Abstract
Background
High blood pressure (BP) is a common chronic disease needs long life drug consumption to control. Spironolactone could be used as the fourth-line therapy in patients with resistant hypertension. However, there is no study to determine the effects of low dose spironolactone as a first line therapy in treatment of essential hypertension. The aim of this study is to investigate the effect of low dose spironolactone monotherapy in management of essential hypertension.
Methods
In this double blind randomized clinical trial, 40 patients who had stage I essential hypertension were randomly divided into two groups: intervention group received spironolactone 25 milligram once daily for one month and control group received placebo once daily. At the baseline and after one month, 24-hour BP holter-monitoring and serum potassium assay were done.
Results
Systolic BP was reduced from 143.5 ± 8.2 mmHg to 137.10 ± 7.57 mmHg in the intervention group, while it did not change significantly in control (between group treatment difference = -4.5 mmHg, p = 0.004). There was no significant reduction of diastolic BP in the intervention group in comparison to placebo group (between group treatment difference = -1.3 mmHg, p = 0.099).
Conclusions
Short course monotherapy with low dose spironolactone is effective in reducing systolic BP in patients with stage I essential hypertension.
Keywords: Aldosterone antagonist, Hypertension, Monotherapy, Spironolactone
INTRODUCTION
Hypertension is one of the most common chronic diseases and public health problems worldwide.1,2 High blood pressure (BP) is an important preventable and modifiable cause of death that affects more than a quarter of all adults and over half of those over the age of 65 years.1,3,4 It has a detrimental effect on endothelial function5-7 and can lead to various end-organ damages.8,9 The World Health Organization predicts that about 600 million people worldwide have high blood pressure and 5.7 million of them will die because of this illness and its complications.10 Some researchers have estimated that 19.4% to 27% of Iranians have hypertension.11-13
Hypertension is classified into two main categories: ~80-95% of patients are diagnosed as having "essential" hypertension (also referred to as primary or idiopathic hypertension). In the remaining 5-20% of cases, a specific underlying disorder causing the elevation of blood pressure can be identified.14-16
There are different classes of antihypertensive medications including angiotensin-converting enzyme (ACE)-inhibitors, angiotensin receptor blockers (ARB), calcium channel blockers and thiazide-type diuretics that can be used as a first line agent in the treatment of hypertension.
Spironolactone is an aldosterone antagonist and a potassium-sparing diuretic that has been used for treatment of hyperaldosteronism and edematous states including congestive heart failure, nephrotic syndrome and liver cirrhosis. Recently, the British Hypertension Society guidelines suggest that spironolactone could be used as the fourth-line therapy in patients that have resistant hypertension.17,18
Several studies have investigated the positive effect of spironolactone in resistant hypertension.19-21 However, there has been no study to determine the effects of low-dose spironolactone as a first-line therapy in the treatment of essential hypertension. The aim of the present study is to determine the effect of low-dose spironolactone monotherapy in the management of essential hypertension.
METHODS
Trial design
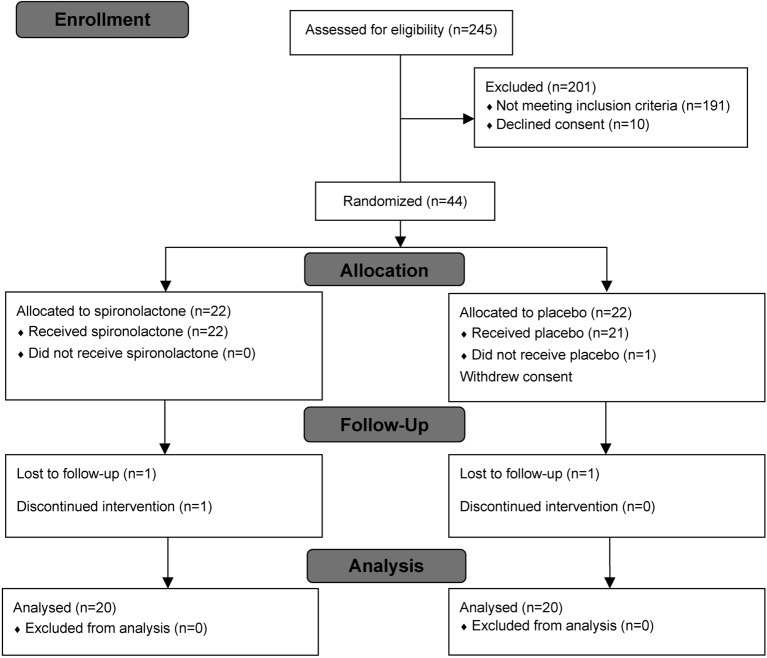
This study was a pilot, randomized, double-blind, placebo-controlled clinical trial conducted from December 2014 to May 2015 on 40 patients with essential hypertension. Figure 1 shows the CONSORT flow diagram of the study. The Medical Ethics Committee of Shiraz University of Medical Sciences approved the protocol of the study, and written informed consent was obtained from each participant. The trial was registered at the Iranian registry of clinical trials (www.IRCT.ir) under the registration number IRCT201502011525N6.
