Abstract
Purpose
To compare the visual performance of prototype contact lenses designed via deliberate manipulation of higher-order spherical aberrations to extend-depth-of-focus with two commercial multifocals, after 1 week of lens wear.
Methods
In a prospective, participant-masked, cross-over, randomized, 1-week dispensing clinical-trial, 43 presbyopes [age: 42–63 years] each wore AIROPTIX Aqua multifocal (AOMF), ACUVUE OASYS for presbyopia (AOP) and extended-depth-of-focus prototypes (EDOF) appropriate to their add requirements. Measurements comprised high-contrast-visual-acuity (HCVA) at 6 m, 70 cm, 50 cm and 40 cm; low-contrast-visual-acuity (LCVA) and contrast-sensitivity (CS) at 6 m and stereopsis at 40 cm. A self-administered questionnaire on a numeric-rating-scale (1–10) assessed subjective visual performance comprising clarity-of-vision and lack-of-ghosting at various distances during day/night-viewing conditions and overall-vision-satisfaction.
Results
EDOF was significantly better than AOMF and AOP for HCVA averaged across distances (p ≤ 0.038); significantly worse than AOMF for LCVA (p = 0.021) and significantly worse than AOMF for CS in medium and high add-groups (p = 0.006). None of these differences were clinically significant (≤2 letters). EDOF was significantly better than AOMF and AOP for mean stereoacuity (36 and 13 seconds-of-arc, respectively: p ≤ 0.05). For clarity-of-vision, EDOF was significantly better than AOP at all distances and AOMF at intermediate and near (p ≤ 0.028). For lack-of-ghosting averaged across distances, EDOF was significantly better than AOP (p < 0.001) but not AOMF (p = 0.186). EDOF was significantly better than AOMF and AOP for overall-vision-satisfaction (p ≤ 0.024).
Conclusions
EDOF provides better intermediate and near vision performance than either AOMF or AOP with no difference for distance vision after 1 week of lens wear.
Keywords: Presbyopia, Multifocal contact lenses, Higher order aberrations, Extended depth of focus contact lenses, Visual performance
Resumen
Objetivo
Comparar el rendimiento visual de un prototipo de lentes de contacto diseñadas mediante manipulación deliberada de aberraciones esféricas de alto orden, para ampliar la profundidad de campo con dos lentes multifocales comerciales, tras una semana de uso.
Métodos
En un ensayo clínico prospectivo, ciego para los participantes, transversal, aleatorizado, con uso de lentes durante una semana, 43 présbitas [Edad: 42–63 años] utilizaron lentes AIROPTIX Aqua multifocal (AOMF), ACUVUE OASYS para presbicia (AOP) y de profundidad de foco extendido (EDOF) adecuados a sus requisitos de adición. Las mediciones incluyeron agudeza visual de alto contraste (HCVA) a 6 m, 70 cm, 50 cm y 40 cm, agudeza visual de bajo contraste (LCVA), sensibilidad de contraste (CS) a 6 m, y estereopsis a 40 cm. Un cuestionario auto-administrado sobre una escala de evaluación numérica (1–10) valoró el rendimiento visual subjetivo incluyendo la nitidez de visión y la ausencia de imágenes fantasma a diversas distancias en condiciones de visión diurna/nocturna, así como la satisfacción sobre la visión general.
Resultados
EDOF fue considerablemente mejor que AOMF y AOP para la media de las distancias HCVA (p ≤ 0,038); considerablemente peor que AOMF para LCVA (p = 0,021) y considerablemente peor que AOMF para CS en los grupos de adición media y elevada (p = 0,006). Ninguna de estas diferencias fueron clínicamente significativas (≤ 2 letras). EDOF fue considerablemente mejor que AOMF y AOP para la estereoagudeza media (36 y 13 segundos de arco, respectivamente: p ≤ 0,05). Para la claridad de visión, EDOF fue considerablemente mejor que AOP en todas las distancias, y AOMF para las distancias intermedia y cercana (p ≤ 0,028). Para la falta de imágenes fantasma promediada a las diferentes distancias, EDOF fue considerablemente mejor que AOP (p < 0,001) pero no así AOMF (p = 0,186). EDOF fue considerablemente mejor que AOMF y AOP en cuanto a satisfacción sobre la visión general (p ≤ 0,024).
Conclusiones
EDOF aporta un mejor desempeño de visión intermedia y cercana que AOMF o AOP, sin diferencia de visión lejana tras una semana de uso de lentes de contacto multifocales.
Palabras clave: Presbicia, Lentes de contacto multifocales, Aberraciones de alto orden, Lentes de contacto de profundidad de campo ampliada, Desempeño visual
Introduction
Presbyopia is an age-dependent progressive reduction of the accommodative amplitude that results in an inability to focus accurately on near objects. Based on population projections, the global presbyopia prevalence is estimated to reach about 1.4 billion people by 2020.1 In developed countries alone, there are about 600 million people over the age of 45 who need some degree of vision correction for near. Although traditional spectacle lenses remain the most common correction method for presbyopes, recent prescribing trends2, 3 have shown that over the last decade multifocal contact lenses are gaining popularity.4 An increasingly more active lifestyle of presbyopes,5 demanding a more comfortable, less distracting correction method, could possibly be one of the reasons for this trend in the more developed countries.
When compared to single vision lenses, visual performance with multifocal contact lenses is often compromised.6, 7 Simultaneous optical correction designed to correct appropriate viewing distances (i.e. far, intermediate and near) over a limited pupillary area leads to degradation in the visual performance. This imaging principle is often associated with an undesirable presence of ghosting,8 in addition to reduction in low-contrast visual acuity7, 9, 10 and contrast sensitivity.6 Depending on lens design (i.e. aspheric centre-near, centre-distance multifocal or concentric bifocal),7 near add power, pupil size,11 inherent spherical aberrations11, 12 and lens centration,7 the extent of visual performance reduction can range from mild to severe and can occur at one or more distances. In light of the visual compromises associated with current multifocal contact lens designs, a globally increasing presbyopic population and a greater demand in contact lens alternatives, the need to design and develop more satisfying presbyopic solutions is imminent.
Via utilization of adaptive optics technology13, 14, 15, 16, 17 and Fourier optics simulations,12 it was demonstrated that interactions of several orders of higher-order spherical aberration terms with Zernike defocus can provide an extension in depth of focus of the corrected eye. Expanding on this concept,18 extended depth-of-focus prototype contact lenses for presbyopic refractive correction (EDOF) have been designed at the Brien Holden Vision Pty Ltd, Sydney, Australia and contract manufactured in poly-HEMA-based (58% water) material. In Part 1 of the study, we explored the performance of the proposed designs using through focus measures; we reported that lenses designed with deliberately manipulated higher order spherical aberration seem to be less susceptible to variations in pupil, inherent ocular aberrations and lens decentration; when compared to commercial alternatives. In this part of the paper, we focus on evaluating if and how these observed incremental improvements seen in ray-tracing experiments translate to clinical outcomes.
Previously, we assessed the visual performance of prototype lenses against two commercial lenses in presbyopes after 1 h of lens wear, and found prototype lenses offered good vision at intermediate and near, without compromising distance vision.19, 20 Although, such initial on-eye results of prototype lenses are encouraging and supportive towards the theory of extension in the depth of focus achieved through manipulation of higher order spherical aberration, several authors have shown that the subjective visual performance of multifocal contact lenses differs from initial fitting and after several days of wear.21, 22, 23 The aim of the current study was therefore to assess the acuities, contrast sensitivity, stereopsis and subjective visual performance of the test and control lenses after one week of wear and to compare clinical findings with theoretical measures obtained through ray-tracing.
