Abstract
Background
Little is known about the long-term prognostic values of both thrombolysis in myocardial infarction (TIMI) and Global Registry of Acute Cardiac Events (GRACE) risk scores (RSs) to the Asian ethnicity. The purpose of this study is to compare the usefulness of these two scores in risk stratification and prediction of long-term (up to 3 years) outcomes for Chinese patients with myocardial infarction (MI).
Methods
We calculated the TIMI and GRACE RSs for 726 consecutive patients with MI [55.6% with ST-segment elevation (STEMI) and 44.4% with non-ST-segment elevation (NSTEMI)].
Results
Although the risk profile of our population (median TIMI score = 5 for STEMI, 4 for NSTEMI, and median GRACE score = 164) was higher, the in-hospital mortality (7.1% for NSTEMI and 6.7% for STEMI) was comparable to that predicted by GRACE RS. The GRACE RS worked well in predicting short-term and long-term death (C-statistics range 0.710 to 0.789) and triple (death, MI, and stroke) endpoints (C-statistics range 0.695 to 0.764) in both subsets of MI. GRACE RS performed significantly better than the TIMIRS in predicting 3-year mortality in NSTEMI (p = 0.035) and 1-year and 3-year mortality in STEMI (p = 0.028 and 0.009, respectively). Stratification by tertiles of GRACERS furnished greater prognostic information versus risk assessment by the TIMI RS.
Conclusions
The use of RSs revealed a fair to good discriminatory accuracy in predicting both short-term and long-term major adverse cardiac events in Asian patients with MI. Compared with the simpler TIMI RS, the GRACERS was more accurate in predicting long-term mortality.
Keywords: GRACE risk score, Myocardial infarction, Prognosis, Risk stratification, TIMI risk score
INTRODUCTION
Despite advances in treatment, acute coronary syndrome (ACS) is still associated with significant mortality.1 Identifying high-risk patients, and hence selecting those who would benefit from more aggressive treatment, is essential for the management of ACS. Furthermore, stratification of the risk of ACS using tools such as risk scores (RSs) is recommended by practice guidelines.1,2
The most widely used RS is the thrombolysis in myocardial infarction (TIMI) algorithm,3,4 which is simple to calculate and is derived from selected clinical-trial cohorts. For ST-segment elevation myocardial infarction (STEMI), the TIMI score is based on eight clinical indicators available on admission with scores ranging from 0 to 14. For non-ST-segment elevation myocardial infarction (NSTEMI), the TIMI score is based on seven clinical indicators with scores ranging from 0 to 7. The second most commonly used score is the Global Registry of Acute Coronary Events (GRACE) risk model,5 which uses eight variables and is applicable to the entire spectrum of ACS. This scoreis derived from a more representative community-based registry.
These two RSs, however, were developed by enrolling patients mostly from countries in North America, South America and Europe, with only Australia and New Zealand providing data from Asian countries to the GRACE registry. In addition, they were developed initially to predict short-term prognoses. Although these RSs have been externally validated in Western countries, their com-parative performance in Asian populations has not been studied in detail. Furthermore, current knowledge about whether the application of these RSs can indeed predict long-term outcomes is inadequate.
The aims of this study were to compare the performance of TIMI and GRACE RSs in the risk stratification of Chinese patients with myocardial infarction (MI), and to examine whether these RSs, when calculated on admission, could be used to predict long-term (up to 3 years) outcomes. Information regarding the long-term prognostic value of RSs may remind patients and physicians of the importance of adherence to secondary prevention measures as recommended by guidelines.1,2
METHODS
Study population
This was a retrospective study of consecutive patients with MI admitted to a coronary care unit of the Cardiology Division at Taipei Veterans General Hospital between May 2002 and August 2005. Patients with MI were classified into two groups: STEMI or NSTEMI. STEMI was defined as having ST-segment elevation ≥ 1 mm in 2 contiguous electrocardiographic leads (or ≥ 2 mm in V1 to V3 leads) or a new left bundle branch block together with chest pain for > 30 minutes and/or evidence of myonecrosis with an elevated troponin I level of ≥ 0.1 ng/mL. NSTEMI was diagnosed in patients with typical chest pain, a troponin I level ≥ 0.1 ng/mL, and no ST-segment elevation detected in electrocardiography. To reduce patient selection bias, there were no other specific exclusion criteria.
RS calculation
TIMI and GRACE scores were calculated from the initial clinical history, electrocardiograms, and laboratory values collected on admission. Although the present study was retrospective, all data were collected prospectively and entered into a computer database.
Endpoint
All of the included patients were followed up for at least 3 years or until the occurrence of a major event. The study endpoint was all-cause mortality and a composite endpoint of death, myocardial (re-)infarction, or stroke. We focused on all-cause mortality because this was the most robust endpoint. Stroke was included in the composite endpoint because cerebrovascular disease remains one of the leading causes of death in Asia. The diagnosis of reinfarction was based on the same criteria as the index event. Stroke was defined using World Health Organization (WHO) criteria as rapidly developing clinical signs of focal or global disturbance in cerebral function lasting for more than 24 hours or leading to death, with no apparent cause other than that of vascular origin.