Figure 1.
CONSORT 2010 flow diagram for this randomized, double-blinded, placebo controlled clinical trial of effects of spironolactone on systolic and diastolic BP in patients with stage one essential hypertension.
Patients
Eligible patients with newly diagnosed stage I essential hypertension were referred to Imam Reza clinic, Shiraz University of Medical Sciences, Shiraz, Iran. The patients with office blood pressure recording of systolic BP = 140-159 mmHg and/or diastolic BP = 90-99 mmHg, and documented 24-hour BP holter monitoring (mean systolic blood pressure ≥ 135 mmHg and/or mean diastolic blood pressure ≥ 85 mmHg) were enrolled. Exclusion criteria were serum creatinine ≥ 2 mg/dl, serum potassium ≥ 5 meq/l, past history of renal or endocrine diseases, and diabetic patients.
Interventions and outcomes
Patients were randomly divided into two groups: the case group received spironolactone 25 mg once daily for one month and the control group received a placebo (starch) as indistinguishable capsules once a day. During treatment all patients were on a low-sodium diet. After one month, 24-hour BP holter monitoring was repeated as a primary outcome. Collection and analyses of all clinical and laboratory data were performed by study personnel blinded for group assignment.
Randomization
Patients were randomized into two groups, the intervention group (n = 20) and control group (n = 20). Study capsules were allocated in separate packs blinded and labeled using a four-digit code. The information regarding which codes corresponded to which treatment was maintained by the project coordinator. Apart from the project coordinator, the patients, the staff involved at the clinical center, and members tasked with collecting and analyzing the data were blinded to the intervention allocation.
Statistical analysis
All data are represented as mean ± SD. The Mann-Whitney test, paired t-test, and Wilcoxon test were used to compare different variables. Because of the possibility of a relationship between serum potassium levels and activity of the renin-angiotensin-aldosterone system, we decided to perform separate analysis of the effect of spironolactone on blood pressure reduction in patients with low-normal and high-normal serum potassium levels. p < 0.05 was considered statistically significant. All the statistical analysis was done by the statistical Package for Social Sciences version 17.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Forty patients were enrolled in the study and categorized into two groups: intervention (n = 20) and control (n = 20). Baseline demographic data of the patients are displayed in Table 1.
Table 1. Baseline characteristics of participants.
| Characteristics | Intervention group (n = 20) | Control group (n = 20) | p value |
| Age (years) | 51.95 ± 7.34 | 51.80 ± 6.02 | 0.51 |
| Sex | 0.11 | ||
| Male (%) | 15 (75%) | 12 (60%) | |
| Female (%) | 5 (25%) | 8 (40%) | |
| BMI (kg/m2) | 27.6 ± 2.4 | 27.2 ± 2.3 | 0.43 |
| Serum potassium (mEq/l) | 4.20 ± 0.44 | 4.10 ± 0.49 | 0.515 |
| Serum creatinine (mg/dl) | 1.09 ± 0.18 | 1.20 ± 0.22 | 0.071 |
| Lipid profiles | |||
| Total cholesterol (mg/dl) | 234.1 ± 33 | 242 ± 38.4 | 0.09 |
| TG (mg/dl) | 194.5 ± 28.2 | 208.1 ± 45.7 | 0.55 |
| LDL (mg/dl) | 144.1 ± 22 | 147.8 ± 35.1 | 0.34 |
| HDL (mg/dl) | 48.3 ± 10.2 | 46.1 ± 11.8 | 0.68 |
| Baseline drugs | |||
| Aspirin, no. (%) | 2 (10%) | 3 (15%) | 0.25 |
| Statin, no. (%) | 4 (20%) | 3 (15%) | 0.32 |
| Antihypertensive drugs, no. | 0 | 0 | - |
BMI, body mass index; HDL, high-density lipoprotein; LDL, low-density lipoprotein; TG, triglyceride.
