Introduction
Recently, pulmonary vein isolation (PVI) with cryoballoon (CB) has been widely accepted as treatment for atrial fibrillation (AF). Especially, second-generation CB (Arctic Front Advance, Medtronic, Inc, Minneapolis, MN) has a high cooling effect, which can achieve durable lesions of pulmonary vein (PV) antrum and better clinical outcomes.1 On the other hand, several complications, such as esophageal erosions and phrenic nerve injuries, have been reported with AF ablation using second-generation CB.2 Lehrmann and colleagues3 have reported a case of near-fatal coronary artery spasm during PVI using second-generation CB. In this case, the mechanism of coronary artery spasm was speculated as cryoenergy-induced blood cooling, which was attributable to the close proximity between the CB and coronary artery spasm site.
We experienced a case in which coronary artery spastic occlusion occurred in the distal right coronary artery during CB application at the left common PV, far from the coronary spasm site.
Case report
A 67-year-old man with paroxysmal AF and history of stroke was referred to our hospital for catheter ablation of AF. He did not have any episodes of vasospastic angina and had not been prescribed any drugs that have a potential to induce coronary artery spasm, such as a beta-blocker. PVI was performed with a second-generation CB catheter under sedation with dexmedetomidine and fentanyl. Left atriography after transseptal approach revealed the left common PV (Figure 1). We scheduled CB ablation of the left common PV with multiple CB applications at the upper and lower portions of the left common PV antrum. One CB application consisted of a 3-minute freezing. The heart rhythm at the start of the left PVI was AF. At 121 seconds after the onset of the third freezing at the upper potion following 2 CB applications at the upper and lower left PV, the patient complained of chest pain, and 12-lead electrocardiogram (ECG) showed prolonged QRS width in all leads and ST elevation in inferior leads (Figure 2). At this time, the thermometer of the CB catheter showed −44°C. Although systolic blood pressure was kept at 120 mm Hg, heart rhythm showed AF bradycardia with heart rate 40 beats/minute, which was suggested to be mediated by a vagal response. Coronary angiography (CAG) showed the occlusion of the right coronary artery, and this coronary occlusion, chest pain, and ECG changes were eliminated rapidly by the intracoronary administration of isosorbide dinitrate (Figures 2 and 3). There was no evident finding suggesting any air or thrombotic embolism during the procedure. Therefore, we concluded that the cause of coronary occlusion was coronary spasm by the procedural course. The left common PV was not isolated with the series of freezing, and was finally isolated with additional radiofrequency applications. Each superior and inferior right PV was isolated with CB ablation with a single 3-minute freezing. After the occurrence of initial coronary spasm, no coronary event occurred during the procedure. After the PV isolation, CAG did not show any occlusion or stenosis in the left and right coronary arteries. We performed a cold finger test on the day after ablation, but no symptoms or ECG changes suggesting vasospastic angina were provoked. The patient has not experienced any episode of AF recurrence or vasospastic angina more than 1 year after ablation.
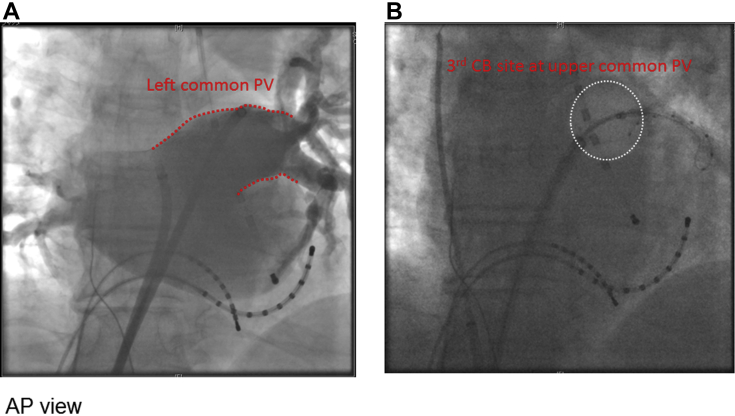
Figure 1.
A: Result of left atriography. Left pulmonary vein (PV) shows common form. B: Cryoballoon (CB) positioning at the upper site of left common PV. White dotted circle indicates the CB positioning at the upper site of left common PV. AP = anteroposterior.
