health‐driven stroke information system. Such a system can be deployed to improve local stroke literacy and lead to near‐total case detection. Following the required community engagements, establishing such an information system could begin with strengthening existing ward health structures and educating the local population about stroke to improve literacy about stroke and cardiovascular events. This information system should use educational materials that have been pretested and documented as culturally sensitive and effective in the communities. Examples include a prevalidated stroke documentary video,47–49 a stroke dance video,50 and a pictographic questionnaire for screening stroke in communities.51,52,45,51,53–56
Furthermore, an mHealth‐driven stroke alert system through which patients with stroke/caregivers/nonorthodox providers can report stroke, and a stroke finding system through which healthcare providers can remotely elicit notifications of stroke cases from all sources can be integrated. Previous research shows mobile phone access approaching 100% in various regions in Africa,17 ,49 which makes an mHealth system appropriate in this population. This option will therefore increase ease of reporting cases in surveillance studies.
4.7. Ethical and infrastructural challenges of conducting accurate stroke surveillance in Africa
Community‐based studies, which constitute the best way to determine the true incidence, prevalence, and mortality of stroke, are few and of uneven quality in Africa because of lack of manpower and research funds.57,61,63,68 Estimating the burden of stroke in the community is complicated by the difficulty in making a retrospective and yet accurate diagnosis of stroke and stroke type.57,63,64,68 Estimations are also biased by an underrepresentation of fatal cases.57,63,64,68 However, in Africa, incidence studies, which require considerable resources, are difficult to conduct and are rare.57,63,64,68 There is a relative scarcity of personnel and neuroimaging machines in most regions of Africa, particularly in rural communities. The long distances needed to travel to seek the standard diagnostic approach to stroke care could worsen the condition with associated risk of aspiration. Most patients who would have been candidates for thrombolysis would have missed the opportunity because of the delay in diagnosis. For ethical reasons and putting the patients’ survival first, in critical situations, diagnosis of stroke could be made in retrospect with pathological evidence at autopsy or neuroimaging at the nearest local facility when the patients are stable.
4.8. Significance of methodological deficiencies
The differences in epidemiologic indices may be attributable to disparities in methodological rigor. For instance:
Prevalence: There are several population‐/community‐based studies reporting crude prevalence rates of stroke survivors ranging from 15 per 100 000 in Ethiopia57–59 to 963 per 100 000 in Egypt10 ,60 and 1460 per 100 000 in the Niger Delta region, Nigeria.9 The wide disparity in these figures could reflect the uneven methodological rigor of the studies even after accounting for geographical and period effects. Therefore, prevalence, which depends on stroke incidence, duration, and mortality, is best estimated from studies that also track first‐ever stroke and survival.57,61
Incidence: Scant data from population‐based studies showed crude incidence rates that ranged from 25 per 100 000 person‐years in Lagos Nigeria,38 ,43,57,58 to 250 per 100 000 person‐years in Al‐Kharga, Egypt, in 2007.57,58,62 This wide disparity is likely caused by variability in methodological rigor and case ascertainment.57,58,63,64 The latter study was more rigorous, while the Lagos study was only for 1 year, with underpresentation of patients with stroke.
Mortality: Mortality data obtained in Africa are usually not from standard vital statistics registration, but are predominantly gathered from verbal autopsy studies, police reports, sibling histories, and burial and mortuary reports.65,66
Trends: Unfortunately, no rigorously conducted community‐based stroke epidemiologic study has been performed at least twice in the same location to provide direct data on the magnitude of change in stroke burden in Africa.
4.9. African Rigorous Innovative Stroke Surveillance
To model the deployment of the recommended solutions listed above, a North‐South collaborative stroke research team has designed an innovative stroke surveillance study: ARISES (African Rigorous Innovative Stroke Surveillance). ARISES aims to conduct a 3‐year surveillance of stroke cases in selected urban and rural sites in Nigeria, which have an existing demographic surveillance system. Clinical and laboratory assessments will utilize an existing network of neurologists, radiologists, and hospitals from earlier SIREN17 and Tailored Hospital‐based Risk reduction to Impede Vascular Events after Stroke (THRIVES)48 studies. ARISES also incorporates innovations such as the pictographic Questionnaire for Verifying Stroke‐Free Status for screening and verifying stroke or stroke‐free phenotype.45,51,53‐56 All study participants will be investigated using CT/MRI to confirm and classify stroke subtype according to a standard protocol, while imaging data from the study will be archived using AIM on Clear Canvas Enriched Stroke‐Phenotyping Software,67 a unique software package. The project will develop an innovative community‐based interactive Stroke Information and Surveillance System for reliable measurement and tracking of the population burden of stroke, as well as discovery and quantification of the factors influencing it, while simultaneously building sustainable capacity for improving stroke literacy, research, and control in Nigeria. ARISES will provide vital burden update information against which existing Global Burden of Disease stroke estimates can be validated. Finally, the study will provide long‐term benefit for stroke research and wider noncommunicable disease research in the target populations.