Methods
Lens designs
The power profiles of the prototype and controls lenses are shown in Fig. 1 of accompanying paper (Part I of the present study). As can be seen, the profile of the AIR OPTIX® Aqua multifocal (AOMF: lotrafilcon b, Alcon laboratories, TX USA) is designed with monotonic distribution of power decreasing from near zone to distance correction. On the other hand, the ACUVUE® OASYS® for presbyopia (AOP: senofilcon A: Johnson & Johnson Vision Care, FL, USA) is a concentric-ring, aspheric, zonal bifocal, where the distinct zones for distance and near correction are separated equally over the optic zone diameter. In contrast with commercial lenses, the prototype EDOF have a series of smooth, non-monotonic, aperiodic, power variation across the optic zone diameter that were designed using deliberate manipulation of multiple higher-order spherical aberration terms. Here, the objective was to achieve an extension in depth of focus that would facilitate a balanced visual performance across a range of predefined dioptric distances. The profiles are designed to satisfy presbyopes with low, medium and high-add requirements.
Participants
This was a prospective, participant-masked cross-over, randomized, 1-week dispensing clinical trial conducted at the Clinical Research Trials Centre of the Brien Holden Vision Institute in Sydney, Australia, commencing in September 2014 and concluding in May 2015. A Human Research Ethics Committee (Bellberry, Adelaide, South Australia) approved the clinical trial. Written informed consent from every participant was obtained prior to commencing any study procedures. The clinical trial conformed to the principles of the Declaration of Helsinki and was registered on the Australian New Zealand Clinical Trials Registry (ACTRN12614000011684) and United States clinical trials registry (NCT02214797). The inclusion criteria for the study were: distance high-contrast visual acuity (HCVA) vision correctable to at least 6/12 in each eye with spherical contact lenses; astigmatism ≤1.00 DC; having a spherical equivalent refraction between −6.00 D and +3.00 D; requiring at least +0.50 D near addition over full distance subjective Rx and having no ocular conditions which would preclude safe contact lens wear. The enrolled participants were a mix of both experienced and non-contact lens wearers. The latter went through a 1-week period of lens adaptation with commercial single vision contact lenses for lens handling (i.e. insertion/removal) training. As they were presbyopes, an appropriate pair of ready-made readers were also given for their near vision needs, only to be used during the adaptation period.
Baseline procedures
All participants attended a baseline visit for subjective distance refraction measurement of near add power and determination of eye dominance. All clinical tests were performed under photopic conditions (∼400 lux). Subjective distance refraction was performed using standard optometric techniques. The near addition was the minimum plus power over full subjective distance Rx needed to read 0.0 logMAR print on a high-contrast, black on white Logarithmic Visual Acuity Chart – ETDRS 2000 Series Chart “1′ (Precision Vision, IL, USA) at 40 cm while wearing a trial frame with full aperture lenses. Participants were stratified as low, medium and high presbyopes based on the near add with low = +0.50 to +1.25 D add, medium = +1.50 to +1.75 D add and high = ≥+2.00 D add. Sensory dominance method was used for determining the dominant eye, as explained in detail elsewhere.19, 24 If the sensory dominance technique was unsuccessful then sighting dominance was used to identify the dominant eye, as described elsewhere.19, 24
Enrolment, contact lens parameters and fitting
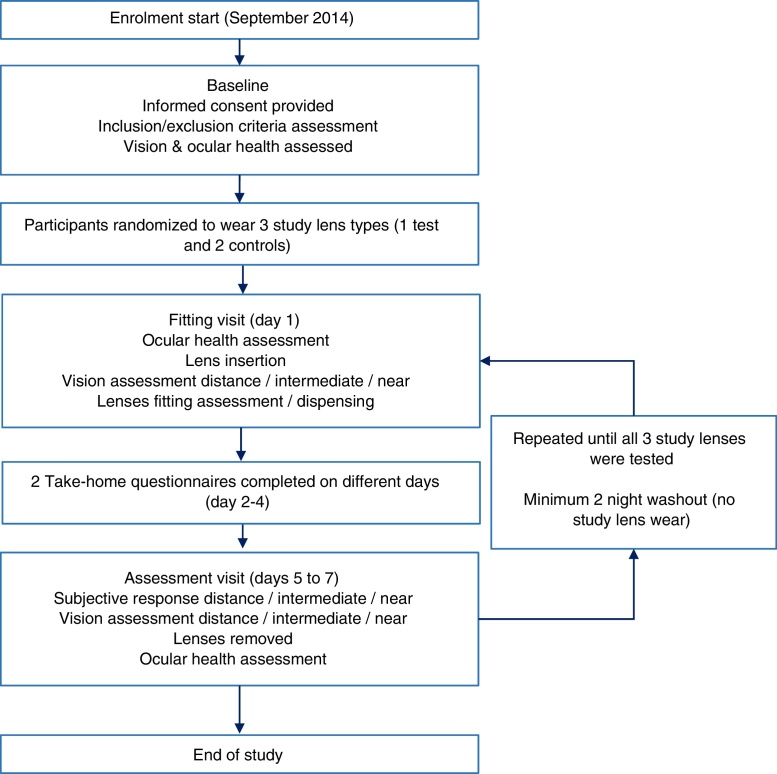
Upon completion of the baseline visit, the participants were considered successfully enrolled and were allocated to three contact lens types (one test and two controls) based on a cross-over, balanced block, randomization scheme generated through http://randomization.com/. The randomization scheme determined the order in which lens types were worn by each participant. Lens identity was masked from participants, who wore all three lens types for approximately one week (minimum period of 5 days) each. A minimum two-night wash-out period with habitual correction between lens types was imposed. For more details, please see participant flow diagram in Fig. 1.
Figure 1.
Participant flow diagram for the clinical trial.
The EDOF prototypes constituted the test lenses. Three different designs, targeting participants with low, medium and high reading additions were used. The base curve and diameters of EDOF were 8.4 mm and 14 mm, respectively. AOMF and AOP constituted the control lenses. The base curves and diameters of AOMF and AOP 8.6 and 8.4 mm, and 14.2 and 14.3 mm, respectively. Both test and control lenses were available from −6.00 D to +3.50 D in 0.25 D steps. With the prototype lenses, presbyopes needing low and medium addition power wore low and medium add designs bilaterally, while those needing high reading addition wore medium-high combination, with the medium-add design in the non-dominant eye. For control lenses, the designs were dispensed based on the manufacturer's package insert and fitting guides.25, 26
Metrology evaluation of prototype lenses
Lens metrology was performed on prototype EDOF lenses to verify that they conformed to the specifications. A quality control protocol was deployed which directed to assess five randomly chosen lenses in each available power for all prototype contact lenses. A custom-written software algorithm was deployed to post-process standard export raw outputs from NIMO TR1504 (Lambda-X, Belgium). A dedicated algorithm compared measured values with the nominal profile to determine conformity to design specifications. The criteria used for quality control was the sum of absolute differences between the measured and nominal profile across the half-chord diameter. The sum of absolute differences value divided by total number of points on the half-chord yielded an average sum of absolute differences for each profile. In addition to power, the same sample were subjected to checks on the sagittal height measurements with a Microscope MM-400 (Nikon, Japan); diameter with a Profile Projector V-12 (Nikon, Japan) and centre-thickness using a soft contact lens thickness gauge ET-3 (Rehder Development Co., CA, USA). The base curve for each lens was then calculated using these measurements.
Contact lenses dispensed
The initial lens power used for test and control contact lenses was based on each participant's spherical equivalent subjective distance refraction. Lenses were allowed to settle for about 10 min followed by over-refraction using a trial frame. Maximum plus to achieve best distance monocular high contrast visual acuity was used. The end point of distance refraction was at least 6/7.5 + 1 (0.08 LogMAR) binocular high contrast visual acuity and the inter-ocular high contrast acuity difference was kept to within 4 letters (0.08 logMAR) to avoid monovision or modified monovision effects. The final lens power was chosen based on the best visual outcome for each participant at both distance and near and within the above constraints. A Test Chart 2000 Pro (Thomson Software Solutions, Hertfordshire, UK) was used for all distance based measurements and high-contrast black on white near LogMAR charts (Precision Vision, USA) were used for all intermediate and near measurements. The control lenses were silicone hydrogels and were dispensed as per manufacturer's guidelines with a lens care system (ClearCare®, Alcon Laboratories, TX, USA), while the test lenses (hydrogels) were prescribed as daily disposables. EDOF, AOMF and AOP contact lenses have distinctly different tints, which made it impractical to mask the investigators.