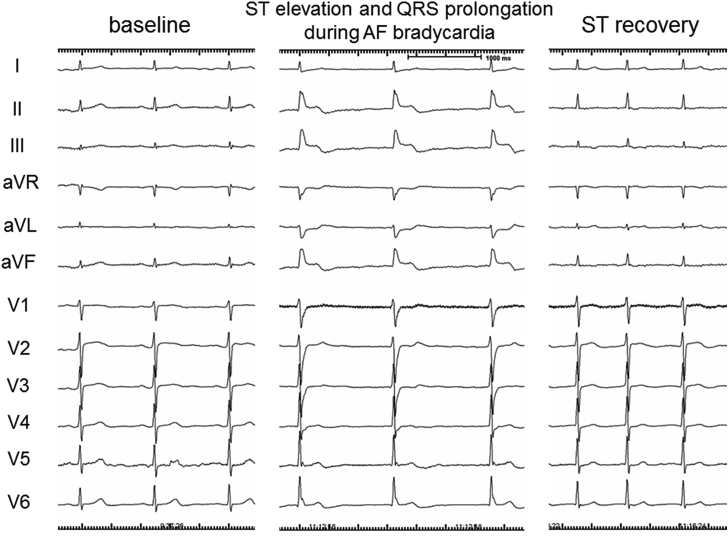
Figure 2.
Time course of 12-lead electrocardiogram (ECG). The heart rhythm at the start of the procedure was sinus rhythm. After completion of the third cryoballoon application at upper site of the left pulmonary vein, ST segment elevation in inferior leads and QRS width prolongation in all leads occurred, accompanied by atrial fibrillation bradycardia. These ECG changes were eliminated after the resolution of coronary spastic occlusion with intracoronary administration of isosorbide dinitrate. AF = atrial fibrillation.
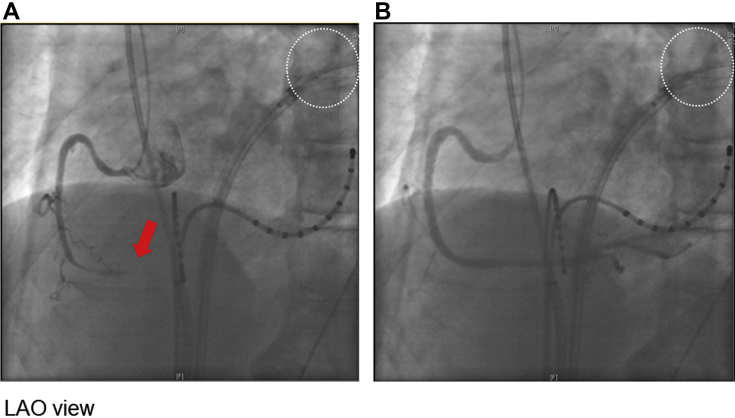
Figure 3.
A: Occlusion of right coronary artery after third cryoballoon (CB) application. B: Recanalization of right coronary artery with intracoronary administration of isosorbide dinitrate. Red arrow indicates the coronary occlusion site; white dotted circle indicates the CB positioning at the upper site of the left common pulmonary vein. LAO = left anterior oblique.
Discussion
Coronary artery spasm is a rare but potentially fatal complication associated with CB ablation. Some cases with a cryoenergy-induced coronary artery spasm by CB ablation and cryocatheter ablation were reported.3, 4 These reports speculated the cause of coronary artery spasm as a cryoenergy-induced blood cooling. However, the coronary spasm site was not necessarily close to the cryoapplication site, and an indirect effect owing to blood cooling was suggested. In the present case, the coronary artery spasm site (distal right coronary artery) was far away from the CB application site (upper site of left PV). It is difficult to speculate that a direct blood-cooling effect in the left atrium could reach the right coronary artery, which is located at the epicardial right atrioventricular groove. Therefore, other than a direct blood-cooling effect by cryoenergy should be considered as the cause of coronary vasospasm.
Vagally mediated response is an important mediator of coronary vasospasm.5 It is known that neurosurgical procedures might induce coronary vasospasm via the vagally mediated response.6 The cranial junction of the left PV and left atrium is known to be the location of superior left ganglionated plexi (GP). Vagal reaction, such as vagally mediated bradycardia or asystole, can occur during ablation near GP with both radiofrequency ablation and cryoenergy ablation.7 Therefore, it is possible to speculate that the cause of coronary artery spasm was the vagally mediated effect via left superior GP by CB application. Actually, the heart rhythm during right coronary spastic occlusion showed AF bradycardia, which was suggested to be mediated with the vagal effect via left superior GP.