According to Table 2, the means of systolic and diastolic BP before treatment were not significantly different in the case and control groups at baseline. Moreover, systolic BP reduction in the case group was significantly more in comparison to the control group (p = 0.004). There was also a trend toward reduction of diastolic BP in the control group in comparison to the case group (p = 0.099).
Table 2. Mean and standard deviation of average of 24-hour ambulatory systolic and diastolic blood pressures before and after treatment.
| Characteristics | Placebo group (n = 20) | Spironolactone group (n = 20) | Treatment difference | p-value | ||
| Baseline | 1 months | Baseline | 1 months | |||
| Blood pressure indices | ||||||
| Systolic blood pressure (mmHg) | 143.70 ± 9.31 | 141.05 ± 9.64 | 143.55 ± 8.23 | 137.10 ± 7.57 | -4.5 | < 0.001 |
| Diastolic blood pressure (mmHg) | 85.55 ± 7.44 | 83.60 ± 5.74 | 89.50 ± 4.69 | 87.15 ± 4.69 | -1.3 | 0.099 |
| Subgroups based on potassium level | ||||||
| SBP in patients with K ≥ 4.2 | 146.87 ± 7.98 | 144.25 ± 8.27 | 142.91 ± 8.25 | 137.16 ± 7.45 | -4.95 | < 0.001 |
| SBP in patients with K < 4.2 | 141.55 ± 9.85 | 138.91 ± 10.2 | 144.55 ± 8.66 | 137.00 ± 8.26 | -3.7 | 0.016 |
| DBP in patients with K ≥ 4.2 | 89.50 ± 6.78 | 85.37 ± 6.34 | 89.83 ± 4.91 | 86.33 ± 4.49 | -2.37 | 0.014 |
| DBP in patients with K < 4.2 | 82.91 ± 6.89 | 82.41 ± 5.24 | 89.00 ± 6.69 | 88.37 ± 5.01 | 0.87 | 0.295 |
| SBP in patients with K ≥ 4.0 | 146.50 ± 6.77 | 143.75 ± 6.86 | 144.23 ± 9.21 | 137.05 ± 7.85 | -5.14 | < 0.001 |
| SBP in patients with K < 4.0 | 139.50 ± 11.3 | 137.00 ± 12.1 | 142.28 ± 6.47 | 135.28 ± 7.22 | -3.28 | 0.078 |
| DBP in patients with K ≥ 4.0 | 87.66 ± 6.38 | 85.08 ± 5.43 | 90.46 ± 5.22 | 86.84 ± 4.68 | -2.96 | 0.001 |
| DBP in patients with K < 4.0 | 82.37 ± 8.19 | 81.37 ± 5.80 | 87.71 ± 6.07 | 87.71 ± 5.02 | 1.78 | 0.058 |
DBP, diastolic blood pressure; SBP, systolic blood pressure.
There was no linear relationship between the baseline serum potassium level and the amount of systolic and diastolic BP reduction in the case group (p = 0.147 and p = 0.127 respectively).
Also, we divided patients in the case group into two subgroups in terms of serum potassium levels: potassium levels lower than or equal to 4.2, and more than 4.2. There was no difference in the amount of systolic and diastolic BP reductions between the two subgroups (p = 0.223 and p = 0.315 respectively).
DISCUSSION
Here, we have shown that low-dose spironolactone can reduce elevated systolic blood pressure levels and this effect is not affected by baseline serum potassium level.
Hypertension is a common chronic disease worldwide that is difficult to treat due to the need for long-term drug consumption and poor compliance of patients. There are different types of antihypertensive medications but none of them are optimal and combination therapy is usually needed to reach goal BP.