5. CONCLUSIONS
The identifiable deficiencies in the methodology of stroke epidemiological studies in Africa are inaccurate and incomplete case ascertainment and classification, poor representation of the population, and insufficient period of study, as well as incorrect denominator population. No epidemiologic study is ideal, but following the standard criteria with the aid of modern investigation modalities,68 reliable epidemiological indices for strategic primary, and secondary stroke prevention measures can be achieved. Innovative measures leveraging available information and communication technology infrastructure are recommended to facilitate rigorous epidemiological studies for accurate stroke surveillance in Africa and other low‐ and middle‐income countries. These novel resources will facilitate the implementation and evaluation of hypertension and stroke control interventions in Africa in synergy with the H3Africa program.69
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
Supporting information
DISCLOSURES
Mayowa Owolabi, Bruce Ovbiagele, Paul Olowoyo, Daniel Lackland, Carolyn Jenkins, Oyedunni Arulogun, Rufus Akinyemi, Onoja Akpa, Odunayo Akinyemi, Olanrewaju Olaniyan, Ezinne Uvere, Issa Kehinde, Mulugeta Gebregziabher, and Raelle Tagge are supported by U54 HG007479 and U01 NS079179 from the National Institutes of Health.
Owolabi M, Olowoyo P, Popoola F, et al. The epidemiology of stroke in Africa: A systematic review of existing methods and new approaches. J Clin Hypertens. 2018;20:47–55. 10.1111/jch.13152
Mayowa Owolabi and Paul Olowoyo contributed equally to this article.
REFERENCES
See supplementary material for references 40 to 98.
- 1. Global Health Observatory (GHO) data. Raised blood pressure. Situations and trends. www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence_text/en/. Accessed July 31, 2017.
- 2. Lackland DT, Roccella EJ, Deutsch AF, et al. Factors influencing the decline in stroke mortality. Stroke. 2014;45:315‐353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Campbell NR, Lackland DT, Lisheng L, et al. The World Hypertension League challenges hypertension and cardiovascular organizations to develop strategic plans for the prevention and control of hypertension. J Clin Hypertens (Greenwich). 2015;17:325‐327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lackland DT. Controlling hypertension to prevent target organ damage: perspectives from the World Hypertension League President. Ethn Dis. 2016;26:267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Owolabi MO, Arulogun O, Melikam S, et al. The burden of stroke in Africa: a glance at the present and a glimpse into the future: review article. Cardiovasc J Afr. 2015;26:27‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jones MR, Horner RD, Edwards LJ, et al. Racial variation in initial stroke severity. Stroke. 2000;31:563‐567. [DOI] [PubMed] [Google Scholar]
- 7. Owolabi M, Ugoya S, Platz T. Racial disparity in stroke risk factors: the Berlin‐Ibadan experience; a retrospective study. Acta Neurol Scand. 2009;119:81‐87. [DOI] [PubMed] [Google Scholar]
- 8. Walker R, Whiting D, Unwin N, et al. Stroke incidence in rural and urban Tanzania: a prospective, community‐based study. Lancet Neurol. 2010;9:786‐792. [DOI] [PubMed] [Google Scholar]
- 9. Ezejimofor MC, Uthman OA, Maduka O, et al. Stroke survivors in Nigeria: a door‐to‐door prevalence survey from the Niger Delta region. J Neurol Sci. 2017;372:262‐269. [DOI] [PubMed] [Google Scholar]
- 10. Khedr EM, Fawi G, Abdela M, et al. Prevalence of ischemic and hemorrhagic strokes in Qena Governorate, Egypt: community‐based study. J Stroke Cerebrovasc Dis. 2014;23:1843‐1848. [DOI] [PubMed] [Google Scholar]
- 11. Agyemang C, Attah‐Adjepong G, Owusu‐Dabo E, et al. Stroke in Ashanti region of Ghana. Ghana Med J. 2012;46:12‐17. [PMC free article] [PubMed] [Google Scholar]
- 12. Walker RW, Jusabani A, Aris E, et al. Post‐stroke case fatality within an incident population in rural Tanzania. J Neurol Neurosurg Psychiatry. 2011;82:1001‐1005. [DOI] [PubMed] [Google Scholar]
- 13. Truelsen T, Bonita R, Jamrozik K. Surveillance of stroke: a global perspective. Int J Epidemiol. 2001;30:S11. [DOI] [PubMed] [Google Scholar]
- 14. Rothwell PM. Incidence, risk factors and prognosis of stroke and TIA: the need for high‐quality, large‐scale epidemiological studies and meta‐analyses. Cerebrovasc Dis. 2003;16:2‐10. [DOI] [PubMed] [Google Scholar]
- 15. Thrift AG. Design and methods of population surveys. Neuroepidemiology. 2010;34:267‐269. [DOI] [PubMed] [Google Scholar]
- 16. Feigin V, Vander Hoorn S. How to study stroke incidence. Lancet. 2004;363:1920‐1921. [DOI] [PubMed] [Google Scholar]
- 17. Akpalu A, Sarfo FS, Ovbiagele B, et al. Phenotyping stroke in sub‐Saharan Africa: stroke investigative research and education network (SIREN) phenomics protocol. Neuroepidemiology. 2015;45:73‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population‐based studies of incidence, prevalence, and case‐fatality in the late 20th century. Lancet Neurol. 2003;2:43‐53. [DOI] [PubMed] [Google Scholar]
- 20. Critical Appraisal Tools. joannabriggs.org/research/critical‐appraisal‐tools.html. Accessed September 24, 2017.