On the other hand, we could not completely deny that right coronary artery spasm and ischemia of the inferior wall was induced by some other cause, and the vagal response occurred consequently as merely a “result” of consecutive events. Moreover, the detailed mechanism of coronary artery spasm is unknown in the present case. We thought that the cause of coronary vasospasm was not thromboembolism because CAG performed just after ECG change did not show a thromboembolic shape and coronary occlusion was rapidly released by intracoronary administration of isosorbide dinitrate. However, we could not deny the possibility that microthrombus or air embolism caused coronary vasospastic occlusion by the clinical course.
These cases, including the present case, suggest that we should pay attention to monitoring the ischemic change in 12-lead ECG during the procedure, and should consider the patient selection for CB ablation, especially the patients with vasospastic angina. At least, we should avoid the cessation of antivasospastic angina agents, such as calcium channel blocker, in the periprocedural period of CB ablation in patients diagnosed with vasospastic angina.
Key Teaching Points.
-
•
Coronary vasospasm can occur during pulmonary vein isolation with cryoballoon (CB) ablation.
-
•
Because the trigger of coronary vasospasm might not necessarily be a cryoenergy-induced blood cooling, the coronary vasospasm might occur far away from the CB site.
-
•
We should pay attention to monitoring the ischemic change in the 12-lead electrocardiogram during the procedure. At least, we should avoid the cessation of antivasospastic angina agents in the periprocedural period of CB ablation in patients diagnosed with vasospastic angina.
References
- 1.Ciconte G., de Asmundis C., Sieira J. Single 3-minute freeze for second-generation cryoballoon ablation: one-year follow-up after pulmonary vein isolation. Heart Rhythm. 2015;12:673–680. doi: 10.1016/j.hrthm.2014.12.026. [DOI] [PubMed] [Google Scholar]
- 2.Su W., Kowal R., Kowalski M., Metzner A., Svinarich J.T., Wheelan K., Wang P. Best practice guide for cryoballoon ablation in atrial fibrillation: the compilation experience of more than 3000 procedures. Heart Rhythm. 2015;12:1658–1666. doi: 10.1016/j.hrthm.2015.03.021. [DOI] [PubMed] [Google Scholar]
- 3.Lehrmann H., Potocnik C., Comberg T., Peck W., Salama A., Schneider J., Park C.I., Jadidi A.S., Weber R., Arentz T. Near-fatal coronary artery spasm during cryoballoon pulmonary vein isolation: an unreported complication. Circ Arrhythm Electrophysiol. 2014;7:1273–1274. doi: 10.1161/CIRCEP.114.001788. [DOI] [PubMed] [Google Scholar]
- 4.Miyazaki S., Ichihara N., Takagi T., Iesaka Y. Coronary artery spasm during cryothermal cavotricuspid isthmus ablation. J Cardiovasc Electrophysiol. 2015;26:1019–1020. doi: 10.1111/jce.12657. [DOI] [PubMed] [Google Scholar]
- 5.Waters D.D., Miller D.D., Bouchard A., Bosch X., Theroux P. Circadian variation in variant angina. Am J Cardiol. 1984;54:61–64. doi: 10.1016/0002-9149(84)90304-7. [DOI] [PubMed] [Google Scholar]
- 6.Chowdhury T., Meuwly C., Sandu N., Cappellani R.B., Schaller B. Coronary spasm in neurosurgical patients and role of trigeminocardiac reflex. Neurol Res Int. 2014;2014:974930. doi: 10.1155/2014/974930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peyrol M., Barraud J., Koutbi L., Maille B., Trevisan L., Martinez E., Lévy S., Paganelli F., Franceschi F. Vagal reactions during cryoballoon-based pulmonary vein isolation: A clue for autonomic nervous system modulation? Biomed Res Int. 2016 doi: 10.1155/2016/7286074. http://dx.doi.org/10.1155/2016/7286074. [DOI] [PMC free article] [PubMed] [Google Scholar]