Spironolactone is an aldosterone antagonist and a potassium-sparing diuretic. It is widely used in the management of congestive heart failure and other edematous states.22,23 Its use in the treatment of hypertension is limited to an adjuvant therapy for resistant hypertension.24,25 There are some studies on spironolactone in the treatment of resistant hypertension. From a total of 25 patients with resistant hypertension prospectively enrolled in a study conducted by Ouzan et al., 23 participants had a clinical BP below 140/90 mmHg and significant reduction in ambulatory blood pressure monitoring after spironolactone (1 mg/kg/day) was added for one month to the existing regimen. They concluded that spironolactone is a safe and effective treatment for patients with resistant hypertension.19 Another study by Nishizaka et al. revealed that adding low-dose spironolactone (12.5 up to 50 mg daily) to multidrug regimens that included a diuretic and an ACE inhibitor or ARB provides significant additive BP reduction in African-American and white subjects with resistant hypertension with and without primary aldosteronism.20 In 2007 Lane et al. described how spironolactone, at a low dose, is an effective add-in drug in patients with hypertension resistant to a regimen including an angiotensin-blocking agent. The reduction of systolic and diastolic blood pressure was statistically significant.25 Although a double-blind, placebo-controlled study in 2011 emphasized that spironolactone is an effective drug for lowering systolic BP in patients with resistant arterial hypertension, the fall of diastolic BP value was not significant (p = 0.079). This effect on diastolic BP is compatible with ours.26
The role of spironolactone in monotherapy has yet to be fully investigated. Most previous studies used a high dose of the drug for treatment of hypertension. Jeunemaitre et al. evaluated the long-term efficacy and tolerance of spironolactone in essential hypertension among 20,815 patients. 182 patients were treated with high dose spironolactone as monotherapy (mean dose of 95.5 mg). Systolic and diastolic BP were decreased 18 and 10 mmHg, respectively. The plasma creatinine level increased modestly, as did the plasma potassium level. Fasting blood glucose and cholesterol levels didn’t change, and triglyceride increased slightly. Also, their results showed that these changes were similar in both sexes and were not influenced by length of follow-ups. They concluded that administration of daily spironolactone effectively reduces BP without inducing adverse metabolic effects in patients with essential hypertension.27 The only study that used low-dose sprinolactone was conducted in 1966 by Wolf and his collegues.28 In their dose determining study, they assigned patients with hypertension three doses of spironolactone (25 mg daily, 100 mg daily, and 200 mg daily) with or without hydrochlorothiazide. 21 patients who received low-dose spironolactone without hydrochlorothiazide, compared to a placebo, showed a 10.5 and 9.9 mmHg reduction in systolic and diastolic blood pressures, respectively. However, none of these differences were statistically significant. In a systematic review of 5 trials, it was shown that spironolactone appears to lower blood pressure compared to a placebo to a similar degree in patients with primary (essential) hypertension when doses of 100-500 mg/day are given. There may be a dose-response effect with spironolactone up to 50 mg/day. However, doses > 50 mg/day do not produce further reductions in either systolic blood pressure (SBP) or diastolic blood pressure (DBP). The authors concluded that: "Given the lack of a dose-response, coupled with a possible increased risk in adverse events with higher doses, doses of 25 to 100 mg/day are reasonable".29 In another meta-analysis on eplerenone, again it was shown that a low dose of 25 mg was ineffective, and doses of 50 to 200 mg/day lowered blood pressure in people with essential hypertension by 9.21 mmHg systolic and 4.18 mmHg diastolic compared to a placebo, with no difference of effect between doses of 50 mg/day to 200 mg/day.30 In the present study, for the first time, we showed efficacy for a low dose (25 mg daily) of spironolactone as a monotherapy. This treatment reduced systolic blood pressure significantly in patients with stage one essential hypertension (mean reduction was 6.45 mmHg). This effect was independent of the level of baseline serum potassium. Also there was a trend to reduce diastolic blood pressure (mean reduction = 2.35 mmHg).
In our study, no side effects (such as gynecomastia and menstrual irregularities) were seen in the patients who received spironolactone and it was well tolerated. In contrast with our findings, Chapman et al. reported gynecomastia or breast discomfort and biochemical abnormalities (principally hyperkalemia) as the most frequent spironolactone adverse events in 6% and 2% of participants, respectively.21 In another study on resistant hypertension, spironolactone was discontinued because of hyperkalemia in 4.1% of the cases. A total of 18% of all patients had adverse effects, which in 9.9% led to discontinuation of the drug, and a total of 5.2% of the males developed gynecomastia.31 Absence of side effects in our study may be related to the lower number of enrolled patients and the shorter duration of follow up.
Activation of aldosterone acts as one of the final steps of the renin-angiotensin-aldosterone system (RAAS) and by stimulating mineralocorticoid receptors in the heart and kidneys, circulating aldosterone may contribute to the development of cardiac and renal fibrosis in hypertension.32 Consequently, an aldosterone receptor blockade may help protect from renal and cardiovascular fibrosis. In addition, the modern high-salt diets interfere significantly with the actions of ACE inhibitor and ARBs by continually inhibiting feedback of the RAAS. Suppression of serum aldosterone triggers sequestration of epithelial sodium channels by endocytosis and increased renal sodium excretion. Thereby, it will shrink plasma volume and may help protect against salt-sensitive hypertension.32
Our study faces some limitations. First of all, as a pilot study, we used a low sample volume and a short duration of treatment. So this study cannot truly reflect the possible side effects which may occur with long-term spironolactone therapy. Furthermore, results should be reevaluated in larger studies with long-term follow ups to see whether these blood pressure-reducing effects can be translated into a reduction in major cardiovascular events.