In-hospital events were recorded from hospital charts. Data on long-term outcomes were obtained from hospital records, or direct telephone contact with the patient or surviving family members (all causes of death were recorded). The endpoints were analyzed at discharge, 6 months, 1 year, and 3 years.
Statistical analysis
Continuous variables with a normal distribution were expressed as medians and 25th and 75th percentiles, and categorical data as percentages. Statistical comparisons of baseline characteristics were performed using the χ2-test with Yates correction or Fisher’s exact test, as appropriate, for categorical variables, and the two-tailed Student’s t-test for continuous variables.
For each of the two RSs, receiver operating characteristic (ROC) curves were used to evaluate associations between the calculated scores and the rate of adverse clinical events at discharge, 6 months, 1 year, and 3 years. The area under the ROC curve or C-statistic was used as a measure of the discriminatory accuracy of the RS. The relative performance of each test was evaluated with a 95% confidence interval (CI) for the difference between two areas under the ROC curves.
To directly compare the utility of the RSs in predicting outcomes, we categorized the study population into low-, intermediate-, and high-risk groups using ascending tertiles of RSs. Rates of the endpoints were compared among risk strata for both RSs separately using χ2-tests.
Statistical analysis was performed using SPSS version 17.0 (SPSS Inc., Chicago, IL, USA) and MedCalc version 4.2 (MedCalc Software, Mariakerke, Belgium). Two-tailed tests of significance are reported. For all comparisons, a p-value of < 0.05 was considered to be statistically significant. When appropriate, 95% CIs were calculated.
RESULTS
Patient population
A total of 726 consecutive patients were included in this study, of whom 404 (55.6%) had STEMI and 322 (44.4%) had NSTEMI. Table 1 shows the baseline characteristics of the study population compared to the original cohort that was used to develop the GRACE RS.5 The in-hospital management strategies of the patients are presented in Table 2. Our patients tended to be older, more often male, have higher prevalence rates of diabetes and hypertension, more likely to present with heart failure, ST-segment depression in NSTEMI, and elevated serum creatinine on admission than the patients in the derivation set,3-5 revealing a significantly higher risk profile.
Table 1. Baseline characteristics of the study population and the GRACE risk score derivation cohort.
| Variable | Total (N = 726) | STEMI (N = 404) | NSTEMI (N = 322) | GRACE RS cohort (N = 11389) |
| Age (years)* | 71 (58, 76) | 68 (55, 75) | 73 (63, 77) | 66 (56, 75) |
| Sex (%) | ||||
| Male | 82.9 | 88.9 | 74.8 | 66.5 |
| Female | 17.1 | 11.1 | 15.2 | 33.5 |
| Risk factors (%) | ||||
| Diabetes mellitus | 36 | 29.2 | 44.7 | 23.3 |
| Hypercholesterolemia | 17.8 | 14.9 | 21.4 | 43.6 |
| Hypertension | 64.2 | 55.0 | 75.8 | 57.8 |
| Smoking | 43.8 | 51.0 | 34.7 | 56.7 |
| Previous history (%) | ||||
| Myocardial infarction | 11.1 | 7.2 | 16.1 | 32.0 |
| Myocardial revascularization | 15.2 | 6.4 | 26.1 | 22.0 |
| PCI | 10.7 | 5.2 | 17.7 | 14.0 |
| CABG | 4.4 | 1.2 | 8.4 | 8.0 |
| Peripheral arterial disease | 4.7 | 1.5 | 8.7 | 10.3 |
| TIA/stroke | 11.9 | 7.4 | 17.4 | 8.3 |
| Previous medication (%) | ||||
| ASA | 17.6 | 8.4 | 29.2 | 43.0 |
| ACE inhibitors/ARBs | 35.4 | 26.2 | 47.0 | 26.0 |
| Statins | 14.1 | 7.2 | 22.8 | 20.4 |
| On admission | ||||
| Heart rate (beat/min)* | 82 (67, 101) | 77 (65, 96) | 88 (74, 106) | 76 (65, 90) |
| Systolic BP (mmHg)* | 129 (108, 150) | 123 (104, 147) | 136 (113, 156) | 140 (120, 160) |
| Diastolic BP (mmHg)* | 71 (61, 85) | 71 (59, 84) | 72 (64, 86) | 80 (70, 90) |
| Serum creatinine (mg/dL)* | 1.2 (1.0, 1.7) | 1.2 (1.0, 1.5) | 1.4 (1.1, 2.1) | 1.0 (0.9, 1.2) |
| Killip class (%) | ||||
| I | 56.3 | 56.7 | 55.9 | 82.7 |
| II | 20.7 | 20.8 | 20.5 | 13.2 |
| III | 13.4 | 8.9 | 19.3 | 3.1 |
| IV | 9.6 | 13.6 | 4.3 | 1.0 |
| ST-segment depression ≥ 1 mm for NSTEMI (%) | 64.1 | 33.7 | ||
| Initial Tn I ≥ 0.1 ng/mL (%) | 84.4 | 79.0 | 91.3 | 31.6 |
| GRACE score* | 164 (134, 197) | 164 (136, 190) | 165 (133, 204) | - |
| In-hospital mortality, n (%) | 50 (6.9) | 27 (6.7) | 23 (7.1) | - |
| 6-month mortality, n (%) | 72 (9.9) | 36 (9.6) | 36 (12.2) | - |
| 1-year mortality, n (%) | 87 (12.0) | 40 (10.8) | 47 (16.4) | - |
| 3-year mortality, n (%) | 128 (17.6) | 50 (14.0) | 78 (27.9) | - |
ACE, angiotensin-converting enzyme inhibitors; ARBs, angiotensin II receptor blockers; ASA, aspirin; BP, blood pressure; CABG, coronary artery bypass grafting; GRACE, Global Registry of Acute Coronary Events; NSTEMI, non-ST-segment elevation myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction; TIA, transient ischemic attack; TIA, transient ischemic stroke.