Acuity, contrast sensitivity and stereopsis measurements
Distance high-contrast visual acuity at 6 m was taken monocularly and binocularly. All other acuity measurements were taken binocularly. Low-contrast visual acuity and contrast sensitivity were measured at 6 m. The HCVA and low-contrast visual acuity (LCVA) charts were set at 100% and 10% contrast levels, respectively and distance contrast sensitivity was measured at 6, 12 and 18 cycles/degree with randomized letter triplets whose contrast is varied logarithmically from top to bottom of the chart (Thomson Software Solutions, Hertfordshire, UK). HCVA was measured for intermediate (70 cm) and near (50 cm and 40 cm). The near LogMAR chart is designed for 40 cm, so HCVA measurements at 70 cm and 50 cm were converted to equivalent values in logMAR for these distances prior to statistical analyses (please see appendix). All acuity measurements were resolution acuity, i.e. participants were instructed to read the smallest line possible. Stereopsis was measured at 40 cm with the Stereo Fly Test Circles (Stereo Optical, IL, USA). The investigator entered all the acuity measurements directly into a central database. All acuity measurements performed at the assessment visit were included in the analysis.
Subjective questionnaire
The subjective questionnaire-instrument used was aimed to encompass a broad range of visual tasks/demands needed on a daily basis. The questionnaire-instrument was administered three times, two take-home (to be filled in different days between the dispensing and assessment visits) and the third one at the assessment visit. The average of responses for the three questionnaires was used for the analysis. All the subjective ratings were based on a numerical rating scale scored on 1–10 interval, in 1-unit steps. Similar questionnaires were used in our previous short-term assessments of contact lenses.19, 20 Unlike these short-term studies, the current study required participants to experience contact lenses under ‘real-world’ conditions, and so vision performance was separated under day and night-time conditions and additional questions were asked for vision when driving and night-time halos. Briefly, the questions comprised clarity of vision (1 = blurred, 10 = clear) and ghosting (1 = none, 10 = severe) for distance, intermediate and near and vision when driving (1 = blurred, 10 = clear) specifically under day and night-time conditions. Participants also rated vision stability (1 = very unstable, 10 = very stable), night-time haloes (1 = not bothersome, 10 = extremely bothersome), overall comfort (1 = uncomfortable and 10 = comfortable) and overall vision satisfaction (1 = not satisfied and 10 = satisfied). Participants recorded average daily contact lens wear-time and number of hours with acceptable vision via recall at each assessment visit.
Lens fit assessment
Lens fit assessment was performed at dispensing and assessment visits. After vision and subjective ratings were complete, lenses were observed on eye with slit-lamp biomicroscopy and assessed for centration (horizontal and vertical, mm), primary lens movement (mm), primary lens lag (mm) and tightness (%).
Data transformations
To simplify interpretation, the scale for ghosting rating and the scale for night-time haloes have been reversed to be consistent with the other ratings, such that a higher rating refers to a better result (i.e. less ghosting and less bothersome haloes). Here and throughout the document, the ghosting variable will be referred to as ‘lack of ghosting’ and the halo variable will be referred to as ‘lack of bothersome haloes’. As the stereopsis data was positively-skewed, a log transform to the raw data was performed prior to statistical analyses. All the data are summarized as observed means ± SD for variables measured on an interval scale and as percentages for all categorical variables.
Statistical analysis
A minimum sample of 27 participants was needed to demonstrate a statistically significant paired difference of 1 ± 1.8 units between lenses types for subjective variables (primary outcome) with 80% power and 5% level of significance. This sample also had 90% power to detect 0.10 ± 0.15 logMAR difference in visual acuity (secondary outcome) between the lens types. All the analyses were performed using SPSS 21 (IBM, USA), and the level of significance was set at 5%. Results of sub groups are presented only if interactions were significant at 5% level. Bonferroni adjustments were made for post hoc analyses.
A 3-way linear mixed model with subject random intercepts and repeated effects of lens types was deployed to test the hypothesis if the test lenses performed differently to the two controls. For the subjective variables (clarity of vision and lack of ghosting), the model included the following study design factors: lens-type (EDOF, AOMF or AOP), test-distance (far, intermediate and near), time-of-day (day/night). For vision-stability and driving-vision variables, the linear mixed model only had lens-type and time-of-day and their interaction as study design factors. For overall vision satisfaction and ocular comfort variables, lens-type was the only study design factor in the model. The add group (low/medium/high) was added as a confounding subject factor in all models. The interaction of lens type with all other factors were tested. The significance of lens type was assessed within a sub level of a factor only if the respective interaction term was significant. In all other instances the results are generalized for the whole group. This modelling approach was used instead of several repeated measures/paired t-tests to avoid inflating the type I error rate. Due to the unequal distribution of add-groups (Table 1), results for subjective variables are presented as ‘observed means’ (actual mean results obtained) and ‘estimated means’ (mean results calculated assuming an equal distribution between add-groups).
Table 1.
Demographic factors for low, medium and high-add participants. Myopes were defined as participants requiring a negative spherical-equivalent distance subjective refraction and all other participants were defined as hyperopes.
| Factor | Total | Low-add | Med-add | High-add |
|---|---|---|---|---|
| n = 43 | n = 13 | n = 18 | n = 12 | |
| Age (years) | 53 ± 5a | 48 ± 4a | 54 ± 5a | 56 ± 4a |
| Age range (years) | 42–63 | 42–57 | 48–63 | 49–63 |
| Female:male (%) | 53:47 | 62:38 | 44:56 | 58:42 |
| Neophytes:experienced contact lens wearers (%) | 30:70 | 15:85 | 44:56 | 25:75 |
| Ethnicity (%) | ||||
| Caucasian:Asian:Others | 74:12:14 | 85:8:8 | 67:17:17 | 75:8:17 |
| Myopesb | ||||
| Spherical equivalent (D) | −2.92 ± 1.50a | −2.94 ± 1.27a | −2.81 ± 1.96a | −3.00 ± 1.34a |
| Range (D) | −6.00 to −0.75 | −5.25 to −0.75 | −6.00 to −0.7 | −6.00 to −1.25 |
| Hyperopesb | ||||
| Spherical equivalent (D) | 1.62 ± 0.84a | 1.31 ± 0.83a | 1.56 ± 0.90a | 1.85 ± 0.73a |
| Range (D) | 0.25–3.25 | 0.50–2.25 | 0.25–3.25 | 0.75–2.75 |
| Keratometryb | ||||
| Flat power (D) | 43.27 ± 1.38a | 43.06 ± 1.53a | 43.35 ± 1.50a | 43.39 ± 1.02a |
| Steep power (D) | 43.84 ± 1.45a | 43.64 ± 1.57a | 43.94 ± 1.59a | 43.91 ± 1.12a |
Data expressed as mean ± SD.
Results presented for both eyes combined.
For HCVA, lens-type, test-distance and their interactions were considered as study design factors. For distance, LCVA (both in high and low illumination conditions) and stereopsis measure, only the lens-type was considered as study design factors. For the distance contrast sensitivity variable, the lens-type, spatial-frequency (cyc/deg) were considered as study design factors. If the interactions of lens-type with test-distances and or spatial frequency were found to be significant, further post hoc tests were deployed to determine significance of lens type within sub levels of the interacting factor. Again, the add-group (low/medium/high) was added as a confounding subject factor in all models. The difference between the dispensed study lens power and vertex-corrected spherical equivalent refraction at baseline was also compared using the linear mixed model to see if they were different between test and control lenses.