CONCLUSIONS
In conclusion, monotherapy with low dose spironolactone is effective in reducing BP in patients with stage I essential hypertension and is well tolerated.
Acknowledgments
The present article was extracted from the thesis written by Dr. Amir-Abbas Sadeghi and was financially supported by Shiraz University of Medical Science grants No. 5874.
The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran and also Center for Development of Clinical Research of Nemazee Hospital and Dr. Nasrin Shokrpour for editorial assistance.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
REFERENCES
- 1.Sarafidis PA, Bakris GL. Resistant hypertension:an overview of evaluation and treatment. J Am Coll Cardiol. 2008;52:1749–1757. doi: 10.1016/j.jacc.2008.08.036. [DOI] [PubMed] [Google Scholar]
- 2.Chiang CE, Wang TD, Lin TH, et al. The 2017 focused update of the guidelines of the Taiwan Society of Cardiology (TSOC) and the Taiwan Hypertension Society (THS) for the management of hypertension. Acta Cardiol Sin. 2017;33:213–225. doi: 10.6515/ACS20170421A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krause T, Lovibond K, Caulfield M, et al. Management of hypertension:summary of NICE guidance. BMJ. 2011;343:d4891. doi: 10.1136/bmj.d4891. [DOI] [PubMed] [Google Scholar]
- 4.Babaee Beigi MA, Zibaeenezhad MJ, Aghasadeghi K, et al. The effect of educational programs on hypertension management. Int J Cardiovasc Res J. 2014;8:94. [PMC free article] [PubMed] [Google Scholar]
- 5.Attar A, Aghasadeghi K, Parsanezhad ME, et al. Absence of correlation between changes in the number of endothelial progenitor cell subsets. Korean Circ J. 2015;45:325–332. doi: 10.4070/kcj.2015.45.4.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Attar A, Khosravi Maharlooi M, Khoshkhou S, et al. Colony forming unit endothelial cells do not exhibit telomerase alternative splicing variants and activity. Iran Biomed J. 2013;17:146–151. doi: 10.6091/ibj.1100.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parsanezhad ME, Attar A, Namavar-Jahromi B, et al. Changes in endothelial progenitor cell subsets in normal pregnancy compared with preeclampsia. J Chin Med Assoc. 2015;78:345–352. doi: 10.1016/j.jcma.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 8.Attar A, Eslaminejad MB, Tavangar MS, et al. Dental pulp polyps contain stem cells comparable to the normal dental pulps. J Clin Exp Dent. 2014;6:e53–e59. doi: 10.4317/jced.51305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iman A, Akbar MA, Mohsen KM, et al. Comparison of intradermal injection of autologous epidermal cell suspension vs. spraying of these cells on dermabraded surface of skin of patients with post-burn hypopigmentation. Indian J Dermatol. 2013;58:240. doi: 10.4103/0019-5154.110844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Poulter NR, Prabhakaran D, Caulfield M. Hypertension. Lancet. 386:801–812. doi: 10.1016/S0140-6736(14)61468-9. [DOI] [PubMed] [Google Scholar]
- 11.Rahimi K, Emdin CA, MacMahon S. The epidemiology of blood pressure and its worldwide management. Circ Res. 2015;116:925–936. doi: 10.1161/CIRCRESAHA.116.304723. [DOI] [PubMed] [Google Scholar]
- 12.Aghajani M, Ajorpaz NM, Atrian MK, et al. Effect of self-care education on quality of life in patients with primary hypertension: comparing lecture and educational package. Nurs Midwifery Stud. 2013;2:71–76. doi: 10.5812/nms.11655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sahraian A, Mokhtari M, Moaref A, et al. Hypertensive patients and normotensive individuals: differences in anger inventory. Int Cardiovasc Res J. 2015;9:216–219. [Google Scholar]
- 14.Messerli FH, Williams B, Ritz E. Essential hypertension. Lancet. 2007;370:591–603. doi: 10.1016/S0140-6736(07)61299-9. [DOI] [PubMed] [Google Scholar]