* Median (percentile 25th, 75th).
Table 2. In-hospital management.
| Total (N = 726) | STEMI (N = 404) | NSTEMI (N =322) | |
| In-hospital medical treatment (%) | |||
| ASA | 98.3 | 99.5 | 96.9 |
| Clopidogrel | 80.6 | 82.9 | 77.6 |
| Beta-blockers | 52.3 | 52.0 | 52.8 |
| Statins | 36.5 | 38.6 | 33.9 |
| UFH/LMWH | 100 | 100 | 100 |
| ACE inhibitors/ARBs | 68.2 | 68.6 | 67.7 |
| Cardiac catheterization (%) | 87.0 | 85.7 | |
| In-hospital coronary revascularization (%) | |||
| PCI | 50.7 | 62.4 | |
| CABG | 10.2 | 9.9 |
ACE, angiotensin-converting enzyme inhibitors; ARBs, angiotensin II receptor blockers; ASA, aspirin; CABG, coronary artery bypass grafting; LMWH, low-molecular-weight heparin; NSTEMI, non-ST-segment elevation myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction; UFH, unfractionated heparin.
The all-cause mortality rate was 6.9% during the index admission, 9.9% at 6 months, 12.0% at 1 year, and 17.6% at 3 years. The composite endpoint of death, myocardial (re-)infarction, or stroke was 8.7% during the index admission, 14.3% at 6 months, 17.8% at 1 year, and 26.2% at 3 years.
Prognostic accuracy of the RSs
The median value of the TIMI RS was 5 (interquartile range 3-7) in the patients with STEMI and 4 (interquartile range 3-5) in those with NSTEMI. The median GRACE RS for all patients was 164 (interquartile range 134-197).
Areas under the ROC curve (C-statistics) of the two RSs to predict death and composite endpoints of death, myocardial (re-)infarction, or stroke at different time points in the patients with STEMI and NSTEMI are listed in Tables 3 and 4. Both the TIMI and GRACE RSs could discriminate patients in both subsets of MI with and without events, including all-cause mortality and composite endpoints of death, myocardial (re-)infarction, or stroke at different time points up to 3 years, even though they were both developed to predict short-term prognoses.
Table 3. C-statistics of the risk scores at different time points in patients with STEMI (n = 404).
| Events | TIMI (95% CI) | GRACE (95% CI) | Δ (95% CI) |
| Death | |||
| In-hospital | 0.738 (0.690 to 0.782) | 0.766 (0.720 to 0.808) | 0.028 (-0.050 to 0.106) |
| 6-month | 0.713 (0.662 to 0.760) | 0.778 (0.731 to 0.821) | 0.065 (-0.003 to 0.133) |
| 1-year | 0.711 (0.660 to 0.758) | 0.789 (0.742 to 0.831) | 0.079 (0.009 to 0.149) |
| 3-year | 0.684 (0.631 to 0.734) | 0.767 (0.718 to 0.812) | 0.083 (0.021 to 0.146) |
| Death/MI/stroke | |||
| In-hospital | 0.748 (0.701 to 0.792) | 0.764 (0.717 to 0.806) | 0.016 (-0.063 to 0.095) |
| 6-month | 0.721 (0.671 to 0.768) | 0.736 (0.686 to 0.782) | 0.015 (-0.051 to 0.081) |
| 1-year | 0.701 (0.650 to 0.749) | 0.745 (0.696 to 0.791) | 0.044 (-0.017 to 0.106) |
| 3-year | 0.695 (0.643 to 0.744) | 0.720 (0.668 to 0.767) | 0.025 (-0.027 to 0.076) |
Δ, difference between the two C-statistics. CI, confidence interval; GRACE, Global Registry of Acute Coronary Events; MI, myocardial infarction; TIMI, thrombolysis in myocardial infarction.