Results
Lens metrology
Five randomly picked samples from each power of the three prototype designs (Range: −6.00 D to +3.00 in 0.25 D steps, a total of 540 lenses) were requested for metrology evaluation. For power-profile measurements, the average range of sum of absolute differences measure for all lenses was 0.05–0.16 D, which is clinically insignificant. For sagittal height, diameter, centre thickness and base curve variables, all lenses were within tolerance specifications (ISO 18369 Section 2).27
Demographics
A total of 43 participants completed the study (13 low-add participants, 18 medium-add participants and 12 high-add participants), of whom 53% were female, the mean ± SD age was 53 ± 5 years, the age range was 42–63 years, and 70% were experienced contact lens wearers. Participant details for each add-group are presented in Table 1.
Data transformations
For all acuity, contrast sensitivity and stereopsis measures, data from the assessment visit was used in the final analysis. However, with the subjective measures, data from the assessment visit and take-home questionnaires were averaged, as they were no different from each other (p > 0.05).
Acuities, contrast sensitivity and near stereopsis
The observed mean (±SD) of visual acuities at various distances, contrast and/or illumination levels, distance contrast sensitivity and near stereopsis for the three study lenses are presented in Table 2. For high-illumination HCVA, there were significant differences between lens-type (p < 0.001), test-distance (p < 0.001) and add-group (p = 0.006). As expected, the acuities were better for distance followed by intermediate and near; and the low adds achieved better acuity followed by medium and high groups. However, considering the interactions, neither lens-type and add-group, nor lens-type and test-distance achieved significance (p ≥ 0.080). Therefore, the post hoc model only included lens-type as a factor at each test-distance. The model indicated that participants wearing EDOF, on average, demonstrated better HCVA (average across all distances) than AOP (p < 0.001) and AOMF (p = 0.038).
Table 2.
Observed mean ± SD of visual acuities, contrast sensitivity and near stereopsis variables for the three study lenses.
| Study variable | EDOF | AOMF | AOP |
|---|---|---|---|
| High illumination, HCVA | |||
| Distance (LogMAR) | −0.07 ± 0.06 | −0.07 ± 0.08 | −0.06 ± 0.08 |
| At 70 cm (LogMAR) | −0.07 ± 0.08 | −0.03 ± 0.09 | 0.00 ± 0.10 |
| At 50 cm (LogMAR) | 0.01 ± 0.10 | 0.03 ± 0.11 | 0.06 ± 0.12 |
| At 40 cm (LogMAR) | 0.10 ± 0.11 | 0.13 ± 0.13 | 0.12 ± 0.11 |
| High illumination, LCVA (Distance) | 0.27 ± 0.10 | 0.22 ± 0.10 | 0.27 ± 0.09 |
| Low illumination, LCVA (Distance) | 0.35 ± 0.12 | 0.30 ± 0.10 | 0.37 ± 0.12 |
| Distance contrast sensitivity | |||
| (6 cyc/deg, Log units) | 1.44 ± 0.11 | 1.47 ± 0.11 | 1.44 ± 0.09 |
| (12 cyc/deg, Log units) | 1.21 ± 0.16 | 1.26 ± 0.15 | 1.21 ± 0.16 |
| (18 cyc/deg, Log units) | 0.95 ± 0.23 | 1.01 ± 0.19 | 0.92 ± 0.20 |
| Stereopsis at 40 cm (arc sec) | 61 ± 37 | 97 ± 129 | 74 ± 63 |
HCVA = high contrast visual acuity.
LCVA = low contrast visual acuity.
EDOF = extended depth of focus.
AOMF = AIR OPTIX Aqua multifocal.
AOP = ACUVUE OASYS for Presbyopia.
For high-illumination LCVA, there were significant differences between lens-type (p = 0.019) and add-group (p < 0.001), however the interaction between lens-type and add-group was not significant (p = 0.292). Post hoc paired analysis demonstrated that EDOF lens was inferior to AOMF by two letters (p = 0.021) and not different from AOP (p = 1.00). For the low-illumination, LCVA at 6 m, there were significant differences between lens-type (p = 0.001) and add-group (p = 0.001), however the interaction between lens-type and add-group was not significant (p = 0.079). Post hoc paired analysis demonstrated that EDOF lens was inferior to AOMF by two letters (p = 0.012) and not different from AOP (p = 1.00). For both high- and low-illumination, the low add participants achieved better LCVA, followed by medium and high add groups.
For distance contrast sensitivity, significant differences were found for lens-type (p = 0.001), spatial-frequency (p < 0.001) and add-group (p = 0.021) factors, however the interaction between lens-type and spatial-frequency factors did not achieve significance (p = 0.529). Nevertheless, the interaction between lens-type and add-group was found to be significant (p = 0.023). Therefore, the data was split by add-group and the contrast sensitivity data was averaged across all spatial frequencies. The model suggested that EDOF lenses were inferior to AOMF by 1–2 letters in the medium and high add group (p < 0.007) but not different in the low-add group (p = 0.876). Distance contrast sensitivity with EDOF lenses were no different from AOP for all add-groups (p > 0.519).
For the near stereopsis variable, there was a significant difference between lens types (p = 0.008). Participants wearing EDOF had significantly better stereopsis than those wearing AOMF (Δ = 36 seconds-of-arc, p = 0.028) and AOP (Δ = 13 seconds-of-arc, p = 0.05). This observation was independent of the add-group (p = 0.731). The difference between the prescribed study lens power and vertex-corrected spherical equivalent at baseline for test and control lenses were insignificant (−0.01 ± 0.08, 0.01 ± 0.05 and −0.01 ± 0.05 for EDOF, AOMF, AOP, respectively, p = 0.102).
Subjective variables
The observed subjective ratings (mean ± SD) obtained from participants wearing all three study lenses at various test distances, during day and night-time conditions, are detailed in Table 3.
Table 3.
Observed mean ± SD of subjective variables for the three study lenses.
| Subjective variables (on a 1–10 scale, higher the better) | EDOF | AOMF | AOP | |
|---|---|---|---|---|
| Distance vision clarity | Day | 7.8 ± 1.7 | 7.9 ± 1.8 | 7.1 ± 2.2 |
| Night | 7.5 ± 1.8 | 7.5 ± 1.7 | 7.0 ± 2.0 | |
| Intermediate vision clarity | Day | 7.9 ± 1.6 | 7.5 ± 1.7 | 6.9 ± 1.6 |
| Night | 7.6 ± 1.7 | 7.2 ± 1.8 | 6.7 ± 1.5 | |
| Near vision clarity | Day | 7.4 ± 1.8 | 6.6 ± 2.0 | 6.0 ± 1.9 |
| Night | 7.1 ± 1.9 | 6.3 ± 2.2 | 5.7 ± 1.9 | |
| Distance lack of ghosting | Day | 8.2 ± 2.0 | 8.3 ± 2.2 | 7.5 ± 2.6 |
| Night | 7.9 ± 2.2 | 7.9 ± 2.2 | 7.4 ± 2.6 | |
| Intermediate lack of ghosting | Day | 8.5 ± 1.7 | 8.1 ± 2.0 | 7.5 ± 2.0 |
| Night | 8.3 ± 1.6 | 7.9 ± 2.1 | 7.6 ± 1.9 | |
| Near lack of ghosting | Day | 8.2 ± 1.9 | 7.6 ± 2.2 | 7.1 ± 2.3 |
| Night | 8.1 ± 1.8 | 7.3 ± 2.3 | 7.1 ± 2.2 | |
| Vision stability | Day | 8.1 ± 1.4 | 7.9 ± 1.7 | 7.3 ± 2.0 |
| Night | 8.2 ± 1.2 | 7.8 ± 1.7 | 7.4 ± 1.7 | |
| Driving vision | Day | 8.0 ± 1.6 | 8.0 ± 1.5 | 7.2 ± 2.1 |
| Night | 7.5 ± 1.7 | 7.4 ± 1.4 | 6.8 ± 2.0 | |
| Lack of bothersome haloes at night | 8.9 ± 1.5 | 8.3 ± 2.0 | 8.3 ± 2.2 | |
| Overall vision satisfaction | 7.6 ± 1.8 | 6.7 ± 2.1 | 5.7 ± 2.6 | |
| Ocular comfort | 8.5 ± 1.3 | 7.6 ± 1.9 | 8.0 ± 1.6 | |
EDOF = extended depth of focus.