- 15.Carretero OA, Oparil S. Essential hypertension part I: definition and etiology. Circulation. 2000;101:329–335. doi: 10.1161/01.cir.101.3.329. [DOI] [PubMed] [Google Scholar]
- 16.Williams B, Poulter N, Brown M, et al. Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004—BHS IV. J Hum Hypertens. 2004;18:139–185. doi: 10.1038/sj.jhh.1001683. [DOI] [PubMed] [Google Scholar]
- 17.Batterink J, Stabler SN, Tejani AM, Fowkes CT. Spironolactone for hypertension. Cochrane Database Syst Rev. 2010;8 doi: 10.1002/14651858.CD008169.pub2. [DOI] [PubMed] [Google Scholar]
- 18.Ouzan J, Pérault C, Lincoff AM, et al. The role of spironolactone in the treatment of patients with refractory hypertension. Am J Hypertens. 2002;15:333–339. doi: 10.1016/s0895-7061(01)02342-1. [DOI] [PubMed] [Google Scholar]
- 19.Nishizaka MK, Zaman MA, Calhoun DA. Efficacy of low-dose spironolactone in subjects with resistant hypertension. Am J Hypertens. 2003;16:925–930. doi: 10.1016/s0895-7061(03)01032-x. [DOI] [PubMed] [Google Scholar]
- 20.Chapman N, Dobson J, Wilson S, et al. Effect of spironolactone on blood pressure in subjects with resistant hypertension. Hypertension. 2007;49:839–845. doi: 10.1161/01.HYP.0000259805.18468.8c. [DOI] [PubMed] [Google Scholar]
- 21.Soberman JE, Weber KT. Spironolactone in congestive heart failure. Curr Hypertens Rep. 2000;2:451–456. doi: 10.1007/s11906-000-0027-x. [DOI] [PubMed] [Google Scholar]
- 22.Qavi AH, Kamal R, Schrier RW. Clinical use of diuretics in heart failure, cirrhosis, and nephrotic syndrome. Int J Nephrol. 2015;2015 doi: 10.1155/2015/975934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Engbaek M, Hjerrild M, Hallas J, Jacobsen IA. The effect of low-dose spironolactone on resistant hypertension. J Am Soc Hypertens. 2010;4:290–294. doi: 10.1016/j.jash.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 24.Sternlicht H, Bakris GL. Spironolactone for resistant hypertension-hard to resist? Lancet. 2015;386:2032–2034. doi: 10.1016/S0140-6736(15)00264-0. [DOI] [PubMed] [Google Scholar]
- 25.Lane DA, Shah S, Beevers DG. Low-dose spironolactone in the management of resistant hypertension: a surveillance study. J Hypertens. 2007;25:891–894. doi: 10.1097/HJH.0b013e328014954d. [DOI] [PubMed] [Google Scholar]
- 26.Václavík J, Sedlák R, Plachý M, et al. Addition of spironolactone in patients with resistant arterial hypertension (ASPIRANT) a randomized, double-blind, placebo-controlled trial. Hypertension. 2011;57:1069–1075. doi: 10.1161/HYPERTENSIONAHA.111.169961. [DOI] [PubMed] [Google Scholar]
- 27.Jeunemaitre X, Chatellier G, Kreft-Jais C, et al. Efficacy and tolerance of spironolactone in essential hypertension. Am J Cardiol. 1987;60:820–825. doi: 10.1016/0002-9149(87)91030-7. [DOI] [PubMed] [Google Scholar]
- 28.Wolf RL, Mendlowitz M, Roboz J, et al. Treatment of hypertension with spironolactone. Double-blind study. JAMA. 1966;198:1143–1149. [PubMed] [Google Scholar]
- 29.Batterink J, Stabler SN, Tejani AM, Fowkes CT. Spironolactone for hypertension. Cochrane Database Syst Rev. 2010;(8):CD008169. doi: 10.1002/14651858.CD008169.pub2. [DOI] [PubMed] [Google Scholar]
- 30.Tam TS, Wu MH, Masson SC, et al. Eplerenone for hypertension. Cochrane Database Syst Rev. 2017;2:CD008996. doi: 10.1002/14651858.CD008996.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Engbaek M, Hjerrild M, Hallas J, Jacobsen IA. The effect of low-dose spironolactone on resistant hypertension. J Am Soc Hypertens. 2010;4:290–294. doi: 10.1016/j.jash.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 32.Briet M, Schiffrin EL. Vascular actions of aldosterone. J Vasc Res. 2012;50:89. doi: 10.1159/000345243. [DOI] [PubMed] [Google Scholar]