Table 4. C-statistics of the risk scores at different time points in patients with NSTEMI (n = 322).
| Events | TIMI (95% CI) | GRACE (95% CI) | Δ (95% CI) |
| Death | |||
| In-hospital | 0.653 (0.597 to 0.707) | 0.710 (0.656 to 0.761) | 0.057 (-0.099 to 0.213) |
| 6-month | 0.664 (0.606 to 0.719) | 0.768 (0.714 to 0.816) | 0.104 (-0.020 to 0.228) |
| 1-year | 0.680 (0.621 to 0.734) | 0.777 (0.724 to 0.825) | 0.097 (-0.007 to 0.202) |
| 3-year | 0.693 (0.634 to 0.747) | 0.780 (0.726 to 0.828) | 0.088 (0.006 to 0.169) |
| Death/MI/stroke | |||
| In-hospital | 0.627 (0.570 to 0.681) | 0.695 (0.640 to 0.747) | 0.069 (-0.073 to 0.211) |
| 6-month | 0.657 (0.599 to 0.712) | 0.716 (0.660 to 0.768) | 0.059 (-0.043 to 0.160) |
| 1-year | 0.650 (0.591 to 0.706) | 0.717 (0.661 to 0.769) | 0.067 (-0.021 to 0.155) |
| 3-year | 0.696 (0.639 to 0.750) | 0.739 (0.683 to 0.790) | 0.043 (-0.032 to 0.117) |
Δ, difference between the two C-statistics. Abbreviations are in Table 3.
In the patients with STEMI, the GRACE risk model was robust in predicting all-cause mortality (C-statistics range 0.766 to 0.789) and triple endpoints (C-statistics range 0.720 to 0.764) throughout the 3-year follow-up period (Table 3). The performance of the TIMI score was somewhat inferior to the GRACE risk model (C-statistics range 0.684 to 0.738 for all-cause mortality, and 0.695 to 0.748 for triple endpoints). The GRACE model demonstrated better discrimination than the TIMI score in predicting long-term mortality (p = 0.028 for 1year, and 0.009 for 3 years).
Regarding the patients with NSTEMI, the GRACE risk model was still robust in predicting all-cause mortality (C-statistics range 0.710 to 0.780) and performed reasonably well in predicting triple endpoints (C-statistics range 0.695 to 0.739) (Table 4). The TIMI score did not perform as well as the GRACE risk model, with C-statistics ranging from 0.653 to 0.693 in predicting all-cause mortality and 0.627 to 0.696 for triple endpoints. The C-statistic for predicting 3-year mortality using the GRACE model was significantly higher than that of the TIMI score (p = 0.035).
When stratifying the patients into ascending risk groups by tertiles of the TIMI and GRACE RSs, a significantly and consistently increasing gradient of risk was shown for both endpoints evaluated (Figures 1 and 2). For all-cause mortality in both subsets of MI, the risk gradient was steeper at all analyzed time points when the patients were stratified by the GRACE risk model. Patients identified to be at high risk by the TIMI score had a 4- to 10-fold higher mortality rate compared to those at low risk. In comparison, the patients in the highest tertile of GRACE RS had a 12- to 29-fold increased risk of death compared to those in the lowest tertile. For composite endpoints of death, myocardial (re-)infarction, or stroke, the risk gradient was also steeper across time when the patients with STEMI were stratified by the GRACE risk model, whereas no difference in the gradient was observed for those with NSTEMI.
Figure 1.
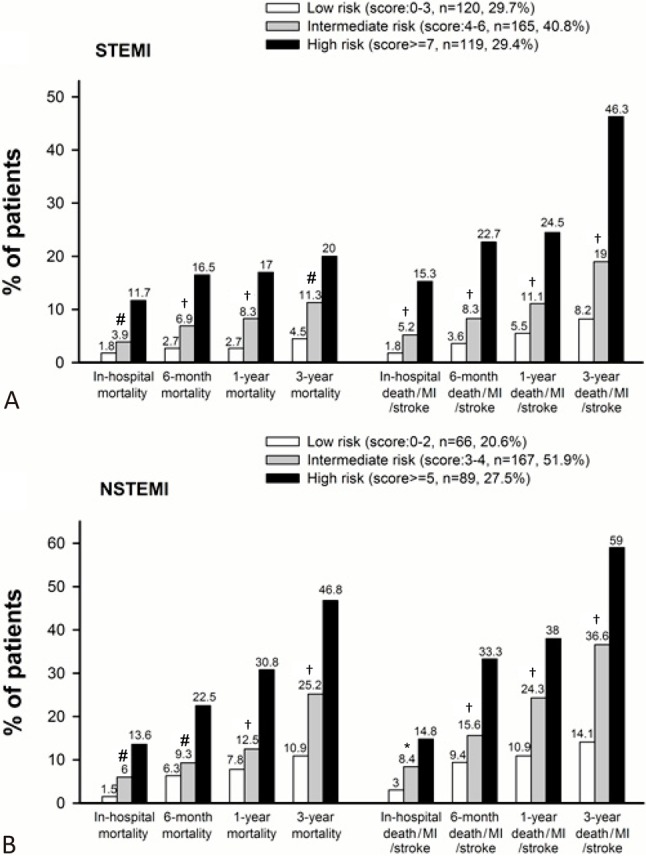
Rates of death and composite endpoints of death, myocardial (re-)infarction, or stroke for patients with STEMI (A) and NSTEMI (B) at all analyzed time points in low-, intermediate-, and high-risk groups by TIMI risk score (tertiles). p values are for trend. * p < 0.05, # p < 0.01, and † p < 0.001. NSTEMI, non-ST-segment elevation myocardial infarction; STEMI, ST-segment elevation myocardial infarction; TIMI, thrombolysis in myocardial infarction.