- 21. Sudlow C, Warlow C. Comparing stroke incidence worldwide. Stroke. 1996;27:550‐558. [DOI] [PubMed] [Google Scholar]
- 22. Aaronson NK. Quality of life assessment in clinical trials: methodologic issues. Control Clin Trials. 1989;10:195‐208. [DOI] [PubMed] [Google Scholar]
- 23. Owolabi MO. Determinants of health‐related quality of life in Nigerian stroke survivors. Trans R Soc Trop Med Hyg. 2008;102:1219‐1225. [DOI] [PubMed] [Google Scholar]
- 24. Williams LS, Weinberger M, Harris LE, Biller J. Measuring quality of life in a way that is meaningful to stroke patients. Neurology. 1999;53:1839. [DOI] [PubMed] [Google Scholar]
- 25. Wagner RG, Ibinda F, Tollman S, Lindholm L, Newton CR, Bertram MY. Differing methods and definitions influence DALY estimates: using population‐based data to calculate the burden of convulsive epilepsy in rural South Africa. PLoS ONE. 2015;10:e0145300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hatano S. Experience from a multicentre stroke register: a preliminary report. Bull World Health Organ. 1976;54:541. [PMC free article] [PubMed] [Google Scholar]
- 27. Ashok P, Radhakrishnan K, Sridharan R, El‐Mangoush M. Incidence and pattern of cerebrovascular diseases in Benghazi, Libya. J Neurol Neurosurg Psychiatry. 1986;49:519‐523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Walker A, Robins M, Weinfeld F. The National Survey of Stroke. Clinical findings. Stroke. 1981;12:I13. [PubMed] [Google Scholar]
- 29. Rosman KD. The epidemiology of stroke in an urban black population. Stroke. 1986;17:667‐669. [DOI] [PubMed] [Google Scholar]
- 30. Mohr J, Caplan LR, Melski JW, et al. The Harvard Cooperative Stroke Registry a prospective registry. Neurology. 1978;28:754. [DOI] [PubMed] [Google Scholar]
- 31. Asplund K, Bonita R, Kuulasmaa K, et al. Multinational comparisons of stroke epidemiology. Stroke. 1995;26:355‐360. [DOI] [PubMed] [Google Scholar]
- 32. Bonita R, Solomon N, Broad JB. Prevalence of stroke and stroke‐related disability. Stroke. 1997;28:1898‐1902. [DOI] [PubMed] [Google Scholar]
- 33. Whisnant JP. Stroke: Populations, Cohorts, and Clinical Trials. Oxford, UK: Butterworth‐Heinemann Medical; 1993. [Google Scholar]
- 34. Nkoke C, Lekoubou A, Balti E, Kengne AP. Stroke mortality and its determinants in a resource‐limited setting: A prospective cohort study in Yaounde, Cameroon. J Neurol Sci. 2015;358:113‐117. [DOI] [PubMed] [Google Scholar]
- 35. Malmgren R, Bamford J, Warlow C, Sandercock P. Geographical and secular trends in stroke incidence. Lancet. 1987;330:1196‐1200. [DOI] [PubMed] [Google Scholar]
- 36. Danesi M, Okubadejo N, Ojini F. Prevalence of stroke in an urban, mixed‐income community in Lagos, Nigeria. Neuroepidemiology. 2007;28:216‐223. [DOI] [PubMed] [Google Scholar]
- 37. Sanya EO, Desalu OO, Adepoju F, Aderibigbe SA, Shittu A, Olaosebikan O. Prevalence of stroke in three semi‐urban communities in middle‐belt region of Nigeria: a door to door survey. Pan Afr Med J. 2015;20:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Osuntokun B, Bademosi O, Akinkugbe O, Oyediran A, Carlisle R. Incidence of stroke in an African City: results from the Stroke Registry at Ibadan, Nigeria, 1973‐1975. Stroke. 1979;10:205‐207. [DOI] [PubMed] [Google Scholar]
- 39. Farghaly WM, El‐Tallawy HN, Shehata GA, et al. Epidemiology of nonfatal stroke and transient ischemic attack in Al‐Kharga District, New Valley, Egypt. Neuropsychiatr Dis Treat. 2013;9:1785‐1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