AOMF = AIR OPTIX Aqua multifocal.
AOP = ACUVUE OASYS for Presbyopia.
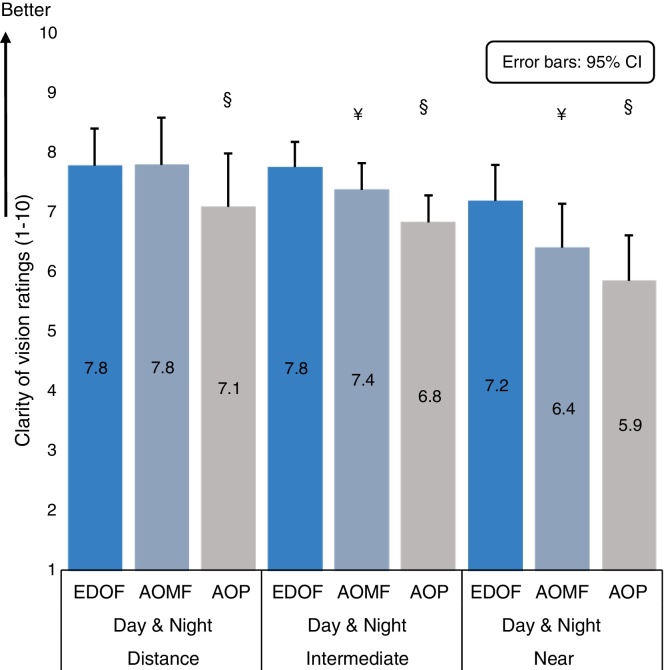
For the clarity of vision variable, significant differences were observed between lens-type (p < 0.001) and test-distance (p < 0.001). The interaction of lens type with test-distance was significant at the 5% level of significance (p = 0.044). Time-of-day was a significant factor (p = 0.001). The ratings obtained during night-time were lower to those obtained during day-time, however the difference between lens types did not interact with time-of-day (p = 0.936) or add-group (p = 0.585). The model indicates that for day/night-time conditions, participants wearing prototype lenses rated their clarity of vision significantly clearer than AOP distance (Δ = 0.7 units, p = 0.021), intermediate (Δ = 1.0 unit, p < 0.001) and near (Δ = 1.3 units, p < 0.001); and significantly clearer than AOMF at intermediate (Δ = 0.4 units, p = 0.028) and near (Δ = 0.8 units, p < 0.001). The estimated means of clarity of vision ratings for all three study lenses determined from the linear mixed model, for each test distance (day and night combined) can be seen in Fig. 2.
Figure 2.
Estimated means (means calculated assuming an equal distribution between add-groups) for ‘clarity of vision’ ratings at each test distance (day and night time measures combined) determined from the linear mixed model for all study lenses. The error bars indicate the upper bound of the 95% confidence interval. The symbol ‘¥’ represents statistically significant difference observed between extended depth-of-focus prototype (EDOF) and AIR OPTIX Aqua multifocal (AOMF) lenses and symbol ‘§’ represents statistically significant difference observed between EDOF and ACUVUE OASYS for presbyopia (AOP) lenses.
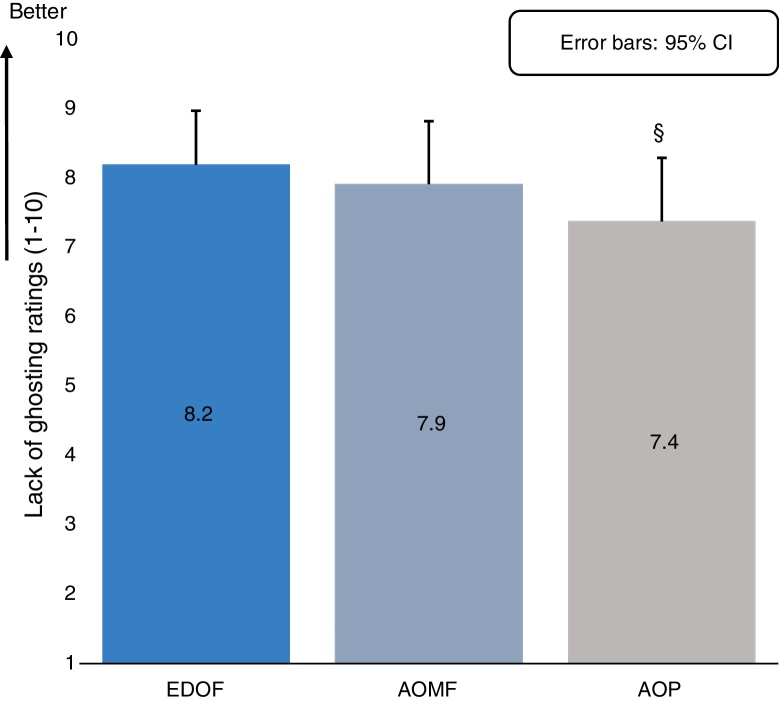
For the lack of ghosting ratings variable, there were significant main effects with lens-type (p < 0.001) and test-distance (p < 0.001) as factors. The lack of ghosting ratings obtained at near were lowest, followed by intermediate and far test distances. Time-of-day was not significant (p = 0.077) nor were any of the interactions (p > 0.056). As the interaction between lens-type and test-distance were insignificant at 5%, the model was adjusted to look at effect of lens type for an average of lack of ghosting measure across test distances and day/night conditions. The results indicate that on average, participants wearing EDOF rated significantly less ghosting than AOP (Δ = 0.8 units, p < 0.001) but not AOMF (Δ = 0.3 units, p = 0.186). The estimated means of lack of ghosting ratings for all three study lenses determined from the linear mixed model, for all test distances combined (day and night combined) is presented in Fig. 3.
Figure 3.
Estimated means (means calculated assuming an equal distribution between add-groups) for ‘lack of ghosting’ ratings averaged across all test distances (day and night time measures combined) determined from the linear mixed model for all study lenses. The error bars indicate the upper bound of the 95% confidence interval. The symbol ‘¥’ represents statistically significant difference observed between extended depth-of-focus prototype (EDOF) and AIR OPTIX Aqua multifocal (AOMF) lenses and symbol ‘§’ represents statistically significant difference observed between EDOF and ACUVUE OASYS for presbyopia (AOP) lenses.
For the vision-stability variable, there was a significant difference between lens-types (p < 0.001) but not with time-of-day (p = 0.787), add-group (p = 0.476) or their interaction (p = 0.788). Participants rated their vision-stability with EDOF significantly better than with AOP (Δ = 0.9 units, p < 0.001) and no different from AOMF (Δ = 0.3 units, p = 0.177).
For driving vision, significant differences were found between lens type (p < 0.001) and time of day (p = 0.009). however, their interaction was not significant (p = 0.849). The ratings obtained during night-time were lower to those obtained during day-time The model predicted that driving vision was significantly better with EDOF compared to AOP (Δ = 0.7 units, p = 0.003) but not different to AOMF (Δ = 0 units, p = 1.00).