Figure 2.
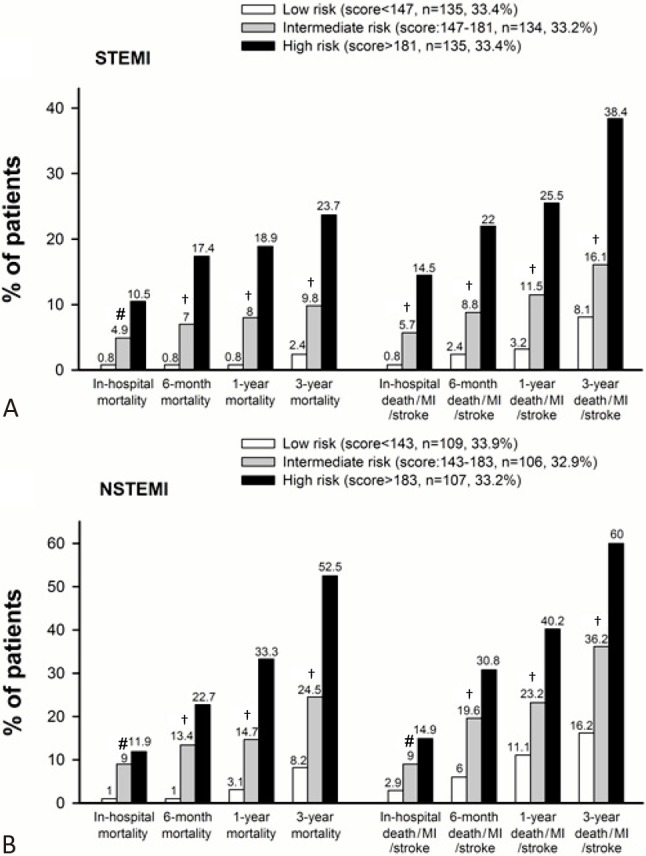
Rates of death and composite endpoints of death, myocardial (re-)infarction, or stroke for patients with STEMI (A) and NSTEMI (B) at all analyzed time points in low-, intermediate-, and high-risk groups by GRACE risk score (tertiles). p values are for trend. * p < 0.05, # p < 0.01, and † p < 0.001. Abbreviations are in Figure 1.
When the actual (observed) in-hospital mortality rate of our patients was compared with those (predicted) of the validation subsets (Figure 3), there was a trend of the TIMI model to overestimate the risk of death in the patients with STEMI and an underestimation of mortality in the patients with NSTEMI. The GRACE model generally overestimated the risk of mortality. Therefore, the predicted probability of in-hospital mortality may require recalibration. However, the discrepancy was not unidirectional (overestimation in the STEMI patients and underestimation in the NSTEMI patients).
Figure 3.
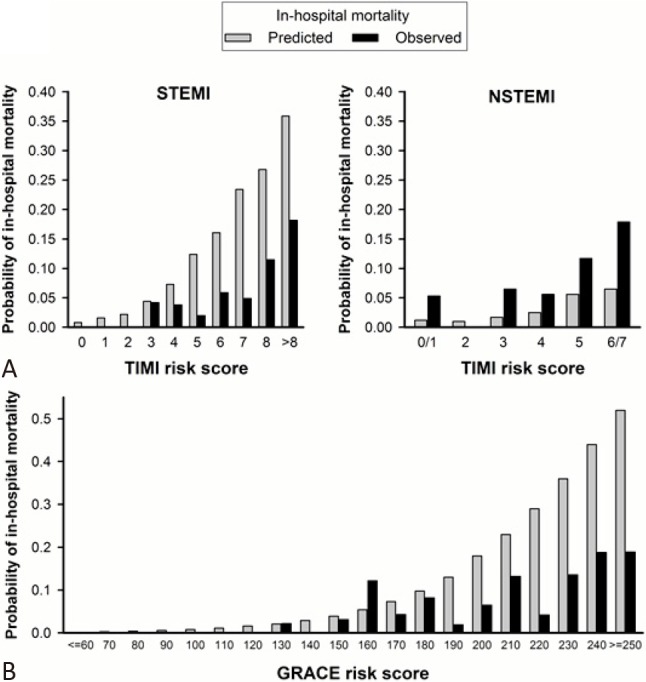
Observed (i.e., actual) vs. predicted in-hospital mortality rates of our patients compared to those of the validation subsets. Abbreviations are in Figure 1.
DISCUSSION
To the best of our knowledge, the present study is the first to show that both the TIMI and GRACE RSs have significant discriminatory ability for mortality and clinical outcomes at different time points up to 3 years in a cohort of Asian patients with MI. Furthermore, we demonstrated that the GRACE risk model had a higher prognostic value than the TIMI RS in predicting long-term mortality.
Although previously used clinical parameters have de-fined risk of ischemic events or death after ACS6,7 stratification of the risk of ACS using tools such as risk scores has contributed to a change in practice and improved outcomes. Nevertheless, both the TIMI and GRACE RSs are derived from studies mainly enrolling patients from Western countries, and both were developed initially only to assess short-term prognoses. Not much was known about their generalizability to patients of Asian ethnicity and the comparative accuracy of these RSs in predicting long-term prognoses in such populations. The TIMI RS (range 0-14) was derived from patients with STEMI who were eligible for thrombolysis in the Intravenous nPA for Treatment of Infarcting Myocardium II trial (InTIME II),4 including eight variables of differing weights. It was shown to provide good discrimination of mortality at 30 days (C-statistic 0.779), and it was later applied to a community-based population of consecutive patients with STEMI in the National Registry of Myocardial Infarction-3 (NRMI-3) with similar prognostic capacity (C-statistic 0.74).8 The more commonly used TIMI RS for unstable angina and NSTEMI (range 0-7) was derived and validated from two trials: TIMI 11B and Efficacy and Safety of Subcutaneous Enoxaparin in Unstable Angina and Non-Q-Wave MI (ESSENCE).3 It consists of seven equally-weighted, dichotomous variables. Although the model was shown to demonstrate reasonable discriminative performance for death or recurrent cardiac events at 14 days (C-statistic 0.65), it was less useful in a real-world dataset with time points at 28 days and 1 year (C-statistics 0.59 and 0.61, respectively).9 The GRACE RS was derived from a large registry of patients across the entire spectrum of ACS and is the preferred RS recommended by the European Society of Cardiology.1 Its performance in discriminating in-hospital mortality was validated using an external dataset from the Global Use of Strategies to Open Occluded Coronary Arteries IIb (GUSTO-IIb; C-statistic 0.79) trial,5 and was intended to assess mortality at 6 months.10 In this study, we extended the clinical applicability of both RSs by demonstrating a fair to good discriminatory accuracy in predicting both short-term and long-term major adverse cardiac events in a cohort of Asian patients with MI.
Compared with patients in the GRACE registry,5 our patients tended to be older, more often male, have higher prevalence rates of diabetes and hypertension, a lower prevalence of hypercholesterolemia, and a higher prevalence of previous stroke. In addition, our cohort was more likely to present with heart failure, ST-segment depression in NSTEMI, positive troponin I and elevated serum creatinine on admission, revealing a significantly higher risk profile (Table 1). There are several possible reasons for the high-risk characteristics of our study population. First, this study was conducted at Taipei Veterans General Hospital, where the patient population consists primarily of elderly men. This may also explain why the average age was higher than in other studies. Hypertension and diabetes are more common in the elderly. Although the prevalence of diabetes in our patients was high, it is comparable to that reported in Japan.11 The higher serum creatinine level on admission may reflect the greater prevalence of risk factors for atherosclerosis (except for hyperlipidemia) and advanced age of our cohort. Second, we restricted our analysis to only patients with STEMI or NSTEMI, but not those with unstable angina who are a much lower risk group than those with MI. Third, unique features with regards to the risk factors and metabolic abnormalities in cardiovascular disease have been reported in Asia.12,13 For example, hypertension plays a more important role in the development of heart disease and stroke in Asia than in Western countries, and Asian countries have disproportionately high rates of morbidity and mortality from stroke compared to Western countries.12,13 In addition, the prevalence rates of diabetes cigarette smoking are high in Asian men. Nevertheless, mean cholesterol levels are lower in most Asian countries than in Western countries. Analysis of the INTERHEART study on the risk of a first acute myocardial infarction among Asians demonstrated that mean low-density lipoprotein cholesterol levels were about 10 mg/dl lower in Asians compared with non-Asians.14 All of these distinctive features were present in our study population.