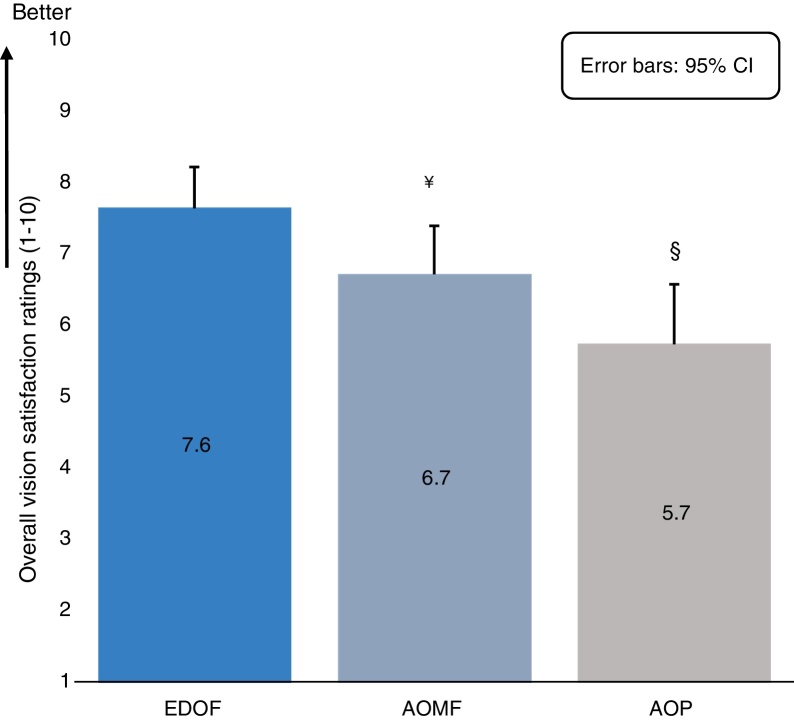
With the overall-vision satisfaction variable, there was a significant effect of lens type (p < 0.001), with participants wearing EDOF rating their overall-vision satisfaction significantly higher than wearing AOMF (Δ = 0.9 units, p = 0.024) and AOP (Δ = 1.9 units, p < 0.001). Fig. 4 presents the estimated means of overall vision satisfaction for all three study lenses determined from the linear mixed model.
Figure 4.
Estimated means (means calculated assuming an equal distribution between add-groups) for ‘overall vision satisfaction’ ratings at each test distance (day and night time measures combined) determined from the linear mixed model for all study lenses. The error bars indicate the upper bound of the 95% confidence interval. The symbol ‘¥’ represents statistically significant difference observed between extended depth-of-focus prototype (EDOF) and AIR OPTIX Aqua multifocal (AOMF) lenses and symbol ‘§’ represents statistically significant difference observed between EDOF and ACUVUE OASYS for presbyopia (AOP) lenses.
With the overall-comfort variable, there was a significant effect of lens type (p = 0.003). Participants rated their overall-comfort significantly higher with EDOF than with AOMF (Δ = 0.9 unit, p = 0.009) and AOP (Δ = 0.5 unit, p = 0.011).
With the lack of bothersome haloes variable, there was no significant effect for the lens-type suggesting that the night-time halo experience with EDOF was no different from AOMF and AOP (p > 0.146).
The average daily contact lens wear-time and number of hours with acceptable vision in participants wearing the three study lenses are detailed in Table 4. For the average daily contact lens wear-time variable, there was a significant effect of the lens-type (p = 0.022) and add group (p = 0.004) but not their interaction (p = 0.680). The low-add participants, on averaged, had a higher lens wear time, followed by medium and high add groups. The model suggests that participants reported significantly greater wearing hours with EDOF over AOP (Δ = 1.3 h, p = 0.012) but not AOMF (Δ = 0.5 h, p = 0.616). For the question on the number hours with acceptable vision with study lenses, again, there was a significant effect of the lens-type (p = 0.001) and add group (p = 0.006) but not their interaction (p = 0.869). The model suggests that participants reported significantly greater number of hours with acceptable vision when wearing EDOF compared to AOP (Δ = 2.9 h, p < 0.001) but not AOMF (Δ = 0.9 h, p = 0.224).
Table 4.
Observed means ± SD of CL wear time for the three study lenses.
| CL wear time | EDOF | AOMF | AOP |
|---|---|---|---|
| Number of hours with acceptable vision | 9.5 ± 3.3 | 8.4 ± 4.1 | 6.6 ± 4.3 |
| Average daily wear time | 10.8 ± 2.9 | 10.3 ± 3.1 | 9.5 ± 3.3 |
EDOF = extended depth of focus.
AOMF = AIR OPTIX Aqua multifocal.
AOP = ACUVUE OASYS for Presbyopia.
Lens fitting
Centration, primary gaze movement, primary gaze lag and tightness (mean ± SD) for all three study lenses at the Assessment Visit are detailed in Table 5. There were no significant differences between lens types for horizontal centration (p = 0.170) while a significant difference was found between lens types for all other lens fitting measures (p ≤ 0.007). All differences between lens types were clinically insignificant.
Table 5.
Lens fitting parameters (mean ± SD) for the three lens types at the assessment visit.
| Lens fitting parameter | EDOF | AOMF | AOP |
|---|---|---|---|
| Horizontal centrationa (mm) | −0.04 ± 012 | −0.05 ± 0.09 | −0.07 ± 0.11 |
| Vertical centrationb (mm) | 0.02 ± 010 | −0.04 ± 0.08 | 0.00 ± 0.09 |
| Primary gaze movement (mm) | 0.16 ± 010 | 0.22 ± 0.09 | 0.13 ± 0.08 |
| Primary gaze lag (mm) | 0.06 ± 0.07 | 0.09 ± 0.06 | 0.05 ± 0.06 |
| Tightness (%) | 50 ± 9 | 46 ± 7 | 55 ± 6 |
EDOF = extended depth of focus.
AOMF = AIR OPTIX Aqua multifocal.
AOP = ACUVUE OASYS for Presbyopia.
Positive values indicate nasal decentration. Negative values indicate temporal decentration.
Positive values indicate superior decentration. Negative values indicate inferior decentration.
Discussion
Overall, the EDOF prototypes demonstrated some improvements over the commercially available zonal-refractive and aspheric centre-near designs, AOP and AOMF, respectively. The improvements in visual performance with EDOF lenses were noticed in clarity of vision (at one or more visual distances), lack of ghosting average across all distances (only with AOP) and overall vision satisfaction variables. Most of these observations were in-line with the outcomes from our previous short-term (1-h) evaluations.19, 20 The insignificant interaction between ‘lens-type’ and ‘add-group’ suggests that the improvements in performance seen with prototypes were not driven by a particular participant pool.
The current study's findings were also in-line with many of the predictions from the theoretical modelling, presented in Part 1 of the study. Improved performance for intermediate and/or near with the new prototype lenses over the controls remained unaffected by the time of day, indicated as performance invariance to pupil diameter changes as described in Part 1. The predicted poor performance with decentered AOMF lenses in Part 1 did not occur because AOMF lenses were well-centred on eye. The theoretical modelling from this profile was in-line with the outcomes the current study. The major discrepancy between theoretical modelling and clinical trial outcomes occurred for near visual performance with AOP lenses. Compared to EDOF, modelling indicated similar distance and near performance with AOP but worse intermediate due to the bimodal nature of AOP. The clinical trial found similar distance but worse intermediate and near. This unexpected near result was probably influenced by the intermediate result – participants experienced a poor intermediate and so expected to experience a poor near, despite the predicted result from theory. This result indicates that while theoretical modelling may be a useful indicator of lens performance, the final determinant of performance is a human clinical trial.
When considering conventional, pupil-dependent multifocal optics, that are based on either centre-distance or centre-near principles, it can be drawn from theory that for any given pupil, the through-focus performance is expected to follow a ‘see–saw’ response. In other words, the better the lens performance is for distance, the worse the performance would be at near and vice versa. This can be observed in the theoretical modelling obtained with AOMF designs. As previously discussed, the EDOF prototypes presented here are optimized via deliberate manipulation of higher order spherical aberrations to yield an extension in depth of focus. This facilitates improvement in visual performance at intermediate and near, without incurring a significant compromise at distance. Comparing prototypes with controls, it is reasonable to state that the design achieved its purpose, at least as gauged by the clarity of vision variable.
There were no significant differences for distance acuities between the prototype and control lenses. Although the observed visual acuity with the prototype lenses was better than with the control lenses at intermediate and near test distances, the differences were not clinically relevant as they were within 2 letters. Unlike our previous short-term studies,19, 20 the current trial used a conventional ‘resolution-based’ acuity test instead of a ‘comfort-based’ reading assessment to measure intermediate and near visual performance. As a result, the average near visual acuity measures with both prototype and control lenses were on average 0.2–0.3 logMAR better than our previous observations with similar lenses. In our previous studies, we reported that the ‘comfort-based’ acuity was able to demonstrate clinically significant differences between prototypes and controls, suggesting that a less sensitive variable like resolution-based acuity may not be an ideal choice when comparing presbyopic visual performance between multifocal contact lenses.