Median RS values can be interpolated for a particular population, thereby providing another simple measure of baseline risk profiles. It has also been applied as a framework for comparisons of outcomes among different clinical trials. For patients with STEMI, the median values of the TIMI RS (25th and 75th percentiles) were 3 (1, 4) in the In TIME II trial, 4 (2, 6) in the NRMI-3 registry,15 and 5 (3, 7) in our patients. For patients with NSTEMI, the median TIMI RS was 3 (3, 4) in the derivation trial,3 and 4 (3, 6) in our patients. The median GRACE RS of our patients (164) was also much higher than that of patients enrolled in the GRACE registry (138), and even that of the patients ineligible for enrollment (151).16 Even though our cohort had a worse status, the in-hospital mortality rate in our study was 6.9%, which is comparable to that calculated from the prediction algorithm developed by the GRACE model (the estimated probabilities of in-hospital death with GRACE scores of 160 and 170 are 5.4% and 7.3%, respectively).5 At 1 year, the mortality rate was 12.0%, which is similar to that reported in a French population with a lower median GRACE RS of 113,17 and lower than that (20%) described in a community-based cohort.9 At 3 years, the mortality rate was 17.6% in our study, again lower than that (25.0%) reported in an unselected population with ACS with a median GRACE RS of 116.18
The main limitation of the GRACE RS is its apparent "complexity" compared to other risk models. However, it has been shown that the GRACE RS is superior in predicting in-hospital and 6-month mortality compared with the TIMI RS in unstable patients with angina/NSTEMI.19 Likewise, in our study, the GRACE risk model was somewhat superior to the TIMI score in predicting all-cause mortality and triple endpoints at all of the analyzed time points, and significantly better than the TIMIRS in predicting long-term mortality.
In patients with STEMI, one major difference between the TIMI and GRACE RSs is the inclusion of serum creatinine at admission, which may explain the superiority of the GRACE RS in predicting long-term outcomes. Renal impairment has been shown to independently predict higher in-hospital,20 short-term (90 days21 and 180 days2), and long-term morbidity and mortality23 after ACS. Of note, in patients with documented left ventricular impairment after MI, even mild renal dysfunction (creatinine clearance < 75 mL/minute per 1.73 m2) can be a strong, independent predictor of mortality and cardiovascular complications, and this risk has been shown to increase proportionally with the decline in renal function.23 The GRACE algorithm does not only include renal impairment but also treats it as a continuous variable along with age, heart rate, and blood pressure, thus allowing for a more refined prognostic prediction. For patients with NSTEMI, the GRACE RS also incorporates Killip class/CHF, systolic blood pressure, heart rate and renal dysfunction. In contrast, the TIMI RS is only composed of dichotomous variables and has a limited range of 0-7, which may result in a trade-off between its ease of use and predictive accuracy.
Strengths and limitations
The present study was limited by being a single-center retrospective analysis. However, it represents a real-world unselected population of consecutive patients with MI using contemporary management strategies.
CONCLUSIONS
The use of RSs developed from databases of clinical trials (TIMI) or registries (GRACE) for the risk stratification of patients with ACS in Western countries revealed fair to good discriminatory accuracy in predicting major adverse cardiac events in a cohort of Asian patients with MI. The performance of both scores held up well for long-term (up to 3 years) outcomes. Compared with the simpler TIMI RS, the GRACE risk model provided better predictive accuracy of long-term death among the patients presenting with both subsets of MI.
Acknowledgments
We thank Pui-Ching Lee for assistance with statistical analysis and Dr. Kuo-Liong Chien for comments on the data analysis.
CONFLICT OF INTEREST
None declared.
REFERENCES
- 1.Bassand JP, Hamm CW, Ardissino D, et al. Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: the Task Force for Diagnosis and Treatment of Non-ST-Segment Elevation Acute Coronary Syndromes of European Society of Cardiology. Eur Heart J. 2007;28:1598–1560. doi: 10.1093/eurheartj/ehm161. [DOI] [PubMed] [Google Scholar]
- 2.Kushner FG, Hand M, Smith SC, Jr., et al. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;54:2205–2241. doi: 10.1016/j.jacc.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 3.Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA. 2000;284:835–842. doi: 10.1001/jama.284.7.835. [DOI] [PubMed] [Google Scholar]
- 4.Morrow DA, Antman EM, Charlesworth A, et al. TIMI risk score for ST-elevation myocardial infarction: a convenient, bedside, clinical score for risk assessment at presentation: an intravenous nPA for treatment of infarcting myocardium early II trial sub-study. Circulation. 2000;102:2031–2037. doi: 10.1161/01.cir.102.17.2031. [DOI] [PubMed] [Google Scholar]
- 5.Granger CB, Goldberg RJ, Dabbous O, et al. Global Registry of Acute Coronary Events Investigators. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163:2345–2353. doi: 10.1001/archinte.163.19.2345. [DOI] [PubMed] [Google Scholar]
- 6.Chu CY, Lin TH, Lai WT. The management and prognostic factors of acute coronary syndrome: evidence from the Taiwan Acute Coronary Syndrome Full Spectrum Registry. Acta Cardiol Sin. 2017;33:329–338. doi: 10.6515/ACS20161205A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wei CC, Lee SH. Predictors of mortality in elderly patients with non-ST elevation acute coronary syndrome - data from Taiwan Acute Coronary Syndrome Full Spectrum Registry. Acta Cardiol Sin. 2017;33:377–383. doi: 10.6515/ACS20170126A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morrow DA, Antman EM, Parsons L, et al. Application of the TIMI risk score for ST-elevation MI in the National Registry of Myocardial Infarction 3. JAMA. 2001;286:1356–1359. doi: 10.1001/jama.286.11.1356. [DOI] [PubMed] [Google Scholar]
- 9.Singh M, Reeder GS, Jacobsen SJ, et al. Scores for post-myocardial infarction risk stratification in the community. Circulation. 2002;106:2309–2314. doi: 10.1161/01.cir.0000036598.12888.de. [DOI] [PubMed] [Google Scholar]
- 10.Fox KA, Dabbous OH, Goldberg RJ, et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE). BMJ. 2006;333:1091–1094. doi: 10.1136/bmj.38985.646481.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ogawa H, Kojima S. Modern state of acute myocardial infarction in the interventional era: observational case–control study–Japanese acute coronary syndrome study (JACSS). J Cardiol. 2009;54:1–9. doi: 10.1016/j.jjcc.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 12.Yusuf S, Reddy S, Ôunpuu S, Anand S. Global Bburden of cardiovascular diseases: part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001;104:2855–2864. doi: 10.1161/hc4701.099488. [DOI] [PubMed] [Google Scholar]
- 13.Sasayama S. Heart disease in Asia. Circulation. 2008;118:2669–2671. doi: 10.1161/CIRCULATIONAHA.108.837054. [DOI] [PubMed] [Google Scholar]
- 14.Karthikeyan G, Teo KK, Islam S, et al. Lipid profile, plasma apolipoproteins, and risk of a first myocardial infarction among Asians:an analysis from the INTERHEART Study. J Am Coll Cardiol. 2009;53:244–253. doi: 10.1016/j.jacc.2008.09.041. [DOI] [PubMed] [Google Scholar]
- 15.Morrow DA, Antman EM, Murphy SA, et al. The risk score profile: a novel approach to characterising the risk of populations enrolled in clinical studies. Eur Heart J. 2004;25:1139–1145. doi: 10.1016/j.ehj.2004.04.036. [DOI] [PubMed] [Google Scholar]
- 16.Steg PG, López-Sendón J, Lopez de Sa E, et al. GRACE Investigators. External validity of clinical trials in acute myocardial infarction. Arch Intern Med. 2007;167:68–73. doi: 10.1001/archinte.167.1.68. [DOI] [PubMed] [Google Scholar]
- 17.Schiele F, Meneveau N, Seronde MF, et al. Compliance with guidelines and 1-year mortality in patients with acute myocardial infarction: a prospective study. Eur Heart J. 2005;26:873–880. doi: 10.1093/eurheartj/ehi107. [DOI] [PubMed] [Google Scholar]
- 18.Tang EW, Wong CK, Herbison P. Global Registry of Acute Coronary Events (GRACE) hospital discharge risk score accurately predicts long-term mortality post acute coronary syndrome. Am Heart J. 2007;153:29–35. doi: 10.1016/j.ahj.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 19.Aragam KG, Tamhane UU, Kline-Rogers E, et al. Does simplicity compromise accuracy in ACS risk prediction? A retrospective analysis of the TIMI and GRACE risk scores. PLoS One. 2009;4:e7947. doi: 10.1371/journal.pone.0007947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santopinto JJ, Fox KA, Goldberg RJ, et al. GRACE Investigators. Creatinine clearance and adverse hospital outcomes in patients with acute coronary syndromes: findings from the Global Registry of Acute Coronary Events (GRACE). Heart. 2003;89:1003–1008. doi: 10.1136/heart.89.9.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reddan DN, Szczech L, Bhapkar MV, et al. Renal function, concomitant medication use and outcomes following acute coronary syndromes. Nephrol Dial Transplant. 2005;20:2105–2112. doi: 10.1093/ndt/gfh981. [DOI] [PubMed] [Google Scholar]
- 22.Al Suwaidi J, Reddan DN, Williams K, et al. GUSTO-IIb, GUSTO-III, PURSUIT. Global Use of Strategies to Open Occluded Coronary Arteries. Platelet Glycoprotein IIb/IIIa in Unstable Angina: Receptor Suppression Using Integrilin Therapy; PARAGON-A Investigators. Platelet IIb/IIIa Antagonism for the Reduction of Acute coronary syndrome events in a Global Organization Network. Prognostic implications of abnormalities in renal function in patients with acute coronary syndromes. . Circulation. 2002;106:974–980. doi: 10.1161/01.cir.0000027560.41358.b3. [DOI] [PubMed] [Google Scholar]
- 23.Anavekar NS, McMurray JJ, Velazquez EJ, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351:1285–1295. doi: 10.1056/NEJMoa041365. [DOI] [PubMed] [Google Scholar]