This study is in agreement with several previous studies assessing AOMF and AOP for many acuity-based measurements including HCVA at 6 m9, 28, 29; LCVA at 6 m under low illumination29; distance contrast sensitivity9; HCVA at 70 cm29 and 40 cm90,29 and near stereopsis.29 A short-term study by Vasudevan et al.28 reported much better LCVA at 6 m and HCVA at 40 cm for participants wearing AOMF and AOP than the current study. However, these discrepancies may be due differences between Vasudevan et al. vs. this study for contrast setting when measuring LCVA (36%28 vs. 10%) and participant age (41 ± 1 years28 vs. 53 ± 5 years).
Enhancements in intermediate and/or near vision performance, while prescribing multifocals can also be achieved by practicing modified monovision techniques,30, 31, 32, 33 where one eye is prescribed to correct a range of distances spanning distance to intermediate, while the other eye is prescribed to correct from intermediate to near. The binocular summation capabilities of the visual system are expected to provide clear images for the whole range.34 In the current clinical trial, efforts were made to refrain from such a correction philosophy. The initial lens dispensing protocol was set up to keep the inter-ocular visual acuity difference within 4 letters for both test and control lenses.
The fitting guides for both AOMF and AOP suggest “trouble-shooting” strategies for improving visual performance following initial lens fitting.25, 26 While these may be routinely performed in clinical practice, these strategies were not performed in the current study due to logistical considerations and so are a study limitation. However, this did not bias results as the limitation was applied to test and control contact lenses.
An independent effort to validate our subjective questionnaires was not deemed necessary due to the simplistic nature and short construct of the questionnaire instrument used. Indeed, similar questions were asked in our previous short-term assessment of prototype contact lenses.19, 20 The primary aim of the current study was to evaluate if visual performance gauged via subjective responses obtained with the prototypes were different from the commercial controls. Given that the study design was executed in a randomized, cross-over manner, the reliability, content and/or criterion bias (if any) remains constant throughout all repeated administrations of the questionnaire. Thus, the bias (if any) will be washed out when considering differences between the subjective ratings with different lens types.
We acknowledge that a double-blind trial would have been more robust. However, due to the study logistics, difference in lens handling tints, slight differences in the prescribed fitting guides between the prototype and controls, we were not able to mask the investigators. However, given that subjective measures are more sensitive than acuity measures23 when assessing visual performance with multifocal contact lenses, we allowed participants to enter their subjective performance directly into the database without investigator's intervention. Thus, we believe that the investigators being unmasked did not bias the overall findings of the study. Some of the participants could have been habitual wearers of the control lenses used in this study. One may argue that this could potentially introduce bias, as they may have been able to identify their lenses. Upon analyzing our baseline data, we identified only 2/43 participants as habitual wearers of AOMF and none habitually wearing AOP. Therefore, it is unlikely that such a small proportion would affect the overall outcome of the study.
One other shortcoming of this study was that the wearing modalities of prototype and controls were different. The former lens was used as a daily-disposable, while the latter were prescribed for multiple-use with peroxide-based lens-care regimen. It is possible that the significantly higher comfort experienced with the test lenses may have been influenced by the wearing modality and therefore it may be perceived that it influenced the visual performance results. However, it is observed that that AOMF performed 0.5–1.0 units better than AOP for various subjective variables despite AOMF 0.5 units worse for comfort compared to AOP. This observation is further supported by the data on the average number of wearing hours per day and the number of hours of acceptable vision per day between AOMF and AOP. Clearly, despite the fact that AOP are more comfortable than AOMF, AOP were on average worn for fewer hours and provided fewer hours of acceptable vision quality than AOMF. It demonstrates that this particular cohort seem to have the ability to distinguish between comfort and vision. Therefore, we do not think the disparity in wearing modality and/or comfort confounded this studies’ overall findings. One may argue that the prototype lenses could have been offered as a frequent replacement lenses (like controls) to further reduce bias, if any. As the optical undulations engraved onto the prototype lenses were sub-micron in dimension, we avoided any chance of affecting the profiles by prescribing them as re-usable lenses. On the other hand, the control lenses were intended by the manufacturer to be used as a monthly-replacement lens; furthermore, the cost involved with using control lenses as daily disposables were prohibitive. Nevertheless, we acknowledge that using the controls as multiple-use may have created some resentment in participants towards these lenses, potentially leading to lower subjective ratings, and so it is important to further investigate prototype lens performance with daily disposable control lenses to confirm this assumption.
Conclusions
After 1 week of lens wear, EDOF prototype contact lenses offer significant improvements in subjective visual performance over AOMF and AOP for clarity of vision at intermediate and near without compromising distance vision.
Conflicts of interest
This project is entirely funded by the Brien Holden Vision Institute and the Institute has proprietary interests in the intellectual property governing extended depth-of-focus contact lenses (Patent application number WO2014059465 A1) and receives royalties from the sale of centre-near contact lenses described in this manuscript.
Acknowledgements
The authors would like to acknowledge the clinical team (Ms. E. Robertson, Ms. K. Wagenfeuhr and Ms. Ludlow), the database management team (Dr. T. John and Ms. K. Laarakkers), the technology team (Ms. Perera, Dr. Kim, Dr. Ehrmann, Dr. Conrad and Dr. Fedtke) and the quality management team (Ms. Morgan, Dr. Erickson and Mr. May) for their invaluable support to run this trial at the Clinical Research Trials Centre, Brien Holden Vision Institute, Sydney, Australia. The authors would like to extend sincere gratitude to the late Professor Holden, whose inspirational leadership and foresight made this project possible.
Appendix. Procedure to convert acuity measures
The near LogMAR chart used in this study was designed to be used at 40 cm. However, the same chart has been used to collect acuity measurements at 50 cm and 70 cm. The following procedure calculated the adjusted visual acuity (logMAR) for these specific distances.
Dstd = the standard distance at which the chart is calibrated (cm).
Dmes = the distance at which visual acuity measurements are taken (cm).
Astd = the angle a specific letter subtends at the eye at the standard distance at which the chart is calibrated (min of arc).
Ames = the angle a specific letter subtends at the eye at the distance at which visual acuity measurements are taken (min of arc).
For example, the letter size of 0 logMAR (6/6 equivalent) on a near acuity chart calibrated at 40 cm (Dstd) subtends 5 min of arc (Astd) at 40 cm. If the same chart was used at 50 cm (Dmes) and 6/6 was achieved, then using the above formula, Ames = 4 min or arc and the adjusted visual acuity = −0.10 logMAR.
References
- 1.Holden B.A., Fricke T.R., May Ho S. Global vision impairment due to uncorrected presbyopia. Arch Ophthalmol. 2008;126:1731–1739. doi: 10.1001/archopht.126.12.1731. [DOI] [PubMed] [Google Scholar]
- 2.Morgan P.B., Efron N., Woods C.A. An international survey of contact lens prescribing for presbyopia. Clin Exp Optom. 2011;94:87–92. doi: 10.1111/j.1444-0938.2010.00524.x. [DOI] [PubMed] [Google Scholar]
- 3.Morgan P.B., Woods C.A., Tranoudis I.G. International contact lens prescribing in 2014. Contact Lens Spectr. 2015;30:28–33. [Google Scholar]
- 4.Efron N., Nichols J.J., Woods C.A., Morgan P.B. Trends in US contact lens prescribing 2002 to 2014. Optom Vis Sci. 2015;92:758–767. doi: 10.1097/OPX.0000000000000623. [DOI] [PubMed] [Google Scholar]
- 5.Agahi N., Parker M.G. Are today's older people more active than their predecessors? Participation in leisure-time activities in Sweden in 1992 and 2002. Ageing Soc. 2005;25:925–941. [Google Scholar]
- 6.Llorente-Guillemot A., Garcia-Lazaro S., Ferrer-Blasco T., Perez-Cambrodi R.J., Cervino A. Visual performance with simultaneous vision multifocal contact lenses. Clin Exp Optom. 2012;95:54–59. doi: 10.1111/j.1444-0938.2011.00666.x. [DOI] [PubMed] [Google Scholar]
- 7.Fedtke C., Bakaraju R.C., Ehrmann K., Chung J., Thomas V., Holden B.A. Visual performance of single vision and multifocal contact lenses in non-presbyopic myopic eyes. Contact Lens Anterior Eye. 2016;39:38–46. doi: 10.1016/j.clae.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 8.Kollbaum P.S., Dietmeier B.M., Jansen M.E., Rickert M.E. Quantification of ghosting produced with presbyopic contact lens correction. Eye Contact Lens. 2012;38:252–259. doi: 10.1097/ICL.0b013e31825aa879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Madrid-Costa D., Garcia-Lazaro S., Albarran-Diego C., Ferrer-Blasco T., Montes-Mico R. Visual performance of two simultaneous vision multifocal contact lenses. Ophthalmic Physiol Opt. 2013;33:51–56. doi: 10.1111/opo.12008. [DOI] [PubMed] [Google Scholar]
- 10.Shah A.S., Gundel R. Low-contrast visual acuity measurements in single-vision and bifocal soft lens wearers. Int Contact Lens Clin. 2000;27:119–123. [Google Scholar]
- 11.Plainis S., Ntzilepis G., Atchison D.A., Charman W.N. Through-focus performance with multifocal contact lenses: effect of binocularity, pupil diameter and inherent ocular aberrations. Ophthalmic Physiol Opt. 2013;33:42–50. doi: 10.1111/opo.12004. [DOI] [PubMed] [Google Scholar]
- 12.Bakaraju R.C. University of New South Wales; Sydney: 2010. Optical Performance of Simultaneous Vision Multifocal Contact Lenses Using Schematic and Physical Eye Models. PhD Thesis. [Google Scholar]
- 13.Rocha K.M., Vabre L., Chateau N., Krueger R.R. Expanding depth of focus by modifying higher-order aberrations induced by an adaptive optics visual simulator. J Cataract Refract Surg. 2009;35:1885–1892. doi: 10.1016/j.jcrs.2009.05.059. [DOI] [PubMed] [Google Scholar]
- 14.Benard Y., Lopez-Gil N., Legras R. Subjective depth of field in presence of 4th-order and 6th-order Zernike spherical aberration using adaptive optics technology. J Cataract Refract Surg. 2010;36:2129–2138. doi: 10.1016/j.jcrs.2010.07.022. [DOI] [PubMed] [Google Scholar]
- 15.Piers P.A., Fernandez E.J., Manzanera S., Norrby S., Artal P. Adaptive optics simulation of intraocular lenses with modified spherical aberration. Invest Ophthalmol Vis Sci. 2004;45:4601–4610. doi: 10.1167/iovs.04-0234. [DOI] [PubMed] [Google Scholar]
- 16.Benard Y., Lopez-Gil N., Legras R. Optimizing the subjective depth-of-focus with combinations of fourth- and sixth-order spherical aberration. Vis Res. 2011;51:2471–2477. doi: 10.1016/j.visres.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 17.Yi F., Iskander D.R., Collins M. Depth of focus and visual acuity with primary and secondary spherical aberration. Vis Res. 2011;51:1648–1658. doi: 10.1016/j.visres.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 18.Bakaraju RC, Ehrmann K, Ho A, Holden BA, inventors. Lenses, devices, methods and systems for refractive error. USA patent US9201250 B2. Brien Holden Vision Institute, assignee; December 1, 2015.
- 19.Tilia D., Bakaraju R.C., Chung J. Short-term visual performance of novel extended depth-of-focus contact lenses. Optom Vis Sci. 2016;93:435–444. doi: 10.1097/OPX.0000000000000806. [DOI] [PubMed] [Google Scholar]
- 20.Tilia D., Munro A., Chung J. Short-term comparison between extended depth-of-focus prototype contact lenses and a commercially-available center-near multifocal. J Optom. 2017;10:14–25. doi: 10.1016/j.optom.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Diec J., Tilia D., Naduvilath T., Bakaraju R.C. Predicting short-term performance of multifocal contact lenses. Eye Contact Lens. 2016 doi: 10.1097/ICL.0000000000000286. [DOI] [PubMed] [Google Scholar]
- 22.Fernandes P.R., Neves H.I., Lopes-Ferreira D.P., Jorge J.M., Gonzalez-Meijome J.M. Adaptation to multifocal and monovision contact lens correction. Optom Vis Sci. 2013;90:228–235. doi: 10.1097/OPX.0b013e318282951b. [DOI] [PubMed] [Google Scholar]
- 23.Papas E.B., Decenzo-Verbeten T., Fonn D. Utility of short-term evaluation of presbyopic contact lens performance. Eye Contact Lens. 2009;35:144–148. doi: 10.1097/ICL.0b013e3181a20361. [DOI] [PubMed] [Google Scholar]
- 24.Lopes-Ferreira D., Neves H., Queiros A., Faria-Ribeiro M., Peixoto-de-Matos S.C., Gonzalez-Meijome J.M. Ocular dominance and visual function testing. Biomed Res Int. 2013;2013:238943. doi: 10.1155/2013/238943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Richdale K., Sinnott L.T., Skadahl E., Nichols J.J. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea. 2007;26:168–174. doi: 10.1097/01.ico.0000248382.32143.86. [DOI] [PubMed] [Google Scholar]
- 26.Alcon Laboratories; Fort Worth, Texas: 2014. Air Optix Aqua Multifocal Professional Fitting Guide. Updated 2014. Available at: http://ecatalog.alcon.com/CL/AirOptixFamily_fg_us_en.pdf. Accessed: 07.10.15. [Google Scholar]
- 27.Garcia-Lazaro S., Ferrer-Blasco T., Madrid-Costa D., Albarran-Diego C., Montes-Mico R. Visual performance of four simultaneous-image multifocal contact lenses under dim and glare conditions. Eye Contact Lens. 2015;41:19–24. doi: 10.1097/ICL.0000000000000060. [DOI] [PubMed] [Google Scholar]
- 28.Vasudevan B., Flores M., Gaib S. Objective and subjective visual performance of multifocal contact lenses: pilot study. Contact Lens Anterior Eye. 2014;37:168–174. doi: 10.1016/j.clae.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 29.Woods J., Woods C., Fonn D. Visual performance of a multifocal contact lens versus monovision in established presbyopes. Optom Vis Sci. 2015;92:175–182. doi: 10.1097/OPX.0000000000000476. [DOI] [PubMed] [Google Scholar]
- 30.Johannsdottir K.R., Stelmach L.B. Monovision: a review of the scientific literature. Optom Vis Sci. 2001;78:646–651. doi: 10.1097/00006324-200109000-00009. [DOI] [PubMed] [Google Scholar]
- 31.Evans B.J. Monovision: a review. Ophthalmic Physiol Opt. 2007;27:417–439. doi: 10.1111/j.1475-1313.2007.00488.x. [DOI] [PubMed] [Google Scholar]
- 32.Fisher K. Presbyopic visual performance with modified monovision using multifocal soft contact lenses. Int Contact Lens Clin. 1997;24:91–100. [Google Scholar]
- 33.Schwarz C., Manzanera S., Prieto P.M., Fernandez E.J., Artal P. Comparison of binocular through-focus visual acuity with monovision and a small aperture inlay. Biomed Opt Express. 2014;5:3355–3366. doi: 10.1364/BOE.5.003355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zheleznyak L., Sabesan R., Oh J.-S., MacRae S., Yoon G. Modified monovision with spherical aberration to improve presbyopic through-focus visual performance. Invest Ophthalmol Vis Sci. 2013;54:3157–3165. doi: 10.1167/iovs.12-11050. [DOI] [PMC free article] [PubMed] [Google Scholar]